PHARMACOLOGY II QUIZ
ATI PHARMACOLOGY II QUIZ
Total Questions : 60
Showing 10 questions Sign up for moreWhich instruction is most appropriate for a client who is prescribed pancrelipase (Cotazym)?
Explanation
A) Increase dosing with a large meal:
Increasing the dosing with a large meal may not be appropriate as it could lead to overdosing and potential side effects. The dosage of pancrelipase should be determined by the healthcare provider based on the individual's needs and response to treatment.
B) Take the medication at least 2 hours prior to meals:
Taking the medication prior to meals may not be effective as the enzymes will not be available when food is consumed, which defeats the purpose of enzyme replacement therapy. The enzymes need to be present simultaneously with the food to aid in digestion.
C) Take the medication with meals.
Pancrelipase, such as Cotazym, is a pancreatic enzyme replacement therapy used to aid in the digestion of fats, proteins, and carbohydrates in individuals with pancreatic insufficiency. Taking the medication with meals is crucial because it helps to ensure that the enzymes are available to aid in the digestion of food. Without proper enzyme supplementation during meals, individuals with pancreatic insufficiency may experience malabsorption, leading to nutritional deficiencies and gastrointestinal symptoms.
D) Decrease fluid intake:
Decreasing fluid intake is not appropriate as it could lead to dehydration and may not have any significant impact on the efficacy of pancrelipase. In fact, adequate fluid intake is important for digestion and overall health.
An adult patient presents to the emergency department with complaints of shortness of breath and increased work of breathing.
Assessment
The patient is alert and oriented times 3, skin is pink, warm and dry. BP 148/88, T98, P92. R 24, pulse oximetry 91% on room air. Assessment of the lung reveals expiratory wheezing throughout the lung fields.
The physician orders an albuterol nebulizer. What assessments should the nurse plan to complete after administering the albuterol?
(Select All that Apply.)
Explanation
A. Respiratory rate and pulse: Albuterol is a bronchodilator medication commonly used to relieve bronchospasm in conditions like asthma and chronic obstructive pulmonary disease (COPD). Monitoring the patient's respiratory rate and pulse is essential to assess the response to the medication and any potential adverse effects.
B. Pulse oximetry: Albuterol helps to open the airways and improve oxygenation in patients with bronchospasm. Monitoring oxygen saturation using pulse oximetry provides valuable information about the patient's respiratory status and response to treatment.
C. Capillary refill: Capillary refill is typically assessed to evaluate peripheral perfusion and circulation. While it is an important assessment in certain clinical situations, it is not directly related to monitoring the response to albuterol administration.
D. Glucose: Glucose monitoring is not typically indicated after administering albuterol nebulizer unless the patient has a history of diabetes or there are specific concerns regarding glucose levels.
E. Lung sounds: Assessing lung sounds before and after administering albuterol helps to evaluate the effectiveness of the medication in relieving bronchospasm. Improvement in lung sounds, such as decreased wheezing or clearer breath sounds, indicates a positive response to treatment.
Which instruction is most appropriate for a client who is prescribed pancrelipase (Cotazym)?
Explanation
A) Increase dosing with a large meal:
Increasing the dosing with a large meal may not be appropriate as it could lead to overdosing and potential side effects. The dosage of pancrelipase should be determined by the healthcare provider based on the individual's needs and response to treatment. There's no evidence to support the need for increased dosing with larger meals.
B) Take the medication at least 2 hours prior to meals:
Taking the medication prior to meals may not be effective as the enzymes will not be available when food is consumed, which defeats the purpose of enzyme replacement therapy. The enzymes need to be present simultaneously with the food to aid in digestion. Waiting 2 hours before meals would mean the enzymes are not available when needed.
C) Take the medication with meals.
Pancrelipase, such as Cotazym, is a pancreatic enzyme replacement therapy used to aid in the digestion of fats, proteins, and carbohydrates in individuals with pancreatic insufficiency. Taking the medication with meals is crucial because it helps ensure that the enzymes are available to aid in the digestion of food. Without proper enzyme supplementation during meals, individuals with pancreatic insufficiency may experience malabsorption, leading to nutritional deficiencies and gastrointestinal symptoms.
D) Decrease fluid intake:
Decreasing fluid intake is not appropriate as it could lead to dehydration and may not have any significant impact on the efficacy of pancrelipase. In fact, adequate fluid intake is important for digestion and overall health. There's no indication that fluid intake needs to be decreased when taking pancrelipase.
An ulcer caused by H. pylori can be successfully treated with which classification of drugs?
Explanation
A) H2-receptor blockers:
H2-receptor blockers, such as ranitidine and famotidine, are used to reduce the production of stomach acid. While they can provide symptomatic relief for ulcers by reducing acid secretion, they do not directly treat the underlying cause of the ulcer, which is the H. pylori infection.
B) Antacids:
Antacids are medications that neutralize stomach acid and can provide temporary relief from ulcer symptoms such as pain and discomfort. However, they do not eradicate the H. pylori bacteria or address the root cause of the ulcer. Antacids only provide symptomatic relief rather than treating the infection.
C) Proton-pump inhibitors:
Proton-pump inhibitors (PPIs), such as omeprazole and pantoprazole, are potent acid-suppressing medications that are commonly used to treat ulcers and gastroesophageal reflux disease (GERD). While they can help in ulcer healing by reducing acid secretion and providing symptomatic relief, they are not effective in eradicating H. pylori infection. PPIs are often used in combination with antibiotics for H. pylori eradication therapy, but they are not the primary treatment on their own.
D) Antibiotics.
H. pylori (Helicobacter pylori) is a bacteria that commonly infects the stomach lining and is a major cause of gastric and duodenal ulcers. Antibiotics are the primary treatment for H. pylori infection. The antibiotics kill the bacteria, allowing the ulcer to heal. Common antibiotics used to treat H. pylori include amoxicillin, clarithromycin, metronidazole, and tetracycline.
Which type of laxative causes peristalsis by irritating the bowel?
Explanation
A) Stool softener:
Stool softeners, such as docusate sodium, work by adding moisture to the stool, making it softer and easier to pass. They do not directly stimulate bowel movements or peristalsis through irritation of the bowel lining.
B) Saline/osmotic laxative:
Saline or osmotic laxatives, such as magnesium hydroxide (milk of magnesia) and polyethylene glycol (PEG), work by drawing water into the intestines, which softens the stool and increases bowel motility. They do not primarily act by irritating the bowel lining.
C) Stimulant laxative.
Stimulant laxatives work by directly stimulating the nerves in the intestines, which increases the rhythmic contractions of the intestines (peristalsis) and promotes bowel movements. These medications irritate the bowel lining, leading to increased motility and expulsion of stool. Examples of stimulant laxatives include bisacodyl and senna.
D) Bulk-forming laxative:
Bulk-forming laxatives, such as psyllium and methylcellulose, work by increasing the bulk and water content of the stool, which stimulates bowel movements. They do not directly irritate the bowel lining to promote peristalsis. Instead, they absorb water and swell in the intestines, creating a larger, softer stool that is easier to pass.
A client has been diagnosed with pancreatic insufficiency. Which treatment option does the nurse anticipate for this client?
Explanation
A) Treatment with PPIs to decrease stomach acid:
Proton-pump inhibitors (PPIs) are used to decrease stomach acid production and are commonly prescribed for conditions such as gastroesophageal reflux disease (GERD) and peptic ulcers. However, they do not address the underlying cause of pancreatic insufficiency, which is the deficiency of pancreatic enzymes.
B) Treatment with stimulant laxatives:
Stimulant laxatives are used to stimulate bowel movements and are not indicated for the treatment of pancreatic insufficiency. Pancreatic insufficiency primarily affects the digestion of nutrients rather than bowel motility.
C) Replacement therapy with pancreatic enzymes.
Pancreatic insufficiency occurs when the pancreas does not produce enough digestive enzymes to properly digest food, leading to malabsorption of nutrients. Replacement therapy with pancreatic enzymes is the mainstay of treatment for pancreatic insufficiency. These enzymes, often prescribed in the form of pancreatic enzyme replacement therapy (PERT), help to supplement the deficient enzymes and aid in the digestion of fats, proteins, and carbohydrates.
D) Decrease food intake:
Decreasing food intake is not an appropriate treatment for pancreatic insufficiency. In fact, individuals with pancreatic insufficiency may need to increase their food intake to compensate for malabsorption and ensure adequate nutrition. Restricting food intake would worsen nutritional deficiencies and symptoms associated with malabsorption.
A nurse is reinforcing teaching to a school-age child who has asthma. Which of the following medications should the nurse instruct the child to use to abort an ongoing attack?
Explanation
A) Montelukast:
Montelukast is a leukotriene receptor antagonist (LTRA) used as a controller or maintenance medication for asthma. It is not used for the immediate relief of asthma symptoms during an acute attack. Montelukast is taken regularly to prevent asthma symptoms and reduce the frequency of asthma attacks, but it does not provide rapid relief during an ongoing attack.
B) Fluticasone:
Fluticasone is an inhaled corticosteroid (ICS) used as a controller medication for asthma. It works by reducing airway inflammation and is taken regularly to control asthma symptoms and prevent exacerbations. Fluticasone is not used for the immediate relief of acute asthma symptoms and is not suitable for aborting an ongoing asthma attack.
C) Cromolyn:
Cromolyn is a mast cell stabilizer used as a controller medication for asthma. It helps prevent the release of inflammatory substances that contribute to asthma symptoms. Cromolyn is taken regularly to prevent asthma symptoms and reduce the frequency of asthma attacks but is not used for the immediate relief of acute asthma symptoms like albuterol.
D) Albuterol.
Albuterol is a short-acting beta agonist (SABA) bronchodilator used for the quick relief of asthma symptoms during an acute asthma attack or exacerbation. It works rapidly to relax the smooth muscles in the airways, opening them up and relieving bronchoconstriction, which improves airflow and alleviates symptoms such as wheezing, shortness of breath, and chest tightness. Albuterol is typically administered via inhalation through a metered-dose inhaler (MDI) or a nebulizer.
A nurse is caring for a client who has asthma. The client asks the nurse how albuterol helps his breathing. Which of the following information should the nurse include in the response? (Select all that apply.)
Explanation
A. The medication will relieve wheezing: Albuterol is a short-acting beta agonist bronchodilator that works by quickly relaxing the smooth muscles of the airways, leading to rapid bronchodilation. This helps relieve symptoms such as wheezing, shortness of breath, and chest tightness commonly associated with asthma exacerbations.
B. The medication will reduce inflammation: Albuterol is not primarily indicated for reducing inflammation in asthma. While it can help alleviate symptoms of bronchospasm, it does not target the underlying inflammation associated with asthma.
C. The medication will increase the amount of mucus: Albuterol does not increase mucus production. In fact, it is a bronchodilator medication that primarily targets airway smooth muscle relaxation and bronchodilation to improve airflow and relieve symptoms.
D. The medication will decrease coughing episodes: Albuterol can help decrease coughing episodes by relieving bronchospasm and improving airflow. However, its primary mechanism of action is bronchodilation rather than directly targeting coughing.
E. The medication will open the airways: Albuterol works by stimulating beta-2 adrenergic receptors in the airway smooth muscles, resulting in relaxation of these muscles and dilation of the bronchial tubes. This action helps to open the airways, allowing for improved airflow and easier breathing.
The patient's family is asking questions about the medications used in the treatment for shock. The nurse explains that dopamine is one of the drugs being used and that it works:
(Select All that Apply.)
Explanation
A. At high doses, to treat anaphylaxis: Dopamine is not used to treat anaphylaxis. Anaphylaxis is typically managed with medications such as epinephrine, antihistamines, and corticosteroids.
B. At high doses, to increase cardiac output: Dopamine is a medication commonly used in the treatment of shock, particularly in cases of hypotension. At higher doses, dopamine acts as a positive inotrope and increases cardiac contractility, thereby improving cardiac output and increasing blood pressure.
C. At low doses, to cause increased blood flow to the kidneys: At lower doses, dopamine primarily acts on dopaminergic receptors in the renal vasculature, leading to vasodilation of the renal blood vessels and increased renal perfusion. This can help improve renal blood flow and urine output, making it beneficial in cases of renal hypoperfusion or acute kidney injury.
D. At low doses, to treat anaphylaxis: Dopamine is not used to treat anaphylaxis at any dose. Anaphylaxis is managed with medications such as epinephrine, which acts on multiple receptors to reverse the systemic effects of the allergic reaction.
E. To cause vasoconstriction and increase blood pressure: Dopamine can also cause vasoconstriction, particularly at higher doses. This effect is mediated through its action on alpha-adrenergic receptors, leading to peripheral vasoconstriction and an increase in systemic vascular resistance, which in turn helps increase blood pressure.
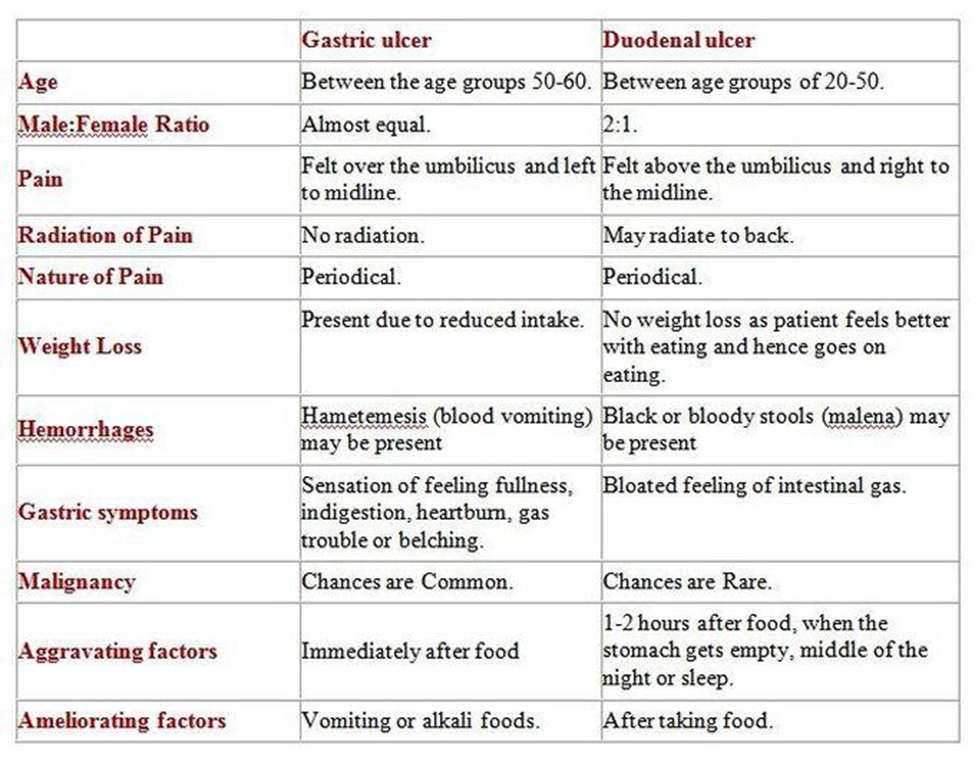
What symptom is more common to a duodenal ulcer than a gastric ulcer?
Explanation
A) Nighttime pain:
Nighttime pain, also known as nocturnal pain, is a symptom associated with both duodenal and gastric ulcers. It occurs when the stomach or duodenal lining is empty and no food is present to buffer the effect of gastric acid. While nighttime pain can occur in both types of ulcers, it is not more specific to duodenal ulcers compared to gastric ulcers.
B) Anorexia:
Anorexia, or loss of appetite, can occur in both duodenal and gastric ulcers due to factors such as pain, discomfort, and inflammation. It is not a symptom that is more commonly associated with one type of ulcer over the other.
C) Postprandial pain (occurring after a meal).
Postprandial pain, which occurs after a meal, is more commonly associated with duodenal ulcers than gastric ulcers. This pain typically occurs 2 to 3 hours after eating, as it is often triggered by the release of gastric acid and duodenal contractions stimulated by food intake. Duodenal ulcers tend to cause this type of pain because they are located in the duodenum, the first part of the small intestine, which is exposed to gastric acid and bile after a meal.
D) Nausea and vomiting:
Nausea and vomiting can occur in both duodenal and gastric ulcers, particularly if the ulcer is accompanied by complications such as obstruction or perforation. These symptoms are not more specific to duodenal ulcers compared to gastric ulcers.
You just viewed 10 questions out of the 60 questions on the ATI PHARMACOLOGY II QUIZ Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



