PN FUNDAMENTALS UPDATED 2023
ATI PN FUNDAMENTALS UPDATED 2023
Total Questions : 41
Showing 10 questions Sign up for moreA nurse on a medical-surgical unit is caring for a group of clients. Which of the following findings should the nurse identify as a safety hazard?
Explanation
Choice A reason: A weight-sensitive sensor mat is a device that alerts the staff when a client tries to get out of bed. It is not a safety hazard, but rather a safety measure to prevent falls.
Choice B reason: A buzzing sensation at the application site of a transcutaneous electrical nerve stimulation unit is normal and expected. It indicates that the unit is delivering electrical impulses to the nerves and muscles. It is not a safety hazard, but rather a therapeutic intervention for pain relief.
Choice C reason: A capillary refill of less than 2 seconds is normal and indicates adequate blood circulation. It is not a safety hazard, but rather a sign of good perfusion.
Choice D reason: Raising all four side rails of a client's bed is a safety hazard because it increases the risk of injury if the client tries to climb over them. It also restricts the client's mobility and may cause feelings of isolation and imprisonment. It is a violation of the client's rights and dignity.
A nurse is preparing to insert an indwelling urinary catheter and is verifying the client’s express consent for this procedure. Which of the following actions should the nurse take?
Explanation
Choice A reason: Witnessing the client’s signature on a consent form is not necessary for an indwelling urinary catheter insertion, which is a routine and noninvasive procedure. The nurse only needs to witness the signature for invasive or high-risk procedures that require written consent.
Choice B reason: Obtaining verbal consent from the client is the appropriate action for the nurse to take before inserting an indwelling urinary catheter. The nurse should explain the purpose, benefits, risks, and alternatives of the procedure and ensure that the client understands and agrees to it.
Choice C reason: Having another nurse co-sign the client’s consent is not required for an indwelling urinary catheter insertion, which is a routine and noninvasive procedure. The nurse only needs to have another nurse co-sign the consent for procedures that involve blood transfusions, organ donations, or research participation.
Choice D reason: Checking the medical record for the client’s signature on a previous consent form is not sufficient for verifying the client’s express consent for an indwelling urinary catheter insertion. The nurse should obtain a new consent for each procedure, as the client has the right to change their mind or refuse the treatment at any time.
A nurse is collecting data regarding home safety from a client who is prone to falls. Which of the following findings should the nurse recognize as placing the client at additional risk?
Explanation
Choice Areason: Removing the wheels from rolling chairs is a good practice to prevent the chairs from sliding or moving unexpectedly. It is not a risk factor for falls, but rather a safety measure to prevent them.
Choice Breason: A stool riser is a device that elevates the toilet seat and makes it easier for the client to sit down and stand up. It is not a risk factor for falls, but rather a safety measure to prevent them.
Choice C reason: Having the mattress directly on the floor may make it harder for the client to get in and out of bed, but it does not increase the risk of falls. In fact, it may reduce the risk of injury if the client falls from the bed, as the height is lower.
Choice D reason: Covering electrical cords with throw rugs is a risk factor for falls, as the client may trip over them or get tangled in them. It is also a fire hazard, as the rugs may overheat or catch fire from the cords. The nurse should advise the client to remove the rugs and secure the cords away from the walking areas.
A nurse is reinforcing teaching with a client about the use of a peak flow meter. Which of the following actions should the nurse take first?
Explanation
Choice A reason: Showing the client a video demonstration of peak flow meter use is a helpful teaching strategy, but it is not the first action that the nurse should take. The nurse should first assess the client's baseline knowledge and readiness to learn before providing any information or instruction.
Choice B reason: Observing the client using the peak flow meter is a way to evaluate the client's learning and skill, but it is not the first action that the nurse should take. The nurse should first determine the client's knowledge of the use of the peak flow meter and then teach the client how to use it correctly.
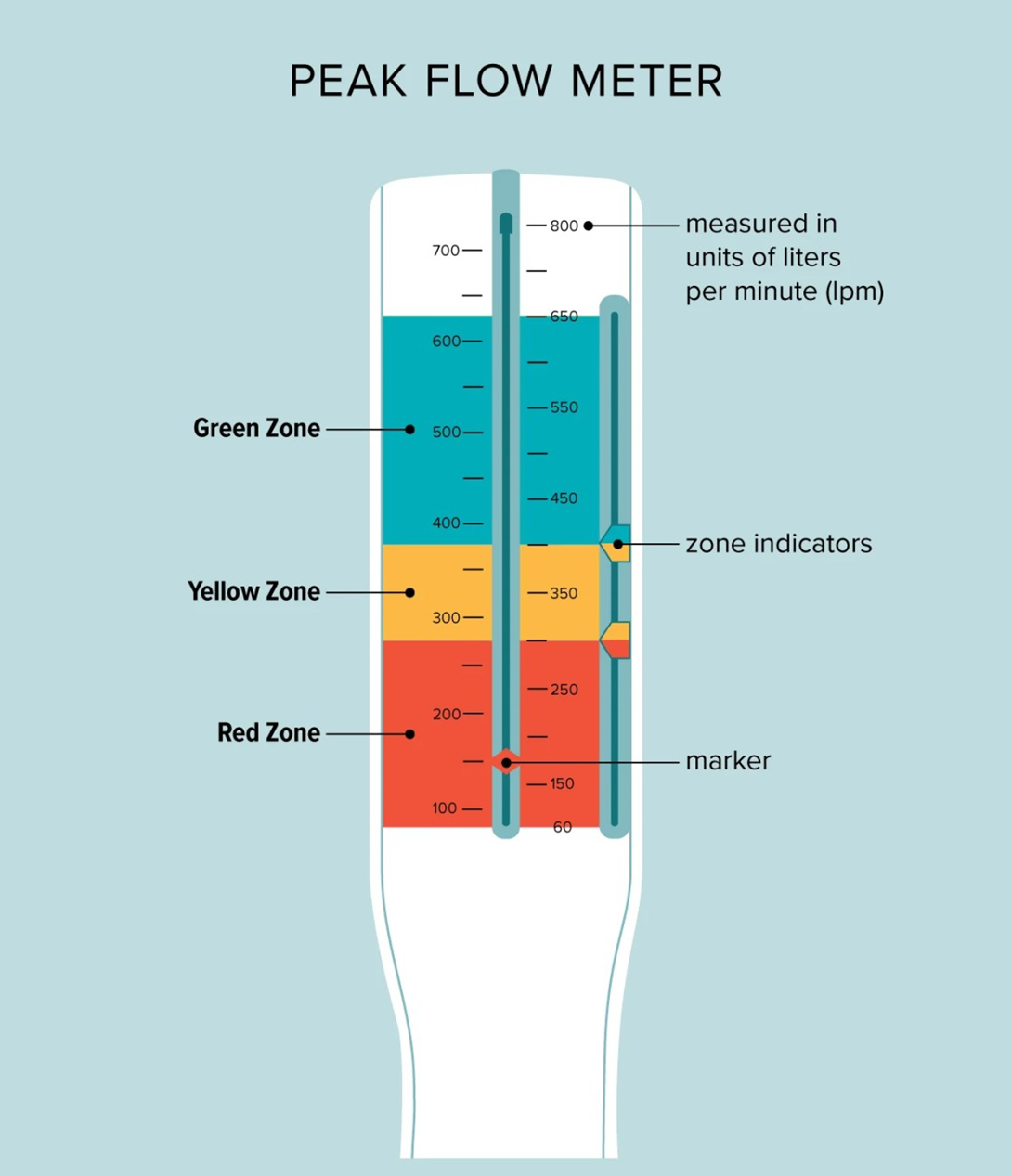
Choice C reason: Emphasizing the importance of the daily use of the peak flow meter is a way to motivate the client to adhere to the treatment plan, but it is not the first action that the nurse should take. The nurse should first assess the client's knowledge of the use of the peak flow meter and then explain the benefits and rationale of using it regularly.
Choice D reason: Determining the client's knowledge of the use of the peak flow meter is the first action that the nurse should take, as it follows the principle of the nursing process. The nurse should start with assessment, then proceed with planning, implementation, and evaluation. By assessing the client's knowledge, the nurse can identify the client's learning needs, gaps, and preferences, and tailor the teaching accordingly.
A nurse observes an assistive personnel (AP) perform mouth care for a client who is unconscious. Which of the following actions by the AP requires intervention by the nurse?
Explanation
The correct answer is d. Using two gloved fingers to open the client’s mouth for cleaning. This action is unsafe as it risks injury to both the AP and the client. A padded tongue blade should be used instead.
Choice A reason:
Using an oral care sponge swab moistened with cool water to clean the client’s mouth is appropriate. Oral care sponge swabs are designed to clean the mouth gently and effectively, especially for unconscious patients.
Choice B reason:
Wearing clean gloves to perform mouth care for the client is a standard precaution to prevent infection. Gloves protect both the caregiver and the patient from potential infections.
Choice C reason:
Lowering the side rail on the side of the bed where they will stand to perform mouth care is necessary to safely access the patient. It allows the AP to perform the task without straining or risking injury.
Choice D reason:
Using two gloved fingers to open the client’s mouth for cleaning is unsafe. This method can cause injury to the AP if the patient bites down reflexively. A padded tongue blade should be used to safely open the mouth.
A nurse on a medical-surgical unit is collecting data from a client who is postoperative following abdominal surgery. The client's BP was 125/85 mm Hg 15 min ago. The nurse now finds that the client’s BP is 176/96 mm Hg. Which of the following actions should the nurse take?
Explanation
Choice A reason: Using a narrower cuff to repeat the BP measurement is an incorrect action by the nurse, as it can result in a falsely high reading. The nurse should use a cuff that fits the client's arm size and circumference.
Choice B reason: Measuring the client's BP in the other arm is the correct action by the nurse, as it can help to confirm the accuracy of the reading and rule out any possible errors or variations. The nurse should compare the readings from both arms and report any significant differences to the provider.
Choice C reason: Deflating the cuff faster when repeating the BP measurement is an incorrect action by the nurse, as it can result in a falsely low reading. The nurse should deflate the cuff at a rate of 2 to 3 mm Hg per second.
Choice D reason: Requesting a prescription for an antihypertensive medication is an inappropriate action by the nurse, as it is premature and unnecessary. The nurse should first verify the BP reading and identify the possible causes of the elevation, such as pain, anxiety, or medication effects. The nurse should also implement nonpharmacological interventions, such as positioning, relaxation, and oxygen therapy, before administering any medication.
A nurse is performing a wound irrigation for a client who has methicillin-resistant Staphylococcus aureus. When removing personal protective equipment, which of the following pieces should the nurse remove first?
Explanation
Choice A reason: Gloves are the first piece of personal protective equipment that the nurse should remove, as they are the most contaminated and can transfer microorganisms to other surfaces. The nurse should remove the gloves by grasping the outside of one glove at the wrist and pulling it off inside out, then holding it in the gloved hand and sliding the fingers of the ungloved hand under the other glove at the wrist and pulling it off inside out over the first glove. The nurse should then discard the gloves in a biohazard container.
Choice B reason: Goggles are the second piece of personal protective equipment that the nurse should remove, as they can protect the eyes from splashes or droplets. The nurse should remove the goggles by grasping the earpieces or headband and lifting them away from the face. The nurse should then discard the goggles in a designated receptacle or place them in a designated area for reprocessing.
Choice C reason: Gown is the third piece of personal protective equipment that the nurse should remove, as it can protect the clothing and skin from contamination. The nurse should remove the gown by untying the neck and waist ties and pulling the gown away from the neck and shoulders, touching only the inside of the gown. The nurse should then turn the gown inside out, fold or roll it into a bundle, and discard it in a biohazard container.
Choice D reason: Mask is the last piece of personal protective equipment that the nurse should remove, as it can protect the nose and mouth from inhalation of microorganisms. The nurse should remove the mask by grasping the bottom ties or elastics and then the top ties or elastics and pulling the mask away from the face. The nurse should then discard the mask in a biohazard container.
A nurse is caring for a client who is 2 days postoperative following a below-the-knee amputation. Which of the following statements by the client should the nurse identify as indicating an acceptance of the limb loss?
Explanation
Choice A reason: This is the correct answer because it reflects acceptance of the limb loss and a positive coping strategy. This statement shows that the client is willing to take responsibility for the care of the residual limb and is ready to learn new skills. The other statements indicate denial, anger, or depression, which are normal stages of grief, but not acceptance.
Choice B reason: This is not the correct answer because it reflects denial of the limb loss and a reluctance to face the reality of the situation.
Choice C reason: This is not the correct answer because it reflects depression and a sense of helplessness and dependency.
Choice D reason: This is not the correct answer because it reflects anger and a difficulty in adjusting to the limb loss.
A nurse is providing teaching with a client who has severe arthritis and has difficulty with stairs. What should the nurse include in the teaching?
Explanation
Choice A reason: This is not the correct answer because it distracts the client from the surroundings and could cause loss of balance or coordination.
Choice B reason: This is the correct answer because it enables the client to use the handrails as a support and reduces the stress on the arms and shoulders.
Choice C reason: This is not the correct answer because it creates an uneven distribution of weight and could cause instability or pain.
Choice D reason: This is not the correct answer because it requires the client to shift the body weight abruptly and could cause muscle strain or joint damage.
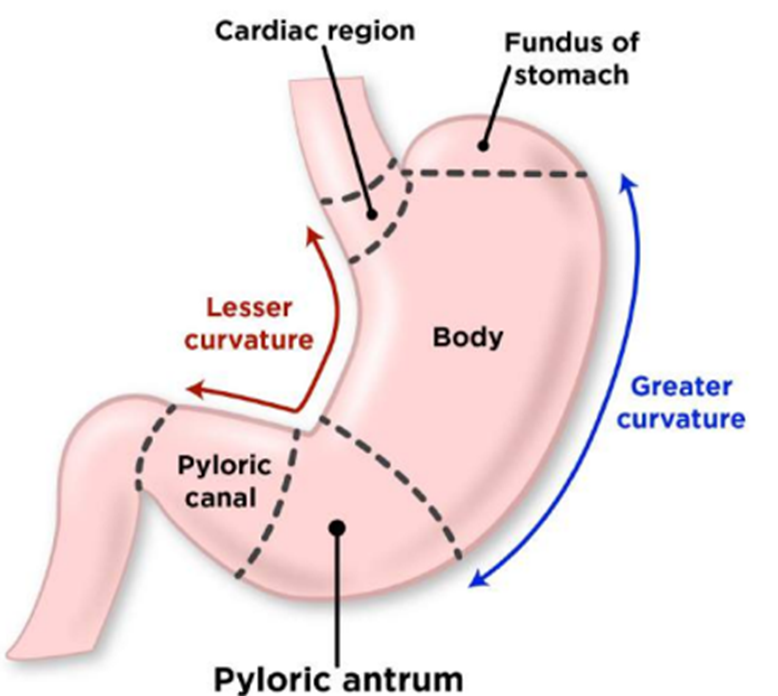
A nurse is collecting data from a client who has an NG tube in place for gastric decompression. Which of the following findings should the nurse report to the provider?
Explanation
Choice A reason: This is not the correct answer because greenish-yellow drainage is a normal color for gastric secretions and does not indicate a problem.
Choice B reason: This is not the correct answer because a report of hunger is common for a client with an NG tube and does not require intervention.
Choice C reason: This is the correct answer because gastric contents in the air vent mean that the NG tube is clogged or kinked and needs to be flushed or replaced. This is the correct answer because it indicates that the NG tube is not functioning properly and could cause aspiration or infection. The other findings are expected or normal for a client with an NG tube.
Choice D reason: This is not the correct answer because abdominal distention is a common reason for placing an NG tube and should improve with gastric decompression.
You just viewed 10 questions out of the 41 questions on the ATI PN FUNDAMENTALS UPDATED 2023 Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



