International College of Health Sciences ICHS OB Pediatrics s
International College of Health Sciences ICHS OB Pediatrics s
Total Questions : 72
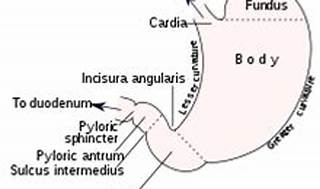
Showing 10 questions Sign up for moreThe nurse is caring for an infant with suspected pyloric stenosis. Which clinical manifestation would indicate pyloric stenosis?
Explanation
Explore
The correct answer is choice C. Visible peristalsis and weight loss.
Choice A rationale:
Abdominal rigidity and pain on palpation are not typically indicative of pyloric stenosis. These symptoms could be associated with a variety of other gastrointestinal conditions.
Choice B rationale:
A rounded abdomen and hypoactive bowel sounds are not specific to pyloric stenosis. These symptoms could be seen in various gastrointestinal disorders.
Choice C rationale:
Visible peristalsis and weight loss are classic symptoms of pyloric stenosis. The condition causes a narrowing of the opening from the stomach to the small intestine, preventing food from passing through. This leads to vomiting after feeding, persistent hunger, and weight loss since very little food passes to the small intestines.
Choice D rationale:
Distention of the lower abdomen and constipation are not typically indicative of pyloric stenosis. These symptoms could be associated with a variety of other gastrointestinal conditions.
Which intervention should be included in the plan of care for an infant with the nursing diagnosis of Excess Fluid Volume related to congestive heart failure?
Explanation
Choice A rationale:
Weighing the infant every day on the same scale at the same time is crucial in monitoring excess fluid volume in congestive heart failure. Sudden weight gain can indicate fluid retention, a common sign of worsening heart failure. Daily weight monitoring helps in early detection and timely intervention.
Choice B rationale:
Notifying the physician when weight gain exceeds more than 20 g/day might be too late for intervention. Daily weight monitoring is essential to detect trends and intervene promptly to manage excess fluid volume.
Choice C rationale:
Placing the infant in a car seat to minimize movement is not directly related to managing excess fluid volume in congestive heart failure. It is essential for safety during transportation but does not address the nursing diagnosis.
Choice D rationale:
Administering digoxin as ordered by the physician is a medical intervention for congestive heart failure. While important, the nursing diagnosis is related to excess fluid volume, and the focus should be on nursing interventions such as monitoring daily weights.
The nurse observes some children in the playroom. Which play situation exhibits the characteristics of parallel play?
Explanation
Choice A rationale:
Kimberly and Amanda sharing clay to each make things represents cooperative play, not parallel play. Cooperative play involves interaction and collaboration between children, whereas parallel play involves children playing side by side without interacting.
Choice B rationale:
Brian playing with his truck next to Kristina playing with her truck demonstrates parallel play. In parallel play, children play independently but alongside others, showing interest in what others are doing but without direct interaction.
Choice C rationale:
Adam playing a board game with Kyle, Steven, and Erich represents cooperative play, not parallel play. Cooperative play involves shared activities and collaboration, while parallel play involves independent activities in proximity to others.
Choice D rationale:
Danielle playing with a music box on her mother's lap is an example of solitary play, where a child plays alone without regard to others. Solitary play is common in younger children and is different from parallel play.
A parent asks the nurse why self-monitoring of blood glucose is being recommended for her child with diabetes. The nurse should base the explanation on what information?
Explanation
Choice A rationale:
Self-monitoring of blood glucose is not recommended primarily because it is a less expensive method of testing. The main reasons for self-monitoring include empowering the child to manage their diabetes, allowing for more frequent monitoring without hospital visits, and facilitating prompt adjustments in insulin or dietary intake.
Choice B rationale:
Self-monitoring of blood glucose can be quite accurate if done correctly. Accuracy depends on proper technique, calibration of the glucometer, and regular maintenance. It is comparable to laboratory testing when performed accurately.
Choice C rationale:
Children with diabetes need to learn to manage their condition as they grow older. Teaching them self-monitoring skills empowers them to take control of their health and make informed decisions about insulin dosages, dietary choices, and physical activity levels.
Choice D rationale:
While parental involvement is essential, self-monitoring of blood glucose is primarily about empowering the child to manage their diabetes. Parents play a supportive role in educating and supervising, but the child's active involvement is crucial for long-term management.
The nurse assessing a premature newborn infant auscultates a continuous machinery-like murmur. This finding is associated with which congenital heart defect?
Explanation
Choice A rationale:
Pulmonary stenosis is characterized by a systolic ejection murmur best heard at the upper left sternal border. It does not typically produce a continuous machinery-like murmur. Pulmonary stenosis results from narrowing at the pulmonary valve, obstructing blood flow from the right ventricle to the pulmonary artery.
Choice B rationale:
A continuous machinery-like murmur is characteristic of patent ductus arteriosus (PDA). PDA is a congenital heart defect where the ductus arteriosus, a fetal blood vessel that should close after birth, remains open, allowing continuous blood flow between the aorta and pulmonary artery. This murmur is often best heard in the left infraclavicular region.
Choice C rationale:
Ventricular septal defect (VSD) typically produces a harsh holosystolic murmur heard best at the lower left sternal border. VSD is a hole in the septum separating the ventricles, allowing blood to flow from the higher-pressure left ventricle to the lower-pressure right ventricle.
Choice D rationale:
Coarctation of the aorta causes a murmur due to increased blood flow across the aortic valve. However, this murmur is not continuous and is usually systolic and best heard in the back over the left scapula.
Which factor is most important in predisposing toddlers to frequent infections such as otitis media, tonsillitis, and upper respiratory tract infections?
Explanation
Choice A rationale:
Abdominal respirations do not directly predispose toddlers to frequent infections such as otitis media, tonsillitis, and upper respiratory tract infections. Abdominal respirations are a normal breathing pattern in toddlers, transitioning from the diaphragmatic breathing seen in infants. This change is due to the toddler's increased chest wall compliance and stronger intercostal muscles, facilitating more efficient breathing.
Choice B rationale:
Slower pulse and respiratory rates in toddlers compared to infants are part of normal physiological development. Toddler's heart rates range from 70 to 110 beats per minute, and respiratory rates range from 20 to 30 breaths per minute. These rates are considered normal for toddlers and do not predispose them to frequent infections.
Choice C rationale:
Toddlers do have less efficient defense mechanisms than infants, making them more susceptible to infections. This is due to the immature immune system in toddlers, which is still developing and learning to respond to various pathogens. However, this choice is not the most important factor predisposing toddlers to frequent infections; other factors play a more significant role.
Choice D rationale:
The presence of short, straight internal ear/throat structures and large tonsil/adenoid lymph tissue in toddlers is the most important factor predisposing them to frequent infections such as otitis media, tonsillitis, and upper respiratory tract infections. These anatomical features make it easier for bacteria and viruses to enter and infect the respiratory and ear passages, leading to recurrent infections.
During a funduscopic examination of a school-age child, the nurse notes a brilliant, uniform red reflex in both eyes. The nurse should recognize that this is:
Explanation
Choice A rationale:
A brilliant, uniform red reflex observed during a funduscopic examination is a normal finding. It indicates the absence of any abnormalities in the retina or lens. A normal red reflex is essential in ruling out serious conditions such as retinoblastoma, cataracts, or other eye abnormalities.
Choice B rationale:
An abnormal red reflex, especially if it is not uniform and brilliant, could indicate underlying eye conditions and would require referral to an ophthalmologist for further evaluation. However, in this scenario, the description provided indicates a normal finding, making this choice incorrect.
Choice C rationale:
A uniform red reflex does not suggest a possible visual defect that requires vision screening. A normal red reflex indicates the absence of significant visual abnormalities, making this choice incorrect.
Choice D rationale:
Small hemorrhages in the eye would not present as a brilliant, uniform red reflex. Hemorrhages typically appear as dark spots or patches and would be an abnormal finding requiring further evaluation. This choice is incorrect in the context of the described scenario.
What should a nurse advise the parents of a child with type 1 diabetes mellitus who is not eating as a result of a minor illness?
Explanation
Choice A rationale:
Adjusting the insulin dosage without proper medical guidance can be dangerous for a child with diabetes. Giving half the regular morning dose without considering the child's current blood glucose levels can lead to hypoglycemia, a potentially life-threatening condition. This choice is unsafe and incorrect.
Choice B rationale:
Substituting simple carbohydrates or calorie-containing liquids for solid foods might help maintain the child's blood glucose levels to some extent. However, it's crucial to ensure that the child's overall nutritional needs are met. In cases of illness, monitoring blood glucose levels and consulting with a healthcare provider are essential. This choice, while not the best option, could be a temporary measure if the child is not eating solid foods due to illness.
Choice C rationale:
Giving the child plenty of unsweetened, clear liquids is the most appropriate choice. This helps prevent dehydration, a common concern when a child is not eating or drinking adequately due to illness. Clear liquids, such as water, clear broths, or oral rehydration solutions, can help maintain hydration and provide some electrolytes. It's essential for parents to monitor the child's condition closely and seek medical advice if the child's condition worsens.
Choice D rationale:
Taking the child directly to the emergency department is not necessary if the child is only experiencing a minor illness and is not eating. However, if the child shows signs of severe dehydration, persistent vomiting, or other concerning symptoms, seeking medical attention promptly is crucial. In the absence of these severe symptoms, choice C is the most appropriate course of action.
Parents of a school-age child with hemophilia ask the nurse, "Which sports are recommended for children with hemophilia?" Which sport should the nurse recommend?
Explanation
Choice A rationale:
Soccer involves running, sudden stops, and potential collisions, which can increase the risk of injuries and bleeding in children with hemophilia. While moderate exercise is generally beneficial for individuals with hemophilia, activities with a high risk of trauma, like soccer, should be avoided to prevent bleeding episodes. Therefore, soccer is not the recommended sport for children with hemophilia.
Choice B rationale:
Swimming is a highly recommended sport for children with hemophilia. It is a low-impact exercise that improves cardiovascular health, strength, and flexibility without putting excessive stress on the joints. Swimming also reduces the risk of bleeding episodes, making it a safe and suitable choice for individuals with hemophilia.
Choice C rationale:
Basketball involves rapid movements, jumping, and physical contact, all of which can increase the risk of injuries and bleeding in children with hemophilia. Engaging in sports that involve frequent collisions or physical impact can lead to joint bleeds and other complications in individuals with hemophilia. Therefore, basketball is not the recommended sport for children with hemophilia.
Choice D rationale:
Football, similar to soccer and basketball, involves intense physical contact and rapid movements, making it a high-risk sport for children with hemophilia. Engaging in such activities significantly increases the likelihood of bleeding episodes and injuries. Therefore, football is not the recommended sport for children with hemophilia.
The nurse is performing an assessment on a child and notes the presence of Koplik's spots. In which communicable disease are Koplik's spots present?
Explanation
Choice A rationale:
Koplik's spots are small white or bluish-white spots with a red halo that appear inside the mouth on the buccal mucosa. They are a characteristic sign of measles (rubeola). Measles is a highly contagious viral infection characterized by fever, cough, runny nose, and a distinctive red rash. The presence of Koplik's spots is a specific diagnostic feature of measles, making choice A incorrect for this scenario.
Choice B rationale:
Koplik's spots are a classic sign of measles (rubeola). These spots typically appear a few days before the onset of the measles rash and are highly indicative of the disease. Measles is a highly contagious viral infection that spreads through respiratory droplets. It is essential to recognize Koplik's spots as they provide an early clue to the diagnosis of measles, enabling healthcare providers to take appropriate precautions and prevent the further spread of the disease.
Choice C rationale:
Chickenpox (varicella) presents with an itchy rash that progresses to fluid-filled blisters. However, Koplik's spots are not associated with chickenpox. Chickenpox is caused by the varicella-zoster virus and is characterized by a widespread rash, fever, and general discomfort. Koplik's spots are specific to measles and do not occur in chickenpox.
Choice D rationale:
Exanthema subitum, also known as roseola, is a viral illness that primarily affects infants and young children. It is characterized by high fever followed by a rash. However, Koplik's spots are not a feature of roseola. The rash in roseola appears after the fever subsides and is typically pink or red, differentiating it from the small white spots seen in measles.
You just viewed 10 questions out of the 72 questions on the International College of Health Sciences ICHS OB Pediatrics s Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



