Med Surg
Med Surg
Total Questions : 87
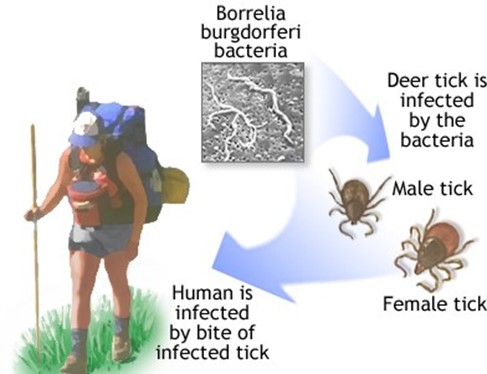
Showing 10 questions Sign up for moreA client calls the clinic and tells the nurse that he was bitten by a tick and is afraid he has Lyme disease. How long does the nurse understand that the tick must be attached to Lyme disease?
Explanation
36 to 48 hours. Lyme disease is caused by the bacterium Borrelia burgdorferi, which is transmitted to humans through the bite of infected black-legged ticks. The tick must be attached to the skin for at least 36 to 48 hours for the bacterium to be transmitted. The nurse should advise the client to seek medical attention promptly.
Choice B is incorrect because the tick must be attached for a longer duration of time for the bacterium to be transmitted.
Choice C is incorrect because the tick must be attached for a longer duration of time for the bacterium to be transmitted.
Choice D is incorrect because the tick must be attached for a longer duration of time for the bacterium to be transmitted.
Which of the following interventions would be appropriate for a client who has undergone surgery for a disorder and has started shivering?
Explanation
Provide the client with warm fluids. Shivering is the body's natural response to try to warm itself up. Providing warm fluids to the client can help to increase the client's core temperature and decrease shivering.
Choice A is incorrect because a hypothermia blanket is used to reduce the client's core temperature, which is not appropriate for a client who is shivering.
Choice C is incorrect because a light blanket may not provide enough warmth for the client who is shivering.
Choice D is incorrect because the room temperature should be kept warm to prevent the client from getting colder and shivering more.
The nurse is talking with a group of clients that are older than age 50 years about the recognition of colon cancer to access early intervention. What should the nurse inform the clients to report immediately to their primary care provider?
Explanation
Change in bowel habits. Change in bowel habits, such as diarrhea, constipation, or a change in stool consistency, is a common early symptom of colon cancer. The nurse should advise clients over age 50 to report any changes in bowel habits to their primary care provider for early intervention.
Choice B is incorrect because abdominal cramping is a common symptom of irritable bowel syndrome and not necessarily an early symptom of colon cancer.
Choice C is incorrect because daily bowel movements are considered normal for some individuals and are not necessarily indicative of colon cancer.
Choice D is incorrect because excess gas is not an early symptom of colon cancer.
The nurse is caring for a client with a deteriorating neurological condition. The nurse is performing an assessment at the beginning of the shift and notes a falling blood pressure and heart rate. The client is lying flat with arms and legs that are extended, stiff, and rigid, and the feet are plantar flexed. What would be the correct documentation of this posturing?
Explanation
Choice A is incorrect because stuporous is a state of reduced consciousness, and does not describe the posturing observed in the client.
Choice B is correct because decerebrate posturing is characterized by extension of the arms, wrists, and fingers, and extension and internal rotation of the legs, with plantar flexion of the feet.
Choice C is incorrect - Decorticate posturing is characterized by flexion of the arms, wrists, and fingers, extension, internal rotation, and adduction of the legs, with plantar flexion of the feet. This is caused by damage to the cerebral cortex and is indicative of a neurological problem.
Choice D is incorrect because flaccidity is a state of complete lack of muscle tone, and does not describe the posturing observed in the client.
A client is taking large amounts of salicylates for the treatment of bursitis of the left shoulder. The client should be aware to report which symptoms of salicylate toxicity (salicylism)?
Explanation
Ringing in the ears. Salicylate toxicity or salicylism is a condition that occurs when a client is taking large amounts of salicylates, which can result in symptoms such as tinnitus or ringing in the ears, nausea, vomiting, and diarrhea. Clients should report these symptoms to their healthcare provider immediately to prevent further complications.

Choice A, diarrhea, is not a symptom of salicylate toxicity, but rather a potential side effect of the medication in normal doses.
Choice C, dry eyes, and choice D, dry hacking cough, are not symptoms of salicylate toxicity.
On initial nursing rounds, the diabetic client reports "not feeling well." Later, the nurse finds the client to be diaphoretic and in a stuporous state. What is the immediate action taken by the nurse?
Explanation
choice A, Obtain a glucometer reading. The immediate action taken by the nurse is to obtain a glucometer reading to determine the client's blood glucose level. The client's symptoms are suggestive of hypoglycemia, a condition that can lead to coma and seizures if left untreated. Administering fruit juice or starting an IV of dextrose without first checking the client's blood glucose level can worsen the condition if the client's blood glucose is high. The physician should be notified if the client's blood glucose level is critically low or high and if the client's condition does not improve after treatment.
B. Administering fruit juice can worsen the condition if the client's blood glucose is high.
C. Starting an IV of dextrose can worsen the condition if the client's blood glucose is high.
D. Calling the physician is not the immediate action, as the client needs urgent treatment.
Following a serious thermal burn, which complication will the nurse take action to prevent first?
Explanation
Hypovolemia. Following a serious thermal burn, the nurse takes action to prevent hypovolemia, which can result from fluid loss due to the burn. Hypovolemia can lead to hypoperfusion of vital organs, including the kidneys, and can cause acute renal failure. Preventing hypovolemia is critical to preventing other complications such as tissue hypoxia, cardiac failure, and infection.
A. Tissue hypoxia and cardiac failure are consequences of hypovolemia due to decreased blood flow to organs.
D. Infection is not the immediate complication to prevent but is a potential complication following burn injury.
The nurse is caring for a postoperative client who had surgery to decrease intracranial pressure after suffering a head injury. Which assessment finding is promptly reported to the physician?
Explanation
The client's vital signs are temperature, 101.9 F; heart rate, 88 beats/minute; respiratory rate, 18 breaths/minute, and blood pressure, 138/80 mm Hg. An elevated temperature is a significant finding that may indicate the presence of an infection, which can cause further neurological damage in a client with an intracranial injury. The physician should be notified promptly, as the client may require antibiotic therapy to prevent the spread of infection.
B. Periorbital edema and ecchymosis are normal findings following head injury and should be monitored but do not require immediate intervention.
C. Resting in semi-Fowler's position is an appropriate position to maintain after intracranial pressure-reducing surgery.
D. Improved level of consciousness is a positive finding and indicates that the client is responding well to treatment.
The nursing student is taking an anatomy and physiology class. What anatomical structure equalizes air pressure in the middle ear?
Explanation
Eustachian tube. The Eustachian tube is a narrow tube that connects the middle ear to the back of the nose and equalizes air pressure in the middle ear.
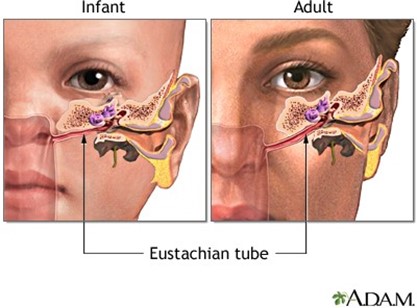
B. The malleus is a bone in the middle ear that transmits sound vibrations.
C. The pinna is the visible part of the ear that collects and directs sound waves.
D. The meatus is a passage or opening leading to the ear or nose.
The nurse is planning care for a client admitted to the neurologic rehabilitation unit following a cerebrovascular accident. Which nursing intervention would be of the highest priority?
Explanation
Assess the client for the ability to ambulate independently. The highest priority nursing intervention for a client admitted to a neurologic rehabilitation unit following a cerebrovascular accident is to assess the client's ability to ambulate independently. This assessment will help the nurse determine the level of assistance required and develop an appropriate care plan.
Option A. Providing instruction on blood-thinning medication is not the highest priority as it can be done later when the client's ambulation status is stable.
Option C. Including the client in the planning of care and setting of goals is important but not the highest priority in this situation as it can be done after assessing the client's ambulation status.
Option D. Praise the client when using adaptive equipment, is not the highest priority as the client's ambulation status is more important at this point.
You just viewed 10 questions out of the 87 questions on the Med Surg Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



