A nurse is assessing a full-term newborn. Which of the following findings should the nurse report to the provider?
Respiratory rate 55/min
Blood pressure 80/50 mm Hg
Temperature 36.5°C (97.7°F)
Heart rate 72/min
The Correct Answer is D
Heart rate is one of the vital signs that reflects the health and well-being of a newborn. It is measured by counting the number of heart beats per minute, either by listening to the chest with a stethoscope or by feeling the pulse at the wrist, elbow, or groin. Heart rate can vary depending on the newborn's activity level, temperature, and emotional state¹.
The normal range for heart rate in full-term newborns is 120 to 160 beats per minute. The heart rate may be slightly higher or lower depending on the newborn's age, weight, and gestational age. For example, premature newborns may have a higher heart rate than term newborns, and heavier newborns may have a lower heart rate than lighter newborns¹².
A heart rate that is too high (tachycardia) or too low (bradycardia) can indicate a problem with the newborn's heart function, oxygenation, or circulation. Some of the possible causes of abnormal heart rate in newborns are:
- Congenital heart defects: structural abnormalities of the heart that are present at birth and affect the blood flow through the heart and the body. They can cause cyanosis (bluish skin color), murmur (abnormal heart sound), poor feeding, or failure to thrive¹³.
- Arrhythmias: irregular or abnormal heart rhythms that can affect the electrical impulses that control the heartbeat. They can cause palpitations (feeling of skipped or extra beats), dizziness, fainting, or cardiac arrest¹³.
- Hypoxia: lack of oxygen in the blood or tissues that can affect the brain and other organs. It can be caused by respiratory distress, anemia, infection, or birth asphyxia. It can cause bradycardia, apnea (pauses in breathing), seizures, or coma¹⁴.
- Hypothermia: low body temperature that can affect the metabolism and organ function. It can be caused by exposure to cold environment, infection, or prematurity. It can cause bradycardia, lethargy, poor feeding, or hypoglycemia (low blood sugar)¹⁴.
- Sepsis: severe infection that can affect the whole body and cause inflammation and organ damage. It can be caused by bacteria, viruses, fungi, or parasites that enter the bloodstream from the mother, the umbilical cord, or the environment. It can cause tachycardia, fever, chills, poor feeding, or shock¹⁴.
Therefore, the nurse should report a heart rate of 72/min to the provider as an abnormal finding and monitor the newborn for any other signs of distress or illness. The provider may order further tests or treatments to determine the cause and severity of the low heart rate and prevent any complications.
The other findings are not findings that the nurse should report to the provider because they are within the
normal range for full-term newborns:
- a) Respiratory rate 55/min is within the normal range for respiratory rate in full-term newborns. The normal range for respiratory rate in full-term newborns is 40 to 60 breaths per minute. The respiratory rate may vary depending on the newborn's activity level, temperature and emotional state¹².
- b) Blood pressure 80/50 mm Hg is within the normal range for blood pressure in full-term newborns. The normal range for blood pressure in full-term newborns is 65 to 95 mm Hg for systolic pressure (the top number) and 30 to 60 mm Hg for diastolic pressure (the bottom number). The blood pressure may vary depending on the newborn's age, weight, and gestational age¹².
- c) Temperature 36.5°C (97.7°F) is within the normal range for temperature in full-term newborns. The normal range for temperature in full-term newborns is 36.5°C to 37.5°C (97.7°F to 99.5°F). The temperature may vary depending on the newborn's activity level, clothing, and environment¹².
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is A
Explanation
Hemolytic disease of the newborn (HDN) is a condition that occurs when there is an incompatibility between the blood types of the mother and the baby. It causes the mother's immune system to produce antibodies that attack and destroy the baby's red blood cells, leading to anemia, jaundice, organ enlargement, and other complications¹.
One of the most common causes of HDN is Rh incompatibility. This happens when the mother is Rh negative and the baby is Rh positive. The Rh factor is a protein that can be present or absent on the surface of red blood cells. People who have the protein are Rh positive and people who do not have it are Rh negative
Rh incompatibility can cause HDN when the baby's Rh positive blood cells cross the placenta and enter the mother's bloodstream. This can happen during delivery, miscarriage, abortion, or invasive prenatal testing. The mother's immune system recognizes the baby's blood cells as foreign and produces antibodies against them. These antibodies can cross back to the baby's bloodstream and attack the baby's red blood cells, causing hemolysis (breakdown) and anemia².
HDN due to Rh incompatibility usually does not affect the first pregnancy, because the mother has not been exposed to Rh positive blood before and has not developed antibodies yet. However, it can affect subsequent pregnancies with Rh positive babies, because the mother has become sensitized and has antibodies ready to attack².
The other options are not causes of HDN:
- a) The mother and the father are both Rh negative. This is not a cause of HDN because both parents have the same Rh factor and there is no incompatibility between them. The baby will also be Rh negative and will not trigger an immune response from the mother².
- b) The mother and the father are both Rh positive. This is not a cause of HDN because both parents have the same Rh factor and there is no incompatibility between them. The baby will also be Rh positive and will not trigger an immune response from the mother².
- c) The mother is Rh positive and the father is Rh negative. This is not a cause of HDN because the mother has a dominant Rh factor and will not produce antibodies against it. The baby will either be Rh positive or Rh negative, depending on whether they inherit the father's gene or not. In either case, the baby's blood type will not trigger an immune response from the mother².

Correct Answer is C
Explanation
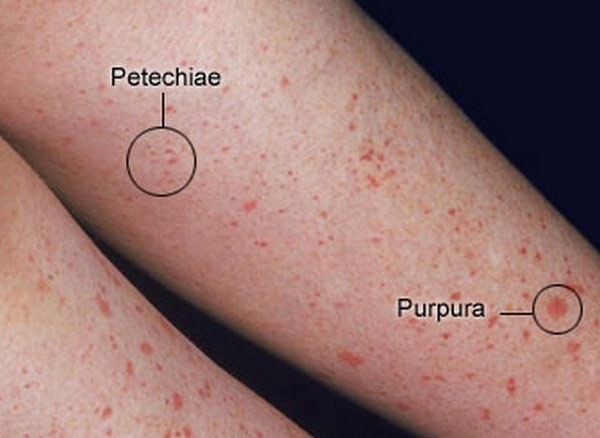
Facial petechiae are small, red or purple spots of bleeding under the skin or mucous membranes of the face. They are caused by the rupture of tiny blood vessels called capillaries. Facial petechiae can occur as a result of prolonged straining, such as during childbirth, vomiting, coughing, or crying¹. The increased pressure in the veins of the head and neck can cause the capillaries to burst, resulting in petechiae. Facial petechiae are usually harmless and resolve on their own without treatment.
The other options are not related to prolonged straining and have different causes and appearances:
a) Periauricular papillomas are benign, wart-like growths that occur near the ear. They are caused by human papillomavirus (HPV) infection and may be present at birth or develop later in life. They are usually painless and do not bleed⁴.
b) Erythema toxicum is a common skin condition in newborn babies. It causes a rash and small, fluid-filled bumps that may appear on the face, limbs, or chest. It is not caused by bleeding, infection, or allergy, but by an unknown mechanism. It does not cause discomfort to the baby and clears up without treatment within one to two weeks⁵.
d) Telangiectatic nevi are birthmarks that are caused by dilated blood vessels near the surface of the skin. They appear as red or purple patches or patterns on the skin that do not fade with pressure. They are present at birth and may grow in proportion to the child's growth. They are not associated with bleeding or infection and do not require treatment unless they cause cosmetic concerns⁶.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
