A nurse is teaching a newly licensed nurse about the uses of ultrasonography in the first trimester of pregnancy. Which of the following statements by the newly licensed nurse indicates an understanding of the teaching?
"Ultrasound is used to observe for placental maturity in the first trimester."
"Ultrasound is used to detect intrauterine growth restriction in the first trimester."
"Ultrasound is used to determine gestational age in the first trimester."
"Ultrasound is used to perform a biophysical profile in the first trimester."
The Correct Answer is C
Ultrasonography is a diagnostic imaging technique that uses high-frequency sound waves to create images of the internal structures of the body. It is a safe and noninvasive method that can provide valuable information about the pregnancy, such as the number, size, location, and health of the fetus(es), the placenta, the amniotic fluid, and the uterus.
Ultrasonography can be performed at any time during pregnancy, but it is especially useful in the first trimester (the first 12 weeks of pregnancy) for several reasons, such as:
- To confirm the pregnancy and rule out ectopic pregnancy (a pregnancy that occurs outside the uterus) or molar pregnancy (a pregnancy that develops into an abnormal mass of tissue)
- To determine gestational age (the length of time since the first day of the last menstrual period) and estimate due date (the expected date of delivery)
- To screen for chromosomal abnormalities (such as Down syndrome) or structural defects (such as spina bifida) in the fetus
- To identify multiple gestations (such as twins or triplets) or complications (such as miscarriage or
bleeding)
One of the main uses of ultrasonography in the first trimester is to determine gestational age. This is important because it can affect many aspects of prenatal care and delivery, such as:
- The timing and accuracy of other tests and procedures
- The monitoring and evaluation of fetal growth and development
- The identification and management of potential problems or complications
- The planning and preparation for labor and delivery
Gestational age can be determined by measuring the crown-rump length (CRL) of the fetus, which is the distance from the top of the head to the bottom of the spine. The CRL can be measured by using a transvaginal ultrasound (an ultrasound probe that is inserted into the vagina) or a transabdominal ultrasound (an ultrasound probe that is moved over the abdomen). The CRL can be compared to a standard growth chart to estimate gestational age. The CRL measurement is most accurate between 7 and 13 weeks of pregnancy .
Therefore, the newly licensed nurse who says that ultrasound is used to determine gestational age in the first trimester indicates an understanding of the teaching.
The other statements show a lack of knowledge or misunderstanding of the uses of ultrasonography in the first trimester:
- a) "Ultrasound is used to observe for placental maturity in the first trimester." This is not correct because placental maturity is not assessed in the first trimester. Placental maturity refers to the changes that occur in the placenta as it ages and prepares for delivery. Placental maturity can be evaluated by using a grading system that ranges from 0 to 3, based on the appearance of calcifications (deposits of calcium) in the placenta. Placental maturity can be assessed by using a transabdominal ultrasound in the third trimester (after 28 weeks of pregnancy).
- b) "Ultrasound is used to detect intrauterine growth restriction in the first trimester." This is not correct because intrauterine growth restriction (IUGR) is not detected in the first trimester. IUGR is a condition in which the fetus does not grow as expected and has a low birth weight for its gestational age. IUGR can be caused by various factors, such as placental insufficiency, maternal malnutrition, infection, or chronic disease. IUGR can affect fetal development and increase the risk of complications, such as hypoxia, hypoglycemia, or stillbirth. IUGR can be diagnosed by measuring fetal growth parameters, such as abdominal circumference, head circumference, femur length, and estimated fetal weight. These measurements can be obtained by using a transabdominal ultrasound in the second or third trimester (after 20 weeks of pregnancy).
- d) "Ultrasound is used to perform a biophysical profile in the first trimester." This is not correct because a biophysical profile (BPP) is not performed in the first trimester. A BPP is a test that evaluates fetal well-being by assessing five parameters: fetal movement, fetal tone, fetal breathing, amniotic fluid volume, and fetal heart rate. A BPP can help detect fetal distress or hypoxia and guide management decisions. A BPP can be performed by using a combination of transabdominal ultrasound and nonstress test (NST) in the third trimester (after 32 weeks of pregnancy).
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
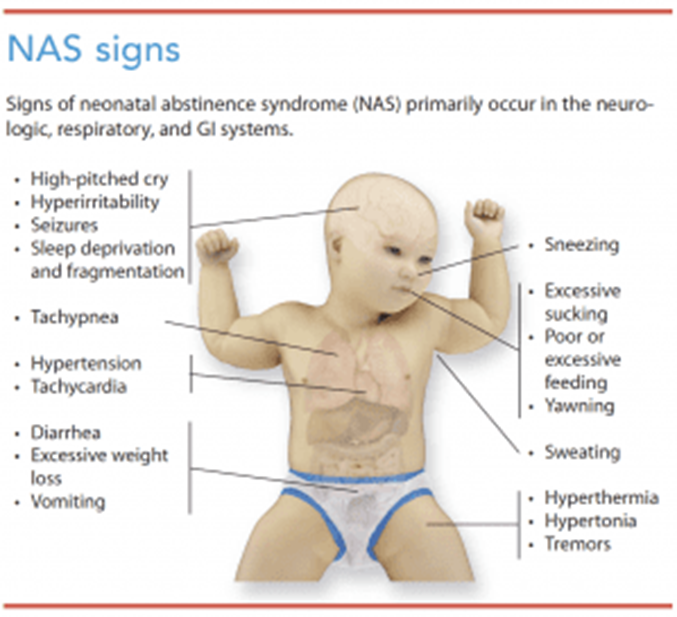
Neonatal abstinence syndrome (NAS) occurs in newborns who were exposed to addictive substances, such as opioids, during pregnancy. Infants with NAS may experience withdrawal symptoms and can be hypersensitive to stimuli. Therefore, it is important to minimize unnecessary handling to help reduce stimulation and discomfort for the newborn.
Option a) Swaddling the newborn with his legs extended may increase discomfort for a newborn with NAS. It is often recommended to swaddle newborns with NAS in a flexed position to provide a sense of security and comfort.
Option b) Maintaining eye contact during feedings may be overwhelming for a newborn with NAS. Maintaining a calm, quiet environment during feedings can help reduce overstimulation and improve feeding success.
Option c) Scheduling larger volume feedings at less frequent intervals may not be appropriate for a newborn with NAS. These infants may have poor feeding tolerance and may benefit from smaller, more frequent feedings to avoid overwhelming their gastrointestinal system.
Therefore, option d) Plan care to minimize handling of the newborn is the correct action to take when caring for a newborn with neonatal abstinence syndrome. It helps reduce stimulation and discomfort for the newborn.
Correct Answer is B
Explanation
Late decelerations are a type of fetal heart rate (FHR) pattern that indicate fetal hypoxia (lack of oxygen) due to uteroplacental insufficiency (decreased blood flow to the placenta). They are defined as a gradual decrease in FHR that occurs after the peak of a uterine contraction and returns to baseline after the end of the contraction¹. Late decelerations are associated with adverse neonatal outcomes, such as low Apgar scores, acidosis, and neonatal intensive care unit admission².
The nurse should take immediate actions to improve fetal oxygenation and blood flow when late decelerations are detected. The first and most important action is to place the client in a lateral position, either left or right, to reduce compression of the inferior vena cava and increase uterine perfusion. This can improve fetal oxygenation and reduce the severity of late decelerations¹³.
The other actions that the nurse should take are:
- Discontinue oxytocin infusion if it is being used for induction or augmentation of labor, as it can cause uterine tachysystole (excessive contractions) and worsen uteroplacental insufficiency¹³.
- Administer oxygen to the client at 8 to 10 L/min via a nonrebreather face mask to increase maternal oxygen saturation and fetal oxygen delivery¹³.
- Increase intravenous (IV) fluid infusion rate to maintain maternal hydration and blood pressure, which can improve uterine blood flow¹³.
- Notify the provider and prepare for possible operative delivery if late decelerations persist or fetal distress occurs¹³.
- Provide emotional support and reassurance to the client and family, as late decelerations can cause anxiety and fear⁴.
The other options are not actions that the nurse should take:
- a) Administer misoprostol 25 mcg vaginally. This is not correct because misoprostol is a medication that is used to induce labor by ripening the cervix and stimulating contractions. It is not indicated for late decelerations and can cause uterine hyperstimulation and fetal distress⁵.
- c) Administer oxygen via a face mask at 2 L/min. This is not correct because this is too low of an oxygen flow rate to improve fetal oxygenation. The recommended oxygen flow rate for late decelerations is 8 to 10 L/min via a nonrebreather face mask¹³.
- d) Decrease the maintenance IV solution infusion rate. This is not correct because this can cause maternal dehydration and hypotension, which can reduce uterine blood flow and worsen fetal hypoxia. The nurse should increase the IV fluid infusion rate to maintain maternal hydration and blood pressure¹³.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
