What is the major effect of calcium channel blockers on cardiac contractions
Increases the rate of cardiac contractions
Decreases the strength of cardiac contractions
Stabilizes the rhythm of cardiac contractions
Stabilizes the vasodilation during cardiac contractions
The Correct Answer is B
Calcium channel blockers (CCBs) are a class of medications that block the influx of calcium ions into cardiac and smooth muscle cells, leading to relaxation of these muscles and dilation of blood vessels.
In the heart, CCBs primarily affect the L-type calcium channels in the cardiac myocytes, which are responsible for the influx of calcium ions during the plateau phase of the cardiac action potential. By blocking these channels, CCBs decrease the amount of calcium that enters the cardiac myocytes, which in turn reduces the strength of cardiac contractions (i.e. contractility). 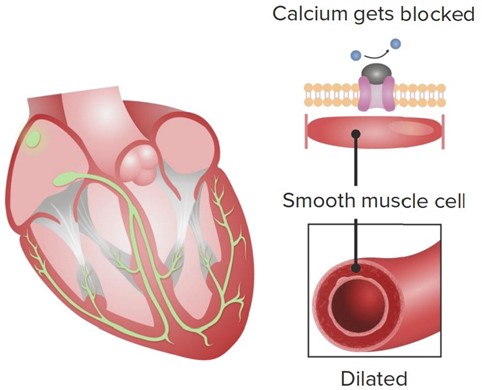
This reduction in contractility can be beneficial in certain conditions where the heart is working too hard or experiencing insufficient blood flow, such as in hypertension, angina, or some forms of arrhythmia. By reducing the workload of the heart, CCBs can help to lower blood pressure, decrease oxygen demand, and improve blood flow to the heart.
While CCBs can also have effects on the rate and rhythm of cardiac contractions, these effects are generally less pronounced than the reduction in contractility. Some CCBs, such as verapamil and diltiazem, can slow the heart rate by blocking the L-type calcium channels in the sinoatrial (SA) and atrioventricular (AV) nodes, while others, such as nifedipine, have little effect on heart rate.
Nursing Test Bank
Naxlex Comprehensive Predictor Exams
Related Questions
Correct Answer is D
Explanation
Tachycardia refers to a heart rate that is faster than the normal range, which is typically considered to be between 60 and 100 beats per minute in adults. A heart rate of 110 beats per minute is above the normal range and is considered tachycardia.
Correct Answer is C
Explanation
Hypertension, or high blood pressure, is a major risk factor for the development of left ventricular hypertrophy (LVH), which is characterized by thickening of the myocardium (heart muscle). LVH occurs in response to increased afterload (the resistance the heart has to pump against), which is a common feature of hypertension.
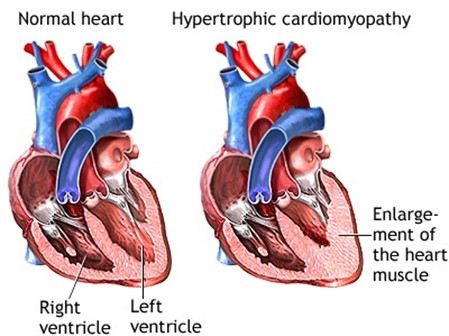
Angiotensin II, a hormone that is activated in response to hypertension, is a major mediator of LVH in this setting. Angiotensin II causes vasoconstriction (narrowing of blood vessels) and promotes the retention of salt and water, which increases blood volume and pressure. Additionally, angiotensin II stimulates the proliferation of cardiac myocytes (heart muscle cells) and the synthesis of extracellular matrix proteins, leading to hypertrophy and fibrosis of the myocardium.
Other factors that may contribute to LVH in hypertension include increased sympathetic nervous system activity, oxidative stress, and inflammation. However, angiotensin II is considered a key mediator of this process, and drugs that block the renin-angiotensin-aldosterone system (RAAS), such as angiotensinconverting enzyme (ACE) inhibitors and angiotensin receptor blockers (ARBs), are often used to treat hypertension and reduce the risk of LVH and other cardiovascular complications.
Whether you are a student looking to ace your exams or a practicing nurse seeking to enhance your expertise , our nursing education contents will empower you with the confidence and competence to make a difference in the lives of patients and become a respected leader in the healthcare field.
Visit Naxlex, invest in your future and unlock endless possibilities with our unparalleled nursing education contents today
Report Wrong Answer on the Current Question
Do you disagree with the answer? If yes, what is your expected answer? Explain.
Kindly be descriptive with the issue you are facing.
