Exam 1 ICU Cardiac, Respiratory, Neuro, Renal, Shock/Skills
Exam 1 ICU Cardiac, Respiratory, Neuro, Renal, Shock/Skills
Total Questions : 55
Showing 10 questions Sign up for moreA 57-year-old male patient in DIC is to receive 1 unit of packed red blood cells over 2 hours. There is 250 mL in the infusion bag. The IV administration infusion set delivers 10 gtts/mL. At what flow rate (in drops per minute) should the nurse run the infusion?
Record your answer using a whole number.
Explanation
flow rate for an infusion= (Volume in mL * Drop factor) / Time in minutes.
volume of the infusion bag is 250 mL, the drop factor is 10 gtts/mL, and the time is 2 hours, which is 120 minutes.
(250 mL * 10 gtts/mL) / 120 minutes = 2500 gtts / 120 minutes ≈ 20.83 gtts/minute. Therefore, the nurse should run the infusion at a rate of approximately 21 drops per minute to deliver 1 unit of packed red blood cells over the 2-hour period.
A 30-year-old female patient is admitted to the emergency department with two systemic inflammatory response syndrome variables: temperature of 100.2°F (35°C) and high blood sugar. Which intervention from the sepsis resuscitation bundle does the nurse initiate?
Explanation
The sepsis resuscitation bundle typically includes the administration of intravenous fluids to restore adequate perfusion and address hypovolemia. The initial fluid of choice is often the crystalloid solution, such as Lactated Ringers (LR), and the recommended initial fluid bolus is 30 ml/kg. This intervention aims to optimize intravascular volume and improve tissue perfusion.
A. Cooling baths in (option A) is incorrect because they may be used in the management of hyperthermia or fever, but they are not specific interventions in the sepsis resuscitation bundle.
B. Blood transfusion in (option B) is incorrect it may be necessary in certain cases of sepsis, such as severe anemia or hypovolemia, but it is not a routine intervention in the sepsis resuscitation bundle based solely on the provided information.
D. NPO status (nothing by mouth) in (option D) is incorrect because it is not a specific intervention in the sepsis resuscitation bundle. It may be indicated in certain cases, such as when surgery is required or if there is a risk of aspiration, but it does not directly address the sepsis-related variables mentioned.
It is important to note that the specific management of sepsis may vary based on the patient's individual condition, clinical presentation, and healthcare provider's orders.
A 61-year-old female patient with hypovolemic shock has these vital signs: temperature 97.9°F (36.6°C): pulse 123 beats/min: blood pressure 85/48 mamite respirations 24 breaths/min; urine output 20 mL for last 2 hours: skin cool and clammy. Which prescription order for this patient does the nurse question?
Explanation
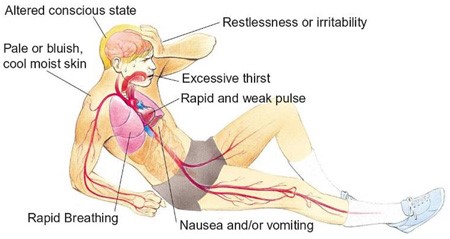
Hypovolemic shock is a life-threatening condition resulting from severe blood or fluid loss. The patient in this scenario exhibits signs of hypovolemic shock, such as low blood pressure, tachycardia, cool and clammy skin, and decreased urine output.
When assessing the prescription options, the nurse should consider the appropriateness of each intervention for hypovolemic shock. Plasmanate is a type of plasma protein fraction that is used for volume expansion in certain situations. However, in hypovolemic shock, the primary intervention is to restore intravascular volume promptly. Plasmanate alone may not be sufficient for rapid-volume resuscitation.
In hypovolemic shock, the initial management typically involves the administration of crystalloid solutions, such as Lactated Ringers or Normal Saline, to restore intravascular volume. Therefore, the prescription of Plasmanate as the primary intervention raises concerns and should be questioned by the nurse.
A. Dopamine (Intropin) 12 mcg/min in (option A) is incorrect because: Dopamine is a vasopressor medication used to increase blood pressure and cardiac output. It is a suitable option for hypovolemic shock to support blood pressure and tissue perfusion.
B. Dobutamine (Dobutrex) 5 mcg/kg/min in (option B) is incorrect because: Dobutamine is an inotropic medication that helps improve cardiac contractility and cardiac output. It can be beneficial in cases of hypovolemic shock with signs of poor cardiac function.
D. Bumetanide (Bumex) 1 mg IV in (option D) is incorrect because: Bumetanide is a loop diuretic used to promote diuresis. However, in the context of hypovolemic shock, diuretics are generally not the first-line treatment as they can further reduce intravascular volume and worsen the patient's condition.
It is essential for the nurse to consult with the healthcare provider regarding the prescription order of Plasmanate and consider alternative interventions for rapid volume resuscitation in hypovolemic shock.
The emergency department nurse provides care for a 50-year-old male patient with septic shock. The nurse recalls that the renin- angiotensin system is activated during which stage of shock?
Explanation
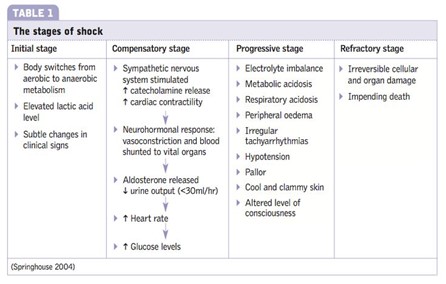
In the compensatory stage of shock, the body initiates various mechanisms to maintain perfusion to vital organs and restore homeostasis. Activation of the renin-angiotensin system is one of the compensatory responses. The decreased blood flow and oxygen delivery to the kidneys stimulate the release of renin from the kidneys. Renin acts on angiotensinogen, converting it into angiotensin I, which is further converted to angiotensin II by the action of angiotensin-converting enzyme (ACE). Angiotensin II is a potent vasoconstrictor and also stimulates the release of aldosterone, leading to sodium and water retention. These mechanisms aim to increase blood pressure and cardiac output and restore fluid balance.
A. The initial stage of shock in (option A) is incorrect because it is characterized by inadequate tissue perfusion and the activation of various compensatory mechanisms, including the release of stress hormones. However, the renin-angiotensin system is not specifically mentioned as activated in this stage.
B. The progressive stage of shock in (option B) is incorrect because it occurs when compensatory mechanisms fail to maintain adequate perfusion, leading to worsening hypoperfusion and organ dysfunction. The renin-angiotensin system continues to be activated during this stage, but it is primarily associated with the compensatory stage.
C. The refractory stage of shock in (option C) is incorrect because it is the stage of severe and prolonged hypoperfusion, where organ failure becomes irreversible. The renin-angiotensin system may still be activated, but it is not the primary focus of this stage.
Therefore, the activation of the renin-angiotensin system occurs during the compensatory stage of shock.
Which conditions can cause hypovolemic shock? Select all that apply.
Explanation
These conditions can lead to fluid loss, either through increased gastrointestinal output (diarrhea, vomiting, lower GI bleeding) or accumulation of air in the pleural space (tension pneumothorax), resulting in a decrease in blood volume and subsequent hypovolemic shock.
E. Diabetes insipidus in (option E) is incorrect because it is not directly associated with hypovolemic shock. Diabetes insipidus is a condition characterized by excessive thirst and the production of large volumes of dilute urine due to insufficient production or response to antidiuretic hormone (ADH). While diabetes insipidus can lead to dehydration and potential hypovolemia, it is not a direct cause of hypovolemic shock.
F. Valvular stenosis in (option F) is incorrect because it is a condition characterized by the narrowing or obstruction of one or more heart valves. While it can cause problems with cardiac output and circulation, it is not specifically related to hypovolemic shock, which is caused by a decrease in blood volume.
Therefore, the conditions that can cause hypovolemic shock include diarrhea, vomiting, lower GI bleeding, and tension pneumothorax.
A 40-year-old female patient with massive trauma and possible spinal cord injury is admitted to the emergency department (ED). The nurse suspects that the patient may be experiencing neurogenic shock in addition to hypovolemic shock, based on which one of the following?
Explanation
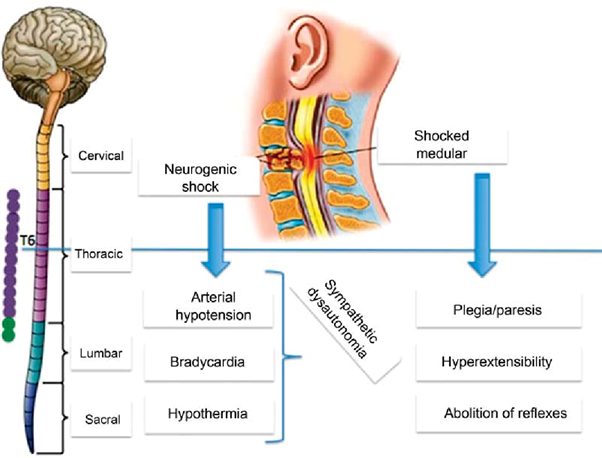
Neurogenic shock is a type of distributive shock that occurs due to the loss of sympathetic nervous system tone after a spinal cord injury or other traumatic brain injuries. This loss of sympathetic tone leads to vasodilation and decreased systemic vascular resistance, resulting in inadequate perfusion to vital organs.
One of the hallmark signs of neurogenic shock is bradycardia (a heart rate less than 60 beats/min) due to the unopposed parasympathetic activity. The parasympathetic system becomes dominant when sympathetic activity is impaired. Therefore, a heart rate of 48 beats/min in this patient suggests the possibility of neurogenic shock.
A. Cool, clammy skin in (option A) is incorrect because Cool, clammy skin is a characteristic of hypovolemic shock, where reduced blood volume leads to vasoconstriction to redirect blood flow to vital organs.
B. BP of 82/40 mm Hg in (option B) is incorrect because: Hypotension is a common finding in both neurogenic shock and hypovolemic shock. A low blood pressure reading alone does not specifically indicate neurogenic shock.
D. Shortness of breath in (option D) is incorrect because Shortness of breath is not specific to neurogenic shock but can occur in various types of shock, including hypovolemic shock. It may result from inadequate oxygenation or impaired respiratory function due to the underlying condition or associated injuries.
Therefore, the heart rate of 48 beats/min suggests the possibility of neurogenic shock in addition to hypovolemic shock in this patient.
The ICU charge nurse will evaluate that teaching about hemodynamic monitoring for a new staff nurse has been effective when the new nurse does which of the following?
Explanation
Positioning the transducer level with the phlebostatic axis is a crucial step in accurate hemodynamic monitoring. The phlebostatic axis is an imaginary reference point located at the fourth intercostal space, mid-anterior/posterior chest. Placing the transducer at this level ensures that the pressure measurements obtained are reflective of the patient's true hemodynamic status.
A. Positioning the limb with the catheter insertion site at the level of the transducer in (option A) is incorrect because: While it is important to position the limb appropriately to avoid kinks or occlusions in the catheter tubing, this is not directly related to the accurate measurement of hemodynamic parameters.
C. Ensuring that the patient is lying with the head of the bed flat for all readings in (option C) is incorrect because The position of the patient's head does not directly impact the accuracy of hemodynamic monitoring unless it specifically relates to changes in preload or intracranial pressure monitoring.
D. Balancing and calibrating the hemodynamic monitoring equipment every hour in (option D) is incorrect because: While it is important to ensure that the monitoring equipment is calibrated and functioning properly, doing so every hour may not be necessary. Calibration frequency may vary based on institutional policies and patient stability.
Therefore, the correct action that demonstrates effective teaching about hemodynamic monitoring is positioning the transducer level with the phlebostatic axis.
A 32-year-old male patient sustains 78% TBSA burn and is currently admitted to the burn unit. Which sequential order would the nurse arrange the events involved in burn shock following a patient's exposure to burns?
Explanation
A. Decreased blood volume: Burn injuries can lead to fluid loss, primarily through damaged skin. This fluid loss causes a decrease in blood volume, leading to hypovolemia. Hypovolemia contributes to decreased cardiac output and tissue perfusion.
B. Increased vascular permeability: Burn injuries cause an inflammatory response, leading to increased vascular permeability. This increased permeability allows fluid, electrolytes, and proteins to leak from the intravascular space into the interstitial space.
C. Development of edema: The increased vascular permeability and fluid leakage lead to the development of edema. Edema occurs as fluid accumulates in the interstitial spaces, further contributing to tissue swelling and compromised perfusion.
D. Increased peripheral resistance: In response to decreased blood volume and tissue hypoperfusion, the body activates compensatory mechanisms to maintain blood pressure and tissue perfusion. One of these mechanisms is increased peripheral resistance, which occurs as blood vessels constrict to maintain blood pressure. Increased peripheral resistance helps redirect blood flow to vital organs but also contributes to increased workload on the heart.
Therefore, the correct sequential order of events involved in burn shock following a patient's exposure to burns is:
A. Decreased blood volume B. Increased vascular permeability D. Development of edema C. Increased peripheral resistance
The emergency department nurse evaluates that fluid resuscitation for a 70 kg patient in shock is effective by finding which one of the following?
Explanation
Urine output is an essential indicator of renal perfusion and overall fluid status. In a patient in shock, maintaining an adequate urine output is a crucial goal of fluid resuscitation. A urine output of 0.5 to 1 mL/kg/hour is generally considered adequate in adults. The given value of 35 ml over the last hour suggests that the patient is producing urine, which indicates that fluid resuscitation is effective in restoring perfusion to the kidneys.
A. The patient's mean arterial pressure (MAP) is 50 mm Hg in (option A) is incorrect because While mean arterial pressure is an important hemodynamic parameter, a single value alone may not provide a comprehensive assessment of the patient's response to fluid resuscitation.
B. The patient's GCS score is 9 in (option B) is incorrect because The Glasgow Coma Scale (GCS) assesses the level of consciousness and neurological function but does not directly reflect fluid resuscitation effectiveness.
D. The patient's hemoglobin is within normal limits: (option D) is incorrect because Haemoglobin levels are important for assessing oxygen-carrying capacity but do not directly indicate the effectiveness of fluid resuscitation.
Therefore, the nurse can evaluate that fluid resuscitation for a 70 kg patient in shock is effective by observing a urine output of 35 ml over the last hour.
A 31-year-old male patient with burn injuries is admitted to the burn unit. Which priority does the nurse anticipate within the first 24 hours?
Explanation
In the initial 24 hours after burn injury, fluid resuscitation is a critical priority in the management of burn patients. Burn injuries can lead to significant fluid loss, both locally at the burn site and systemically due to increased capillary permeability. Fluid resuscitation aims to restore and maintain adequate intravascular volume, ensuring sufficient tissue perfusion and organ function.
The Parkland Formula is commonly used to guide fluid resuscitation in burn patients. It involves calculating the total volume of fluid needed in the first 24 hours, with a portion given in the initial hours after injury and the remainder given over the remaining hours.
A. Sterile dressing changes (option A) are incorrect because they are important in wound care management for burn patients to prevent infection. However, fluid resuscitation takes precedence within the first 24 hours.
B. Emotional support (option B) is incorrect because it is an essential aspect of burn care, as burn injuries can have a significant psychological impact. While emotional support is crucial for the patient's overall well-being, it may not be the highest priority within the first 24 hours compared to addressing the physiological needs of fluid resuscitation.
D. Range-of-motion exercises (option D) are incorrect because they are important for preventing contractures and maintaining joint mobility in burn patients. However, they are typically initiated after the initial fluid resuscitation phase and wound stabilization.
Therefore, the priority the nurse anticipates within the first 24 hours for a 31-year-old male patient with burn injuries is fluid resuscitation.
You just viewed 10 questions out of the 55 questions on the Exam 1 ICU Cardiac, Respiratory, Neuro, Renal, Shock/Skills Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



