Ati med surg(health assesment)quiz
Ati med surg(health assesment)quiz
Total Questions : 40
Showing 10 questions Sign up for moreThe nurse read the patient's health history cranial nerve III oculomotor paralysis. Which of the following would the nurse expect?
Explanation
(a) Mydriasis:
While mydriasis (dilated pupil) can be associated with cranial nerve III damage, it does not fully describe the range of symptoms expected with oculomotor paralysis. Cranial nerve III controls more functions than pupil dilation, such as eyelid elevation and certain eye movements.
(b) Normal eye movement:
Cranial nerve III paralysis would result in abnormal eye movement due to the loss of control over muscles responsible for moving the eye. Expecting normal eye movement would be incorrect since the paralysis affects the eye's ability to move properly.
(c) Ptosis will be evident and no pupillary constriction:
Cranial nerve III (oculomotor nerve) paralysis leads to ptosis (drooping eyelid) because it innervates the levator palpebrae superioris muscle. It also affects the pupillary constrictor muscles, resulting in a dilated pupil (lack of pupillary constriction), making this the most comprehensive and accurate answer.
(d) The eye cannot look to the outside side:
Inability to look to the outside (lateral movement) is typically associated with cranial nerve VI (abducens nerve) paralysis, which controls the lateral rectus muscle. Cranial nerve III primarily affects vertical and medial movements, so this is not the expected finding.
A patient is diagnosed with Homonymous Hemianopsia. The nurse expects to find what defects in the visual field of this patient:
Explanation
a) The patient is unable to see in half of the visual field (same visual field) in each eye:
Homonymous hemianopsia is a condition where there is a loss of vision in the same side of the visual field in both eyes. This occurs due to damage to the visual pathways after the optic chiasm, often from a stroke or brain injury, resulting in the loss of either the right or left visual field in both eyes.
b) The patient can see from one eye but not through the other one:
This description fits a condition called monocular blindness, which is typically caused by damage to the optic nerve before it reaches the optic chiasm. Homonymous hemianopsia involves both eyes and specific visual fields, not complete loss of vision in one eye.
c) The patient is unable to see in half of the visual field (opposite visual field) in each eye:
This option describes bitemporal hemianopsia, which results in loss of vision in the outer (temporal) fields of both eyes and is often due to damage at the optic chiasm. Homonymous hemianopsia involves the same side of the visual field in both eyes, not the opposite visual fields.
d) No visual impairment:
Homonymous hemianopsia is characterized by significant visual impairment, specifically the loss of half the visual field in both eyes on the same side. Therefore, it is incorrect to say there is no visual impairment with this condition.
A 57-year-old client reports, "I am having the worst headache I have ever experienced." Which action/Priority should the nurse perform next?
Explanation
(a) Inquire about family history of headaches:
While understanding the client's family history of headaches can be important for a comprehensive assessment, it is not the immediate priority. The description of "the worst headache" ever experienced could indicate a serious condition that needs urgent attention.
(b) Review the client's medical record:
Reviewing the client's medical record provides valuable information about their history and potential underlying conditions. However, given the severity of the reported headache, it is crucial to perform a more immediate physical assessment to rule out life-threatening conditions.
(c) Assess the client's blood pressure:
Assessing the client's blood pressure is a critical initial action. A severe headache can be a symptom of hypertensive crisis, stroke, or other serious conditions. High blood pressure could provide an immediate clue to the severity and cause of the headache, allowing for quicker intervention.
(d) Provide medication for pain relief:
Providing pain relief is important, but it should not be the first action without determining the cause of the headache. Administering medication without assessing the client's condition could mask symptoms of a potentially serious underlying issue such as a stroke or hypertensive emergency.
In which disease process should a nurse expect to see a client with the presence of pitting edema?
Explanation
(a) Liver Disease:
Pitting edema is commonly seen in liver disease, especially in conditions like cirrhosis. Liver disease can lead to hypoalbuminemia, where low levels of albumin in the blood cause fluid to leak into the interstitial spaces, resulting in edema. Additionally, liver disease often leads to portal hypertension, which can also contribute to the development of edema.
(b) Diabetes mellitus:
While diabetes can cause complications such as diabetic nephropathy, which may lead to fluid retention, pitting edema is not a primary symptom directly associated with diabetes mellitus. Diabetic patients may develop edema due to kidney issues, but it is not as directly associated as with liver disease.
(c) End Stage Renal Disease:
End-stage renal disease (ESRD) can indeed cause significant fluid retention and edema, including pitting edema. The kidneys' inability to excrete excess fluid leads to its accumulation in tissues. However, the question seems to point towards liver disease, which directly leads to conditions causing pitting edema.
(d) Colon Cancer:
Colon cancer is not typically associated with pitting edema. While advanced cancer can lead to various complications, including fluid imbalances, it is not a primary cause of pitting edema. Edema related to cancer is often more localized and associated with tumor sites or treatment areas.
An overweight African-American female client with a diagnosis of hypothyroidism asks the nurse why she has begun to gain body weight. Which is the best explanation the Medical Surgical nurse can provide?
Explanation
(a) "Your metabolism is slowing down.":
Hypothyroidism leads to a decrease in the production of thyroid hormones, which are critical in regulating metabolism. With lower levels of these hormones, the body's metabolic rate decreases, resulting in reduced calorie burning and subsequent weight gain. This explanation directly addresses the underlying cause of weight gain in hypothyroidism.
(b) "You should be exercising for longer periods of time.":
While exercise is beneficial for overall health and can help manage weight, it does not directly address the reason for weight gain in hypothyroidism. The primary issue is the slowed metabolism due to thyroid hormone deficiency, not a lack of exercise.
(c) "You could be making healthier food choices.":
Although diet plays a role in weight management, this response does not explain the root cause of weight gain in hypothyroidism. The condition itself slows metabolism, leading to weight gain even if dietary habits remain unchanged.
(d) "You are retaining fluid.":
Fluid retention can occur in hypothyroidism but is not the primary reason for weight gain in this condition. The main cause is a decreased metabolic rate, which leads to the accumulation of body fat. Fluid retention might contribute to some weight gain, but it is not the best explanation in this context.
While working in the Emergency department a Rapid response nurse is evaluating a patient in acute respiratory failure after a motor vehicle crash. Which of the following areas should the nurse evaluate as the most reliable indicator of central cyanosis?
Explanation
(a) Soles of the feet:
The soles of the feet are not considered the most reliable indicator of central cyanosis because peripheral areas can be affected by various factors, including temperature and circulation. Changes in color here might not accurately reflect central oxygenation status.
(b) Oral mucosa:
The oral mucosa is the most reliable indicator of central cyanosis because it reflects the oxygenation status of the central circulatory system. Cyanosis in this area indicates a significant drop in arterial oxygen saturation and is a more direct indicator of hypoxemia compared to peripheral sites.
(c) Ear lobes:
Ear lobes, like the soles of the feet, can be influenced by peripheral circulation and environmental factors. While cyanosis can be observed here, it is not as reliable as central sites like the oral mucosa for assessing systemic oxygenation.
(d) Conjunctivae:
The conjunctivae can show signs of cyanosis, but the oral mucosa is still a more sensitive and reliable indicator for central cyanosis. The oral mucosa provides a clear and consistent site to assess oxygenation in emergency situations.
A nurse is assessing a client who has hypothyroidism. The nurse should expect which of the following findings?
Explanation
Exophthalmos:
Exophthalmos, or protruding eyeballs, is typically associated with hyperthyroidism (Graves' disease) rather than hypothyroidism. It results from the accumulation of fluid and swelling behind the eyeballs.
(b) Palpitations:
Palpitations, or rapid heartbeat, are more commonly associated with hyperthyroidism due to the increased metabolic rate and sympathetic nervous system stimulation. In hypothyroidism, bradycardia (slow heart rate) is more likely.
(c) Diaphoresis:
Diaphoresis, or excessive sweating, is not a typical finding in hypothyroidism. It is more commonly associated with conditions that cause autonomic dysfunction or hypermetabolic states.
(d) Weight gain:
Weight gain is a hallmark symptom of hypothyroidism. It occurs due to a slowing down of the metabolic rate, leading to reduced calorie expenditure and potential fluid retention.
What abnormal physical response should the nurse be prepared to manage after noting pallor in a client?
Explanation
(a) Diarrhea: Diarrhea is an abnormal gastrointestinal response characterized by frequent, loose, or watery stools. It can be caused by infections, medications, or underlying gastrointestinal disorders. Pallor, or paleness of the skin, typically does not directly lead to diarrhea unless there are specific underlying conditions affecting both circulation and gastrointestinal function.
(b) Diaphoresis: Diaphoresis refers to excessive sweating, which can occur due to sympathetic nervous system activation, fever, or anxiety. While diaphoresis may be associated with conditions causing increased sympathetic activity, it is not directly related to pallor, which indicates reduced blood flow to the skin.
(c) Fainting: Pallor is often a sign of decreased blood flow to the skin, indicating potential hypoperfusion. If severe, this reduced circulation can lead to fainting (syncope) due to inadequate blood supply to the brain. Therefore, after noting pallor, the nurse should be prepared to manage the client for potential fainting episodes by ensuring safety and providing appropriate interventions.
(d) Vomiting: Vomiting is the forceful expulsion of stomach contents through the mouth and can be caused by various factors such as gastrointestinal irritation, infection, or systemic illnesses. Pallor does not directly cause vomiting, although severe systemic conditions affecting circulation could potentially lead to nausea and vomiting as part of a broader clinical picture.
The nurse asks the client to perform the action pictured. What is the nurse assessing?
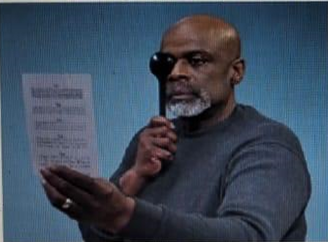
Explanation
A) Color discrimination:
Color discrimination involves assessing the client's ability to differentiate between various colors, typically using color plates like the Ishihara test. This test is often used to detect color blindness or deficiencies in color vision. The action depicted in the image, which involves reading text up close, is not relevant to assessing color vision capabilities.
B) Near vision:
Near vision is assessed by having the client read small text or print held at a close distance, often using a near vision chart or card. The image shows the client covering one eye with an occluder while reading text, which is a common method to test the clarity and focus of near vision. This helps determine if the client has issues such as presbyopia, which affects near vision acuity.
C) Distance vision:
Distance vision is typically evaluated using a Snellen chart, where the client reads letters or symbols from a distance of 20 feet. The test aims to assess the clarity of vision at a distance. The action in the image does not align with this type of assessment, as it focuses on close-up reading rather than distance.
D) Intraocular pressure:
Intraocular pressure is measured using tools like a tonometer to assess the fluid pressure inside the eye, which is crucial for diagnosing conditions like glaucoma. This test involves specific instruments and procedures, unlike the reading task depicted in the image, which is unrelated to measuring eye pressure.
A client complains of excessive tearing of the eyes. Which assessment would the nurse do next?
Explanation
A) Assess the nasolacrimal sac: Excessive tearing, or epiphora, can result from an obstruction in the nasolacrimal duct, which drains tears from the eye into the nasal cavity. By assessing the nasolacrimal sac, the nurse can determine if there is any blockage or infection causing the excessive tearing, making this the most appropriate next step.
B) Test pupillary reaction to light: While testing pupillary reaction to light is important in a comprehensive eye exam, it does not directly address the issue of excessive tearing. This test is more focused on evaluating neurological function and overall eye health.
C) Inspect the palpebral conjunctiva: Inspecting the palpebral conjunctiva can help identify inflammation, infection, or foreign bodies that may cause discomfort or tearing. However, it does not specifically address the cause of excessive tearing related to nasolacrimal duct obstruction.
D) Perform the eye positions test: The eye positions test assesses extraocular muscle function and cranial nerve integrity. While it is important for a complete eye examination, it is not directly related to the symptom of excessive tearing, which is more likely due to issues with tear drainage.
You just viewed 10 questions out of the 40 questions on the Ati med surg(health assesment)quiz Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



