Ivytech community college Med Surg II exam
Ivytech community college Med Surg II exam
Total Questions : 36
Showing 10 questions Sign up for moreWhat is the best indication if the client with congestive heart failure is holding excess fluid?
Explanation
A. Intake and output:
Intake and output refer to monitoring the amount of fluids a person consumes (intake) and eliminates (output) through urine, feces, and other means. While tracking fluid intake and output is important, it may not provide a direct indication of excess fluid retention.
B. Pitting pedal edema:
Pitting pedal edema is swelling in the lower extremities, particularly the ankles and feet, that leaves an indentation (pit) when pressure is applied. This can be a sign of fluid retention but may not always be the earliest or most reliable indicator.
C. Crackles in the bases of the lungs:
Crackles or rales in the bases of the lungs can be indicative of pulmonary congestion, which may occur due to fluid accumulation. However, crackles alone may not always be specific to fluid overload and can be present in other respiratory conditions.
D. Daily weights:
Daily weights are a critical and sensitive measure for assessing fluid balance. Sudden weight gain, especially over a short period, can be a strong indicator of fluid retention. Monitoring weight on a daily basis helps to detect changes early, allowing for prompt intervention.
A client is being admitted to the medical unit to rule out cardiac issues related to valve malfunction. Which question should the nurse ask the client during the admission interview to support this diagnosis?
Explanation
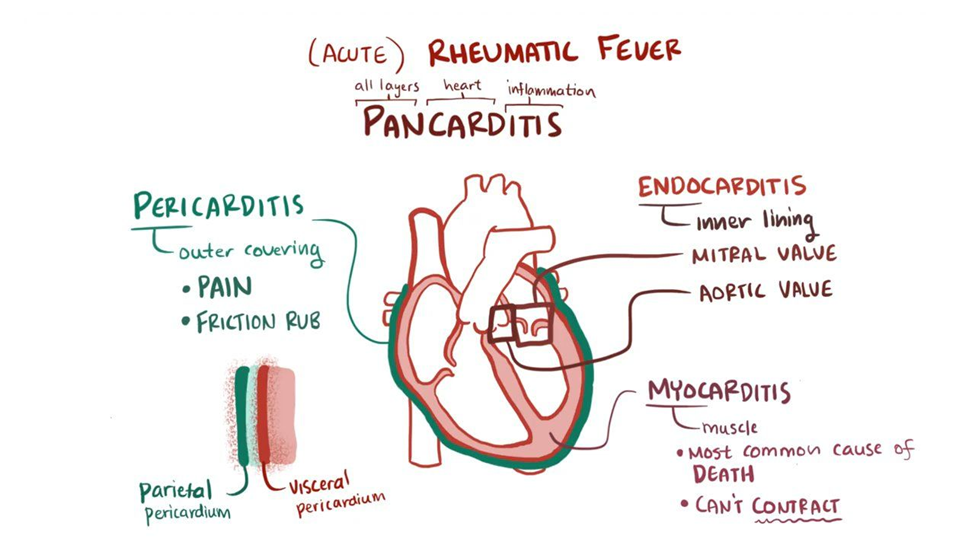
A. "Did you have rheumatic fever as a child?"
Rheumatic fever is an inflammatory condition that can affect the heart, especially the heart valves. Rheumatic fever is a known risk factor for the development of valvular heart disease. Asking about a history of rheumatic fever helps identify a potential cause for valve malfunction.
B. "Do you have a family history of valve problems?"
Family history can be relevant in understanding genetic predispositions to certain cardiac conditions. While it may contribute to the overall assessment of cardiac risk, it may not be as directly linked to valve malfunction as a history of rheumatic fever.
C. "Do you have a history of MRSA?"
MRSA (Methicillin-resistant Staphylococcus aureus) is a type of bacterial infection and is not directly associated with valve malfunction. This question may be relevant for other aspects of the client's health but is not specific to ruling out cardiac issues related to valve malfunction.
D. "What over-the-counter medications do you take?"
While knowing the medications a client takes is important for a comprehensive assessment, asking about over-the-counter medications may not be as directly related to ruling out cardiac issues related to valve malfunction. It is more relevant for assessing potential interactions or effects on cardiovascular health.
A group of student nurses are practicing taking blood pressures. A 56-year-old male student has a blood pressure reading of 146/96 mm Hg. Upon hearing the reading, he exclaims, “My pressure has never been this high. Do you think my doctor will prescribe medication to reduce it?” Which of the following responses by the nursing instructor would be best?
Explanation
A. "A single elevated blood pressure does not confirm hypertension. A diagnosis of hypertension requires two or more elevated readings taken by your physician before a diagnosis can be made."
This response emphasizes the need for multiple elevated readings for a diagnosis of hypertension. It educates the individual about the diagnostic criteria and encourages them to seek further evaluation from their physician.
B. "We will need to reevaluate your blood pressure because your age places you at high risk for hypertension."
This response might be seen as implying that age alone is a significant factor in determining hypertension, which may not be accurate. While age is a risk factor, the emphasis should be on the need for multiple readings and a physician's evaluation rather than attributing it solely to age.
C. "Hypertension is prevalent among men: it is fortunate we caught this during your routine examination."
This response suggests that the elevated blood pressure is automatically assumed to be hypertension based on gender. It is important to avoid making assumptions and instead focus on the need for proper evaluation and multiple readings for a hypertension diagnosis.
D. "You have no need to worry. Your pressure is probably elevated because you are being tested."
This response dismisses the individual's concerns and attributes the elevated blood pressure solely to the testing situation. While stress or anxiety can influence blood pressure readings, it's essential to address the need for further evaluation and not completely disregard the possibility of hypertension.
A client with a complex cardiac history is scheduled for transesophageal echocardiography. Which of the following statements, if made by the nurse, is inappropriate?
Explanation
A. "The test will provide a detailed profile of the heart’s electrical activity."
This statement is inappropriate because transesophageal echocardiography (TEE) primarily provides detailed images of the heart's structure, such as the valves and chambers, rather than focusing on the heart's electrical activity. The assessment of electrical activity is typically associated with electrocardiography (ECG or EKG) rather than echocardiography.
B. "I will need to start an IV in your arm before the test."
This statement is appropriate. It is common for medical procedures, including TEE, to require an intravenous (IV) line for administration of medications or fluids during or after the procedure.
C. "Your throat may be a little sore after the exam."
This statement is appropriate. TEE involves inserting a probe through the esophagus, and it is common for patients to experience a sore throat afterward due to the presence of the probe.
D. "You will need to refrain from eating and drinking 6-8 hours before this test."
This statement is appropriate. It is standard practice to ask patients to fast for a specific period before TEE to minimize the risk of complications, such as aspiration, during the procedure.
The nurse is taking health history for a client who reports pain in his lower left leg and foot when walking. The pain is relieved with rest, and the nurse observes the left leg is hairless and slightly edematous. The nurse recognizes this as which medical diagnosis or health problem?
Explanation
A. Coronary artery disease (CAD):
Coronary artery disease primarily affects the blood vessels supplying the heart muscle. Symptoms often include chest pain (angina) rather than pain in the lower extremities. The symptoms described in the scenario are not characteristic of CAD.
B. Arterial embolus:
An arterial embolus is a blood clot or debris that travels through the bloodstream and can block an artery. While it can cause decreased blood flow and pain, the presentation in the lower left leg and foot with relief of pain at rest is more suggestive of peripheral arterial disease (PAD) or intermittent claudication rather than an acute arterial embolus.
C. Raynaud disease:
Raynaud's disease is characterized by episodes of reduced blood flow to the extremities, usually triggered by cold or stress. It typically involves color changes (white, blue, red) in the fingers or toes. The symptoms described, including pain in the lower leg and foot during walking, are not typical of Raynaud's disease.
D. Intermittent claudication:
Intermittent claudication is a symptom associated with peripheral arterial disease (PAD). It involves pain or cramping in the legs during physical activity, such as walking, due to reduced blood flow to the muscles. Rest typically relieves the pain. The observation of a hairless leg and slight edema suggests potential vascular compromise in the lower extremity, supporting the diagnosis of intermittent claudication.
An emergency department nurse is assessing an adult woman for a suspected myocardial infarction (MI). When planning the assessment, the nurse should be aware that female patients may have which of the following symptoms for an MI? (SELECT ALL THAT APPLY)
Explanation
A. Shortness of breath
Shortness of breath can be a symptom of a myocardial infarction in both men and women.
B. Anxiety
Anxiety can be a symptom in some cases, as individuals may feel a sense of impending doom or anxiety during an MI.
C. Unusual fatigue
Unusual fatigue, especially if it is severe or occurs with exertion, can be a symptom of a myocardial infarction.
D. Back pain
Back pain, particularly between the shoulder blades, can be a symptom of a myocardial infarction in women.
E. Chest pain
Chest pain or discomfort is a classic symptom of a myocardial infarction. While women may experience chest pain, they are also more likely than men to have atypical symptoms.
The nurse on a cardiac unit is caring for a client admitted with an acute exacerbation of heart failure. The nurse concludes that the client’s condition is worsening after noting which client data during assessment. (SELECT ALL THAT APPLY)
Explanation
A. Normal sinus rhythm that becomes sinus tachycardia
Sinus tachycardia can be an indication of increased sympathetic activity in response to decreased cardiac output. It may suggest the heart's compensatory response to maintain adequate perfusion.
B. Onset of a cough with pink, frothy sputum
Pink, frothy sputum is a classic sign of pulmonary edema, which can occur in the setting of worsening heart failure. It indicates the presence of blood-tinged fluid in the alveoli.
C. Presence of dyspnea at rest
Dyspnea at rest suggests that the client is experiencing difficulty breathing even without physical exertion. This can be indicative of more severe heart failure.
D. Falls asleep when not disturbed
Falling asleep when not disturbed may indicate fatigue or exhaustion, which is common in individuals with heart failure. However, it is not a direct indicator of worsening heart failure and can be influenced by various factors.
E. Urine drainage is increased in amount
Increased urine output can be a sign of diuretic therapy or an attempt by the body to compensate for fluid overload. However, it is essential to consider other factors such as renal function and medication effects.
The nurse is planning the care of a client with heart failure. The nurse should identify what overall goals for the client’s care? (SELECT ALL THAT APPLY)
Explanation
A. Limit physical activity
Limiting physical activity is not a primary goal in heart failure care. In fact, promoting appropriate and monitored physical activity is often part of the overall management plan. Exercise, when tailored to the client's condition, can improve functional status and quality of life.
B. Prevent endocarditis
While preventing endocarditis is important for individuals with certain cardiac conditions, it is not a primary goal in the care of heart failure. The focus is typically on optimizing cardiac function and managing heart failure symptoms.
C. Relieve the patient’s symptoms
Managing and relieving symptoms, such as dyspnea, fatigue, and fluid retention, are crucial goals in heart failure care. This includes optimizing medication management and other therapeutic interventions.
D. Extend survival
While heart failure is a chronic condition, the goal is to optimize treatment to improve the client's prognosis and overall survival. This involves the use of evidence-based therapies to address the underlying causes and contributing factors.
E. Improve functional status
Enhancing the client's ability to perform activities of daily living and improving functional capacity are important goals. This can involve a combination of medications, lifestyle modifications, and rehabilitation.
The nurse is teaching a client about some of the health consequences of uncontrolled hypertension. What health problems should the nurse describe. (SELECT ALL THAT APPLY)
Explanation
A. Retinal Hemorrhage
Uncontrolled hypertension can damage the blood vessels in the eyes, leading to retinal hemorrhages. This can result in vision problems and, in severe cases, vision loss.
B. Ventricular Hypertrophy
Uncontrolled hypertension causes the heart to pump against increased resistance, leading to the thickening and enlargement of the left ventricle. Ventricular hypertrophy is a response to the increased workload on the heart and is associated with an increased risk of heart failure.
C. Cerebrovascular Disease
Hypertension is a major risk factor for cerebrovascular diseases, including strokes. Elevated blood pressure can damage the blood vessels in the brain, increasing the risk of stroke. Strokes can have serious consequences, affecting various neurological functions.
D. Venous Insufficiency
Venous insufficiency is not typically directly associated with uncontrolled hypertension. It is more commonly related to problems with the venous system, such as damaged valves in the veins, leading to poor blood flow back to the heart. While hypertension can affect arteries, venous insufficiency is a distinct condition.
E. Transient Ischemic Attacks (TIAs)
Uncontrolled hypertension increases the risk of transient ischemic attacks (TIAs), which are brief episodes of neurological dysfunction caused by temporary disruption of blood flow to the brain. TIAs are often considered warning signs of an increased risk of stroke.
The nursing student is reviewing interventions which are part of nursing care and prevention of atelectasis. What are some of the interventions nurses can do to prevent atelectasis? (SELECT ALL THAT APPLY)
Explanation
A. Administer antibiotics
Administering antibiotics is not a direct intervention for preventing atelectasis. Antibiotics are typically prescribed to treat bacterial infections, and atelectasis is more related to lung collapse or incomplete lung expansion.
B. Encourage increased oral fluid intake
Adequate hydration is important for maintaining the moisture of respiratory secretions. This helps prevent mucus from becoming thick and sticky, making it easier for the patient to cough and clear the airways.
C. Early mobilization after surgery
Early mobilization, including activities such as getting out of bed and walking, helps improve lung expansion. It promotes better ventilation and prevents areas of the lungs from collapsing, reducing the risk of atelectasis.
D. Frequent turning of the patient
Turning the patient regularly is crucial for preventing pooling of respiratory secretions in dependent areas of the lungs. By changing the patient's position, nurses can facilitate drainage and ventilation throughout the lungs, minimizing the risk of atelectasis.
E. Use of incentive spirometry
Incentive spirometry is a breathing exercise device that encourages the patient to take slow, deep breaths. This helps expand the lungs and prevents atelectasis by maintaining lung volume and promoting alveolar recruitment.
You just viewed 10 questions out of the 36 questions on the Ivytech community college Med Surg II exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



