Pathophysiology
Pathophysiology
Total Questions : 39
Showing 10 questions Sign up for moreThe risk of developing coronary artery disease is increased up to threefold by
Explanation
Coronary artery disease (CAD) is a condition where the arteries that supply blood to the heart become narrowed or blocked due to a buildup of plaque. Several risk factors contribute to the development of CAD, including diabetes mellitus, hypertension, obesity, high alcohol consumption, smoking, and a family history of CAD.
Research suggests that individuals with diabetes mellitus are two to four times more likely to develop CAD than those without diabetes. This is because diabetes can lead to damage to the blood vessels and nerves that control the heart, as well as increased inflammation and high levels of blood glucose that can contribute to the buildup of plaque in the arteries.
While hypertension, obesity, and high alcohol consumption are also known risk factors for CAD, they generally do not increase the risk to the same degree as diabetes. Nonetheless, these factors can contribute to the development and progression of CAD and should be addressed through lifestyle modifications and medical interventions.
What is the usual source of pulmonary emboli
Explanation
A pulmonary embolism (PE) occurs when a blood clot, typically originating from the deep veins of the legs or pelvis, travels through the bloodstream and lodges in one of the pulmonary arteries in the lungs.
Deep venous thrombosis (DVT) is the most common source of pulmonary emboli. DVT occurs when a blood clot forms in the deep veins of the legs, pelvis, or arms, and can develop due to prolonged immobility, surgery, trauma, cancer, pregnancy, hormone therapy, or genetic factors.
Endocarditis, valvular heart disease, and left heart failure are not typical sources of pulmonary emboli. Endocarditis is an infection of the heart valves and lining, which can lead to valve damage and heart failure, but does not usually cause blood clots. Valvular heart disease, which includes conditions such as aortic stenosis and mitral regurgitation, can cause blood flow disturbances and increase the risk of thrombosis, but does not directly cause blood clots. Left heart failure, which occurs when the left ventricle of the heart is unable to pump effectively, can cause fluid buildup in the lungs, but does not typically cause blood clots to form.
A patient is diagnosed with pulmonary disease and elevated pulmonary valvular resistance. Which of the following heart failures may result from this condition?
Explanation
Elevated pulmonary valvular resistance refers to a condition where there is increased resistance to blood flow through the pulmonary valve and into the lungs. This can lead to an increase in pressure within the right ventricle of the heart, which can eventually lead to right heart failure.
Right heart failure occurs when the right ventricle of the heart is unable to pump blood effectively, which can result in symptoms such as fatigue, shortness of breath, and fluid retention in the legs and abdomen. Causes of right heart failure include pulmonary hypertension, chronic obstructive pulmonary disease (COPD), pulmonary embolism, and other conditions that increase pressure within the pulmonary circulation.
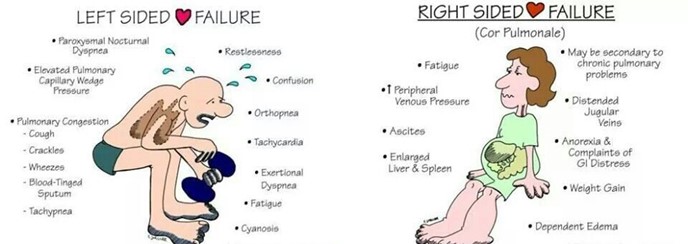
Left heart failure, on the other hand, occurs when the left ventricle of the heart is unable to pump blood effectively, which can lead to symptoms such as shortness of breath, fatigue, and fluid retention in the lungs and legs. Causes of left heart failure include coronary artery disease, hypertension, and valvular heart disease.
Low output failure occurs when the heart is unable to pump enough blood to meet the body's needs, and can result from a variety of conditions affecting the heart muscle or heart valves. High output failure occurs when the heart is working harder than normal to meet the body's demands, such as in conditions such as hyperthyroidism or severe anemia
What is the major effect of calcium channel blockers on cardiac contractions
Explanation
Calcium channel blockers (CCBs) are a class of medications that block the influx of calcium ions into cardiac and smooth muscle cells, leading to relaxation of these muscles and dilation of blood vessels.
In the heart, CCBs primarily affect the L-type calcium channels in the cardiac myocytes, which are responsible for the influx of calcium ions during the plateau phase of the cardiac action potential. By blocking these channels, CCBs decrease the amount of calcium that enters the cardiac myocytes, which in turn reduces the strength of cardiac contractions (i.e. contractility). 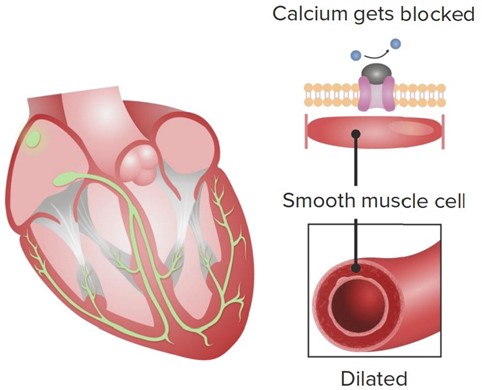
This reduction in contractility can be beneficial in certain conditions where the heart is working too hard or experiencing insufficient blood flow, such as in hypertension, angina, or some forms of arrhythmia. By reducing the workload of the heart, CCBs can help to lower blood pressure, decrease oxygen demand, and improve blood flow to the heart.
While CCBs can also have effects on the rate and rhythm of cardiac contractions, these effects are generally less pronounced than the reduction in contractility. Some CCBs, such as verapamil and diltiazem, can slow the heart rate by blocking the L-type calcium channels in the sinoatrial (SA) and atrioventricular (AV) nodes, while others, such as nifedipine, have little effect on heart rate.
The mitral and tricuspid valves close after the ventricles are filled with blood because the
Explanation
The mitral and tricuspid valves are located between the atria and ventricles in the heart, and they open and close to allow blood to flow in one direction through the heart. During diastole, when the heart is relaxed and filling with blood, the mitral and tricuspid valves are open to allow blood to flow from the atria into the ventricles.
Once the ventricles are filled with blood, they begin to contract during systole to pump the blood out to the lungs (right ventricle) and the rest of the body (left ventricle). As the ventricles contract, the pressure within them increases, which causes the mitral and tricuspid valves to be pushed closed by the blood within the ventricles. This closure prevents the backflow of blood into the atria during ventricular contraction (systole).
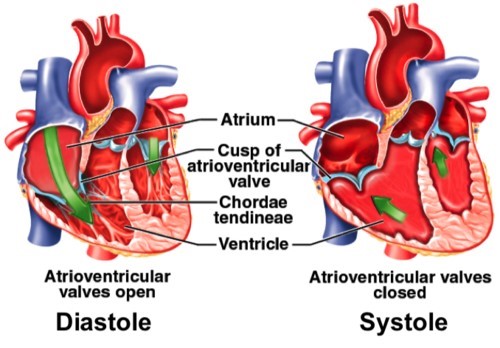
The chordae tendineae are thin, fibrous cords that connect the mitral and tricuspid valves to the papillary muscles within the ventricles. These structures help to anchor the valves in place during ventricular contraction, and prevent them from prolapsing (bulging back into the atria) and causing regurgitation (backflow of blood).
The trabeculae carneae are muscular ridges within the ventricles that help to increase the force of ventricular contraction, but they do not play a direct role in closing the mitral and tricuspid valves. Similarly, the reduced pressure in the atria during ventricular contraction is due to the fact that blood is being pumped out of the atria and into the ventricles, rather than the atria "pulling" the valves closed.
Explanation
Clubbing is a medical condition characterized by bulbous enlargement of the distal portion of a digit (usually a finger, but sometimes a toe) due to soft tissue proliferation and increased bone deposition. The affected digit takes on a rounded or "club-like" appearance, and the angle between the nail and nail bed (known as the Lovibond angle) increases to greater than 180 degrees.

Clubbing is commonly associated with a variety of medical conditions that interfere with oxygenation of the blood, including lung diseases such as chronic obstructive pulmonary disease (COPD), interstitial lung disease, and bronchiectasis; heart diseases such as congenital heart defects and cyanotic heart disease; and gastrointestinal diseases such as inflammatory bowel disease and cirrhosis.
The exact mechanism underlying clubbing is not fully understood, but it is thought to involve a combination of vascular, inflammatory, and neurogenic factors. Hypoxia (low oxygen levels) is believed to play a central role in the development
of clubbing, leading to the release of growth factors and cytokines that promote soft tissue and bone proliferation.
Clubbing is typically diagnosed based on physical examination findings, including the Lovibond angle and the presence of nail bed fluctuation (when the nail bed feels spongy or compressible). It is important to identify and treat any underlying medical conditions that may be contributing to clubbing, as these can have significant implications for the patient's health and quality of life.
Which elevated value may be protective of the development of atherosclerosis
Explanation
Atherosclerosis is a disease in which fatty deposits (plaques) build up in the walls of arteries, leading to narrowing and reduced blood flow. Elevated levels of certain lipids, including low density lipoprotein (LDL) cholesterol and triglycerides, are well-established risk factors for the development of atherosclerosis.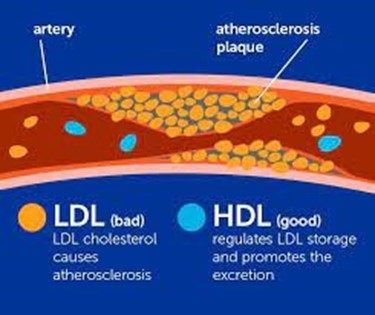
In contrast, high density lipoprotein (HDL) cholesterol has been shown to have a protective effect against atherosclerosis. HDL is often referred to as "good cholesterol" because it helps to transport excess cholesterol from peripheral tissues (including the walls of arteries) back to the liver for processing and excretion. HDL also has anti-inflammatory and antioxidant properties that may help to reduce the risk of atherosclerosis.
In general, higher levels of HDL cholesterol are associated with a lower risk of cardiovascular disease and atherosclerosis. However, the protective effect of HDL may vary depending on other factors such as smoking, obesity, and diabetes. It is important to maintain a healthy balance of lipids in the bloodstream, including a high level of HDL and low levels of LDL and triglycerides, in order to reduce the risk of atherosclerosis and other cardiovascular diseases.
Which of the following type of croup is most common
Explanation
Croup is a common respiratory illness in young children, characterized by inflammation of the upper airways (including the larynx and trachea) that leads to a characteristic barking cough and difficulty breathing. Croup is most commonly caused by viral infections, particularly parainfluenza virus, although other viruses such as respiratory syncytial virus (RSV) and influenza virus can also be responsible. 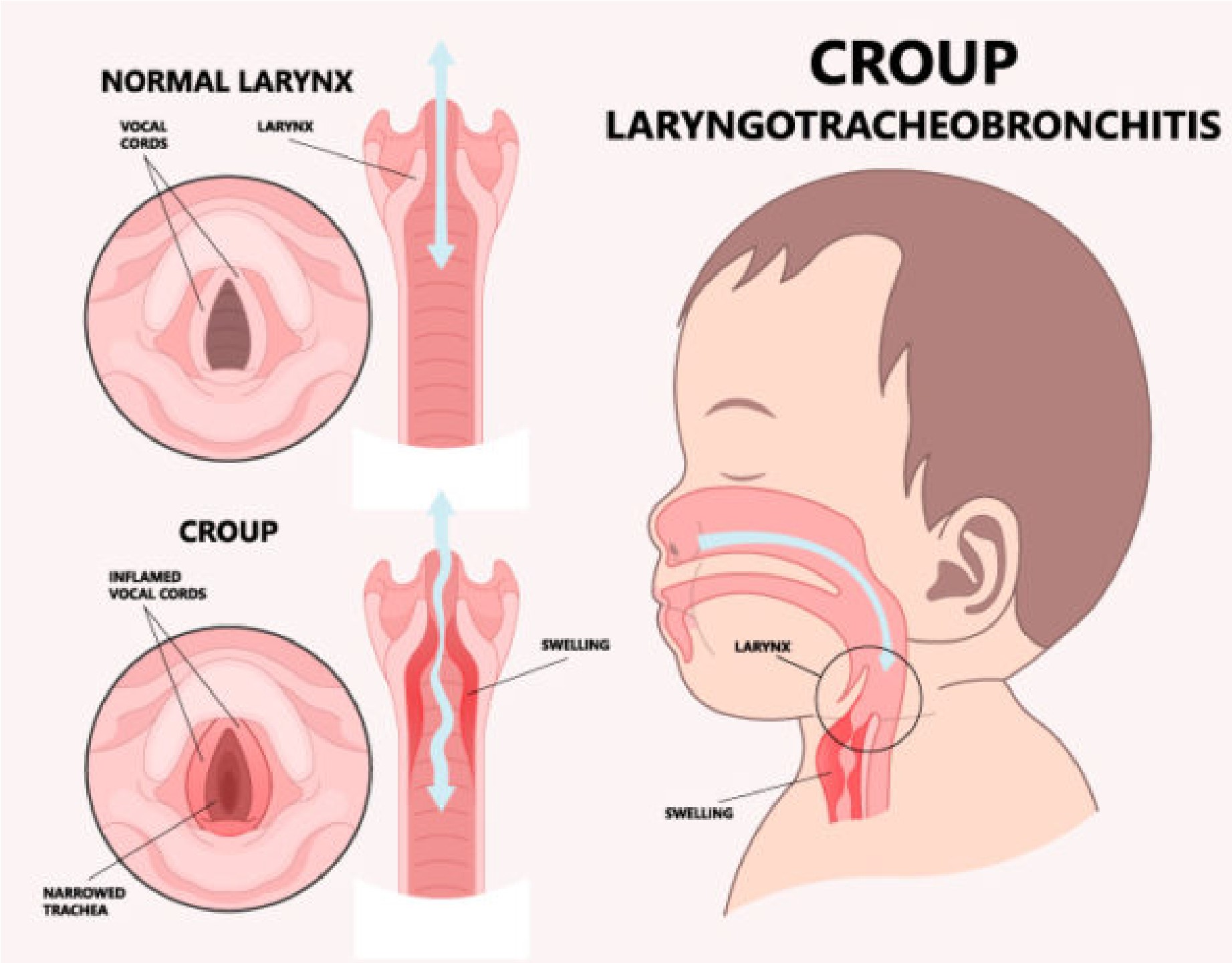
Bacterial croup is rare and usually occurs in children who have an underlying condition that makes them more susceptible to bacterial infections, such as immunodeficiency or a history of recurrent respiratory infections. Fungal croup is also rare and usually occurs in children with a weakened immune system or a history of exposure to contaminated soil or other environmental sources of fungi.
Autoimmune croup is not a recognized medical condition. While some autoimmune disorders can affect the respiratory system (such as systemic lupus erythematosus), they do not typically cause croup-like symptoms.
Patient wants to know what causes atherosclerosis. How should the nurse respond? In general, atherosclerosis is caused by
Explanation
Atherosclerosis is a complex disease process that involves the gradual buildup of plaques (fatty deposits) in the walls of arteries, leading to narrowing and reduced blood flow. The exact cause of atherosclerosis is not fully understood, but it is thought to involve a combination of genetic, lifestyle, and environmental factors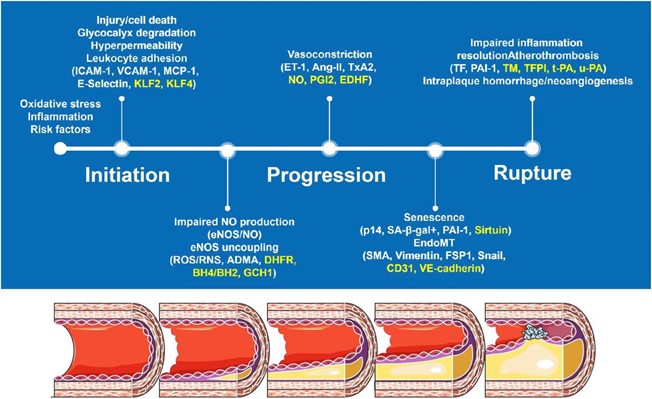
One of the key contributing factors to atherosclerosis is damage to the endothelial cells that line the walls of arteries. This damage can be caused by a variety of factors, including high blood pressure, smoking, high levels of lowdensity lipoprotein (LDL) cholesterol, and other inflammatory factors. When the endothelial cells are damaged, they release chemicals that attract white blood cells to the area. These white blood cells then migrate into the arterial wall, where they begin to accumulate and form fatty deposits called plaques.
Over time, these plaques can grow and calcify, leading to further narrowing of the artery and reducing blood flow to the affected tissue. In addition, plaques can rupture and form blood clots, which can completely block blood flow to the affected area and cause a heart attack or stroke.
While high serum cholesterol levels are a risk factor for atherosclerosis, they are not the sole cause. Similarly, an increase in antithrombotic substances (substances that prevent blood clots) and congenital heart disease are not primary causes of atherosclerosis, although they may contribute to the disease process in some cases.
The progression of chronic bronchitis is best halted by?
Explanation
Chronic bronchitis is a type of chronic obstructive pulmonary disease (COPD) that is characterized by inflammation and narrowing of the bronchial tubes, which can lead to symptoms such as cough, shortness of breath, and wheezing. The primary cause of chronic bronchitis is smoking, and the most effective way to halt its progression is by quitting smoking.
Smoking cessation is the cornerstone of treatment for chronic bronchitis, as continued smoking can worsen inflammation in the airways and accelerate the progression of the disease. In addition to smoking cessation, other treatments may include bronchodilators (such as albuterol) to help open the airways and improve breathing, postural chest drainage techniques to help clear mucus from the lungs, and antibiotics to treat bacterial infections.
While these treatments can help manage symptoms and prevent complications, they are not as effective as smoking cessation in halting the progression of chronic bronchitis. Therefore, it is important for individuals with chronic bronchitis to quit smoking as soon as possible to slow the disease process and improve their overall health.
You just viewed 10 questions out of the 39 questions on the Pathophysiology Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



