LPN Med Surg Cohort 6 Exam
ATI LPN Med Surg Cohort 6 Exam
Total Questions : 48
Showing 10 questions Sign up for moreA nurse teaches a patient who is at risk for mild hypernatremia. Which statement does the nurse include in this patient's teaching?
Explanation
A. "Bake or grill the meat rather than frying it."
This statement is more related to reducing fat intake rather than managing sodium levels. While reducing fried foods can be beneficial for overall health, it doesn't directly address the issue of sodium intake, which is crucial in managing hypernatremia.
B. “Check your radial pulse twice a day.”
Checking the radial pulse is a method used to monitor heart rate and rhythm. It is not directly related to managing sodium levels or hypernatremia. Although monitoring vital signs is important in general health care, it is not specific to addressing mild hypernatremia.
C. "Read food labels to determine sodium content."
This statement is the correct choice. Managing sodium intake is a key component in managing hypernatremia. Reading food labels helps patients identify high-sodium foods and make choices that are lower in sodium content, which can be crucial in preventing or managing mild hypernatremia.
D. “Weigh yourself every morning and every night."
While regular weight monitoring can be important for certain health conditions, it is not directly related to managing mild hypernatremia. Weight changes may occur with fluid retention or loss, but monitoring sodium intake and hydration status is more directly relevant to managing hypernatremia.
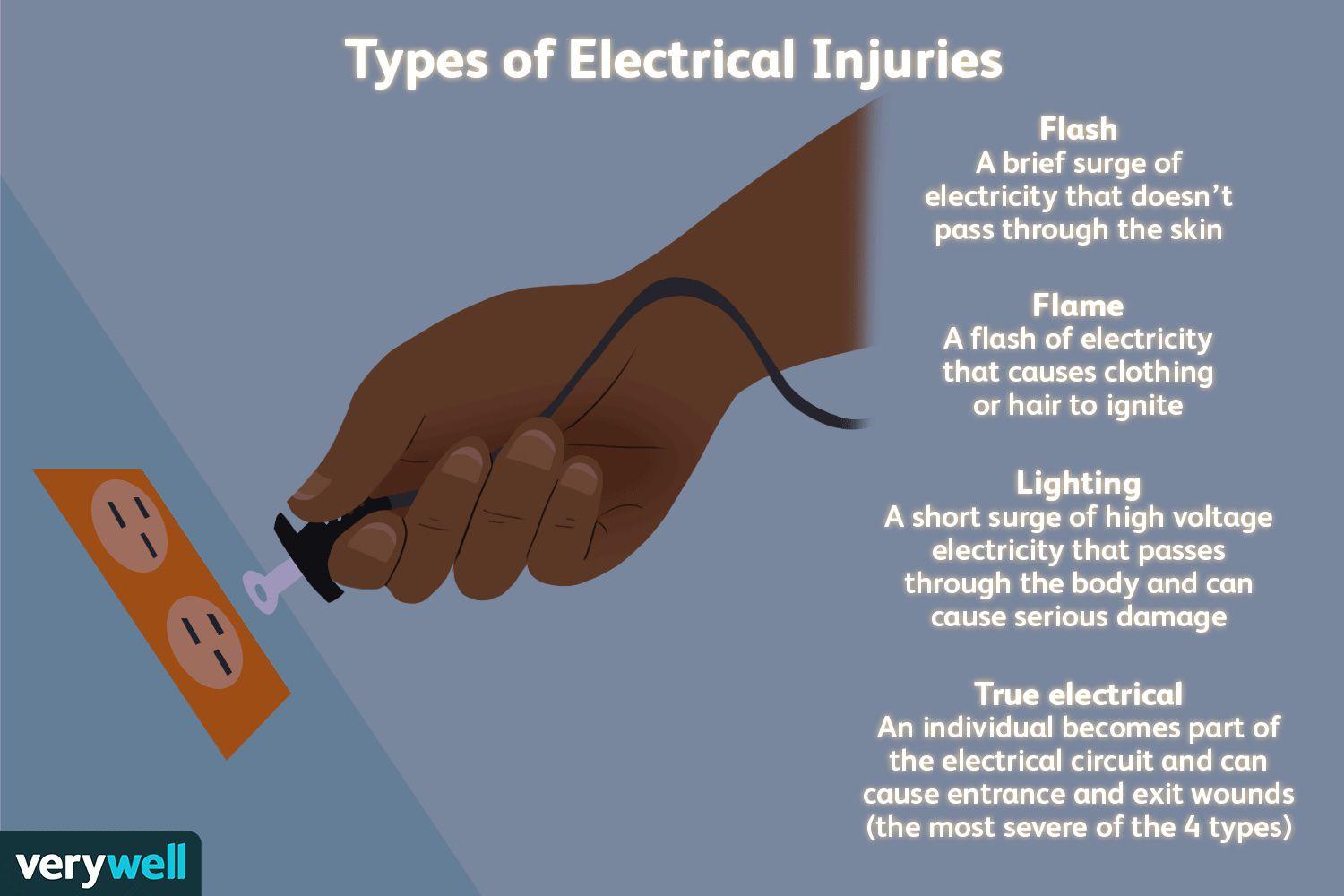
A nurse is caring for a client with an electrical burn. The client states that since the wound on the skin is small, the burn must not be too bad. Which of the following is the best response by the nurse?
Explanation
A. Electrical burns can have small amounts of skin damage, but more extensive damage beneath the skin.
This response is the best choice because it educates the client about the potential for deeper tissue damage associated with electrical burns. It acknowledges that while the burn on the skin may appear small, the damage underneath could be more extensive, affecting muscles, nerves, and blood vessels.
B. Electrical burns commonly cause reddened/purplish skin without blistering.
This statement is not the best response because it focuses solely on the appearance of the skin without addressing the potential for deeper tissue damage. While it is true that electrical burns can present with reddened or purplish skin without blistering, this response does not provide comprehensive information about the nature and severity of electrical burns.
C. Electrical burns typically are minor.
This response is incorrect because it downplays the seriousness of electrical burns. While some electrical burns may indeed be minor, others can cause significant tissue damage and complications. It's important for the nurse to educate the client about the range of severity that electrical burns can present.
D. Electrical burns usually cause much more skin damage than what can be seen on your skin.
This statement is partially accurate but does not provide as much information as choice A. While it acknowledges that electrical burns can cause more damage than what is visible on the skin's surface, it doesn't emphasize the potential for deeper tissue damage as effectively as choice A does.
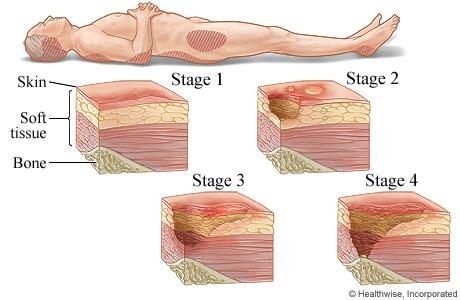
A nurse is caring for a client that is immobile. The nurse recognizes that the appearance of non-blanchable erythema on the heels most likely indicates which of the following stages of pressure injuries?
Explanation
A. Stage III pressure injury
Stage III pressure injuries involve full-thickness skin loss, extending into the subcutaneous tissue but not through the fascia. These wounds typically present as deep craters and may involve undermining or tunneling. Non-blanchable erythema alone without visible skin loss is not characteristic of a Stage III pressure injury.
B. Stage IV pressure injury
Stage IV pressure injuries are the most severe and involve full-thickness tissue loss with exposed bone, tendon, or muscle. These wounds often have extensive tissue damage and can be difficult to manage. Again, non-blanchable erythema without visible skin loss is not indicative of a Stage IV pressure injury.
C. Stage II pressure injury
Stage II pressure injuries involve partial-thickness skin loss with damage to the epidermis and possibly the dermis. These wounds often present as shallow open ulcers or blisters and may have characteristics such as intact or ruptured blisters. While Stage II injuries can present with erythema, non-blanchable erythema specifically indicates a Stage I injury.
D. Stage I pressure injury
Stage I pressure injuries are the earliest stage and involve non-blanchable erythema of intact skin. The skin may be warmer or cooler than surrounding tissue and may have changes in sensation. There is no visible skin loss at this stage, but the area is at risk for further injury if pressure is not relieved. Therefore, non-blanchable erythema on the heels most likely indicates a Stage I pressure injury.
A nurse is caring for a client who has sustained a gasoline burn to 25% of the body. Which of the following is a priority safety concern when caring for this client?
Explanation
A. Elevation of the head of the bed by 30 degrees: While elevation of the head of the bed may be necessary for certain medical conditions, it is not the priority concern in a client with a gasoline burn. Decontamination and assessment of the burn injury take precedence.
B. Determining the amount of gasoline that the client encountered: While it's important to gather information about the circumstances of the injury, including the amount of gasoline involved, this is not the priority concern at the immediate moment. Decontamination and assessment of the burn take precedence over obtaining historical information.
C. Asking the client when they last ate a meal: While assessing the client's nutritional status and potential need for dietary interventions is important, it is not the priority safety concern in the context of a gasoline burn. Decontamination and assessment of the burn injury are more critical at this time.
D. Decontamination of the client
When a client sustains a gasoline burn, the priority safety concern is to decontaminate the client. Gasoline can cause chemical burns and can be absorbed through the skin, leading to systemic effects. Therefore, it's crucial to remove any remaining gasoline from the client's skin and clothing to prevent further absorption and minimize the risk of complications.
A nurse is caring for a client with a pressure injury. Which of the following should the nurse recognize as a priority in the plan of care?
Explanation
A. Keeping the wound clean and non-infected: When caring for a client with a pressure injury, the priority in the plan of care is to keep the wound clean and prevent infection. This involves regular wound assessment, proper wound cleaning techniques, application of appropriate dressings, and monitoring for signs of infection such as increased redness, swelling, warmth, or drainage. Preventing infection is crucial for promoting healing and preventing complications.
B. Application of a negative pressure wound care device: While negative pressure wound therapy (NPWT) can be beneficial in promoting wound healing, it may not be the immediate priority unless specifically indicated by the healthcare provider based on the stage and characteristics of the pressure injury. Keeping the wound clean and preventing infection take precedence over NPWT in the initial plan of care.
C. Client education on wound prevention: While client education is important for preventing future pressure injuries, it is not the immediate priority when caring for an existing pressure injury. The focus initially should be on managing the current wound to promote healing and prevent complications.
D. Promoting a high carbohydrate, low protein diet: Nutritional interventions are important in wound healing, but promoting a specific diet is not the immediate priority in the plan of care for a pressure injury. Providing adequate nutrition and addressing any nutritional deficiencies may be part of the overall plan, but it is secondary to keeping the wound clean and preventing infection.
The nurse takes a client's temperature before giving a blood transfusion. The temperature is 100 F orally. The nurse reports the finding to the registered nurse (RN) and anticipates that which action will take place?
Explanation
A. The transfusion will begin after the administration of 650 mg of acetaminophen (Tylenol).
This option suggests that the nurse would administer acetaminophen to lower the client's temperature and then proceed with the blood transfusion. While acetaminophen can be used to reduce fever, the decision to administer medication should be made by the healthcare provider after assessing the client's overall condition and determining the cause of the fever. Administering medication without proper evaluation and orders from the healthcare provider is not appropriate.
B. The blood will be held, and the health care provider will be notified.
This option is the correct choice. When a client has an elevated temperature before a blood transfusion, it is standard practice to hold the transfusion and notify the healthcare provider. An elevated temperature could indicate an underlying infection or another condition that needs to be evaluated before proceeding with the transfusion to ensure the client's safety.
C. The transfusion will begin after the administration of an antihistamine.
Administering an antihistamine would not be the appropriate action in response to an elevated temperature before a blood transfusion. Antihistamines are typically used to treat allergic reactions, not fevers. Holding the transfusion and notifying the healthcare provider to assess the situation would be the correct course of action.
D. The transfusion will begin as prescribed.
This option is not appropriate because starting the transfusion without addressing the elevated temperature could pose risks to the client's health. Elevated temperatures may indicate an underlying infection or other conditions that need to be evaluated before proceeding with the transfusion. Holding the transfusion and seeking further guidance from the healthcare provider is the recommended action in this scenario.
A frail, older adult home health patient who had chickenpox as a child has been exposed to varicella (chickenpox) several days ago. What should the nurse do?
Explanation
A. Arrange for the patient to receive gamma globulin.
Gamma globulin is a blood product that contains antibodies and is sometimes used for post-exposure prophylaxis in certain situations, such as for individuals who are immunocompromised or pregnant and have been exposed to varicella (chickenpox) or measles. However, for a frail, older adult who had chickenpox as a child and has been exposed to varicella again, arranging for gamma globulin may not be necessary if the patient is already immune to chickenpox.
B. Assess frequently for herpes zoster.
Herpes zoster (shingles) is caused by the reactivation of the varicella-zoster virus, the same virus that causes chickenpox. While exposure to varicella can increase the risk of developing shingles in individuals who are susceptible, frequent assessment for herpes zoster is not necessary in this case if the patient is known to have had chickenpox in the past.
C. Be aware of the patient's immunity to chickenpox.
This option is the correct choice. Since the patient had chickenpox as a child, they likely have immunity to chickenpox. Being aware of this immunity helps the nurse understand that the patient may not develop chickenpox again even after exposure to varicella.
D. Encourage the patient to have a pneumonia vaccine.
Encouraging the patient to have a pneumonia vaccine is unrelated to the immediate concern of exposure to varicella. While pneumonia vaccines are important for older adults, especially those who are frail, the priority in this scenario is to determine the patient's immunity to chickenpox due to prior infection.
A patient is prescribed oral acyclovir for type 1 herpes simplex virus. What is the expected outcome if the patient is compliant with the medication regimen?
Explanation
A. Prevents complications, such as meningitis or pneumonitis
While oral acyclovir can be effective in managing HSV infections and reducing the severity of symptoms, it is not primarily used to prevent complications such as meningitis or pneumonitis. These complications may occur in severe cases of HSV infections, but oral acyclovir's main goal is to manage outbreaks and reduce symptoms.
B. Decreases the probability of recurrent outbreaks
Oral acyclovir can help reduce the frequency of recurrent outbreaks in individuals with HSV infections. However, it does not completely eliminate the probability of recurrent outbreaks. Some individuals may still experience occasional outbreaks even with regular use of oral acyclovir. The medication is more focused on managing outbreaks when they occur rather than preventing them entirely.
C. Shortens the outbreak and lessens the severity of symptoms
This option is the correct choice. Oral acyclovir is effective in shortening the duration of HSV outbreaks and reducing the severity of symptoms such as pain, itching, and lesions. It works by inhibiting the replication of the virus, which helps in faster healing and symptom relief. However, it does not cure the infection or eliminate the virus from the body.
D. Eliminates the likelihood of spreading the infection to others
While oral acyclovir can help manage outbreaks and reduce viral shedding, it does not completely eliminate the risk of spreading the infection to others. It can reduce the likelihood of transmission during active outbreaks, but individuals with HSV can still shed the virus and be contagious even when they are not experiencing visible symptoms. Therefore, other precautions such as practicing safe sex and avoiding close contact during outbreaks are also important for preventing transmission.
A nurse is caring for a client during the fluid resuscitation phase of burn management. Which of the following is the best method for assessing the results of the fluid resuscitation?
Explanation
A. Urine output is greater than 0.5 mL/kg/hr
During the fluid resuscitation phase of burn management, one of the primary goals is to maintain adequate tissue perfusion and organ function by ensuring sufficient fluid intake. The best method for assessing the results of fluid resuscitation is by monitoring urine output. A urine output of greater than 0.5 mL/kg/hr is indicative of adequate renal perfusion and kidney function, suggesting that fluid resuscitation is effective in maintaining tissue perfusion and preventing complications such as acute kidney injury.
B. Serum hemoglobin is 11 gm/dL
Serum hemoglobin levels can be affected by various factors, including fluid resuscitation, blood loss, and other medical conditions. While monitoring hemoglobin levels is important in overall patient assessment, it is not the best method specifically for assessing the results of fluid resuscitation during the initial phase of burn management.
C. Breath sounds are clear bilaterally
Clear bilateral breath sounds indicate adequate lung function and ventilation but may not directly reflect the effectiveness of fluid resuscitation in maintaining tissue perfusion. Lung sounds can be influenced by factors such as lung injury from smoke inhalation or mechanical ventilation settings, which may not correlate directly with fluid resuscitation outcomes.
D. Heart rate is 122/min
Heart rate can be influenced by various factors such as pain, stress, medications, and underlying medical conditions. While monitoring heart rate is important in assessing patient status, it is not the most reliable method for specifically evaluating the results of fluid resuscitation during the fluid resuscitation phase of burn management.
A nurse recently hired to the preoperative area learns that certain patients are at higher risk for venous thromboembolism (VTE). Which patients are considered to be at high risk? (Select all that apply.)
Explanation
A. Morbidly obese patient: Obesity is a known risk factor for VTE due to several reasons. Morbidly obese individuals often have impaired mobility, which can lead to venous stasis (sluggish blood flow in the veins). Additionally, obesity is associated with inflammation and changes in blood clotting factors, increasing the risk of developing blood clots in the veins.
B. A woman who smokes and takes oral contraceptives or smokes: Both smoking and oral contraceptive use are independent risk factors for VTE. Smoking can cause damage to blood vessels and alter blood clotting mechanisms, while oral contraceptives can increase the risk of blood clots due to hormonal changes.
C. Wheelchair-bound patient: While being wheelchair-bound alone may not always indicate a high risk for VTE, immobility is a significant risk factor for developing blood clots. Prolonged periods of immobility can lead to blood stasis in the veins, making wheelchair-bound patients susceptible to VTE, especially if other risk factors are present.
D. Patient with a humerus fracture: A humerus fracture on its own may not necessarily increase the risk of VTE significantly. However, if the fracture requires immobilization or surgery, especially if it affects the lower extremities or leads to prolonged immobility, the risk of VTE can increase due to decreased blood flow and stasis.
E. Patient who underwent a prolonged surgical procedure: Prolonged surgical procedures often involve anesthesia, immobility during surgery, and postoperative immobilization, all of which can contribute to venous stasis and increase the risk of developing VTE. Additionally, the surgical trauma itself can trigger inflammatory responses and alterations in blood clotting factors, further elevating the risk of blood clots.
You just viewed 10 questions out of the 48 questions on the ATI LPN Med Surg Cohort 6 Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



