Ati Lpn Med Surg Concept 2 Proctored Exam
Ati Lpn Med Surg Concept 2 Proctored Exam
Total Questions : 46
Showing 10 questions Sign up for moreWhich time would be ideal for the LPN/LVN to collect a sputum specimen?
Explanation
B. Morning is considered the ideal time for collecting a sputum specimen. Overnight, mucus accumulates in the respiratory tract because the patient is less active and not clearing their throat or coughing as much. This means that the mucus is more concentrated and has had time to build up, providing a more substantial and representative sample of what is in the lungs.
A. Collecting a sputum specimen at bedtime is generally not ideal. By the end of the day, the patient’s respiratory tract might have cleared some of the accumulated mucus naturally through coughing or other activities.
C. Collecting a sputum specimen after meals is not recommended. Eating can introduce food particles and bacteria from the mouth into the sputum, contaminating the sample.
D. Starting antibiotics before collecting a sputum specimen can alter the bacterial flora present in the respiratory tract. This can lead to a false-negative result or an inaccurate representation of the pathogens causing the infection.
Which patient does the LPN/LVN identify at high risk for hospital-acquired pneumonia?
Explanation
C. This patient is at high risk for hospital-acquired pneumonia. After a splenectomy (removal of the spleen), patients may experience pain and discomfort, which can make them reluctant to perform necessary activities like coughing and deep breathing. These activities are crucial for preventing lung complications such as atelectasis and pneumonia.
A. This patient is actively using an incentive spirometer, which is a device that encourages deep breathing and helps keep the lungs clear. This practice significantly reduces the risk of developing pneumonia by preventing atelectasis (collapse of part of the lung) and promoting lung expansion.
B. This patient is out of bed and eating, which indicates they are relatively mobile and maintaining normal respiratory function. Rhinoplasty, a surgical procedure on the nose, generally does not impair lung function or significantly increase the risk of pneumonia. Being active and upright further reduces the risk of HAP.
D. This patient is actively ambulating, which is highly beneficial for lung function and overall recovery. Walking and moving around helps to prevent respiratory complications, including pneumonia, by promoting lung expansion and circulation.
A nurse is reinforcing discharge teaching with a client following an episode of status asthmaticus. The client has a prescription for two inhalations from an albuterol metered-dose inhaler. Which of the following statements by the client indicates an understanding of the teaching?
Explanation
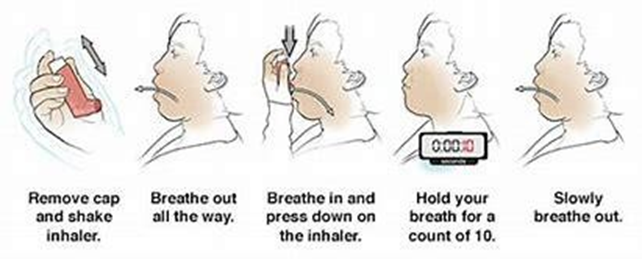
A. Holding the breath for at least 10 seconds after inhaling the medication allows the medication to settle in the lungs and increases its effectiveness. This ensures maximum delivery of the drug to the respiratory tract.
B. The recommended time to wait between inhalations is typically around 1 to 2 minutes, not 10 minutes. Waiting too long between puffs may reduce the effectiveness of the medication and is not necessary.
C. There is no specific recommendation that the inhaler must be held with the non-dominant hand. The inhaler should be held in the hand that feels most comfortable and provides the best control, which is usually the dominant hand for most people.
D. The correct technique involves tilting the head slightly back to open the airway, making it easier for the medication to reach the lungs. Tilting the head forward could restrict the airflow and reduce the effectiveness of the inhalation.
The nurse is teaching a patient recently diagnosed with type 1 diabetes mellitus (DM) about the disease. What information should the nurse include?
Explanation
A. Type 1 diabetes is an autoimmune condition where the body's immune system attacks and destroys the insulin-producing beta cells in the pancreas. As a result, the pancreas produces little to no insulin, which is essential for regulating blood glucose levels.
B. Type 1 diabetes is not reversible. It is a lifelong condition that requires ongoing management with insulin therapy. While diet, exercise, and weight management are important for overall health and can help manage blood glucose levels, they cannot reverse type 1 diabetes.
C. This description is characteristic of type 2 diabetes, not type 1. In type 2 diabetes, the body’s cells become resistant to the effects of insulin, and the pancreas may not produce enough insulin. In type 1 diabetes, the problem is the lack of insulin production due to autoimmune destruction of the pancreatic beta cells.
D. Insulin is not released into the gastrointestinal tract. Insulin is a hormone that is released into the bloodstream by the pancreas. Its primary role is to help regulate blood glucose levels by facilitating the uptake of glucose into the body's cells for energy.
A nurse is reinforcing teaching for a client who has a duodenal ulcer and a new prescription for sucralfate. The client asks the nurse how sucralfate works. Which of the following statements should the nurse make?
Explanation
A. Sucralfate works by forming a protective barrier over the ulcer site. It adheres to the ulcer, shielding it from the harmful effects of gastric acid, pepsin, and bile salts. This protection allows the ulcer to heal by preventing further irritation and damage.
B. Medications that prevent gastric acid secretion are typically proton pump inhibitors (PPIs) or H2 receptor antagonists. Sucralfate does not reduce or inhibit the production of gastric acid; instead, it protects the ulcer from the acid already present.
C. Antacids are the type of medication that neutralize gastric acid. Sucralfate does not neutralize acid; it acts locally at the ulcer site to create a protective coating.
D. Antibiotics are used to kill Helicobacter pylori, the bacteria often responsible for causing peptic ulcers. Sucralfate does not have antibacterial properties and does not target or eliminate bacteria.
A nurse is collecting data from a client who has gastroesophageal reflux disease (GERD) and reports having heartburn every night. Which of the following actions should the nurse identify as a contributing factor to the client's heartburn?
Explanation
B. Orange juice is highly acidic and can irritate the esophagus, leading to increased heartburn symptoms. Regular consumption of acidic beverages like orange juice can exacerbate GERD symptoms, making this a likely contributing factor to the client's heartburn.
A. Consuming low-fat meats is generally not a contributing factor to heartburn. Low-fat meats are less likely to cause reflux compared to high-fat foods, which can relax the lower esophageal sphincter and increase the risk of acid reflux.
C. Eating dinner early in the evening is generally recommended for managing GERD. This practice allows more time for the stomach to empty before lying down to sleep, reducing the likelihood of acid reflux during the night.
D. Sleeping on a large wedge-style pillow is also generally recommended for managing GERD. Elevating the head and upper body during sleep can help prevent acid from flowing back into the esophagus.
A nurse is reinforcing teaching with the parents of a child who is starting to use a spacer with a metered-dose inhaler (MDI) to treat asthma. Which of the following information should the nurse include in the teaching?
Explanation
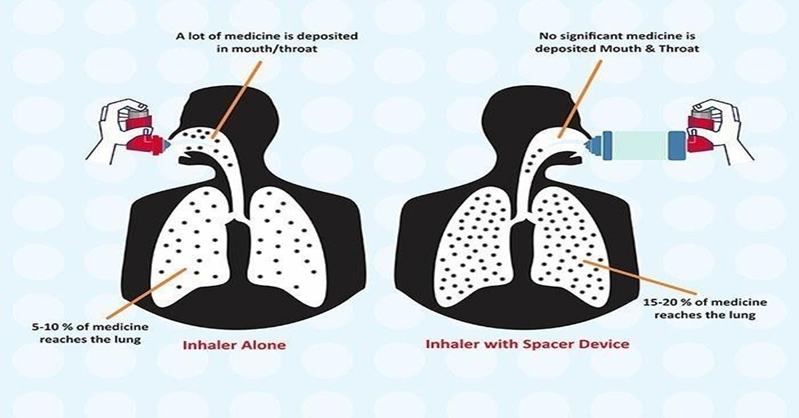
C. The spacer helps to deliver more medication to the lungs by holding the medication in the chamber, allowing the patient to inhale it more slowly and deeply. This results in better deposition of the medication in the lower airways and reduces the amount of medication that is deposited in the mouth and throat.
A. The primary purpose of the spacer is to increase the amount of medication that reaches the lungs and to reduce the amount deposited in the oropharynx (throat). The spacer helps to ensure that more medication is delivered directly to the airways where it is needed, thereby enhancing the effectiveness of the treatment and reducing side effects.
B. The exhalation slots or vents on a spacer are designed to allow the patient to exhale easily without removing the device from the mouth. The lips should form a tight seal around the mouthpiece of the spacer to ensure effective inhalation, but the exhalation slots should not be intentionally covered.
D. When using a spacer with an MDI, the patient should inhale slowly and deeply. Rapid inhalation can cause the medication to be deposited in the upper airways rather than reaching the lungs. A slow and deep inhalation allows for better medication delivery to the lower airways.
Which breakfast menu is most appropriate for a patient with diabetes?
Explanation
A. Oatmeal is a good source of fiber, which can help manage blood sugar levels. Whole-grain toast provides complex carbohydrates and fiber, and using an artificial sweetener in oatmeal reduces sugar intake. Tea is a good beverage choice as it does not contain sugar or calories if not sweetened.
B. This option is less appropriate for a patient with diabetes. While eggs are a good source of protein, bacon is high in saturated fat and sodium, which is not ideal for cardiovascular health. Orange juice contains a high amount of natural sugar and can cause a rapid increase in blood glucose levels. Coffee is fine if consumed without sugar or high-fat creamers.
C. Whole-grain toast with peanut butter provides fiber, protein, and healthy fats, which are beneficial. Skim milk is a good source of calcium and protein. However, the inclusion of orange juice is problematic due to its high sugar content, which can spike blood sugar levels.
D. While grapefruit is a low-sugar fruit, cranberry juice often contains added sugars and can increase blood glucose levels. A bagel, even with sugar-free jelly, is high in refined carbohydrates, which can cause a rapid rise in blood sugar.
A patient is admitted to a respiratory unit with a diagnosis of bacterial pneumonia. Findings include a fever and a weak, congested-sounding cough with moist crackles throughout the lung fields. How should the nurse prioritize care?
Explanation
B. The inability to clear the airway is a critical issue. This patient has a weak, congested-sounding cough and moist crackles, indicating that secretions are present and not being effectively cleared. This can lead to airway obstruction, decreased oxygenation, and further respiratory complications. Clearing the airway is a top priority to ensure the patient can breathe properly and prevent further deterioration.
A. Difficulty breathing (dyspnea) is a serious concern as it can indicate respiratory distress or failure. However, it is often a symptom rather than a primary issue, and its underlying causes (such as an inability to clear the airway or inadequate oxygen levels) must be addressed first.
C. Confusion can result from high fever, infection, or hypoxia. While it is important to address the fever and its underlying cause, confusion itself is usually a secondary issue. Addressing the primary respiratory issues will often improve the patient's mental status as well.
D. Hypoxia can result from severe pneumonia, and resolving it involves ensuring the patient has a clear airway and adequate ventilation. Measuring and correcting oxygen levels (e.g., with supplemental oxygen) is crucial, but the underlying cause (such as airway obstruction) must also be managed.
A patient with type 1 DM expresses concern about developing retinopathy due to a chronic disease. How should the nurse reply?
Explanation
C. Good control of blood glucose levels and blood pressure is essential in reducing the risk of diabetic retinopathy and its progression. Research has shown that maintaining tight glycemic control and managing hypertension can significantly decrease the likelihood and severity of retinopathy in patients with diabetes.
A. Laser surgery is a treatment option for certain complications of diabetic retinopathy, such as retinal hemorrhage or retinal detachment. However, it's essential to emphasize that prevention through good glycemic control and regular eye exams is key to reducing the risk of these complications, rather than relying solely on surgical interventions after they occur.
B. Cataracts are more common in individuals with diabetes and can be surgically corrected but this statement does not directly address the concern about retinopathy. Cataracts and retinopathy are separate ocular complications of diabetes, each requiring different management strategies.
D. Diabetes remains one of the leading causes of blindness in the United States, primarily due to its association with diabetic retinopathy. While advancements in diabetes management and eye care have helped reduce the incidence of blindness, it is still a significant concern for individuals with diabetes.
You just viewed 10 questions out of the 46 questions on the Ati Lpn Med Surg Concept 2 Proctored Exam Exam. Subscribe to our Premium Package to obtain access on all the questions and have unlimited access on all Exams. Subscribe Now



