Please set your exam date
Brain Tumors
Study Questions
Practice Exercise 1
A nurse is caring for a patient with a newly diagnosed brain tumor. The primary reason a brain tumor, whether benign or malignant, causes significant neurological symptoms is due to:
Explanation
Brain tumors, whether benign or malignant, produce neurological symptoms mainly because they occupy space within the rigid skull, leading to compression of brain tissue and increased intracranial pressure (ICP). Even benign tumors can be life-threatening because they displace or infiltrate brain tissue, disrupting normal neurological function. The severity of symptoms depends on the tumor’s size, location, and rate of growth, rather than its ability to produce toxins or trigger systemic inflammation.
Rationale for correct answer:
C. The compression and infiltration of brain tissue, leading to increased intracranial pressure: This is the primary mechanism for neurological symptoms in brain tumors. Space-occupying effects compromise blood flow, damage neurons, and can result in herniation if untreated.
Rationale for incorrect answers:
A. The tumor's ability to produce toxins that poison brain cells: Brain tumors do not release toxins; their effects are due to mechanical compression and infiltration.
B. Its ability to create an inflammatory response throughout the body: Brain tumors cause local effects in the CNS rather than widespread systemic inflammation.
D. The breakdown of the blood-brain barrier, allowing harmful substances to enter the brain: While tumors may affect the blood-brain barrier, this is not the primary cause of neurological symptoms.
Take home points
- Brain tumor symptoms are caused by compression, infiltration, and rising ICP, not toxin release.
- Benign tumors can still be dangerous if they displace critical brain structures.
- Early detection and ICP management are essential to prevent permanent neurological damage.
A nurse is caring for a client who has a benign brain tumor. The client asks the nurse if he can expect this same type of tumor to occur in other areas of his body. Which of the following is an appropriate response by the nurse?
Explanation
Benign brain tumors are noncancerous growths that develop only within the brain tissue and do not metastasize to other parts of the body. Unlike malignant tumors, they remain localized but can still cause significant neurological symptoms by compressing nearby brain structures. Educating patients about the localized nature of benign tumors helps reduce anxiety and clarify the difference from metastatic brain cancer.
Rationale for correct answer:
C. It is limited to brain tissue: Benign brain tumors do not spread to other organs. They grow locally and only affect surrounding brain structures.
Rationale for incorrect answers:
A. It can spread to breasts and kidneys: Benign tumors do not metastasize to other organs; only malignant tumors have this capability.
B. It can develop in your GI tract: Tumors in the gastrointestinal tract would be separate conditions and are unrelated to a primary brain tumor.
D. It probably started in another area of your body and spread to your brain: This describes metastatic brain cancer, not a benign primary tumor.
Take home points
- Benign brain tumors remain localized and do not metastasize.
- They may still cause neurological problems due to compression.
- Patient education helps reduce fear and clarify tumor behavior.
Which statement correctly differentiates between a primary and a metastatic brain tumor?
Explanation
Brain tumors are classified as primary or metastatic based on where they originate. Primary brain tumors develop from cells within the brain or meninges, whereas metastatic brain tumors spread from cancers in other organs, such as the lungs, breast, or kidneys. Understanding this distinction is essential for diagnosis, treatment planning, and prognosis, as metastatic tumors often indicate systemic cancer progression.
Rationale for correct answer:
B. Primary tumors originate from cells within the brain, while metastatic tumors originate elsewhere and spread to the brain: This is the fundamental difference between the two types. It guides diagnostic evaluation and affects the overall treatment approach.
Rationale for incorrect answers:
A. Primary tumors are more common in adults, while metastatic tumors are more common in children: The opposite is generally true; metastatic tumors are more common in adults, and some primary brain tumors (like medulloblastoma) are more common in children.
C. Primary tumors are always malignant, and metastatic tumors are always benign: Both primary and metastatic tumors can be malignant, and benign metastatic tumors do not exist.
D. Primary tumors are typically easier to treat than metastatic tumors due to their slower growth rate: Treatment difficulty depends on tumor type, location, and accessibility, not simply growth rate.
Take home points
- Primary tumors originate in the brain, while metastatic tumors spread from another organ.
- Metastatic tumors are more common in adults and usually indicate systemic cancer spread.
- Tumor origin influences prognosis, treatment options, and long-term outcomes.
A nurse is assessing a patient for signs of increased intracranial pressure (ICP) related to a brain tumor. Which of the following clinical manifestations are classic signs of increased ICP? Select all that apply.
Explanation
Increased intracranial pressure (ICP) occurs when tumor growth or edema raises pressure within the rigid skull, compromising cerebral perfusion. Classic signs include headache, bradycardia, widened pulse pressure, and projectile vomiting, which are part of the Cushing triad and related neurological responses. Early recognition of these symptoms is essential to prevent brain herniation and preserve neurological function.
Rationale for correct answers:
A. Bradycardia: Part of Cushing’s triad; results from brainstem compression affecting autonomic regulation. Slow heart rate is an early warning of rising ICP.
B. Projectile vomiting: Caused by direct pressure on the vomiting center in the medulla. It often occurs without nausea and is a classic ICP sign.
C. Hypertension with widened pulse pressure: Another component of Cushing’s triad. It reflects the body’s attempt to maintain cerebral perfusion despite rising ICP.
D. Headache, especially worse in the morning: Results from nocturnal hypoventilation and increased CO₂, which raises ICP when the patient is supine. Morning headaches are a common early symptom of brain tumors.
Rationale for incorrect answer:
E. Tachycardia: This is not a classic sign of ICP and usually occurs in response to hypovolemia, fever, or pain. Increased ICP typically causes bradycardia instead.
Take home points
- Classic ICP signs include headache, projectile vomiting, bradycardia, and widened pulse pressure.
- Cushing’s triad (bradycardia, hypertension with widened pulse pressure, irregular respirations) indicates impending brain herniation.
- Early recognition and intervention are critical to prevent permanent neurological damage.
Which of the following describes a meningioma?
Explanation
Meningiomas are typically benign tumors that arise from the meninges, the protective layers surrounding the brain and spinal cord. Although they are usually slow-growing and noncancerous, they can still cause neurological symptoms due to compression of adjacent brain tissue. Early recognition is important because even benign tumors can increase intracranial pressure and affect neurological function if left untreated.
Rationale for correct answer:
B. A benign tumor arising from the meninges that surround the brain: This is the defining feature of meningiomas. Their symptoms result from pressure effects rather than infiltration of brain tissue.
Rationale for incorrect answers:
A. A highly malignant tumor that originates from astrocytes: This describes glioblastoma multiforme, not meningioma.
C. A tumor of the pituitary gland that always causes hormone-related symptoms: Pituitary adenomas may or may not produce hormones and are not meningiomas.
D. A tumor of the cranial nerve VIII, responsible for hearing: This describes a vestibular schwannoma (acoustic neuroma), not a meningioma.
Take home points
- Meningiomas are usually benign and arise from the meninges.
- They can compress brain tissue and raise ICP even without malignancy.
- Differentiating tumor types is crucial for prognosis and treatment planning.
Practice Exercise 2
A client has a hearing loss from a suspected acoustic neuroma. Which diagnostic test should a nurse plan to prepare the client to confirm the presence of a tumor?
Explanation
Acoustic neuroma (vestibular schwannoma) is a benign tumor of cranial nerve VIII that often presents with progressive hearing loss, tinnitus, and balance disturbances. Magnetic resonance imaging (MRI) with contrast is the diagnostic test of choice because it provides high-resolution images of the cerebellopontine angle and internal auditory canal where these tumors arise. Early and accurate detection is essential to prevent permanent hearing loss and brainstem compression.
Rationale for correct answer:
C. Magnetic resonance imaging (MRI): MRI with contrast can detect even small acoustic neuromas. It allows for precise visualization of the tumor’s location and size for surgical planning.
Rationale for incorrect answers:
A. Tympanometry: Evaluates middle ear function and eardrum compliance. It does not detect tumors of cranial nerve VIII.
B. Arteriogram of the cranial vessels: Visualizes blood vessels but is not useful for identifying a solid tumor in the auditory canal.
D. Auditory canal biopsy: Rarely indicated and highly risky because acoustic neuromas are located internally along the nerve, not in the accessible canal.
Take home points
- MRI with contrast is the gold standard for diagnosing acoustic neuroma.
- Middle ear tests or vascular studies are not effective for tumor detection.
- Early diagnosis helps prevent complications like hearing loss and brainstem compression.
A patient with a brain tumor of the temporal lobe is most likely to experience which of the following focal symptoms?
Explanation
Temporal lobe brain tumors commonly affect hearing, smell, memory, and speech comprehension because this lobe houses the auditory cortex and olfactory pathways. Patients may experience auditory or olfactory hallucinations as early focal symptoms, reflecting abnormal cortical stimulation rather than generalized neurological impairment. Recognizing these lobe-specific symptoms helps in localizing brain tumors and guiding diagnostic imaging.
Rationale for correct answer:
C. Auditory or olfactory hallucinations: Temporal lobe tumors irritate sensory pathways for hearing and smell. This leads to hallucinations or unusual sensory experiences as focal neurological signs.
Rationale for incorrect answers:
A. Paralysis on one side of the body: This is more characteristic of frontal lobe or motor cortex involvement, not the temporal lobe.
B. Difficulty with spatial orientation: This is typically associated with parietal lobe dysfunction, which processes spatial awareness.
D. Balance and coordination problems: These symptoms suggest cerebellar involvement, not temporal lobe pathology.
Take home points
- Temporal lobe tumors often present with auditory or olfactory hallucinations.
- Focal neurological signs help localize brain tumor origin.
- Symptom patterns differ by lobe, guiding diagnostic and treatment strategies.
A nurse is caring for a patient with a cerebellar tumor. The nurse should be vigilant for which of the following clinical manifestations? Select all that apply.
Explanation
Cerebellar tumors primarily affect balance, coordination, and motor control because the cerebellum is responsible for equilibrium and fine motor movement. Patients may present with ataxia, dizziness, nystagmus, and dysarthric speech, which reflect impaired coordination and vestibular function. Unlike frontal lobe tumors, cerebellar tumors rarely cause personality changes, but they can significantly impact mobility and speech.
Rationale for correct answers:
A. Ataxia: The cerebellum controls voluntary coordination, so a tumor often causes unsteady gait and poor balance.
C. Dizziness: Cerebellar and vestibular pathway involvement can produce vertigo and disequilibrium.
D. Nystagmus: Abnormal, rapid eye movements occur due to impaired coordination between the cerebellum and ocular motor nerves.
E. Speech difficulties: Dysarthria or slurred speech occurs when the cerebellum’s coordination of tongue and facial muscles is disrupted.
Rationale for incorrect answer:
B. Personality changes: These are typically associated with frontal lobe involvement, not cerebellar pathology.
Take home points
- Cerebellar tumors cause ataxia, dizziness, nystagmus, and dysarthric speech due to motor coordination deficits.
- Behavioral or personality changes are not typical of cerebellar lesions.
- Early recognition of these focal signs can guide prompt imaging and treatment.
Which diagnostic tool is considered the "gold standard" for imaging a brain tumor, providing detailed images of brain structures and tumor location?
Explanation
Magnetic Resonance Imaging (MRI) is considered the gold standard for brain tumor imaging because it provides high-resolution, detailed images of brain structures and tumor location. MRI allows for precise tumor visualization, assessment of surrounding edema, and planning for surgery or radiation therapy. Compared to other imaging techniques, MRI is more sensitive for detecting small or deep-seated lesions and avoids radiation exposure.
Rationale for correct answer:
C. Magnetic Resonance Imaging (MRI): MRI provides superior soft tissue contrast and detailed anatomical views. It is ideal for localizing tumors and evaluating surrounding brain involvement.
Rationale for incorrect answers:
A. Computed Tomography (CT) scan: CT is useful for initial screening or detecting calcifications and bleeding but is less detailed than MRI for tumor evaluation.
B. Cerebral Angiography: This is primarily used to visualize cerebral blood vessels or assess tumor vascularity, not for first-line tumor detection.
D. Positron Emission Tomography (PET) scan: PET evaluates metabolic activity and recurrence but is less precise for initial tumor localization than MRI.
Take home points
- MRI is the gold standard for detailed brain tumor imaging.
- CT is faster for emergencies but less sensitive for small or deep tumors.
- Angiography and PET are adjuncts for vascular mapping or metabolic assessment, not primary diagnosis.
Which of the following statements about the diagnostic process for brain tumors are correct? Select all that apply.
Explanation
The diagnostic process for brain tumors involves multiple imaging and procedural steps to evaluate tumor presence, location, vascularity, and type. A CT scan is often used in emergencies to quickly assess for hemorrhage or mass effect, while cerebral angiography helps in mapping the tumor’s blood supply, especially before surgery. A stereotactic biopsy provides a definitive tissue diagnosis, which is essential for determining tumor grade and planning treatment.
Rationale for correct answers:
A. A CT scan is useful in an emergency to rule out hemorrhage: CT is fast and readily available, making it ideal for detecting bleeding or large masses in acute settings.
B. A cerebral angiography is used to visualize the tumor's blood supply: Angiography helps determine if a tumor is highly vascular, which is critical for surgical planning and embolization.
D. A stereotactic biopsy is necessary for a definitive tissue diagnosis: Imaging shows the presence of a mass, but biopsy confirms the tumor type and grade under microscopic examination.
Rationale for incorrect answers:
C. A PET scan is the definitive diagnostic method for all brain tumors: PET scans assess metabolic activity but are not definitive; they are usually used in combination with MRI or CT.
E. A spinal tap is the first-line diagnostic test for primary brain tumors: Lumbar puncture is not first-line due to the risk of herniation in the presence of increased ICP; it's only used in select cases like suspected leptomeningeal spread.
Take home points
- CT, MRI, and angiography assist in imaging and surgical planning.
- Biopsy is required for definitive tumor diagnosis.
- PET and lumbar puncture are specialized tools, not used routinely or first-line.
Practice Exercise 3
An anxious client is seen in a clinic because the client suspects that he or she has a brain tumor. The client questions a nurse about treatment options if tests show the presence of a tumor. The nurse answers the client based on the knowledge that treatment of a brain tumor depends on (Select all that apply)
Explanation
Treatment of brain tumors is highly individualized and depends on a combination of tumor characteristics and patient factors. Key determinants include the tumor’s growth rate, location, malignancy status, and histologic type. The likelihood of recurrence is also considered because it influences long-term planning and the aggressiveness of therapy. A multidisciplinary approach ensures that treatment is tailored for optimal outcomes.
Rationale for correct answers:
A. Rate of growth of the tumor: Rapidly growing tumors require urgent or aggressive therapy, while slow-growing tumors may allow for conservative management or observation.
B. Whether the tumor is malignant or benign: Malignant tumors typically require multimodal therapy (surgery, radiation, chemotherapy), while benign tumors may be managed with surgery or monitoring.
C. Cell type from which the tumor originates: Histology guides treatment because tumor type determines responsiveness to chemotherapy and radiation.
D. Location within the brain: Tumor site impacts surgical accessibility, neurological risk, and treatment planning.
E. Whether the tumor will reoccur: Anticipated recurrence affects decisions on adjuvant therapy and the intensity of follow-up care.
Rationale for incorrect answer:
F. The client’s age and type of insurance: While these may affect access to care, they are not medical determinants of the treatment plan.
Take home points
- Brain tumor treatment is guided by tumor growth rate, type, location, and recurrence risk.
- Benign tumors can still require treatment if they threaten neurological function.
- Long-term planning considers recurrence risk to reduce complications and improve survival.
A 6-year-old child is being seen in a clinic after discharge from a hospital for removal of a brain tumor. Which finding, reported by a parent, best suggests the child has likely developed a complication?
Explanation
After brain tumor surgery, certain complications may arise related to brain function or fluid balance. One concerning sign is polyuria with dilute urine, which suggests diabetes insipidus (DI)—a potential complication caused by damage to the hypothalamus or pituitary gland during surgery. Early recognition and treatment of DI are critical to prevent severe dehydration and electrolyte imbalance in pediatric patients.
Rationale for correct answer:
B. Voiding large amounts of dilute urine: This indicates possible diabetes insipidus, a common postoperative complication affecting water regulation. It requires prompt medical intervention to manage fluid and electrolyte balance.
Rationale for incorrect answers:
A. Reports occasional headaches: Some headache is common after brain surgery and does not necessarily indicate a complication.
C. Able to walk with use of crutches: Using crutches postoperatively may reflect temporary weakness or recovery status, not a complication.
D. Ventricular–peritoneal: This option is incomplete but likely refers to a shunt placement, which is a treatment, not a reported symptom or complication.
Take home points
- Diabetes insipidus is a serious complication after brain tumor surgery, especially in children.
- Excessive dilute urine warrants urgent evaluation and treatment.
- Headache and mobility changes are expected postoperative findings but require monitoring.
A 72-year-old client with a deep vein thrombosis in the left leg and a history of a brain tumor is hospitalized for 3 days. The client’s care plan indicates a nursing diagnosis of Imbalanced nutrition: less than body requirements related to poor appetite and decreased oral intake. Which assessment finding would best indicate a need to revise the care plan related to the nursing diagnosis?
Explanation
Dry oral mucous membranes are a direct physical sign of dehydration, which often accompanies or worsens malnutrition and poor oral intake. This finding indicates that the client’s nutritional and hydration status may be declining and that the current care plan might not be adequately addressing these needs. Recognizing such clinical signs is critical for timely revision of the care plan to prevent further complications.
Rationale for correct answer:
A. Oral mucous membranes are dry due to dehydration: This physical sign reflects inadequate fluid intake and possible nutritional deficits, signaling the need to reassess and modify the care plan.
Rationale for incorrect answers:
B. Daily intake and output reveals that daily caloric intake is inadequate: While important, intake/output records may lag behind clinical signs and do not always reflect hydration status immediately.
C. Client is not receptive to education regarding nutrition: This affects teaching strategies but does not directly indicate a worsening nutritional problem.
D. Client states that he or she is not hungry: Subjective reports are helpful but less reliable than objective clinical signs for assessing the need to revise care plans.
Take home points
- Physical signs like dry mucous membranes provide immediate evidence of nutritional or hydration compromise.
- Regular clinical assessment should complement intake/output monitoring for a comprehensive evaluation.
- Prompt revision of the care plan can prevent worsening malnutrition and dehydration.
A nurse is providing post-operative care for a patient who has undergone a craniotomy for a brain tumor. Which of the following are essential nursing interventions in the immediate post-operative period? Select all that apply.
Explanation
Post-operative care after a craniotomy requires close monitoring and specific interventions to prevent complications and promote recovery. Proper head elevation helps reduce intracranial pressure, while vigilant fluid balance monitoring is essential for early detection of diabetes insipidus, a common complication. Frequent neurological assessments enable early recognition of changes that may indicate bleeding or swelling. Some interventions, like coughing, must be carefully managed to avoid increasing intracranial pressure.
Rationale for correct answers:
A. Position the patient with the head of the bed elevated to 30−45°: Elevating the head facilitates venous drainage from the brain and reduces ICP.
B. Monitor for fluid balance and signs of diabetes insipidus: Surgery near the pituitary can cause DI, leading to severe fluid imbalances that need early detection and treatment.
D. Perform frequent neurological checks to detect changes in status: Continuous monitoring helps detect deterioration early, guiding timely interventions.
Rationale for incorrect answers:
C. Encourage the patient to cough and deep breathe frequently to prevent pneumonia: While important, coughing can increase ICP and may be contraindicated or done cautiously after brain surgery.
E. Administer pain medication only after a physician's approval: Nurses can usually administer prescribed pain medications per protocol; delaying pain control can increase patient stress and ICP.
Take home points
- Head elevation, fluid monitoring, and neuro checks are critical post-craniotomy.
- Coughing should be carefully timed to avoid spikes in ICP.
- Pain management should be timely to reduce stress and complications.
Nurse admitting post-craniotomy client from PACU. Client's incision is supratentorial, nurse will assist client into which position?
Explanation
After a supratentorial craniotomy, the head of the bed should be elevated to 30 degrees to promote venous drainage from the brain and help reduce intracranial pressure (ICP). Proper positioning also helps prevent complications like cerebral edema and facilitates respiratory function. Elevating the head is a standard nursing intervention to optimize cerebral perfusion and support recovery.
Rationale for correct answer:
C. Elevate HOB to 30 degrees: This position decreases ICP by promoting venous outflow without compromising cerebral perfusion pressure.
Rationale for incorrect answers:
A. Head of bed flat: Flat positioning can increase ICP and is generally avoided post-craniotomy.
B. Supine: Lying completely flat can increase ICP and is not recommended.
D. Lying on operative side: This may impair venous drainage and increase pressure on the surgical site, increasing risk of complications.
Take home points
- Elevating the head to 30 degrees is essential to reduce ICP after supratentorial surgery.
- Avoid positions that can increase ICP or impair venous drainage.
- Proper positioning supports brain healing and reduces postoperative complications.
Comprehensive Questions
A nurse is caring for a client who is having surgery for the removal of an encapsulated acoustic tumor. Which of the following potential complications should the nurse monitor for postoperatively? (Select all that apply.)
Explanation
Surgical removal of an encapsulated acoustic tumor (vestibular schwannoma) carries a high risk for neurological complications due to its location near the brainstem and cranial nerves. Key postoperative risks include increased intracranial pressure (ICP), hydrocephalus, and seizures, which require close monitoring for early intervention.
Rationale for correct answers:
A. Increased intracranial pressure (ICP): Swelling or CSF accumulation after brain surgery can elevate ICP, leading to headache, vomiting, or altered consciousness. Prompt recognition is vital to prevent brain herniation.
C. Hydrocephalus: Obstruction of CSF pathways during surgery can cause hydrocephalus with headache, nausea, and mental status changes. Ventricular drainage may be required to relieve pressure.
E. Seizures: Brain tissue irritation or postoperative edema can trigger seizures. Clients are often placed on prophylactic anticonvulsants to minimize this risk.
Rationale for incorrect answers:
B. Hemorrhagic shock: This surgery rarely causes systemic blood loss severe enough to induce shock because it is localized to the brain. Shock would be an unusual and late complication.
D. Hypoglycemia: This is not a typical postoperative risk unless the client has comorbid diabetes or inadequate perioperative glucose management.
Take home points
- Major postoperative risks are neurologic: ICP increase, hydrocephalus, and seizures.
- Hemorrhagic shock and hypoglycemia are uncommon in acoustic tumor removal.
- Early recognition of neurologic changes is essential for preventing complications.
A nurse is caring for a client who has just undergone a craniotomy for a supratentorial tumor. Which of the following postoperative prescriptions should the nurse clarify with the provider?
Explanation
After a craniotomy for a supratentorial tumor, careful postoperative management is essential to reduce intracranial pressure (ICP) and prevent neurological complications. Opioid analgesics are used cautiously because they can mask neurological changes and depress respirations, which may worsen ICP.
Rationale for correct answer:
B. Morphine sulfate 2 mg IV PRN: Opioids can cause sedation, respiratory depression, and mask neurological decline after craniotomy. Non-opioid analgesics or carefully titrated alternatives are preferred to allow accurate neuro assessment.
Rationale for incorrect answers:
A. Dexamethasone: This corticosteroid reduces cerebral edema and helps control ICP, making it appropriate post-craniotomy. It is commonly prescribed to prevent or manage swelling.
C. Ondansetron: Controlling nausea and vomiting is essential to prevent spikes in ICP, and ondansetron is a safe antiemetic choice. Its use supports comfort without altering neurological assessments.
D. Phenytoin: Seizure prophylaxis is routine after brain surgery because cerebral irritation may trigger seizures. This medication is appropriate and protective postoperatively.
Take home points
- Opioids are generally avoided after craniotomy because they can mask neurological changes and increase ICP risk.
- Steroids, antiemetics, and anticonvulsants are key medications to reduce edema, prevent vomiting, and lower seizure risk.
- Accurate neurological assessment is the priority in the immediate postoperative period.
A nurse is completing an assessment of a client who has increased intracranial pressure. Which of the following are expected findings? (Select all that apply.)
Explanation
Increased intracranial pressure (ICP) occurs when the volume of brain tissue, blood, or cerebrospinal fluid rises within the rigid skull. This condition leads to impaired cerebral perfusion, which can quickly progress to brain herniation if unaddressed. Early recognition of signs and symptoms is critical for preventing permanent neurological damage. Common early findings include changes in mental status, behavioral changes, headache, and pupil abnormalities, which reflect pressure on brain tissue and cranial nerves.
Rationale for correct answers:
A. Disoriented to time and place: Confusion and disorientation are early indicators of cerebral hypoperfusion. They reflect rising ICP affecting the cerebral cortex.
B. Restlessness and irritability: These are early behavioral changes caused by decreased cerebral oxygenation and pressure on brain tissue. They often precede more severe neurological deterioration.
C. Unequal pupils: Indicates pressure on cranial nerve III or brain herniation risk. Pupil asymmetry is a critical neurologic warning sign.
E. Headache: A common manifestation of stretching meninges and pressure changes. It often worsens with coughing, straining, or position changes.
Rationale for incorrect answer:
D. ICP 15 mmHg: Normal ICP ranges from 10–15 mmHg, so 15 is at the upper limit but not elevated. Clinically significant ICP is typically >20 mmHg.
Take home points
- Early signs of ICP increase include confusion, restlessness, headache, and pupil changes.
- Unequal pupils are an emergency indicator of possible herniation.
- ICP is considered elevated above 20 mmHg, requiring prompt intervention.
A nurse is reviewing a prescription for dexamethasone (Decadron) with a client who has an expanding brain tumor. Which of the following are appropriate statements by the nurse? (Select all that apply.)
Explanation
Dexamethasone (Decadron) is a corticosteroid commonly prescribed to clients with expanding brain tumors to reduce cerebral edema. By decreasing swelling and inflammation, it helps relieve intracranial pressure and associated neurological symptoms such as headache or vomiting. Corticosteroids, however, are associated with metabolic and fluid retention side effects that require client education. Monitoring and teaching about weight gain, fluid retention, and hyperglycemia are essential to safe therapy.
Rationale for correct answers:
A. “It is given to reduce swelling of the brain.” Dexamethasone decreases cerebral edema and relieves symptoms of increased ICP. This is the primary therapeutic purpose in brain tumor management.
C. “You may notice weight gain.” Corticosteroids can increase appetite and cause fat redistribution, resulting in weight gain. This is a common, expected side effect of therapy.
E. “It can cause you to retain fluids.” Steroids promote sodium and water retention, which can lead to peripheral edema. Clients should be taught to monitor for swelling or sudden weight changes.
Rationale for incorrect answers:
B. “You will need to monitor for low blood sugar.” Dexamethasone can raise, not lower, blood glucose levels. Hyperglycemia is a more likely concern, especially in clients with diabetes.
D. “Tumor growth will be delayed.” Dexamethasone does not affect tumor growth; it only reduces surrounding edema. Definitive tumor treatment requires surgery, radiation, or chemotherapy.
Take home points
- Dexamethasone reduces cerebral edema but does not shrink the tumor itself.
- Weight gain, fluid retention, and hyperglycemia are key side effects requiring education.
- Client teaching helps ensure early recognition of complications during corticosteroid therapy.
A nurse is caring for a client who has a benign brain tumor. The client asks the nurse if he can expect this same type of tumor to occur in other areas of his body. Which of the following is an appropriate response by the nurse?
Explanation
A benign brain tumor is a noncancerous growth that develops only within the brain tissue and does not metastasize to other parts of the body. Unlike malignant tumors, benign tumors grow slowly and remain localized, though they can still cause significant neurological symptoms by compressing brain structures. Educating the client about the localized nature of benign brain tumors helps reduce anxiety and clarify the difference from metastatic disease. Treatment focuses on surgical removal or monitoring rather than systemic therapy.
Rationale for correct answer:
C. “It is limited to brain tissue.” Benign brain tumors do not spread outside the central nervous system. They are localized growths that remain within the brain.
Rationale for incorrect answers:
A. “It can spread to breasts and kidneys.” Benign brain tumors do not metastasize to other organs. This pattern is only seen with malignant or metastatic cancers.
B. “It can develop in your gastrointestinal tract.” Benign brain tumors do not spontaneously appear in other organ systems. Tumors in the GI tract would have a separate origin.
D. “It probably started in another area of your body and spread to your brain.” This describes metastatic brain cancer, not a benign primary brain tumor. Benign tumors originate in the brain itself.
Take home points
- Benign brain tumors remain localized and do not metastasize to other organs.
- They can still cause serious neurological effects by compressing surrounding tissue.
- Patient education reduces anxiety and helps distinguish benign from metastatic disease.
A nurse is reviewing the health record of a client who has a malignant brain tumor and notes the client has a positive Romberg sign. Which of the following actions should the nurse take to assess for this sign?
Explanation
A positive Romberg sign indicates impaired balance or proprioception, which can occur with malignant brain tumors affecting the cerebellum or sensory pathways. To assess for this sign, the nurse evaluates the client’s ability to maintain posture and equilibrium with visual input removed. A positive result suggests that visual cues are compensating for poor proprioception, leading to swaying or loss of balance when the eyes are closed. This test helps identify neurological impairment that increases the client’s fall risk.
Rationale for correct answer:
D. Have the client stand erect with eyes closed. This position removes visual input, revealing balance or proprioception deficits. Swaying or falling indicates a positive Romberg sign.
Rationale for incorrect answers:
A. Stroke the lateral aspect of the sole of the foot. This elicits the Babinski reflex, which assesses upper motor neuron function, not balance.
B. Ask the client to blink his eyes. This assesses cranial nerve function (CN V and VII) but is unrelated to the Romberg test.
C. Observe for facial drooping. This evaluates facial nerve function and stroke symptoms, not proprioception or balance.
Take home points
- A positive Romberg sign indicates impaired balance due to cerebellar or sensory pathway dysfunction.
- Testing involves standing with eyes closed to assess reliance on visual cues for balance.
- Fall precautions are essential for clients with positive Romberg results.
A patient is suspected of having a brain tumor. The signs and symptoms include memory deficits, visual disturbances, weakness of right upper and lower extremities, and personality changes. The nurse recognizes that the tumor is most likely located in the
Explanation
Brain tumor location determines the type of neurological symptoms a client experiences. The frontal lobe is responsible for personality, judgment, voluntary motor control, and memory, so tumors here often cause behavioral changes, weakness, and cognitive deficits. Symptoms such as right-sided weakness indicate involvement of the motor cortex, while personality and memory changes reflect disruption of frontal lobe function. Recognizing these patterns assists in localizing brain tumors and guiding further evaluation.
Rationale for correct answer:
A. Frontal lobe: Controls personality, voluntary motor activity, and higher cognitive functions. Tumors here cause weakness, personality changes, and memory deficits consistent with the client’s presentation.
Rationale for incorrect answers:
B. Parietal lobe: Primarily involved in sensory interpretation and spatial awareness. Tumors here typically cause sensory loss or neglect rather than personality changes.
C. Occipital lobe: Responsible for vision and visual processing. While visual disturbances may occur, isolated occipital tumors would not cause personality changes or hemiparesis.
D. Temporal lobe: Involved in auditory processing and language interpretation. Tumors here are more likely to cause aphasia, auditory hallucinations, or memory issues without hemiparesis.
Take home points
- Frontal lobe tumors often cause personality changes, cognitive deficits, and contralateral weakness.
- Tumor location correlates closely with neurological presentation, guiding diagnostic evaluation.
- Symptom mapping helps clinicians localize and prioritize brain imaging studies.
A nurse plans care for the patient with increased intracranial pressure with the knowledge that the best way to position the patient is to
Explanation
Positioning is a critical intervention for clients with increased intracranial pressure (ICP) to promote venous drainage from the brain without compromising cerebral perfusion. Elevating the head of the bed (HOB) to 30 degrees optimizes venous outflow, reduces ICP, and helps prevent further cerebral edema. Extreme flexion or rotation of the head should be avoided, as these positions can impede venous return and worsen pressure. Proper positioning is a first-line nursing intervention in ICP management.
Rationale for correct answer:
B. Elevate the head of the bed to 30 degrees: This position facilitates cerebral venous drainage while maintaining adequate cerebral perfusion. It is the recommended standard for clients with increased ICP.
Rationale for incorrect answers:
A. Keep the head of the bed flat: Flat positioning can increase ICP by reducing venous outflow from the brain. This position is generally avoided unless specifically ordered for procedures like lumbar puncture.
C. Maintain patient on the left side with the head supported on a pillow: Lateral positioning may cause neck flexion and impaired venous return. Side-lying does not optimize ICP reduction.
D. Use a continuous-rotation bed: Frequent or continuous rotation can cause spikes in ICP. This therapy is reserved for preventing pulmonary complications, not for ICP management.
Take home points
- HOB elevated 30 degrees is the safest and most effective position for ICP reduction.
- Avoid neck flexion, extreme rotation, or flat positioning, as these can worsen ICP.
- Positioning is a noninvasive, first-line nursing intervention to protect the brain.
Nursing management of a patient with a brain tumor includes. Select all that apply
Explanation
Nursing management of clients with brain tumors focuses on safety, family support, and complication prevention. Brain tumors can cause neurological deficits, behavioral changes, and seizures, which affect both the patient and family. Nurses are responsible for educating caregivers, reinforcing safety measures, and implementing seizure precautions. These interventions help prevent injury and improve coping during the course of the disease.
Rationale for correct answers:
C. Assisting and supporting the family in understanding any changes in behavior: Family education helps relatives adapt to personality and cognitive changes caused by tumor progression. This support facilitates safe and effective home care.
E. Planning for seizure precautions and teaching the patient and the caregiver about antiseizure drugs: Brain tumors increase seizure risk. Teaching about seizure precautions and medication use promotes safety and adherence to treatment.
Rationale for incorrect answers:
A. Discussing with the patient methods to control inappropriate behavior: This is less effective because neurological impairment often limits the patient’s ability to control behavior. Family support is more appropriate than expecting behavioral self-regulation.
B. Using diversion techniques to keep the patient stimulated and motivated: Excessive stimulation can increase fatigue or irritability. A calm and restful environment is preferred for neurological stability.
D. Limiting self-care activities until the patient has regained maximum physical functioning: Encouraging safe participation in self-care promotes independence and prevents deconditioning. Limiting all activity is not recommended.
Take home points
- Family education and seizure precautions are the cornerstones of brain tumor nursing care.
- Overstimulation and unrealistic behavior expectations are not appropriate interventions.
- Safe home care depends on caregiver understanding and injury prevention strategies.
When the patient has a rapidly growing brain tumor, what slows expansion of cerebral brain tissue into the adjacent hemisphere?
Explanation
Brain tumors that grow rapidly can compress or displace surrounding structures. The falx cerebri is a rigid fold of dura mater that separates the two cerebral hemispheres and acts as a barrier to tumor expansion across the midline. This dural structure temporarily slows tumor spread into the opposite hemisphere, although pressure can eventually cause midline shift or herniation. Understanding the role of intracranial anatomy is important in predicting tumor progression and complications.
Rationale for correct answer:
B. Falx cerebri: A strong dural fold that separates the cerebral hemispheres. It limits early tumor expansion across the midline until pressure forces tissue displacement.
Rationale for incorrect answers:
A. Ventricles: These structures contain CSF and may become compressed but do not block tumor growth. Tumor expansion can eventually distort or obstruct them, leading to hydrocephalus.
C. Arachnoid layer: A thin meningeal membrane that encloses the subarachnoid space. It is not structurally strong enough to prevent tumor spread.
D. Tentorium cerebelli: This dural fold separates the cerebrum from the cerebellum. It limits downward expansion, not horizontal spread between hemispheres.
Take home points
- The falx cerebri provides a temporary barrier to tumor growth across hemispheres.
- Ventricles and meninges do not significantly resist tumor expansion.
- Anatomical barriers influence tumor progression and patterns of brain herniation.
The patient is suspected of having a new brain tumor. Which test will the nurse expect to be ordered to detect a small tumor?
Explanation
Early detection of brain tumors relies on imaging tests that can visualize small masses and structural changes. A CT scan is often the first diagnostic tool ordered because it provides detailed images of the brain, allowing detection of small tumors, edema, and mass effect. CT scans are quick, widely available, and highly sensitive for structural abnormalities, making them ideal for initial evaluation of new neurological symptoms.
Rationale for correct answer:
A. CT scan: Provides clear structural images that can identify small tumors and associated edema. It is fast and widely available, making it the first-line imaging study in suspected brain tumor cases.
Rationale for incorrect answers:
B. Angiography: Evaluates cerebral blood vessels and tumor vascularity but is not typically used for initial tumor detection. It is reserved for surgical planning or assessing vascular involvement.
C. Electroencephalography (EEG): Records electrical brain activity and is used for seizure evaluation, not structural tumor detection.
D. Positron emission tomography (PET) scan: Identifies areas of metabolic activity or recurrence but is not the primary tool for detecting small, new tumors.
Take home points
- CT scan is the first-line imaging study to detect new or small brain tumors.
- Angiography and PET scans are used for tumor characterization or surgical planning, not initial detection.
- EEG is useful for evaluating seizures but does not visualize structural lesions.
Assisting the family to understand what is happening to the patient is an especially important role of the nurse when the patient has a tumor in which part of the brain?
Explanation
Tumors in the frontal lobe often cause behavioral, cognitive, and personality changes because this area controls judgment, emotions, problem-solving, and voluntary movement. These changes can be distressing for families, as the patient may display inappropriate behavior, impaired decision-making, or apathy. Assisting the family to understand and cope with these changes helps reduce stress, improve support, and facilitate safer home care. Family education is a key nursing role in managing the psychosocial impact of frontal lobe tumors.
Rationale for correct answer:
B. Frontal lobe: Responsible for personality, behavior, and decision-making. Tumors here often cause dramatic changes that are difficult for families to understand without guidance.
Rationale for incorrect answers:
A. Ventricles: Tumors here mainly affect CSF flow and can lead to hydrocephalus. They are less likely to cause personality or behavior changes that families would struggle to interpret.
C. Parietal lobe: Primarily responsible for sensory processing and spatial awareness. Tumors may cause sensory loss or neglect but rarely dramatic personality changes.
D. Occipital lobe: Primarily involved in vision and visual interpretation. Tumors here typically result in visual field deficits without major behavioral effects.
Take home points
- Frontal lobe tumors frequently lead to behavioral and personality changes.
- Family education and support are crucial to help caregivers cope with emotional and cognitive changes.
- Other lobes mainly affect sensory or visual functions, with less psychosocial impact.
What is the best explanation of stereotactic radiosurgery?
Explanation
Stereotactic radiosurgery (SRS) is a highly precise, noninvasive radiation therapy used to treat brain tumors and vascular malformations. It works by focusing multiple beams of radiation on a single target to destroy abnormal cells without opening the skull. This therapy is particularly useful for small or inoperable tumors, as it minimizes damage to healthy brain tissue. SRS offers shorter recovery times and fewer complications compared to traditional brain surgery.
Rationale for correct answer:
B. Very precisely focused radiation destroys tumor cells: SRS delivers converging radiation beams that effectively target and kill tumor cells. It avoids the need for open craniotomy while preserving surrounding brain tissue.
Rationale for incorrect answers:
A. Radioactive seeds are implanted in the brain: This describes brachytherapy, which involves direct radioactive implantation rather than external focused radiation.
C. Tubes are placed to redirect CSF from one area to another: This is a shunt procedure for hydrocephalus and does not treat brain tumors.
D. The cranium is opened with removal of a bone flap to open the dura: This is a craniotomy, an invasive surgical procedure unlike the noninvasive SRS.
Take home points
- SRS is a noninvasive radiation therapy that destroys tumor cells without open surgery.
- Brachytherapy, shunts, and craniotomy are invasive procedures used for different purposes.
- Precision targeting in SRS reduces damage to healthy brain tissue and shortens recovery.
Successful achievement of patient outcomes for the patient with cranial surgery would best be indicated by what?
Explanation
Post-cranial surgery care focuses on preventing life-threatening complications, with increased intracranial pressure (ICP) being the most critical concern. A successful recovery is primarily indicated by neurological stability and the absence of ICP-related symptoms, which reflects effective postoperative management. While functional independence and emotional adaptation are important, ensuring brain safety is the top priority for patient outcomes.
Rationale for correct answer:
D. Absence of signs and symptoms of increased ICP: Stable ICP indicates that the brain is not under harmful pressure following surgery. This demonstrates that interventions to manage cerebral edema and promote venous drainage are effective. Achieving this outcome reflects the primary goal of postoperative neurological care.
Rationale for incorrect answers:
A. Ability to return home in 6 days: Discharge timing varies with each patient and is influenced by multiple factors beyond neurological status. Some patients with complications may stay longer, while others may be discharged earlier. Therefore, it is not a reliable indicator of successful surgical outcomes.
B. Ability to meet all self-care needs: Patients may still require assistance with activities of daily living due to weakness or fatigue, even if surgery is successful. Functional independence is a secondary goal and may take weeks to months to achieve. It does not necessarily reflect the immediate success of cranial surgery.
C. Acceptance of residual neurologic deficits: Emotional adaptation is part of long-term rehabilitation but does not indicate the immediate physiological success of surgery. A patient can accept deficits while still experiencing complications like increased ICP. Therefore, acceptance alone is not a measure of successful postoperative outcomes.
Take home points
- Neurological stability and normal ICP are the primary indicators of successful cranial surgery.
- Functional and emotional milestones are important but occur after physiological safety is ensured.
- Early recognition and prevention of ICP elevation are essential to protect brain function.
The nurse is aware that the client with a brain tumor can be medically managed with which treatments? Select all that apply
Explanation
Medical management of brain tumors often involves a multimodal approach aimed at reducing tumor size, controlling symptoms, and preventing complications. Surgery is commonly performed for tumor removal or debulking, while radiation therapy targets residual or inoperable tumor tissue. Chemotherapy may be used, although its effectiveness is limited by the blood-brain barrier. Treatments like bone marrow transplant or blood transfusion are not part of routine brain tumor management.
Rationale for correct answers:
A. Chemotherapy: Certain agents can cross the blood-brain barrier to shrink or slow tumor growth. It is typically used for malignant or recurrent tumors in combination with other therapies.
B. Radiation: This therapy targets tumor tissue that cannot be completely removed surgically. It helps prevent regrowth and manage inoperable tumors.
C. Surgery: Surgical removal or debulking is often the first step in management. It reduces mass effect and relieves symptoms of increased intracranial pressure.
Rationale for incorrect answers:
D. Bone marrow transplant: This is used for hematologic cancers like leukemia or lymphoma. It does not treat primary brain tumors.
E. Blood transfusion: Transfusions correct anemia but have no effect on tumor treatment. They are only supportive if the patient is critically anemic or undergoing major surgery.
Take home points
- Surgery, radiation, and chemotherapy are the mainstays of brain tumor management.
- Supportive therapies like transfusions do not treat the tumor itself.
- Multimodal treatment is used to reduce tumor burden, relieve symptoms, and prevent recurrence.
Exams on Brain Tumors
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Describe the pathophysiology and differentiate between primary and secondary brain tumors.
- Identify the common and focal clinical manifestations of a brain tumor.
- Explain the key diagnostic procedures used to confirm a brain tumor diagnosis.
- Summarize the various interprofessional treatment options, including surgical, radiation, and chemotherapy.
- Outline the critical components of nursing management, from pre-operative and post-operative care to managing complications.
Introduction
A brain tumor is an abnormal growth of cells within the brain or spinal cord. These growths can be primary, originating in the brain itself, or secondary (metastatic), originating in another part of the body and spreading to the brain. Tumors are also classified as benign or malignant. Benign tumors grow slowly, have defined borders, and rarely spread, but can still cause significant damage due to their location and mass effect. Malignant tumors are fast-growing, invasive, and can spread to other areas of the central nervous system. The damage caused by a brain tumor is a result of compression and infiltration of brain tissue, leading to increased intracranial pressure (ICP), cerebral edema, and focal neurological deficits.
Classification And Types
Primary Brain Tumors
Primary tumors are categorized by the type of cell from which they arise.
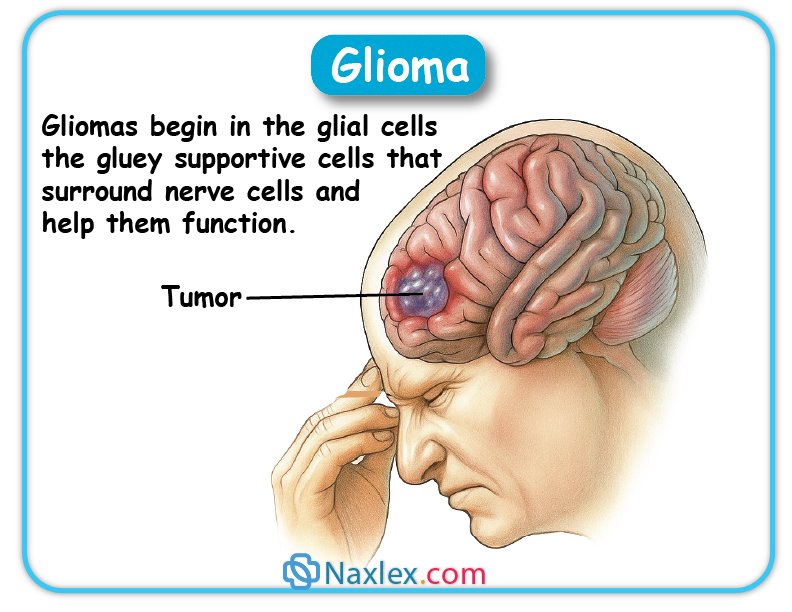
Gliomas
These are the most common type of primary brain tumor and originate from glial cells (supportive cells of the brain). They include:
- Astrocytoma: Arises from astrocytes and can be low-grade or high-grade (e.g., glioblastoma multiforme, a highly aggressive type).
- Oligodendroglioma: Arises from oligodendrocytes.
- Ependymoma: Arises from ependymal cells, which line the ventricles.
 Meningiomas
Meningiomas
These are typically benign tumors that arise from the meninges, the membranes that surround the brain and spinal cord. They are usually slow-growing and can be surgically removed if accessible.
Acoustic Neuromas
These are benign tumors of the cranial nerve VIII, which is responsible for hearing and balance. They can cause hearing loss, vertigo, and tinnitus.
Pituitary Adenomas
These are benign tumors of the pituitary gland. They can cause symptoms by compressing the optic chiasm (leading to visual disturbances) or by secreting hormones (leading to endocrine disorders like Cushing's syndrome or acromegaly).
Metastatic (Secondary) Brain Tumors
These are the most common type of brain tumor overall. The primary cancers that most frequently metastasize to the brain include lung cancer, breast cancer, melanoma, colon cancer, and kidney cancer.
Clinical Manifestations
The signs and symptoms of a brain tumor depend on the size, location, and rate of growth.
- Headache: The most common symptom, often worse in the morning and aggravated by coughing, straining, or a change in position.
- Nausea and Vomiting: Often projectile and not associated with food intake, a classic sign of increased ICP.
- Seizures: Can be a focal or generalized seizure and is often the initial symptom, especially with tumors of the frontal and temporal lobes.
- Papilledema: Swelling of the optic disc, caused by increased ICP. This can be seen on an ophthalmic examination.
- Cognitive Dysfunction: Memory loss, personality changes, or confusion.
Focal Symptoms (Based on Location)
- Frontal Lobe: Personality changes, inappropriate behavior, memory impairment, speech difficulties (Broca's aphasia), or paralysis on one side of the body.
- Parietal Lobe: Sensory deficits, difficulty with spatial orientation, or a neglect of one side of the body.
- Temporal Lobe: Auditory or olfactory hallucinations, seizures, or speech comprehension difficulties (Wernicke's aphasia).
- Occipital Lobe: Visual disturbances, such as blurred vision or loss of half of the visual field.
- Cerebellum: Balance and coordination problems (ataxia), dizziness, or nystagmus.
- Brainstem: Cranial nerve dysfunction, difficulty swallowing, or vital sign instability.
Diagnostic Studies
Imaging
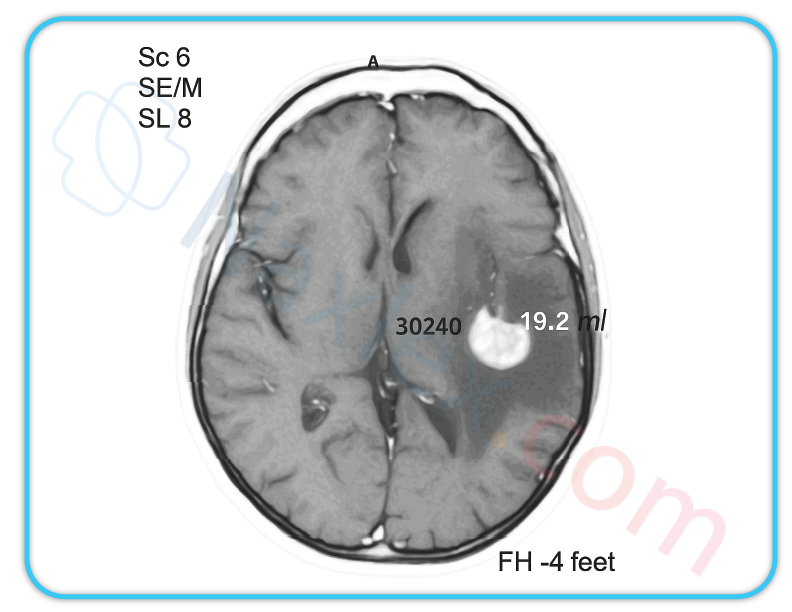
- Magnetic Resonance Imaging (MRI): The gold standard for brain tumors, providing detailed images of brain structures and tumor location.
- Computed Tomography (CT) Scan: Used to identify the tumor's location and size, especially useful in emergencies to rule out hemorrhage.
 Positron Emission Tomography (PET) Scan: Can help differentiate between a recurrent tumor and radiation necrosis.
Positron Emission Tomography (PET) Scan: Can help differentiate between a recurrent tumor and radiation necrosis.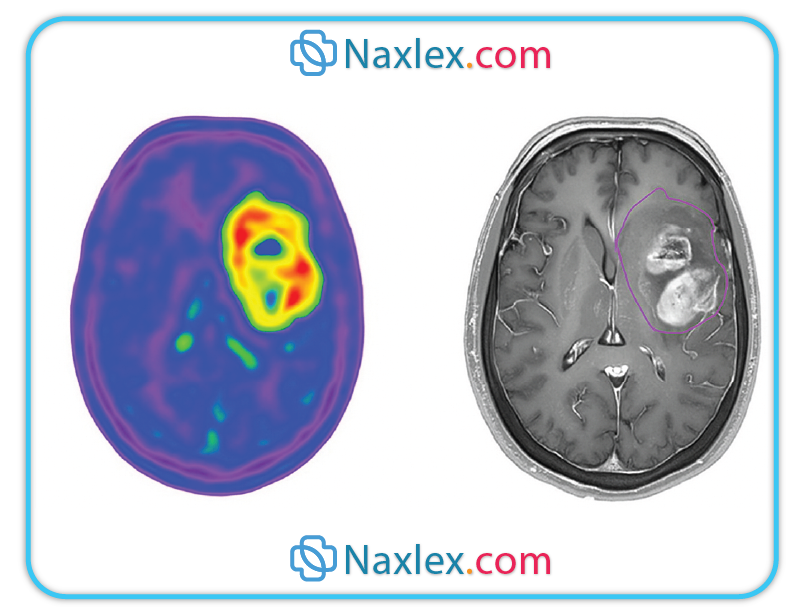 Cerebral Angiography: Provides visualization of the tumor's blood supply, which is important for surgical planning.
Cerebral Angiography: Provides visualization of the tumor's blood supply, which is important for surgical planning.
- Stereotactic Biopsy: A definitive diagnosis is made by obtaining a tissue sample of the tumor for microscopic examination. This is often done using a CT or MRI-guided needle.
Interprofessional Care
Surgical Therapy
- Craniotomy: Surgical removal of the tumor is the preferred treatment if the tumor is accessible and the removal will not cause irreversible neurological damage.
- Ventricular Shunt: May be inserted to drain cerebrospinal fluid (CSF) and relieve hydrocephalus.
- External Beam Radiation: Used post-surgery or as a primary treatment for inaccessible tumors.
- Stereotactic Radiosurgery (Gamma Knife or CyberKnife): Delivers a high dose of radiation to a precise area, minimizing damage to surrounding healthy tissue.
Chemotherapy drugs are used, but their effectiveness is limited due to the blood-brain barrier. The drug temozolomide (Temodar) is a common oral agent used for gliomas.
Nursing Management
Nursing Assessment
- Neurological Assessment: A thorough and continuous assessment of the patient's neurological status, including level of consciousness, motor and sensory function, cranial nerve function, and pupil response.
- Vital Signs: Monitor for signs of increased ICP, such as Cushing's triad (hypertension with a widened pulse pressure, bradycardia, and irregular respirations).
- Symptoms: Assess for the presence and severity of headaches, nausea, vomiting, seizures, and cognitive changes.
- Pre-operative: Assess baseline neurological function and prepare the patient psychologically and physically for surgery.
- Risk for Ineffective Cerebral Tissue Perfusion related to cerebral edema.
- Acute Pain related to increased intracranial pressure.
- Risk for Injury related to seizures.
- Disturbed Thought Processes related to brain tumor effects.
Nursing Interventions and Implementation
Pre-operative Care
- Provide education on the surgical procedure and what to expect post-operatively.
- Administer corticosteroids (e.g., dexamethasone) as ordered to reduce cerebral edema.
- Administer anti-seizure medications as prescribed.
Post-operative Care
- Positioning: Position the patient to prevent increased ICP. Avoid a sharp hip flexion or a head-down position. The head of the bed should be elevated to 30−45∘.
- Fluid and Electrolyte Management: Monitor for fluid balance and signs of diabetes insipidus or syndrome of inappropriate antidiuretic hormone (SIADH).
- Pain Management: Administer pain medication as needed, carefully monitoring for respiratory depression.
- Neurological Monitoring: Perform frequent neurological checks to detect any changes and report them immediately.
- Wound Care: Monitor the surgical site for signs of infection or CSF leakage.
- Increased Intracranial Pressure (ICP): Monitor for signs of increased ICP. Implement interventions such as head of bed elevation, avoidance of Valsalva maneuvers, and administration of mannitol or hypertonic saline as ordered.
- Cerebral Edema: Administer corticosteroids to reduce swelling.
- Seizures: Ensure seizure precautions are in place. Administer anti-seizure medications as prescribed.
- Hydrocephalus: Monitor for signs of hydrocephalus (e.g., headache, lethargy, vomiting) and prepare the patient for a ventricular shunt if needed.
Evaluation
- The patient maintains a stable neurological status.
- The patient's pain is managed effectively.
- The patient and family demonstrate an understanding of the plan of care and post-discharge needs.
- Complications are identified and managed promptly.
Summary
- Brain tumors are abnormal growths of cells in or around the brain that may be benign or malignant.
- They can be primary when they start in the brain or secondary when they spread from other body parts.
- The exact cause is often unknown, but genetic changes, radiation exposure, and certain inherited conditions increase risk.
- Common symptoms include headaches, seizures, nausea, vomiting, vision changes, weakness, and personality changes.
- Diagnosis is done through neurological exams, imaging tests like MRI or CT scans, and sometimes a biopsy.
- Treatment options include surgery, radiation therapy, chemotherapy, targeted therapy, and immunotherapy.
- Prognosis depends on the tumor’s type, size, location, growth rate, and the patient’s overall health.
- Complications may involve brain swelling, increased pressure, neurological problems, recurrence, and reduced quality of life.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Brain Tumors
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


