Please set your exam date
Pregnancy Signs
Study Questions
Practice Exercise 1
Which of the following is considered a presumptive sign of pregnancy?
Explanation
Pregnancy is identified through presumptive, probable, and positive signs, categorized by specificity. Presumptive signsare subjectiveand experienced by the woman. Probable signsare objective, observed by providers. Positive signsare definitiveevidence of a fetus. Nausea and vomiting, amenorrhea, breast changes, and quickeningare presumptive. Positive signs include fetal heart tones, visualization via ultrasound, and fetal movement felt by the examiner. Human chorionic gonadotropin (hCG) becomes detectable around day 8 post-fertilization and peaks between 60–70 days, but a positive test alone is not diagnostic.
Rationale for correct answers
3.Nausea and vomiting are classic presumptive signs of pregnancy, resulting from elevated estrogen and hCG levels. These symptoms are common in early pregnancy but are subjective and not exclusive to pregnancy.
Rationale for incorrect answers
1.A positive pregnancy test is a probable sign. It detects hCG, which rises after implantation. However, elevated hCG can also occur in trophoblastic disease or recent miscarriage, making it insufficient alone for diagnosis.
2.Auscultation of fetal heart tones is a positive sign. Fetal heart sounds are independent of the mother’s and confirm fetal presence. They can be detected by Doppler from 10–12 weeks of gestation.
4.Visualization of the fetus by ultrasound is a positive sign. Seeing the embryo or fetus with cardiac activity confirms intrauterine pregnancy. Cardiac motion can be seen by transvaginal ultrasound at approximately 5–6 weeks.
Take home points
• Nausea and vomiting are presumptive signs because they are subjective experiences.
• Positive pregnancy tests are probable signs due to the possibility of false positives.
• Fetal heart tones and ultrasound visualization are definitive indicators of pregnancy.
• Presumptive signs alone cannot confirm pregnancy; positive signs are required for confirmation.
A nurse is assessing a patient who reports nausea and vomiting at 8 weeks gestation. What is the most likely physiological cause of this symptom?
Explanation
Pregnancy is identified through presumptive, probable, and positive signs, categorized by specificity. Presumptive signsare subjectiveand experienced by the woman. Probable signsare objective, observed by providers. Positive signsare definitiveevidence of a fetus. Nausea and vomiting, amenorrhea, breast changes, and quickeningare presumptive. Positive signs include fetal heart tones, visualization via ultrasound, and fetal movement felt by the examiner. Human chorionic gonadotropin (hCG) becomes detectable around day 8 post-fertilization and peaks between 60–70 days, but a positive test alone is not diagnostic.
Rationale for correct answers
2.Elevated hCG levels are strongly associated with nausea and vomiting in early pregnancy. hCG peaks between 8–11 weeks and directly stimulates the chemoreceptor trigger zone in the brainstem, inducing nausea. This explains the timing and severity of symptoms during the first trimester.
Rationale for incorrect answers
1.Increased progesterone suppresses uterine contractions by relaxing smooth muscle but is not the primary cause of nausea and vomiting. Its main effects are maintaining the endometrial lining and reducing uterine irritability, not stimulating the vomiting center.
3.Increased blood volume begins rising early in pregnancy but peaks around 32–34 weeks. It does not directly irritate the gastric lining nor explain first-trimester nausea, which is hormonally mediated.
4.Uterine pressure on the stomach becomes relevant later in pregnancy, particularly in the third trimester, leading to reflux or reduced gastric capacity—not nausea at 8 weeks.
Take home points
• Nausea and vomiting at 8 weeks are primarily due to elevated hCG stimulating the chemoreceptor trigger zone.
• Progesterone relaxes smooth muscle but is not the main cause of nausea.
• Blood volume increases later and does not directly cause early pregnancy nausea.
• Uterine compression of the stomach causes late pregnancy symptoms, not first-trimester nausea.
Goodell’s sign is characterized by:
Explanation
Pregnancy is identified through presumptive, probable, and positive signs, categorized by specificity. Probable signsare objectivefindings observed by clinicians that strongly suggest pregnancy but are not definitive. These include Goodell’s sign, Chadwick’s sign, Hegar’s sign, and a positive pregnancy test. Goodell’s signis the softening of the cervical tipdue to increased vascularization caused by rising estrogen levels. It typically occurs around 6–8 weeksof gestation. Unlike presumptive signs, probable signs are observable and measurable, but still not conclusive without positive confirmation.
Rationale for correct answers
2.Goodell’s sign refers to softening of the cervical tip, detectable during a pelvic exam around 6–8 weeks. This change occurs due to increased vascularity and hypertrophy from elevated estrogen, classifying it as a probable sign of pregnancy.
Rationale for incorrect answers
1.Bluish discoloration of the vaginal mucosa is Chadwick’s sign, not Goodell’s. It results from increased blood flow to the cervix and vagina and appears around 6–8 weeks, also classified as a probable sign.
3.Softening of the lower uterine segment is Hegar’s sign, not Goodell’s. It is detected during bimanual examination around 6–12 weeks and reflects uterine softening below the cervix, also a probable sign.
4.Passive movement of the unengaged fetus during palpation is ballottement, not Goodell’s. It occurs between 16–18 weeks and is another probable sign, observed during a physical exam when the fetus rebounds after being pushed.
Take home points
• Goodell’s sign is cervical softening due to increased vascularization from estrogen.
• Chadwick’s sign is bluish discoloration of the cervix and vaginal mucosa.
• Hegar’s sign is softening of the lower uterine segment below the cervix.
• Ballottement is the passive rebound of the fetus when tapped during a pelvic exam.
Which of the following are presumptive signs of pregnancy? Select all that apply.
Explanation
Pregnancy is identified through presumptive, probable, and positive signs, categorized by specificity. Presumptive signsare subjectiveand experienced only by the pregnant individual. Probable signsare objective, observable by clinicians, but not definitive. Positive signsare conclusiveand confirm the presence of a fetus. Presumptive signsinclude nausea and vomiting, amenorrhea, breast tenderness, fatigue, and quickening(first fetal movement felt by the mother, usually at 16–20 weeks). These signs can result from causes other than pregnancy, thus are not diagnostic.
Rationale for correct answers
1.Amenorrhea is a presumptive sign because it is a subjective experience commonly caused by pregnancy. It occurs due to suppression of the hypothalamic–pituitary–ovarian axis by rising hCG and progesterone.
3.Nausea and vomiting are presumptive signs caused by rising hCG levels stimulating the chemoreceptor trigger zone. These symptoms are subjective and occur in other conditions, making them non-definitive.
5.Quickening refers to the woman’s first perception of fetal movement, usually between 16–20 weeks. It is a subjective experience and can be confused with gastrointestinal activity, classifying it as presumptive.
Rationale for incorrect answers
2.Fetal heart sounds are a positive sign. They provide direct evidence of fetal life and are detected by Doppler around 10–12 weeks. This confirms pregnancy beyond doubt.
4.Uterine enlargement is a probable sign. It is an objective finding noted during bimanual examination or ultrasound but may also result from tumors or fibroids. It suggests pregnancy but is not conclusive without positive signs.
Take home points
• Presumptive signs are subjective and felt only by the pregnant individual.
• Amenorrhea, nausea, and quickening are classic presumptive signs.
• Fetal heart tones and uterine growth are not presumptive—they are positive and probable, respectively.
• Presumptive signs must be confirmed with objective or positive findings.
Which of the following are probable signs of pregnancy? Select all that apply.
Explanation
Pregnancy is identified through presumptive, probable, and positive signs, categorized by specificity. Probable signsare objectivefindings noted by clinicians that suggest pregnancy but are not definitive. They include Chadwick’s sign, Goodell’s sign, Hegar’s sign, ballottement, uterine enlargement, and a positive hCG test. These signs result from physiological changes due to pregnancy but can also be mimicked by other gynecologic conditions such as tumors or hormonal imbalances. Unlike presumptive signs, they are observable; however, only positive signs can confirm pregnancy.
Rationale for correct answers
2.Chadwick’s sign is a probable sign. It is the bluish discoloration of the vaginal mucosa and cervix due to increased vascularity, seen around 6–8 weeks of gestation and detectable during pelvic examination.
3.Ballottement is a probable sign. It refers to the passive rebound of the fetus when the cervix is tapped, typically evident between 16–18 weeks. It is a physical exam finding that may suggest pregnancy.
5.Uterine enlargement, when palpated by a clinician, is a probable sign. The uterus increases in size due to the growing embryo, but similar enlargement can occur in cases of fibroids or adenomyosis.
Rationale for incorrect answers
1.Auscultation of fetal heart tones is a positive sign. It confirms the presence of a viable fetus and is typically detected by Doppler at 10–12 weeks. It is definitive and diagnostic for pregnancy.
4.Fatigue is a presumptive sign. It is a subjective experience reported by the pregnant woman and can be caused by many non-pregnancy-related conditions such as anemia, stress, or hypothyroidism.
Take home points
• Probable signs are objective but not conclusive for pregnancy.
• Chadwick’s sign, ballottement, and uterine enlargement are all probable signs.
• Fetal heart tones confirm pregnancy and are positive signs.
• Fatigue is a subjective presumptive sign and not observable by clinicians.
Practice Exercise 2
What is the definition of gravidity in the context of maternal-newborn nursing?
Explanation
Gravidity refers to the total number of pregnancies, regardless of their outcome or duration. In maternal-newborn nursing, gravidadenotes any instance of conception, including ectopic, miscarriage, or molarpregnancies. Paritydiffers, referring to the number of pregnancies reaching viability (≥20 weeks gestation). A nulligravidahas never been pregnant; a primigravidais pregnant once; a multigravidahas had two or more pregnancies. This terminology is essential in clinical documentation and the GTPAL system, which includes Gravida, Term births, Preterm births, Abortions, and Living children.
Rationale for correct answers
2.Gravidity is defined as the total number of times a woman has been pregnant, irrespective of duration or outcome. This includes current pregnancies, miscarriages, abortions, and ectopic pregnancies.
Rationale for incorrect answers
1.The number of pregnancies reaching 20 weeks refers to parity, not gravidity. Parity indicates pregnancies that progressed to viability, regardless of whether the fetus was born alive or not.
3.The number of living children refers to the "L"in the GTPALsystem (Living), not gravidity. It indicates the number of children currently alive.
4.The number of preterm births before 37 weeks is captured under "P"in GTPAL, specifically for preterm deliveries, not gravidity.
Take home points
• Gravidity counts all pregnancies, regardless of duration or outcome.
• Parity refers to pregnancies that reached 20 weeks gestation.
• Living children are documented separately under "L" in GTPAL.
• GTPAL is used to provide a full obstetric history overview.
A woman is pregnant for the third time. Her first pregnancy resulted in a live birth at 40 weeks, and her second ended in a stillbirth at 28 weeks. What is her gravidity?
Explanation
Gravidity refers to the total number of times a woman has been pregnant, regardless of the outcome, duration, or number of fetuses. Each conceptionevent counts as one, whether the pregnancy ends in live birth, stillbirth, abortion, or is ongoing. Parity, in contrast, reflects the number of pregnancies that progressed to 20 or more weeks. In the GTPALsystem, Gstands for gravidity, which includes currentand prior pregnancies, no matter the outcome or gestational age.
Rationale for correct answers
3.She is currently pregnant for the third time. Gravidity includes all pregnancies: the first (live birth at 40 weeks), the second (stillbirth at 28 weeks), and the current (ongoing) pregnancy. Thus, gravidity = 3.
Rationale for incorrect answers
1.This would only be correct if she had been pregnant once, which is not the case. She has two completed pregnancies and is currently pregnant.
2.This excludes the current pregnancy. Gravidity includes all pregnancies, including the ongoing one.
4.This would suggest she has had four pregnancies, but the case describes only three: two prior and one current.
Take home points
• Gravidity counts all pregnancies, including the current one, regardless of outcome.
• Stillbirths are included in gravidity and parity (if ≥20 weeks).
• Parity is determined by gestational age, not fetal outcome (live vs. stillbirth).
• GTPAL helps differentiate gravidity from specific birth outcomes.
A nurse is assessing a patient who reports four pregnancies: two term births, one preterm birth, and one miscarriage. What is the patient’s GTPAL if all children are living?
Explanation
The GTPAL systemis a structured method to summarize a woman’s obstetric history. It breaks down into:
G(Gravida) = total number of pregnancies, including current and past, regardless of outcome.
T(Term births) = number of deliveries at ≥37 weeks gestation.
P(Preterm births) = number of deliveries between 20–36⁶⁄₇ weeks gestation.
A(Abortions) = number of pregnancies ending before 20 weeks, including spontaneous and elective abortions.
L(Living) = number of currently living children. Each component refers to pregnancies—not number of fetuses (e.g., twins count as one birth).
Rationale for correct answers
1.G4 T2 P1 A1 L3 accurately reflects:
• 4 total pregnancies (G4)
• 2 term births (T2)
• 1 preterm birth (P1)
• 1 miscarriage before 20 weeks (A1)
• All 3 children alive (L3)
Rationale for incorrect answers
2.This lists 2 abortions (A2), which is incorrect—the patient had only 1 miscarriage. Also, P0 suggests no preterm birth, but one preterm delivery is reported.
3.G3 undercounts the number of pregnancies. The patient had 4 pregnancies (2 term, 1 preterm, 1 miscarriage), so G should be 4, not 3.
4.T1 is incorrect—the patient had 2 term births. A2 is also wrong—only one miscarriage is noted. L2 is inaccurate, as all 3 children are alive.
Take home points
• GTPAL reflects all pregnancies, not number of children born.
• Miscarriages and abortions before 20 weeks count under “A”.
• Preterm birth = delivery from 20 to 36⁶⁄₇ weeks gestation.
• Living = number of currently living children, not deliveries.
Which of the following statements accurately describe "gravidity"? Select all that apply.
Explanation
Gravidityrefers to the total number of pregnancies, including the current pregnancy, regardless of outcome, gestational age, or number of fetuses. It does not count individual fetuses—a twin pregnancy still counts as one gravida. Paritydiffers from gravidity by measuring pregnancy outcomes, including term and preterm deliveries. Gravidity is strictly quantitative and does not reflect fetal viability or number of living children.
Rationale for correct answers
1.Gravidity includes all confirmed pregnancies, regardless of outcome—whether the pregnancy ended in miscarriage, abortion, stillbirth, or live birth.
3.The current pregnancy is always includedin the gravidity count. If a woman is pregnant now and had two previous pregnancies, she is gravida 3.
Rationale for incorrect answers
2.Gravidity does not count fetusesindividually. A pregnancy with twins or triplets is still counted as a single pregnancy under gravidity, not multiple.
4.Gravidity includes all pregnancies, not just those that result in live births. It encompasses miscarriages, ectopic pregnancies, and stillbirths as well.
5.Gravidity is not synonymouswith the number of living children. A woman may be gravida 3 with no living children if all ended in miscarriage or stillbirth.
Take home points
• Gravidity includes all pregnancies, regardless of number of fetuses or outcome.
• The current pregnancy is always counted in gravidity.
• Gravidity is not affected by whether the child was born alive or survived.
• Gravidity differs from parity, which relates to pregnancy outcomes.
Which of the following are included in the parity count? Select all that apply.
Explanation
Parity countrefers to the number of pregnancies carried beyond 20 weeks gestation, regardless of the outcome. Parityreflects the uterine exposure to pregnancy, not the viability of the fetus. A fetus delivered after 20 weeks(≥20 0/7 weeks), whether live or stillborn, is counted in parity. Gestational age is measured from the first day of the last menstrual period. Preterm refers to 20 to 36 6/7 weeks, and term is 37 to 41 6/7 weeks. A pregnancy loss before 20 weeks(miscarriage or elective abortion) is counted under gravidity, not parity.
Rationale for correct answers
1.A delivery at 39 weeks is considered a term delivery. Since it is beyond 20 weeks, it is included in the parity count regardless of the outcome.
2.A birth at 34 weeks is a preterm delivery. Preterm means between 20 and 36 6/7 weeks. This gestation qualifies as a pregnancy that has progressed beyond 20 weeks and is thus counted in parity.
4.A stillbirth at 22 weeks qualifies for parity because it exceeds the 20-week threshold. Parity includes pregnancies ending in stillbirth as long as the gestational age was ≥20 weeks.
Rationale for incorrect answers
3.A miscarriage at 15 weeks is not counted in parity because it occurred before 20 weeks gestation. Pregnancies ending before 20 weeks are classified under gravidity. The fetus was not viable, and the uterus was not exposed to the pregnancy long enough to meet parity criteria.
5.An elective abortion at 10 weeks does not meet the threshold of 20 weeks gestation and is not included in parity. It is counted only under gravidity. Regardless of the reason for the termination, the pregnancy did not progress far enough for parity.
Take home points
• Parity includes all pregnancies that reached 20 weeks gestation or more, regardless of the outcome.
• Miscarriages and abortions before 20 weeks are not included in parity but are part of gravidity.
• Stillbirths after 20 weeks are counted in parity, despite the absence of live birth.
• Term is 37 to 41 6/7 weeks; preterm is 20 to 36 6/7 weeks; viability starts near 24 weeks but parity starts at 20 weeks.
Practice Exercise 3
A pregnant client reports her last menstrual period (LMP) began on May 10, 2020. Using Näegele’s Rule, what is her estimated date of delivery (EDD)?
Explanation
Nägele’s Ruleestimates the expected date of delivery (EDD)by calculating 280 days (40 weeks)from the first day of the last menstrual period (LMP). It assumes a 28-day menstrual cyclewith ovulation on day 14. The standard formula is: LMP + 1 year − 3 months + 7 days. This rule provides an approximate due date for full-term pregnancy, but its accuracy decreases in clients with irregular cycles or uncertain LMP. Ultrasounddating is preferred if menstrual history is unreliable. Normal gestation ranges from 37 to 42 weeks.
Rationale for correct answer
1.LMP = May 10, 2020. Using Nägele’s Rule:
→ Add 1 year = May 10, 2021
→ Subtract 3 months = February 10, 2021
→ Add 7 days = February 17, 2021
This gives an estimated date of delivery of February 17, 2021.
Rationale for incorrect answers
2.February 3, 2021 is incorrect. This would only be accurate if the LMP had been April 27, 2020. It results from either miscalculating the LMP or adding the wrong number of days. It shortens gestation to about 38 weeks instead of 40.
3.August 17, 2021 is 15 months from the LMP, extending the pregnancy far beyond the normal 280-day gestation. This choice reflects a critical misunderstanding of the formula and is not physiologically plausible.
4.March 10, 2021 is incorrect. It adds 10 months rather than adjusting by Nägele’s Rule. This calculation mistakenly adds only months without following the 1 year − 3 months + 7 days pattern. It leads to a gestation of about 44 weeks.
Take home points
• Nägele’s Rule: LMP + 1 year − 3 months + 7 days.
• Full-term pregnancy is 280 days (40 weeks) from LMP.
• Normal range for delivery is 37 to 42 weeks gestation.
• LMP-based EDD is less reliable with irregular cycles.
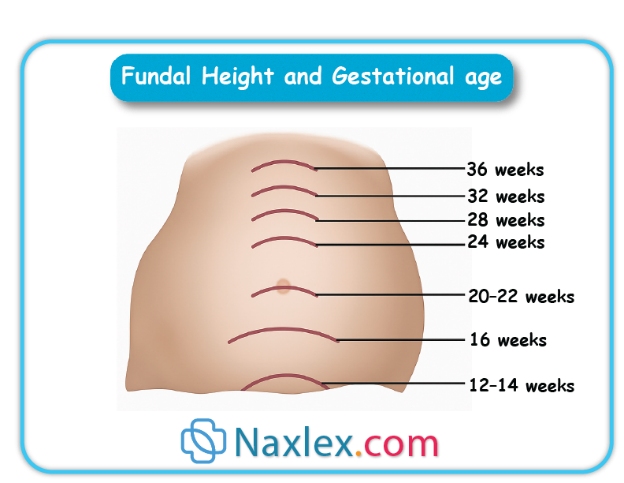
A nurse is assessing a patient at 28 weeks gestation. Which physical assessment finding supports the estimation of gestational age?
Explanation
Fundal height measurementis a key tool for estimating gestational ageduring pregnancy, particularly from 20 to 36 weeks. The height of the uterine fundus, measured in centimeters from the symphysis pubis to the top of the fundus, roughly correlates with gestational age in weeks(±2 cm). This correlation is most accurate between 20 and 36 weeks, when the uterus grows at a consistent rate. Deviations outside this range may indicate intrauterine growth restriction, macrosomia, polyhydramnios, or oligohydramnios. Normal fetal heart tonesrange from 110 to 160 beats per minuteand are typically heard by 10 to 12 weekswith Doppler.
Rationale for correct answer
4.A fundal height of 28 cm at 28 weeks gestation directly supports normal growth and matches the expected correlation between fundal height and gestational age. This is within the normal ±2 cm range, indicating appropriate fetal development.
Rationale for incorrect answers
1.A fundal height of 20 cm is consistent with approximately 20 weeks gestation, not 28 weeks. This finding suggests either incorrect dating or possible intrauterine growth restriction and does not support a 28-week pregnancy.
2.Fetal heart tones should be clearly audible by 10 to 12 weeks gestation. At 28 weeks, absence of fetal heart tones is an abnormal and concerning finding and may indicate fetal demise, not normal gestational progression.
3.Quickening, or the mother's perception of fetal movement, usually occurs between 16 and 20 weeksgestation. By 28 weeks, fetal movement should be regularly felt. Not yet reporting quickening at this stage is abnormal and does not support a 28-week gestation.
Take home points
• Fundal height in cm = gestational age in weeks (±2 cm) from 20 to 36 weeks.
• At 28 weeks, expected fundal height is around 28 cm.
• Absence of fetal heart tones after 12 weeks is abnormal.
• Quickening is typically felt between 16 to 20 weeks.
Which of the following methods is considered the most accurate for estimating gestational age in the first trimester?
Explanation
Crown-rump length (CRL)is the most accurate methodfor estimating gestational ageduring the first trimester. CRL is measured via transvaginal or transabdominal ultrasoundfrom the top of the fetal head (crown)to the bottom of the torso (rump). This measurement is reliable between 6 and 13 6/7 weeks gestation, with an accuracy of ±3 to 5 days. It is superior to other methods due to low biological variabilityin early fetal growth. After 14 weeks, other biometric parameters like biparietal diameter (BPD)and femur length (FL)are used.
Rationale for correct answer
3.CRL via ultrasound in the first trimester is the gold standard for dating pregnancy. It has the least margin of error compared to other methods, especially before 14 weeks gestation. It provides a highly reproducible and objective measurement.
Rationale for incorrect answers
1.Fundal height measurement is not accurate in the first trimester. Uterine growth is not easily palpable or consistent before 20 weeks. This method becomes more useful only after 20 weeks gestation when the fundal height correlates with gestational age.
2.LMP is commonly used but less accurate than CRL because it relies on patient memory and assumes a regular 28-day cycle with ovulation on day 14. Cycle variability, implantation timing, and irregular periods can lead to dating errors.
4.Fetal heart tones with a fetoscope are typically not heard until around 18 to 20 weeks gestation. Auscultation does not provide precise gestational dating and is not a first-trimester tool.
Take home points
• CRL on first-trimester ultrasound is the most precise method for early gestational age assessment.
• LMP can be inaccurate if cycles are irregular or dates are uncertain.
• Fundal height is useful only from 20 weeks onward.
• Fetoscope detects heart tones late; not reliable for early dating.
Which of the following factors can affect the accuracy of fundal height measurements? Select all that apply.
Explanation
Fundal height measurementis a clinical method used from 20 to 36 weeks gestationto estimate fetal growth and gestational age. It involves measuring the distance in centimeters from the symphysis pubis to the uterine fundus, which should approximately equal the number of weeks gestation (±2 cm). However, measurement accuracycan be affected by several physiological and anatomical factors, especially those that alter abdominal wall thickness, uterine shape, or fluid content. Fundal height is not influencedby maternal blood pressure or fetal heart rate.
Rationale for correct answers
1.Maternal obesity can affect accuracy by increasing abdominal wall thickness, which can make palpation of the fundus difficult and lead to underestimation or overestimation of fundal height.
2.Fetal position impacts fundal height. For example, a transverse lie or breech presentation may alter uterine shape and cause the fundal height to be lower or higher than expected.
3.Amniotic fluid volume affects uterine distention. Polyhydramnioscan elevate fundal height, while oligohydramnioscan decrease it, leading to inaccurate correlation with gestational age.
Rationale for incorrect answers
4.Maternal blood pressure does not alter uterine size or fundal height. Hypertension may impact placental perfusion and fetal growth over time, but it does not acutely change fundal height measurement.
5.Fetal heart rate does not influence fundal height. While it is a vital sign of fetal well-being, it has no structural or volumetric effect on uterine growth or size.
Take home points
• Fundal height ≈ gestational age in cm from 20 to 36 weeks.
• Maternal obesity, fetal lie, and amniotic fluid volume affect measurement accuracy.
• Blood pressure and heart rate do not influence fundal height.
• Ultrasound should confirm growth if measurements are abnormal.
Which of the following are methods used to estimate fetal age? Select all that apply.
Explanation
Fetal age estimationis essential for monitoring fetal development, planning care, and timing interventions. The most common methods include last menstrual period (LMP), ultrasound, and maternal perception of fetal movement (quickening). Each method varies in accuracy depending on gestational age. Ultrasoundis most accurate in the first trimester, particularly using crown-rump length (CRL). LMPrelies on regular 28-day cycles and may be inaccurate if dates are uncertain. Quickeningis subjective but can help confirm gestational progress. Maternal weight gainand fetal heart ratedo not accurately indicate fetal age.
Rationale for correct answers
1.LMP is a traditional method used to estimate gestational age. It assumes a 28-day cycle with ovulation on day 14. The expected date of delivery is calculated using Nägele’s Rule: LMP + 1 year − 3 months + 7 days.
2.Ultrasound is the most accurate method, especially in the first trimester. Crown-rump length (CRL) gives precise gestational age (±3–5 days). In the second and third trimesters, biparietal diameter, femur length, and head/abdominal circumference are used.
5.Quickening refers to the first maternal perception of fetal movement, usually between 16 and 20 weeks gestation. While subjective and variable, it supports estimation when combined with other clinical data.
Rationale for incorrect answers
3.Maternal weight gain is influenced by many variables such as pre-pregnancy BMI, diet, metabolism, and edema. It does not provide a reliable or consistent method for estimating fetal age.
4.Fetal heart rate ranges from 110 to 160 bpm and can vary with gestational age, activity, and oxygenation. However, it does not correlate linearly with gestational age and cannot be used to accurately date a pregnancy.
Take home points
• LMP, early ultrasound, and quickening are valid tools for fetal age estimation.
• Ultrasound is the most accurate in the first trimester.
• Weight gain and fetal heart rate are not valid dating tools.
• First-trimester CRL has a ±3–5 day accuracy range.
Comprehensive Questions
What is the primary hormonal contributor to the softening of the cervix, known as Goodell’s sign?
Explanation
Goodell’s signrefers to the softening of the cervix, typically observed around 4 to 6 weeks of gestation, and is considered a probable sign of pregnancy. This softening is primarily due to the action of estrogen, which increases vascularization, promotes edema, and causes hypertrophy of cervical glands. Estrogen also stimulates growth of uterine tissues and prepares the reproductive tract for pregnancy. Normal estrogen levels vary by trimester, but in pregnancy, estriol(an estrogen subtype) increases significantly and plays a key role in uteroplacental blood flow.
Rationale for correct answer
3.Estrogen is the primary hormone responsible for cervical softening in early pregnancy. It enhances vascularity and tissue remodeling in the cervix, leading to the soft, velvety texture characteristic of Goodell’s sign.
Rationale for incorrect answers
1.Prolactin is produced by the anterior pituitary and primarily supports lactogenesis. It prepares breast tissue for milk production and has no direct role in cervical softening or changes associated with Goodell’s sign.
2.Human chorionic gonadotropin (hCG) is secreted by the trophoblast after implantation and maintains the corpus luteum in early pregnancy. While it sustains progesterone production, it does not directly affect cervical softening.
4.Oxytocin is a posterior pituitary hormone responsible for uterine contractionsduring labor and milk ejectionpostpartum. It plays no role in the early cervical changes observed in Goodell’s sign.
Take home points
• Goodell’s sign is softening of the cervix by 4–6 weeks gestation.
• Estrogen is the main hormone responsible for cervical softening.
• hCG supports corpus luteum but doesn’t soften the cervix.
• Prolactin and oxytocin are unrelated to early cervical changes.
The Linea Nigra is a dark line on the abdomen caused by:
Explanation
1.Muscle stretching contributes to striae gravidarum (stretch marks)but does not cause pigmentation. It does not influence melanin activity or result in the darkening of the linea alba.
3.Fat deposition occurs during pregnancy as maternal energy storage, but it is not responsible for pigmentation changes. It may contribute to skin stretching but not to linea nigra formation.
4.Uterine contractions are related to labor and Braxton Hicks activity. They have no effect on skin pigmentation or MSH levels.
Take home points
• Linea nigra results from hormonal stimulation of melanocytes.
• MSH, along with estrogen and progesterone, causes hyperpigmentation.
• Linea nigra is a normal finding and not associated with pathology.
• Muscle stretch and fat deposition do not cause pigmentation.
A nurse is using a Doppler device to assess a patient at 11 weeks gestation. What is the expected range for fetal heart rate?
Explanation
Fetal heart rate (FHR)is an important indicator of fetal well-beingand can be detected by Doppler ultrasoundas early as 10 to 12 weeks gestation. The normal fetal heart rate rangethroughout pregnancy is 110 to 160 beats per minute (bpm). Rates above or below this range may indicate fetal distress, hypoxia, or cardiac abnormalities. The FHR is regulated by the autonomic nervous system, particularly the sympathetic and parasympathetic balance, and gradually decreases as the pregnancy progresses from early tachycardia to a stable range.
Rationale for correct answer
2.At 11 weeks gestation, a Doppler device should detect a fetal heart rate between 110 and 160 bpm, which is the established normal range. This rate reflects normal autonomic regulation and cardiac development at this gestational age.
Rationale for incorrect answers
1.80–100 bpm is below the normal fetal range and may suggest bradycardiaor an inability to distinguish maternal from fetal heart sounds. Fetal bradycardia at this stage would be considered pathological.
3.160–200 bpm exceeds the upper limit of normal. While early in the first trimester fetal heart rate may be transiently high, by 11 weeks, it typically stabilizes below 160 bpm. A sustained rate >160 bpm suggests tachycardiaand may signal infection, maternal fever, or hypoxia.
4.200–240 bpm is dangerously high and not typical for any normal stage of fetal development. This level of tachycardia suggests a serious arrhythmiaor fetal compromiseand warrants immediate investigation.
Take home points
• Normal fetal heart rate from 10 weeks onward is 110–160 bpm.
• Doppler can detect fetal heart tones reliably by 10–12 weeks.
• Persistent rates <110 or >160 bpm require evaluation.
• Maternal pulse must be differentiated from fetal heart tones.
Which term describes a woman who has never completed a pregnancy to 20 weeks gestation or more?
Explanation
Gravidity and parity terminology is used to describe a woman’s obstetric history. Gravidityrefers to the number of times a woman has been pregnant, regardless of outcome. Parityis the number of pregnanciesthat progressed to viability, which is defined as ≥20 weeks gestation. A pregnancy that ends before 20 weeks, whether spontaneous or elective, does not count toward parity. This system helps clinicians determine reproductive risks and outcomes. A pregnancy reaching 20 weeks, even if ending in stillbirth, counts in parity.
Rationale for correct answers
3.Nullipara describes a woman who has never completed a pregnancy to the point of viability (20 weeks or more). This includes women who have had abortions or miscarriages before 20 weeks, or who have never been pregnant. The stem specifically asks about not completing a pregnancy to 20 weeks or more, making this the correct term.
Rationale for incorrect answers
1.Primigravida refers to a woman who is pregnant for the first time. This term does not convey whether the pregnancy reached 20 weeks. It describes the number of pregnancies, not outcomes.
2.Multipara describes a woman who has completed two or more pregnancies to ≥20 weeks gestation. The question describes someone who has not completed even one pregnancy to that point, making this term inaccurate.
4.Primipara refers to a woman who has completed one pregnancy to 20 weeks gestation or more, regardless of whether the infant was born alive or stillborn. Since the individual in the question has never completed a pregnancy to 20 weeks, this term is not applicable.
Take home points
• Nullipara means no completed pregnancy beyond 20 weeks gestation.
• Parity includes all pregnancies ≥20 weeks, regardless of fetal outcome.
• Gravidity refers to number of pregnancies, not their outcomes.
• Primigravida is unrelated to pregnancy duration or viability.
and one ongoing pregnancy. What is the patient’s gravidity?
Explanation
Gravidityis the total number of confirmed pregnancies a woman has had, regardless of the outcome or duration. It includes the current pregnancy, any live births, miscarriages, abortions, and ectopic pregnancies. A pregnancyis a period of about 9 months in humans, where one or more offspring develop inside a woman's uterus. The normal gestation period is 37 to 42 weeks. Parity refers to the number of times a woman has given birth to a fetus that has reached 20 weeks of gestation or more.
Rationale for correct answers
3.Gravidity is the number of all confirmed pregnancies a woman has had, regardless of the outcome or how long each pregnancy lasted. In this case, the patient had 1 term birth, 1 miscarriage, and 1 ongoing pregnancy, for a total of 3 pregnancies. Therefore, the patient is a gravida 3.
Rationale for incorrect answers
1.Gravida 1 indicates a woman who is in her first pregnancy. The patient in the question has had a total of 3 pregnancies, with 2 previous pregnancies that ended in a term birth and a miscarriage. Therefore, this choice is incorrect.
2.Gravida 2 indicates a woman who is in her second pregnancy. The patient in the question has had a total of 3 pregnancies, with 2 previous pregnancies that ended in a term birth and a miscarriage. Therefore, this choice is incorrect.
4.Gravida 4 indicates a woman who has had 4 pregnancies. The patient in the question has had 1 term birth, 1 miscarriage, and 1 ongoing pregnancy, which adds up to a total of 3 pregnancies. Therefore, this choice is incorrect.
Take home points
• Gravidity is the number of all confirmed pregnancies.
• Parity is the number of pregnancies carried to at least 20 weeks.
• The G in the GTPAL system stands for gravidity.
• The P in the GTPAL system stands for parity.
A client has a GTPAL of 4-2-1-1-3. How many living children does she have?
Explanation
The GTPAL system is a standardized method for documenting a woman’s obstetric history. It includes gravida, term births, preterm births, abortions, and living children. Gravida refers to the total number of pregnancies regardless of outcome. Term births are deliveries after 37 weeks gestation, while preterm births occur between 20 and 36 weeks. Abortions include both spontaneous and elective losses before 20 weeks. Living children are those currently alive. This format helps assess maternal and fetal risk and guides prenatal care planning.
Rationale for correct answers
4.The fifth digit in the GTPAL sequence represents the number of living children. In the sequence 4-2-1-1-3, the final digit is 3, indicating the client has 3 living children. This is a direct interpretation based on the GTPAL format.
Rationale for incorrect answers
1.A value of 0 for living children contradicts the fifth digit of the GTPAL sequence, which is 3. This indicates that 3 children are currently alive.
2.A value of 1 is incorrect because the fifth digit clearly states 3 living children. There is no ambiguity in this representation.
3.A value of 2 does not match the fifth digit of the GTPAL sequence. The client has 3 living children, as indicated by the final number.
Take home points
• GTPAL documents gravida, term, preterm, abortions, and living children.
• The fifth digit in GTPAL directly indicates the number of living children.
• Term births are ≥37 weeks; preterm births are 20–36 weeks.
• Abortions include all pregnancy losses before 20 weeks.
Which condition may be indicated by a fundal height measurement significantly larger than expected for gestational age?
Explanation
Fundal height measurement is a clinical method used to assess fetal growth and uterine size. From 20 to 36 weeks gestation, fundal heightin centimeters should approximate gestational agein weeks (±2 cm). A significantly larger measurement may suggest polyhydramnios, multiple gestation, or macrosomia. Polyhydramniosis defined by an amniotic fluid index (AFI)>24 cm or a single deepest pocket >8 cm. Excess fluid volume increases uterine distension, leading to a fundal height greater than expected. Normal AFI ranges from 8 to 18 cm.
Rationale for correct answers
3.Polyhydramnios causes excessive accumulation of amniotic fluid, increasing intrauterine volume and resulting in a fundal height larger than expected. It may be associated with fetal anomalies, maternal diabetes, or idiopathic causes.
Rationale for incorrect answers
1.Intrauterine growth restriction (IUGR) is characterized by fetal weight below the 10th percentile for gestational age. It typically presents with a fundal height smaller than expected due to reduced fetal size or placental insufficiency.
2.Oligohydramnios is defined by AFI <5 cm or deepest pocket <2 cm. It leads to decreased uterine volume and a fundal height smaller than expected, not larger.
4.Correct dating of pregnancy ensures accurate correlation between gestational age and fundal height. It does not cause abnormal fundal height measurements; rather, it helps detect discrepancies due to pathological conditions.
Take home points
• Fundal height should match gestational age ±2 cm between 20–36 weeks.
• Polyhydramnios causes elevated fundal height due to excess amniotic fluid.
• IUGR and oligohydramnios typically present with reduced fundal height.
• Accurate dating is essential for interpreting fundal height measurements.
Which of the following methods is considered the most accurate for estimating gestational age in the first trimester?
Explanation
Gestational age estimation in early pregnancy is critical for guiding prenatal care, screening, and delivery planning. The most accurate method in the first trimesteris ultrasound measurement of crown-rump length (CRL). CRL is the length from the top of the fetal head to the bottom of the torso and is highly reliable between 7 and 13 weeks gestation, with an accuracy of ±3 to 5 days. Fundal heightbecomes useful only after 20 weeks. LMPcan be imprecise due to cycle variability. Fetal heart tonesare typically detectable by fetoscope after 18 to 20 weeks.
Rationale for correct answers
3.Crown-rump length measured via ultrasound between 7 and 13 weeks is the most accurate method for estimating gestational age. It provides precision within ±3 to 5 days and is unaffected by maternal recall or uterine anomalies.
Rationale for incorrect answers
1.Fundal height measurement is not reliable in the first trimester due to the small uterine size. It becomes clinically useful only from 20 weeks onward, with a ±2 cm margin of error.
2.Last menstrual period (LMP) is subject to inaccuracies due to irregular cycles, implantation bleeding, or poor recall. It assumes ovulation on day 14, which is not consistent across all women.
4.Auscultation of fetal heart tones with a fetoscope is not possible in the first trimester. Heart tones are typically audible by fetoscope only after 18 to 20 weeks, making it unsuitable for early gestational dating.
Take home points
• CRL via ultrasound is the most accurate method for dating in the first trimester.
• LMP-based dating is prone to error due to cycle variability.
• Fundal height is useful only after 20 weeks gestation.
• Fetal heart tones by fetoscope are detectable after 18–20 weeks.
A nurse is preparing to measure the fundal height of a pregnant patient at 28 weeks gestation. What is the expected fundal height measurement in centimeters?
Explanation
Fundal height measurement is a clinical tool used to assess fetal growth and gestational age from 20 to 36 weeks. During this period, fundal height in centimetersshould approximately equal gestational age in weeks(±2 cm). At 28 weeks gestation, the expected fundal height is 26 to 30 cm. Deviations may indicate conditions such as polyhydramnios, oligohydramnios, IUGR, or incorrect dating. Measurement is taken from the pubic symphysisto the top of the uterine fundususing a non-stretchable tape.
Rationale for correct answers
3.At 28 weeks gestation, the expected fundal height is 28 cm ±2 cm, which corresponds to a range of 26 to 30 cm. This makes 28–30 cm the most accurate choice.
Rationale for incorrect answers
1.A fundal height of 20–22 cm is expected around 20 to 22 weeks gestation. At 28 weeks, this would be significantly below expected and may suggest IUGR or oligohydramnios.
2.A range of 25–27 cm is slightly below the expected value for 28 weeks. While it may still fall within the ±2 cm margin, 28–30 cm is more precise and appropriate.
4.A fundal height of 32–34 cm is expected around 32 to 34 weeks gestation. At 28 weeks, this would be elevated and may suggest polyhydramnios, macrosomia, or incorrect dating.
Take home points
• Fundal height ≈ gestational age in weeks ±2 cm from 20–36 weeks.
• At 28 weeks, expected fundal height is 26–30 cm.
• Deviations may indicate growth abnormalities or fluid volume issues.
• Measurement technique must be standardized for accuracy.
The primary reason for accurately determining gestational age is to:
Explanation
Accurate determination of gestational ageis essential for guiding prenatal care, assessing fetal development, and timing clinical interventions. Gestational age influences decisions regarding screening tests, growth monitoring, and delivery planning. It is calculated using last menstrual period (LMP)and confirmed by ultrasound, especially crown-rump length in the first trimester. Normal fetal growth follows predictable patterns; deviations may indicate IUGR, macrosomia, or congenital anomalies. Accurate dating ensures appropriate timing of interventions such as corticosteroid administration for lung maturity or induction of labor.
Rationale for correct answers
3.Monitoring fetal growth and development and timing interventions is the primary reason for determining gestational age. It allows clinicians to assess whether the fetus is growing appropriately and to plan interventions like antenatal corticosteroids or delivery in cases of fetal compromise.
Rationale for incorrect answers
1.Birth weight cannot be predicted exactly based on gestational age alone. While gestational age provides a framework for expected growth, many factors including genetics and maternal health influence final birth weight.
2.Labor induction is not scheduled solely based on gestational age unless medically indicated. Induction before 39 weeks without indication increases neonatal risks. Accurate dating helps avoid premature or delayed induction.
4.Fetal gender determination is not the primary reason for dating. Gender can be identified via ultrasound or genetic testing, but gestational age is critical for broader clinical decisions.
Take home points
• Gestational age guides fetal growth monitoring and clinical interventions.
• Accurate dating is essential for timing prenatal tests and delivery.
• Birth weight prediction is multifactorial, not solely based on gestational age.
• Gender determination is not a clinical priority for dating.
Which of the following are positive signs of pregnancy? Select all that apply.
Explanation
Positive signs of pregnancy are those that provide objective, direct evidenceof a developing fetus. These signs are observableand measurableby a clinician, confirming pregnancy beyond doubt. They include fetal heart tones, ultrasound visualization, and palpable fetal movements. In contrast, probable signsare suggestive but not definitive, and presumptive signsare subjective experiences reported by the patient. Fetal heart tones are typically detectable by Doppler around 10–12 weeks, and fetal movements can be palpated by the examiner after 20 weeks. Ultrasound can confirm fetal presence as early as 5–6 weeks gestation.
Rationale for correct answers
1.Fetal heart sounds detected by Doppler or fetoscope are a direct, objective confirmation of fetal life, making this a positive sign of pregnancy.
3.Ultrasound visualization of the fetus provides indisputable evidence of pregnancy. Gestational sac can be seen by 5 weeks, and fetal pole with cardiac activity by 6–7 weeks.
5.Fetal movements palpated by the examiner are a positive sign, typically detectable after 20 weeks gestation. This is distinct from maternal perception of movement (quickening), which is subjective.
Rationale for incorrect answers
2.Quickening refers to the mother’s subjective sensation of fetal movement, usually felt between 16–20 weeks. It is a presumptive sign, not confirmatory.
4.Hegar’s sign is softening of the lower uterine segment, detected during bimanual exam around 6–8 weeks. It is a probable sign, suggestive but not definitive.
Take home points
• Positive signs of pregnancy are objective and directly confirm fetal presence.
• Fetal heart tones, ultrasound visualization, and examiner-palpated movements are positive signs.
• Quickening is a presumptive sign based on maternal perception.
• Hegar’s sign is a probable sign based on physical changes.
Which of the following are true regarding the distinction between gravidity and parity? Select all that apply.
Explanation
Gravidity and parity are terms used to describe a woman’s obstetric history. Gravidityrefers to the total number of pregnancies, regardless of outcome, including the current pregnancy. Parityrefers to the number of pregnancies reaching viability, typically defined as ≥20 weeks gestation, regardless of whether the fetus was born alive or stillborn. Multiple gestations(e.g., twins) count as one pregnancy for both gravidity and parity. Stillbirthsafter 20 weeks are included in parity but do not affect gravidity beyond the pregnancy count.
Rationale for correct answers
1.Gravidity includes all pregnancies, regardless of outcome, while parity only includes pregnancies that reached ≥20 weeks gestation. This distinction is fundamental in obstetric documentation.
4.Both gravidity and parity count multiple gestations (e.g., twins, triplets) as one pregnancy event. Gravidity counts the pregnancy itself, not the number of fetuses.
Rationale for incorrect answers
2.Gravidity includes the current pregnancy, as it reflects the total number of pregnancies. Parity does not include the current pregnancy until it reaches viability (≥20 weeks), so this statement is incorrect.
3.Gravidity does not count individual fetuses; it counts pregnancies. For example, a twin pregnancy counts as one gravid event. Parity also counts pregnancies, not individual fetuses.
5.Stillbirths after 20 weeks are included in parity because they meet the viability threshold. Gravidity encompasses live births,
stillbirths, spontaneous abortions (miscarriages), elective abortions, and ectopic pregnancies.
Take home points
• Gravidity counts all pregnancies, including current, regardless of outcome.
• Parity counts pregnancies reaching ≥20 weeks, regardless of fetal survival.
• Multiple gestations count as one event for both gravidity and parity.
• Stillbirths ≥20 weeks are included in parity but do not alter gravidity beyond the pregnancy count.
Which of the following pregnancies are included in the gravidity count? Select all that apply.
Explanation
Gravidity refers to the total numberof times a woman has been pregnant, regardless of the pregnancy outcome or gestational age. This includes ectopic, molar, and current pregnancies. It also includes spontaneous abortionsand elective abortions. Gravidity does not change based on the viability or number of fetuses. A woman who has been pregnant 3 times, including one miscarriage and one current pregnancy, is gravida 3. Gravidity is different from parity, which considers pregnancies reaching ≥20 weeks gestation.
Rationale for correct answers
1.This is a completed pregnancy at 38 weeks, which qualifies as a pregnancy regardless of the outcome. It counts in gravidity because gravidity includes all pregnancies.
2.A miscarriage at 12 weeks is considered a pregnancy. Gravidity includes pregnancies that end before viability, including first-trimester losses.
3.An ectopic pregnancy at 8 weeks qualifies as a pregnancy and thus is counted in gravidity, regardless of implantation site or gestational age.
4.A preterm birth at 35 weeks is a pregnancy that progressed past conception. Gravidity includes pregnancies that end preterm or term.
Rationale for incorrect answers
5.A non-pregnant state is not a pregnancy and therefore does not count in gravidity. Gravidity only includes confirmed pregnancies, not periods between pregnancies or nulligravid states.
Take home points
• Gravidity includes all pregnancies regardless of duration, number of fetuses, or outcome.
• Parity only counts pregnancies ≥20 weeks gestation, not early miscarriages or ectopics.
• Miscarriages, ectopic pregnancies, and elective abortions are included in gravidity.
• A non-pregnant state is not included in gravidity or parity calculations.
Which of the following are reasons why early ultrasound (6-12 weeks) is considered more accurate for gestational age dating than later ultrasounds? Select all that apply.
Explanation
Early ultrasoundperformed between 6–12 weeksis the most accurate methodfor determining gestational age. During this period, embryonic developmentfollows a highly predictable pattern, with minimal biological variation. The crown-rump length (CRL)is the most reliable biometric parameter and correlates strongly with gestational age, with a margin of error of ±3–5 days. Beyond 14 weeks, fetal growthis influenced by geneticand environmental factors, reducing precision. Normal fetal heart rate at this stage ranges from 110–160 beats per minute, and CRL grows approximately 1 mm/day.
Rationale for correct answers
1.Fetal growth during 6–12 weeks is highly linear and consistent across pregnancies, making it ideal for gestational age estimation.
2.At this stage, individual genetic and environmental factors have not significantly influenced fetal size, so variability is minimal.
3.The crown-rump length (CRL) is measurable only in early pregnancy and is the most precise indicator of gestational age in the first trimester.
Rationale for incorrect answers
4.While early ultrasound may detect some markers for chromosomal abnormalities (e.g., nuchal translucency), this is not its purpose in gestational dating and does not enhance dating accuracy.
5.Although the fetus is larger in later weeks, biological variability increases, making measurements less reliable for accurate dating.
Take home points
• Gestational dating is most accurate when done between 6–12 weeks using CRL.
• Early fetal growth is linear, with low variability, enhancing dating accuracy.
• Later ultrasounds are less reliable due to individual fetal growth differences.
• Chromosomal screening and gestational dating are distinct purposes of ultrasound.
Which of the following conditions may be indicated by a fundal height larger than expected for gestational age? Select all that apply.
Explanation
Fundal height assessmentFundal height is a clinical measurement used to estimate fetal growth, gestational age, and uterine size. It is measured in centimeters from the pubic symphysisto the top of the uterine fundus. After 20 weeks gestation, fundal height typically correlates with gestational age in weeks (±2 cm). A larger-than-expected fundal heightmay indicate conditions such as macrosomia, polyhydramnios, or multiple gestations, which increase uterine volume. Amniotic fluid volumenormally ranges from 500 to 1000 mLat term. IUGRand oligohydramniosare associated with smaller fundal height due to reduced fetal or fluid volume.
Rationale for correct answers
1.Macrosomia refers to excessive fetal growth, typically >4000 g. It increases uterine size, leading to a larger fundal height than expected.
2.Polyhydramnios is defined as excessive amniotic fluid volume (>2000 mL). It distends the uterus, resulting in increased fundal height.
4.Multiple gestations (e.g., twins, triplets) increase uterine volume due to the presence of more than one fetus, leading to a larger fundal height.
Rationale for incorrect answers
3.Intrauterine growth restriction (IUGR) results in a fetus that is smaller than expected for gestational age. It typically presents with a fundal height smaller than expected due to reduced fetal size.
5.Oligohydramnios is characterized by reduced amniotic fluid volume (<500 mL). This condition leads to decreased uterine distension and a smaller fundal height.
Take home points
• Fundal height > gestational age suggests macrosomia, polyhydramnios, or multiple gestations.
• Fundal height < gestational age suggests IUGR or oligohydramnios.
• Normal fundal height after 20 weeks ≈ gestational age in cm (±2 cm).
• Amniotic fluid abnormalities significantly affect uterine size and fundal height.
Exams on Pregnancy Signs
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
• Comprehensively elucidate the clinical distinctions between presumptive, probable, and positive signs of pregnancy, emphasizing their physiological bases and diagnostic reliability.
• Delineate the concepts of gravidity, parity, and the GTPAL system, ensuring accurate application in obstetric history documentation.
• Explain the methodology and clinical significance of fundal height measurement as a tool for assessing fetal growth and gestational age.
• Integrate practical nursing insights to enhance clinical competency in maternal-newborn care.
• Provide high-yield practice questions to reinforce critical concepts for nursing students.
Introduction
Maternal-newborn nursing is a specialized field requiring a robust understanding of pregnancy-related physiological changes, obstetric history documentation, and fetal growth assessment. The identification of pregnancy signs—presumptive, probable, and positive—forms the foundation for confirming pregnancy and guiding prenatal care. Gravidity and parity, encapsulated in the GTPAL system, provide a standardized framework for documenting a patient’s obstetric history, informing risk assessment and care planning. Fundal height measurement serves as a non-invasive method to monitor fetal growth, with correlations to gestational age aiding in the detection of potential complications. These notes are designed to equip nursing students with comprehensive, scientifically grounded knowledge to excel in maternal-newborn care.
Pregnancy Signs
Pregnancy signs are categorized into presumptive, probable, and positive, based on their specificity and reliability in confirming pregnancy. These classifications guide nurses in assessing patients and determining the need for further diagnostic evaluation.
1.1. Presumptive Signs
Presumptive signs are subjective symptoms reported by the patient, often attributable to physiological changes but not exclusive to pregnancy. These signs are non-diagnostic due to their potential association with other conditions.
• Amenorrhea: The cessation of menstruation is a hallmark presumptive sign, typically occurring due to elevated progesterone levels suppressing ovulation. However, amenorrhea may also result from stress, hormonal imbalances, or lactation.
• Nausea and Vomiting: Often termed "morning sickness," nausea and vomiting are driven by elevated human chorionic gonadotropin (hCG) and estrogen levels stimulating the chemoreceptor trigger zone. These symptoms typically manifest between 4-8 weeks gestation and may persist into the second trimester.

• Breast Tenderness and Enlargement: Increased estrogen, progesterone, and prolactin levels promote mammary gland development, leading to breast tenderness and enlargement. This is most pronounced in the first trimester.
• Fatigue: Elevated progesterone exerts a sedative effect on the central nervous system, coupled with increased metabolic demands, resulting in profound fatigue, especially in early pregnancy.
• Urinary Frequency: Uterine enlargement exerts pressure on the bladder, reducing its capacity and causing frequent urination, particularly in the first and third trimesters.
• Quickening: The maternal perception of fetal movements, typically felt by primigravidas at 16-20 weeks and multigravidas at 14-18 weeks, is a subjective sign influenced by fetal activity and maternal sensitivity.
• Skin Changes: Hormonal changes, particularly increased melanocyte-stimulating hormone (MSH), lead to melasma (chloasma), linea nigra, and darkening of the areolae. Striae gravidarum result from connective tissue stretching and glucocorticoid effects.
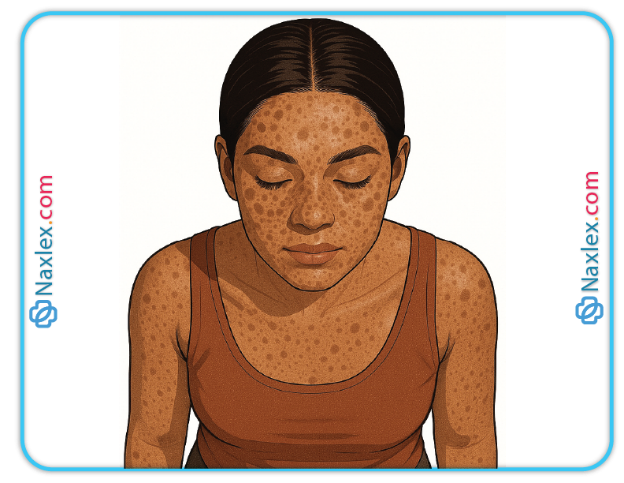
Melasma (chloasma)

Nursing Insights
• Nurses must elicit a thorough patient history to differentiate presumptive signs from symptoms of non-pregnancy conditions, such as thyroid disorders or gastrointestinal issues.
• Educate patients that presumptive signs, while common, are not diagnostic and require confirmation with objective tests.
• Assess the timing and severity of symptoms like nausea to identify potential complications, such as hyperemesis gravidarum, which may require medical intervention.
• Use culturally sensitive communication to address patient concerns about symptoms like melasma, which may impact self-esteem.
1.2. Probable Signs
Probable signs are objective findings observed by healthcare providers, often detectable through physical examination or diagnostic tests. While highly suggestive of pregnancy, they are not conclusive due to potential non-pregnancy causes.
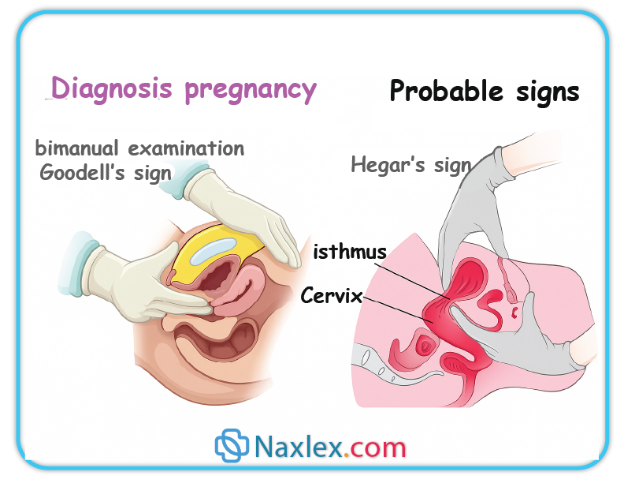
• Goodell’s Sign: Softening of the cervix, observed as early as 6-8 weeks gestation, results from increased vascularity, hyperplasia, and hypertrophy of cervical glands, driven by estrogen.
• Chadwick’s Sign: A bluish-purple discoloration of the cervix and vagina, noted around 6-8 weeks, is caused by increased vascularity and venous congestion due to elevated estrogen levels.
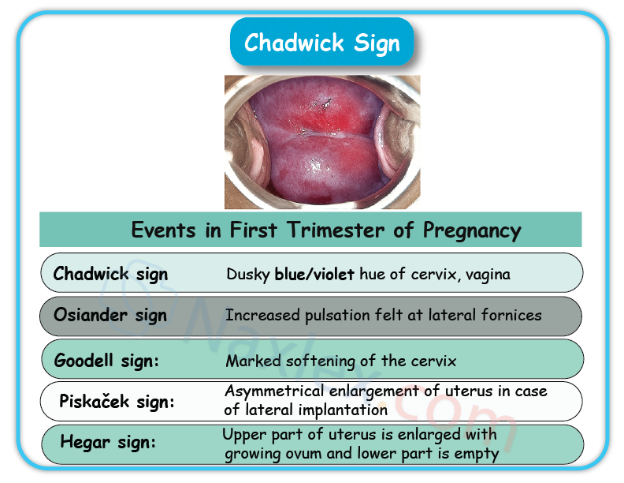
• Hegar’s Sign: Softening and compressibility of the lower uterine segment, detectable by bimanual examination at 6-12 weeks, reflect myometrial changes induced by estrogen and progesterone.
• Positive Pregnancy Test: Detection of hCG in urine or serum, typically positive by 4-5 weeks gestation, indicates placental production. False positives may occur with molar pregnancy or recent miscarriage.
• Uterine Enlargement: The uterus becomes palpable above the symphysis pubis by 12 weeks due to myometrial hypertrophy and hyperplasia, driven by estrogen and progesterone.
• Braxton Hicks Contractions: Painless, irregular uterine contractions, typically noted after 20 weeks, prepare the uterus for labor but may be mistaken for true labor.
• Ballottement: During bimanual examination, the fetus rebounds when gently pushed, reflecting its buoyancy in amniotic fluid, typically observed in the second trimester.
Nursing Insights
• Perform bimanual pelvic examinations with precision to detect Hegar’s and Goodell’s signs, ensuring patient comfort and consent.
• Recognize that positive pregnancy tests must be confirmed with clinical assessment, as false positives can occur in conditions like choriocarcinoma.
• Educate patients about Braxton Hicks contractions to differentiate them from true labor, reducing unnecessary hospital visits.
• Document probable signs accurately, noting their gestational timing, to support pregnancy confirmation and monitor progression.
1.3. Positive Signs
Positive signs provide irrefutable evidence of pregnancy, directly attributable to the presence of a fetus, and are observed by healthcare providers using diagnostic tools.
• Fetal Heart Tones: Detection of fetal heart tones via Doppler ultrasound at 10-12 weeks or fetoscope at 18-20 weeks confirms fetal viability. The normal fetal heart rate ranges from 110-160 beats per minute.
• Fetal Movements Palpated by Examiner: Palpation of distinct fetal movements by a healthcare provider, typically after 20 weeks, verifies fetal presence and activity.
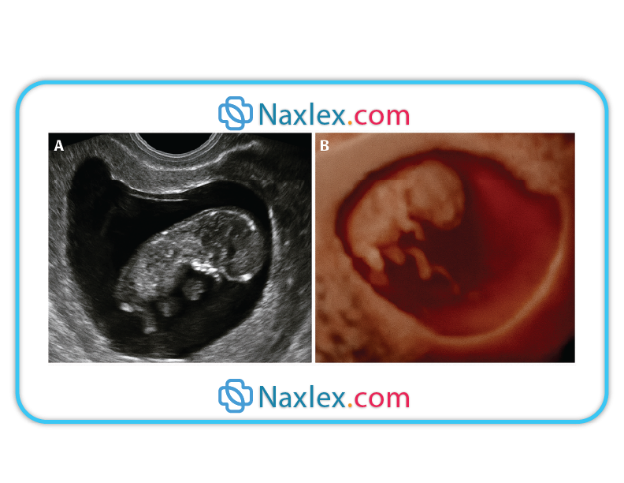
• Ultrasound Visualization of Fetus: Transvaginal ultrasound can detect a gestational sac as early as 4-5 weeks and confirm fetal cardiac activity by 6-7 weeks, providing definitive evidence of pregnancy.
Nursing Insights
• Master the use of Doppler ultrasound to detect fetal heart tones, positioning the device in the lower abdominal quadrants for optimal signal detection.
• Ensure accurate documentation of positive signs, including gestational age and fetal heart rate, to establish a baseline for ongoing prenatal care.
• Reassure patients that ultrasound visualization is a definitive confirmation, alleviating anxiety about pregnancy status.
• Be vigilant for discrepancies in expected findings, such as absent fetal heart tones, prompting immediate referral for further evaluation.
Gravidity And Parity
Gravidity and parity are critical components of obstetric history, providing a framework to assess a patient’s pregnancy outcomes and associated risks. The GTPAL system enhances this assessment by categorizing pregnancies based on specific criteria, while gestational age estimation, including Näegele’s Rule, supports accurate prenatal care planning.
1.1. Gravidity
Gravidity refers to the total number of confirmed pregnancies, regardless of outcome, including the current pregnancy, miscarriages, ectopic pregnancies, and stillbirths.
• Definition: Gravidity encompasses all pregnancies, whether they result in live births, abortions, or other outcomes. For example, a woman with two prior pregnancies and a current pregnancy is gravida 3.
• Clinical Relevance: High gravidity may indicate increased obstetric risks, such as uterine atony or placenta previa, necessitating vigilant monitoring.
• Calculation: Include all confirmed pregnancies, verified through patient history or medical records, ensuring nonjudgmental inquiry into sensitive outcomes like abortions.
Nursing Insights
• Use empathetic, nonjudgmental communication to elicit accurate pregnancy histories, as patients may underreport sensitive outcomes like abortions.
• Verify gravidity through medical records when possible to ensure accuracy in risk assessment.
• Educate patients about the importance of disclosing all pregnancies to tailor prenatal care effectively.
1.2. Parity
Parity denotes the number of pregnancies reaching at least 20 weeks gestation, regardless of whether the outcome is a live birth or stillbirth.
• Definition: A single parous event includes any pregnancy reaching 20 weeks, such as a term birth, preterm birth, or stillbirth. Multiple gestations (e.g., twins) count as one parous event.
• Clinical Implications: High parity, especially grand multiparity (≥5), increases risks for complications like postpartum hemorrhage and uterine rupture.
• Calculation: Count only pregnancies reaching the viability threshold of 20 weeks, excluding miscarriages or ectopic pregnancies before this point.
Nursing Insights
• Clarify the gestational age of prior pregnancy outcomes to accurately categorize term versus preterm births.
• Assess patients with high parity for signs of uterine fatigue during labor, as it may impact contraction strength.
• Document parity clearly in the patient’s chart to inform delivery planning and postpartum care.
1.3. GTPAL System
The GTPAL system provides a detailed snapshot of obstetric history: Gravida (total pregnancies), Term births (≥37 weeks), Preterm births (20-36 weeks), Abortions (<20 weeks), and Living children.
• Gravida (G): Total number of pregnancies, including current pregnancy, regardless of outcome.
• Term Births (T): Pregnancies delivered at or after 37 weeks gestation.
• Preterm Births (P): Pregnancies delivered between 20 weeks 0 days and 36 weeks 6 days gestation.
• Abortions (A): Spontaneous or induced pregnancy losses before 20 weeks gestation, including ectopic pregnancies and miscarriages.
• Living Children (L): Number of currently living children, updated dynamically if a child dies.
• Example: A patient with three pregnancies (one term birth, one preterm birth, one miscarriage, two living children) is documented as G3 T1 P1 A1 L2.
Nursing Insights
• Meticulously gather gestational age details for each pregnancy to ensure accurate GTPAL documentation.
• Recognize that a high “A” value may indicate recurrent pregnancy loss, prompting referral for genetic or endocrine evaluation.
• Update the “L” component if informed of a child’s death, as it impacts the patient’s obstetric profile.
• Use the GTPAL system consistently in electronic health records to facilitate interdisciplinary communication.
1.4. Gestational Age and Näegele’s Rule
Gestational age estimation is critical for monitoring fetal development and timing prenatal interventions. Näegele’s Rule provides a standardized method to calculate the estimated due date (EDD).
• Gestational Age: Measured from the first day of the last menstrual period (LMP), assuming a 28-day cycle with ovulation on day 14. It differs from fetal age, which begins at conception.
• Näegele’s Rule: To calculate the EDD, add 7 days to the first day of the LMP, subtract 3 months, and add 1 year. For example, an LMP of March 15, 2025, yields an EDD of December 22, 2025.
• Limitations: Näegele’s Rule assumes regular 28-day cycles, making it unreliable in cases of irregular menstruation or recent hormonal contraceptive use.
• Ultrasound Confirmation: First-trimester ultrasound, particularly crown-rump length (CRL) measurement, is the gold standard for gestational age estimation, with an accuracy of ±5-7 days.
• Clinical Application: Accurate gestational age informs the timing of prenatal screening tests, such as nuchal translucency, and delivery planning.
Nursing Insights
• Educate patients that the EDD is an estimate and may be refined by ultrasound, especially if LMP is uncertain.
• Prioritize early ultrasound dating (6-12 weeks) for patients with irregular cycles or unclear LMP.
• Document gestational age discrepancies between LMP and ultrasound, using the latter if performed in the first trimester.
• Assess for factors like breastfeeding or recent contraception use that may affect LMP reliability.
Fundal Height
Fundal height measurement is a non-invasive technique to assess fetal growth and estimate gestational age, serving as a critical tool in prenatal care.
1.1. Measurement Techniques
Fundal height is measured in centimeters from the pubic symphysis to the top of the uterine fundus, correlating with gestational age in the second and third trimesters.
• Procedure: Position the patient supine with an empty bladder to relax abdominal muscles. Use a non-elastic measuring tape, placing the zero mark at the pubic symphysis and extending to the fundus.

- Accuracy Factors: Ensure consistent technique, as maternal obesity, full bladder, or fetal position (e.g., transverse lie) can affect measurements.
• Documentation: Record the measurement in centimeters alongside the gestational age to track trends over time.
• Best Practices: Obtain verbal consent, explain the procedure to the patient, and perform measurements at each prenatal visit after 20 weeks.
Nursing Insights
• Ensure the patient empties her bladder before measurement to avoid falsely elevated readings.
• Use a non-elastic tape to maintain accuracy, calibrating the measurement in centimeters.
• Document findings meticulously, noting any discrepancies that may warrant ultrasound evaluation.
• Educate patients about the purpose of fundal height measurement to alleviate anxiety about fetal growth.
1.2. Correlations with Fetal Age
Fundal height typically correlates with gestational age in centimeters from 20-36 weeks, with a measurement of 28 cm at 28 weeks indicating normal growth.
• Expected Measurements: At 20 weeks, the fundus is at the umbilicus (approximately 20 cm); at 36 weeks, it reaches 33-36 cm, near the xiphoid process.
• Deviations: A fundal height significantly larger than expected may indicate macrosomia, polyhydramnios, or multiple gestations, while a smaller measurement may suggest intrauterine growth restriction (IUGR) or oligohydramnios.
• Ultrasound Confirmation: Discrepancies of ±2-3 cm from expected gestational age warrant ultrasound to evaluate fetal growth and amniotic fluid volume.
• Limitations: Maternal factors (e.g., obesity) and fetal factors (e.g., position) can reduce measurement accuracy, necessitating serial measurements and ultrasound correlation.
Nursing Insights
• Monitor serial fundal height measurements to detect trends, such as slow growth, which may indicate IUGR.
• Recommend ultrasound promptly for significant deviations to assess fetal well-being and guide interventions.
• Educate patients that fundal height is a screening tool, not a definitive diagnostic measure, requiring confirmation for abnormalities.
• Assess maternal factors like BMI or uterine fibroids that may skew measurements, adjusting clinical interpretation accordingly.
Summary
The study of maternal-newborn nursing encompasses critical concepts for assessing pregnancy and fetal development. Pregnancy signs are categorized into presumptive (subjective symptoms like amenorrhea and nausea), probable (objective findings like Goodell’s and Chadwick’s signs), and positive (definitive evidence like fetal heart tones and ultrasound visualization). Gravidity and parity, detailed through the GTPAL system, provide a structured approach to documenting obstetric history, with gravidity counting all pregnancies and parity focusing on those reaching viability. Näegele’s Rule and ultrasound refine gestational age estimation, critical for timing prenatal interventions. Fundal height measurement serves as a practical tool to monitor fetal growth, with deviations prompting further evaluation for conditions like IUGR or polyhydramnios. Nursing insights emphasize accurate assessment, patient education, and culturally sensitive care to optimize maternal and fetal outcomes.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Pregnancy Signs
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


