Please set your exam date
The Nurse-Client Relationship and Therapeutic Communication Process
Study Questions
Practice Exercise
Which of the following is the most effective nursing intervention to establish trust in the initial phase of the nurse-client relationship?
Explanation
Therapeutic nurse–client relationship involves purposeful, goal-directed interactions that foster trust, respect, and collaboration. Trust is established through consistency, honesty, and reliability. Early rapport depends on predictable boundaries, active listening, and meeting agreed expectations. Trust deficits delay disclosure and hinder recovery, especially in psychiatric and trauma-informed care.
Rationale for correct answers
B. Consistent follow-through shows reliability, reinforcing the client’s sense of safety and predictability. This strengthens the therapeutic bond during the orientation phase, encouraging disclosure and engagement.
Rationale for incorrect answers
A. Over-sharing personal details shifts focus away from the client and may blur boundaries, risking role confusion and loss of professional trust.
C. Avoiding discussion of client concerns communicates disinterest, delaying rapport and potentially worsening anxiety or mistrust.
D. Instructing trust without earning it undermines autonomy, triggering resistance and reducing the likelihood of open communication.
Take Home Points
- Trust in therapeutic relationships is built through consistent actions and clear professional boundaries.
- Early communication should focus on client needs, not the nurse’s personal experiences.
- Avoidance or demands for trust can harm rapport development.
- Reliability and follow-through are foundational to effective nurse–client interactions.
Which actions by the nurse demonstrate self-awareness in the nurse-client relationship? Select all that apply.
Explanation
Self-awareness in nursing is the conscious understanding of one’s own beliefs, values, emotions, and behaviors and how these influence professional interactions. It promotes therapeutic communication, prevents bias, and enhances individualized care. This process involves reflection, feedback, and recognition of internal triggers.
Rationale for correct answers
A. Awareness of personal values helps the nurse avoid imposing them on clients, ensuring culturally sensitive and patient-centered care.
C. Seeking feedback allows recognition of blind spots in interpersonal skills, enhancing relationship-building and professional growth.
D. Recognizing emotions toward client behaviors prevents countertransference and maintains therapeutic boundaries during challenging interactions.
Rationale for incorrect answers
B. Avoiding reflection hinders self-understanding, allowing unconscious bias to influence care delivery.
E. Using the same approach for all clients ignores individuality and can result in culturally insensitive or ineffective care plans.
Take Home Points
- Self-awareness is a foundational skill for building therapeutic relationships and avoiding bias in care.
- Reflection and feedback are essential for recognizing and managing personal influences on professional practice.
- Emotional self-recognition helps prevent countertransference and preserve boundaries.
- Individualized approaches promote culturally competent and patient-centered care.
In Peplau’s working phase, which nurse action best supports client self-management?
Explanation
Working phase in Peplau’s therapeutic relationship model focuses on active problem-solving and skill-building to promote independence. The nurse facilitates behavior change, helps the client apply coping mechanisms, and supports achievement of treatment goals while maintaining professional boundaries.
Rationale for correct answers
B. Exploring coping strategies during the working phase empowers the client to develop adaptive responses, enhancing self-management and reducing relapse risk.
Rationale for incorrect answers
A. Setting the relationship time frame is part of the orientation phase, which establishes structure before active problem-solving begins.
C. Discharge planning is addressed later in the termination phase, when the focus shifts to transitioning care and summarizing progress.
D. Avoiding difficult topics limits therapeutic progress by preventing the exploration and resolution of issues critical to recovery.
Take Home Points
- The working phase is centered on active problem-solving, coping skill enhancement, and goal achievement.
- Each therapeutic phase has distinct objectives and nurse-client interactions.
- Avoidance behaviors by the nurse hinder client growth and autonomy.
- Effective coping strategies foster resilience and improve long-term outcomes in mental health care.
Practice Exercise 2
A nurse is caring for a client from a culture where avoiding eye contact shows respect. The nurse should:
Explanation
Cultural competence in nursing involves adapting care to meet the client’s beliefs and communication patterns without imposing personal norms. Recognizing cultural variation in nonverbal behaviors helps preserve trust and therapeutic rapport.
Rationale for correct answers
C. Respecting culturally based practices while using other engagement methods maintains rapport and ensures culturally sensitive communication without causing discomfort.
Rationale for incorrect answers
A. Forcing direct eye contact disregards cultural norms, potentially causing distress and reducing client openness.
B. Assuming shame from eye contact avoidance is an incorrect interpretation that risks stereotyping and misjudging the client’s feelings.
D. Avoiding interaction until eye contact occurs delays care and damages therapeutic relationship-building.
Take Home Points
- Nonverbal communication patterns vary widely between cultures and must be respected in care delivery.
- Cultural competence requires avoiding ethnocentric interpretations of client behaviors.
- Alternative engagement methods should be used when standard cues differ culturally.
- Respecting communication norms fosters trust, safety, and effective nurse-client relationships.
Which of the following are examples of clear family boundaries? Select all that apply.
Explanation
Family boundaries are the rules and limits that define roles, responsibilities, and relationships among members, promoting autonomy while preserving connection. Healthy boundaries support emotional safety, respect privacy, and allow adaptability in relationships.
Rationale for correct answers
A. Distinct roles prevent role confusion and foster stable functioning within the family system.
B. Respecting reasonable privacy promotes trust and healthy adolescent development while maintaining parental guidance.
E. Allowing individual opinions within unity fosters open communication and mutual respect in relationships.
Rationale for incorrect answers
C. Sharing identical emotions erases individuality and reflects enmeshment rather than healthy boundaries.
D. Absolute rigidity limits adaptability and can harm family resilience during stress or change.
Take Home Points
- Healthy family boundaries balance individuality and connectedness.
- Boundaries must allow role clarity and privacy without isolation.
- Flexibility supports family coping in changing circumstances.
- Enmeshment or rigidity are signs of dysfunctional boundaries.
A nurse wants to provide culturally competent care for a client with strong spiritual beliefs. The most important first step is to:
Explanation
Culturally competent care involves tailoring healthcare to align with a patient’s cultural identity, beliefs, and values, ensuring respectful and effective interactions. It encompasses understanding ethnicity, religion, spirituality, and social norms to address needs holistically. Effective communication, respect for preferences, and addressing spiritual needs enhance patient trust, satisfaction, and outcomes, particularly when navigating diverse belief systems.
Rationale for correct answers
B. Understanding a patient’s cultural and spiritual preferences is critical for delivering personalized care that respects their beliefs, fostering trust and improving outcomes by aligning interventions with their values.
Rationale for incorrect answers
A. Replacing coping strategies disregards the patient’s existing beliefs, undermining trust and cultural sensitivity, which are essential for effective, patient-centered care.
C. Avoiding religion discussion risks missing key aspects of the patient’s identity, potentially leading to misaligned care and reduced therapeutic rapport.
D. Referring to a spiritual leader without assessing individual needs skips understanding the patient’s specific beliefs, which is foundational for culturally competent care.
Take Home Points
- Culturally competent care prioritizes understanding and respecting patients’ cultural and spiritual beliefs to enhance trust and outcomes.
- Spiritual assessments identify beliefs that influence coping and healthcare decisions, ensuring personalized care.
- Effective communication and respect for preferences are key to addressing diverse cultural and spiritual needs.
- Avoid imposing interventions or bypassing assessments, as this disregards patient autonomy and cultural identity.
Practice Exercise 3
Which communication technique involves restating the client’s main ideas in the nurse’s own words to ensure understanding?
Explanation
Paraphrasing is a communication technique where the nurse restates a client’s message in their own words to confirm understanding. It promotes active listening, clarifies meaning, and builds trust by showing the client their thoughts are valued. This technique ensures accurate interpretation of the client’s emotional needs and concerns, fostering effective therapeutic communication, especially in addressing psychological or physiological needs.
Rationale for correct answers
B. Restating the client’s ideas in the nurse’s own words ensures clear understanding, aligns with the question’s focus on verifying comprehension, and supports therapeutic communication.
Rationale for incorrect answers
A. Reflecting mirrors the client’s emotions or feelings, not necessarily restating main ideas, and focuses on emotional content rather than ensuring understanding.
C. Validating confirms the accuracy of information or feelings without necessarily rephrasing the client’s main thoughts, differing from the technique described.
D. Summarizing condenses key points over a conversation, not specifically restating a single idea to ensure understanding, as paraphrasing does.
Take Home Points
- Paraphrasing restates a client’s message in the nurse’s words to confirm understanding and promote effective communication.
- Reflecting focuses on mirroring emotions, not restating ideas, and is distinct from paraphrasing.
- Validating confirms accuracy but does not involve rephrasing the client’s main thoughts.
- Summarizing condenses multiple points, unlike paraphrasing, which targets specific ideas for clarity.
Which of the following are considered nontherapeutic communication techniques? Select all that apply.
Explanation
Nontherapeutic communication hinders effective interaction by dismissing or misdirecting a client’s emotional needs. It includes techniques that block open dialogue, such as minimizing feelings, probing inappropriately, or giving unsolicited advice. These actions disrupt trust building, impede emotional expression, and fail to address psychological needs, potentially escalating distress or disengagement in therapeutic settings.
Rationale for correct answers
A. Changing the subject during emotional disclosure interrupts the client’s expression, blocking therapeutic dialogue and dismissing their emotional needs.
C. Asking “Why” can feel judgmental, pressuring the client and hindering open emotional exploration in therapeutic communication.
D. Minimizing distress invalidates the client’s feelings, reducing trust and impeding emotional processing critical for therapeutic support.
E. Giving advice without exploring options disregards the client’s autonomy, limiting their ability to address personal concerns collaboratively.
Rationale for incorrect answers
B. Sitting quietly with the client demonstrates presence, fostering trust and supporting emotional expression, which is a therapeutic technique.
Take Home Points
- Nontherapeutic communication, like minimizing feelings or changing topics, disrupts trust and emotional expression in client interactions.
- Asking “Why” can feel judgmental, hindering open dialogue and emotional exploration in therapeutic settings.
- Offering unsolicited advice dismisses client autonomy, unlike collaborative exploration, which supports psychological needs.
- Therapeutic techniques, like being present, encourage trust and differentiate from nontherapeutic actions that block communication.
During a difficult conversation, the client becomes silent for a prolonged period. The nurse should:
Explanation
Therapeutic silence allows clients to process emotions and thoughts, fostering reflection and emotional expression. It respects individual pacing, supports psychological needs, and builds trust in therapeutic communication. Silence can be powerful in addressing emotional distress, enabling clients to articulate concerns at their own pace without pressure.
Rationale for correct answers
C. Sitting quietly allows the client to process thoughts, supporting emotional reflection and aligning with therapeutic communication principles during difficult conversations.
Rationale for incorrect answers
A. Filling silence quickly disrupts the client’s reflective process, potentially increasing discomfort and hindering emotional expression.
B. Changing the subject dismisses the client’s emotional needs, preventing processing of difficult topics and breaking therapeutic rapport.
D. Asking multiple closed-ended questions pressures the client, limiting open dialogue and failing to respect their need for reflective silence.
Take Home Points
- Therapeutic silence supports emotional processing and reflection, fostering trust in difficult conversations.
- Filling silence or changing topics disrupts the client’s ability to process emotions, hindering therapeutic communication.
- Closed-ended questions can pressure clients, unlike open-ended approaches that encourage voluntary expression.
- Respecting silence differentiates therapeutic communication from nontherapeutic actions that dismiss emotional needs.
Comprehensive Questions
A nursing assistant (NA) comments to the nurse about a recently admitted client. “I think the new admit is just faking being sick. Yesterday we couldn’t get a word out of the client and today the client is talking nonstop.” Which response by the nurse is most appropriate in reflecting empathy for the client?
Explanation
Rapid-cycle bipolar disorder involves lability and swift mood shifts, with clients oscillating between quiet and manic speech rapidly. It often manifests as hyperverbal periods alternating with mutism. Understanding this helps nurses display empathetic and supportive communication.
Rationale for correct answers
C. The explanation that the client has rapid-cycle bipolar disorder directly acknowledges the medical condition causing mood swings, offering an empathetic, educational response rooted in clinical understanding.
Rationale for incorrect answers
A. This response labels the client as attention-seeking, which dismisses their legitimate mood fluctuations, lacks empathy and does not support a therapeutic environment.
B. Although encouraging using the client’s name aids respect, it does not address the underlying mood dynamics or teach about the illness itself.
D. While client autonomy is important, stating the client “has the right to be difficult” normalizes problematic behavior without offering clarity or empathy toward the mental health condition.
Take Home Points
- Rapid-cycle bipolar disorder presents with frequent, extreme mood shifts including silence and hyperverbal states.
- Empathetic nursing communication validates clinical understanding while educating staff and supporting client dignity.
- Disease-focused language helps reframe staff perceptions from personal judgment to medical insight.
- Educating caregivers fosters more consistent, therapeutic attitudes and aligns with Maslow's respect needs.
A nurse includes the nursing diagnosis of Disturbed thought processes secondary to paranoia in the care plan for a newly admitted client diagnosed with schizophrenia. Which approach is most appropriate for this client?
Explanation
Disturbed thought processes in schizophrenia commonly involve paranoia, leading to mistrust and misinterpretation of neutral actions. Clients may believe others are mocking or plotting against them, requiring calm, respectful, and clear therapeutic communication.
Rationale for correct answers
A. Avoiding laughing or whispering demonstrates respectful communication, reducing perceived threats and building trust by addressing paranoia and distorted perception inherent in thought disturbances.
Rationale for incorrect answers
B. Identifying social supports is premature; until trust and accurate perception stabilize, focusing on community connections does not alleviate paranoia-driven thought disorder.
C. Encouraging social interaction may worsen paranoia; engaging peers without first establishing trust and reality orientation can intensify distress or withdrawal.
D. Requiring a release of information form does not address immediate thought disturbances; it overlooks therapeutic needs and may exacerbate mistrust during acute paranoid episodes.
Take Home Points
- Avoid behaviors perceived as secretive (laughing, whispering) to reduce paranoia and foster trust.
- Therapeutic communication should be clear, respectful, and non-threatening in disturbed thought issues.
- Interventions must first address reality orientation and safety before advancing social or community support.
- Building trust lays the foundation for later psychosocial goals (socialization, information sharing).
A client who is experiencing paranoid delusions asks a nurse to turn off the television stating, “It controls my thoughts.” Which is the most appropriate intervention by the nurse?
Explanation
This psychotic symptom involves false beliefs that others intend to harm, deceive, or control the individual. It commonly occurs in schizophrenia and severe mood disorders. Patients often misinterpret neutral stimuli as threatening, such as thinking media devices are invasive. The nurse’s response should maintain reality orientation without reinforcing false beliefs. While empathy is essential, delusions must not be validated. Managing the environment must strike a balance between therapeutic support and reality-based limits.
Rationale for correct answers
D. Delusional reinforcement must be avoided to maintain reality testing. Turning off the TV implies agreement with the delusion, which impedes recovery and distorts perception. Refusal supports clear boundaries and therapeutic integrity.
Rationale for incorrect answers
A. Showing control over the client risks escalating paranoia and aggression. This approach lacks therapeutic communication and violates the client's dignity, potentially increasing resistance or noncompliance.
B. Complying solely to reduce fear may temporarily reduce anxiety but inadvertently validates the delusion. It reinforces the client’s belief that external control is real, worsening psychosis.
C. Although showing understanding appears therapeutic, acting on the delusion by turning off the TV affirms the distorted belief. This approach blurs reality testing and undermines cognitive restructuring.
Take Home Points
- Never validate or act on a client’s delusions, even when attempting to reduce distress.
- Paranoid delusions require clear, consistent reality orientation from healthcare providers.
- Therapeutic communication includes empathy, but must not support false beliefs or perceptions.
- Differentiating between showing empathy and reinforcing delusions is critical in managing psychotic disorders.
A nurse observes a client with a history of violent command hallucinations mumbling erratically while making threatening gestures directed toward a particular staff member. Which nursing intervention is most appropriate when working with a client with violent command hallucinations?
Explanation
These are auditory hallucinations instructing individuals to act, often with violent or harmful content. They may be ego-dystonic or ego-syntonic depending on the individual's insight. Clients with a history of violence due to hallucinations need vigilant clinical assessment, but engagement is crucial. Exploring the underlying emotion allows the nurse to assess the client's intent, determine risk, and apply the most appropriate safety interventions without escalating the situation prematurely.
Rationale for correct answers
A. Verbal engagement allows early assessment of internal triggers and possible acting-out risks. Asking about anger reveals if the hallucinations involve threats and provides insight into the client’s reality testing and impulse control. This creates an opportunity for therapeutic de-escalation and safety planning.
Rationale for incorrect answers
B. Immediate seclusion without assessing intent violates least-restrictive protocols. It may increase paranoia or trauma responses, especially if the client is hallucinating or misinterpreting the environment.
C. Warning about restraints can intensify fear, especially if the client feels controlled by hallucinations. This can trigger aggression and reduce the client’s trust in the treatment team.
D. Passive observation delays intervention. In cases with a known history of violence, early therapeutic dialogue is more proactive than waiting for worsening behaviors.
Take Home Points
- Command hallucinations may lead to violence; assessing client perception and intent is the first step in risk management.
- Therapeutic dialogue helps assess danger, build trust, and reduce the need for restrictive interventions.
- Seclusion and restraint should only follow failed de-escalation and when there’s imminent risk to safety.
- Passive observation is insufficient in clients with a documented history of acting on violent hallucinations.
A charge nurse overhears a new nurse talking with a client who is dying. The client states to the nurse, “Today is the day that I know I am going to die.” Which statements made by the new nurse indicate that the new nurse is uncomfortable caring for dying clients? Select all that apply
Explanation
End-of-life communication requires active listening and emotional presence to address psychological, spiritual, and existential distress. Clients facing imminent death often express anticipatory awareness or fears, which should be acknowledged without dismissal, redirection, or avoidance. Poor communication reflects nurse discomfort, often shown through minimizing, false reassurance, or bypassing the client’s emotional process. Verbal cues should support patient-centered dialogue rather than silence or deny reality.
Rationale for correct answers
A. Avoidance behavior is evident in this statement, redirecting the conversation rather than validating the client’s reality. It shows emotional discomfort and an inability to remain present with the client's experience.
C. Minimizing statements invalidate the client’s subjective feelings. Suggesting things “aren’t that bad” implies judgment and denies the client’s perceived condition, showing avoidance of confronting death.
D. Overgeneralization avoids personal engagement. It distances the nurse emotionally and prevents therapeutic exploration. This reflects a defensive mechanism to bypass the nurse’s own fear of death.
E. Premature action without client request demonstrates an external attempt to manage the situation. It implies panic or uncertainty, not therapeutic presence. Comfort measures must first involve emotional processing with the client.
Rationale for incorrect answers
B. This response is reflective and invites the client to elaborate on their thoughts. It uses therapeutic communication by acknowledging the client’s statement, showing interest, and allowing for emotional exploration without avoidance.
Take Home Points
- End-of-life communication must validate client concerns without redirecting or minimizing their emotions.
- Nurse discomfort often manifests as generalization, false reassurance, or premature action without patient direction.
- Reflective listening helps clients explore their own meaning and emotions around death.
- Comfort in caring for dying patients is demonstrated through presence, not distraction or avoidance.
A nurse is interacting with a client who abuses methamphetamine. The client appears not to be willing to give up the drug use, evidenced by statements such as, “I don’t plan to quit meth. I can work for days when I’m high.” Which is the best response by the nurse to the client’s statement?
Explanation
Clients with methamphetamine addiction often show resistance and minimization of harm. Effective therapeutic communication uses open-ended questions to explore beliefs, rather than confronting or judging. Motivational interviewing is a person-centered approach to evoke the client’s own motivation for change.
Rationale for correct answers
C. Open-ended engagement facilitates client reflection and insight. This neutral question encourages the client to explore their reasoning without feeling judged or dismissed.
Rationale for incorrect answers
A. This response is confrontational and implies judgment. It discourages open dialogue and can cause defensiveness, blocking therapeutic rapport.
B. Labeling the client as being in denial is accusatory. It lacks empathy and creates resistance by confronting instead of inviting self-exploration.
D. This reinforces the client’s distorted belief. Agreeing with a harmful behavior validates drug use and misses the opportunity to explore motivation for change.
Take Home Points
- Motivational interviewing uses open-ended, nonjudgmental questions to promote client insight and motivation for change.
- Direct confrontation increases resistance and decreases client willingness to engage in treatment.
- Methamphetamine users may idealize the drug’s effects; neutral exploration helps shift perspective.
- Reflective listening and avoiding argumentation are essential in substance use interventions.
A nurse is assessing a client diagnosed with paranoid personality disorder. The nurse understands that the client most likely:
Explanation
Paranoid personality disorder involves a pattern of distrust and suspicion toward others without sufficient basis. It often develops from early emotional rejection, humiliation, or harsh criticism in childhood, leading to defensive and guarded interpersonal behaviors.
Rationale for correct answers
A. Early rejection and lack of affection contribute to long-standing mistrust. Emotional neglect or criticism fosters defensive thinking, which is central to paranoid personality features.
Rationale for incorrect answers
B. Lack of empathy and nurturing is more associated with narcissistic or antisocial traits, where entitlement or exploitation may develop instead of suspicion.
C. Discomfort with affection due to indifference aligns more with schizoid personality disorder, which involves detachment, not paranoia.
D. Recognition in early life followed by its absence in adolescence does not reflect the developmental pattern seen in paranoid personality disorder. It lacks connection to the pervasive distrust seen in this condition.
Take Home Points
- Paranoid personality disorder stems from early emotional rejection and mistrust, not merely lack of empathy.
- Clients display pervasive suspicion and may misinterpret benign interactions as threats.
- Developmental roots often involve criticism, humiliation, or lack of consistent emotional support.
- It is distinct from schizoid and narcissistic traits which reflect different interpersonal challenges.
A nurse is discussing discharge plans with a homeless client diagnosed with paranoid schizophrenia. What is the primary factor that will affect the formulation of the discharge plan for this client?
Explanation
This is a chronic psychotic disorder marked by delusions, disorganized thinking, and impaired reality testing. Clients often exhibit mistrust, suspicion, and social withdrawal, which complicates therapeutic communication and discharge planning. Building a rapport is especially difficult when homelessness and cognitive impairment coexist. The nurse’s ability to develop trust, structure, and safety in planning directly impacts adherence, engagement, and success in transitioning the client to stable outpatient care.
Rationale for correct answers
B. Therapeutic alliance is foundational for effective discharge in paranoid schizophrenia. Clients with persecutory delusions often resist care and reject interventions. The nurse’s ability to establish a working relationship determines how well the client accepts planning, engages in services, and complies with post-discharge instructions.
Rationale for incorrect answers
A. While helpful, social support systems are often absent or fragmented in homeless populations. Discharge can still be structured effectively through professional collaboration even when family support is lacking.
C. Compliance depends heavily on external supports and cognitive engagement. Without trust and nurse-client rapport, the client may not understand or agree to the plan regardless of ability.
D. Community resources are important but secondary. If the client rejects referrals due to mistrust or lack of engagement, resources alone do not ensure follow-through or safety.
Take Home Points
- Establishing trust with clients who have paranoid schizophrenia is the most important factor in effective discharge planning.
- Homeless clients often lack stable support, so nurse-client communication must be grounded in consistency and non-threatening interaction.
- Community resources are valuable but insufficient if the client lacks therapeutic engagement or insight into their needs.
- Delusional thinking may interfere with planning unless the nurse carefully navigates interactions to build acceptance of care.
A client is being discharged after hospitalization for a suicide attempt. Which question asked by the nurse assesses the learned prevention and future coping strategies of the client?
Explanation
Post-suicide attempt care focuses on evaluating the client’s protective factors and readiness to manage future stress. Identifying coping strategies and strengthening them reduces recurrence risk. Asking about actionable skills ensures the client has tools to face emotional crises safely.
Rationale for correct answers
C. Future planning and skills assessment help evaluate readiness for discharge. It encourages the client to identify effective coping tools, promoting self-efficacy and relapse prevention.
Rationale for incorrect answers
A. Asking about the method is part of risk assessment but does not evaluate prevention learning or future strategy.
B. Asking about a phone number checks resource access, not the client’s internal coping ability or skill development.
D. This question focuses on past emotions, not on learned strategies. It may evoke guilt or discomfort rather than build future focus.
Take Home Points
- Post-crisis care must assess coping skills and protective strategies to prevent repeat suicide attempts.
- Asking about future strategies ensures discharge readiness and enhances self-management.
- Risk-focused questions are vital earlier in care, but coping assessment is key at discharge.
- Effective prevention involves both external support and internal coping mechanisms.
A nurse is discussing treatment plan with a client diagnosed with paranoid schizophrenia. Which nurse-client communication-centered skill implies “genuineness”?
Explanation
Genuineness is a core component of therapeutic communication, marked by the nurse being real, authentic, and emotionally present in the interaction. It involves self-congruence, where the nurse’s verbal and nonverbal expressions align, fostering trust and openness with the client.
Rationale for correct answers
C. Authentic presence and self-congruence define genuineness. When the nurse is emotionally transparent and consistent, the client feels safe and respected, enabling a more open therapeutic relationship.
Rationale for incorrect answers
A. This describes unconditional positive regard, which emphasizes valuing the client without judgment, not the nurse’s authenticity.
B. This is empathy, focusing on understanding the client’s inner world and communicating that understanding with emotional sensitivity.
D. This reflects concreteness, which is the use of clear, specific language rather than vague or abstract terms, aiding comprehension but not reflecting genuineness.
Take Home Points
- Genuineness is demonstrated when the nurse is authentic, consistent, and emotionally honest with the client.
- It differs from empathy, which focuses on understanding the client's emotional experience from their perspective.
- Unconditional positive regard involves nonjudgmental acceptance, not necessarily the nurse’s personal transparency.
- Concreteness supports clarity in communication but does not imply emotional authenticity or self-congruence.
A nurse is interviewing a client who’s currently under the influence of a controlled substance and shows signs of becoming agitated. What should the nurse do?
Explanation
Agitation during substance intoxication is often triggered by altered sensorium, heightened threat perception, and impaired impulse control. CNS stimulants like cocaine and amphetamines commonly cause paranoia, aggression, and disorganized behavior. During this state, clients may misinterpret benign cues as hostile, escalating aggression rapidly. Clinical management prioritizes staff safety, environmental control, and verbal de-escalation.
Rationale for correct answers
C. Be aware of hospital security – The correct response involves situational awareness and anticipating escalation. Clients under the influence may become physically aggressive. Early preparation, such as alerting security personnel or ensuring exit access, protects both the nurse and others while allowing for de-escalation techniques. Safety is a basic physiological need and must be addressed before therapeutic communication.
Rationale for incorrect answers
A. Confrontation escalates hostility in intoxicated clients, whose cognitive and emotional processing is impaired. It increases defensiveness and the risk of violence.
B. Expressing disgust is judgmental and non-therapeutic. It undermines trust, provokes shame, and can intensify agitation or withdrawal.
D. A scolding or intimidating tone increases power struggles and can precipitate aggression or resistance, worsening the client’s behavioral instability.
Take Home Points
- Substance-induced agitation requires early recognition and safety-focused responses.
- Intoxicated clients may misinterpret interactions, escalating quickly into aggression.
- Avoid confrontation or judgmental behavior, which worsens agitation.
- Awareness of security is essential in early management of behaviorally unpredictable clients.
A depressed client is voluntarily admitted to the inpatient unit after a suicide attempt. The next day the client asks the nurse when he can leave the hospital. Which response by the nurse gives the client accurate information?
Explanation
Voluntary admission in suicidal depression
Voluntary admission allows a client to seek psychiatric care while retaining some civil rights, including the right to request discharge. However, when suicidal ideation is present, clinicians can delay discharge if safety is a concern. Clients must undergo thorough psychiatric evaluation before being cleared. The evaluation involves assessing mood stability, suicidal intent, and response to treatment. Even in voluntary admissions, if a client is deemed a danger, the facility can initiate an involuntary hold to prevent premature discharge.
Rationale for correct answers
B. Let’s talk more about discharge after you have been fully evaluated – This acknowledges the client's rights under voluntary admission while setting clear expectations. It emphasizes the need for clinical evaluation before discharge decisions are made, especially following a suicide attempt. This response is informative and therapeutic.
Rationale for incorrect answers
A. Deflecting responsibility by stating only the psychiatrist can answer avoids addressing the client's concern and provides no therapeutic value.
C. This is false and violates patient autonomy. A voluntarily admitted client retains rights and does not require legal representation for discharge discussions unless involuntary commitment is initiated.
D. Making a prediction about a 1-week timeline is inaccurate and misleading. Discharge depends on clinical progress and safety evaluation, not fixed durations.
Take Home Points
- Voluntary clients retain the right to request discharge unless deemed unsafe.
- A suicide attempt requires comprehensive evaluation before discharge is considered.
- Nurses should provide accurate, respectful, and non-dismissive responses about discharge.
- Predicting discharge timelines without evaluation is clinically inappropriate and unethical.
An elderly Vietnamese client is admitted to a psychiatric unit with a diagnosis of major depression. The client is despondent over the recent death of his wife. The nursing student suggests calling a member of the clergy for him. The client vehemently refuses. What understanding does the nursing student need to have regarding this Vietnamese client?
Explanation
In some Vietnamese cultures, especially among elderly individuals, the presence of clergy in hospital settings may be closely associated with end-of-life rituals, including last rites or impending death. This association can trigger fear, discomfort, or even panic in a patient who is not at that stage. It’s essential for clinicians to consider how cultural frameworks shape the interpretation of seemingly helpful actions and avoid imposing interventions without cultural sensitivity.
Rationale for correct answers
B. The client is associating clergy visitation with last rites – In many traditional Vietnamese customs, clergy involvement is linked with death preparation rather than emotional support. A depressed patient may misinterpret the student’s suggestion as confirmation of impending death, causing distress. Cultural meaning matters in how care is perceived.
Rationale for incorrect answers
A. While some Vietnamese individuals may identify as atheist due to historical political influences, many still engage in ancestor worship, Buddhism, or syncretic practices. Assuming atheism ignores cultural and spiritual diversity.
C. There is no indication the client is struggling with language comprehension. His strong refusal suggests understanding of the suggestion rather than a communication barrier.
D. There is no evidence the client disrespects healthcare staff or Western medicine. His refusal is specifically related to a culturally charged suggestion, not general attitude.
Take Home Points
- Cultural beliefs influence how clients perceive spiritual care and death-related rituals.
- In some cultures, clergy presence signals impending death, not comfort.
- Avoid assumptions; assess the patient’s specific cultural and spiritual context first.
- Misinterpreted support interventions can increase emotional distress in vulnerable clients.
A religious Jewish client on a psychiatric unit pushes the tray away without eating any of the ham, rice, and vegetable entrée. Which information about Jewish culture would the nurse attribute to this behavior?
Explanation
Kashrut refers to the traditional dietary laws followed in Judaism, which define which foods are permissible (kosher) and how they must be prepared. Pork, including ham, is strictly forbidden in all forms. Additionally, Jewish law prohibits the mixing of meat and dairy, and requires specific preparation and sourcing of meat (ritually slaughtered and certified). Observant individuals often avoid any food not certified kosher, especially in institutional settings, due to concerns about preparation and contamination.
Rationale for correct answers
C. The client follows religious dietary laws – The rejection of ham reflects adherence to kosher restrictions, which prohibit pork. This behavior is consistent with observant Jewish practices, where meals must meet strict religious criteria to be acceptable.
Rationale for incorrect answers
A. There is no indication of a food allergy to rice or any other ingredient; the objection was directed at the presence of ham.
B. Vegetarianism would not explain refusal of the rice and vegetables, and the primary concern was likely the presence of pork, not meat in general.
D. The dietary laws of Islam (halal) also forbid pork, but the client is described as religious Jewish, not Muslim, making this rationale culturally inaccurate.
Take Home Points
- Observant Jewish clients avoid pork and require kosher-prepared food.
- Kashrut involves not just food type but also preparation and separation of meat and dairy.
- Misunderstanding religious dietary needs can lead to distress or non-compliance.
- Cultural competence includes recognizing dietary practices linked to religious identity.
A nurse is assessing five clients in the psychiatric unit. Which of the following cultures might interpret therapeutic touch as uncomfortable? Select all that apply
Explanation
Touch is a form of nonverbal communication, but its interpretation is culturally defined. While some cultures perceive it as comforting or familiar, others may see it as invasive or inappropriate, especially in professional or therapeutic settings. Cultural norms around personal space, gender interactions, and spiritual boundaries greatly influence whether touch is accepted or rejected in care. Respecting these norms is essential for building trust and maintaining therapeutic relationships.
Rationale for correct answers
A. Norwegians, Swedes, and Danes – These northern European cultures value personal space and are generally low-touch societies. Physical touch from strangers, even healthcare providers, can be seen as intrusive or uncomfortable.
C. Germans, British Americans, and Swiss – These cultures also maintain strong boundaries regarding personal space. Formality and privacy are highly valued, and unsolicited touch, particularly in clinical interactions, may be unwelcome.
D. Asian Indians, Chinese Americans, and Native Americans – Many individuals from these backgrounds consider touch—especially by unrelated or opposite-gender individuals—as culturally sensitive. Native Americans may also view touch as spiritually significant, requiring careful respect for boundaries.
Rationale for incorrect answers
B. French, Italians, and Russians generally come from high-touch cultures where physical contact such as handshakes, cheek kisses, or arm touches is common and often considered a sign of warmth and engagement.
E. African Americans, Haitians, and individuals from the Dominican Republic may come from cultures where touch is often accepted or even expected in communication, especially in emotionally expressive or community-based interactions.
Take Home Points
- Cultural norms shape how touch is perceived, some cultures value space and minimal physical contact.
- Northern and central European cultures often maintain low-touch boundaries.
- Many Asian and Native American groups may view touch as sensitive or spiritually significant.
- Misuse of therapeutic touch without cultural understanding may cause discomfort or mistrust.
Exams on The Nurse-Client Relationship and Therapeutic Communication Process
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- The Nurse-Client Relationship
- Principles of a Therapeutic Nurse-Client Relationship
- Phases of a Therapeutic Nurse-Client Relationship
- Practice Exercise
- Family as an Extension of the Client
- Impact of Culture, Ethnicity, Religion, and Spirituality on Client Care
- Practice Exercise 2
- Therapeutic Communication Process
- Therapeutic and Nontherapeutic Communication Techniques
- Practice Exercise 3
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Identify the essential components and principles of a therapeutic nurse-client relationship.
- Describe the phases of the nurse-client relationship based on Peplau's model.
- Explain the importance of self-awareness and the therapeutic use of self in nursing.
- Recognize the role of the family as an extension of the client in mental health care.
- Analyze the impact of culture, ethnicity, religion, and spirituality on client care.
- Apply culturally competent and culturally relevant care in nursing practice.
- Define the principles of therapeutic communication in nursing.
- Distinguish between therapeutic and nontherapeutic communication techniques.
- Explain the importance of attending behavior and self-awareness in effective communication.
The Nurse-Client Relationship
- A therapeutic nurse-client relationship is central to effective mental health nursing.
- It involves essential qualities such as trust, rapport, respect, empathy, and positive regard.
- Nurses must be self-aware and understand their own beliefs to avoid bias.
- Peplau's model describes the relationship in four interrelated phases: pre-interaction, orientation, working, and termination.
- The family is considered an extension of the client and plays a key role in the client’s support system.
- Culturally competent care is vital, requiring nurses to adapt communication, care strategies, and interventions based on patients’ cultural and spiritual backgrounds.
Principles of a Therapeutic Nurse-Client Relationship
- Essential Conditions: Several characteristics are essential to developing a therapeutic relationship, including rapport, trust, and respect.
- Rapport: This is the primary task in relationship development and implies special feelings on the part of both the client and the nurse based on acceptance, warmth, friendliness, common interest, a sense of trust, and a nonjudgmental attitude.
- Trust: To trust another, one must feel confidence in that person’s presence, reliability, integrity, veracity, and sincere desire to help when requested. Trust is the basis of a therapeutic relationship and must be established for the relationship to progress beyond a superficial level.
- Examples of nursing interventions to promote trust include: providing a blanket when the client is cold, providing food when the client is hungry, keeping promises, and being honest.
- Other components involved in building a therapeutic relationship are genuine interest, empathy, acceptance, and positive regard.
- Self-Awareness: It is crucial for nurses to understand their own values and attitudes to become aware of beliefs that may interfere with establishing positive relationships. Self-awareness is also an important component for developing the nurse-client relationship and involves understanding what you value and what beliefs guide your behavior. Nurses' values and beliefs reflect their own culture/subculture and are chosen from a variety of influences and role models.
- Therapeutic Use of Self: This is a crucial skill for a nurse to develop. A professional nurse-patient relationship consists of a nurse with skills and expertise and a patient who wants to alleviate suffering, find solutions to problems, or find an advocate.
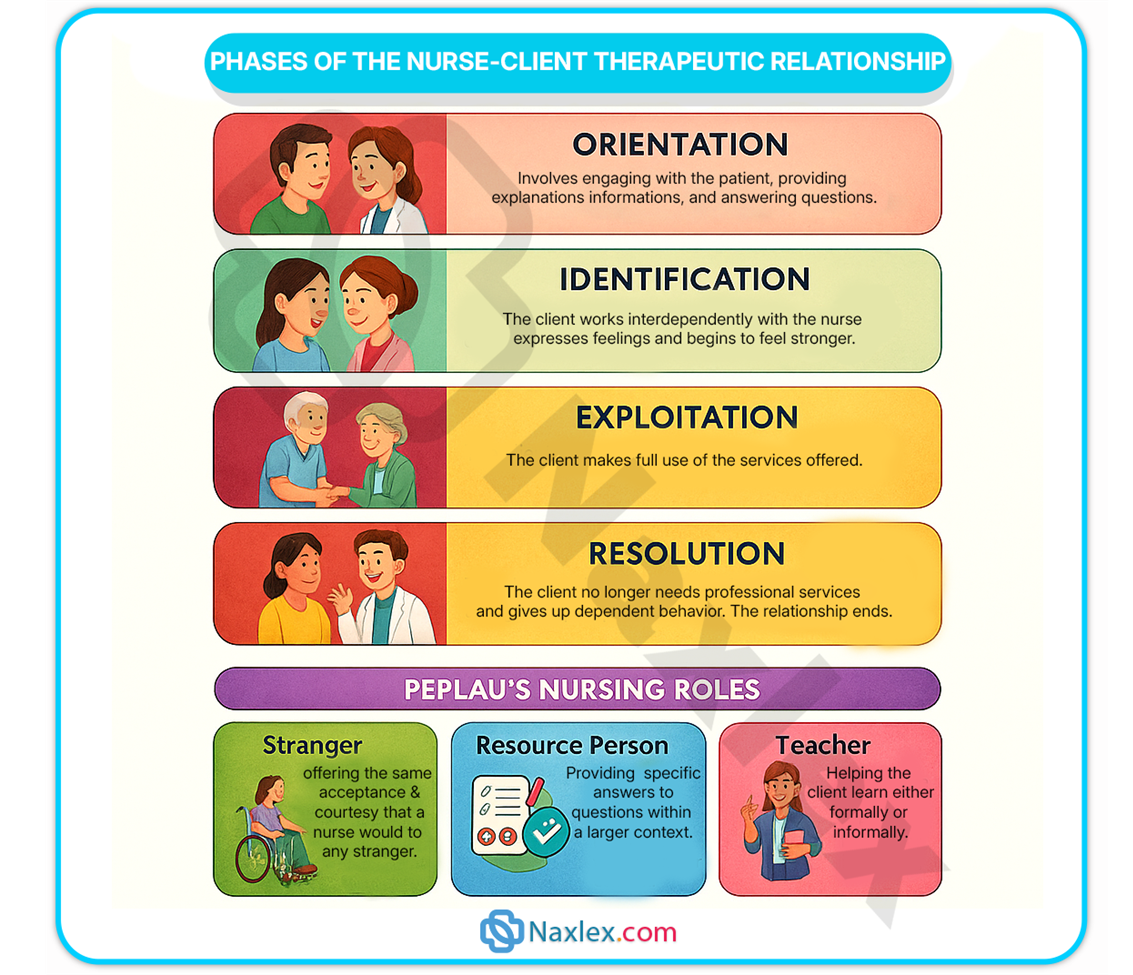
Phases of a Therapeutic Nurse-Client Relationship
- Hildegard Peplau's model of the nurse-patient relationship is a well-accepted tool in the United States and Canada. She proposed that the nurse-patient relationship "facilitates forward movement" for both the nurse and the patient.
- The relationship evolves through three distinct, interlocking, and overlapping phases, with an additional preorientation phase. The four phases are:
- Preorientation phase: This phase is when the nurse prepares for the orientation phase.
- Orientation phase: This is the first stage of the relationship.
- Working phase: This is the second stage of the relationship.
- Termination phase: This is the final stage that begins when the client's problems are resolved and ends when the relationship concludes.
- The nurse-patient relationship evolves through three distinct interlocking and overlapping phases. Hildegard Peplau introduced the concept of the nurse-patient relationship.
- Pre-interaction phase:
-
- Begins before the nurse’s first contact with the client.
- Orientation or introductory phase:
-
- This phase begins when the nurse and client meet and ends when the client begins to identify problems to be examined. This is when rapport is established.
- The nurse introduces herself or himself to the client by using first and last name and designation.
- The purpose and time frame of the relationship are identified, establishing a contract.
- The client’s strengths and needs are identified.
- Termination and separation of the relationship are discussed in anticipation of the time-limited nature of the relationship.
- Working phase:
-
- The working phase begins when the client actively identifies and explores his or her problems.
- Exploring, focusing on, and evaluating the client’s concerns and problems occur.
- The nurse uses interpersonal strategies to help the client identify effective coping strategies.
- Encourages self-direction and self-management whenever possible to promote health and wellness.
- Termination or separation phase:
-
- This is the final stage in the nurse–client relationship.
- It begins when the client’s problems are resolved and concludes when the relationship ends.
- It is a time to evaluate progress and achievement of goals.
Family as an Extension of the Client
- Assessment of the family begins with information presented on the "face" of the family, including the family constellation and identification of individual family members.
- Family history should include past medical and mental illnesses across at least three generations.
- Families are a major part of the support system for patients with mental illness.
- Client and family teaching is an important part of the nurse-client relationship.
- Boundaries: Clear boundaries maintain distinctions between individuals within the family and between the family and the outside world.
- Diffuse or enmeshed boundaries: These are a blending of roles, thoughts, and feelings among individuals.
- Rigid or disengaged boundaries: These are when rules and roles are adhered to no matter what.
- Family Interventions: The nurse's role in family intervention includes setting clear limits and being consistent and fair.
- Family life cycle: This concept is important for understanding the family system, which includes different stages, such as "The Family in Later Life," which begins with retirement and lasts until the death of both spouses.
Impact of Culture, Ethnicity, Religion, and Spirituality on Client Care
- Cultural Competence: This is required of nurses to assist patients in achieving mental health and well-being. It is defined as attitudes and behaviors that enable a nurse to work effectively within the patient’s cultural context.
- Cultural competence goes beyond cultural sensitivity by adapting care to the patient’s cultural needs and preferences.
- Culturally Relevant Care: This is important for meeting the needs of culturally diverse patients.
- Western Psychological Theory: There are potential problems in applying Western psychological theory to patients of other cultures.
- Beliefs and Practices: It is important to compare Western nursing beliefs with the beliefs and practices of patients from diverse cultures. For some Asians and Latinos, the "hot and cold" theory of disease is important to their well-being.
- Communication: In some cultures, such as Haitian culture, people may avoid direct eye contact as a sign of politeness and shyness with authority figures, and handshakes are a formal greeting. They may also smile and nod as a sign of respect even if they don't understand what is being said. Tone of voice and hand gestures may be used to emphasize what is being said.
- Personal Space and Touch: Cultural groups differ in their valuation of personal space and comfort with touch.
- Spirituality and Religious Beliefs: These are often overlooked elements of patient care, but being part of a spiritual community is helpful to people coping with illness. Forgiveness is essential to a spiritual nature, which is the ability to release from the mind all past hurts, failures, guilt, and loss.
- Barriers to Care: Culturally inappropriate services are a reason why minority groups in the United States may not receive or benefit from mental health services.
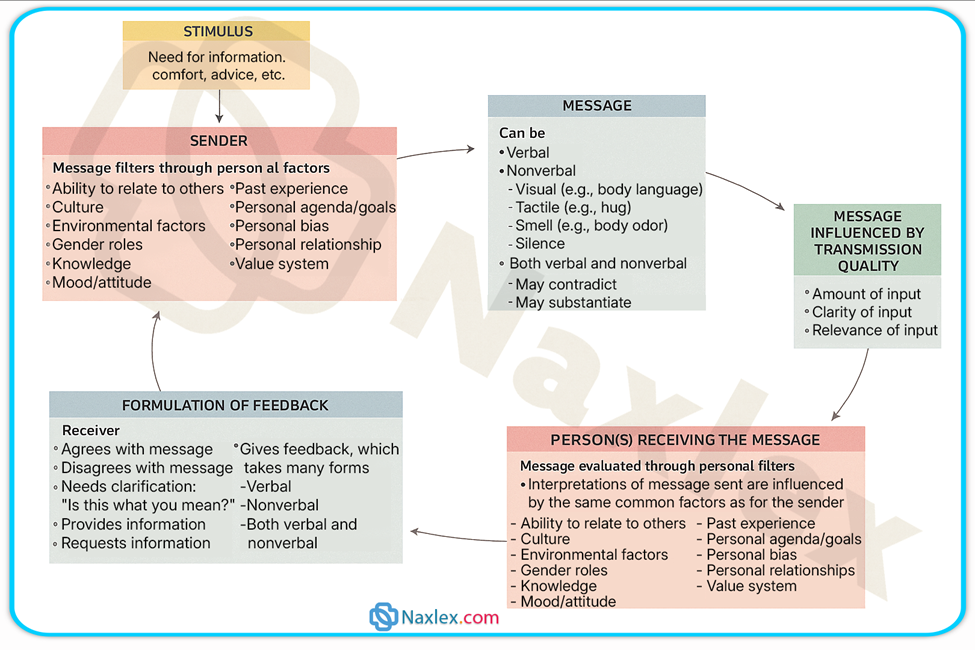
Therapeutic Communication Process
- Therapeutic communication is central to building trust and promoting healing in the nurse-client relationship.
- Nonverbal cues such as posture, eye contact, and body language play a key role in effective communication.
- Effective communication involves honesty, assertiveness, empathy, and self-awareness.
- Anxiety may be present during initial interactions until rapport is established.
- The therapeutic relationship allows for problem identification and resolution through active nurse involvement.
- Nurses must avoid projecting personal biases and instead foster a safe space for open communication.
-
1.1. Principles
- Posture, eye contact, and body language are nonverbal behaviors that reflect the degree of attending.
- Thoughts and feelings can be openly, honestly, and assertively expressed in families where communication is healthy.
- The nurse needs to be aware of how their preconceptions may affect their ability to care for individual clients.
- Attending behavior is the foundation of interviewing.
- Introductions are often uncomfortable, and the participants may experience some anxiety until a degree of rapport has been established. Interactions may remain on a superficial level until anxiety subsides.
- The nurse who is stressed or overwhelmed tends to lose the objectivity that comes with self-awareness and personal growth activities.
- Attempts to dispel the client’s anxiety by implying that there is not sufficient reason for concern completely devalue the client’s feelings.
- The therapeutic interpersonal relationship is the means by which the nursing process is implemented. Through the relationship, problems are identified and resolution is sought.
- The experience is viewed not as “a job,” “part of a course,” or “time spent talking” but as an opportunity to work with patients to help them develop personal resources and actualize more of their potential in living.
- The nurse’s guidance helps the client examine and make changes.
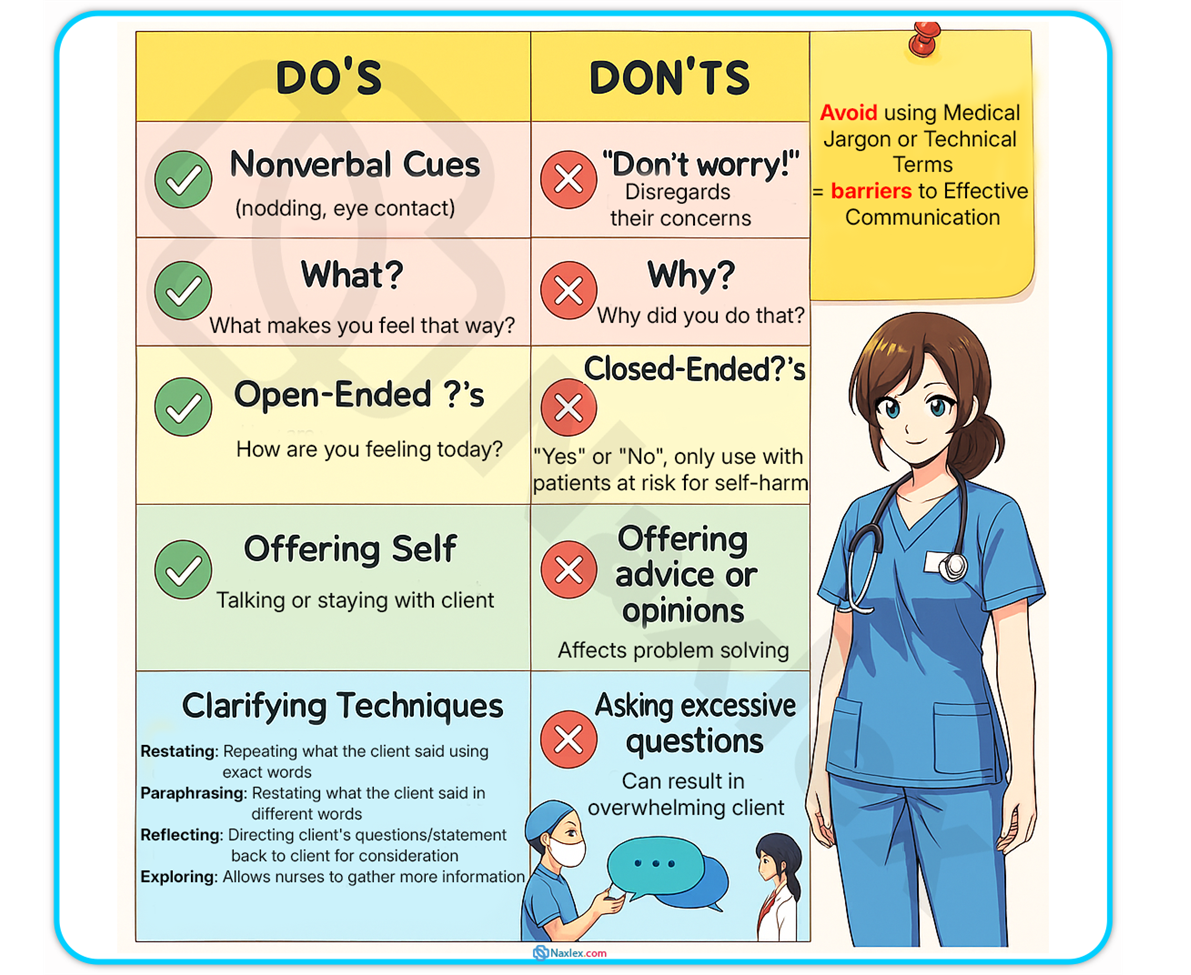
Therapeutic and Nontherapeutic Communication Techniques
1.1 Therapeutic Techniques
- Attending: This is a special kind of listening that refers to an intensity of presence, or being with the patient. At times, simply being with another person during a painful time can make a difference.
- Suspending Value Judgments: Nurses are more effective when they guard against using their own value systems to judge patients’ thoughts, feelings, or behaviors.
- Helping Patients Develop Resources: The nurse becomes aware of patients’ strengths and encourages patients to work at their optimal level of functioning.
- Empathetic response: The nurse reflects the client's feelings back to them to encourage expression.
- Setting clear limits: Stating what is and is not okay in a situation (e.g., “Peter, it is okay to state when you are angry about something that has been said. It is not okay to throw the chair against the wall.”).
- Being consistent and fair: This encourages everyone to contribute and to respect one another’s opportunity to contribute equally.
1.2 Nontherapeutic Techniques
- Reassuring: Attempts to dispel the client’s anxiety by implying that there is not sufficient reason for concern completely devalue the client’s feelings. Vague reassurances without accompanying facts are meaningless to the client.
- Rejecting: Refusing to consider or showing contempt for the client’s ideas or behaviors, which closes off the topic from exploration and may make the client feel personally rejected.
- Requesting an explanation ("Why" questions): Asking the client to provide reasons for thoughts, feelings, behaviors, or events is often intimidating. The client is unlikely to know “why” and may become defensive trying to explain themself.
- Testing: Appraising the client’s degree of insight, which forces the client to try to recognize their problems.
- Using denial: Refusing to admit that a problem exists by dismissing the client's comments without attempting to discover the feelings or meaning behind them.
Therapeutic Techniques Summary Table
|
Technique |
Description |
|
Active listening |
Carefully noting what the client is saying and observing the client’s nonverbal behavior |
|
Broad openings |
Encouraging the client to select topics for discussion |
|
Clarifying |
Providing a means for making the message clearer, correcting misunderstandings, and promoting mutual understanding |
|
Focusing |
Directing the conversation on the topic being discussed |
|
Informing |
Giving information to the client |
|
Offering self to help |
Includes staying with the client, talking to the client, and offering to help the client |
|
Open-ended questions |
Encouraging conversation because these questions require more than one-word answers |
|
Paraphrasing |
Restating in different words what the client said |
|
Reflecting |
Directing the client’s question or statement back to the client for consideration |
|
Restating |
Repeating what the client has said and directing the statement back to the client to provide the client the opportunity to agree or disagree or to clarify the message further |
|
Silence |
Allowing time for formulating thoughts |
|
Summarizing |
Stating briefly what was discussed during the conversation |
|
Validating |
Verifying that both the nurse and the client are interpreting the topic or message in the same way |
Nontherapeutic Techniques Summary Table
|
Technique |
Description |
|
Approval |
Implying that the client is thinking or doing the right thing and is not thinking or doing what is wrong; this may direct the client to focus on behavior that pleases the nurse |
|
Asking excessive questions |
Demanding information from the client without respect for the client’s willingness or readiness to respond |
|
Changing the subject |
Avoiding addressing the client’s thoughts, feelings, or concerns; implying that the client’s statement is not important |
|
Closed-ended questions |
Questions that ask for specific information such as a “yes” or “no” answer and therefore inhibit communication |
|
Disagreeing |
Opposing the client’s thinking or opinions, implying that the client is wrong |
|
Disapproving |
Indicating a negative value judgment about the client’s behavior or thoughts |
|
False reassurance |
Making a statement that implies the client has no reason to be worried or concerned; belittling a client’s concerns |
|
Giving advice |
Assuming that the client cannot think for herself or himself, which inhibits problem solving and fosters dependence |
|
Minimizing the client’s feelings |
Making a statement that implies that the client’s feelings are not important |
|
Parroting |
Repeating the client’s words before determining what the client has said |
|
Placing the client’s feelings on hold |
Avoiding addressing the client’s thoughts, feelings, or concerns; making a statement that places the responsibility of addressing the client’s thoughts, feelings, or concerns elsewhere or on another person |
|
Value judgments |
Making a comment that addresses the client’s morals; this can make the client feel angry or guilty or as though she or he is not being supported |
|
“Why?” questions |
Cause the client to feel defensive, because many times she or he does not know the reason “why”; these types of questions also often imply criticism |
Summary
- A strong nurse-client relationship is built on trust, rapport, respect, and effective communication.
- Self-awareness and therapeutic use of self are foundational skills for mental health nurses.
- Peplau’s phases—pre-interaction, orientation, working, and termination—guide the development of therapeutic relationships.
- Family involvement is crucial in assessment, support, and education of the client.
- Cultural competence involves understanding and respecting the client’s cultural, ethnic, religious, and spiritual background.
- Barriers such as cultural misunderstandings and inappropriate services can hinder effective mental health care.
- Nurses must provide culturally relevant and individualized care to promote mental well-being.
- Attending behavior—including focused listening and presence—is foundational to therapeutic interactions.
- Nurses must reflect empathy and suspend personal value judgments to fully support clients.
- Techniques such as setting limits, being consistent, and helping clients identify resources foster client growth.
- Empathetic responses validate client emotions and promote further expression.
- Nontherapeutic techniques—like giving false reassurance, asking "why" questions, or rejecting ideas—can shut down communication and harm trust.
- Self-awareness, emotional regulation, and consistency are critical to effective, therapeutic communication.
- The goal is not just to complete a task but to help clients develop insight, coping skills, and autonomy through guided interactions.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on The Nurse-Client Relationship and Therapeutic Communication Process
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


