Please set your exam date
Drugs Used for Psychoses
Study Questions
Practice Exercise 1
Case scenario to use for the questions:
A patient with a known diagnosis of schizophrenia was admitted to the psychiatric area of the hospital after an episode of psychotic behavior.
A nurse is assessing the patient in the scenario who has been admitted to the psychiatric unit and who has been hearing voices that told them to lock all the doors and not answer any phone calls. The nurse recognizes which of the signs and symptoms of psychotic behavior that may be exhibited? Indicate with an X the significant factors and the unrelated factors associated with psychotic behavior.
Explanation
In patients with schizophrenia, assessment focuses on identifying core psychotic symptoms such as hallucinations, delusions, disorganized thinking, and speech disturbances. Recognizing these signs early allows for timely interventions and supports safety and therapeutic planning. Differentiating between symptoms directly related to psychosis and those linked to other mental health conditions (e.g., anxiety behaviors) is essential for accurate nursing assessment and care.
Rationale for correct answer:
- Auditory hallucinations – Significant factor
Hearing voices is a hallmark symptom of schizophrenia and psychosis. In this scenario, the patient hears voices giving commands, which directly indicates a psychotic feature. - Grandiose delusions – Significant factor
Fixed, false beliefs that are not based in reality (e.g., exaggerated self-importance or powers) are core symptoms of psychotic disorders, including schizophrenia. - Wringing hands – Unrelated factor
Repetitive hand-wringing is typically linked to anxiety, agitation, or obsessive-compulsive behaviors rather than a defining sign of psychosis. - Flight of ideas – Significant factor
Rapid shifting from one thought to another, often without clear connections, is common in certain psychotic episodes and can be present alongside schizophrenia symptoms. - Garbled speech – Significant factor
Disorganized speech, such as incoherent or illogical sentences, reflects disorganized thought processes—another key feature of psychotic behavior.
Take-Home Points:
- Hallucinations, delusions, and disorganized speech are hallmark indicators of psychotic behavior.
- Behaviors such as hand-wringing may reflect anxiety but are not primary signs of psychosis.
- Accurate symptom differentiation guides appropriate treatment and nursing interventions in schizophrenia care.
Practice Exercise 2
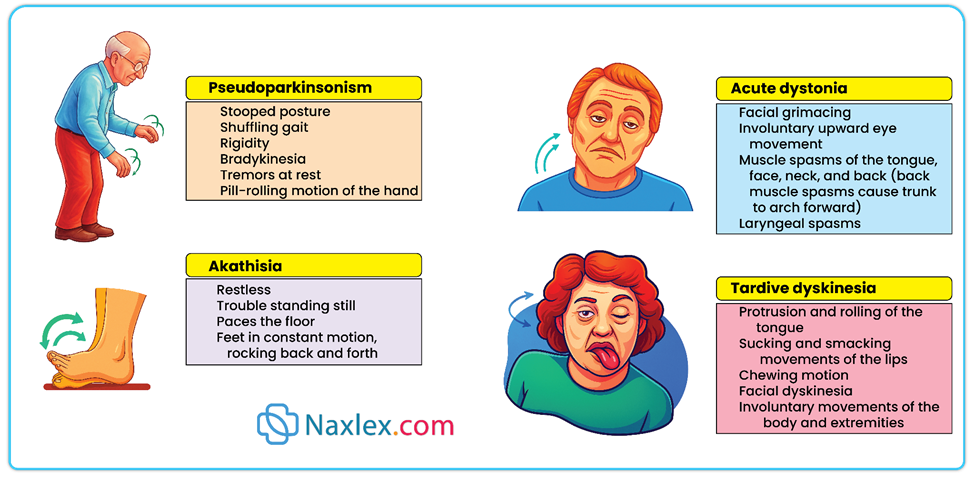
A patient who is taking an antipsychotic agent develops extrapyramidal symptoms. Which of these symptoms, if observed by the nurse, would indicate the presence of extrapyramidal effects? Select all that apply.
Explanation
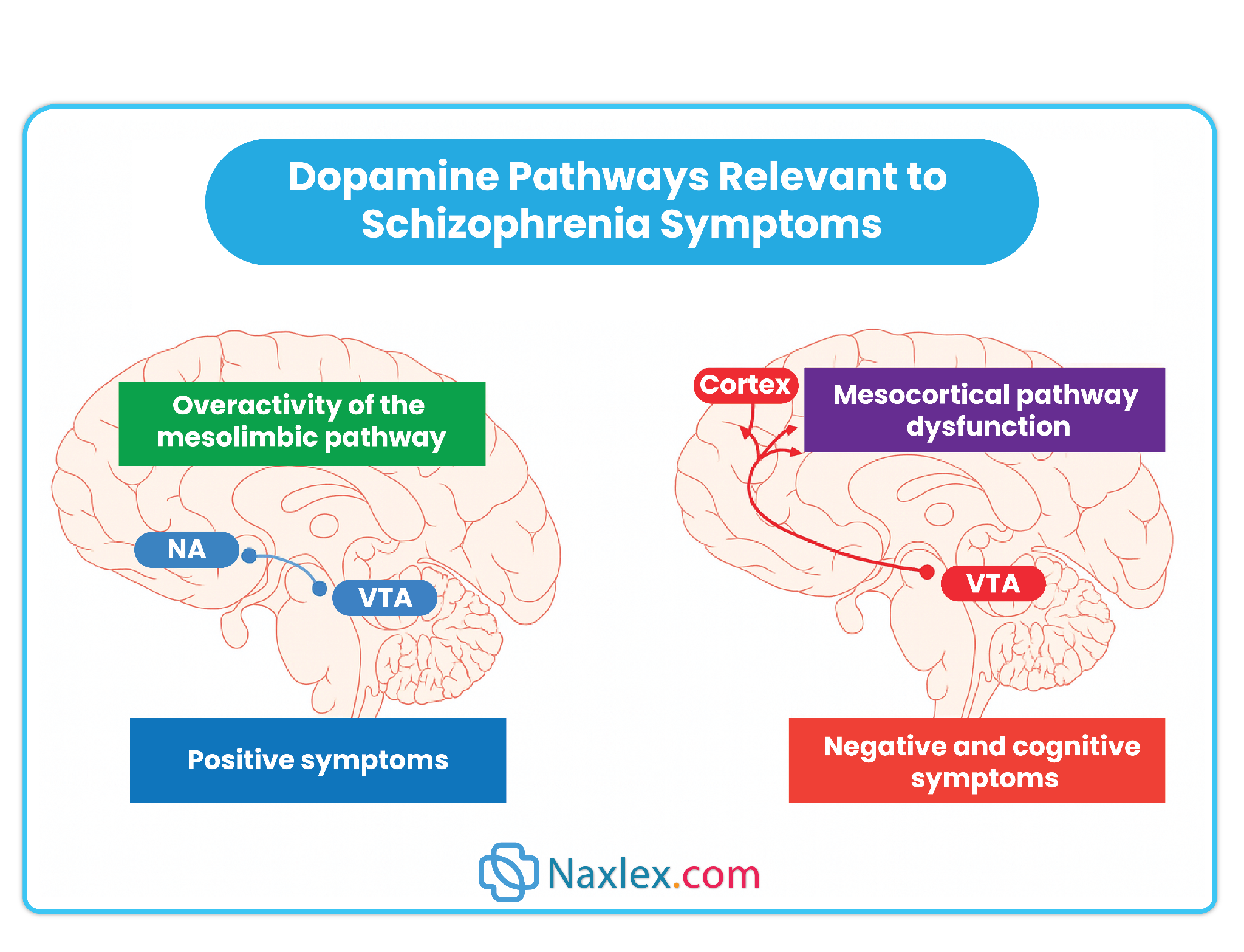
Extrapyramidal symptoms (EPS) are a group of movement disorders that can occur as adverse effects of antipsychotic medications, particularly first-generation (typical) antipsychotics. These symptoms result from dopamine receptor blockade in the basal ganglia and can significantly affect mobility, coordination, and quality of life. The nurse must routinely assess for these signs and intervene promptly to reduce the risk of complications and improve adherence to therapy.
Rationale for correct answer:
A. Tongue protrusion: A hallmark of tardive dyskinesia, a late-onset EPS, reflecting involuntary movements of the tongue and mouth.
C. Neck torsions: Represent dystonic reactions, an acute form of EPS causing painful, involuntary muscle contractions.
E. Shuffling gait: Reflects pseudo-parkinsonism, an EPS characterized by slowed movements, stooped posture, and reduced arm swing.
F. Pacing or rocking: Indicative of akathisia, an EPS that manifests as inner restlessness and repetitive movements.
H. Jaw spasms: Another form of dystonia, involving sudden, involuntary contraction of jaw muscles.
I. Mask-like expression: Represents rigidity and bradykinesia associated with parkinsonian EPS, leading to reduced facial expressiveness.
Rationale for incorrect answer:
B. Pressured speech: This is more characteristic of mania or psychosis, not EPS, and is not related to medication-induced movement disorders.
D. Seizures: Not typically a manifestation of EPS; seizures are a separate neurological concern that may arise from other causes or medications.
G. Frequent blinking: This is not a specific EPS sign; may be benign or related to anxiety.
Take-home points:
- EPS can manifest as dystonia, akathisia, pseudo-parkinsonism, or tardive dyskinesia.
- Early recognition and treatment of EPS improve patient safety and medication adherence.
- Regular assessment using tools like the Abnormal Involuntary Movement Scale (AIMS) is recommended.
A patient appears to have had an overdose of phenothiazines. The nurse anticipates that which intervention(s) may be used to treat phenothiazine overdose? Select all that apply.
Explanation
Phenothiazine overdose is a medical emergency that can result in severe central nervous system depression, hypotension, and respiratory compromise. Nursing priorities focus on stabilizing vital functions, preventing further drug absorption, and supporting organ systems until the toxic effects resolve. Interventions are largely supportive and aimed at minimizing complications rather than reversing the drug's effects with another antipsychotic.
Rationale for correct answer:
A. Gastric lavage: Gastric lavage may be performed soon after ingestion to remove unabsorbed drug from the stomach, reducing systemic toxicity. It is most effective within the first hour of ingestion.
B. Adequate hydration: Hydration helps maintain blood pressure, support renal function, and facilitate drug elimination. This is essential in cases of hypotension or when high doses of phenothiazines have been ingested.
C. Maintaining an airway: Phenothiazine overdose can lead to CNS depression and respiratory compromise. Ensuring a patent airway and supporting ventilation are critical nursing priorities.
F. Activated charcoal administration: Activated charcoal binds the drug in the gastrointestinal tract, limiting absorption into the bloodstream, and is a common intervention for oral overdoses.
Rationale for incorrect answer:
D. Fluphenazine (Prolixin): Administering another antipsychotic is not appropriate and could worsen toxicity. Management focuses on supportive care, not adding additional dopamine blockade.
E. Risperidone (Risperdal): Similarly, adding another antipsychotic is contraindicated during an overdose. It does not reverse toxicity and may compound CNS depression.
Take-home points:
- Phenothiazine overdose is managed with supportive care, including airway protection, hydration, and limiting further absorption.
- Gastric lavage and activated charcoal are effective if administered promptly after ingestion.
- Additional antipsychotics are contraindicated during overdose management.
A nurse observes a patient with involuntary lip-smacking and tongue movements after chronic haloperidol use. What is the most likely condition?
Explanation
Tardive dyskinesia (TD) is a late-onset extrapyramidal symptom that typically occurs after long-term use of antipsychotics, particularly first-generation agents like haloperidol. It is characterized by involuntary, repetitive movements of the face, tongue, lips, and extremities, and can be irreversible if not recognized early. Nurses must assess for TD regularly using tools like the Abnormal Involuntary Movement Scale (AIMS) to monitor for early signs and collaborate with prescribers for management.
Rationale for correct answer:
B. Tardive dyskinesia
Chronic antipsychotic use, especially with haloperidol, can lead to lip-smacking, tongue protrusion, and grimacing. Early detection is critical, as these movements may become permanent without intervention.
Rationale for incorrect answers:
A. Akathisia
Involves restlessness, pacing, or an inability to remain still, rather than involuntary facial movements. It typically occurs within days to weeks of starting antipsychotics.
C. Acute dystonia
Characterized by sudden, severe muscle contractions, often affecting the neck, face, or back, occurring hours to days after starting therapy, not after chronic use.
D. Neuroleptic malignant syndrome (NMS)
A rare, life-threatening reaction to antipsychotics, presenting with hyperthermia, muscle rigidity, altered mental status, and autonomic instability, not isolated facial movements.
Take-home points:
- Tardive dyskinesia is associated with chronic antipsychotic therapy and involves involuntary facial and tongue movements.
- Early identification using AIMS can prevent progression to irreversible symptoms.
- Collaborate with prescribers to adjust therapy and consider switching to atypical antipsychotics if TD develops.
A patient develops severe rigidity, high fever, and altered mental status after starting chlorpromazine. What is the nurse’s priority action?
Explanation
Neuroleptic malignant syndrome (NMS) is a rare but life-threatening reaction to antipsychotic medications like chlorpromazine. It is characterized by severe muscle rigidity, hyperthermia, altered mental status, and autonomic dysfunction. Early recognition and rapid intervention are critical to prevent complications such as rhabdomyolysis, renal failure, or death.
Rationale for correct answer:
D. Notify the provider immediately: This is the priority action. Prompt medical management may include discontinuation of the antipsychotic, supportive care (hydration, cooling measures), and possible pharmacologic treatment such as dantrolene or bromocriptine to reduce muscle rigidity and hyperthermia.
Rationale for incorrect answers:
A. Monitor vital signs before the next dose: Monitoring alone is insufficient in NMS, as the condition requires immediate medical intervention. Delaying action can be fatal.
B. Administer an anticholinergic: Anticholinergics treat extrapyramidal symptoms, not the systemic complications of NMS. This would not address the critical, life-threatening effects.
C. Encourage frequent ambulation: While mobility may prevent minor complications in psychiatric patients, ambulation does not treat NMS and could worsen the patient’s condition due to extreme rigidity and instability.
Take-home points:
- Neuroleptic malignant syndrome is life-threatening and requires immediate reporting.
- Key signs include high fever, rigidity, altered mental status, and autonomic instability.
- Early intervention can prevent severe complications and improve outcomes.
Which pathway is primarily targeted by first-generation antipsychotics to reduce hallucinations and delusions?
Explanation
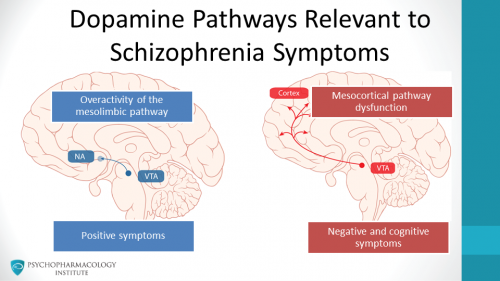
First-generation antipsychotics (FGAs) primarily act by blocking dopamine D2 receptors in the mesolimbic pathway, which is associated with positive symptoms of schizophrenia, such as hallucinations and delusions. Targeting this pathway helps reduce these psychotic manifestations while other pathways may contribute to adverse effects.
Rationale for correct answer:
B. Mesolimbic: Dopamine hyperactivity in this pathway contributes to positive psychotic symptoms. FGAs effectively reduce hallucinations and delusions by dampening this overactive dopaminergic signaling.
Rationale for incorrect answers:
A. Nigrostriatal: This pathway regulates movement. Dopamine blockade here is responsible for extrapyramidal symptoms (EPS), not the reduction of hallucinations or delusions.
C. Mesocortical: This pathway is involved in cognition and negative symptoms. Dopamine blockade here may worsen negative symptoms such as apathy or social withdrawal.
D. Tuberoinfundibular: This pathway regulates prolactin secretion. Blockade can lead to hyperprolactinemia, resulting in galactorrhea, amenorrhea, or sexual dysfunction, but it does not target positive psychotic symptoms.
Take-home points:
- Mesolimbic pathway hyperactivity drives positive symptoms; first-generation antipsychotics reduce these symptoms.
- Other dopaminergic pathways are associated with side effects, not therapeutic benefits.
- Understanding pathway-specific effects helps anticipate both therapeutic outcomes and adverse effects.
A patient initiated on chlorpromazine is at risk for which common cardiovascular side effect that the nurse should monitor for?
Explanation
Chlorpromazine, a first-generation (typical) antipsychotic, exerts alpha-1 adrenergic receptor blockade, leading to vasodilation and a drop in blood pressure upon standing, known as orthostatic hypotension. This effect is especially pronounced during initial therapy or rapid dose escalation, placing patients at risk for dizziness, syncope, and falls. Nursing assessment should include frequent monitoring of vital signs, patient education about slow positional changes, and precautions to prevent injury from falls.
Rationale for correct answer:
C. Orthostatic hypotension: This is the most clinically significant cardiovascular effect. Alpha-1 blockade causes blood pooling in lower extremities when standing, decreasing cerebral perfusion and resulting in dizziness, lightheadedness, or syncope. Older adults or patients on concurrent antihypertensives are particularly vulnerable, making vital signs and safety monitoring essential.
Rationale for incorrect answers:
A. Hypertension: Chlorpromazine primarily causes hypotension rather than elevated blood pressure due to its peripheral alpha-adrenergic blockade, making hypertension an unlikely side effect.
B. Bradycardia: While heart rate changes can occur, reflex tachycardia is more typical as a compensatory response to hypotension, rather than bradycardia.
D. Tachycardia: May occur as a compensatory response to hypotension, but it is secondary and not the primary concern when initiating therapy.
Take-home points:
- Monitor blood pressure lying, sitting, and standing to detect orthostatic changes early.
- Educate patients to rise slowly and remain seated briefly before standing to reduce fall risk.
- Implement safety precautions, especially for older adults or those with comorbid cardiovascular conditions.
A nurse observes a patient with involuntary lip-smacking and tongue movements after chronic haloperidol use. What is the most likely condition?
Explanation
Tardive dyskinesia is a late-onset extrapyramidal symptom that often develops after long-term use of first-generation antipsychotics such as haloperidol. It is characterized by involuntary, repetitive movements, including lip-smacking, tongue protrusion, grimacing, and rapid blinking. Nurses should regularly assess for these movements using tools like the AIMS scale, educate patients about early recognition, and collaborate with providers for medication adjustments to prevent progression.
Rationale for correct answer:
B. Tardive dyskinesia: Occurs after chronic antipsychotic use, typically months to years, with persistent, involuntary movements of the face, tongue, and extremities. The symptoms may be irreversible, making early identification critical.
Rationale for incorrect answers:
A. Akathisia: Involves inner restlessness and pacing, not the involuntary facial and tongue movements seen here. It usually appears within days to weeks of starting therapy.
C. Acute dystonia: Presents as sustained muscle contractions, often affecting the neck, eyes, or back, and typically appears within hours to days of starting therapy, not after chronic use.
D. Neuroleptic malignant syndrome: Manifests with fever, rigidity, autonomic instability, and altered mental status, which is acute and life-threatening, not characterized by repetitive oral movements.
Take-home points:
- Tardive dyskinesia is associated with long-term antipsychotic therapy and may be irreversible.
- Regular monitoring using standardized assessments is essential for early detection.
- Collaborate with the healthcare provider regarding potential dose adjustment or switching to atypical antipsychotics if symptoms appear.
Practice Exercise 3
Case scenario to use for the questions:
A patient with a known diagnosis of schizophrenia was admitted to the psychiatric area of the hospital after an episode of psychotic behavior.
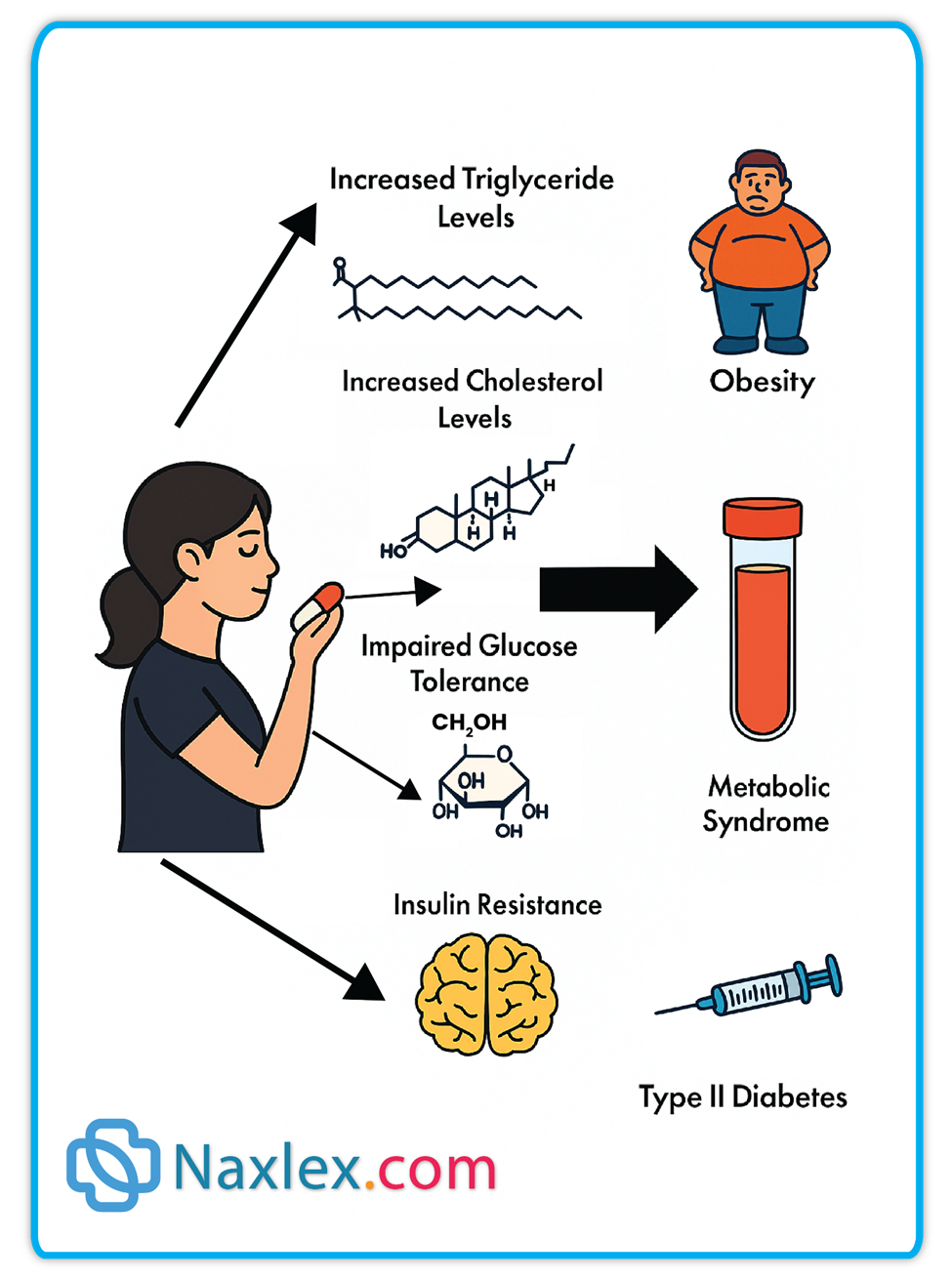
The nurse knows that extrapyramidal effects may be seen with antipsychotic medications; what other adverse effects should be monitored for? Select all that apply.
Explanation
Antipsychotic medications, particularly both typical and atypical agents, can cause a range of adverse effects beyond extrapyramidal symptoms (EPS). Nurses must monitor patients for neurological complications, metabolic disturbances, and cardiovascular risks to ensure early detection and prevention of long-term harm.
Rationale for correct answer:
A. Seizures:
Some antipsychotics, especially at higher doses or in susceptible patients, lower the seizure threshold, increasing the risk of seizure activity. Regular neurological assessment and monitoring for unusual movements or episodes of loss of consciousness are critical.
D. Dyslipidemia:
Atypical antipsychotics can disrupt lipid metabolism, leading to elevated cholesterol and triglyceride levels. This increases the risk of cardiovascular disease, making regular lipid panel monitoring an essential nursing responsibility.
E. Hyperglycemia:
Antipsychotic therapy, particularly with atypical agents, may impair glucose regulation, causing hyperglycemia or new-onset diabetes mellitus. Monitoring blood glucose and educating patients on signs of hyperglycemia are necessary to prevent complications.
Rationale for incorrect answer:
B. Weight loss:
Weight loss is uncommon; most antipsychotics are associated with weight gain, not loss.
C. Chronic fatigue:
While sedation may occur, chronic fatigue is not a primary adverse effect requiring routine monitoring in the same way as seizures, dyslipidemia, or hyperglycemia.
Take-home points:
- Monitor for neurological complications such as seizures during antipsychotic therapy.
- Assess metabolic parameters, including lipid profiles and blood glucose levels, regularly.
- Early detection of adverse effects can prevent long-term complications and improve patient safety.
The nurse is discussing with the patient in the scenario being treated for psychoses with antipsychotic medications what to expect. Which statement by the nurse needs to be revised?
Explanation
Antipsychotic medications, used for the treatment of psychoses, work by modulating dopamine and other neurotransmitter activity in the brain. While they are effective in reducing positive symptoms such as hallucinations and delusions, therapeutic effects are typically gradual and may take several weeks to become noticeable. Nurses play a critical role in educating clients on realistic timelines, monitoring for side effects, and supporting adherence to prevent relapse or exacerbation of symptoms.
Rationale for correct answer:
A. “While you take these medications they should work within the week to reduce auditory hallucinations or those voices you hear.”
This statement is inaccurate because antipsychotic medications generally take 2–6 weeks to achieve full effectiveness for positive symptoms like hallucinations. Stating that relief occurs within a week may create unrealistic expectations and reduce medication adherence if improvement is not immediate.
Rationale for incorrect answer:
B. “These medications will be effective in reducing your feelings of agitation.”
Antipsychotics can have a sedating effect and help reduce agitation associated with psychosis, making this statement appropriate and therapeutically accurate.
C. “While you take these medications you may find that you start to gain weight.”
Many antipsychotics, particularly atypical agents, are associated with weight gain and metabolic changes. This is an important part of client teaching and monitoring, making this statement correct.
D. “These medications will allow you to get a good night’s sleep.”
Sedative properties of some antipsychotics can improve sleep patterns, which is a valid expected effect and appropriate to communicate to the client.
Take-home points:
- Antipsychotics take several weeks to reduce hallucinations and delusions.
- Educate clients on realistic timelines for symptom improvement to support adherence.
- Monitor for sedation, weight gain, and metabolic changes while on antipsychotic therapy.
The nurse reviewing a patient’s medication list recognized which one as the antipsychotic?
Explanation
Antipsychotic medications, such as olanzapine, are used to treat psychotic disorders including schizophrenia and bipolar disorder by modulating dopamine and serotonin neurotransmission. Nurses must be able to identify antipsychotic agents to monitor for therapeutic effects, prevent adverse reactions, and provide accurate patient teaching regarding side effects and safety precautions.
Rationale for correct answer:
C. Olanzapine (Zyprexa)
This is an atypical antipsychotic that targets both dopamine and serotonin receptors, reducing positive symptoms like hallucinations and delusions, as well as some negative symptoms such as social withdrawal. Monitoring for weight gain, metabolic syndrome, and sedation is important during therapy.
Rationale for incorrect answer:
A. Lithium carbonate
Lithium is a mood stabilizer, primarily used in bipolar disorder, and does not directly treat psychotic symptoms. Its mechanism involves modulating neurotransmission, but it is not classified as an antipsychotic.
B. Sertraline (Zoloft)
Sertraline is a selective serotonin reuptake inhibitor (SSRI) used to treat depression and anxiety disorders. It is not an antipsychotic and does not target dopamine pathways involved in psychosis.
D. Amitriptyline (Elavil)
Amitriptyline is a tricyclic antidepressant used for depression and chronic pain, not for psychotic disorders. It affects norepinephrine and serotonin reuptake, not dopamine pathways.
Take-home points:
- Olanzapine is an atypical antipsychotic used for schizophrenia and bipolar disorder.
- Monitor for metabolic changes, sedation, and weight gain during therapy.
- Be able to differentiate antipsychotics from mood stabilizers and antidepressants for safe patient management.
The nurse knows that the patient in the scenario who has schizophrenia will need to have their medication dose adjusted if they develop which of the following?
Explanation
Patients with schizophrenia may require medication dose adjustments if they report a perceived loss of efficacy, as this may indicate tolerance, subtherapeutic dosing, or nonadherence. Nurses play a critical role in assessing symptom recurrence, monitoring side effects, and collaborating with prescribers to optimize antipsychotic therapy while ensuring patient safety.
Rationale for correct answer:
D. The sense that the medications do not work anymore
This may indicate tolerance, suboptimal plasma levels, or nonadherence. It signals the need for reassessment of dosage, medication type, or adherence strategies to ensure continued symptom control.
Rationale for incorrect answer:
A. Significant weight gain
While weight gain is a common adverse effect of antipsychotics, it does not automatically require a dose adjustment. Management usually focuses on lifestyle interventions, dietary counseling, and monitoring metabolic parameters.
B. Delusions that they are perceived as being controlled by radio waves
This represents ongoing psychotic symptoms, but the presence of delusions alone does not necessarily indicate a need for a dose change unless symptoms are worsening or not controlled with the current regimen.
C. Loss of their sense of taste and smell
Changes in taste or smell are not typical indicators for adjusting antipsychotic dosing. These sensory alterations are usually unrelated to drug efficacy.
Take-home points:
- Patient-reported loss of medication efficacy is a key indicator for reassessment.
- Dose adjustments should be considered only after evaluating adherence, drug interactions, and therapeutic levels.
- Ongoing monitoring and collaboration with the prescriber optimize treatment outcomes.
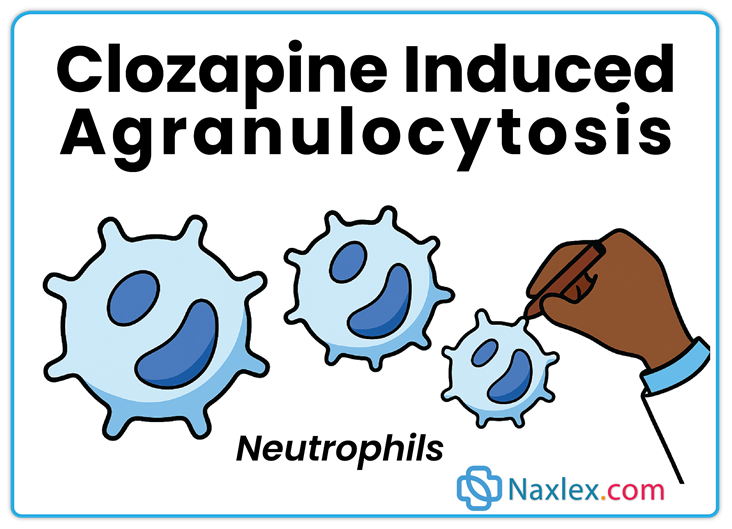
The nurse is caring for a patient who has been taking clozapine (Clozaril) for 2 months. Which laboratory test(s) should be performed regularly while the patient is taking this medication?
Explanation
Clozapine (Clozaril) is an atypical antipsychotic with a well-documented risk of agranulocytosis, a potentially life-threatening decrease in white blood cells (WBCs). Regular monitoring of WBC count is essential for early detection of this adverse effect and for ensuring patient safety during ongoing therapy. Nursing care includes educating the patient about infection signs and emphasizing the importance of adherence to scheduled lab testing.
Rationale for correct answer:
B. WBC count: Clozapine can cause agranulocytosis, which increases the patient’s risk for serious infections. Regular WBC monitoring is critical to detect decreases early and prevent complications. This includes baseline testing and weekly or biweekly checks during initial therapy, with gradual spacing as stability is achieved.
Rationale for incorrect answer:
A. Platelet count: While important for general hematologic monitoring, clozapine specifically affects WBCs, not platelets, so routine platelet checks are not the primary safety measure.
C. Liver function studies: Liver function may be monitored periodically, but hepatotoxicity is less common and not the primary concern with clozapine.
D. Renal function studies: Clozapine is not nephrotoxic, and routine renal monitoring is not a standard requirement for safety.
Take-home points:
- Clozapine carries a high risk of agranulocytosis; WBC monitoring is essential.
- Patients should report fever, sore throat, or signs of infection immediately.
- Monitoring schedules typically start weekly and may become less frequent if counts remain stable.
Which of the following second-generation antipsychotics is considered most effective for treatment-resistant schizophrenia and requires strict hematologic monitoring?
Explanation
Clozapine is a second-generation (atypical) antipsychotic reserved for treatment-resistant schizophrenia when other antipsychotics have failed. It has a superior efficacy for reducing both positive and some negative symptoms, but carries a risk of agranulocytosis, requiring strict and regular monitoring of white blood cell (WBC) and absolute neutrophil counts. Nurses must educate patients on signs of infection and ensure adherence to blood monitoring schedules to safely use this medication.
Rationale for correct answer:
B. Clozapine: Reserved for patients unresponsive to other antipsychotics; the risk of agranulocytosis necessitates weekly WBC monitoring initially, then biweekly/monthly, making monitoring and patient education essential.
Rationale for incorrect answers:
A. Risperidone: Effective for schizophrenia but not the first choice for treatment-resistant cases and does not require the same intensive hematologic monitoring.
C. Olanzapine: Effective for positive and negative symptoms but less potent than clozapine for treatment-resistant cases and does not carry the same severe risk of blood dyscrasias.
D. Ziprasidone: Less effective for treatment-resistant schizophrenia and mainly monitored for cardiac effects (QT prolongation) rather than hematologic complications.
Take-home points:
- Clozapine is the most effective antipsychotic for treatment-resistant schizophrenia.
- Strict hematologic monitoring is mandatory to detect agranulocytosis early.
- Patient education on infection signs and adherence to blood tests is crucial for safe therapy.
A patient with a feeding tube will be receiving risperidone (Risperdal) 8 mg in two divided doses via the feeding tube. The medication is available in a 1 mg/mL solution. How many milliliters will the nurse administer for each dose?
Explanation
Determine the dose for each administration:
The total daily dose is 8 mg, which is to be divided into two equal doses.
8mg divide by 2 is 4mg
Calculate the volume to be administered for each dose:
The concentration of the medication is 1 mg/mL. To find the volume in milliliters (mL) for the 4 mg dose, you can use the following formula:
Volume to be administered = Prescribed dose ÷ Concentration of the solution
The prescribed dose is 4 mg.
The concentration is 1 mg/mL.
Calculation: 4 divide by 1 is 4
The volume to be administered is 4 mL.
Take-home points:
- Always determine the individual dose to be given at each administration time.
- Use the "Prescribed dose ÷ Concentration of the solution" formula to calculate the Volume.
- Double-check the total dose, the number of divided doses, and the medication's concentration to avoid any errors.
Nursing implications of the administration of haloperidol (Haldol) to a client exhibiting psychotic behavior include which of the following? Select all that apply.
Explanation
When administering haloperidol (Haldol) to a client with psychotic behavior, the nurse must be vigilant for specific precautions due to the drug’s high risk of extrapyramidal symptoms (EPS) and other significant side effects. Understanding safe administration timing, contraindications, and monitoring needs helps prevent complications and promotes therapeutic outcomes.
Rationale for correct answer:
A. Take 1 hour before or 2 hours after antacids. Antacids can reduce the absorption of haloperidol, potentially decreasing therapeutic effects. Separating administration times ensures optimal drug bioavailability.
B. The incidence of EPS is high. Haloperidol is a high-potency first-generation antipsychotic, and its strong dopamine blockade in the basal ganglia makes EPS symptoms—such as dystonia, akathisia, and pseudo-parkinsonism—more likely. Early detection allows prompt intervention.
D. Haldol is contraindicated in Parkinson’s disease, seizure disorders, alcoholism, and severe mental depression. Dopamine blockade can worsen Parkinson’s disease symptoms, lower seizure threshold, and exacerbate CNS depression, making these conditions unsafe for use.
Rationale for incorrect answer:
C. It is therapeutic if ordered on an as-needed (PRN) basis. PRN dosing is generally not recommended for maintenance therapy in psychotic disorders because steady plasma levels are essential for symptom control. Inconsistent use increases relapse risk.
E. Crush the sustained-release form for easier swallowing. Sustained-release tablets should not be crushed, as doing so alters the pharmacokinetics and may lead to rapid release, toxicity, or loss of prolonged effect.
Take-home points:
- Haloperidol carries a high EPS risk, requiring close monitoring.
- Administration timing in relation to antacids is essential for drug absorption.
- Know contraindications to avoid worsening underlying health conditions.
A nurse is preparing to perform a follow-up assessment on a client who takes chlorpromazine (Thorazine) for the treatment of schizophrenia. The nurse should expect to find the greatest improvement in which of the following manifestations? Select all that apply.
Explanation
Chlorpromazine (Thorazine) is a first-generation antipsychotic primarily effective for positive symptoms of schizophrenia, which are those that represent an excess or distortion of normal function. Positive symptoms include hallucinations, delusions, disorganized thinking, and bizarre behavior. Nurses should focus assessments on improvement in these areas to evaluate therapeutic effectiveness.
Rationale for correct answer:
A. Disorganized speech – First-generation antipsychotics help clarify thought processes and reduce incoherent or tangential speech, improving communication and cognitive clarity.
B. Bizarre behavior – Chlorpromazine targets agitation, inappropriate social behavior, and unusual motor activity, helping normalize behavioral patterns.
D. Hallucinations – Positive symptoms like auditory and visual hallucinations are significantly reduced, which improves client safety and insight into reality.
Rationale for incorrect answer:
C. Impaired social interactions – Social withdrawal is a negative symptom and often shows limited improvement with first-generation antipsychotics. These symptoms may require psychosocial interventions or second-generation antipsychotics for better response.
E. Decreased motivation – This is a negative symptom (avolition) that does not respond well to first-generation antipsychotics and often persists despite treatment.
Take-home points:
- First-generation antipsychotics are most effective for positive symptoms of schizophrenia.
- Negative symptoms such as social withdrawal and decreased motivation may persist despite therapy.
- Nursing assessments should focus on reduction in hallucinations, disorganized speech, and bizarre behavior to gauge effectiveness.
An atypical antipsychotic is prescribed for a patient with psychosis. The nurse understands that this category of medications includes which drugs? Select all that apply.
Explanation
Atypical antipsychotics, also known as second-generation antipsychotics, are commonly prescribed to treat psychotic disorders, including schizophrenia and bipolar disorder. These medications work by blocking dopamine and serotonin receptors, which helps reduce both positive and negative symptoms of psychosis while generally causing fewer extrapyramidal symptoms compared to first-generation antipsychotics. Nurses must monitor clients for therapeutic effects, metabolic changes, and other adverse reactions when administering these drugs.
Rationale for correct answer:
A. clozapine (Clozaril): Clozapine is a second-generation antipsychotic that blocks dopamine and serotonin receptors. It is effective for treatment-resistant schizophrenia and helps reduce hallucinations and delusions. Monitoring for agranulocytosis is essential.
D. olanzapine (Zyprexa): Atypical antipsychotic that acts on dopamine and serotonin receptors, helping reduce psychotic symptoms and improve mood. Metabolic monitoring is required due to risks of weight gain, diabetes, and dyslipidemia.
E. aripiprazole (Abilify): Atypical antipsychotic with a partial dopamine agonist effect, useful for schizophrenia, bipolar disorder, and as an adjunct in depression. It has a lower risk of EPS but still requires monitoring for akathisia and metabolic changes.
Rationale for incorrect answer:
B. fluphenazine (Prolixin): This is a first-generation antipsychotic. It primarily blocks dopamine and is associated with a higher risk of extrapyramidal symptoms and tardive dyskinesia, making it distinct from atypical antipsychotics.
C. haloperidol (Haldol): Also a first-generation antipsychotic, haloperidol is potent for positive symptoms of psychosis but carries a significant risk of EPS and neuroleptic malignant syndrome, unlike atypical agents.
Take-home points:
- Atypical antipsychotics treat both positive and negative symptoms of psychosis while generally causing fewer motor side effects.
- Metabolic monitoring is essential due to risks of weight gain, hyperglycemia, and dyslipidemia.
- First-generation antipsychotics (fluphenazine, haloperidol) primarily target dopamine and have a higher risk of extrapyramidal side effects.
Comprehensive Questions
The client states that he has not taken his antipsychotic drug for the past 2 weeks because it was causing sexual dysfunction. What is the nurse’s primary concern at this time?
Explanation
When a patient abruptly stops taking an antipsychotic medication, the therapeutic dopamine blockade is lost, often leading to a rapid recurrence of hallucinations, delusions, and disorganized thinking. The nurse’s priority is to address and prevent relapse of psychosis to ensure safety.
Rationale for correct answer:
D. Symptoms of psychosis are likely to return.
Stopping antipsychotics abruptly can cause rapid reemergence or worsening of psychotic symptoms, greatly increasing the risk of self-harm or harm to others. Immediate intervention is vital to maintain mental stability.
Rationale for incorrect answer:
A. A hypertensive crisis may occur with such abrupt withdrawal of the drug.
Hypertensive crisis is mainly linked to monoamine oxidase inhibitors (MAOIs), not antipsychotics, so it is not the primary concern.
B. Significant muscle twitching may occur, increasing fall risk.
Muscle twitching is not a common withdrawal effect of antipsychotics and is less urgent than psychosis relapse.
C. EPS symptoms such as pseudo-parkinsonism are likely to occur.
Extrapyramidal symptoms are usually a side effect during ongoing therapy, not after discontinuation.
Take-home points:
- Abrupt cessation of antipsychotics can trigger psychotic relapse.
- The nurse’s priority is patient safety and symptom management.
- Hypertensive crisis is not associated with antipsychotic withdrawal.
Prior to discharge, the nurse plans for client teaching related to side effects of phenothiazines to the client, family, or caregiver. Which of the following should be included?
Explanation
Phenothiazines, a class of first-generation antipsychotics, can cause acute dystonia early in treatment. This is a type of extrapyramidal symptom (EPS) characterized by severe, involuntary muscle spasms that may affect the neck, face, tongue, or back, and require prompt medical attention.
Rationale for correct answer:
B. Severe muscle spasms may occur early in therapy.
Acute dystonic reactions are a known early adverse effect, often appearing within hours to days of starting phenothiazines. Education should stress reporting these symptoms immediately, as they can compromise breathing or swallowing.
Rationale for incorrect answer:
A. The client may experience withdrawal and slowed activity.
Phenothiazines more commonly cause sedation, not withdrawal-like symptoms, and this is not the most urgent teaching point before discharge.
C. Tardive dyskinesia is likely early in therapy.
Tardive dyskinesia usually develops after months to years of therapy, not in the early stages.
D. Medications should be taken as prescribed to prevent adverse effects.
While adherence is important, this statement does not address a specific high-priority side effect for early treatment.
Take-home points:
- Acute dystonia can occur within the first days of phenothiazine use.
- Early recognition and reporting of muscle spasms is critical to prevent complications.
- Tardive dyskinesia develops later, not at the start of therapy.
A 20-year-old man is admitted to the psychiatric unit for treatment of acute schizophrenia and is started on risperidone (Risperdal). Which client effects should the nurse assess for to determine whether the drug is having therapeutic effects?
Explanation
Risperidone is a second-generation antipsychotic used to treat schizophrenia by blocking dopamine D2 and serotonin 5-HT2 receptors. The primary goal of therapy is the reduction of positive symptoms such as hallucinations, delusions, and disorganized thinking, which are most distressing in acute episodes.
Rationale for correct answer:
B. Decreased delusional thinking and lessened auditory/visual hallucinations.
This is the main therapeutic effect of risperidone in schizophrenia. Improvement in positive symptoms indicates the drug is effectively modulating dopamine activity in the mesolimbic pathway.
Rationale for incorrect answer:
A. Restful sleep, elevated mood, and coping abilities.
These outcomes are more associated with treatment of mood disorders such as depression or bipolar disorder, not the primary therapeutic goal for acute schizophrenia.
C. Orthostatic hypotension, reflex tachycardia, and sedation.
These are adverse effects, not therapeutic outcomes. While important to monitor, they do not reflect whether the drug is achieving its intended purpose.
D. Relief of anxiety and improved sleep and dietary habits.
These effects may occur secondarily but are not primary indicators of antipsychotic therapeutic effectiveness.
Take-home points:
- Risperidone’s main goal in schizophrenia is to reduce positive symptoms like hallucinations and delusions.
- Symptom improvement is the best measure of therapeutic success, not the absence of side effects.
- Adverse effects such as orthostatic hypotension must still be monitored but do not confirm drug effectiveness.
A client is treated for psychosis with fluphenazine. What drug will the nurse anticipate to given to prevent the development of acute dystonia?
Explanation
When clients are treated for psychosis with first-generation antipsychotics like fluphenazine, there is an increased risk of developing extrapyramidal symptoms (EPS), particularly acute dystonia in the early stages of therapy. Nurses must anticipate prophylactic measures, including the use of specific medications to prevent or manage these symptoms, to ensure patient safety and comfort during antipsychotic treatment.
Rationale for correct answer:
A. Benztropine (Cogentin) – Anticholinergic medications like benztropine are frequently prescribed to prevent or treat EPS, including acute dystonia caused by dopamine blockade in the nigrostriatal pathway. By restoring the dopamine-acetylcholine balance in the CNS, benztropine helps reduce muscle rigidity, spasms, and abnormal postures that can occur shortly after initiating antipsychotic therapy.
Rationale for incorrect answer:
B. Diazepam (Valium) – This benzodiazepine is primarily used for anxiety, muscle relaxation, and seizure control, not for preventing EPS. While it may reduce anxiety related to symptoms, it does not address the underlying neurotransmitter imbalance that causes acute dystonia.
C. Haloperidol (Haldol) – Another first-generation antipsychotic, haloperidol can actually increase the risk of EPS, making it inappropriate for prevention. Administering it alongside fluphenazine could worsen movement-related side effects.
D. Lorazepam (Ativan) – This benzodiazepine can help relieve agitation or anxiety in psychotic patients, but it does not prevent acute dystonia because it does not correct the dopamine-acetylcholine imbalance in the basal ganglia.
Take-home points:
- Benztropine is the drug of choice for preventing acute dystonia caused by high-potency first-generation antipsychotics.
- Acute dystonia is an early-onset EPS that can occur within hours to days of starting antipsychotic therapy.
- Prevention is important because untreated acute dystonia can cause airway compromise or severe discomfort.
The nurse should immediately report the development of which of the following symptoms in a client taking antipsychotic medication?
Explanation
Clients on antipsychotic medications are at risk for both common and life-threatening adverse effects. While many side effects are uncomfortable but manageable, the sudden onset of certain symptoms may indicate a medical emergency such as neuroleptic malignant syndrome (NMS), which requires immediate intervention to prevent serious complications or death.
Rationale for correct answer:
A. Fever, tachycardia, confusion, incontinence – These symptoms suggest neuroleptic malignant syndrome, a rare but potentially fatal reaction to antipsychotics. NMS is characterized by hyperthermia, autonomic instability, altered mental status, and severe muscle rigidity. Immediate discontinuation of the drug, rapid medical management, and supportive care are critical.
Rationale for incorrect answer:
B. Pacing, squirming, or difficulty with gait such as bradykinesia – These are signs of akathisia or drug-induced parkinsonism, which are types of extrapyramidal symptoms (EPS). While uncomfortable and requiring prompt treatment, they are not typically life-threatening emergencies.
C. Severe spasms of the muscles of the tongue, face, neck, or back – This describes acute dystonia, an early-onset EPS that can be distressing and potentially dangerous if airway muscles are involved, but it is generally managed quickly with anticholinergic medications like benztropine or diphenhydramine.
D. Sexual dysfunction or gynecomastia – These are related to endocrine side effects from increased prolactin levels. They are bothersome and may affect adherence but are not medical emergencies.
Take-home points:
- NMS is a life-threatening complication of antipsychotic therapy and must be recognized early.
- Key warning signs include hyperthermia, autonomic instability, altered mental status, and muscle rigidity.
- Immediate drug discontinuation and emergency medical care are essential for survival.
A nurse is teaching a client who has schizophrenia strategies to cope with anticholinergic effects of fluphenazine. Which of the following should the nurse suggest to the client to minimize anticholinergic effects?
Explanation
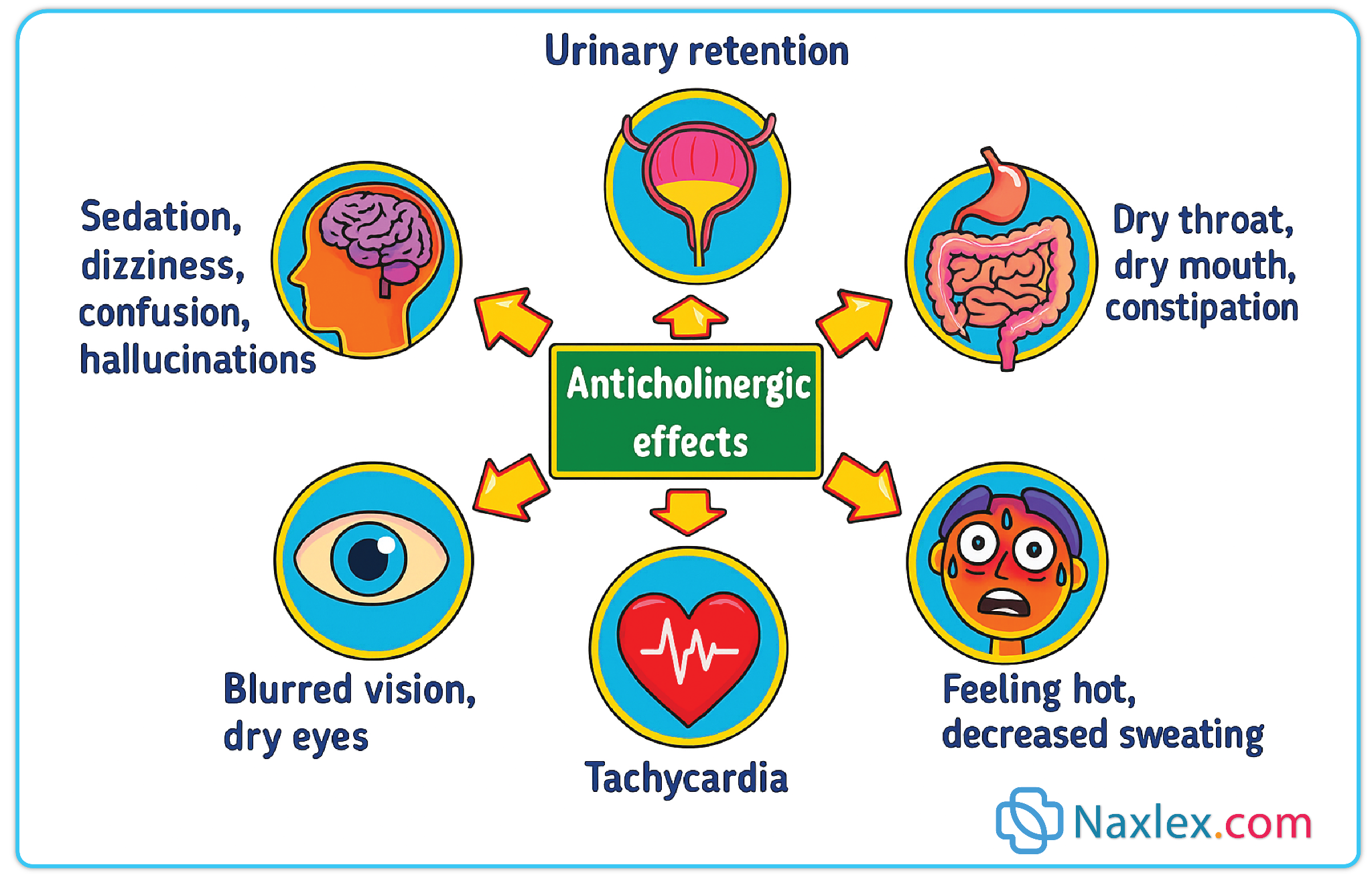
Many antipsychotic medications, such as fluphenazine, have anticholinergic side effects due to their blockade of muscarinic receptors. These effects—dry mouth, blurred vision, constipation, and urinary retention—can significantly impact comfort and adherence. Nurses play a key role in teaching clients self-care strategies to reduce these symptoms and maintain compliance with therapy.
Rationale for correct answer:
B. Chew sugarless gum to moisten the mouth – Dry mouth is a common anticholinergic effect of fluphenazine. Chewing sugarless gum stimulates salivary flow, helping to moisten the oral mucosa and prevent dental problems. This is an effective, nonpharmacologic coping strategy.
Rationale for incorrect answer:
A. Take the medication in the morning to prevent insomnia – Fluphenazine is more likely to cause sedation than insomnia. Adjusting the time of administration does not address anticholinergic effects such as dry mouth.
C. Use cooling measures to decrease fever – While anticholinergic drugs can reduce sweating and theoretically contribute to heat intolerance, fever is not the most common issue. Cooling measures are not a primary intervention for typical anticholinergic effects in this context.
D. Take an antacid to relieve nausea – Antacids are not indicated for anticholinergic effects. In addition, they can interfere with the absorption of some oral medications, including certain antipsychotics.
Take-home points:
- Anticholinergic effects of fluphenazine include dry mouth, constipation, urinary retention, and blurred vision.
- Nonpharmacologic interventions, such as chewing sugarless gum or sipping water, can improve comfort and adherence.
- Client education should focus on practical, daily strategies to manage side effects without introducing unnecessary medications.
A nurse is assessing a male client who recently began taking haloperidol (Haldol). Which of the following findings is the highest priority to report to the provider?
Explanation
Correct answer: 2
Haloperidol, a first-generation antipsychotic, can cause extrapyramidal symptoms (EPS), including acute dystonia, parkinsonism, akathisia, and tardive dyskinesia. Among these, acute dystonic reactions, such as neck spasms, are a high-priority finding because they can rapidly progress to laryngeal dystonia, compromising the airway. Prompt recognition and treatment are essential to prevent life-threatening complications.
Rationale for correct answer:
B. Neck spasms – Neck spasms may be a sign of acute dystonia, a severe EPS that can develop within hours or days of starting antipsychotic therapy. It may involve muscles of the neck, tongue, and larynx, leading to airway obstruction. This is an urgent condition requiring immediate treatment with an anticholinergic agent such as benztropine or diphenhydramine.
Rationale for incorrect answer:
A. Shuffling gait – This finding indicates parkinsonism, an EPS that can occur with haloperidol. While it requires intervention, it does not pose an immediate threat to life like acute dystonia does.
C. Drowsiness – Sedation is a common side effect of haloperidol but is not life-threatening. Monitoring and dose adjustments can address this over time.
D. Impotence – Sexual side effects are possible with haloperidol but are not urgent or dangerous. They can be addressed during routine follow-up.
Take-home points:
- Acute dystonia from haloperidol can be life-threatening if it affects respiratory muscles.
- Early signs include neck stiffness, facial grimacing, and abnormal tongue movements.
- Immediate treatment with parenteral anticholinergics is essential to prevent airway compromise.
A nurse is providing discharge teaching for a client who has a new prescription for clozapine (Clozaril). Which of the following statements is appropriate for the nurse to include in the teaching?
Explanation
Clozapine is an atypical antipsychotic reserved for treatment-resistant schizophrenia due to its superior efficacy but significant risk profile. Its most serious adverse effect is agranulocytosis, a potentially life-threatening drop in white blood cells that severely compromises the immune system. Strict hematologic monitoring is mandatory to detect early changes and prevent severe infection.
Rationale for correct answer:
D. “You should have your white blood cell count monitored every week.” – This is essential because clozapine can cause agranulocytosis, often within the first 6 months of treatment. Weekly WBC and ANC monitoring is required at treatment initiation to ensure early detection and prompt discontinuation if levels drop dangerously.
Rationale for incorrect answer:
A. “You should have a high-carbohydrate snack between meals and at bedtime.” – Clozapine can cause weight gain and metabolic changes, so increased carbohydrate intake would worsen these effects rather than help. Dietary guidance should focus on balanced nutrition and weight control.
B. “You are likely to develop hand tremors if you take this medication for a long period of time.” – Tremors are more commonly linked to first-generation antipsychotics and some atypicals, but they are not a hallmark risk of clozapine. EPS incidence is generally lower with clozapine compared to conventional antipsychotics.
C. “You may experience temporary numbness of your mouth after each dose.” – Oral numbness is not a typical side effect of clozapine. Notable adverse effects include sedation, weight gain, hypersalivation, seizures, myocarditis, and agranulocytosis.
Take-home points:
- Clozapine requires weekly blood monitoring initially due to agranulocytosis risk.
- Signs of infection (fever, sore throat) must be reported immediately.
- Weight gain, sedation, and hypersalivation are common non-life-threatening side effects.
A nurse performs an Abnormal Involuntary Movement Scale (AIMS) assessment on a client who began taking loxapine 2 years ago for the treatment of schizophrenia. Findings include lip smacking, tongue protrusion, and facial grimacing. The nurse should suspect which of the following?
Explanation
Tardive dyskinesia (TD) is a late-onset, potentially irreversible movement disorder associated with long-term use of first-generation antipsychotics like loxapine. It is characterized by involuntary, repetitive movements, particularly of the face, lips, tongue, and sometimes the extremities. Regular monitoring using the Abnormal Involuntary Movement Scale (AIMS) is crucial for early detection and intervention.
Rationale for correct answer:
B. Tardive dyskinesia – Correct. TD often develops after months to years of antipsychotic therapy. The hallmark signs include lip smacking, tongue protrusion, chewing motions, and facial grimacing, matching the client’s AIMS findings. Early detection is important, as symptoms may become irreversible if the drug is continued.
Rationale for incorrect answer:
A. Parkinsonism – Typically presents with rigidity, bradykinesia, and tremors, resembling Parkinson’s disease. These symptoms usually appear early in treatment, not after long-term use.
C. Anticholinergic effects – These include dry mouth, blurred vision, constipation, and urinary retention. They do not explain the involuntary facial and tongue movements observed in this client.
D. Akathisia – Characterized by inner restlessness, inability to sit still, and pacing, typically occurring shortly after starting or increasing antipsychotic therapy. The client’s symptoms are distinctly involuntary movements, not restlessness.
Take-home points:
- Tardive dyskinesia is a late-onset, often irreversible adverse effect of long-term antipsychotic therapy.
- Regular AIMS assessments are essential for early detection and intervention.
- Prompt reporting of symptoms can guide the provider in adjusting therapy to prevent progression.
The nurse suspects that a patient who is experiencing facial grimacing, involuntary upward eye movement, and muscle spasms of the tongue and face may have which condition?
Explanation
Acute dystonia is an extrapyramidal side effect (EPS) that can occur soon after starting or increasing the dose of antipsychotic medications, particularly first-generation agents. It is characterized by sustained muscle contractions that can affect the face, neck, tongue, and eyes, potentially causing significant discomfort and posing a risk for airway compromise. Prompt recognition and intervention are essential to prevent complications.
Rationale for correct answer:
B. Acute dystonia – Correct. This condition is marked by sudden, painful, involuntary muscle contractions, including facial grimacing, tongue protrusion, neck stiffness, and oculogyric crises (upward eye movement). Immediate treatment with anticholinergic agents such as benztropine or diphenhydramine is often required.
Rationale for incorrect answer:
A. Akathisia – Akathisia presents as restlessness, pacing, or an inability to sit still. It does not involve sustained muscle contractions or abnormal postures, making it distinct from acute dystonia.
C. Tardive dyskinesia – Tardive dyskinesia typically develops after months to years of antipsychotic therapy and involves slow, repetitive, involuntary movements, most commonly of the face and mouth, unlike the sudden onset seen in acute dystonia.
D. Pseudo-parkinsonism – This EPS mimics Parkinson’s disease, presenting with tremors, bradykinesia, rigidity, and shuffling gait, but does not include the acute, sustained muscle contractions seen in dystonia.
Take-home points:
- Acute dystonia is a sudden-onset EPS requiring prompt intervention.
- Facial grimacing, tongue spasms, and upward eye movement are hallmark signs.
- Treatment often involves anticholinergic medications and close monitoring for airway compromise.
A patient asks the nurse to explain how antipsychotic drugs work to make him feel better. The nurse understands that antipsychotics act in which way?
Explanation
Antipsychotic medications, particularly first-generation (typical) and many second-generation (atypical) agents, are primarily used to manage psychotic symptoms such as hallucinations, delusions, and disorganized thinking. Their main mechanism involves modulating neurotransmitter activity in the brain, especially by affecting dopamine pathways, which play a key role in regulating mood, cognition, and perception.
Rationale for correct answer:
A. Blocking actions of dopamine – Antipsychotics exert their therapeutic effect by blocking dopamine D2 receptors in the mesolimbic pathway, which reduces positive symptoms of psychosis such as hallucinations and delusions. Some atypical antipsychotics also target serotonin receptors, improving negative symptoms.
Rationale for incorrect answer:
B. Blocking actions of epinephrine – Epinephrine is involved in the fight-or-flight response and does not play a central role in psychotic symptom development. Blocking epinephrine would not relieve hallucinations or delusions.
C. Promoting prostaglandin synthesis – Prostaglandins are mediators of inflammation and pain, unrelated to the mechanism of antipsychotic drugs.
D. Enhancing the action of gamma-aminobutyric acid (GABA) – GABA enhancement is the mechanism of benzodiazepines and some sedative-hypnotics, not antipsychotics. It primarily produces CNS depression rather than antipsychotic effects.
An antipsychotic agent, fluphenazine (Prolixin), is ordered for a patient with psychosis. The nurse understands that this agent can lead to extrapyramidal symptoms that may be treated with which medication?
Explanation
Fluphenazine (Prolixin) is a first-generation (typical) antipsychotic commonly prescribed for schizophrenia and other psychotic disorders. These drugs are effective at controlling positive psychotic symptoms such as hallucinations and delusions, but they carry a significant risk of extrapyramidal symptoms (EPS) due to potent dopamine D2 receptor blockade in the nigrostriatal pathway.
Rationale for correct answer:
C. Benztropine (Cogentin) – Benztropine is an anticholinergic agent used specifically to treat EPS, including acute dystonia, parkinsonism, and akathisia. By restoring the balance between acetylcholine and dopamine in the CNS, it alleviates involuntary movements and muscle rigidity caused by dopamine blockade. Administering benztropine promptly can prevent progression of symptoms and reduce patient distress.
Rationale for incorrect answer:
A. Quetiapine (Seroquel) – This atypical antipsychotic has a lower risk of EPS and is not used to treat EPS caused by other antipsychotics. It primarily targets positive and negative symptoms of psychosis without reversing motor side effects.
B. Aripiprazole (Abilify) – Another second-generation antipsychotic, aripiprazole is not indicated for managing EPS. Its mechanism is a partial dopamine agonist, which does not reverse EPS caused by dopamine antagonists.
D. Chlorpromazine (Thorazine) – This is a typical antipsychotic that can also cause EPS. Using it would worsen extrapyramidal symptoms, making it inappropriate for treatment.
Take-home points:
- Benztropine is first-line therapy for EPS caused by typical antipsychotics.
- Early identification of EPS is crucial to prevent falls, injury, and medication nonadherence.
- Nurses should educate patients and caregivers to report involuntary movements promptly and monitor for both acute and long-term side effects.
Exams on Drugs Used for Psychoses
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Introduction
Psychoses
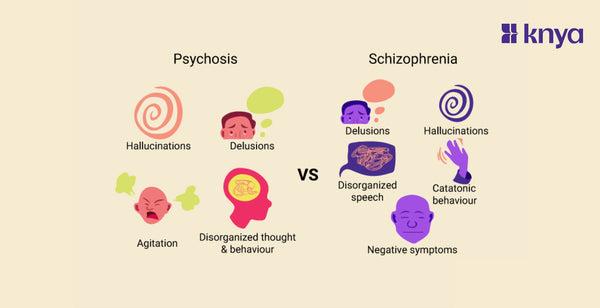
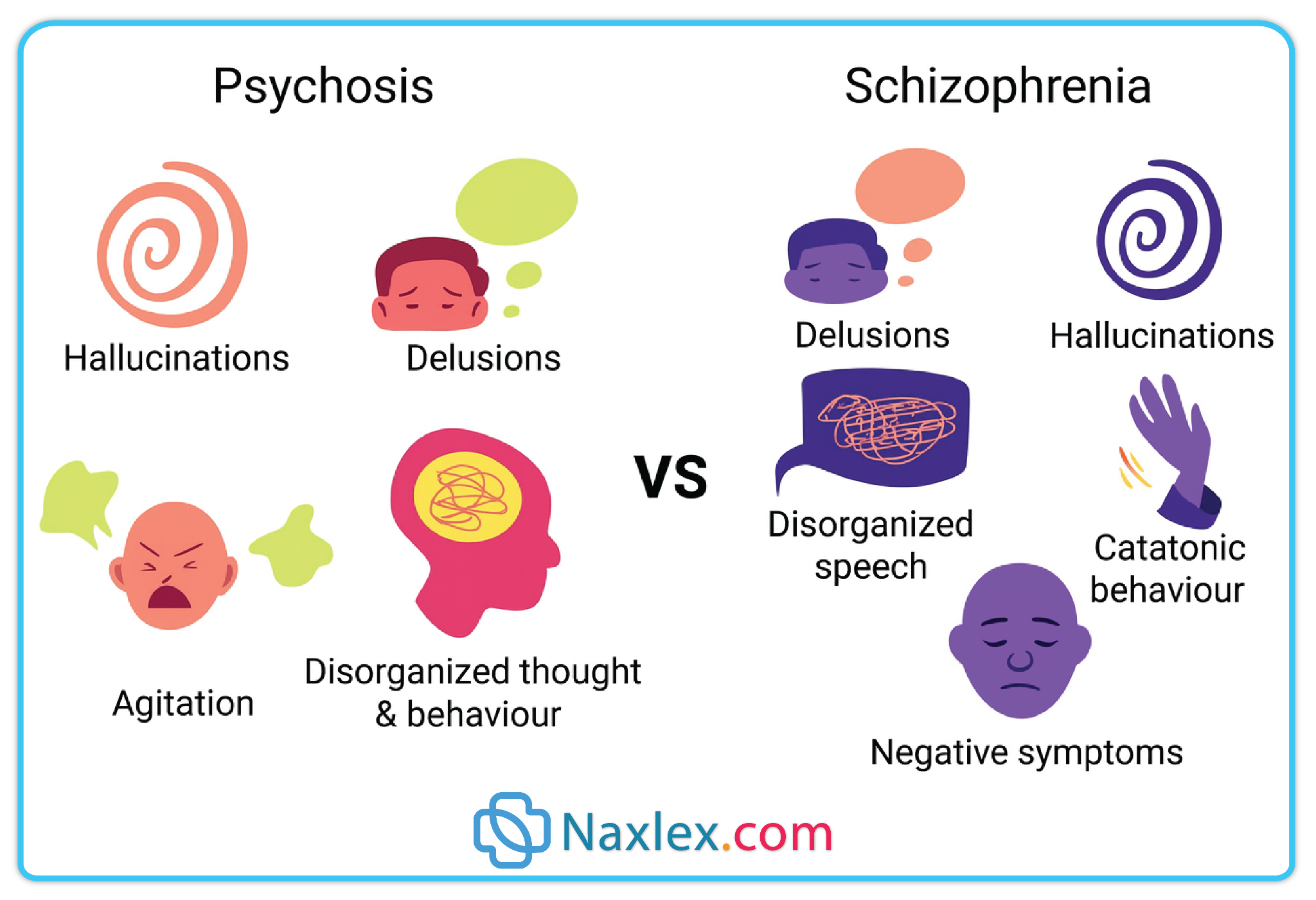
- Psychoses are a group of severe mental health disorders characterized by a loss of contact with reality, leading to disorganized thinking, distorted perceptions, abnormal emotions, and impaired judgment.
- The hallmark symptoms involve delusions (false fixed beliefs) and hallucinations (false sensory perceptions), often accompanied by disorganized speech, abnormal motor behavior, and social withdrawal.
- Can result from psychiatric disorders (e.g., schizophrenia, schizoaffective disorder, bipolar disorder with psychotic features).
- May also be secondary to medical conditions (e.g., brain tumors, dementia, endocrine disorders) or substance-induced (e.g., due to stimulants, hallucinogens, or withdrawal from certain drugs).
- The most common psychotic disorder is schizophrenia, which can be acute (sudden onset, often reversible) or chronic (long-term, persistent symptoms).
- Antipsychotics are medications designed to reduce psychotic symptoms, improve functional ability, and help patients integrate into community life.
- These drugs do not cure the underlying disease but control symptoms by altering dopamine and serotonin neurotransmission in the brain.
- They are divided into first-generation (typical) and second-generation (atypical) agents, each with distinct mechanisms, benefits, and side effect profiles.
Schizophrenia
Schizophrenia is the most well-known and extensively studied psychotic disorder. Nurses must understand its features thoroughly before exploring treatment options.
Definition
Schizophrenia is a chronic, severe mental disorder characterized by episodes of psychosis, disturbances in thought, perception, and behavior, and long-term functional impairment.
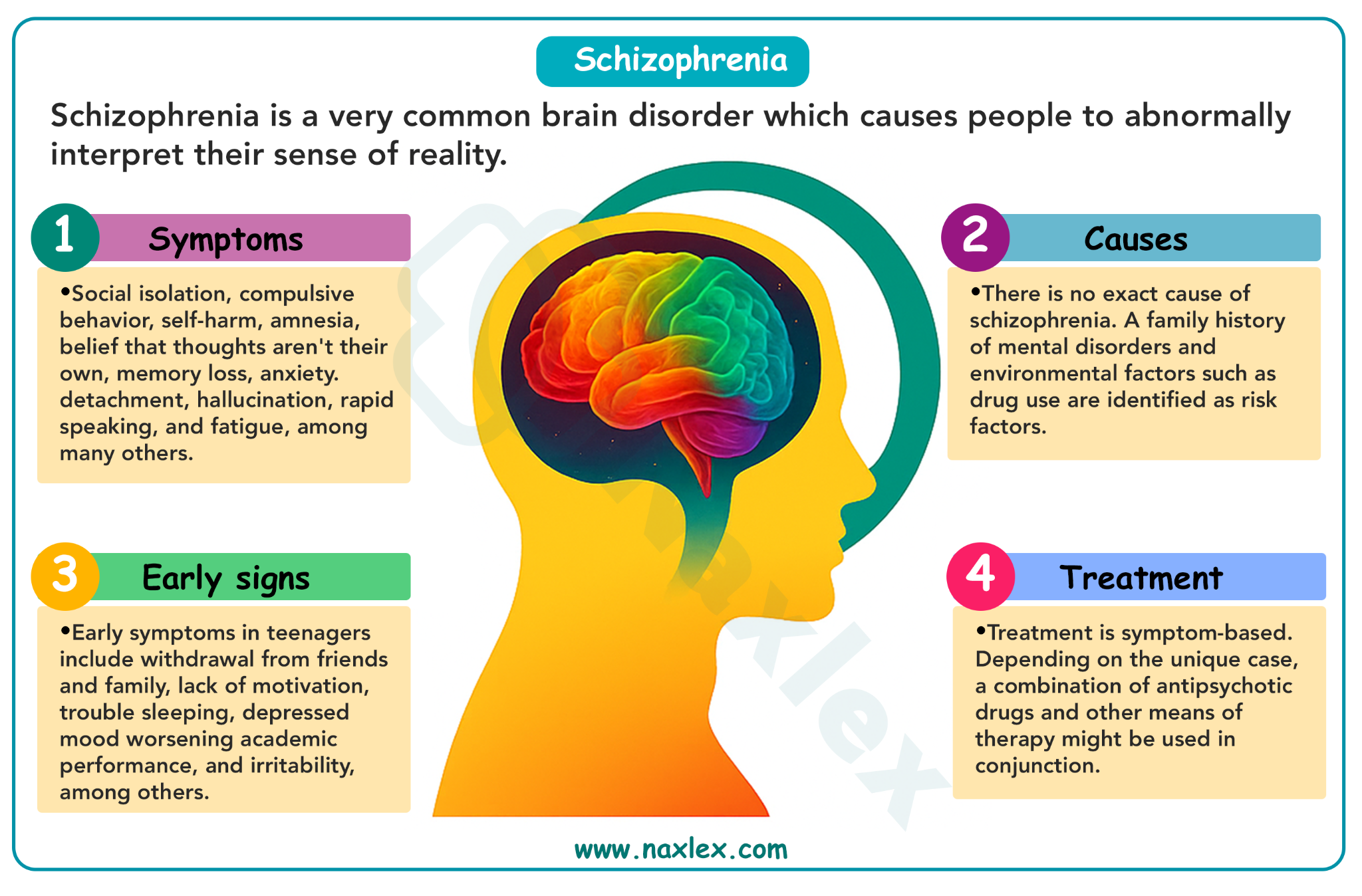
Epidemiology
- Affects approximately 1% of the population worldwide.
- Onset typically occurs in late adolescence to early adulthood (males often earlier than females).
Etiology & Risk Factors
- Genetic predisposition: Strong hereditary component.
- Neurodevelopmental factors: Abnormal brain structure and development.
- Neurochemical factors: Dopaminergic hyperactivity, serotonin and glutamate imbalances.
- Environmental triggers: Early life stress, trauma, drug use (especially cannabis, amphetamines), perinatal complications.
Clinical Features
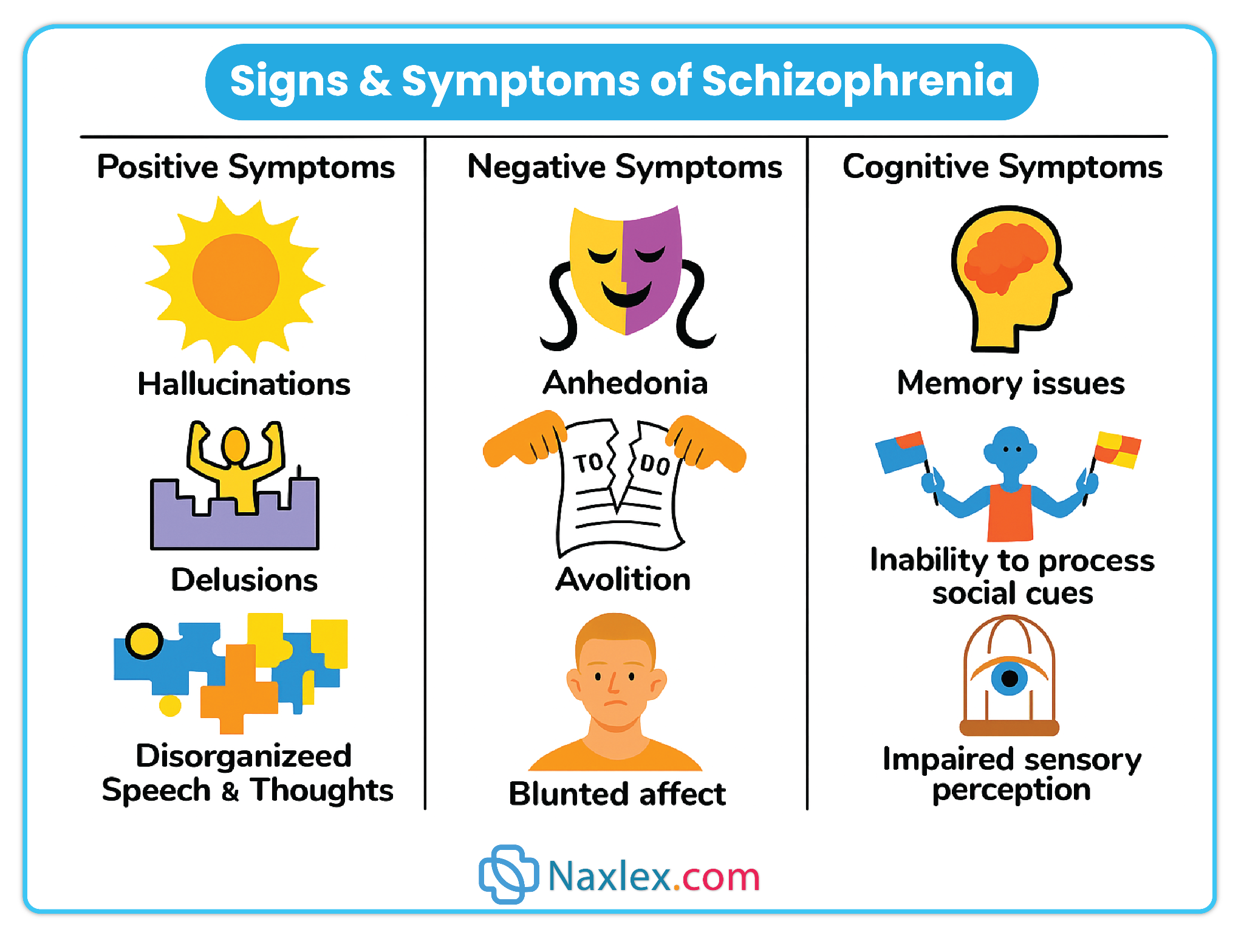
Schizophrenia is characterized by positive, negative, and cognitive symptoms:
- Positive symptoms (excess or distortion of normal function):
- Delusions (e.g., paranoid, grandiose, bizarre).
- Hallucinations (most commonly auditory).
- Disorganized speech and thought patterns.
- Grossly disorganized or catatonic behavior.
- Negative symptoms (loss or reduction of normal functions):
- Flat or blunted affect.
- Alogia (poverty of speech).
- Anhedonia (loss of pleasure).
- Avolition (lack of motivation).
- Social withdrawal.
- Cognitive symptoms:
- Impaired attention, memory, and executive function.
- Difficulty planning or completing tasks.
Course of Illness
- Chronic course with acute exacerbations and partial remissions.
- Functional outcomes vary; early intervention and adherence to treatment improve prognosis.
Nursing Insights
- Build trust through consistent, nonjudgmental communication.
- Ensure medication adherence — nonadherence is a major cause of relapse.
- Monitor for side effects of antipsychotics, including extrapyramidal symptoms (EPS), tardive dyskinesia, and metabolic changes.
- Encourage family involvement in care and psychoeducation.
- Promote social skills training and rehabilitation activities.
Antipsychotics
Antipsychotics are a class of medications used to manage the symptoms of psychotic disorders such as schizophrenia, schizoaffective disorder, and certain severe mood disorders.
These drugs work primarily by altering neurotransmitter activity in the brain, especially dopamine and serotonin, to reduce hallucinations, delusions, disorganized thinking, and agitation.
While they do not cure the underlying illness, antipsychotics help stabilize mood, improve thought processes, and enhance daily functioning, often forming the cornerstone of long-term management in combination with psychosocial therapies.
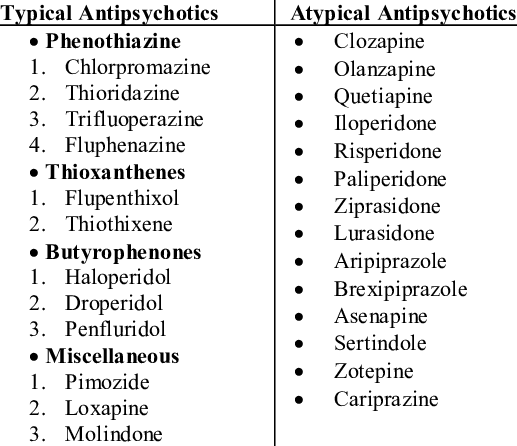
Classification of Antipsychotics
-
First-Generation Antipsychotics (FGAs)
- Also called typical antipsychotics.
- Primarily dopamine D2 receptor antagonists.
- Examples include:
- Chlorpromazine
- Haloperidol
- Fluphenazine
- Thioridazine
- Perphenazine
- Thiothixene
- Loxapine
- Second-Generation Antipsychotics (SGAs)
- Also called atypical antipsychotics.
- Block both dopamine D2 and serotonin 5-HT2A receptors.
- Examples include:
- Clozapine
- Risperidone
- Olanzapine
- Quetiapine
- Ziprasidone
- Aripiprazole
- Paliperidone
- Asenapine
- Lurasidone
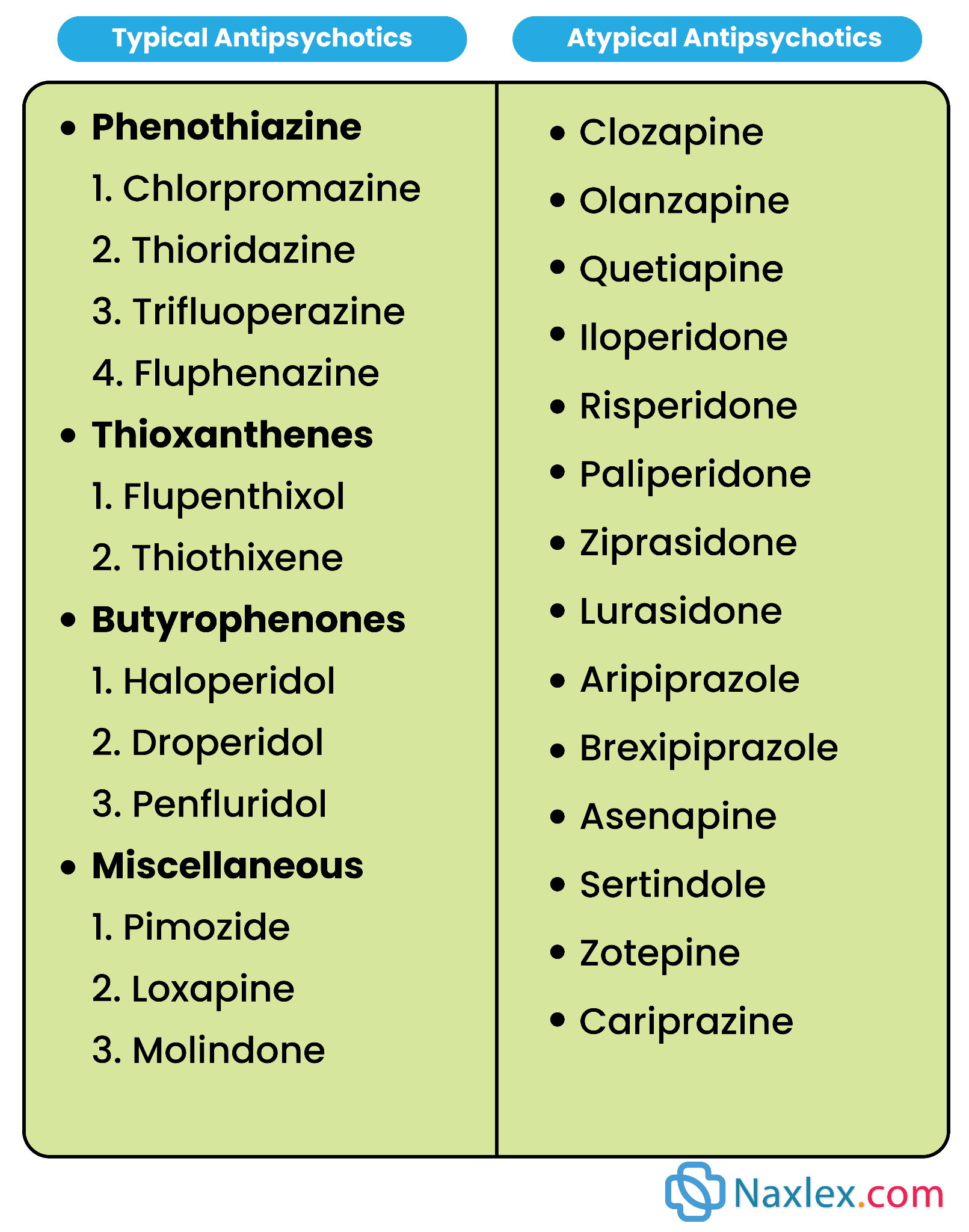
First-generation antipsychotics
First-generation antipsychotics (FGAs), also called typical antipsychotics, are a group of medications primarily used in the treatment of psychotic disorders, such as schizophrenia, schizoaffective disorder, delusional disorder, and in some cases, acute mania or severe agitation.
These medications were the first class of drugs developed to manage psychosis and have been in clinical use since the 1950s.
FGAs exert their therapeutic effects mainly by blocking dopamine D₂ receptors in the brain, especially in the mesolimbic pathway, which is thought to be overactive in psychosis.
By reducing dopamine activity in this pathway, FGAs alleviate positive symptoms such as hallucinations, delusions, and disorganized thinking.
However, because they also block dopamine in other pathways (nigrostriatal, mesocortical, tuberoinfundibular), they are associated with significant side effects, particularly extrapyramidal symptoms (EPS) and hyperprolactinemia.
Classification of First-Generation Antipsychotics
FGAs are commonly classified by potency, which refers to their affinity for dopamine receptors and the dose required to achieve therapeutic effects.
These drugs bind strongly to dopamine D₂ receptors and require lower doses for effect. They tend to produce more EPS but less sedation and fewer anticholinergic effects.
- Examples:
- Haloperidol (Haldol)
- Fluphenazine (Prolixin)
- Pimozide (Orap)
- Trifluoperazine (Stelazine)
These bind less tightly to D₂ receptors and require higher doses. They produce fewer EPS but more sedation, orthostatic hypotension, and anticholinergic effects.
- Examples:
- Chlorpromazine (Thorazine)
- Thioridazine (Mellaril)
- Mesoridazine (Serentil)
- Primary Action: FGAs block dopamine D₂ receptors in multiple brain pathways.
- Pathway Effects:
- Mesolimbic pathway: Reduces positive symptoms of psychosis (beneficial effect).
- Mesocortical pathway: May worsen negative symptoms and cognitive deficits in some patients due to further dopamine reduction.
- Nigrostriatal pathway: Dopamine blockade here causes extrapyramidal symptoms such as dystonia, parkinsonism, and akathisia.
- Tuberoinfundibular pathway: Dopamine blockade increases prolactin release, leading to hyperprolactinemia, which can cause galactorrhea, gynecomastia, and menstrual irregularities.
FGAs are used for:
- Schizophrenia – effective in managing positive symptoms.
- Acute psychotic episodes – rapid sedation and control of agitation.
- Mania in bipolar disorder – sometimes used for short-term control.
- Severe behavioral problems in children (off-label in some cases).
- Tourette’s syndrome – pimozide and haloperidol can reduce tics.
- Intractable hiccups – chlorpromazine is sometimes used.
- Delirium with severe agitation – in some controlled settings.
- Absorption: Well absorbed orally; intramuscular (IM) and intravenous (IV) forms available for acute management.
- Distribution: Lipophilic; widely distributed in tissues, including the brain.
- Metabolism: Primarily metabolized in the liver via CYP450 enzymes.
- Excretion: Metabolites excreted in urine and bile.
- Onset of Action: Sedative effects may occur within hours; antipsychotic effects usually require days to weeks for full benefit.
FGAs have a wide range of side effects, often related to dopamine blockade and interactions with other neurotransmitter systems.
1. Extrapyramidal Symptoms (EPS)
-
Acute Dystonia: Sudden, severe muscle spasms (neck, face, back); occurs within hours to days.
-
Parkinsonism: Tremor, rigidity, bradykinesia; develops within weeks.
-
Akathisia: Restlessness and inability to stay still; may occur within days to weeks.
-
Tardive Dyskinesia (TD): Involuntary repetitive movements (mouth, tongue, limbs); may be irreversible and develop after months to years.
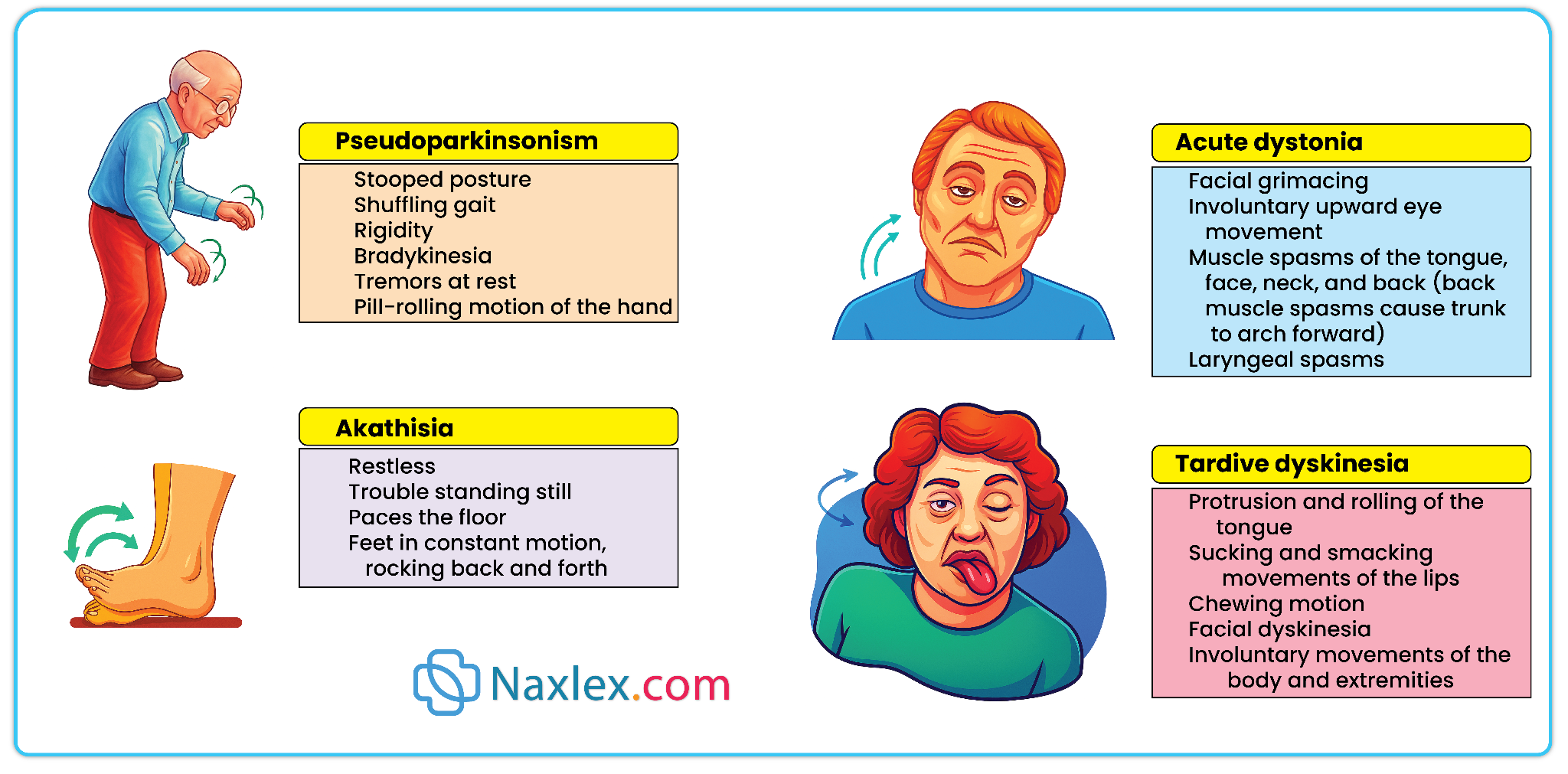
2. Neuroleptic Malignant Syndrome (NMS)
- Rare but life-threatening.
- Symptoms: Severe muscle rigidity, hyperthermia, altered mental status, autonomic instability.
- Requires immediate discontinuation of drug and emergency treatment.
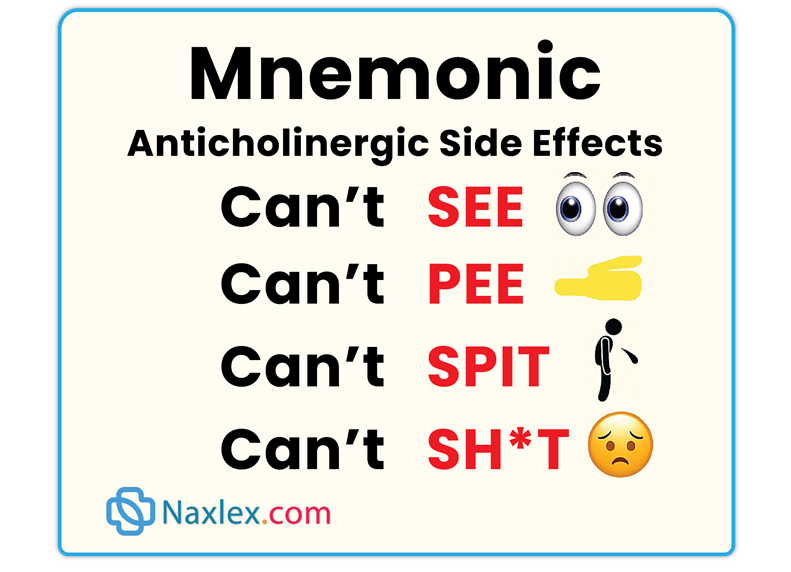
3. Anticholinergic Effects
- Dry mouth, blurred vision, constipation, urinary retention.
- More common with low-potency FGAs.
4. Cardiovascular Effects
- Orthostatic hypotension (especially with low-potency FGAs).
- QT prolongation (especially with thioridazine).
5. Endocrine Effects
- Hyperprolactinemia → galactorrhea, gynecomastia, amenorrhea, sexual dysfunction.
6. Sedation
- More pronounced with low-potency FGAs.
Assessment
- Obtain baseline mental status, vital signs, and ECG (especially if cardiac risk factors).
- Assess for history of EPS or movement disorders.
- Check baseline prolactin levels if indicated.
- Evaluate adherence potential and substance use history.
Diagnosis
- Risk for injury related to medication side effects (orthostatic hypotension, sedation, EPS).
- Disturbed thought processes related to psychosis.
- Nonadherence risk due to side effects.
Planning
- Set realistic goals for symptom control while minimizing side effects.
- Plan patient and family education regarding medication effects, expected onset, and side effect management.
Implementation
- Administer oral forms with food or milk to reduce GI upset.
- For IM injections, use deep gluteal site; long-acting depot forms available (haloperidol decanoate, fluphenazine decanoate).
- Titrate dose gradually to minimize side effects.
- Monitor for early signs of EPS and treat promptly (e.g., benztropine for dystonia).
Evaluation
- Improvement in positive symptoms (hallucinations, delusions).
- Tolerability of medication without severe adverse effects.
- Patient adherence to medication regimen.
- Explain that symptom improvement may take several weeks.
- Stress the importance of taking medication consistently.
- Advise about possible side effects and when to seek medical help (e.g., severe muscle stiffness, fever, irregular heartbeat).
- Caution about orthostatic hypotension – rise slowly from sitting/lying.
- Avoid alcohol and CNS depressants.
- Encourage reporting early signs of EPS.
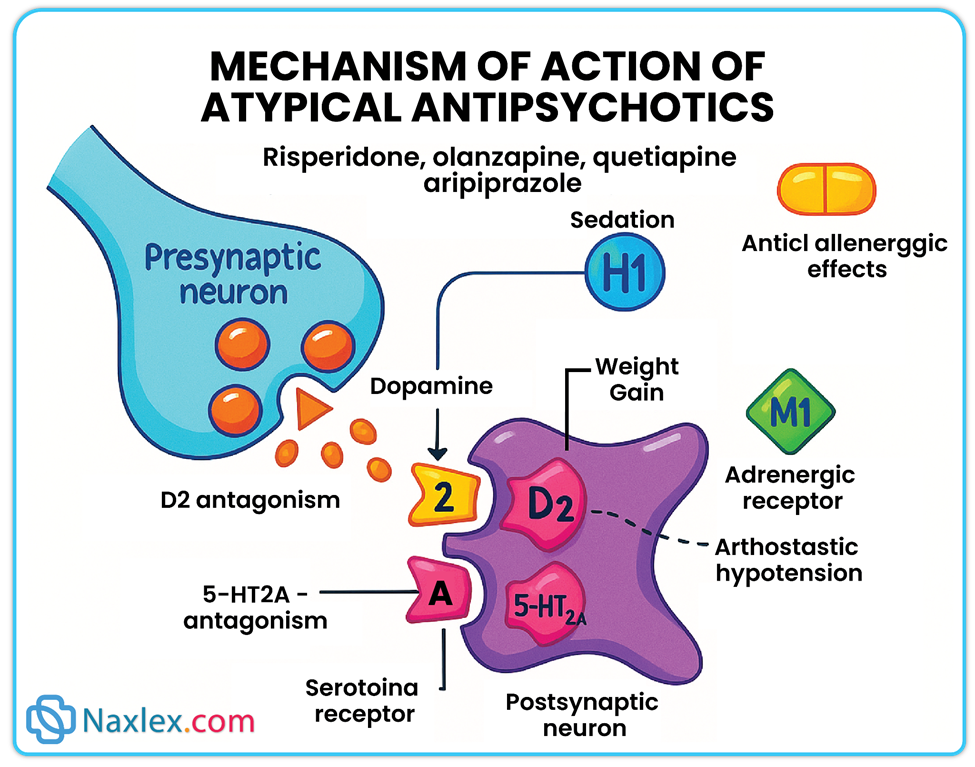
Second-generation antipsychotics
Overview
-
Second-Generation Antipsychotics (SGAs), also known as atypical antipsychotics, are a newer generation of antipsychotic medications introduced to improve upon the safety and tolerability of First-Generation Antipsychotics (FGAs).
-
They are prescribed to treat schizophrenia, schizoaffective disorder, bipolar disorder, and certain other psychiatric conditions.
-
SGAs are preferred in many cases because they have a lower risk of causing extrapyramidal symptoms (EPS), such as muscle rigidity, tremors, and involuntary movements, which are common with FGAs.
-
These drugs are effective in treating both:
-
Positive symptoms of psychosis (hallucinations, delusions, disorganized speech/behavior)
-
Negative symptoms of psychosis (lack of motivation, emotional flatness, social withdrawal), which FGAs often fail to improve.
-
-
Their broader receptor activity makes them more tolerable for many patients and sometimes more effective for cognitive and mood symptoms.
-
SGAs act on multiple neurotransmitter systems in the brain, which is why they are called “atypical.”
-
Primary mechanism:
-
Antagonism of serotonin 5-HT2A receptors – This reduces serotonin activity in certain brain areas, which in turn increases dopamine release in pathways involved in movement and mood.
-
Dopamine D2 receptor blockade – This decreases overactive dopamine signaling in brain regions responsible for psychotic symptoms, but the blockade is less intense and more selective than in FGAs.
-
-
Why this matters clinically:
-
The stronger serotonin antagonism and relatively weaker dopamine blockade result in lower EPS risk.
-
This balance allows dopamine function to remain intact in pathways important for movement and motivation, helping with negative symptoms and cognition.
-
-
Other receptor actions:
-
Histamine (H1) receptor blockade → causes sedation and weight gain.
-
Alpha-adrenergic receptor blockade → leads to orthostatic hypotension and dizziness.
-
Muscarinic cholinergic receptor blockade → causes anticholinergic side effects (dry mouth, constipation, blurred vision, urinary retention).
-
SGAs are widely used for the following psychiatric conditions:
-
Schizophrenia – Effective for both acute psychotic episodes and maintenance therapy to prevent relapse.
-
Schizoaffective disorder – Improves both psychotic symptoms and mood disturbances.
-
Bipolar disorder – Treats acute manic or mixed episodes; some SGAs (e.g., quetiapine, lurasidone) are also used for bipolar depression.
-
Treatment-resistant depression – Certain SGAs (e.g., aripiprazole, quetiapine XR) can be used as adjunctive therapy when antidepressants alone are insufficient.
-
Autism spectrum disorder – Some SGAs (e.g., risperidone, aripiprazole) are approved to reduce severe irritability, aggression, and self-injury.
-
Off-label uses – Severe behavioral disturbances in dementia, Tourette’s disorder, and agitation in other psychiatric or neurological conditions.
-
Clozapine – Considered the most effective SGA for treatment-resistant schizophrenia but requires strict monitoring due to the risk of agranulocytosis (dangerously low white blood cell count).
-
Risperidone – Effective for a broad range of psychotic and mood symptoms; higher doses increase risk for prolactin elevation and EPS.
-
Olanzapine – Highly effective for psychosis and mood stabilization but carries the highest risk of weight gain, hyperlipidemia, and type 2 diabetes.
-
Quetiapine – Sedating and commonly used in bipolar depression; minimal EPS risk but can cause metabolic syndrome.
-
Ziprasidone – Lower metabolic risk but associated with QT interval prolongation, requiring caution in patients with cardiac history.
-
Aripiprazole – A partial dopamine agonist; tends to cause less sedation and metabolic effects but may lead to akathisia in some patients.
-
Paliperidone – Active metabolite of risperidone; available as a long-acting injectable for maintenance therapy.
-
Lurasidone – Favorable metabolic profile and approved for bipolar depression; must be taken with food for optimal absorption.
Advantages Over First-Generation Antipsychotics
-
Lower incidence of EPS and tardive dyskinesia due to less dopamine blockade in movement-related brain pathways.
-
Better efficacy for negative symptoms, improving quality of life and social functioning.
-
May have positive effects on mood and anxiety symptoms due to broader receptor activity.
-
Long-acting injectable (LAI) options available, which can improve adherence and reduce relapse risk.
-
Lower rates of neuroleptic malignant syndrome compared to FGAs.
While generally safer than FGAs in terms of movement disorders, SGAs have their own set of side effects that nurses must monitor:
-
Metabolic Effects
-
Significant weight gain, particularly with clozapine and olanzapine.
-
Dyslipidemia – increases in triglycerides and cholesterol.
-
Hyperglycemia – risk of new-onset type 2 diabetes.
-
-
Cardiovascular Effects
-
Orthostatic hypotension – due to alpha-adrenergic blockade.
-
QT prolongation – most notable with ziprasidone; may predispose to arrhythmias.
-
-
Hematologic Effects
-
Agranulocytosis – rare but serious; primarily with clozapine.
-
-
Endocrine Effects
-
Hyperprolactinemia – common with risperidone and paliperidone; may cause menstrual changes, sexual dysfunction, galactorrhea, or gynecomastia.
-
-
Neurological Effects
-
Lower EPS risk than FGAs, but high doses can still cause parkinsonism, akathisia, or dystonia.
-
-
Other Effects
-
Sedation – especially with quetiapine, clozapine, olanzapine.
-
Anticholinergic symptoms – dry mouth, constipation, urinary retention, blurred vision.
-
-
Baseline and ongoing monitoring is critical for early detection of adverse effects:
-
Weight and BMI
-
Waist circumference
-
Fasting glucose and lipid panel
-
Blood pressure
-
-
Cardiac monitoring:
-
ECG for patients on QT-prolonging SGAs or those with cardiac risk factors.
-
-
Hematologic monitoring:
-
Clozapine: weekly CBC for first 6 months, then every 2 weeks for the next 6 months, then monthly if stable.
-
-
Neurologic assessment:
-
Regular EPS screening using tools such as the AIMS scale.
-
-
Patient education:
-
Stress importance of adherence even during symptom remission.
-
Encourage prompt reporting of infection signs (fever, sore throat, malaise).
-
-
Lifestyle support:
-
Counseling on healthy diet, exercise, and smoking cessation to reduce metabolic risk.
-
-
Collaborative care:
-
Work with the mental health team, dietitians, and social workers for comprehensive support.
-
-
Take the medication exactly as prescribed; do not stop abruptly.
-
Report fever, sore throat, or flu-like symptoms immediately (possible agranulocytosis).
-
Follow a balanced diet and engage in regular physical activity to manage weight.
-
Avoid alcohol and non-prescribed sedatives due to increased CNS depression risk.
-
Change positions slowly to avoid dizziness from orthostatic hypotension.
-
Keep all scheduled blood tests and follow-up appointments.
-
Clozapine: Strict blood monitoring required; missing lab checks may result in discontinuation.
-
Metabolic syndrome prevention: Nurses are frontline in monitoring, counseling, and referring for medical management.
-
Long-acting injectables: Follow manufacturer guidelines for preparation, administration site, and storage to ensure safety and efficacy.
Summery
Psychotic disorders, such as schizophrenia, are characterized by disturbances in thought processes, perception, and emotional responsiveness.
The dopamine hypothesis remains the most widely accepted explanation, proposing that excess dopamine activity in certain brain pathways contributes to positive symptoms.
Other neurotransmitter systems (serotonin, glutamate) may influence negative and cognitive symptoms.
Positive symptoms (hallucinations, delusions, disorganized speech) often respond well to dopamine antagonists.
Negative symptoms (social withdrawal, apathy, flattened affect) are less responsive and may require broader-acting agents.
Antipsychotic medications are categorized into:
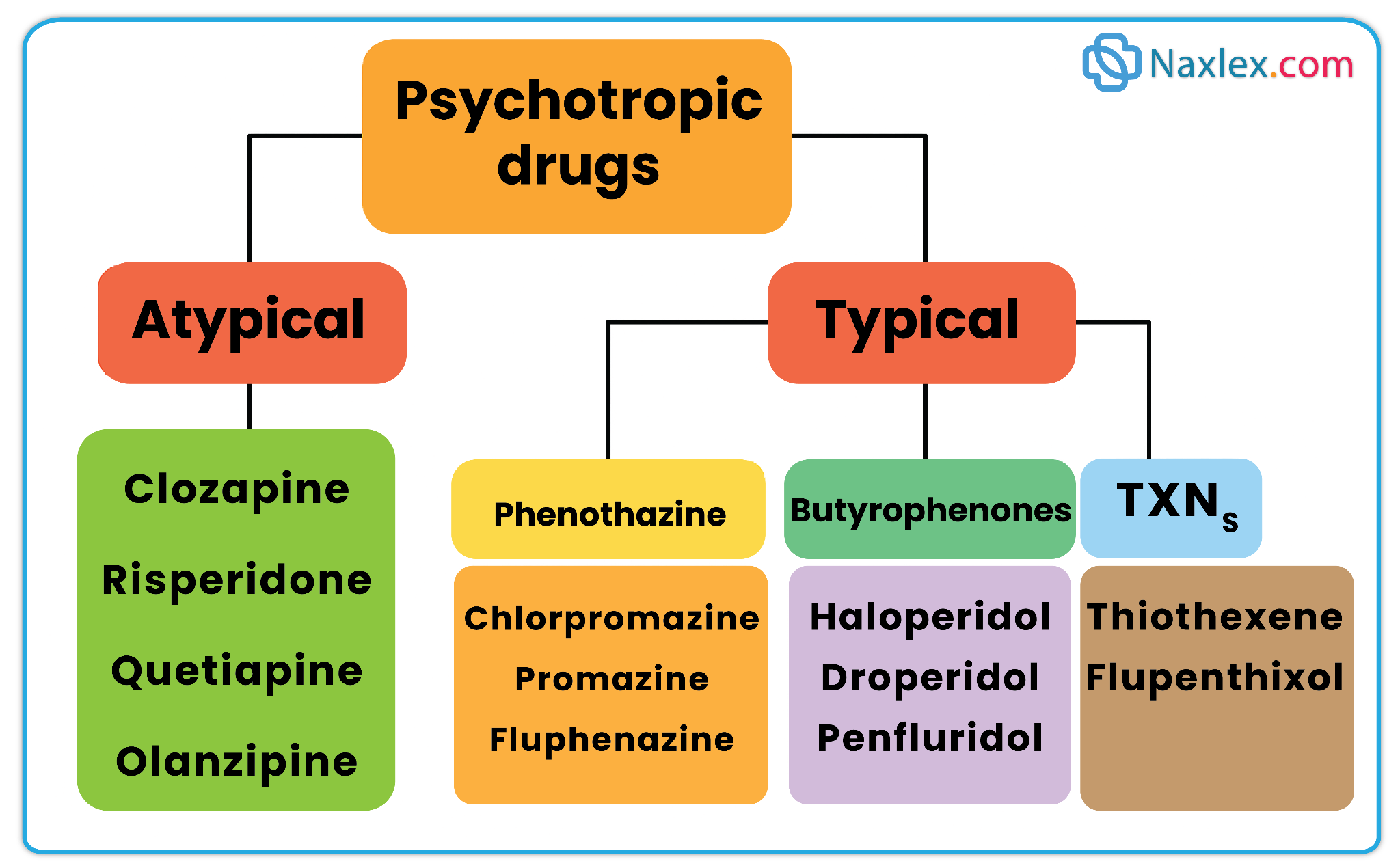
- First-Generation (Typical) Antipsychotics – e.g., haloperidol, chlorpromazine; primarily block D₂ receptors, effective for positive symptoms but carry a higher risk of extrapyramidal symptoms (EPS) and tardive dyskinesia.
- Second-Generation (Atypical) Antipsychotics – e.g., risperidone, olanzapine, clozapine; block both D₂ and serotonin (5-HT₂A) receptors, addressing both positive and negative symptoms, with lower EPS risk but higher metabolic adverse effects.
Major adverse effects include extrapyramidal symptoms (EPS) (acute dystonia, akathisia, parkinsonism, tardive dyskinesia), neuroleptic malignant syndrome (rare but life-threatening), and metabolic effects (weight gain, dyslipidemia, hyperglycemia). Clozapine carries a risk of agranulocytosis and requires regular blood count monitoring.
Pharmacokinetics vary by drug but generally involve good oral absorption, high protein binding, hepatic metabolism (CYP450 enzymes), and renal or biliary excretion.
Long-acting injectable forms improve adherence in patients with poor insight or medication compliance issues.
Nursing care emphasizes thorough assessment (baseline mental status, vitals, weight, metabolic profile), monitoring for side effects, and early recognition of serious reactions.
Patient education should cover adherence importance, safety precautions (e.g., orthostatic hypotension risk), healthy lifestyle practices to counter metabolic effects, and reporting of new or worsening symptoms.
Successful management combines pharmacologic therapy with psychosocial interventions and strong nurse-patient collaboration to improve outcomes and reduce relapse rates.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drugs Used for Psychoses
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


