Please set your exam date
Drugs Affecting the Autonomic Nervous System
Study Questions
Practice Exercise 1
The adrenal medulla plays a key role in the sympathetic response by:
Explanation
The adrenal medulla is a crucial component of the sympathetic nervous system, especially during the fight-or-flight response. It functions as an endocrine organ that amplifies the effects of sympathetic stimulation by releasing catecholamines directly into circulation. This systemic release rapidly prepares the body for emergency responses by increasing heart rate, blood pressure, and energy availability.
Rationale for correct answer:
3. Secreting epinephrine directly into the bloodstream
The adrenal medulla contains chromaffin cells that secrete epinephrine (and some norepinephrine) into the circulation. This results in widespread sympathetic effects like increased heart rate, blood pressure, and glucose availability.
Rationale for incorrect answer:
1. Releasing norepinephrine into the synaptic cleft
This describes the action of sympathetic postganglionic neurons, not the adrenal medulla. The adrenal medulla releases hormones, not neurotransmitters into synapses.
2. Stimulating muscarinic receptors in the brain
Muscarinic receptors are part of the parasympathetic system and are activated by acetylcholine, not by the adrenal medulla or sympathetic output.
4. Blocking beta receptors on the heart
Beta receptor blockade is a pharmacological effect (e.g., from beta-blocker drugs), not a function of the adrenal medulla. In fact, epinephrine stimulates beta receptors.
Take-home points:
- The adrenal medulla releases epinephrine and norepinephrine into the bloodstream during sympathetic activation.
- Epinephrine causes widespread effects such as increased heart rate, blood pressure, and glucose mobilization.
- Unlike sympathetic nerves, the adrenal medulla acts hormonally, not through direct synaptic neurotransmission.
A drug classified as a cholinergic agonist would most likely produce which effect?
Explanation
Cholinergic agonists stimulate the parasympathetic nervous system by mimicking the action of acetylcholine at muscarinic receptors. These agents promote "rest-and-digest" responses, including increased glandular secretions, smooth muscle contraction, and enhanced urinary and gastrointestinal activity. Understanding these systemic effects helps nurses anticipate therapeutic outcomes and potential side effects.
Rationale for correct answer:
3. Enhanced urinary output
Cholinergic agonists increase detrusor muscle tone and relax the urinary sphincter, promoting bladder emptying and urination. This effect is often used therapeutically in urinary retention.
Rationale for incorrect answer:
1. Increased heart rate
Cholinergic agonists typically cause bradycardia by stimulating the vagus nerve, decreasing sinoatrial node activity. Increased heart rate is associated with sympathetic activation, not cholinergic stimulation.
2. Pupil dilation (mydriasis)
Mydriasis is a sympathetic effect. Cholinergic agonists instead cause miosis (pupil constriction), enhancing near vision and limiting light entry.
4. Decreased gastrointestinal motility
These drugs actually increase GI motility by stimulating smooth muscle activity in the intestines, potentially causing cramping or diarrhea.
Take-home points:
- Cholinergic agonists enhance parasympathetic functions like urination, salivation, and GI motility.
- These agents are useful in treating urinary retention and some cases of GI hypomotility.
- Nurses should monitor for excessive parasympathetic effects such as bradycardia, hypotension, and diarrhea.
Activation of beta1 receptors will most likely lead to which of the following physiological effects?
Explanation
Beta1-adrenergic receptors are primarily located in the heart. When activated—whether by endogenous catecholamines like epinephrine or pharmacologic agents—they increase heart rate, contractility, and conduction velocity. This enhances cardiac output, a critical function in stress, shock, and heart failure management.
Rationale for correct answer:
3. Increased myocardial contractility
Beta1 receptor stimulation increases the force of cardiac contractions (positive inotropic effect), which improves cardiac output and tissue perfusion—especially important in conditions like heart failure.
Rationale for incorrect answer:
1. Bronchodilation
This effect is mediated by beta2 receptors in the bronchial smooth muscle, not beta1 receptors. Beta1 stimulation primarily affects cardiac function.
2. Decreased heart rate
Beta1 activation leads to a positive chronotropic effect (increased heart rate). A decreased heart rate would result from beta-blockade or parasympathetic stimulation.
4. Vasodilation of skeletal muscles
Vasodilation in skeletal muscle vasculature is primarily a beta2 receptor effect. Beta1 receptors do not mediate vascular smooth muscle relaxation.
Take-home points:
- Beta1 receptors are located mainly in the heart and increase heart rate and contractility when stimulated.
- Activation of beta1 receptors improves cardiac output but may increase myocardial oxygen demand.
- Understanding receptor-specific effects helps guide safe use of adrenergic drugs and anticipate cardiovascular responses.
A client receiving albuterol for asthma would most likely experience which therapeutic effect?
Explanation
Albuterol is a selective beta2-adrenergic agonist commonly used in the treatment of asthma and other obstructive airway diseases. It exerts its effects by stimulating beta2 receptors in bronchial smooth muscle, leading to muscle relaxation and airway dilation. This pharmacologic action makes albuterol effective in relieving bronchospasm and improving airflow during acute asthma attacks.
Rationale for correct answer:
3. Bronchodilation
This is the primary therapeutic effect of albuterol. By activating beta2 receptors, albuterol causes smooth muscle relaxation in the airways, improving ventilation and reducing wheezing and shortness of breath.
Rationale for incorrect answer:
1. Decreased heart rate
Beta2 agonists have minimal direct effects on heart rate. In some cases, albuterol may cause a mild increase in heart rate due to peripheral vasodilation or systemic absorption, but a decrease is not expected.
2. Bronchoconstriction
This is the opposite of albuterol’s action. Albuterol promotes bronchodilation by relaxing bronchial smooth muscle, making breathing easier for clients with asthma.
4. Increased salivation
Albuterol does not increase salivation. Increased salivation is more commonly associated with cholinergic drugs, not beta2 agonists.
Take-home points:
- Albuterol is a beta2 agonist that produces bronchodilation by relaxing bronchial smooth muscle.
- It is commonly used to manage acute asthma attacks and other reversible obstructive airway conditions.
- Nurses should monitor for side effects such as tachycardia, tremors, or nervousness due to systemic beta2 stimulation.
Which autonomic receptor subtype is primarily responsible for vasoconstriction?
Explanation
Vasoconstriction is a hallmark sympathetic response that helps maintain blood pressure and redistribute blood flow during stress or shock. This effect is mediated primarily by stimulation of alpha1-adrenergic receptors, which are located on vascular smooth muscle in the arteries and veins. Understanding which receptors regulate vascular tone is critical for interpreting the effects of adrenergic drugs and autonomic stimulation.
Rationale for correct answer:
1. Alpha1
Stimulation of alpha1 receptors causes vasoconstriction by promoting contraction of vascular smooth muscle. This response increases peripheral resistance and raises blood pressure—especially important in hypotensive states.
Rationale for incorrect answer:
2. Beta2
Beta2 receptors mediate vasodilation, particularly in skeletal muscle and coronary arteries. Their activation promotes increased blood flow, not vasoconstriction.
3. Muscarinic
Muscarinic receptors are part of the parasympathetic system and typically promote vasodilation, particularly via nitric oxide release in endothelial cells. They do not cause vasoconstriction.
4. Beta3
Beta3 receptors are primarily found in adipose tissue and the bladder. They are involved in lipolysis and bladder relaxation, not vascular tone.
Take-home points:
- Alpha1 receptor activation causes vasoconstriction by contracting vascular smooth muscle.
- Drugs that stimulate alpha1 receptors (e.g., phenylephrine) raise blood pressure and are used in hypotension or shock.
- Knowing receptor locations helps predict therapeutic and adverse effects of autonomic drugs
Practice Exercise 2
Nadolol (Corgard) is prescribed for a patient. The nurse realizes that this drug is a beta-adrenergic blocker and that this drug classification is contraindicated for patients with which condition?
Explanation
Nadolol (Corgard) is a non-selective beta-adrenergic blocker used in the treatment of hypertension and angina. It blocks both beta-1 (cardiac) and beta-2 (pulmonary) receptors, which can cause bronchoconstriction. Nurses must be aware of patient conditions that contraindicate non-selective beta blocker use.
Rationale for correct answer:
3. Bronchial asthma – Non-selective beta blockers can cause bronchospasm by blocking beta-2 receptors in the lungs, which may trigger life-threatening asthma exacerbations.
Rationale for incorrect answer:
1. Hypothyroidism – Nadolol does not directly worsen hypothyroidism; however, it may mask symptoms like bradycardia. It is not absolutely contraindicated.
2. Angina pectoris – Nadolol is commonly used to manage angina by reducing myocardial oxygen demand and controlling heart rate.
4. Liver dysfunction – Nadolol is excreted primarily through the kidneys, so liver dysfunction does not strongly affect its metabolism compared to other drugs.
Take-home points:
- Nadolol is contraindicated in patients with bronchial asthma due to risk of bronchospasm.
- Non-selective beta blockers affect both cardiac and pulmonary beta receptors.
- Always assess respiratory history before initiating beta-adrenergic blocker therapy.
The nurse realizes that beta1 receptor stimulation is differentiated from beta2 stimulation in that stimulation of beta1 receptors leads to which condition?
Explanation
Understanding the distinction between beta-1 and beta-2 receptor stimulation is essential for anticipating therapeutic effects and adverse reactions. Beta-1 receptors are primarily located in the heart, while beta-2 receptors are found in the lungs, vascular smooth muscle, and uterus.
Rationale for correct answer:
3. Increased myocardial contractility
Beta1 receptors are located mainly in the heart, and their stimulation results in increased heart rate (positive chronotropic effect) and increased contractility (positive inotropic effect), enhancing cardiac output. This is a hallmark effect of beta1 receptor activation.
Rationale for incorrect answer:
1. Increased bronchodilation
This effect is associated with beta2 receptor stimulation, primarily found in bronchial smooth muscle, leading to relaxation and airway dilation. It is not the action of beta1 stimulation.
2. Decreased uterine contractility
Beta2 receptors also mediate uterine relaxation, which can be beneficial in preterm labor. Beta1 receptors do not influence uterine activity.
4. Decreased blood flow to skeletal muscles
Beta2 stimulation leads to vasodilation in skeletal muscles, enhancing blood flow. A decrease in blood flow would result from vasoconstriction, which is more related to alpha receptor activation, not beta1.
Take-home points:
- Beta1 receptors are primarily found in the heart and increase heart rate and contractility.
- Beta2 receptors are found in the lungs, uterus, and vasculature, promoting relaxation of smooth muscles.
- Knowing receptor locations and effects helps guide safe administration and monitoring of adrenergic medications.
A client is given epinephrine (Adrenalin), an adrenergic agonist (sympathomimetic). The nurse should monitor the client for which condition?
Explanation
Epinephrine is a nonselective adrenergic agonist that stimulates alpha and beta receptors, leading to widespread sympathetic nervous system activation. Nurses must understand its systemic effects to monitor for therapeutic outcomes and potential adverse reactions, especially in cardiovascular and respiratory systems.
Rationale for correct answer:
4. Increased blood pressure
Alpha1 receptor stimulation by epinephrine leads to vasoconstriction, raising systemic vascular resistance and thereby increasing blood pressure. This is a primary therapeutic effect in shock or cardiac arrest situations.
Rationale for incorrect answer:
1. Decreased pulse
Epinephrine typically increases the heart rate (positive chronotropic effect) through beta1 stimulation. A decreased pulse would be contrary to its expected action.
2. Pupil constriction
Sympathomimetic drugs like epinephrine cause pupil dilation (mydriasis) via alpha1 stimulation, not constriction. Miosis is associated with parasympathetic stimulation.
3. Bronchial constriction
Epinephrine activates beta2 receptors, causing bronchodilation, which helps open the airways. Bronchial constriction would be a parasympathetic effect or due to allergic reactions, not epinephrine.
Take-home points:
- Epinephrine stimulates alpha and beta receptors, leading to increased BP, HR, and bronchodilation.
- Nurses should monitor cardiovascular and respiratory parameters closely during administration.
- Recognizing the adrenergic effects of epinephrine is essential for safely managing emergencies like anaphylaxis or cardiac arrest.
A client who is taking epinephrine is also taking several other medications. The nurse should realize that there is a possible drug interaction with which drugs? Select all that apply.
Explanation
Epinephrine is a potent adrenergic agonist used in emergencies, but when combined with other cardiovascular or autonomic drugs, it may produce interactions that require close monitoring. Nurses should be aware of drug combinations that enhance, oppose, or intensify epinephrine's effects.
Rationale for correct answers:
2. Metoprolol (Lopressor)
Metoprolol is a selective beta1 blocker. It may antagonize epinephrine's beta1 effects on the heart, potentially reducing its efficacy or causing unpredictable cardiovascular responses, such as hypertension from unopposed alpha effects.
3. Propranolol (Inderal)
Propranolol is a non-selective beta blocker, which can block both beta1 and beta2 receptors. This may lead to bronchospasm and hypertension when combined with epinephrine due to unopposed alpha-adrenergic vasoconstriction.
4. Digoxin (Lanoxin)
Both digoxin and epinephrine affect cardiac rhythm. When combined, there is an increased risk of cardiac dysrhythmias, particularly in clients with preexisting cardiac conditions.
Rationale for incorrect answers:
1. Albuterol (Proventil)
Albuterol is a beta2-adrenergic agonist like epinephrine. While this combination may increase the risk of side effects like tachycardia or tremors, a significant interaction is less likely unless used in high doses. They may actually be used together in acute asthma.
5. Methyldopa (Aldomet)
Methyldopa is a centrally acting antihypertensive that reduces sympathetic outflow. Although it works on the same system, a direct interaction with epinephrine is not well-established and is generally less clinically significant than with beta blockers or digoxin.
Take-home points:
- Combining epinephrine with beta blockers can cause unopposed alpha stimulation, leading to severe hypertension.
- The combination of epinephrine and digoxin may increase the risk of arrhythmias.
- Nurses should closely monitor cardiac and blood pressure parameters when epinephrine is used with drugs affecting the autonomic or cardiovascular system.
A client is prescribed metoprolol (Lopressor) to treat hypertension. It is important for the nurse to monitor the client for which condition? Select all that apply
Explanation
Metoprolol (Lopressor) is a cardioselective beta1-adrenergic blocker commonly used to treat hypertension and other cardiovascular conditions. While effective, beta blockers can significantly affect cardiovascular function, and nurses must monitor for key adverse effects to ensure patient safety.
Rationale for correct answers:
1. Bradycardia
Metoprolol slows heart rate by blocking beta1 receptors in the sinoatrial (SA) node. This can result in bradycardia, which requires close monitoring especially in patients also on other rate-lowering agents or with conduction abnormalities.
2. Hypotension
As an antihypertensive, metoprolol decreases blood pressure by reducing cardiac output. Hypotension is a common side effect and should be monitored, especially when therapy is initiated or doses are adjusted.
Rationale for incorrect answers:
3. Ankle edema
While not typical of metoprolol alone, peripheral edema may occur due to reduced cardiac output or if combined with other agents like calcium channel blockers. However, it is more commonly associated with vasodilators.
4. Decreased respirations
Metoprolol is cardioselective and does not usually affect respiratory rate at therapeutic doses. Non-selective beta blockers would pose more risk for bronchospasm or respiratory suppression, especially in patients with respiratory disorders.
5. Increased respirations
This is not a known adverse effect of metoprolol. The drug does not stimulate the respiratory center and typically would not result in increased respiratory rate unless hypotension causes a compensatory response.
Take-home points:
- Monitor for bradycardia and hypotension as primary cardiovascular effects of metoprolol.
- Although selective, beta blockers still warrant caution in patients with respiratory or conduction issues.
- Dose titration and close assessment of vitals are essential when initiating beta-blocker therapy.
Practice Exercise 3
The nurse teaches the patient receiving atropine (Atreza) to expect which side effect?
Explanation
Atropine (Atreza) is an anticholinergic (parasympatholytic) medication that blocks the effects of acetylcholine on muscarinic receptors. It is used preoperatively to reduce secretions, increase heart rate in bradycardia, and as an antidote for certain types of poisoning. Its anticholinergic effects can lead to a range of side effects, especially in the eyes and gastrointestinal system.
Rationale for correct answer:
3. Blurred vision
Atropine causes pupil dilation (mydriasis) and inhibits accommodation, leading to blurred near vision. This is a common and expected side effect, especially with ophthalmic or systemic use.
Rationale for incorrect answer:
1. Diarrhea
Atropine decreases gastrointestinal motility, which can cause constipation rather than diarrhea. Diarrhea would be inconsistent with its anticholinergic action.
2. Bradycardia
Although a very low dose of atropine may briefly lower heart rate due to paradoxical central effects, its primary clinical use is to treat bradycardia by increasing heart rate via vagal inhibition.
4. Frequent urination
Urinary retention is more likely than frequent urination with atropine due to decreased bladder muscle tone. Patients may have difficulty initiating urination, not increased frequency.
Take-home points:
- Atropine’s anticholinergic properties frequently lead to blurred vision, dry mouth, and urinary retention.
- It increases heart rate by inhibiting vagal stimulation of the SA node.
- Patient teaching should include warnings about visual disturbances and the need for caution when performing tasks requiring clear vision.
When benztropine (Cogentin) is ordered for a patient, the nurse acknowledges that this drug is an effective treatment for which condition?
Explanation
Benztropine (Cogentin) is a centrally acting anticholinergic medication used primarily in the treatment of Parkinson’s disease and drug-induced extrapyramidal symptoms (EPS). By inhibiting acetylcholine, it helps restore the balance between dopamine and acetylcholine in the brain, which improves motor symptoms associated with Parkinsonism.
Rationale for correct answer:
1. Parkinsonism
Benztropine is commonly used to manage symptoms such as tremors, rigidity, and bradykinesia in Parkinson’s disease. It blocks cholinergic activity in the central nervous system, helping to restore the dopamine–acetylcholine balance.
Rationale for incorrect answer:
2. Paralytic ileus
Benztropine is contraindicated in patients with paralytic ileus due to its anticholinergic properties, which reduce GI motility and may worsen the condition.
3. Motion sickness
Although anticholinergics like scopolamine are used for motion sickness, benztropine is not indicated for this use. It is more targeted toward extrapyramidal symptoms and Parkinsonian syndromes.
4. Urinary retention
Benztropine may actually worsen urinary retention due to its anticholinergic effects, which relax the detrusor muscle and can impede bladder emptying.
Take-home points:
- Benztropine is used to manage Parkinsonism and extrapyramidal symptoms, not for GI or vestibular conditions.
- Its anticholinergic effects may cause dry mouth, blurred vision, constipation, and urinary retention.
- It should be used cautiously in patients with glaucoma, GI obstruction, or urinary retention.
Dicyclomine (Bentyl) is an anticholinergic, which the nurse realizes is given to treat which condition?
Explanation
Dicyclomine (Bentyl) is an anticholinergic medication that works by inhibiting the actions of acetylcholine on smooth muscle, especially in the gastrointestinal (GI) tract. Nurses should understand the pharmacologic effect of this drug and assess for appropriate therapeutic use, especially in clients with GI motility disorders like irritable bowel syndrome (IBS).
Rationale for correct answer:
4. Irritable bowel syndrome
Dicyclomine is commonly prescribed to manage abdominal cramping and pain associated with IBS. Its antispasmodic properties reduce smooth muscle spasms in the GI tract, helping to relieve symptoms of IBS.
Rationale for incorrect answer:
1. Mydriasis
While anticholinergics may cause pupil dilation as a side effect, dicyclomine is not prescribed for mydriasis. Medications used for diagnostic pupil dilation include agents like tropicamide or atropine eye drops.
2. Constipation
Dicyclomine can actually contribute to constipation as a side effect due to its anticholinergic action, which slows gastrointestinal motility. It is not used to treat constipation but may worsen it.
3. Urinary retention
Anticholinergics may cause urinary retention, particularly in older adults or those with prostatic hypertrophy. Dicyclomine is not used to treat urinary retention; in fact, it is used cautiously in patients at risk for this condition.
Take-home points:
- Dicyclomine is an anticholinergic primarily used to relieve abdominal pain and cramps in IBS by reducing GI smooth muscle spasms.
- Side effects include dry mouth, blurred vision, constipation, and urinary retention, which must be monitored.
- It should be avoided in clients with glaucoma, urinary retention, or severe ulcerative colitis due to potential complications.
The nurse realizes that cholinergic agonists mimic which parasympathetic neurotransmitter?
Explanation
Cholinergic agonists are medications that activate the parasympathetic nervous system by mimicking the effects of acetylcholine, the primary neurotransmitter involved in parasympathetic transmission. These drugs can stimulate muscarinic and nicotinic receptors, resulting in rest-and-digest responses such as increased gastrointestinal motility and decreased heart rate.
Rationale for correct answer:
2. Acetylcholine
Acetylcholine is the principal neurotransmitter of the parasympathetic nervous system. Cholinergic agonists mimic its action, producing effects such as pupil constriction, salivation, and slowed heart rate.
Rationale for incorrect answer:
1. Dopamine
Dopamine is a catecholamine involved primarily in the central nervous system and sympathetic responses, not in parasympathetic neurotransmission.
3. Cholinesterase
Cholinesterase is an enzyme that breaks down acetylcholine in the synaptic cleft. It is not a neurotransmitter and is not mimicked by cholinergic drugs.
4. Monoamine oxidase
Monoamine oxidase is an enzyme involved in breaking down monoamines like serotonin and norepinephrine. It plays no role in parasympathetic neurotransmission.
Take-home points:
- Cholinergic agonists simulate the effects of acetylcholine, the main neurotransmitter of the parasympathetic nervous system.
- These drugs can enhance parasympathetic activity, leading to effects such as bradycardia, bronchoconstriction, and increased secretions.
- Understanding neurotransmitter roles is essential for predicting drug effects and potential adverse reactions.
The nurse is administering bethanechol (Urecholine), a cholinergic agonist, and should know that the expected cholinergic effects include which of the following?
Explanation
Bethanechol is a direct-acting cholinergic agonist that stimulates muscarinic receptors, enhancing the effects of the parasympathetic nervous system. Expected cholinergic responses include increased smooth muscle tone in the GI and urinary tracts, pupil constriction (miosis), and enhanced secretory activity.
Rationale for correct answer:
4. Increased pupil constriction
Cholinergic agonists like bethanechol cause miosis by contracting the circular muscles of the iris, consistent with parasympathetic activation.
Rationale for incorrect answer:
1. Increased heart rate
Cholinergic agonists tend to decrease heart rate due to enhanced vagal (parasympathetic) tone rather than increase it.
2. Decreased peristalsis
Cholinergic stimulation increases gastrointestinal motility and tone, promoting peristalsis rather than reducing it.
3. Decreased salivation
Bethanechol increases salivation by stimulating muscarinic receptors, which promote glandular secretions, not inhibit them.
Take-home points:
- Bethanechol enhances parasympathetic activity, promoting effects like miosis, bradycardia, increased secretions, and smooth muscle contraction.
- Pupillary constriction (miosis) is a classic sign of cholinergic stimulation.
- Understanding parasympathetic responses is crucial when evaluating the therapeutic effects and adverse reactions of cholinergic agonists.
Comprehensive Questions
Following administration of phenylephrine (Neo-Synephrine), the nurse would assess for which of the following adverse drug effects?
Explanation
Phenylephrine (Neo-Synephrine) is a selective alpha-1 adrenergic agonist used for nasal congestion, hypotension, and sometimes to prolong local anesthetic action. Due to its mechanism of vasoconstriction via stimulation of alpha-1 receptors, it can lead to systemic cardiovascular and central nervous system effects that nurses must monitor closely after administration.
Rationale for correct answer:
1. Insomnia, nervousness, and hypertension
These are common adverse effects of phenylephrine due to CNS stimulation and peripheral vasoconstriction. The alpha-1 receptor activation increases blood pressure, and stimulation of the sympathetic nervous system can lead to restlessness and sleep disturbances.
Rationale for incorrect answer:
2. Nausea, vomiting, and hypotension
While nausea and vomiting can occasionally occur, hypotension is not expected with phenylephrine since it is primarily used to increase blood pressure in hypotensive states through vasoconstriction.
3. Dry mouth, drowsiness, and dyspnea
These symptoms are more consistent with anticholinergic agents or CNS depressants, not alpha-1 agonists. Phenylephrine does not typically cause drowsiness or impair airway function.
4. Increased bronchial secretions, hypotension, and bradycardia
Phenylephrine does not increase secretions or cause hypotension. While reflex bradycardia may occur from elevated BP, this triad does not represent typical adverse effects of the drug.
Take-home points:
- Phenylephrine, an alpha-1 agonist, causes vasoconstriction, which can lead to hypertension and reflex bradycardia.
- Nurses should monitor for CNS stimulation symptoms like insomnia and nervousness after administration.
- Adverse effects align with sympathomimetic activity, not parasympathetic or cholinergic effects.
Anticholinergics may be ordered for which of the following conditions? Select all that apply.
Explanation
Anticholinergic drugs block the action of acetylcholine in the parasympathetic nervous system. They are often used to decrease secretions, relax smooth muscles, and increase heart rate. Understanding their therapeutic use is essential for selecting appropriate treatment conditions.
Rationale for correct answers:
1. Peptic ulcer disease
Anticholinergics reduce gastric acid secretion and slow gastrointestinal motility, which can help alleviate ulcer symptoms and reduce acid-related irritation in the GI tract.
2. Bradycardia
By inhibiting parasympathetic stimulation to the heart, anticholinergics like atropine can increase heart rate, making them useful in treating symptomatic bradycardia.
4. Irritable bowel syndrome (IBS)
Anticholinergics can reduce abdominal cramping and spasms in IBS by relaxing intestinal smooth muscle and decreasing motility.
Rationale for incorrect answer:
3. Decreased sexual function
Anticholinergics are not prescribed to treat decreased libido or sexual dysfunction. In fact, they may worsen this issue due to side effects like decreased lubrication or erectile difficulty.
Take-home points:
- Anticholinergics are helpful in conditions involving excessive secretions, smooth muscle spasms, or parasympathetic overactivity.
- Common therapeutic uses include bradycardia, IBS, and peptic ulcer disease.
- They are not indicated for sexual dysfunction and may even contribute to it as a side effect.
Propranolol (Inderal) has been ordered for a client with hypertension. Because of adverse effects related to this drug, the nurse would carefully monitor for which adverse effect?
Explanation
Propranolol (Inderal) is a non-selective beta-adrenergic blocker used to manage hypertension, arrhythmias, and angina. It works by blocking beta-1 and beta-2 receptors, leading to slowed heart rate and decreased cardiac output. Nurses must monitor cardiovascular and respiratory systems closely due to potential serious adverse effects.
Rationale for correct answer:
4. Bradycardia
Bradycardia is a major adverse effect due to beta-1 receptor blockade in the heart. Propranolol slows the SA node and AV node conduction, making it essential to monitor pulse and withhold the drug if the heart rate falls below safe limits (usually <60 bpm).
Rationale for incorrect answer:
1. Bronchodilation
Propranolol blocks beta-2 receptors in bronchial smooth muscle, which can cause bronchoconstriction, not bronchodilation. This effect is especially dangerous in clients with asthma or COPD.
2. Tachycardia
Propranolol decreases sympathetic stimulation of the heart, leading to slower heart rate, not tachycardia. It is often prescribed to prevent tachycardic conditions like atrial fibrillation or performance anxiety.
3. Edema
Edema is more commonly associated with calcium channel blockers or heart failure. Although beta blockers can worsen heart failure, peripheral edema is not a primary expected adverse effect of propranolol.
Take-home points:
- Propranolol causes bradycardia by blocking beta-1 receptors, reducing heart rate and cardiac output.
- It can also cause bronchoconstriction due to beta-2 blockade, so it must be used cautiously in patients with respiratory disease.
- Always assess pulse before administration and hold the medication if bradycardia is present.
Older adult clients taking bethanechol (Urecholine) need to be assessed more frequently because of which of the following adverse effects?
Explanation
Bethanechol (Urecholine) is a direct-acting cholinergic agonist prescribed to stimulate bladder emptying in clients with urinary retention. Older adults are more vulnerable to its parasympathomimetic effects, which can lead to cardiovascular and neurological side effects that require close monitoring.
Rationale for correct answer:
3. Dizziness
Dizziness is a common concern in older adults taking bethanechol due to the risk of orthostatic hypotension and decreased cardiac output. This increases the risk for falls, making frequent assessment essential in this population.
Rationale for incorrect answer:
1. Tachycardia
Bethanechol typically causes bradycardia by stimulating the parasympathetic nervous system. Tachycardia is not a common effect of this drug and would not be the primary concern.
2. Hypertension
Cholinergic agonists tend to lower blood pressure through vasodilation and enhanced parasympathetic tone. Hypertension is not a typical adverse reaction.
4. Urinary retention
Bethanechol is used to treat urinary retention by stimulating the bladder. Retention would indicate a lack of therapeutic effect rather than an adverse one.
Take-home points:
- Bethanechol stimulates the parasympathetic system and can cause dizziness from hypotension, especially in older adults.
- Older clients require close monitoring for orthostatic changes and fall risks while on cholinergic medications.
- This drug is intended to treat urinary retention, not cause it, so effectiveness is measured by successful voiding.
The client taking benztropine (Cogentin) should be provided education on methods to manage which common adverse effect?
Explanation
Benztropine (Cogentin) is an anticholinergic medication commonly used to manage extrapyramidal symptoms in Parkinson’s disease or from antipsychotic use. Like other anticholinergics, it reduces parasympathetic activity, which can lead to various systemic effects—particularly those involving the gastrointestinal tract.
Rationale for correct answer:
2. Constipation
Constipation is a frequent side effect of anticholinergic medications due to slowed peristalsis and reduced secretions. Clients should be educated on increasing fluid and fiber intake and the possible need for stool softeners.
Rationale for incorrect answer:
1. Heartburn
Benztropine decreases gastric motility and acid secretion, which may actually reduce the risk of heartburn rather than cause it. This is not considered a common adverse effect.
3. Hypothermia
Benztropine may impair heat dissipation and lead to hyperthermia, not hypothermia, especially in hot environments due to inhibited sweating.
4. Increased gastric motility
This medication reduces gastric and intestinal motility, not increases it. Slowed GI transit is why constipation becomes a primary concern during therapy.
Take-home points:
- Constipation is a common and expected side effect of benztropine due to reduced GI motility.
- Client education should include preventive strategies such as hydration, dietary fiber, and physical activity.
- Anticholinergics may also reduce the ability to sweat, increasing the risk of heat-related complications.
The client or family of a client taking tacrine (Cognex) should be taught to be observant for which of the following adverse effects that may signal that a possible overdose has occurred?
Explanation
Tacrine (Cognex) is a cholinesterase inhibitor used in the treatment of Alzheimer’s disease. It increases acetylcholine levels in the brain to enhance memory and cognition. However, excessive cholinergic stimulation from overdose can lead to signs of cholinergic toxicity, which nurses and caregivers must closely monitor.
Rationale for correct answer:
1. Excessive sweating, salivation, and drooling
These are hallmark signs of cholinergic toxicity. Tacrine increases parasympathetic activity, and an overdose may lead to excessive secretions, bradycardia, muscle weakness, and in severe cases, respiratory compromise.
Rationale for incorrect answer:
2. Extreme constipation
Constipation is more typical of anticholinergic toxicity, not cholinergic excess. Tacrine enhances cholinergic activity, which usually increases GI motility rather than slowing it down.
3. Hypertension and tachycardia
These are signs more often associated with sympathetic nervous system overactivity, not with cholinergic overstimulation caused by drugs like tacrine.
4. Excessively dry eyes and reddened sclera
Dry eyes are an anticholinergic effect. Tacrine, being a cholinergic agent, would more likely cause increased lacrimation (tear production), not dryness.
Take-home points:
- Tacrine overdose manifests with signs of cholinergic excess, including sweating, salivation, drooling, and bradycardia.
- Cholinergic drugs increase parasympathetic activity; caregivers should know the early signs of overdose to act promptly.
- Differentiating between cholinergic and anticholinergic effects is essential for safe medication management in Alzheimer’s care.
A 59-year-old patient came to see the primary healthcare provider regarding some discomfort that was being experienced as shooting down the left arm. The patient has a history of hypertension, asthma, and glaucoma. Currently the patient is taking the following medications: atenolol for hypertension, albuterol for asthma (as needed), and pilocarpine drops for glaucoma.
The nurse discussed with the patient in the scenario the effects of the medications that they are currently taking. When explaining this the nurse described the common neurotransmitters and how they affect the central nervous system by stating which of the following? (Select all that apply.)
Explanation
Understanding how medications influence the autonomic nervous system (ANS) helps both nurses and clients anticipate expected effects and manage adverse reactions. Knowledge of neurotransmitters and receptor activity is fundamental when explaining the pharmacologic actions of medications, especially those affecting heart rate, blood pressure, and intraocular pressure.
Rationale for correct answers:
1. “The major neurotransmitters of the autonomic nervous system are acetylcholine and norepinephrine.”
Acetylcholine is the primary neurotransmitter of the parasympathetic nervous system, and norepinephrine is the primary neurotransmitter of the sympathetic nervous system. These two chemicals regulate many involuntary body functions through the ANS.
2. “You see, the medications you take have an effect on the neurotransmitters of the nervous system since this is what controls your heart rate and blood pressure.”
This statement accurately reflects how autonomic drugs work by mimicking or blocking neurotransmitter actions, thereby influencing cardiovascular parameters like heart rate and BP.
3. “The medication that you take for glaucoma stimulates the cholinergic receptors to decrease the intraocular pressure.”
Cholinergic agonists (e.g., pilocarpine) lower intraocular pressure by increasing aqueous humor outflow through ciliary muscle contraction, which is a parasympathetic (cholinergic) action.
5. “The two main branches of the autonomic nervous system are complementary, since one branch speeds processes up and the other slows things down.”
This reflects the balance between sympathetic ("fight or flight") and parasympathetic ("rest and digest") systems. Their opposing actions help maintain homeostasis depending on the body’s needs.
Rationale for incorrect answer:
4. “The cholinergic side of the nervous system is subdivided into alpha, beta, and dopamine receptors.”
Alpha, beta, and dopamine receptors are classifications under the adrenergic (sympathetic) system, not the cholinergic system. Cholinergic receptors are categorized as nicotinic and muscarinic.
Take-home points:
- The autonomic nervous system functions through two main neurotransmitters: acetylcholine and norepinephrine.
- Cholinergic and adrenergic medications influence vital functions like heart rate, blood pressure, and intraocular pressure.
- Alpha, beta, and dopamine receptors belong to the adrenergic (not cholinergic) system and should not be confused with muscarinic or nicotinic receptors.
A male patient was discussing with the nurse that he was experiencing problems urinating after taking an antihistamine that has anticholinergic properties and was wondering why this was happening. Which statement by the nurse explains this effect?
Explanation
Anticholinergic effects of certain medications, including some antihistamines, can impact the parasympathetic nervous system. This can lead to reduced smooth muscle activity, especially in organs like the bladder. Nurses must be able to explain these effects clearly to help clients understand and manage their symptoms.
Rationale for correct answer:
4. “Your medication is causing your bladder to relax because it is inhibiting the cholinergic receptors, therefore the bladder is slower to contract to expel the urine.”
This explanation is accurate and appropriate. Anticholinergic activity reduces detrusor muscle contraction, which delays urine expulsion and may lead to urinary retention.
Rationale for incorrect answer:
1. “Antihistamines are used to treat allergy symptoms, and do not affect the bladder.”
This response is inaccurate. Many antihistamines with anticholinergic effects can impair bladder contraction, especially in older adults or males with prostatic hypertrophy.
2. “This medication you are taking has the effect of causing dry mouth and sedation, but I never heard of it causing urinary retention.”
Minimizing or being unaware of a known side effect such as urinary retention reflects a lack of pharmacologic understanding and could delay proper client education or treatment.
3. “I am sure your symptoms will get better if you wait a few weeks and let your body adjust to the medication.”
Telling the client to wait without addressing a potentially serious side effect may risk complications like urinary retention and bladder distention.
Take-home points:
- Anticholinergic drugs can cause urinary retention by reducing bladder muscle contractility.
- Nurses should assess for and educate clients about common anticholinergic side effects such as dry mouth, constipation, and urinary retention.
- Client concerns about side effects should be addressed with clear explanations based on the drug’s mechanism of action.
The patient in the scenario is taking a cholinergic agent. Indicate which medication is being used, what clinical effect the nurse can expect, and for what adverse effect the nurse should monitor.
Choose the most likely option for the information missing from the statements below by selecting from the list of options provided.
The nurse will discuss with the patient the use of
Explanation
Rationale for correct answer:
Pilocarpine is a direct-acting cholinergic agonist that stimulates muscarinic receptors. It is primarily used in the treatment of glaucoma to reduce intraocular pressure by increasing aqueous humor outflow. Nurses administering cholinergic agents like pilocarpine should anticipate both therapeutic effects and systemic adverse effects associated with parasympathetic activation.
Pilocarpine
Pilocarpine is the appropriate choice as it is a cholinergic agent used in ophthalmology to treat glaucoma by activating muscarinic receptors in the eye. This enhances aqueous humor drainage, thereby lowering intraocular pressure.
Glaucoma; reducing intraocular pressure
Glaucoma is managed by lowering intraocular pressure to prevent optic nerve damage. Pilocarpine constricts the pupil (miosis) and opens the trabecular meshwork, facilitating fluid drainage from the anterior chamber.
Bradycardia
Systemic absorption of pilocarpine may stimulate muscarinic receptors in the heart, resulting in slowed heart rate (bradycardia), especially with higher doses or in sensitive individuals. This is a common systemic adverse effect of cholinergic agonists.
Take-home points:
- Pilocarpine is a cholinergic agonist used to treat glaucoma by lowering intraocular pressure via miosis and enhanced aqueous humor outflow.
- Nurses should monitor for systemic cholinergic effects, including bradycardia, excessive salivation, or sweating.
- Understanding the systemic effects of ophthalmic medications is crucial, especially in older adults or those with preexisting cardiac conditions.
The patient in the scenario who has recently been prescribed a beta-adrenergic blocking agent now presents to the emergency department with shortness of breath. Which adverse effect from the medications is the patient likely exhibiting?
Explanation
Beta-adrenergic blocking agents (beta blockers) are commonly used for hypertension, arrhythmias, and other cardiovascular disorders. However, non-selective beta blockers can block beta-2 receptors in the lungs, which may lead to bronchoconstriction, especially in patients with a history of asthma or COPD.
Rationale for correct answer:
3. Bronchoconstriction
Non-selective beta blockers can block beta-2 receptors in bronchial smooth muscle, leading to bronchoconstriction. This is particularly dangerous in individuals with underlying reactive airway disease.
Rationale for incorrect answer:
1. Pneumonia
Pneumonia may cause shortness of breath, but it is unrelated to beta-blocker therapy and would typically present with fever, cough, and crackles rather than sudden respiratory distress.
2. Pulmonary embolism
A pulmonary embolism is a possible cause of acute shortness of breath, but it is not a common adverse effect of beta blockers and requires other risk factors for thrombosis.
4. Bronchodilation
Bronchodilation is caused by beta-2 agonists, not beta blockers. Beta blockers would have the opposite effect on the airways.
Take-home points:
- Non-selective beta blockers may induce bronchoconstriction by blocking beta-2 receptors in the lungs.
- Patients with asthma or COPD should be prescribed cardio-selective beta blockers with caution.
- Shortness of breath following beta-blocker initiation requires immediate assessment for potential respiratory complications.
The nurse reviewing a patient’s preoperative medications noted that atropine sulfate was listed. In which diagnoses should atropine sulfate be used with caution? Select all that apply
Explanation
Atropine sulfate is an anticholinergic medication commonly used preoperatively to reduce secretions and prevent bradycardia. However, because of its systemic antimuscarinic effects, it should be used cautiously in patients with certain chronic conditions where these effects may worsen the clinical status.
Rationale for correct answer:
1. Hypertension
Atropine can increase heart rate and reduce vagal tone, potentially worsening blood pressure in hypertensive patients by increasing sympathetic activity.
2. Asthma
Although anticholinergics can have bronchodilating effects, atropine may thicken bronchial secretions, posing a risk of airway obstruction in patients with reactive airway disease like asthma.
3. Closed-angle glaucoma
Atropine causes pupil dilation (mydriasis), which can precipitate acute angle closure in patients with closed-angle glaucoma, leading to severe eye pain and vision loss.
5. Enlarged prostate (BPH)
Anticholinergic effects of atropine can worsen urinary retention in patients with benign prostatic hyperplasia by inhibiting bladder contraction and detrusor muscle tone.
Rationale for incorrect answer:
4. Open-angle glaucoma
Although less risky than closed-angle glaucoma, atropine is generally avoided in open-angle glaucoma unless the benefits outweigh potential increases in intraocular pressure.
6. Irritable bowel syndrome
Atropine may actually be therapeutic in IBS due to its ability to reduce gastrointestinal spasms, making it generally appropriate in this context.
Take-home points:
- Atropine should be used cautiously in patients with glaucoma, BPH, asthma, or hypertension due to risk of worsening symptoms.
- Its anticholinergic properties can increase intraocular pressure and urinary retention.
- Preoperative medication review must always consider comorbidities that may be aggravated by prescribed drugs.
A client is receiving bethanechol (Urecholine). The nurse realizes that the action of this drug is to treat which condition?
Explanation
Bethanechol (Urecholine) is a direct-acting cholinergic agonist used primarily to stimulate bladder contraction and restore normal urinary function in non-obstructive urinary retention. It enhances parasympathetic activity, making it useful in clients with bladder atony.
Rationale for correct answer:
2. Urinary retention
Bethanechol stimulates muscarinic receptors in the bladder, promoting detrusor muscle contraction and improving bladder emptying in clients with neurogenic or non-obstructive urinary retention.
Rationale for incorrect answer:
1. Glaucoma
While cholinergic agents are sometimes used for glaucoma, bethanechol is not indicated for this purpose; it primarily targets the urinary and GI systems.
3. Delayed gastric emptying
Although it may mildly stimulate GI motility, it is not the preferred treatment for delayed gastric emptying or gastroparesis.
4. Gastroesophageal reflux disease
Bethanechol is not commonly used for GERD; other agents like proton pump inhibitors or prokinetics (e.g., metoclopramide) are more appropriate.
Take-home points:
- Bethanechol is a cholinergic agonist used to treat non-obstructive urinary retention by promoting bladder contraction.
- It should not be confused with medications used for glaucoma or GI reflux.
- Always assess for contraindications such as asthma or bradycardia before administering cholinergic agents.
When a patient has a cholinergic overdose from excessive dosing of bethanechol (Urecholine), the nurse anticipates administration of which drug as the antidote?
Explanation
Cholinergic overdose from medications like bethanechol results in excessive stimulation of the parasympathetic nervous system. Signs include bradycardia, hypotension, excessive salivation, and diarrhea. Atropine, a muscarinic antagonist, is the antidote used to reverse these effects.
Rationale for correct answer:
1. Atropine
Atropine is the first-line antidote for cholinergic toxicity. It competitively blocks muscarinic receptors, thereby reversing the muscarinic overstimulation seen in cholinergic overdose.
Rationale for incorrect answer:
2. Tolterodine
Although it is an anticholinergic used to treat overactive bladder, it is not typically used in emergencies or acute overdose situations.
3. Benztropine
Benztropine is an anticholinergic primarily used to treat extrapyramidal symptoms from antipsychotic drugs. It is not used as a cholinergic antidote.
4. Metoclopramide
This is a prokinetic and antiemetic drug with cholinergic activity, which could worsen symptoms of a cholinergic overdose.
Take-home points:
- Atropine is the antidote for cholinergic toxicity, such as from bethanechol overdose.
- Cholinergic overdose presents with symptoms like bradycardia, excessive salivation, and hypotension.
- Prompt recognition and reversal of parasympathetic overstimulation can prevent complications like respiratory distress or shock.
The nurse will monitor the patient taking albuterol (Proventil) for which conditions? Select all that apply.
Explanation
Albuterol (Proventil) is a short-acting beta-2 adrenergic agonist commonly used to relieve bronchospasm in conditions like asthma and COPD. While effective in relaxing bronchial smooth muscle, its adrenergic effects can also stimulate beta-1 receptors at higher doses, leading to cardiovascular side effects that nurses must monitor carefully.
Rationale for correct answers:
1. Palpitations – Albuterol can cause cardiac stimulation by activating beta-1 receptors at higher or repeated doses, resulting in palpitations, tachycardia, or other dysrhythmias.
2. Hypertension – Beta-agonists may increase heart rate and contractility, potentially raising blood pressure in some patients, especially in those with underlying cardiovascular conditions.
Rationale for incorrect answers:
3. Hypoglycemia – Albuterol is more commonly associated with hyperglycemia, not hypoglycemia. It stimulates glycogenolysis, potentially increasing blood glucose levels.
4. Bronchospasm – Albuterol is used to relieve, not cause, bronchospasm. However, paradoxical bronchospasm is rare and would be an adverse reaction, not a typical side effect to monitor for routinely.
5. Uterine contractions – Albuterol is sometimes used off-label to inhibit uterine contractions due to its smooth muscle relaxing effects. It does not typically cause uterine contractions.
Take-home points:
- Albuterol may cause palpitations and increased blood pressure due to beta-1 receptor stimulation at higher doses.
- Nurses should monitor cardiovascular effects when administering adrenergic agonists like albuterol.
- Though primarily a bronchodilator, albuterol can have systemic effects, especially if overused.
The nurse is administering atenolol (Tenormin) to a patient. Which concurrent drugs does the nurse expect to most likely cause an interaction? Select all that apply.
Explanation
Atenolol (Tenormin) is a cardioselective beta-1 blocker prescribed for hypertension, angina, and cardiac arrhythmias. Nurses must evaluate potential drug interactions that could reduce atenolol’s effectiveness or amplify its adverse effects, especially those that affect heart rate, blood pressure, or renal perfusion.
Rationale for correct answers:
2. An NSAID, such as aspirin – NSAIDs can reduce the antihypertensive effects of beta-blockers like atenolol by inhibiting renal prostaglandins, potentially increasing blood pressure.
3. Atropine, an anticholinergic – Atropine increases heart rate by blocking parasympathetic input, which may counteract atenolol’s beta-blocking effect, potentially complicating heart rate control.
Rationale for incorrect answers:
1. Ginseng supplement – While ginseng may have mild cardiovascular effects, it has not been shown to consistently interfere with atenolol. It is not a well-documented interaction.
4. Haloperidol (Haldol) – Although both drugs may prolong the QT interval, there is no direct, frequent interaction reported between haloperidol and atenolol affecting the drug's main mechanism.
5. Methyldopa (Aldomet) – Both methyldopa and atenolol lower blood pressure, but they are sometimes used together. Their additive effect is monitored, but this is not considered a strong or dangerous interaction.
Take-home points:
- NSAIDs can blunt the antihypertensive effect of beta-blockers like atenolol.
- Atropine may reduce atenolol's therapeutic effect by increasing heart rate.
- Always evaluate over-the-counter medications or supplements for potential cardiovascular interactions.
Exams on Drugs Affecting the Autonomic Nervous System
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Identify the basic functions of the nervous system.
- Differentiate between the central nervous system (CNS) and peripheral nervous system (PNS), with emphasis on the autonomic division.
- Compare and contrast the sympathetic ("fight-or-flight") and parasympathetic ("rest-and-digest") divisions of the ANS.
- Explain synaptic transmission and identify the key neurotransmitters—norepinephrine (NE) and acetylcholine (ACh)—involved in autonomic signaling.
- Describe the effects of activating alpha1, alpha2, beta1, beta2, muscarinic, and nicotinic receptors.
- Classify autonomic drugs into four main categories: adrenergic agonists (sympathomimetics), adrenergic antagonists (sympatholytics), cholinergic agonists (parasympathomimetics), and cholinergic antagonists (anticholinergics).
- Understand the mechanism of action, therapeutic uses, adverse effects, and nursing implications for each drug class.
- Apply the nursing process when caring for patients receiving autonomic drugs, including assessment, monitoring, patient education, and emergency interventions.
Introduction
This chapter provides a comprehensive review of drugs affecting the autonomic nervous system (ANS), a critical foundation for understanding pharmacology in clinical nursing practice.
The autonomic nervous system regulates involuntary bodily functions such as heart rate, blood pressure, respiration, digestion, pupil size, and glandular secretions.
Drugs that influence this system are widely used across multiple medical specialties—including cardiology, pulmonology, ophthalmology, urology, and emergency medicine—and are essential in managing conditions like shock, asthma, glaucoma, bradycardia, and hypertension.
2.1. Overview of the Nervous System
The nervous system is divided into two primary components: the central nervous system (CNS) and the peripheral nervous system (PNS). The CNS consists of the brain and spinal cord and serves as the command center for processing sensory input and coordinating responses. The PNS includes all nerves outside the CNS and is responsible for transmitting signals between the CNS and the rest of the body.
The PNS is further subdivided into the sensory (afferent) and motor (efferent) divisions. Sensory neurons detect internal and external changes—such as pain, temperature, or light—and transmit this information to the CNS. Motor neurons carry signals from the CNS to effector organs, such as muscles and glands, to produce a response.
The motor division is split into two functional systems: the somatic nervous system and the autonomic nervous system (ANS). The somatic nervous system controls voluntary movements of skeletal muscles and operates via a single neuron pathway from the spinal cord to the muscle. In contrast, the ANS regulates involuntary functions of smooth muscle, cardiac muscle, and exocrine glands through a two-neuron chain: a preganglionic neuron originating in the CNS and a postganglionic neuron that innervates the target organ.
Organs controlled by the ANS include the heart, lungs, gastrointestinal tract, urinary bladder, blood vessels, salivary glands, and parts of the eye. Because these systems are continuously regulated without conscious effort, understanding how drugs affect them is essential for maintaining physiological balance during illness.
The Autonomic Nervous System
3.1. Sympathetic vs. Parasympathetic Divisions
The autonomic nervous system is subdivided into the sympathetic and parasympathetic nervous systems, which generally exert opposing effects on target organs to maintain homeostasis. Most organs receive dual innervation, allowing fine-tuned control based on physiological demands.
The sympathetic nervous system becomes dominant during stress, danger, or physical exertion—activating what is commonly known as the "fight-or-flight" response. This system prepares the body for immediate action by increasing heart rate, elevating blood pressure, dilating the bronchi for enhanced oxygen intake, and redirecting blood flow to skeletal muscles. Simultaneously, nonessential functions such as digestion and urination are suppressed. Key actions include tachycardia, vasoconstriction, glycogenolysis, lipolysis, and pupil dilation (mydriasis).
In contrast, the parasympathetic nervous system predominates during periods of rest, promoting energy conservation and restoration—the so-called "rest-and-digest" state. It slows heart rate, enhances gastrointestinal motility and secretions, stimulates salivation, promotes urination, and constricts the pupils (miosis). These actions support digestion, nutrient absorption, and waste elimination.
While the two divisions typically oppose each other, they often work together in a complementary manner. For example, in sexual function, parasympathetic activity mediates penile erection, while sympathetic activity controls ejaculation. Additionally, some tissues are regulated exclusively by one branch. Arteriolar tone is controlled solely by the sympathetic system through vasoconstriction; absence of sympathetic stimulation leads to passive vasodilation. Sweat glands are also exclusively innervated by sympathetic fibers, although they release acetylcholine rather than norepinephrine.
3.2. Structure and Function of Autonomic Synapses
Autonomic signaling occurs through a two-neuron pathway. The preganglionic neuron originates in the brainstem or spinal cord and extends to an autonomic ganglion, where it synapses with the postganglionic neuron. The postganglionic neuron then travels to the target organ, forming the second synapse at the neuroeffector junction.
At the ganglionic synapse, both sympathetic and parasympathetic preganglionic neurons release acetylcholine (ACh), which binds to nicotinic receptors on the postganglionic neuron. This binding generates an action potential that propagates down the postganglionic fiber.
At the neuroeffector junction, the neurotransmitter released depends on the division:
- Parasympathetic postganglionic neurons release ACh, which acts on muscarinic receptors located on target organs.
- Sympathetic postganglionic neurons primarily release norepinephrine (NE), which binds to adrenergic receptors (alpha and beta types). Exceptions include sympathetic innervation of sweat glands and some blood vessels, where ACh is the neurotransmitter acting on muscarinic receptors.
The adrenal medulla is a unique component of the sympathetic system. Instead of synapsing with a postganglionic neuron, preganglionic fibers directly stimulate chromaffin cells in the adrenal medulla to release epinephrine (and some norepinephrine) into the bloodstream. This hormonal release amplifies and prolongs the sympathetic response throughout the body.
Drugs can influence autonomic function at various points in this pathway, including neurotransmitter synthesis, storage, release, receptor binding, and degradation. Understanding these mechanisms is crucial for predicting drug effects and adverse reactions.
3.3. Neurotransmitters of the Autonomic Nervous System
Two primary neurotransmitters mediate autonomic function: acetylcholine (ACh) and norepinephrine (NE). Their actions depend on the type of receptor they bind to and the location of that receptor.
Acetylcholine is released by all preganglionic neurons (both sympathetic and parasympathetic) and by parasympathetic postganglionic neurons. It is also released by sympathetic postganglionic neurons that innervate sweat glands and certain blood vessels. ACh acts on two main receptor types:
- Nicotinic receptors: Ligand-gated ion channels found at autonomic ganglia and neuromuscular junctions. Activation leads to rapid depolarization and excitation.
- Muscarinic receptors: G-protein coupled receptors located on effector organs of the parasympathetic system, such as the heart, smooth muscle, and glands. These receptors mediate slower, modulatory responses.
Norepinephrine is the primary neurotransmitter released by most sympathetic postganglionic neurons. It binds to adrenergic receptors, which are classified as alpha (α) and beta (β) subtypes, each with further subdivisions. Epinephrine, released by the adrenal medulla, circulates in the blood and activates the same receptors, producing widespread sympathetic effects.
Dopamine, though not traditionally considered a primary autonomic neurotransmitter, plays a role in renal and mesenteric vasculature at low doses, activating dopaminergic receptors (D1) to cause vasodilation. At higher doses, it stimulates beta1 and then alpha1 receptors, leading to increased cardiac output and vasoconstriction.
These neurotransmitters are tightly regulated. ACh is rapidly broken down in the synaptic cleft by acetylcholinesterase (AChE). NE is primarily terminated by reuptake into the presynaptic neuron, followed by enzymatic degradation via monoamine oxidase (MAO) and catechol-O-methyltransferase (COMT).
3.4. Adrenergic Receptors – Types and Physiological Effects
Adrenergic receptors respond to norepinephrine and epinephrine and are divided into alpha (α) and beta (β) families, each with distinct subtypes and tissue distributions.
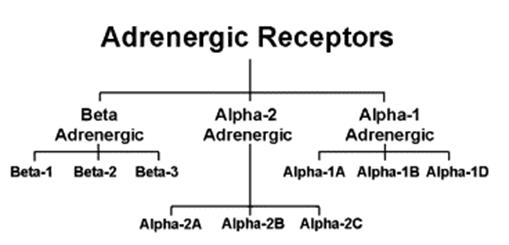
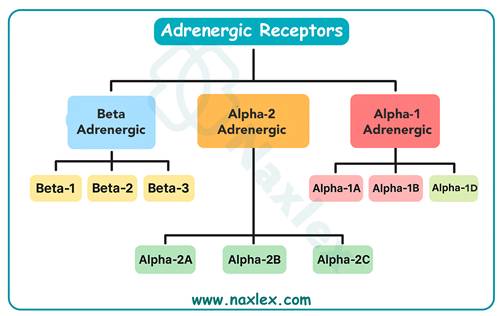
Alpha1 receptors are located on vascular smooth muscle, the iris dilator muscle, prostate, and bladder sphincter. Stimulation causes vasoconstriction (raising blood pressure), mydriasis (pupil dilation), and urinary retention due to sphincter contraction. These effects are exploited therapeutically in treating hypotension, nasal congestion, and during ophthalmic examinations.
Alpha2 receptors are primarily found on presynaptic nerve terminals in both the central and peripheral nervous systems. When activated, they inhibit further release of norepinephrine, serving as a negative feedback mechanism. Centrally acting alpha2 agonists, such as clonidine, reduce sympathetic outflow from the brain, making them useful in managing hypertension.
Beta1 receptors are predominantly located in the heart (SA node, myocardium, AV node) and the kidneys (juxtaglomerular cells). Activation increases heart rate (chronotropy), contractility (inotropy), conduction velocity (dromotropy), and renin release. These effects are beneficial in treating heart failure, shock, and bradycardia.
Beta2 receptors are found in bronchial smooth muscle, uterine smooth muscle, liver, and skeletal muscle vasculature. Their stimulation results in bronchodilation, relaxation of the uterus (useful in delaying preterm labor), glycogenolysis (increasing blood glucose), and vasodilation in select vascular beds. Beta2 agonists are cornerstone treatments for asthma and chronic obstructive pulmonary disease (COPD).
Beta3 receptors, located in adipose tissue, mediate lipolysis but have limited clinical relevance in current pharmacotherapy.
Understanding receptor specificity allows clinicians to select drugs that target desired tissues while minimizing systemic side effects.
Autonomic Drugs
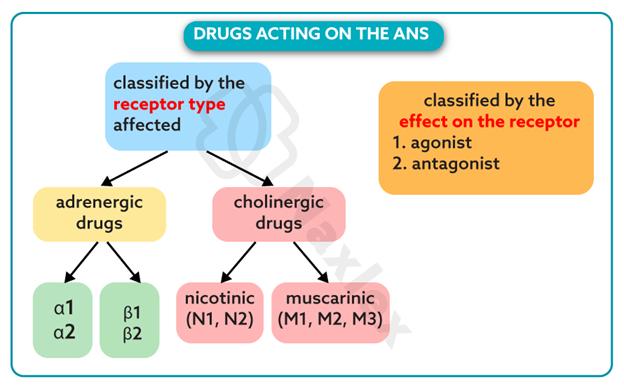
5.1. Classification of Autonomic Drugs
Autonomic drugs are categorized based on their functional impact on the nervous system into four major classes:
- Adrenergic agonists (sympathomimetics): These drugs mimic the effects of sympathetic stimulation by activating adrenergic receptors. Examples include epinephrine, norepinephrine, dopamine, albuterol, and phenylephrine. They are used in emergencies such as anaphylaxis, cardiac arrest, and shock, as well as in asthma and nasal decongestion.
- Adrenergic antagonists (sympatholytics or beta-blockers/alpha-blockers): These agents block the effects of norepinephrine and epinephrine. Alpha-blockers like doxazosin lower blood pressure and treat benign prostatic hyperplasia (BPH), while beta-blockers such as atenolol and propranolol are used for hypertension, angina, heart failure, and dysrhythmias.
- Cholinergic agonists (parasympathomimetics): These drugs enhance parasympathetic activity by either directly stimulating muscarinic receptors or inhibiting acetylcholinesterase. Bethanechol is used for urinary retention, while neostigmine and pyridostigmine treat myasthenia gravis. Donepezil, a cholinesterase inhibitor, is used in Alzheimer’s disease to improve cognitive function.
- Cholinergic antagonists (anticholinergics or muscarinic blockers): These drugs inhibit parasympathetic activity by blocking muscarinic receptors. Atropine increases heart rate and dries secretions, making it useful in bradycardia and pre-anesthesia. Ipratropium is used in asthma and COPD for bronchodilation, while oxybutynin treats overactive bladder.
A helpful learning strategy is to master one class—such as sympathomimetics—and deduce the others based on opposing or similar actions. For example, both sympathomimetics and anticholinergics cause tachycardia and mydriasis, whereas cholinergics and beta-blockers slow the heart and constrict pupils.
-
- Adrenergic drugs
Mechanisms and Chemical Classification
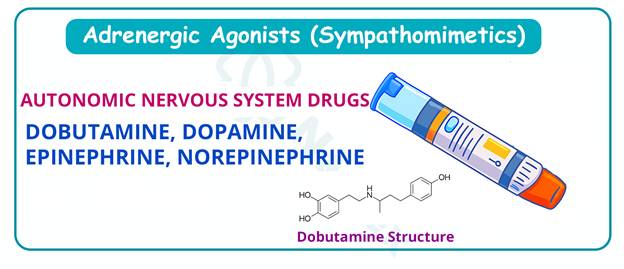
Adrenergic drugs, or sympathomimetics, stimulate the sympathetic nervous system and produce effects characteristic of the "fight-or-flight" response. They are used therapeutically to treat conditions such as shock, hypotension, cardiac arrest, asthma, and nasal congestion.
These drugs can act through different mechanisms:
- Direct-acting: Bind directly to adrenergic receptors. Examples include epinephrine, norepinephrine, dopamine, phenylephrine, and albuterol.
- Indirect-acting: Increase the release of stored norepinephrine or prevent its reuptake. Amphetamines and cocaine fall into this category and are primarily used for their central nervous system effects.
- Mixed-acting: Possess both direct and indirect actions. Ephedrine is an example, historically used as a decongestant and stimulant.
Chemically, sympathomimetics are classified as catecholamines or non-catecholamines. Catecholamines—epinephrine, norepinephrine, dopamine, isoproterenol, and dobutamine—contain a catechol ring and are rapidly metabolized by MAO and COMT. As a result, they have a short duration of action and must be administered parenterally (IV, IM, or endotracheal). Non-catecholamines—such as phenylephrine, terbutaline, ephedrine, and oxymetazoline—lack the catechol structure, are resistant to enzymatic degradation, and can be given orally or via inhalation with longer durations of action.
The choice between catecholamine and non-catecholamine agents depends on the clinical scenario, desired speed of onset, route of administration, and duration of effect.
Selectivity of Sympathomimetics and Therapeutic Applications
The therapeutic utility of sympathomimetics depends on their receptor selectivity. Some agents are highly selective, while others are nonselective and activate multiple receptor types.
Epinephrine is a nonselective adrenergic agonist that activates alpha1, alpha2, beta1, and beta2 receptors. It is the drug of choice for anaphylaxis due to its ability to reverse bronchospasm (beta2), increase blood pressure (alpha1), and support cardiac output (beta1). It is also used in cardiac arrest, acute asthma exacerbations, and open-angle glaucoma (to reduce intraocular pressure).
Norepinephrine primarily activates alpha1 and beta1 receptors with minimal beta2 activity. It is a potent vasoconstrictor used in septic shock to restore perfusion pressure.
Dopamine has dose-dependent effects. At low doses (1–2 mcg/kg/min), it activates dopaminergic receptors in the renal and mesenteric arteries, promoting vasodilation and improving organ perfusion. At moderate doses (2–10 mcg/kg/min), it stimulates beta1 receptors, increasing heart rate and contractility. At high doses (>10 mcg/kg/min), alpha1 effects dominate, causing systemic vasoconstriction and increased blood pressure. It is used in shock states, particularly cardiogenic and septic shock.
Phenylephrine is a selective alpha1 agonist used to treat hypotension, cause mydriasis during eye exams, and relieve nasal congestion as a decongestant.
Albuterol and terbutaline are selective beta2 agonists used for bronchodilation in asthma and COPD. Terbutaline can also be used as a tocolytic to delay preterm labor.
Isoproterenol, a nonselective beta agonist, stimulates both beta1 and beta2 receptors and is used to increase heart rate in bradycardia or heart block, though its use is limited due to risk of tachycardia and arrhythmias.
Side Effects and Nursing Implications of Sympathomimetics
The adverse effects of sympathomimetics are largely extensions of their pharmacological actions. Cardiovascular complications are among the most concerning, including tachycardia, hypertension, palpitations, and dysrhythmias. These effects can exacerbate underlying cardiac conditions and may limit therapeutic use.
Central nervous system stimulation is common, especially with agents that cross the blood-brain barrier. Patients may experience anxiety, restlessness, tremors, insomnia, and, in high doses, seizures. Metabolic effects include hyperglycemia due to beta2-mediated glycogenolysis and hypokalemia from potassium shift into cells.
Other side effects include dry mouth, nausea, vomiting, and urinary retention. Historically, some sympathomimetics were used as appetite suppressants due to their anorectic effects, but this use has been discontinued due to cardiovascular risks.
Nursing considerations include:
- Assessing baseline vital signs before administration.
- Monitoring ECG for dysrhythmias, especially with epinephrine or isoproterenol.
- Using infusion pumps for continuous IV administration of vasoactive drugs.
- Preventing extravasation, as alpha1 agonists can cause severe tissue necrosis if they leak into surrounding tissue.
- Educating patients to report chest pain, severe headache, or palpitations.
- Advising diabetic patients to monitor blood glucose more frequently.
- Cautioning against the use of over-the-counter decongestants in patients with hypertension or cardiovascular disease.
Epinephrine remains the first-line treatment for anaphylaxis and must be administered promptly via intramuscular injection into the anterolateral thigh.
-
- Adrenergic-Blocking Drugs
Mechanism and Classification
Adrenergic-blocking agents, also known as sympatholytics or adrenergic antagonists, inhibit the effects of norepinephrine and epinephrine by blocking adrenergic receptors. They produce effects opposite to sympathomimetics, promoting "rest-and-digest" symptoms such as bradycardia, vasodilation, and decreased renin release.
These drugs are divided into alpha-blockers and beta-blockers, each with distinct mechanisms and clinical applications.
Alpha-adrenergic antagonists block alpha1 receptors on vascular smooth muscle, leading to vasodilation and decreased systemic vascular resistance. This results in lowered blood pressure. Doxazosin is a prototype alpha1 blocker used in hypertension and benign prostatic hyperplasia (BPH), where it relaxes smooth muscle in the prostate and bladder neck, improving urine flow.
A notable side effect is first-dose phenomenon, characterized by severe orthostatic hypotension after the initial dose. Other adverse effects include reflex tachycardia, nasal congestion, and impotence. Nurses should administer the first dose at bedtime and monitor blood pressure in both lying and standing positions.
Beta-adrenergic antagonists block beta1 and/or beta2 receptors. They decrease heart rate, myocardial contractility, and AV node conduction, reducing cardiac workload and oxygen demand. They also suppress renin release from the kidneys, contributing to blood pressure reduction.
Beta-Blockers – Types and Clinical Uses
Beta-blockers are among the most widely prescribed autonomic drugs and are used in a variety of cardiovascular conditions.
Nonselective beta-blockers, such as propranolol, block both beta1 and beta2 receptors. While effective, they can cause bronchoconstriction and are contraindicated in patients with asthma or COPD.
Cardioselective beta-blockers, including atenolol and metoprolol, primarily block beta1 receptors in the heart, minimizing respiratory side effects. They are preferred in patients with reactive airway disease.
Some beta-blockers have additional properties:
- Labetalol blocks both alpha1 and beta receptors, making it useful in hypertensive emergencies.
- Carvedilol has alpha1-blocking activity and is used in heart failure.
- Pindolol has intrinsic sympathomimetic activity (partial agonist effect), causing less bradycardia but rarely used due to limited efficacy.
Therapeutic applications include:
- Hypertension: Reduces blood pressure through decreased cardiac output and renin suppression.
- Angina pectoris: Decreases myocardial oxygen demand.
- Myocardial infarction: Improves survival by reducing cardiac workload and arrhythmia risk.
- Heart failure: Certain beta-blockers (carvedilol, metoprolol, bisoprolol) improve ejection fraction and reduce mortality.
- Dysrhythmias: Slows conduction through the AV node, useful in atrial fibrillation.
- Migraine prophylaxis: Reduces frequency and severity.
- Glaucoma: Topical timolol reduces aqueous humor production, lowering intraocular pressure.
-
- Cholinergic Drugs
Mechanism and Classification
Cholinergic drugs, or parasympathomimetics, enhance parasympathetic activity by mimicking acetylcholine. They are used to treat conditions where increased parasympathetic tone is beneficial, such as urinary retention, neurogenic ileus, glaucoma, and myasthenia gravis.
These drugs are classified into two groups based on their mechanism:
Direct-acting cholinergic agonists, such as bethanechol, bind directly to muscarinic receptors on target organs. They are resistant to acetylcholinesterase, have a longer duration than ACh, and are poorly absorbed from the gastrointestinal tract. They do not cross the blood-brain barrier and are selective for muscarinic receptors at therapeutic doses.
Indirect-acting cholinergic agonists, or cholinesterase inhibitors, prevent the breakdown of endogenous ACh by inhibiting acetylcholinesterase. This increases ACh concentration at synapses, prolonging its action. Examples include neostigmine, pyridostigmine, physostigmine, donepezil, and rivastigmine.
Unlike direct agonists, cholinesterase inhibitors affect all cholinergic sites—autonomic ganglia, muscarinic receptors, neuromuscular junctions, and central nervous system synapses. This broad activity increases their therapeutic versatility but also their risk of toxicity.
Physostigmine, derived from the Calabar bean, was one of the first cholinesterase inhibitors discovered. Its use in chemical warfare research led to the development of organophosphate insecticides (e.g., malathion) and nerve gases (e.g., sarin), which irreversibly inhibit AChE, causing a life-threatening cholinergic crisis.
Therapeutic Uses of Cholinergic Drugs
Cholinergic drugs have several important clinical applications despite their potential for serious side effects.
In ophthalmology, pilocarpine and other muscarinic agonists are used to treat open-angle glaucoma by causing miosis and increasing aqueous humor outflow, thereby reducing intraocular pressure.
For gastrointestinal and urinary dysfunction, bethanechol stimulates smooth muscle contraction in the bladder and bowel, making it useful for postoperative or neurogenic urinary retention and ileus.
In myasthenia gravis, a condition characterized by autoimmune destruction of nicotinic receptors at the neuromuscular junction, cholinesterase inhibitors like neostigmine and pyridostigmine increase ACh availability, improving muscle strength and reducing fatigue.
In Alzheimer’s disease, centrally acting cholinesterase inhibitors such as donepezil and rivastigmine enhance cholinergic transmission in the brain, providing modest cognitive improvement.
Neostigmine is also used postoperatively to reverse the effects of nondepolarizing neuromuscular blocking agents.
However, due to the risk of cholinergic crisis, these drugs require careful dosing. Symptoms include excessive salivation, lacrimation, urination, defecation, GI cramps, emesis, bronchospasm, bradycardia, and miosis—summarized by the mnemonic SLUDGE.
The antidote for cholinergic toxicity is atropine, a muscarinic antagonist.
-
- Cholinergic-Blocking Drugs
Mechanism and Overview
Cholinergic-blocking agents, commonly known as anticholinergics or muscarinic antagonists, inhibit the parasympathetic nervous system by blocking acetylcholine at muscarinic receptors. This results in unopposed sympathetic activity, producing "fight-or-flight" symptoms.
The prototype drug is atropine, derived from the deadly nightshade plant (Atropa belladonna). Historically used in ancient rituals and cosmetics (hence the name "belladonna," meaning "beautiful woman"), atropine causes mydriasis, tachycardia, dry mouth, and sedation.
Anticholinergics compete with ACh for binding sites on muscarinic receptors. When they occupy these receptors, no response is generated at the effector organ, leading to reduced glandular secretions, increased heart rate, bronchodilation, urinary retention, and constipation.
While these effects can be therapeutic, they also contribute to a high incidence of adverse reactions, especially in older adults.
Therapeutic Uses of Anticholinergics
Anticholinergics are used in a wide range of clinical conditions:
- Bradycardia: Atropine blocks vagal tone on the SA node, increasing heart rate in symptomatic bradycardia.
- Pre-anesthesia: Used to reduce respiratory secretions and prevent bradycardia induced by anesthetic agents.
- GI disorders: Drugs like hyoscyamine and dicyclomine reduce gastric acid secretion and intestinal motility, useful in peptic ulcer disease and irritable bowel syndrome.
- Ophthalmic procedures: Tropicamide and atropine induce mydriasis and cycloplegia for eye exams and surgery.
- Respiratory conditions: Ipratropium, delivered by inhalation, causes bronchodilation with minimal systemic absorption, making it safe for asthma and COPD.
- Overactive bladder: Oxybutynin and tolterodine relax the detrusor muscle, reducing urgency and incontinence.
- Parkinson’s disease: Benztropine and trihexyphenidyl reduce tremor and rigidity by restoring balance between acetylcholine and dopamine in the basal ganglia.
- Motion sickness: Scopolamine, administered via transdermal patch, acts centrally to prevent nausea and vomiting.
Adverse Effects and Toxicity of Anticholinergics
Anticholinergic drugs have a broad side effect profile due to widespread muscarinic receptor blockade.
Common adverse effects include:
- Dry mouth, dry eyes, and decreased sweating (leading to hyperthermia)
- Blurred vision and photophobia due to mydriasis
- Urinary retention, especially problematic in men with BPH
- Constipation
- Tachycardia
- Central nervous system effects: drowsiness, confusion, hallucinations, agitation—particularly in elderly patients
Severe overdose produces a characteristic syndrome remembered by the mnemonic: “Hot as hades, blind as a bat, dry as a bone, mad as a hatter.” This includes hyperthermia, mydriasis, anhydrosis, and delirium.
Nurses must monitor for these signs, especially in older adults, and educate patients on managing dry mouth and constipation. Caution is advised in patients with glaucoma, BPH, or cognitive impairment.
The antidote for severe anticholinergic toxicity is physostigmine, which crosses the blood-brain barrier and reverses central effects.
-
- Special Considerations and Drug Examples
Some autonomic drugs have unique properties or routes of administration that enhance safety and efficacy.
Ipratropium (Atrovent) is a quaternary ammonium compound that does not cross membranes easily. When delivered by inhalation, it acts locally in the lungs with minimal systemic absorption, reducing side effects compared to atropine.
Scopolamine, used for motion sickness, acts centrally and causes sedation. It is available as a transdermal patch, providing sustained release.
Donepezil, though classified as a cholinesterase inhibitor, is used for its central effects in Alzheimer’s disease rather than autonomic actions.
Dopamine’s dose-dependent effects make it a versatile agent in critical care, but careful titration is required to avoid unwanted vasoconstriction at high doses.
Labetalol’s combined alpha and beta blockade makes it ideal for hypertensive emergencies, especially in pregnancy.
Nursing Insights
7.1. The Nursing Process and Patient Education
The nursing process is essential in managing patients on autonomic drugs.
Assessment includes baseline vital signs, ECG, respiratory status, urinary output, and mental status. Monitor for contraindications such as asthma (with beta-blockers) or glaucoma (with anticholinergics).
Diagnosis may include risk for falls, ineffective tissue perfusion, or impaired urinary elimination.
Planning and Implementation involve correct dosing, route, and monitoring parameters. Use IV pumps for vasoactive drugs. Administer first doses of alpha-blockers at bedtime.
Evaluation focuses on therapeutic response and adverse effects.
Patient education is crucial:
- Teach patients to recognize side effects.
- Advise against OTC cold medications if on beta-blockers or anticholinergics.
- Emphasize adherence, especially in chronic conditions like hypertension or glaucoma.
7.2. Nursing insights
Vital Sign Monitoring Is Critical with Autonomic Drugs
Drugs like adrenergic agonists or beta-blockers can cause significant changes in heart rate and blood pressure. Baseline and ongoing monitoring help prevent complications such as bradycardia, tachycardia, or hypotension.
Receptor Specificity Affects Patient Response
Knowing whether a drug targets beta-1 (heart), beta-2 (lungs), or alpha receptors (vasculature) helps the nurse anticipate drug actions and side effects, especially in patients with comorbidities like asthma or hypertension.
Elderly Patients Are Highly Sensitive to Anticholinergics
Older adults are more prone to side effects such as dry mouth, urinary retention, confusion, and constipation. Dosing should be conservative, and close monitoring is required to prevent adverse outcomes.
Avoid Beta-Blockers in Asthma Unless Cardioselective
Non-selective beta-blockers like propranolol can induce bronchospasm. Nurses should question such orders in patients with respiratory conditions and monitor for dyspnea or wheezing.
Patient Education Prevents Medication Misuse
Teaching patients about expected effects—such as blurred vision with anticholinergics or increased urination with cholinergics—helps them distinguish between therapeutic outcomes and adverse effects.
Drug Interactions Can Exacerbate Autonomic Effects
Combining adrenergic drugs with digoxin, MAOIs, or other sympathomimetics increases the risk of arrhythmias or hypertensive crises. Nurses must review all current medications for potential interactions.
Anticholinergic Toxicity Requires Prompt Recognition
Signs like dry skin, flushed face, hyperthermia, and delirium signal anticholinergic overdose. Immediate medical attention and supportive care, including possible use of cholinesterase inhibitors, may be necessary.
Cholinergic Agonists Require GI and GU Assessment
Drugs like bethanechol enhance smooth muscle contraction. Nurses should assess bowel sounds and monitor for signs of bowel obstruction, abdominal pain, or excessive salivation.
Orthostatic Hypotension Is Common with Alpha Blockers
Alpha-adrenergic antagonists like prazosin can cause first-dose syncope. Instructing patients to change positions slowly and take the medication at bedtime can reduce fall risk.
Atropine Is Both Therapeutic and Antidotal
Nurses should recognize atropine's dual role: as a treatment for bradycardia and as an antidote for cholinergic overdose. Knowledge of its dosing and contraindications is crucial in emergencies.
Summary
Adrenergic agonists (sympathomimetics) like epinephrine and albuterol stimulate alpha and beta receptors, leading to increased heart rate, bronchodilation, pupil dilation, and vasoconstriction.
Adrenergic antagonists (beta-blockers) such as atenolol and metoprolol selectively block beta-1 receptors, lowering heart rate and blood pressure; must be used cautiously in asthma due to risk of bronchoconstriction.
Alpha blockers like prazosin cause vasodilation and are commonly used to manage hypertension and symptoms of benign prostatic hyperplasia (BPH).
Cholinergic agonists (parasympathomimetics) like bethanechol stimulate muscarinic receptors to enhance bladder and GI motility, commonly used to treat urinary retention and atonic bowel.
Cholinergic antagonists (anticholinergics) such as atropine and benztropine inhibit muscarinic receptors, leading to effects like increased heart rate, pupil dilation, decreased GI motility, and urinary retention.
Anticholinergic side effects—dry mouth, blurred vision, constipation, and urinary retention—are particularly pronounced in older adults and require careful monitoring.
Nursing considerations include monitoring vital signs, assessing for side effects (e.g., bradycardia, hypotension, bronchospasm), and educating patients on avoiding overheating and staying hydrated, especially with anticholinergics.
Adrenergic agents may interact with other sympathomimetics, beta-blockers, or digoxin, leading to altered cardiovascular effects and arrhythmias.
Parasympathomimetic overdose (e.g., from bethanechol) may cause cholinergic crisis (salivation, diarrhea, bradycardia, hypotension) and is treated with atropine, a muscarinic antagonist.
Understanding receptor selectivity (e.g., beta-1 vs beta-2) is essential to predict drug effects and minimize adverse reactions, especially in patients with comorbid respiratory or cardiovascular diseases.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drugs Affecting the Autonomic Nervous System
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


