Please set your exam date
Inflammation And Wound Healing
Study Questions
Practice Exercise 1
Which of the following is the primary role of macrophages during the proliferative phase of wound healing?
Explanation
Secreting growth factors that stimulate angiogenesis and collagen synthesis is the primary role of macrophages during the proliferative phase. In this phase, macrophages shift from primarily phagocytic activity (in the inflammatory phase) to a reparative role, releasing cytokines and growth factors such as VEGF and TGF-β, which promote new blood vessel formation and stimulate fibroblasts to produce collagen for tissue repair.
Rationale for correct answer:
3. Secreting growth factors: Macrophages act as key regulators of wound healing by promoting angiogenesis, fibroblast proliferation, and extracellular matrix production, all critical for granulation tissue formation.
Rationale for incorrect answers:
1. Initiating vasoconstriction: This is the role of platelets and vascular smooth muscle during the hemostasis phase, not the proliferative phase.
2. Phagocytizing bacteria and debris: This is the main macrophage role in the inflammatory phase, though some clearance may continue early in the proliferative stage.
4. Producing histamine: Histamine release comes mainly from mast cells and basophils during the early inflammatory response, not from macrophages in the proliferative phase.
Take home points:
- The proliferative phase focuses on tissue rebuilding, not just inflammation control.
- Macrophages transition from “clean-up crew” to “construction managers,” directing fibroblasts and endothelial cells.
- Growth factors from macrophages are essential for angiogenesis, collagen deposition, and granulation tissue formation.
Select all the cardinal signs of inflammation. Select all that apply
Explanation
Inflammation is the body’s protective response to injury, infection, or irritation. It aims to remove harmful stimuli, initiate tissue repair, and restore homeostasis. Clinically, inflammation is identified by a set of classic physical signs, first described in ancient Roman medicine, which indicate localized vascular and immune system activity in the affected area.
Rationale for correct answers:
1. Tumor: Refers to swelling, which occurs due to fluid accumulation and increased vascular permeability in the inflamed tissue.
3. Calor: Heat develops as a result of increased blood flow (hyperemia) to the inflamed area.
4. Rubor: Redness results from vasodilation and increased perfusion to the site of injury or infection.
5. Dolor: Pain occurs when chemical mediators such as bradykinin and prostaglandins stimulate sensory nerve endings.
Rationale for incorrect answer:
2. Palor: Paleness is not a feature of inflammation; in fact, inflammation typically causes redness (rubor), making palor the opposite of what is expected.
Take home points:
- The classic cardinal signs of inflammation are Rubor (redness), Calor (heat), Tumor (swelling), Dolor (pain), and sometimes Functio laesa (loss of function).
- These signs were first described by the Roman physician Celsus and remain key indicators of inflammation in modern medicine.
A patient presents with a deep, full-thickness burn. The wound bed is covered with eschar and a significant amount of necrotic tissue. Which of the following phases of wound healing is most likely to be delayed or inhibited by this condition?
Explanation
The proliferation phase of wound healing is most likely to be delayed or inhibited by the presence of eschar and necrotic tissue. During proliferation, fibroblasts, keratinocytes, and endothelial cells work to form granulation tissue, re-epithelialize the wound, and promote angiogenesis. Necrotic tissue and eschar act as a physical and biological barrier, preventing cell migration, impeding oxygen and nutrient delivery, and increasing infection risk. Debridement is often required to progress healing.
Rationale for correct answer:
3. Proliferation: This phase depends on a clean wound bed for granulation tissue formation and epithelialization. Necrotic tissue and eschar block this process, trapping bacteria and preventing new tissue growth.
Rationale for incorrect answers:
1. Hemostasis: This occurs immediately after injury to stop bleeding and would have already taken place before the proliferation phase begins.
2. Inflammation: While necrotic tissue can prolong inflammation, it doesn’t prevent it; in fact, it often triggers more inflammatory activity.
4. Maturation: This is the final phase involving collagen remodeling and scar strengthening, which occurs after proliferation; it cannot proceed until earlier phases are completed.
Take home points
- The proliferation phase requires a clean, well-vascularized wound bed.
- Necrotic tissue and eschar must be removed to allow granulation and re-epithelialization.
- Without debridement, wounds can stall in the inflammatory phase and fail to progress.
During the inflammatory phase of wound healing, which of the following events occur at the site of injury? Select all that apply
Explanation
During the inflammatory phase of wound healing, the body responds to injury by initiating immune and vascular processes to prevent infection and prepare the wound for tissue repair. Neutrophils are the first phagocytic cells to arrive, removing debris and bacteria. Local vasodilation increases blood flow, platelets release growth factors and cytokines to recruit immune cells, and increased vascular permeability allows plasma proteins and leukocytes to enter the wound site. Fibroblast migration and collagen synthesis occur later in the proliferative phase, not during inflammation.
Rationale for correct answers:
A. Neutrophils are the first phagocytic cells to arrive: Neutrophils infiltrate the wound within hours, removing pathogens and damaged tissue.
B. Vasodilation of local blood vessels: Mediated by histamine, prostaglandins, and nitric oxide, vasodilation increases delivery of immune cells and nutrients.
C. Platelets release growth factors and cytokines: These signals initiate inflammation and recruit additional immune cells to the wound.
E. Increased vascular permeability: This allows immune cells and plasma proteins to leave the bloodstream and enter the wound area for defense and repair preparation.
Rationale for incorrect answer:
D. Fibroblasts migrate into the wound to begin collagen synthesis: This is a hallmark of the proliferative phase, not the inflammatory phase.
Take home points
- Inflammation involves immune cell recruitment, vasodilation, and increased permeability.
- Platelets not only form clots but also signal immune and repair processes.
- Fibroblast-driven collagen synthesis occurs later, after the wound is cleaned and prepared.
What is the primary function of fibroblasts during the maturation phase of wound healing?
Explanation
-
During the maturation phase of wound healing, fibroblasts play a key role in producing and remodeling the collagen matrix, which increases the wound’s tensile strength. Collagen fibers are reorganized from a random to a parallel alignment, and excess collagen is broken down to improve the functional and structural integrity of the repaired tissue. This phase can last for months to years, depending on the wound.
Rationale for correct answer:
C. Producing and remodeling the collagen matrix to increase tensile strength: Fibroblasts are responsible for ongoing collagen production and remodeling, which gradually restores the wound’s structural stability and reduces scar thickness.Rationale for incorrect answers:
A. Clearing the wound of pathogens and dead cells: This is primarily the role of neutrophils and macrophages during the inflammatory phase.
B. Forming a fibrin clot to stop bleeding: This is the function of platelets during the hemostasis phase.
D. Creating new blood vessels to supply oxygen and nutrients: This occurs during angiogenesis in the proliferative phase, not during maturation.Take home points
- The maturation phase focuses on collagen remodeling and increased tensile strength.
- Fibroblasts remain active long after the wound has closed to optimize scar quality.
- Full tensile strength is never completely restored—healed wounds typically regain about 80% of their original strength.
Practice Exercise 2
Select all the modifiable risk factors for the development of pressure ulcers. Select all that apply
Explanation
Modifiable risk factors are those that can be changed or improved to reduce the likelihood of developing pressure ulcers. Immobility can be addressed through repositioning and mobility aids, incontinence can be managed with skin care and protective measures, and nutritional status can be improved with adequate protein, calorie, and micronutrient intake. Age and sensory perception deficits are non-modifiable, though their effects can be mitigated with preventive strategies.
Rationale for correct answers:
A. Immobility: Regular repositioning, mobility exercises, and assistive devices can significantly reduce ulcer risk.
C. Incontinence: Moisture from urine or feces breaks down skin; managing continence and protecting the skin can prevent ulcers.
D. Nutritional status: Adequate nutrition supports skin integrity and wound healing; deficiencies increase ulcer susceptibility.
Rationale for incorrect answers:
B. Age: Older adults are more susceptible due to thinner skin and comorbidities, but age itself cannot be changed.
E. Sensory perception deficits: Conditions like neuropathy reduce the ability to feel pressure, but the underlying deficit cannot be reversed (though compensatory measures can help).
Take home points
- Modifiable factors can be improved to lower ulcer risk, even in high-risk patients.
- Immobility, moisture, and poor nutrition are major preventable contributors.
- Non-modifiable risks require compensatory preventive care rather than direct change.
The primary etiological factor in the development of a pressure ulcer is:
Explanation
The primary cause of a pressure ulcer is prolonged compression of soft tissue between a bony prominence and an external surface. This sustained pressure exceeds capillary closing pressure, leading to impaired blood flow, tissue ischemia, and eventual cell death. While shear, friction, and moisture can worsen skin breakdown, they are considered contributing factors rather than the main cause.
Rationale for correct answer:
C. Compression of soft tissue between a bony prominence and an external surface: Continuous pressure obstructs blood supply, depriving tissues of oxygen and nutrients, which leads to ischemia and necrosis.
Rationale for incorrect answers:
A. Shear force, which is the stretching of the blood vessels: Shear exacerbates injury by distorting tissues and damaging blood vessels, but it is secondary to direct pressure.
B. Friction, which is the rubbing of skin against a surface: Friction removes superficial skin layers, increasing vulnerability but does not directly cause deep tissue ischemia.
D. Moisture, which leads to skin maceration: Moisture weakens the skin and increases susceptibility to pressure injury but is not the initiating cause.
Take home points
- Prolonged pressure over bony prominences is the main driver of pressure ulcer formation.
- Shear, friction, and moisture accelerate damage when pressure is already present.
- Prevention strategies focus on pressure redistribution and regular repositioning.
A nurse assesses a patient's sacral area and observes a shallow, open ulcer with a red-pink wound bed and no slough. This ulcer is best described as a:
Explanation
A shallow, open ulcer with a red-pink wound bed and no slough is characteristic of a Stage 2 pressure ulcer. This stage involves partial-thickness loss of the dermis and may present as an open ulcer or an intact/ruptured serum-filled blister. There is no exposure of subcutaneous tissue, muscle, or bone at this stage.
Rationale for correct answer:
B. Stage 2 pressure ulcer: Defined by partial-thickness skin loss involving the epidermis and/or dermis, presenting with a red-pink wound bed without slough.
Rationale for incorrect answers:
A. Stage 1 pressure ulcer: Involves non-blanchable erythema of intact skin, without ulceration or open wound.
C. Stage 3 pressure ulcer: Involves full-thickness skin loss with possible exposure of subcutaneous fat but no bone, tendon, or muscle.
D. Unstageable pressure ulcer: The wound base is obscured by slough or eschar, preventing accurate staging until debridement.
Take home points
- Stage 2 ulcers are partial-thickness and present as shallow red-pink wounds or blisters.
- Absence of slough and exposure of deeper structures differentiates Stage 2 from more severe stages.
- Accurate staging guides treatment and monitoring of healing progress.
A nurse assesses a pressure ulcer that is completely covered by thick, black eschar. Which of the following statements are true regarding this type of ulcer?
Explanation
A pressure ulcer covered completely by thick, black eschar is classified as unstageable because the wound bed and depth cannot be visualized. Debridement is typically necessary to remove the eschar and reveal the underlying tissue damage for accurate staging. Once treated, such wounds usually heal by secondary intention, where granulation tissue gradually fills the defect from the base upward.
Rationale for correct answers:
A. The true stage of the ulcer cannot be determined: The eschar blocks visibility of the wound base, making staging impossible until removal.
C. Debridement is necessary to determine the stage: Without removing the necrotic tissue, the extent of damage cannot be assessed.
D. The wound is likely to heal by secondary intention: This type of wound closes gradually through granulation tissue formation, contraction, and epithelialization.
Rationale for incorrect answer:
B. The wound bed is likely to be a Stage 2 or 3 ulcer beneath the eschar: The actual depth could range from Stage 3 to Stage 4; it cannot be assumed without direct visualization.
Take home points
- Ulcers fully covered by eschar are unstageable until debridement reveals the true depth.
- Secondary intention healing is common for deep pressure ulcers.
- Accurate staging is essential for selecting appropriate treatment and predicting outcomes.
A nurse is using the Braden Scale to assess a patient's risk for developing a pressure ulcer. A lower score on the Braden Scale indicates:
Explanation
B. Higher risk for pressure ulcer development: Scores of 18 or lower typically signal increased risk, with lower numbers indicating more severe risk factors.
Rationale for incorrect answers:
A. Lower risk for pressure ulcer development: A higher, not lower, Braden score indicates reduced risk.
C. The patient's skin is intact: Skin status is assessed separately; intact skin does not guarantee a low risk for ulcers.
D. The patient is fully mobile: Mobility is one factor in the scale, but the total score considers multiple risk factors.
Practice Exercise 3
When a nurse is performing patient teaching for a family member about preventing pressure ulcers, which of the following topics should be included? Select all that apply
Explanation
When teaching a family member about preventing pressure ulcers, the nurse should emphasize repositioning the patient at least every two hours, keeping the skin clean and dry to prevent maceration, encouraging a high-calorie, high-protein diet to promote skin integrity and healing, and providing range-of-motion exercises to improve circulation and reduce immobility. Donut-shaped cushions should be avoided because they concentrate pressure on surrounding tissue and can worsen skin breakdown.
Rationale for correct answers:
A. Repositioning the patient at least every two hours: Reduces prolonged pressure on bony prominences and promotes blood flow.
B. Keeping the skin clean and dry: Moisture control prevents maceration and reduces infection risk.
C. Encouraging the patient to eat a high-calorie, high-protein diet: Adequate nutrition supports skin repair and immune defense.
E. Providing range-of-motion exercises: Helps maintain mobility, prevent stiffness, and improve circulation.
Rationale for incorrect answer:
D. Using a donut-shaped cushion when the patient is sitting: These can create localized areas of high pressure, increasing the risk of ulcer development.
Take home points
- Prevention strategies focus on pressure relief, moisture control, good nutrition, and mobility.
- Donut-shaped cushions are harmful and should be avoided.
- Family education is essential to ensure consistent preventive care at home.
Which of the following is the most appropriate action for a nurse to take to prevent a pressure ulcer from becoming infected?
Explanation
The most appropriate action to prevent a pressure ulcer from becoming infected is ensuring proper hand hygiene and using aseptic technique during dressing changes. This reduces the introduction of pathogens into the wound and helps maintain a clean healing environment. While dressings, debridement, and antibiotics may be part of treatment, infection prevention starts with meticulous aseptic care.
Rationale for correct answer:
C. Ensuring proper hand hygiene and using aseptic technique during dressing changes: This is the most effective first-line measure to prevent contamination and infection in an open wound.
Rationale for incorrect answers:
A. Applying a transparent film dressing to the ulcer: May protect against external contaminants, but does not replace the need for aseptic handling.
B. Debriding the wound with a scalpel: Debridement is performed to remove necrotic tissue, but it is not specifically the primary infection prevention measure.
D. Administering a broad-spectrum antibiotic intravenously: Antibiotics are used when infection is present; they are not given prophylactically for all ulcers due to resistance risk.
Take home points
- Hand hygiene and aseptic technique are the foundation of infection prevention in wound care.
- Dressings and debridement support healing but are secondary to proper sterile handling.
- Antibiotics should be reserved for confirmed or strongly suspected infections, not routine prevention.
A patient with a Stage 4 pressure ulcer is being evaluated by a dietitian. Which of the following nutritional interventions are most important for promoting wound healing? Select all that apply
Explanation
For a patient with a Stage 4 pressure ulcer, adequate nutrition is essential to promote tissue repair and immune function. Increasing protein intake supports collagen synthesis and granulation tissue formation, vitamin C and zinc aid in collagen production and immune defense, and fruits and vegetables provide antioxidants, vitamins, and minerals that support healing. Fluid restriction and caloric restriction are generally not recommended unless medically indicated, as adequate hydration and energy intake are vital for repair.
Rationale for correct answers:
B. Increasing protein intake: Protein is essential for rebuilding damaged tissue and supporting immune function.
C. Providing vitamin C and zinc supplements: Vitamin C promotes collagen synthesis; zinc supports cell proliferation and immune function.
E. Increasing the intake of fruits and vegetables: Supplies essential vitamins, minerals, and antioxidants for wound healing and overall health.
Rationale for incorrect answers:
A. Limiting fluid intake to prevent edema: Adequate hydration is necessary for wound healing; fluid restriction can impair tissue repair unless clinically required.
D. Restricting caloric intake to prevent weight gain: Healing requires increased energy; calorie restriction can delay repair and worsen outcomes.
Take home points
- Wound healing demands increased protein, micronutrients, and antioxidants.
- Hydration and sufficient caloric intake are essential for repair.
- Nutritional deficiencies can significantly delay healing in advanced pressure ulcers.
A nurse is documenting a pressure ulcer on the heel of a bed-bound patient. The ulcer has full-thickness tissue loss, and subcutaneous fat is visible, but bone and muscle are not exposed. This is consistent with which stage of a pressure ulcer?
Explanation
A pressure ulcer with full-thickness tissue loss and visible subcutaneous fat, but without exposed bone, tendon, or muscle, is classified as Stage C. This stage may include undermining or tunneling, and slough may be present, but it does not obscure the depth of tissue loss.
Rationale for correct answer:
C. Stage 3: Defined by full-thickness skin loss extending into the subcutaneous tissue, with fat visible but no exposure of deeper structures such as bone or muscle.
Rationale for incorrect answers:
A. Stage 1: Involves non-blanchable erythema of intact skin, without any break in the surface.
B. Stage 2: Involves partial-thickness skin loss, presenting as a shallow ulcer or blister without visible fat or deeper structures.
D. Stage 4: Involves full-thickness tissue loss with exposed bone, tendon, or muscle, often with undermining or tunneling.
Take home points
- Stage 3 ulcers show full-thickness skin loss with visible subcutaneous fat but no deeper tissue exposure.
- Staging guides treatment and helps track healing progress.
- Correct identification ensures appropriate interventions to prevent further deterioration.
During patient teaching, a nurse should inform a patient with a pressure ulcer that the most effective way to reduce pressure on the wound is by:
Explanation
The most effective way to reduce pressure on a wound is by using specialized support surfaces, such as pressure-relieving mattresses or cushions. These devices help distribute weight more evenly, reduce pressure over bony prominences, and promote circulation, which is critical for healing. While dressings, elevation, and wound VACs can aid in healing, they do not directly relieve pressure to the same extent.
Rationale for correct answer:
C. Using specialized support surfaces, such as a pressure-relieving mattress or cushion: These are specifically designed to minimize sustained pressure, preventing further tissue damage and supporting wound healing.
Rationale for incorrect answers:
A. Using a wound vacuum-assisted closure (VAC) device: Promotes healing by removing exudate and improving blood flow, but it does not address the root cause of pressure injury—sustained pressure.
B. Elevating the affected body part with pillows: Can help in certain cases but may create new pressure points and is less effective than a full support surface.
D. Applying a hydrocolloid dressing to the wound: Helps maintain a moist healing environment but does not reduce pressure.
Take home points
- Pressure redistribution is the most important intervention for healing pressure ulcers.
- Support surfaces complement, but do not replace, repositioning schedules.
- Treating the cause (pressure) is as important as treating the wound itself.
Comprehensive Questions
A patient 1 day postoperative after abdominal surgery has incisional pain, 99.5° F temperature, slight erythema at the incision margins, and 30 mL serosanguineous drainage in the Jackson-Pratt drain. Based on this assessment, what conclusion would the nurse make?
Explanation
The normal inflammatory response is a complex and essential defense mechanism triggered by tissue injury, infection, or harmful stimuli. It involves vascular changes, cellular infiltration, and the release of chemical mediators like histamine, prostaglandins, and cytokines. This response aims to eliminate the cause of injury, clear out damaged cells, and initiate tissue repair. Recognizing the signs of acute inflammation, including redness, swelling, heat, pain, and loss of function, is critical in clinical assessment.
Rationale for Correct Answer:
B. The described findings are consistent with a normal localized inflammatory response to surgery. Mild fever (under 100.4°F), incisional discomfort, slight redness, and minimal serosanguineous drainage are common in the immediate postoperative period and typically resolve as healing progresses.
Rationale for Incorrect Answers:
A. Signs of infection include increasing erythema, purulent drainage, swelling, worsening pain, and a temperature greater than 100.4°F. The patient's symptoms do not meet the criteria for infection.
C. Impending dehiscence is often signaled by sudden drainage of large amounts of serosanguineous fluid, separation of wound edges, or visible underlying tissue. These signs are not present in this case.
D. Notifying the physician is not necessary at this time since the findings are within expected postoperative parameters. Routine monitoring is appropriate unless changes occur.
Key Takeaways:
- Mild erythema, low-grade fever, and minimal drainage are expected in early postoperative healing.
- A normal inflammatory response should not be mistaken for infection or dehiscence.
- Knowing typical vs. abnormal postoperative signs is essential for accurate nursing assessments.
The nurse assessing a patient with a chronic leg wound finds local signs of erythema and pain at the wound site. What would the nurse anticipate being ordered to assess the patient’s systemic response?
Explanation
The systemic response to inflammation occurs when inflammatory mediators affect the entire body rather than just the site of injury. Key features include fever, leukocytosis, malaise, anorexia, and increased heart rate and respiratory rate. These effects are triggered by cytokines such as interleukin-1 (IL-1) and tumor necrosis factor (TNF) released into the bloodstream. The systemic response plays a vital role in enhancing immune function and supporting the body’s effort to fight infection or injury.
Rationale for Correct Answer:
B. WBC count and differential are standard laboratory tests used to evaluate for systemic inflammation or infection. In a patient with local signs such as erythema and pain, the WBC can help determine whether the infection is spreading or remains localized.
Rationale for Incorrect Answers:
A. Serum protein analysis evaluates nutritional status and protein levels (e.g., albumin), which can affect wound healing, but it does not directly assess for systemic infection or inflammation.
C. A punch biopsy can provide histological information about chronic wounds, especially if malignancy or atypical causes are suspected, but it is not routinely used to assess systemic response.
D. Culture and sensitivity are used to identify the causative organism at the wound site and guide antibiotic therapy but do not measure the body’s systemic response to infection.
Key Takeaways:
- A WBC count with differential helps determine the presence and extent of systemic infection or inflammation.
- Culture and sensitivity assess local infection but not systemic response.
- Nutritional markers and biopsy may support wound management but are not first-line tests for systemic assessment.
A patient in the unit has a 10C.7°F temperature. Which intervention would be most effective in restoring normal body temperature?
Explanation
Fever management involves strategies to reduce elevated body temperature and alleviate discomfort while addressing the underlying cause. Key interventions include administering antipyretic medications such as acetaminophen or ibuprofen, promoting adequate fluid intake to prevent dehydration, and ensuring rest to conserve energy. In cases of high fever, cooling measures like tepid sponge baths or a cooling blanket may be used. It is important to monitor for signs of infection, dehydration, and worsening symptoms requiring further medical attention.
Rationale for Correct Answer:
B. Antipyretics such as acetaminophen or ibuprofen act on the hypothalamus to lower the body’s set point for temperature regulation. Administering them on a scheduled basis helps control fever more effectively than PRN dosing, preventing temperature spikes and promoting patient comfort.
Rationale for Incorrect Answers:
A. A cooling blanket may be used for very high fevers, but it can cause shivering, which increases metabolic demand and discomfort. It is typically reserved for heatstroke or when antipyretics are ineffective.
C. Increased fluids and sponge baths help with hydration and comfort but do not directly affect the hypothalamic temperature regulation set point. These are supportive measures, not primary interventions.
D. Antibiotics treat the underlying cause if the fever is due to a bacterial infection, but they do not directly reduce fever. Warm blankets may provide comfort during chills but will not help reduce body temperature.
Key Takeaways:
- Around-the-clock antipyretic administration is the most effective intervention for sustained fever reduction.
- Supportive measures like fluids and sponge baths help with comfort but do not replace pharmacologic treatment.
- Cooling blankets and antibiotics have specific roles but are not first-line interventions for fever control.
A nurse is caring for a patient who has a pressure ulcer that is treated with debridement, irrigations, and moist gauze dressings. How should the nurse anticipate healing to occur?
Explanation
Healing by secondary intention occurs when a wound is left open and allowed to heal naturally without primary closure. This process is typical for wounds with extensive tissue loss, infection, or irregular wound edges, such as pressure ulcers, traumatic injuries, or surgical wounds left open. Healing involves granulation tissue formation, wound contraction, and epithelialization, resulting in longer healing time, increased scar formation, and higher risk of infection compared to primary intention healing.
Rationale for Correct Answer:
B. Secondary intention healing is typical for pressure ulcers and other wounds with significant tissue loss. These wounds are not closed surgically but instead heal gradually through the formation of granulation tissue, wound contraction, and epithelialization over time.
Rationale for Incorrect Answers:
A. Tertiary intention healing (also called delayed primary closure) involves initially leaving a wound open due to contamination or infection risk, then surgically closing it later. This is not typical for pressure ulcers managed conservatively.
C. Regeneration of cells refers to the replacement of lost cells with the same type of cells (as in superficial skin wounds or liver tissue), but pressure ulcers usually involve deeper tissue layers requiring granulation and scarring.
D. Remodeling of tissues is the final phase of wound healing, not the type or process of healing. It involves strengthening of collagen and scar formation after the wound has closed.
Key Takeaways:
- Pressure ulcers typically heal by secondary intention due to tissue loss and open wound management.
- Secondary intention involves granulation, contraction, and epithelialization.
- Tertiary intention and regeneration apply to different wound contexts and healing types.
A nurse is caring for a patient with diabetes who is scheduled for amputation of his necrotic left great toe. The patient’s WBC count is 1E.0 × 106/μL, and he has coolness of the lower extremities, weighs 75 lb more than his ideal body weight, and smokes two packs of cigarettes per day. Which priority nursing diagnosis addresses the primary factor affecting the patient’s ability to heal?
Explanation
Several factors affect wound healing, influencing the speed and quality of recovery. Local factors include infection, poor blood supply, edema, and excessive pressure at the wound site. Systemic factors involve age, nutritional status, chronic diseases such as diabetes, smoking, obesity, and the use of immunosuppressive drugs like corticosteroids. Effective wound care requires addressing both local and systemic factors to promote tissue regeneration, prevent complications, and support optimal healing outcomes.
Rationale for Correct Answer:
C. Diabetes and smoking both lead to vascular damage and peripheral arterial disease, severely impairing tissue perfusion. Impaired blood flow prevents oxygen and nutrient delivery to the wound, which is essential for healing. This makes ineffective peripheral tissue perfusion the most critical concern.
Rationale for Incorrect Answers:
A. While imbalanced nutrition contributes to poor healing, in this case it is not the most immediate or primary barrier. The necrosis and need for amputation point to severely compromised circulation as the priority.
B. Impaired tissue integrity reflects the wound’s condition, but it does not directly address the underlying cause of poor healing. A diagnosis focusing on perfusion is more appropriate and foundational.
D. Coping may be an issue, but addressing physiological needs like perfusion takes priority in wound healing and surgical recovery.
Key Takeaways:
- Peripheral perfusion is essential for tissue healing, especially in diabetic clients with vascular disease.
- Smoking and diabetes compound the risk of poor wound healing due to impaired circulation.
- Addressing ineffective perfusion takes precedence over nutritional or psychosocial concerns in this context.
Which one of the orders should a nurse question in the plan of care for a patient with a stage III pressure ulcer?
Explanation
Care for a stage III pressure ulcer focuses on promoting healing, preventing infection, and relieving pressure. These full-thickness wounds extend into subcutaneous tissue but not through underlying fascia. Key interventions include regular repositioning to reduce pressure, using pressure-relieving devices (e.g., specialty mattresses), cleansing the wound with non-cytotoxic solutions, and debriding necrotic tissue as needed. Apply moist dressings like foam or hydrocolloid, monitor for signs of infection, and ensure adequate nutrition to support tissue repair.
Rationale for Correct Answer:
C. Dakin’s solution is cytotoxic and can harm viable tissue if used too frequently or without clear indication of heavy infection. Its routine use every shift is not evidence-based for a stage III pressure ulcer, which requires promotion of healing through preservation of healthy tissue and moisture balance.
Rationale for Incorrect Answers:
A. Packing with foam dressing is appropriate for stage III ulcers, which may have depth requiring absorbent and conformable dressings that maintain moisture and fill dead space.
B. Turning and positioning every 2 hours is a critical intervention to prevent worsening of pressure ulcers and support healing by reducing pressure on affected areas.
D. Pain assessment and pre-medication before dressing changes are standard practice to improve patient comfort and compliance with wound care.
Key Takeaways:
- Dakin’s solution can impair healing if used excessively due to its cytotoxic effects.
- Appropriate wound care for stage III ulcers includes moist dressings, pressure relief, and pain control.
- Nursing interventions should support healing while minimizing tissue damage.
An 85-year-old patient is assessed to have a score of 16 on the Braden Scale. Based on this information, how should the nurse plan for this patient’s care?
Explanation
Pressure ulcer prevention involves strategies to reduce prolonged pressure, enhance skin integrity, and promote mobility. Key interventions include frequent repositioning (at least every 2 hours), using pressure-relieving surfaces such as specialty mattresses or cushions, and conducting daily skin assessments for early signs of breakdown. Maintain clean, dry skin, manage moisture from incontinence or perspiration, ensure adequate hydration and nutrition, and encourage mobility or activity as tolerated to reduce the risk of pressure injury.
Rationale for Correct Answer:
A. A Braden Scale score of 16 signifies moderate risk for skin breakdown. Evidence-based care for such patients includes repositioning every 2 hours and routine skin assessments to prevent pressure ulcer development.
Rationale for Incorrect Answers:
B. DuoDerm is typically used to protect areas at higher risk or to treat existing ulcers. It may be appropriate later but is not the first-line preventive action for a score of 16.
C. Elevating the head of bed to 90 degrees increases pressure and shear on the sacrum and is contraindicated in patients at risk for skin breakdown.
D. Weekly skin assessments without any special precautions are inadequate for someone with a moderate risk. Regular assessment and repositioning are essential.
Key Takeaways:
- A Braden Scale score of 16 indicates moderate risk and necessitates proactive measures.
- Turning every 2 hours and frequent skin assessments are standard prevention practices.
- Avoid high Fowler's position (90°) to reduce shear and pressure on vulnerable areas.
A 65-year-old stroke patient with limited mobility has a purple area of suspected deep tissue injury on the left greater trochanter. Which nursing diagnoses is/are most appropriate? Select all that apply
Explanation
A pressure ulcer, also known as a decubitus ulcer or bedsore, is a localized injury to the skin and underlying tissue usually over a bony prominence, caused by prolonged pressure, shear, or friction. These ulcers commonly develop in individuals with limited mobility, such as those who are bedbound or wheelchair-bound. Pressure ulcers are staged from Stage I (non-blanchable erythema) to Stage IV (full-thickness tissue loss with exposed bone, tendon, or muscle). Prevention and early intervention are key to improving outcomes.
Rationale for Correct Answers:
A. Acute pain is appropriate because deep tissue injuries can be painful due to underlying tissue inflammation and damage.
B. The patient is experiencing reduced mobility and sensation, increasing their risk for skin breakdown
C. Impaired tissue integrity is the correct diagnosis for suspected deep tissue injury, which affects underlying tissues and not just the skin surface.
D. Risk for infection is valid as tissue breakdown compromises the skin barrier, and undernutrition post-stroke further impairs immune response and healing capacity.
Key Takeaways:
- Deep tissue injuries are best described by impaired tissue integrity, not skin integrity.
- Pain and risk for infection are key concerns in managing pressure-related injuries.
- Accurate nursing diagnoses guide appropriate interventions and care planning.
An 82-year-old man is being cared for at home by his family. A pressure ulcer on his right buttock measures 1 × 2 × 0.8 cm in depth, and pink subcutaneous tissue is completely visible on the wound bed. Which stage would the nurse document on the wound assessment form?
Explanation
Pressure ulcer staging is a standardized method used by healthcare professionals to assess the severity, depth, and extent of tissue damage caused by prolonged pressure. Accurate staging is essential for effective treatment planning, monitoring wound healing, and preventing complications. The stages range from non-blanchable erythema in intact skin to full-thickness tissue loss with exposed muscle or bone, including unstageable wounds and suspected deep tissue injuries.
Rationale for Correct Answer:
C. Stage III pressure ulcers involve full-thickness tissue loss with visible subcutaneous fat. The presence of depth (0.8 cm) and exposure of subcutaneous tissue confirms it is beyond a superficial wound, placing it in Stage III.
Rationale for Incorrect Answers:
A. Stage I involves intact skin with non-blanchable erythema—there is no open wound or tissue loss.
B. Stage II includes partial-thickness loss of dermis and presents as a shallow open ulcer, but subcutaneous tissue is not exposed.
D. Stage IV includes full-thickness tissue loss with exposed bone, tendon, or muscle—none of which are visible in this case.
Key Takeaways:
- Stage III ulcers show full-thickness tissue loss with subcutaneous fat visible but no exposure of bone or muscle.
- Stage II ulcers involve partial-thickness skin loss, while Stage IV involves deeper structures like bone or tendon.
- Accurate staging is essential for appropriate wound care planning and documentation.
Key interventions for treating soft tissue injury and resulting inflammation are remembered using the acronym RICE. What are the most important actions for the emergency department nurse to do for the patient with an ankle injury?
Explanation
The RICE method—Rest, Ice, Compression, and Elevation—is a first-line intervention used to manage soft tissue injuries such as sprains, strains, and contusions. This approach helps reduce inflammation, minimize pain, and promote healing. Rest prevents further injury, ice constricts blood vessels to decrease swelling, compression supports the injured area, and elevation aids in venous return, reducing fluid accumulation and tissue damage.
Rationale for Correct Answer:
C. RICE stands for Rest, Ice, Compression, and Elevation. These actions reduce swelling, limit further injury, decrease pain, and promote healing in acute soft tissue injuries such as ankle sprains.
Rationale for Incorrect Answers:
A. Shining light on the wound and eliciting history are not part of RICE and do not address immediate injury management.
B. Rubbing the wound clean is inappropriate and can cause further tissue damage. Exercising the leg immediately after injury can worsen it.
D. Rinsing the wound and imaging may be needed but are not components of the RICE protocol. Carrying and extending the ankle are also not appropriate immediate interventions.
Key Takeaways:
- RICE stands for Rest, Ice, Compression, and Elevation, and is the standard first-aid for soft tissue injuries.
- These measures help reduce inflammation, swelling, and pain.
- Immediate exercise or rubbing the wound can worsen injury and delay healing.
What is characteristic of chronic inflammation?
Explanation
Chronic inflammation is a prolonged and often maladaptive immune response that can last for weeks, months, or even years. Unlike acute inflammation, which resolves after the harmful stimulus is removed, chronic inflammation occurs when the injurious agent persists or the body’s immune regulation fails. It is characterized by ongoing tissue destruction, lymphocyte and macrophage infiltration, and fibrosis or scarring. Chronic inflammation underlies many conditions like rheumatoid arthritis, inflammatory bowel disease, and atherosclerosis.
Rationale for Correct Answer:
B. Chronic inflammation occurs when the harmful stimulus is not removed, causing ongoing tissue injury and repair. This leads to a prolonged inflammatory response that can last months or years.
Rationale for Incorrect Answers:
A. Inflammation lasting 2 to 3 weeks is more typical of subacute or acute inflammation, not chronic.
C. Infective endocarditis may have both acute and chronic features but is not exclusively a classic example of chronic inflammation.
D. Neutrophils dominate in acute inflammation; chronic inflammation is characterized more by macrophages, lymphocytes, and plasma cells.
Key Takeaways:
- Chronic inflammation involves a persistent or recurring injurious agent.
- It leads to prolonged tissue damage and repair, often involving different immune cells than acute inflammation.
- Neutrophils are predominant in acute inflammation, whereas chronic inflammation involves macrophages and lymphocytes.
What is the primary difference between healing by primary intention and healing by secondary intention?
Explanation
Healing by primary intention refers to the process in which a clean surgical or traumatic wound with well-approximated edges heals with minimal tissue loss and low risk of infection. This type of healing involves epithelial regeneration, minimal granulation tissue formation, and rapid wound closure. Typically seen in surgical incisions closed with sutures, staples, or adhesive strips, primary intention results in faster healing, less scarring, and a lower complication rate compared to other healing types.
Rationale for Correct Answer:
C. Secondary intention healing occurs when wounds are left open to heal naturally, resulting in abundant granulation tissue formation and a larger scar. Primary intention involves clean, surgically closed wounds with minimal granulation and scarring.
Rationale for Incorrect Answers:
A. Secondary healing does not always require surgical debridement; it depends on wound condition.
B. Primary healing involves suturing the edges of a clean wound, not suturing granulation tissue.
D. Secondary intention takes longer, but the main difference is the amount of granulation tissue and scarring, not merely the number of healing steps.
Key Takeaways:
- Primary intention involves direct closure with minimal granulation and scarring.
- Secondary intention involves open wound healing with extensive granulation and more scarring.
- Healing duration is longer in secondary intention due to tissue loss and repair needs.
The patient is admitted from home with a stage II pressure ulcer. This wound is classified as a yellow wound using the red-yellow-black concept of wound care. What is the nurse likely to observe when she does her wound assessment?
Explanation
Yellow wounds are characterized by the presence of slough, which is a soft, moist, yellowish necrotic tissue made up of dead white blood cells, fibrin, and cellular debris. These wounds often have drainage and may show signs of infection or delayed healing. The primary goal in managing yellow wounds is to remove slough through cleansing, irrigation, or debridement, and to create a moist wound environment that promotes granulation tissue formation and tissue regeneration.
Rationale for Correct Answer:
D. Yellow wounds contain slough, which appears as creamy or yellow-green drainage. This exudate often indicates the presence of dead tissue and possibly infection, requiring cleansing and debridement.
Rationale for Incorrect Answers:
A. Serosanguineous drainage is usually seen in clean, healing wounds and is more associated with red wounds.
B. Adherent gray necrotic tissue describes a black wound with eschar, not a yellow wound.
C. Clean, moist granulating tissue is characteristic of a red wound, indicating healthy healing tissue.
Key Takeaways:
- Yellow wounds contain slough and have yellowish exudate, requiring cleansing.
- Red wounds show granulation tissue and are signs of healing.
- Black wounds have necrotic eschar and require debridement.
Which patient is at the greatest risk for developing pressure ulcers?
Explanation
Risk factors for pressure ulcers include conditions and circumstances that compromise skin integrity or reduce blood flow, leading to tissue breakdown. Key risk factors are immobility, incontinence, malnutrition, advanced age, neurological impairments, and chronic illnesses such as diabetes or vascular disease. Other contributors include friction, shear, and moisture, which weaken the skin barrier. Identifying these risk factors early allows for targeted preventive interventions to reduce the risk of pressure ulcer development.
Rationale for Correct Answer:
C. Comatose patients have severely limited mobility and impaired ability to sense and respond to pressure, which greatly increases the risk of pressure ulcer development. Prolonged immobility and inability to reposition independently are primary risk factors.
Rationale for Incorrect Answers:
A. Although obesity and diabetes increase risk factors for complications, the patient’s mobility is likely better preserved compared to a comatose patient.
B. Advanced age, confusion, and malnutrition increase risk but a comatose state generally presents a more immediate and severe risk due to total immobility.
D. Incontinence increases moisture-related skin breakdown but is less critical compared to the immobility and sensory loss in coma.
Key Takeaways:
- Complete immobility and inability to reposition, such as in coma, is a major risk factor for pressure ulcers.
- Sensory loss and impaired consciousness increase risk due to lack of protective responses.
- Other factors like malnutrition, age, and incontinence compound the risk but immobility is the greatest risk.
The patient’s wound is not healing, so the health care provider is going to send the patient home with negative pressure wound therapy or a “wound vac” device. What will the caregiver need to understand about the use of this device?
Explanation
A wound VAC (Vacuum-Assisted Closure) is a type of negative pressure wound therapy used to promote wound healing in both acute and chronic wounds. The device uses controlled suction to remove exudate, decrease bacterial load, and increase blood flow to the wound bed. A foam dressing is applied to the wound, sealed with an occlusive drape, and connected to a vacuum pump. This method supports the formation of granulation tissue and faster wound closure.
Rationale for Correct Answer:
C. The wound vac works by applying negative pressure to the wound through a sealed, airtight dressing. Proper sealing is essential to maintain suction, remove exudate, reduce edema, and promote granulation tissue formation.
Rationale for Incorrect Answers:
A. The wound is not cleaned daily; the dressing changes and wound care follow specific protocols, often less frequently than daily.
B. Hyperbaric oxygen therapy is a separate treatment and not part of wound vac therapy.
D. Nutrition remains critically important for wound healing, even when using wound vac therapy.
Key Takeaways:
- A tightly sealed occlusive dressing is essential for effective negative pressure wound therapy.
- Wound vac therapy promotes healing by removing fluid and stimulating tissue growth.
- Proper nutrition continues to play a vital role in wound healing with or without wound vac therapy.
Practice Exercise 3
A nurse is teaching a client with COPD about a newly prescribed albuterol (Proventil). Which statement by the client demonstrates correct understanding of the medication?
Explanation
Albuterol is a selective beta2-adrenergic agonist that induces bronchial smooth muscle relaxation. It works by stimulating adenyl cyclase to increase cyclic AMP levels, effectively reversing bronchoconstriction during acute exacerbations. However, higher doses can lose selectivity, affecting cardiac receptors and causing transient systemic side effects during clinical respiratory therapy.
Rationale for correct answer
3. Albuterol primarily targets beta2 receptors but can stimulate beta1 receptors in the heart, leading to a faster heart rate or palpitations. This is a common and expected sympathomimetic side effect that the nurse must include in the patient education to prevent unnecessary anxiety during medication use.
Rationale for incorrect answers
1. Systemic corticosteroids are well-known to increase blood glucose levels, but short-acting beta2 agonists like albuterol do not typically have this metabolic effect. Therefore, the client's statement regarding hyperglycemia is clinically incorrect for this specific rescue inhaler and would indicate a need for further medication clarification.
2. Unlike inhaled or systemic corticosteroids which can cause localized or systemic immune suppression, albuterol does not impair the body’s defenses. It is a bronchodilator with no anti-inflammatory or immunosuppressive properties, making this statement an incorrect understanding of how the drug affects the client's overall health.
4. Development of mouth sores or oral candidiasis is a classic side effect associated with inhaled corticosteroids, not bronchodilators like albuterol. These fungal infections occur due to local immunosuppression in the oropharynx, whereas albuterol’s side effect profile is primarily related to nervous system and cardiovascular stimulation.
Test-taking strategy
- Identify the drug class of albuterol as a sympathomimetic bronchodilator and recall its common side effects.
- Differentiate between the effects of bronchodilators (tachycardia, tremors) and inhaled corticosteroids (thrush, immune suppression).
- Recognize that sympathetic nervous system activation naturally results in an increased heart rate and potentially mild tremors.
- Rule out metabolic or immunological changes that are characteristic of different classes of respiratory medications like steroids.
Take home points
- Albuterol is a rescue medication used for rapid relief of acute bronchospasm in obstructive lung diseases.
- Common side effects include tachycardia, palpitations, tremors, and occasionally a sense of nervousness or anxiety.
- Use of albuterol can cause a temporary shift of potassium into cells, potentially leading to mild hypokalemia.
- Clients should be taught to monitor their pulse and report any significant or persistent cardiac palpitations.
A nurse is educating a client on the proper use of an incentive spirometer. Which statement made by the client indicates correct understanding of the instructions?
Explanation
Incentive spirometry utilizes sustained maximal inspiration to increase transpulmonary pressure and inspiratory volumes. This mechanical intervention promotes alveolar expansion, effectively reversing atelectasis by facilitating collateral ventilation through the pores of Kohn. Improved surfactant distribution and gas exchange make it a critical tool in postoperative pulmonary hygiene.
Rationale for correct answer
4. The client must inhale deeply and perform a brief end-inspiratory pause to stabilize the distal air spaces for maximal recruitment. This hold of the breath ensures the inspired air distributes evenly throughout the lung parenchyma. Such action maximizes the therapeutic effect on pulmonary expansion.
Rationale for incorrect answers
1. The client is confusing the incentive spirometer with a pulse oximeter, which non-invasively monitors arterial oxygen saturation. An incentive spirometer is a mechanical breathing tool requiring active patient participation through inhalation. It is not a passive sensor attached to the finger or earlobe.
2. Patients should be positioned in a high-Fowler or semi-Fowler position to allow for maximum diaphragmatic excursion and chest wall expansion. Recumbent positioning increases abdominal pressure against the diaphragm. This significantly hinders the patient's ability to achieve the deep inspiratory volumes required for effective therapy.
3. Placing a hand over the abdomen is a technique used in diaphragmatic breathing to monitor muscle movement. It does not add resistance to the incentive spirometer. The device provides visual feedback for flow, and manual resistance would be counterproductive to achieving a slow, deep inspiratory effort.
Test-taking strategy
- Identify the primary goal of the incentive spirometer as encouraging deep inhalation to prevent or treat atelectasis.
- Distinguish between inhalation (correct for spirometry) and exhalation (correct for peak flow meters or pursed-lip breathing).
- Rule out positioning errors because upright posture is essential for optimal lung expansion and diaphragmatic movement.
- Connect the concept of collateral ventilation to the need for a sustained breath-hold at the peak of inspiration.
Take home points
- The incentive spirometer is used to encourage voluntary, deep, and sustained inhalation.
- Patients should be instructed to perform 5 to 10 repetitions every hour while awake to prevent respiratory complications.
- A visual indicator on the device helps the patient maintain a slow and steady inspiratory flow rate.
- Effective use requires an upright sitting position and a tight seal around the mouthpiece to ensure accurate volume measurement.
A nurse is teaching a client about oxygen delivery systems. The nurse asks which feature is characteristic of a partial rebreathing mask.
Explanation
A partial rebreathing mask is an oxygen-delivery device that provides moderate to high concentrations of oxygen (≈40–70%) at flow rates of 6–10 L/min. It has a reservoir bag without one-way valves, allowing the client to rebreathe the first portion of exhaled air (rich in oxygen) while preventing carbon dioxide accumulation when used correctly.
Rationale for correct answer
2. The defining characteristic of a partial rebreathing mask is the reservoir bag, which collects the first third of the client's exhaled air. Because this initial portion of exhaled air comes from the anatomic dead space, it is rich in oxygen and lacks carbon dioxide, allowing it to be re-inhaled alongside fresh oxygen. This mechanism significantly increases the inspired oxygen concentration compared to a standard simple mask.
Rationale for incorrect answers
1. Partial rebreathing masks are generally used for short-term therapy in patients who require higher oxygen concentrations during acute respiratory distress. They are not suitable for long-term therapy because the mask is hot, confining, and interferes with essential activities like eating and talking. Long-term management typically utilizes more stable and comfortable devices like a nasal cannula.
3. The non-rebreather mask, not the partial rebreather, provides the highest oxygen concentrations (up to 90% to 100%). The non-rebreather is equipped with one-way valves that prevent any exhaled air from entering the reservoir bag and prevent room air from entering the mask. The partial rebreather allows some mixing of air, resulting in a lower fraction of inspired oxygen (FiO2).
4. The nasal cannula is the device that is most comfortable and causes the least restriction on the patient's activities. It allows the client to eat, drink, and speak without interrupting the oxygen flow. Masks, by contrast, are more restrictive and can cause skin breakdown over the bridge of the nose and behind the ears during prolonged use.
Test-taking strategy
- Differentiate between the Partial Rebreather (no valves) and the Non-Rebreather (one-way valves) to identify which provides higher FiO2.
- Associate the term "Reservoir" with masks designed to deliver oxygen concentrations between 40% and 70%.
- Evaluate the patient's activity level; if they need to eat, a mask is never the "most comfortable" or "least restrictive" choice.
- Remember that any device with a bag must have the flow rate high enough (usually 6 to 15 L/min) to keep the bag from collapsing during inspiration.
Take home points
- A partial rebreather delivers an FiO2 of approximately 40% to 70%.
- The reservoir bag must remain at least one-third to one-half full on inspiration to ensure the patient receives the intended dose.
- Partial rebreathers do not have the one-way valves found on non-rebreather masks, allowing the "partial rebreathing" of dead-space air.
- Close monitoring for skin irritation and proper mask seal is required to maintain therapeutic oxygen levels.
A nurse is planning postural drainage for a client with COPD. The nurse considers which actions are essential to ensure safety and effectiveness during the procedure.
Explanation
Postural drainage utilizes specific body positions to harness gravity for the clearance of tracheobronchial secretions. Segmental bronchi are aligned vertically to facilitate the movement of mucus from peripheral lung fields toward the central airways. This mechanical intervention is essential for managing mucus hypersecretion and preventing secondary bacterial colonization in patients with impaired mucociliary clearance or chronic obstructive lung disease.
Rationale for correct answer
3. The nurse must prioritize the assessment of the patient's tolerance for Trendelenburg or head-down positions to prevent dangerous complications. Significant physiological stress from these positions can increase intracranial pressure or cause severe dyspnea. This safety evaluation is the most critical step before beginning the drainage procedure for a compromised client.
Rationale for incorrect answers
1. Standard nursing protocols typically recommend scheduling the procedure at least 2 hours after meals to minimize the risk of vomiting or aspiration. A timeframe of only 1 hour after a meal is insufficient and could lead to gastric distress. Positional changes require an empty stomach to ensure patient safety and comfort.
2. Effective airway clearance requires the patient to remain in the drainage position for several minutes to allow gravity to mobilize the secretions. A cough before positioning is counterproductive because the mucus has not yet moved into the larger, central airways. The final step of the procedure should be expectoration once secretions have migrated.
4. The correct clinical sequence requires the nurse to place the patient in the appropriate positioning first before applying manual techniques like percussion or vibration. These adjunctive maneuvers are specifically designed to shake secretions loose while the lung segment is superior to the carina. This ensures that the loosened mucus moves toward the trachea immediately.
Test-taking strategy
- Identify the safety priority among the options, as nursing questions often emphasize the assessment of patient stability and risk reduction.
- Recognize that gravity is the primary driver of postural drainage, meaning positioning must occur before manual techniques like vibration.
- Apply knowledge of gastric emptying to rule out timing that occurs too soon after a meal.
- Distinguish between the functional goal of the procedure and the final step of coughing to expectorate.
Take home points
- Postural drainage positions are held for 3 to 15 minutes to allow gravity to mobilize secretions.
- Head-down positions are contraindicated in patients with increased intracranial pressure, heart failure, or severe hypertension.
- Percussion and vibration should be performed during the drainage session to enhance mucus movement.
- Always encourage the patient to perform huff coughing or a deep cough after the drainage is complete.
A nurse is caring for a client experiencing an acute exacerbation of mild COPD. The nurse identifies ineffective breathing pattern related to airway obstruction and anxiety. What is the best immediate action for the nurse to take?
Explanation
Acute exacerbations induce severe airway resistance and dynamic hyperinflation, significantly increasing the work of breathing. Patients often adopt the tripod position to optimize the mechanical advantage of the diaphragm and accessory muscles. This posture stabilizes the pectoralis muscles to assist in thoracic expansion while reducing the metabolic demand of ventilation.
Rationale for correct answer
4. Upright positioning with the elbows resting on an over-the-bed table facilitates the use of accessory muscles and improves diaphragmatic excursion. This immediate intervention provides the fastest mechanical relief for dyspnea by maximizing thoracic volume. Correct posture also helps stabilize the patient and reduces the anxiety associated with the feeling of suffocation.
Rationale for incorrect answers
1. Administration of routine medications is a necessary component of long-term management but does not address the immediate, acute distress. The nurse must prioritize non-pharmacological stabilization techniques that offer instant relief before waiting for the onset of pharmacological agents. Routine orders may not be sufficient during an acute exacerbation requiring rapid stabilization.
2. Chest physiotherapy is an intensive procedure that can actually increase the oxygen demand and worsen the anxiety of a patient. Such techniques are generally reserved for periods of stability to manage chronic secretions. Performing percussion during an active dyspneic episode can further compromise the patient’s limited respiratory reserve and increase the physical workload.
3. Delivery of oxygen at 5 L/min is inappropriately high for a COPD patient and carries the risk of suppressing the hypoxic respiratory drive. Excessive oxygenation can lead to carbon dioxide retention and worsening respiratory acidosis. Oxygen therapy must be titrated carefully to maintain a saturation between 88% and 92% rather than using high flow rates.
Test-taking strategy
- Identify the immediate nursing action that provides the fastest relief for an ineffective breathing pattern and anxiety.
- Choose the least invasive and most rapid physiological intervention, which is typically repositioning the patient.
- Recall the contraindications of high-flow oxygen in COPD patients to eliminate unsafe interventions.
- Distinguish between acute stabilization maneuvers and chronic maintenance therapies like chest physiotherapy.
Take home points
- The tripod position helps stabilize the shoulder girdle to allow accessory muscles to assist in ventilation.
- Upright positioning reduces the pressure of abdominal organs against the diaphragm to improve tidal volume.
- High-flow oxygen is avoided in COPD to prevent the loss of the stimulus to breathe.
- Immediate nursing care focuses on reducing the work of breathing and calming the patient’s anxiety.
Exams on Inflammation And Wound Healing
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
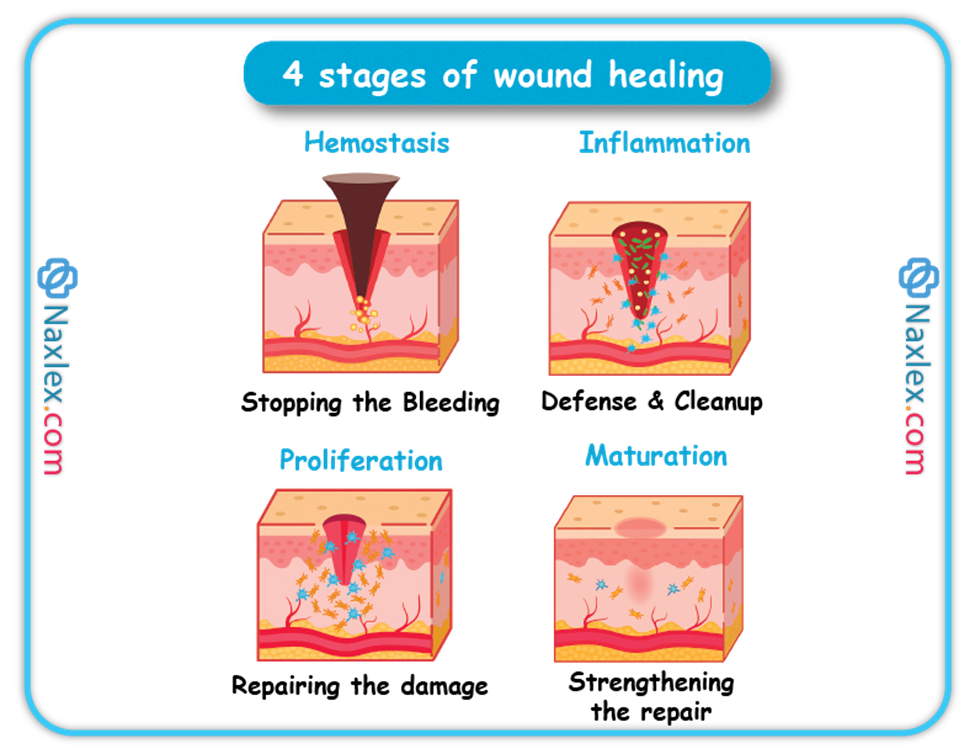
- Define and differentiate the major phases of the wound healing process: hemostasis, inflammation, proliferation, and remodeling.
- Describe the key cellular and molecular events that occur during the inflammatory phase, including the roles of mast cells, macrophages, neutrophils, and inflammatory mediators such as cytokines and chemokines.
- Explain the physiological purpose of the inflammatory response in the context of wound healing, distinguishing between acute and chronic inflammation and their respective outcomes.
- Identify the major cellular components involved in the proliferative phase of wound healing, including fibroblasts, endothelial cells, and keratinocytes, and explain their specific functions.
- Analyze the role of key growth factors in stimulating cell proliferation and tissue regeneration during wound healing.
- Characterize the process of tissue remodeling and scar formation, including the mechanisms of collagen deposition and cross-linking, and the eventual maturation of the scar tissue.
- Evaluate the factors that can impair or delay wound healing, such as infection, poor nutrition, age, and systemic diseases.
- Compare and contrast the processes of primary and secondary intention wound healing, providing examples of each and explaining the underlying differences in tissue loss and wound closure.
Introduction
- Inflammation is the body's immediate response to injury or infection, aiming to eliminate the initial cause of cell injury, clear out necrotic cells and tissues, and establish a repair process.
- Wound healing is a complex process that restores tissue integrity after injury, involving multiple overlapping phases.
The Inflammatory Response
Purpose and Function
- Neutralizes and dilutes the injurious agent.
- Removes necrotic materials.
- Establishes an environment suitable for healing and repair.
Vascular Response
- Vasodilation increases blood flow to the injured area.
- Increased capillary permeability allows plasma proteins and leukocytes to migrate into the tissue.
- Chemical mediators like histamine and prostaglandins contribute to these changes.
Cellular Response
- Neutrophils arrive first to phagocytize pathogens and debris.
- Monocytes follow, transforming into macrophages that continue phagocytosis and release growth factors.
- Lymphocytes may also be involved in immune responses.
Exudate Formation
- Serous exudate: clear, watery plasma.
- Purulent exudate: thick, yellow-green, indicating infection.
- Hemorrhagic exudate: contains blood, indicating severe tissue injury.
Systemic Manifestations
- Fever, leukocytosis, malaise, and increased heart rate are common systemic signs.
Wound Healing Processes
Types of Wound Healing
- Primary Intention
- Edges are approximated (e.g., surgical incision).
- Minimal tissue loss and scarring.
- Secondary Intention
- Wound edges not approximated.
- Greater tissue loss; healing occurs by granulation.
- Tertiary Intention
- Delayed primary closure due to infection or contamination.
Phases of Wound Healing
- Hemostasis
- Immediate vasoconstriction and clot formation.
- Inflammatory Phase
- Lasts 3–5 days.
- Characterized by redness, heat, swelling, pain, and loss of function.
- Proliferative Phase
- Lasts 5–21 days.
- Fibroblasts produce collagen; granulation tissue forms.
- Maturation (Remodeling) Phase
- Can last months.
- Collagen is remodeled; tensile strength increases.
Factors Affecting Wound Healing
Local Factors
- Infection delays healing.
- Necrotic tissue impedes granulation.
- Oxygenation is essential for collagen synthesis.
Systemic Factors
- Age: Older adults may have delayed healing.
- Nutrition: Protein, vitamin C, and zinc are vital.
- Chronic diseases: Diabetes impairs circulation and immune response.
- Medications: Steroids can suppress inflammation.
Complications of Wound Healing
- Dehiscence: Separation of wound edges.
- Evisceration: Protrusion of internal organs.
- Infection: Signs include redness, warmth, swelling, and purulent drainage.
- Hypertrophic scars and keloids: Excessive collagen formation.
Nursing Management
Assessment
- Monitor wound size, color, drainage, and signs of infection.
- Assess patient's nutritional status and comorbid conditions.
Interventions
- Maintain a moist wound environment.
- Ensure adequate nutrition and hydration.
- Educate the patient on wound care and signs of complications.
Documentation
- Record wound characteristics and any changes.
- Note interventions and patient responses.
Patient Education
- Importance of hand hygiene.
- Proper wound care techniques.
- Recognizing signs of infection or complications.
- Adherence to follow-up appointments.
Pressure Ulcers
Etiology and Pathophysiology
- Pressure ulcers are localized injuries to the skin and/or underlying tissue, typically over bony prominences.
- Caused by pressure, or pressure combined with shear and/or friction.
- Heal by secondary intention.
- Common locations: sacrum (most frequent), followed by heels.
- Contributing mechanical factors:
- Intensity of pressure
- Duration of pressure
- Tissue tolerance
- Other contributing factors:
- Shear: skin adherence with underlying sliding movement
- Friction: skin rubbing against another surface
- Moisture: especially from incontinence
Risk Factors For Pressure Ulcers
- Advanced age
- Anemia
- Contractures
- Diabetes mellitus
- Elevated body temperature
- Immobility
- Impaired circulation
- Incontinence
- Low diastolic blood pressure (<60 mm Hg)
- Mental deterioration
- Neurologic disorders
- Obesity
- Pain
- Prolonged surgery
- Vascular disease
Clinical Manifestations
- Vary by extent of tissue damage.
- Staging is based on deepest level of tissue involvement.
- Infected ulcers may present with:
- Leukocytosis, fever
- Increased size, odor, drainage
- Necrotic tissue, induration, warmth, pain
- Complications:
- Cellulitis
- Chronic infection
- Sepsis
- Death
- Recurrence is most common
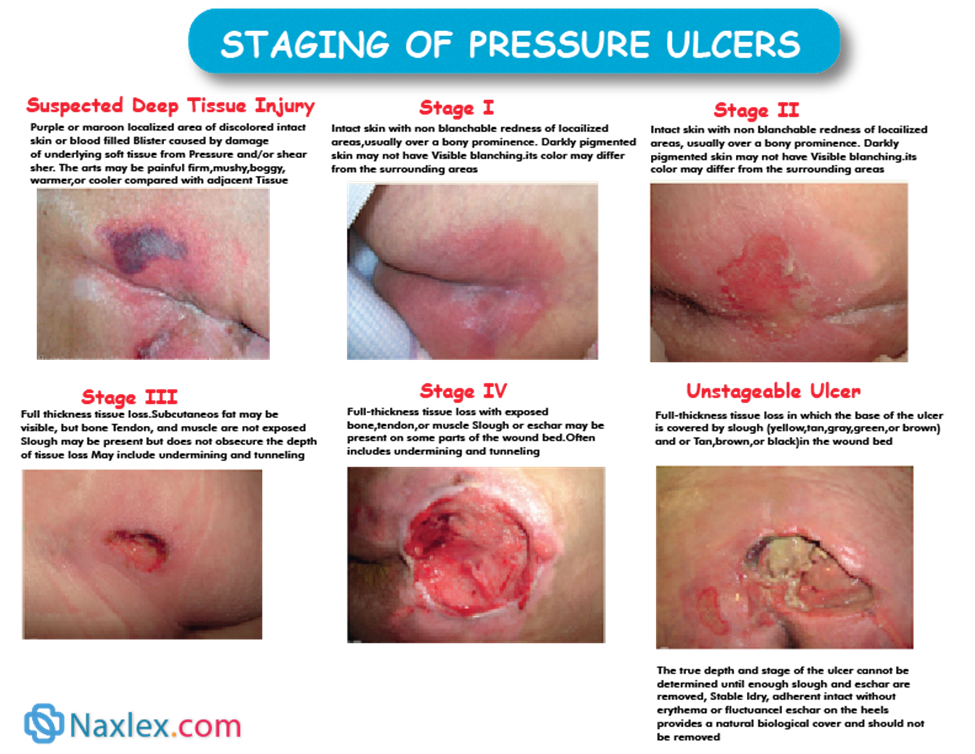
Staging Of Pressure Ulcers
Staging of Pressure Ulcers (NPUAP Guidelines)
|
Stage |
Description |
|
Suspected Deep Tissue Injury |
Purple/maroon discolored intact skin or blood-filled blister; may be painful or boggy |
|
Stage I |
Nonblanchable redness of intact skin |
|
Stage II |
Partial-thickness dermis loss; red-pink wound bed or serum-filled blister |
|
Stage III |
Full-thickness tissue loss; subcutaneous fat may be visible; no bone, tendon, or muscle exposed |
|
Stage IV |
Full-thickness loss with exposed bone, tendon, or muscle; slough/eschar may be present |
|
Unstageable |
Full-thickness tissue loss covered by slough/eschar; depth cannot be determined until removal |
Note: Stable eschar on heels should not be removed.
Staging of pressure ulcers
- Use aseptic technique to prevent infection.
- Restrict patient contact with the wound.
- Minimize environmental contamination.
- Antibiotics may be used prophylactically or based on culture results.
- Wound cultures should be done before antibiotics are given.
- Swab technique (performed by nurses)
- Wound exudates
- Z-technique: 10-point Z pattern on clean wound bed
- Levine’s technique: 1 cm² area with pressure to extract deep fluid
- Avoid culturing eschar or exudate
- Do not use cotton-tipped swabs
- Swab technique (performed by nurses)
- Inadequate nutrition disrupts protein, fat, and carbohydrate metabolism.
- Vitamin A aids epithelialization, increases collagen synthesis and wound strength.
- Use enteral nutrition if GI tract is functional.
- Use parenteral nutrition if enteral is contraindicated or not tolerated.
- Patients may fear disfigurement, odor, and drainage.
- Educate patients on normal wound healing.
- Maintain a respectful and reassuring demeanor during dressing changes.
- Avoid negative facial expressions to prevent patient anxiety.
- Wounds may take 4 to 6 weeks or longer to heal.
- Promote:
- Adequate nutrition and rest
- Minimal stress (emotional and physical)
- Monitor for:
- Contractures
- Adhesions
- Secondary infections
- Abnormal drainage or wound color
- Teach signs of infection and abnormal healing.
- Review medication instructions and potential side effects.
Nursing and Collaborative Management
- Prevention is the best treatment.
- Interprofessional collaboration includes:
- Nurse
- Wound care specialist
- Dietitian
- Physical therapist
- Occupational therapist
- Plastic surgeon
- Assess pressure ulcer risk on admission and at appropriate intervals:
- Acute care: every 24 hours
- Long-term care: weekly x4 weeks, then monthly/quarterly
- Home care: every visit
- Use validated tools (e.g., Braden Scale).
- Assess and document existing pressure ulcers.
- Special assessment considerations for darker skin tones.
Common Nursing Diagnoses
- Impaired skin integrity related to mechanical stress and immobility
- Impaired tissue integrity related to poor circulation and poor nutrition
- No worsening of existing ulcer
- Eliminate contributing factors
- Prevent infection
- Promote healing
- Prevent recurrence
- Frequent repositioning (typically every 2 hours)
- Use pressure-reducing devices (e.g., low-air-loss mattresses, heel boots, lift sheets)
- Pressure-relieving equipment does not replace repositioning
Summary
- Inflammation is the body's protective, vascular, and cellular response to injury, characterized by the four cardinal signs: redness (rubor), heat (calor), swelling (tumor), and pain (dolor).
- The wound healing process proceeds through four overlapping phases: hemostasis, inflammation, proliferation, and maturation.
- The inflammatory phase of wound healing begins immediately and involves vasoconstriction to control bleeding, followed by vasodilation, allowing immune cells like neutrophils and macrophages to clear debris and pathogens.
- The proliferative phase is marked by the formation of new tissue, including the growth of new blood vessels (angiogenesis), the production of collagen by fibroblasts, and the contraction of the wound.
- The final maturation phase involves the remodeling and strengthening of the collagen matrix, which can take up to two years to reach its maximum tensile strength.
- Pressure ulcers are a type of localized injury to the skin and underlying tissue caused by prolonged pressure that impedes blood flow, leading to tissue ischemia and death.
- Major risk factors for pressure ulcers include immobility, poor nutrition (especially low protein intake), incontinence (which causes skin moisture and maceration), and sensory deficits.
- Pressure ulcers are classified using a staging system from Stage 1 (non-blanchable redness) to Stage 4 (full-thickness tissue loss with exposed bone, tendon, or muscle), with categories for unstageable and deep tissue injury.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Inflammation And Wound Healing
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


