Please set your exam date
Family Planning
Study Questions
Practice Exercise 1
Which contraceptive method is most effective at preventing both pregnancy and sexually transmitted infections?
Explanation
Barrier contraceptionis a primary method to prevent both pregnancyand sexually transmitted infections(STIs). Male condoms provide a physical barrier that blocks sperm and pathogens, reducing transmission of Neisseria gonorrhoeae, Chlamydia trachomatis, HIV, and other organisms. Typical-use pregnancy prevention rate is 82% effective, with correct use up to 98%. Semen pH is normally 7.2–8.0, and vaginal pH is 3.8–4.5, which supports the barrier's role in reducing sperm motility.
Rationale for correct answers
2.Male condoms provide both contraception and STI prevention by preventing contact between genital mucosa and infectious secretions. Their latex or polyurethane structure blocks sperm entry into the vagina and physically prevents transmission of viruses and bacteria. They are effective against infections spread via semen, vaginal fluid, and genital contact.
Rationale for incorrect answers
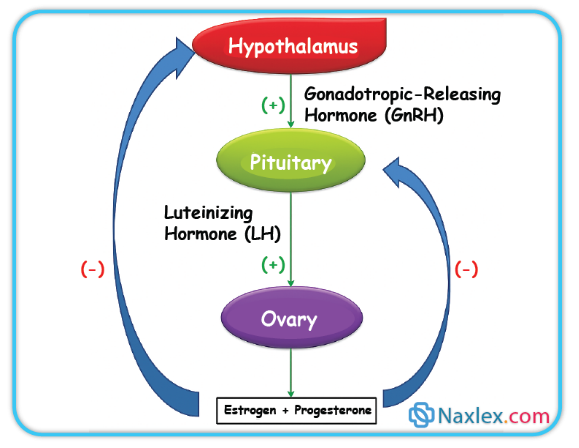
1.Combined oral contraceptives prevent pregnancy by inhibiting ovulation through suppression of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) but have no protective effect against STIs. They do not prevent pathogen transmission because they act systemically rather than as a physical barrier.
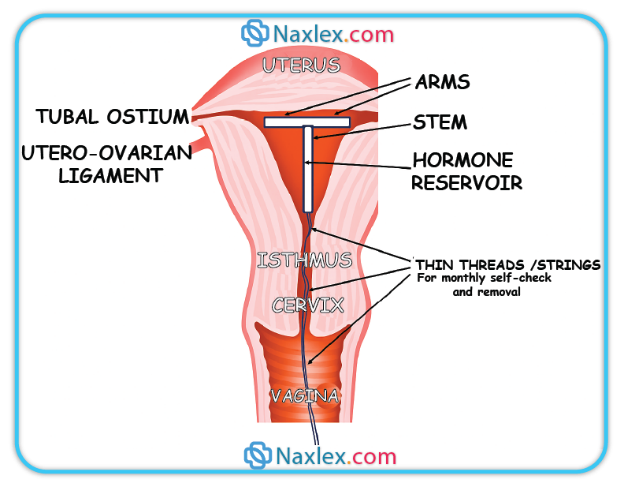
3.Intrauterine devices (IUDs) prevent pregnancy by causing a local inflammatory reaction toxic to sperm and ova or releasing hormones to thicken cervical mucus. They do not prevent STIs and can increase the risk of pelvic inflammatory disease if inserted in women with an active infection.
4.Contraceptive implants release progestin to inhibit ovulation and thicken cervical mucus. While highly effective for pregnancy prevention, they do not prevent exposure to pathogens during sexual activity and thus offer no protection from STIs.
Take home points
- Male condoms are the only contraceptive method that reliably prevents both pregnancy and STIs.
- Hormonal contraceptives prevent pregnancy but not STIs.
- IUDs are highly effective for pregnancy prevention but not infection prevention.
- STI prevention requires a barrier method or abstinence, regardless of hormonal contraceptive use.
A 28-year-old female client is considering various contraceptive options. She expresses a desire for a highly effective, long-acting method that does not require daily attention. She also prefers a method that does not contain estrogen due to a history of migraines with aura. Which of the following contraceptive methods would be the most appropriate recommendation for this client?
Explanation
Progestin-only contraceptionprovides effective pregnancy prevention without estrogen exposure, making it suitable for women with migraine with auradue to the increased risk of ischemic stroke with estrogen-containing methods. Depot medroxyprogesterone acetate suppresses ovulation, thickens cervical mucus, and thins the endometrium. Ovulation typically occurs when luteinizing hormone (LH) surges above 10–12 mIU/mL, which DMPA effectively prevents. Serum progesterone levels remain <3 ng/mL in anovulatory states. Injection efficacy exceeds 99% with correct use.
Rationale for correct answers
3.Depot medroxyprogesterone acetate is a progestin-only injectable given every 12 weeks, offering long-acting contraception without estrogen. It is appropriate for clients with migraine with aura due to the absence of thromboembolic risk from estrogen. It maintains high efficacy (>99%) without daily adherence and is safe in estrogen contraindications.
Rationale for incorrect answers
1.Combined oral contraceptives contain both estrogen and progestin, increasing the risk of ischemic stroke in women with migraine with aura. Estrogen elevates hepatic production of clotting factors II, VII, IX, X, and fibrinogen, promoting a hypercoagulable state. This makes them contraindicated in such patients despite high contraceptive efficacy.
2.Transdermal contraceptive patches deliver systemic estrogen and progestin, carrying the same thromboembolic and cerebrovascular risks as COCs. They are contraindicated in women with migraine with aura due to estrogen’s vascular effects, even though they avoid daily pill intake.
4.Vaginal contraceptive rings release estrogen and progestin locally but still achieve systemic estrogen absorption comparable to COCs. This retains the same contraindications in women with migraine with aura due to increased stroke risk, making them inappropriate despite convenience and high efficacy.
Take home points
- Migraine with aura is an absolute contraindication to estrogen-containing contraceptives due to increased ischemic stroke risk.
- Progestin-only methods are safer in women with vascular risk factors.
- Depot medroxyprogesterone acetate provides long-acting, highly effective contraception without daily use.
- Estrogen-containing methods include pills, patches, and vaginal rings and should be avoided in high-risk patients.
Which of the following are true about the copper IUD? Select all that apply.
Explanation
Copper intrauterine deviceis a non-hormonallong-acting reversible contraceptive that releases copper ions, creating a spermicidaluterine environment by increasing inflammatory reaction in the endometrium and altering cervical mucus. It is effective for up to 10–12 years, with pregnancy rates <1% per year. Normal menstrual blood loss is 30–40 mL per cycle, and copper IUDs can increase this volume, potentially causing anemia if hemoglobin falls below the normal range of 12–16 g/dL in females.
Rationale for correct answers
1.The copper IUD contains no hormones; contraception is achieved through copper ion release, which is toxic to sperm and ova, preventing fertilization without systemic hormonal effects.
2.Copper IUDs provide long-term contraception for up to 10–12 years, depending on the brand, due to sustained copper ion release maintaining spermicidal activity over time.
4.Copper IUDs have a contraceptive efficacy exceeding 99% due to their continuous local effect on sperm motility and viability, making them among the most effective reversible contraceptive methods.
Rationale for incorrect answers
3.Copper IUDs typically increase, not decrease, menstrual bleeding and cramping, especially in the first months after insertion, due to endometrial inflammation; this contrasts with levonorgestrel IUDs, which can reduce bleeding.
5.Copper IUDs do not require daily monitoring; they only require monthly self-checks for string position and routine medical follow-up, unlike methods such as oral contraceptives that demand daily adherence.
Take home points
- Copper IUDs are hormone-free, highly effective, and long-acting reversible contraceptives.
- They may increase menstrual bleeding and dysmenorrhea.
- Efficacy remains >99% for up to 10–12 years.
- They require minimal maintenance, with only monthly string checks.
A nurse is counseling a postpartum client who is exclusively breastfeeding her 4-week-old infant. The client asks about contraceptive options that will not interfere with her milk supply. Which method would be the most appropriate initial recommendation?
Explanation
Progestin-only contraceptionis preferred during exclusive breastfeedingin the first 6 weeks postpartum to avoid the negative impact of estrogen on milk production. Estrogen suppresses prolactin secretion from the anterior pituitary, which is essential for lactogenesis II. Normal prolactin levels in lactating women range from 100–300 ng/mL during the first 3 months postpartum, supporting milk synthesis and secretion. Progestin-only methods such as the hormonal IUD release levonorgestrel locally, inhibiting fertilization without systemic estrogen exposure, thus preserving lactation while maintaining high contraceptive efficacy (>99%).
Rationale for correct answers
3.A hormonal IUD releases low-dose levonorgestrel directly into the uterine cavity, suppressing sperm motility and thickening cervical mucus without affecting prolactin levels. It is >99% effective, long-acting (3–8 years depending on device), and safe for breastfeeding mothers after 4 weeks postpartum.
Rationale for incorrect answers
1.Combined oral contraceptives contain estrogen, which reduces prolactin secretion and may decrease milk volume, especially within the first 6 weeks postpartum. Estrogen also increases the risk of thromboembolism during this period due to pregnancy-induced hypercoagulability, evidenced by elevated fibrinogen (normal 200–400 mg/dL) and clotting factors.
2.The transdermal contraceptive patch delivers systemic estrogen and progestin, posing the same risks to milk supply and thrombosis as COCs. Its estrogen exposure is continuous, potentially reducing daily milk output by disrupting prolactin-mediated milk synthesis.
4.The vaginal contraceptive ring releases estrogen and progestin, achieving systemic estrogen levels sufficient to impact prolactin. This estrogen exposure during exclusive breastfeeding may compromise milk production and should be avoided in the first 6 weeks postpartum.
Take home points
- Progestin-only methods are preferred for breastfeeding women in the early postpartum period.
- Estrogen-containing contraceptives can suppress prolactin and reduce milk supply.
- Hormonal IUDs provide long-acting, highly effective contraception without estrogen exposure.
- Postpartum hypercoagulability increases estrogen-related thromboembolic risk.
Which of the following are contraindications for combined oral contraceptives? Select all that apply.
Explanation
1.Breast cancer is a contraindication because COCs contain estrogen and progestin, which can stimulate hormone-sensitive tumors. A history of breast cancer increases recurrence risk with hormonal exposure.
2.Smoking in women over 35 years significantly increases the risk of thromboembolism and myocardial infarction when combined with estrogen-containing contraceptives. This is a well-established absolute contraindication.
4.Hypertension ≥140/90 mmHg is a contraindication due to increased risk of stroke and cardiovascular events with estrogen use. Estrogen promotes sodium retention and increases blood pressure.
Rationale for incorrect answers
3.Nulliparity is not a contraindication. It may be associated with a slightly increased risk of certain cancers, but COCs are safe and often used in nulliparous women for cycle regulation and contraception.
5.Regular menstrual cycles do not contraindicate COC use. In fact, COCs are often prescribed to regulate cycles further or reduce dysmenorrhea. Regularity does not affect safety or efficacy.
Take home points
- COCs are contraindicated in women with hypertension ≥140/90 mmHg due to stroke risk.
- Smoking in women >35 years increases thrombotic risk when using estrogen-containing contraceptives.
- History of breast cancer contraindicates COC use due to hormone sensitivity.
- Nulliparity and regular cycles are not contraindications for COCs.
Practice Excercise 2
A nurse is teaching a patient about the cervical mucus method. What indicates fertile days?
Explanation
Cervical mucus methodis a natural fertility awareness technique based on observing mucus characteristicsduring the menstrual cycle. Estrogen levels rise before ovulation, causing clear, stretchy, and copiousmucus that facilitates sperm transport. Progesterone post-ovulation leads to thick, scant, and stickymucus. Normal ovulation occurs around day 14 of a 28-day cycle, with estrogen peaking at 200–600 pg/mL and progesterone rising to 5–20 ng/mL post-ovulation.
Rationale for correct answers
2.Clear, stretchy mucus indicates high estrogen levels and imminent ovulation. It resembles raw egg white and allows sperm to swim easily through the cervix, marking the fertile window.
Rationale for incorrect answers
1.Thick, sticky mucus is progesterone-dominant and occurs after ovulation. It forms a barrier to sperm and indicates non-fertile days.
3.Dry, minimal mucus is typical in the early follicular phase or post-ovulation. It reflects low estrogen and is not conducive to sperm survival or transport.
4.Cloudy, opaque mucus appears during transitional phases but does not indicate peak fertility. It lacks the elasticity and clarity of fertile mucus and impedes sperm motility.
Take home points
- Fertile mucus is clear, stretchy, and estrogen-dominant.
- Progesterone causes thick, sticky, non-fertile mucus post-ovulation.
- Dry or cloudy mucus indicates low fertility phases.
- Cervical mucus method requires daily observation and cycle tracking.
A client presents to the clinic requesting emergency contraception after unprotected intercourse 48 hours ago. She has no contraindications to any method. Which of the following emergency contraceptive options is generally considered the most effective?
Explanation
Emergency contraceptionprevents pregnancy after unprotected intercourse by delaying ovulation, impairing fertilization, or preventing implantation. The most effective method is copper IUD, which creates a spermicidalintrauterine environment. Copper ions induce an inflammatory response toxic to sperm and ova. It remains effective up to 120 hours post-intercourse. Ulipristal acetate delays ovulation even after LH surge; levonorgestrel is less effective if LH surge has begun. Combined estrogen-progestin (Yuzpe) is least effective and has more side effects.
Rationale for correct answers
4.Copper IUD is the most effective emergency contraceptive, with failure rates <0.1%. It prevents fertilization and implantation and is effective up to 120 hours post-intercourse regardless of cycle timing.
Rationale for incorrect answers
1.Yuzpe method has a failure rate of 2–3% and causes nausea and vomiting due to high estrogen. It is less effective than other options and not preferred when better alternatives exist.
2.Levonorgestrel is effective only if taken before LH surge. Its efficacy drops significantly after ovulation begins. It is less reliable than ulipristal or copper IUD.
3.Ulipristal acetate is more effective than levonorgestrel, especially closer to ovulation, but still less effective than copper IUD. It delays ovulation even after LH surge but does not prevent implantation.
Take home points
- Copper IUD is the most effective emergency contraceptive, effective up to 120 hours.
- Ulipristal acetate is superior to levonorgestrel near ovulation.
- Levonorgestrel is less effective if LH surge has started.
- Yuzpe method is least effective and causes more side effects.
Which of the following are advantages of barrier methods? Select all that apply.
Explanation
Barrier methodsprevent pregnancy by physically blocking spermfrom reaching the egg, thereby avoiding fertilization. They include male condoms, female condoms, diaphragms, and cervical caps. These methods offer STI protection, especially latex condoms, and are often female-controlledand accessible without a prescription. Typical-use failure rates vary: male condoms ≈13%, diaphragms ≈17%. Barrier methods do not alter hormonal levelsand are used per intercourse episode, not long-term.
Rationale for correct answers
1.Barrier methods, especially latex condoms, reduce transmission of STIs including Chlamydia trachomatis, Neisseria gonorrhoeae, and HIV. They form a physical barrier preventing exchange of genital secretions.
3.Female-controlled options like female condoms, diaphragms, and cervical caps allow women to initiate and manage contraception independently, enhancing autonomy and accessibility.
5.Most barrier methods, including male and female condoms, are available over-the-counter and do not require a prescription, making them easily accessible and usable without clinical intervention.
Rationale for incorrect answers
2.High efficacy with typical use is not a feature of barrier methods. Male condoms have a typical-use failure rate of ≈13%, and diaphragms ≈17%. These rates are higher than hormonal methods or IUDs, which have failure rates <1%.
4.Barrier methods are not long-term contraception. They must be used with each act of intercourse and do not provide continuous protection. Long-term methods include IUDs, implants, and sterilization.
Take home points
- Barrier methods protect against STIs, especially latex condoms.
- Female-controlled barrier options enhance reproductive autonomy.
- Most barrier methods are available without prescription.
- Barrier methods are not long-term and have higher failure rates with typical use.
A nurse is reinforcing education on male condom use for a sexually active adolescent. Which of the following instructions is crucial for effective condom use and STI prevention?
Explanation
Male condom useis a barrier method that prevents pregnancyand reduces STI transmissionby physically blocking spermand infectious secretions. For maximum effectiveness, condoms must be applied before genital contactto prevent exposure to pre-ejaculate and mucosal pathogens. Latex condoms are sensitive to heat, friction, and oil-based lubricants, which degrade material integrity. Typical-use failure rate is ≈13%, but perfect use reduces it to ≈2%. Condoms should be stored in cool, dry places and never reused.
Rationale for correct answers
3.Applying the condom before any genital contact is essential to prevent transmission of STIs and pregnancy from pre-ejaculate fluid, which may contain sperm and pathogens like HIV or Chlamydia trachomatis.
Rationale for incorrect answers
1.Storing condoms in a wallet exposes them to heat and friction, which degrade latex and increase the risk of breakage. Ideal storage is in a cool, dry place away from direct sunlight.
2.Oil-based lubricants (e.g., petroleum jelly) weaken latex and increase the risk of tearing. Only water-based or silicone-based lubricants are safe with latex condoms.
4.Re-using condoms is unsafe and ineffective. Microscopic tears and loss of elasticity compromise barrier function, increasing risk of pregnancy and STI transmission.
Take home points
- Condoms must be applied before any genital contact to prevent STI and pregnancy.
- Oil-based lubricants degrade latex and should be avoided.
- Condoms should be stored in cool, dry places, not wallets.
- Condoms are single-use only; re-use increases failure risk.
Which of the following are true about emergency contraception? Select all that apply.
Explanation
Emergency contraceptionprevents pregnancy after unprotected intercourse by interfering with ovulation, fertilization, or implantation, but does not affect an established pregnancy. Methods include levonorgestrel, ulipristal acetate, and copper IUD. Effectiveness is time-sensitive, with optimal use within 72–120 hours. Endometrial changes impair implantation. Serum hCG in early pregnancy is normally <5 mIU/mL; emergency contraception does not alter hCG if implantation has occurred.
Rationale for correct answers
1.Emergency contraception acts before implantation and does not terminate an established pregnancy. It is ineffective once the embryo has implanted and hCG levels begin to rise above 5 mIU/mL.
2.Copper IUD is a highly effective emergency contraceptive option. It creates a spermicidal intrauterine environment and prevents fertilization and implantation when inserted within 120 hours post-intercourse.
4.Emergency contraception is time-sensitive. Levonorgestrel is most effective within 72 hours, ulipristal acetate within 120 hours, and copper IUD up to 120 hours. Delay reduces efficacy due to progression of ovulation and fertilization.
5.Hormonal emergency contraceptives alter the endometrial lining, making it unreceptive to implantation. This shedding effect contributes to their mechanism of action, especially if ovulation has already occurred.
Rationale for incorrect answers
3.Emergency contraception does not require daily administration. Levonorgestrel and ulipristal acetate are single-dose regimens. Copper IUD is a one-time insertion. Daily dosing is not part of emergency contraceptive protocols.
Take home points
- Emergency contraception prevents pregnancy before implantation, not after.
- Copper IUD is the most effective emergency contraceptive option.
- Timely administration is critical for hormonal methods.
- Endometrial changes contribute to prevention of implantation.
Practice Excercise 3
When counseling a client about the contraceptive implant (e.g., Nexplanon), the nurse should inform them that it is effective for approximately how long?
Explanation
The contraceptive implantis a long-acting reversible contraceptive that releases etonogestrel, a synthetic progestin, into systemic circulation. It works primarily by inhibiting ovulation, thickening cervical mucus, and thinning the endometrial lining. Nexplanon is a single-rod subdermal implant effective for 3 years, though some studies show efficacy up to 5 years. Serum etonogestrel levels remain above the ovulation suppression threshold of 90 pg/mLfor at least 3 years, with gradual decline thereafter. Common side effects include irregular bleeding, weight gain, and acne. Contraindications include active liver disease, breast cancer, and unexplained vaginal bleeding.
Rationale for correct answers
3.Nexplanon is FDA-approved for 3 years of use. Clinical trials demonstrate sustained ovulation suppression and contraceptive efficacy for up to 3 years, with some off-label data supporting up to 5 years. The question asks for approximate duration, making 3–5 years the most scientifically accurate range.
Rationale for incorrect answers
1.The 1-year duration is incorrect. Etonogestrel levels remain well above the ovulation suppression threshold for at least 3 years. There is no scientific basis for replacing the implant annually.
2.While 2 years falls within the effective window, it underestimates the approved and evidence-based duration. Nexplanon maintains contraceptive efficacy beyond 2 years, making this choice incomplete and misleading.
4.7–10 years is incorrect. No contraceptive implant maintains therapeutic etonogestrel levels for this duration. Long-term options like intrauterine devices may last this long, but not subdermal implants.
Take home points
- Nexplanon is a progestin-only subdermal implant effective for approximately 3–5 years.
- It suppresses ovulation by maintaining serum etonogestrel levels above 90 pg/mL.
- Common side effects include irregular bleeding and acne; contraindications include breast cancer.
- It should not be confused with intrauterine devices which have longer durations.
Which permanent contraceptive method requires semen analysis to confirm efficacy?
Explanation
Vasectomyis a permanent male contraceptive method involving ligation or occlusion of the vas deferens, preventing sperm transportfrom the testes to the urethra. It does not immediately render a man sterile; residual sperm may persist in the ejaculatory ducts for weeks. Semen analysisis required post-procedure to confirm azoospermia, typically performed at 8–16 weeksor after 20 ejaculations. Normal semen should contain sperm concentration >15 million/mL, motility >40%, and volume >1.5 mL. Vasectomy has no effect on testosterone levels, libido, or erectile function.
Rationale for correct answers
2.Vasectomy interrupts sperm transport but does not eliminate existing sperm immediately. Semen analysis is essential to confirm azoospermia and ensure contraceptive efficacy. Without this confirmation, pregnancy risk remains.
Rationale for incorrect answers
1.Tubal ligation is a female sterilization method involving occlusion of fallopian tubes. It prevents egg-sperm meeting and does not require semen analysis, as male fertility is unaffected.
3.Copper IUD insertion provides long-term contraception by inducing a local inflammatory response toxic to sperm. It is not a sterilization method and does not require semen analysis.
4.Hormonal IUDs release levonorgestrel to thicken cervical mucus and suppress endometrial growth. They are reversible and do not affect sperm production or transport, so semen analysis is not relevant.
Take home points
- Vasectomy requires post-procedure semen analysis to confirm azoospermia.
- Tubal ligation does not affect male fertility and needs no semen testing.
- IUDs are reversible and do not require semen analysis.
- Semen analysis confirms absence of sperm: azoospermia = no pregnancy risk.
Which of the following are considered permanent contraceptive methods? Select all that apply.
Explanation
Permanent contraceptionrefers to methods intended to provide lifelong sterilitywithout the need for ongoing maintenance or repeat procedures. These include tubal ligationin females and vasectomyin males. Tubal ligation involves surgical occlusion of the fallopian tubes, preventing fertilization. Vasectomy involves cutting or sealing the vas deferens, blocking sperm transport. Both are considered irreversible, though reversal is technically possible but not guaranteed. These methods do not alter hormone levels or sexual function. They are chosen by individuals who have completed childbearing or seek definitive contraception.
Rationale for correct answers
2.Tubal ligation is a surgical sterilization method that permanently blocks the fallopian tubes, preventing fertilization. It is classified as a permanent contraceptive method.
3.Vasectomy is a male sterilization procedure that permanently interrupts sperm transport. It is considered a permanent method and requires semen analysis to confirm efficacy.
Rationale for incorrect answers
1.The contraceptive implant (e.g., Nexplanon) is a long-acting reversible method effective for 3–5 years. It does not cause permanent sterility and can be removed to restore fertility.
4.Depot medroxyprogesterone acetate (DMPA) is an injectable progestin given every 3 months. It suppresses ovulation temporarily and is fully reversible upon discontinuation.
5.Hormonal IUDs release levonorgestrel locally and are effective for 3–8 years depending on the type. They are reversible and fertility returns quickly after removal.
Take home points
- Tubal ligation and vasectomy are permanent sterilization methods.
- Contraceptive implants, DMPA, and hormonal IUDs are reversible.
- Permanent methods do not affect hormone levels or sexual function.
- Reversal of sterilization is possible but not guaranteed.
What is the primary benefit of family planning?
Explanation
Family planninginvolves the deliberate control of fertility, enabling individuals and couples to determine the number and spacing of children. It utilizes contraceptive methodsto prevent unintended pregnancies, thereby improving maternal and child health outcomes. Scientifically, it reduces maternal mortality by preventing high-risk pregnancies, lowers infant mortality through optimal birth spacing, and enhances socioeconomic stability. The World Health Organization estimates that family planning could prevent up to 30%of maternal deaths. It also reduces the burden on healthcare systems and supports sustainable population growth.
Rationale for correct answers
2.Family planning directly reduces unintended pregnancies by enabling access to effective contraception. This leads to improved maternal health, reduced abortion rates, and better outcomes for children.
Rationale for incorrect answers
1.Family planning reduces maternal mortality, not increases it. By preventing high-risk and closely spaced pregnancies, it lowers complications and deaths.
3.Family planning lowers healthcare costs by reducing the need for emergency obstetric care, unsafe abortion management, and neonatal intensive care due to preterm births.
4.While decreased family size may result, it is not the primary benefit. The main goal is to prevent unintended pregnancies and improve health outcomes.
Take home points
- Family planning reduces unintended pregnancies and maternal mortality.
- It improves child health through optimal birth spacing.
- It lowers healthcare costs by preventing high-risk pregnancies.
- Decreased family size is a secondary outcome, not the primary benefit.
What are key components of effective, client-centered family planning counseling? Select all that apply.
Explanation
Client-centered family planning counselingprioritizes the individual's autonomy, informed choice, and reproductive goals. It involves active listening, respectful communication, and provision of accurate, unbiased informationabout all contraceptive options. The counselor must assess medical eligibility, personal preferences, and lifestyle factors without imposing personal beliefs. Effective counseling empowers clients to make decisions that align with their values and health needs. It also includes discussing side effects, contraindications, and method efficacy. The goal is to support voluntary, informed, and respectful contraceptive choice.
Rationale for correct answers
2.Actively listening ensures the counselor understands the client’s values, concerns, and reproductive goals. It builds trust and supports personalized care.
3.Providing accurate and unbiased information allows the client to compare methods based on efficacy, side effects, and suitability, facilitating informed decision-making.
4.Empowering the client respects autonomy and supports voluntary contraceptive choice, which is central to ethical and effective family planning counseling.
Rationale for incorrect answers
1.Presenting only the most effective methods disregards client preferences and medical eligibility. Counseling must include all options to support informed choice.
5.Recommending based on personal experience introduces bias and undermines client autonomy. Counseling should be evidence-based and client-focused, not anecdotal.
Take home points
- Client-centered counseling respects autonomy and supports informed choice.
- Active listening and unbiased information are essential.
- Empowerment is central to ethical family planning.
- Personal bias must be avoided in contraceptive counseling.
Comprehensive Questions
A patient asks about the mechanism of emergency contraception. What should the nurse explain?
Explanation
Emergency contraception works by interfering with ovulation, fertilization, or implantationdepending on the type and timing of administration. The most common forms include levonorgestrel and ulipristal acetate. Levonorgestrel inhibits LH surge, preventing ovulation, while ulipristal delays follicular rupture. Normal serum LH levels range from 5–25 IU/L during the mid-cycle surge. These agents do not affect an already implanted embryo and are ineffective once pregnancy is established. Side effects include nausea, headache, and menstrual irregularities. Contraindications include known pregnancy and hypersensitivity to components.
Rationale for correct answers
2.Emergency contraception prevents ovulation or fertilization. Levonorgestrel inhibits the luteinizing hormone surge, blocking ovulation if taken before the peak. Ulipristal acetate delays follicular rupture. These mechanisms act before fertilization, making this the correct explanation.
Rationale for incorrect answers
1.Emergency contraception does not terminate an established pregnancy. It is ineffective once implantation has occurred. Agents like mifepristone are used for termination, not levonorgestrel or ulipristal. Emergency contraception is not abortifacient.
3.Endometrial shedding is not the primary mechanism. While some thinning of the endometrium may occur, it is not reliable or consistent enough to prevent implantation. The dominant action is inhibition of ovulation.
4.Emergency contraception does not immobilize sperm permanently. Sperm motility is unaffected by these agents. Barrier methods or spermicides are used to impair sperm movement, not hormonal emergency contraception.
Take home points
- Emergency contraception prevents ovulation or fertilization, not implantation.
- It is ineffective once pregnancy is established.
- It does not cause permanent sperm immobilization.
- It must be differentiated from abortifacients like mifepristone.
A nurse is educating a client about the mechanism of action of Combined Oral Contraceptives (COCs). Which of the following is the primary way COCs prevent pregnancy?
Explanation
Combined oral contraceptives (COCs)prevent pregnancy primarily by suppressing ovulation, thickening cervical mucus, and altering endometrial receptivity. They contain synthetic estrogenand progestin, which inhibit the hypothalamic-pituitary-ovarian axis. Estrogen suppresses follicle-stimulating hormone (FSH), while progestin inhibits luteinizing hormone (LH) surge, preventing ovulation. Normal FSH levels range from 3–20 IU/L and LH from 5–25 IU/L mid-cycle. Progestin also thickens cervical mucus, making it hostile to sperm penetration, and alters the endometrium to reduce implantation likelihood. Side effects include nausea, breast tenderness, and thromboembolic risk. Contraindications include active thromboembolism, estrogen-sensitive cancers, and severe liver disease.
Rationale for correct answers
3.COCs primarily prevent pregnancy by thickening cervical mucus and consistently suppressing ovulation. Estrogen and progestin inhibit FSH and LH, preventing follicular development and ovulation. Progestin also thickens cervical mucus, impeding sperm entry.
Rationale for incorrect answers
1.A sterile inflammatory reaction in the uterus is the mechanism of intrauterine devices (IUDs), particularly copper IUDs. COCs do not induce uterine inflammation and act hormonally, not mechanically.
2.Physical blockage of sperm is the mechanism of barrier methods like condoms or diaphragms. COCs do not create a physical barrier but alter cervical mucus and hormonal cycles.
4.Copper ions impair sperm motility and viability, a mechanism specific to copper IUDs. COCs do not contain copper and do not alter sperm function directly through ionic interference.
Take home points
- COCs suppress ovulation and thicken cervical mucus
- They do not act via inflammation or physical barriers
- Copper IUDs impair sperm via ionic mechanisms
- Barrier methods physically block sperm entry
Which group requires tailored contraceptive counseling due to higher risks of unintended pregnancy?
Explanation
Adolescentsrequire tailored contraceptive counseling due to high rates of unintended pregnancy, variable adherence, limited knowledge, and developmental factors. They often face barriers such as lack of access, confidentiality concerns, and misinformation. The adolescent pregnancy rate remains significantly higher than other age groups, with unintended pregnancy rates exceeding 80% in some populations. Normal menstrual cycles may be irregular in early adolescence, complicating fertility awareness methods. Cognitive and emotional maturity also influences decision-making and consistency in contraceptive use. Long-acting reversible contraceptives (LARCs) are recommended due to their high efficacy and low maintenance.
Rationale for correct answers
2.Adolescents have the highest rates of unintended pregnancy due to inconsistent contraceptive use, limited access, and developmental factors. Tailored counseling improves method selection, adherence, and understanding, reducing risk.
Rationale for incorrect answers
1.Postmenopausal women are not at risk of pregnancy due to cessation of ovulation. Their counseling focuses on hormone replacement therapy and other health concerns, not contraception.
3.Women over 50 years typically have declining fertility due to reduced ovarian reserve and anovulatory cycles. While contraception may be needed until menopause is confirmed, their risk of unintended pregnancy is much lower than adolescents.
4.Nulliparous women may have specific considerations for method selection (e.g., IUD insertion technique), but they do not inherently have higher unintended pregnancy risk. Counseling may be individualized but not necessarily tailored due to elevated risk.
Take home points
- Adolescents have the highest unintended pregnancy risk
- Tailored counseling improves contraceptive adherence and understanding
- Postmenopausal and older women have low fertility risk
- Nulliparity affects method choice, not pregnancy risk
A client using a progestin-only injectable contraceptive (DMPA) asks the nurse about potential side effects. Which of the following is a common and important side effect associated with long-term DMPA use?
Explanation
Depot medroxyprogesterone acetate (DMPA)is a progestin-only injectable contraceptiveadministered every 12 weeks. It works by inhibiting ovulation, thickening cervical mucus, and altering the endometrium. A common and important side effect is delayed return to fertility, with ovulation resuming on average 9–10 months after the last injection. DMPA also causes menstrual irregularities, including amenorrhea. It may reduce bone mineral density with long-term use; normal bone mineral density (BMD) values are ≥1.0 g/cm². DMPA does not increase thromboembolic risk and is safe for women with estrogen contraindications. Other side effects include weight gain and mood changes.
Rationale for correct answers
2.DMPA is associated with a delayed return to fertility, often taking 9–10 months after the last injection for ovulation to resume. This is a well-documented and important counseling point for users considering future pregnancy.
Rationale for incorrect answers
1.DMPA does not cause a significant increase in libido. In fact, some users report decreased libido or mood changes. Libido effects vary and are not a consistent or prominent side effect.
3.While DMPA does not increase the risk of venous thromboembolism, this is not a side effect but rather a safety advantage. It is suitable for women with contraindications to estrogen, but the question asks for a side effect.
4.DMPA often causes unpredictable menstrual cycles, especially in the first year. Many users experience irregular bleeding or amenorrhea. Predictable cycles are not a feature of DMPA use.
Take home points
- DMPA delays return to fertility after discontinuation
- Menstrual irregularities are common with DMPA
- DMPA is safe for women with estrogen contraindications
- Bone density loss is a concern with long-term use
What is the typical-use efficacy of male condoms?
Explanation
Male condoms are a barrier method of contraception that prevent sperm from entering the vaginal canal. Their typical-use failure ratereflects real-world usage, including incorrect or inconsistent use. Typical-use efficacyis lower than perfect-use efficacy. Breakage, slippage, and incorrect applicationare common causes of failure. Latex condoms also reduce transmission of Neisseria gonorrhoeae, Chlamydia trachomatis, and HIV. The typical-use efficacyof male condoms is approximately 82%, meaning 18 out of 100 women will become pregnant in the first year of use. Perfect-use efficacy is about 98%.
Rationale for correct answers
2.Typical-use efficacy of male condoms is 82%. This accounts for human error such as delayed application, early removal, or improper storage. The question asks for typical-use, not perfect-use, making 82% the correct figure.
Rationale for incorrect answers
1.98% reflects perfect-use efficacy, not typical-use. This figure assumes correct and consistent use every time, which is not representative of real-world behavior. It overestimates protection in typical scenarios.
3.91% is the typical-use efficacy of female condoms, not male condoms. This figure is often confused with male condom data but is specific to the internal barrier method.
4.99% is an exaggerated figure not supported by clinical data for either typical or perfect use. No barrier method achieves 99% efficacy under typical-use conditions.
Take home points
- Male condoms have a typical-use efficacy of 82%, meaning 18% failure rate annually.
- Perfect-use efficacy of male condoms is 98%, assuming no user error.
- Female condoms have a typical-use efficacy of 91%.
- Barrier methods also reduce STI transmission, unlike hormonal methods.
What is the primary reason why combined hormonal contraceptives are often contraindicated for women who smoke and are over the age of 35?
Explanation
Combined hormonal contraceptives (CHCs) contain estrogenand progestin, and are widely used for pregnancy prevention, cycle regulation, and acne management. In women over 35 who smoke, CHCs are contraindicated due to a synergistic increase in cardiovascular risk. Estrogenpromotes hepatic synthesis of clotting factors, increasing the risk of venous thromboembolism (VTE). Smoking accelerates atherogenesis, raising the risk of myocardial infarctionand stroke. The baseline VTE risk in reproductive-age women is approximately 1–5 per 10,000 annually; CHCs increase this to 9–10 per 10,000, and smoking compounds it further. Blood pressure should be <140/90 mmHg before initiating CHCs.
Rationale for correct answers
3.Women over 35 who smoke have a significantly elevated risk of thrombotic events when using CHCs. Estrogen increases clotting factor production, and smoking promotes endothelial damage and platelet aggregation. Together, they markedly increase the risk of VTE, myocardial infarction, and stroke.
Rationale for incorrect answers
1.Smoking does not reduce the effectiveness of CHCs. The contraceptive efficacy remains high (>99% with perfect use), and metabolism of hormones is not significantly altered to reduce effectiveness.
2.Bone mineral density loss is associated with long-term use of depot medroxyprogesterone acetate (DMPA), not CHCs. Estrogen in CHCs actually helps maintain bone density.
4.Irregular bleeding and spotting are more common with progestin-only methods or during initial CHC use, but not a primary contraindication in smokers over 35. The cardiovascular risk is the dominant concern.
Take home points
- CHCs are contraindicated in women >35 who smoke due to elevated cardiovascular risk.
- Estrogen increases clotting factors; smoking promotes vascular injury.
- CHCs do not reduce bone density; DMPA does.
- CHCs remain highly effective regardless of smoking status.
Which contraceptive method requires daily temperature monitoring?
Explanation
The symptothermal method is a fertility awareness-basedapproach that combines basal body temperature (BBT)tracking with cervical mucus observationand calendar calculations. Ovulationcauses a measurable rise in BBT due to progesteroneeffects on the hypothalamus. BBT typically increases by 0.3–0.6°C after ovulation and remains elevated until menstruation. Normal BBT ranges from 36.1°C to 36.4°C pre-ovulation and rises to 36.4°C to 37.0°C post-ovulation. Accurate daily temperature monitoring, taken at the same time each morning before activity, is essential for identifying the fertile window.
Rationale for correct answers
1.The symptothermal method requires daily BBT monitoring to detect the post-ovulatory temperature rise. This helps identify the fertile and infertile phases of the menstrual cycle. It is combined with cervical mucus tracking for improved accuracy.
Rationale for incorrect answers
2.The cervical cap is a barrier method that does not involve cycle tracking or temperature monitoring. It is inserted before intercourse and blocks sperm entry into the cervix.
3.Progestin-only pills require strict daily intake but do not involve temperature monitoring. Their efficacy depends on consistent timing, not physiological tracking.
4.The contraceptive patch delivers hormones transdermally and is replaced weekly. It does not require any temperature monitoring or cycle observation.
Take home points
- The symptothermal method uses BBT and cervical mucus to track fertility.
- BBT rises 0.3–0.6°C post-ovulation due to progesterone.
- Barrier and hormonal methods do not require temperature monitoring.
- Accurate daily measurement is essential for symptothermal effectiveness.
Which of the following is a primary advantage of female condoms over male condoms?
Explanation
Female condomsare barrier contraceptives designed for internal vaginal use. They provide dual protectionagainst pregnancy and sexually transmitted infections (STIs). Their polyurethaneor nitrilecomposition makes them non-latex and suitable for latex-allergic individuals. They can be inserted up to 8 hoursbefore intercourse, offering flexibility. Unlike male condoms, female condoms cover the external genitalia, reducing exposure to pathogens. They do not require an erection for placement and are not dependent on male cooperation. Normal vaginal pH is 3.8–4.5; female condoms do not alter this environment.
Rationale for correct answers
3.Female condoms can be inserted up to 8 hours before intercourse, allowing for spontaneity and convenience. This feature is unique to female condoms and is not shared by male condoms, which must be applied immediately before intercourse. The question stem asks for a primary advantage, and this timing flexibility is a scientifically supported benefit.
Rationale for incorrect answers
1.Female condoms are generally more expensive than male condoms. The cost per unit is higher due to manufacturing complexity and lower market volume. This makes them less accessible in low-resource settings, negating cost as an advantage.
2.Aesthetic preference is subjective and not a scientifically validated advantage. Studies show mixed responses regarding user satisfaction and appearance. The bulkiness and external ring may be considered less appealing by some users.
4.Female condoms offer comparable, not superior, protection against STIs. While they cover more external genitalia, male latex condoms have higher tensile strength and lower breakage rates. Neither offers complete protection against all STIs, especially those transmitted via skin-to-skin contact like herpes simplex virus or human papillomavirus.
Take home points
- Female condoms can be inserted up to 8 hours before intercourse, offering timing flexibility.
- They are more expensive than male condoms and less widely available.
- Both male and female condoms offer protection against STIs but not complete coverage.
- Aesthetic preference is not a scientifically supported advantage of female condoms.
A nurse is teaching about diaphragms. What is required for effective use?
Explanation
Diaphragmsare dome-shaped barrier contraceptives placed over the cervix to prevent sperm entry. Effective use requires spermicide, which immobilizes or kills sperm. Diaphragms must be fitted by a provider to ensure proper cervical coverage. They should be inserted before intercourseand left in place for at least 6 hourspost-coitus but not more than 24 hoursto reduce risk of Toxic Shock Syndrome. They do not protect against STIs. Normal vaginal pH (3.8–4.5) is not altered by diaphragm use, but spermicide may cause irritation in some users.
Rationale for correct answers
2.Diaphragms must be used with spermicide to ensure contraceptive efficacy. The spermicide acts as a chemical barrier, enhancing the physical barrier provided by the diaphragm. Without spermicide, the diaphragm alone is insufficient to prevent pregnancy.
Rationale for incorrect answers
1.Diaphragms are not inserted daily but only before intercourse. Daily insertion is unnecessary and may increase risk of irritation or infection. The timing of insertion is intercourse-dependent, not routine.
3.Prescription antibiotics are not required for diaphragm use. There is no prophylactic indication unless an infection is present. Routine use of antibiotics would pose unnecessary risk of resistance and side effects.
4.Diaphragms must remain in place for at least 6 hours after intercourse to ensure sperm are immobilized or killed. Removal after 2 hours is too early and compromises effectiveness. Maximum retention should not exceed 24 hours to avoid Toxic Shock Syndrome.
Take home points
- Diaphragms require spermicide for effective contraception.
- They must remain in place for at least 6 hours post-intercourse.
- Daily insertion is not recommended or necessary.
- Antibiotics are not part of routine diaphragm use.
A nurse is counseling a couple considering permanent contraception. The male partner is interested in a vasectomy. What is a key piece of information the nurse must convey about the effectiveness of a vasectomy?
Explanation
Vasectomyis a permanent male sterilization procedure involving ligation or occlusion of the vas deferensto prevent sperm transport. It does not affect testosterone production, libido, or ejaculation volume. Post-procedure, residual sperm may persist in the distal reproductive tract for several weeks. Azoospermia, defined as absence of sperm in semen, must be confirmed via semen analysis, typically performed at 8–16 weeks post-procedure. Normal sperm concentration is ≥15 million/mL; azoospermia is <1000 sperm/mL or none detected. Vasectomy does not protect against STIsand is not guaranteed reversible.
Rationale for correct answers
2.Vasectomy requires follow-up semen analysis to confirm azoospermia. Sperm may remain in the ejaculatory ducts for weeks, and contraception must continue until semen is confirmed clear. This is essential for ensuring effectiveness and preventing unintended pregnancy.
Rationale for incorrect answers
1.Vasectomy is not immediately effective. Sperm distal to the occlusion site can persist for up to 20 ejaculations or several weeks. Immediate reliance on vasectomy without confirmation risks pregnancy.
3.Vasectomy does not reduce STI risk. It only prevents sperm transport, not transmission of infectious agents. Barrier methods like condoms are still required for STI protection.
4.Vasectomy is considered permanent. While reversal is possible via vasovasostomy or vasoepididymostomy, success rates vary and are not guaranteed. Reversal is complex, costly, and not universally successful.
Take home points
- Vasectomy requires semen analysis to confirm azoospermia before discontinuing contraception.
- It is not immediately effective post-procedure.
- It does not protect against STIs.
- Reversal is possible but not guaranteed; vasectomy should be considered permanent.
Which of the following are benefits of using long-acting reversible contraceptives (LARCs)? Select all that apply.
Explanation
Long-acting reversible contraceptives (LARCs)include intrauterine devices (IUDs) and subdermal implants. They provide extended contraceptionwithout user action, lasting from 3 to 10 yearsdepending on type. They are highly effective, with failure rates <1%, and are reversibleupon removal, allowing rapid return to fertility. LARCs do not protect against STIs, and barrier methods are still required. They are suitable for adolescents, with no age restrictions. Normal menstrual cycle length is 21–35 days; LARCs may alter bleeding patterns but do not affect systemic hormone levels significantly.
Rationale for correct answers
1.LARCs have efficacy >99%, with failure rates <1% per year. This is due to minimal user dependency and continuous hormone or copper release. Their effectiveness surpasses that of pills, patches, or rings.
3.LARCs are reversible upon removal. Fertility typically returns within days to weeks. This reversibility distinguishes them from permanent methods like sterilization.
5.LARCs are suitable for adolescents. They are safe, effective, and recommended by major guidelines including ACOG and WHO. They reduce unintended pregnancy rates in this population.
Rationale for incorrect answers
2.LARCs do not require daily adherence. This is a major advantage over oral contraceptives, which have typical-use failure rates of 7% due to missed doses. LARCs eliminate user error.
4.LARCs do not protect against STIs. They prevent pregnancy but offer no barrier to pathogens. Condoms remain necessary for STI prevention, especially in high-risk populations.
Take home points
- LARCs are >99% effective and user-independent.
- They are reversible and fertility returns quickly after removal.
- Adolescents can safely use LARCs.
- LARCs do not protect against STIs; condoms are still needed.
Which of the following are recognized advantages of using a hormonal Intrauterine Device (IUD) like Mirena? Select all that apply.
Explanation
Hormonal intrauterine devices (IUDs)such as levonorgestrel-releasingsystems (e.g. Mirena) are long-acting reversible contraceptivesthat deliver localized progestinto the endometrium. They suppress endometrial proliferation, reduce menstrual bleeding, and alleviate dysmenorrhea. Mirena releases 20 µg/day of levonorgestrel and is effective for up to 5 to 8 years. It does not contain estrogen, making it suitable for women with contraindications to estrogen. Hormonal IUDs do not protect against STIs. Normal menstrual blood loss is <80 mL per cycle; Mirena can reduce this by up to 90%.
Rationale for correct answers
1.Hormonal IUDs significantly reduce menstrual bleeding and dysmenorrhea by thinning the endometrial lining and suppressing prostaglandin synthesis. Clinical trials show up to 90% reduction in menstrual blood loss.
3.Hormonal IUDs provide long-acting contraception with failure rates <1% per year. Mirena is effective for up to 8 years, requiring no user action after insertion.
4.Hormonal IUDs contain only progestin, not estrogen. They are suitable for women with estrogen-sensitive conditions such as migraine with aura, thromboembolic disorders, or hypertension.
Rationale for incorrect answers
2.Hormonal IUDs do not offer protection against STIs. They act locally to prevent pregnancy but do not form a barrier to infectious agents. Barrier methods are still required for STI prevention.
5.Hormonal IUDs do not require daily attention or insertion. They are placed once by a provider and remain effective for years. Daily maintenance is unnecessary and not part of their mechanism.
Take home points
- Hormonal IUDs reduce menstrual bleeding and dysmenorrhea.
- They are highly effective and long-acting.
- Suitable for women who cannot use estrogen.
Do not protect against STIs; condoms are still needed.
Which of the following are side effects of depot medroxyprogesterone acetate (DMPA)? Select all that apply.
Explanation
Depot medroxyprogesterone acetate (DMPA)is a progestin-only injectable contraceptiveadministered every 12 weeks. It suppresses ovulation, thickens cervical mucus, and thins the endometrium. Common side effects include weight gain, irregular bleeding, and bone mineral density lossdue to hypoestrogenic effects. DMPA delays return to fertility by 9 to 10 monthson average. It is safe during lactation, but does not increase milk supply. Normal bone mineral density (BMD) T-score is ≥−1.0; prolonged DMPA use may reduce BMD, especially in adolescents.
Rationale for correct answers
1.Weight gain is a documented side effect of DMPA, with average increases of 2–4 kg in the first year. It is attributed to increased appetite and fluid retention.
3.DMPA can reduce bone mineral density due to suppression of estrogen. This effect is reversible upon discontinuation but is significant in long-term use, especially in adolescents.
5.Irregular bleeding is common, especially in the first 6–12 months. It results from endometrial thinning and unpredictable shedding. Amenorrhea may develop with continued use.
Rationale for incorrect answers
2.DMPA does not result in immediate return to fertility. Ovulation may be delayed for 9–10 months after the last injection. This is due to prolonged suppression of the hypothalamic-pituitary-ovarian axis.
4.DMPA is compatible with breastfeeding but does not increase milk supply. It does not contain estrogen, which can suppress lactation, but its progestin component does not stimulate milk production.
Take home points
- DMPA causes weight gain, irregular bleeding, and potential bone density loss.
- Fertility return is delayed after discontinuation.
- Safe during lactation but does not enhance milk supply.
- Long-term use requires monitoring of bone health.
Which criteria must be met for the Lactational Amenorrhea Method (LAM) to be an effective contraceptive method? Select all that apply.
Explanation
Lactational amenorrhea method (LAM)is a temporary contraceptive strategybased on exclusive breastfeeding, amenorrhea, and infant age <6 months. It relies on prolactin-mediated suppressionof the hypothalamic-pituitary-ovarian axis, inhibiting gonadotropin-releasing hormone (GnRH)and thus ovulation. For LAM to be effective, breastfeeding must be frequent, including night feeds, and the mother must remain amenorrheic. Normal prolactin levels during lactation range from 100 to 400 ng/mL; elevated levels suppress GnRH. Once menstruation resumes or supplementation begins, contraceptive efficacy declines sharply.
Rationale for correct answers
1.Exclusive or near-exclusive breastfeeding maintains high prolactin levels, which suppress ovulation. Introduction of formula or solids reduces prolactin and compromises contraceptive efficacy.
3.LAM is only effective if the infant is <6 months old. After 6 months, complementary feeding begins and ovulatory cycles may resume, reducing reliability.
4.Frequent breastfeeding, including night feeds, sustains prolactin levels. Infrequent nursing allows prolactin to drop, increasing risk of ovulation and pregnancy.
Rationale for incorrect answers
2.Resumption of menses indicates return of ovulatory cycles. LAM is no longer effective once menstruation occurs, even if breastfeeding continues.
5.Regular formula supplementation reduces breastfeeding frequency and prolactin levels. This undermines the hormonal suppression of ovulation, making LAM ineffective.
Take home points
- LAM requires exclusive breastfeeding, amenorrhea, and infant age <6 months.
- Resumption of menses or formula use invalidates LAM.
- Frequent day and night breastfeeding maintains contraceptive efficacy.
- LAM is a temporary method and must transition to other contraception after 6 months.
Which of the following are key components of contraceptive counseling? Select all that apply.
Explanation
Contraceptive counselingis a patient-centered processthat integrates medical assessment, individual preferences, and educational supportto guide informed decision-making. It involves evaluating medical eligibility, discussing method efficacy, and respecting cultural and personal values. Effective counseling includes providing written materials, using shared decision-making, and avoiding bias or coercion. Blood pressure should be <140/90 mmHg for combined hormonal contraceptive eligibility. Counseling must be nonjudgmental, evidence-based, and tailored to the patient's reproductive goals.
Rationale for correct answers
1.Assessing medical history is essential to determine contraindications and eligibility for specific methods. Conditions like hypertension, migraines with aura, or thromboembolism affect method selection.
3.Addressing patient preferences ensures autonomy and satisfaction. Counseling must incorporate lifestyle, reproductive goals, and comfort with method characteristics.
4.Providing written materials reinforces verbal counseling, supports literacy, and allows patients to review information independently. It enhances retention and informed choice.
Rationale for incorrect answers
2.Coercive tactics violate ethical standards and undermine patient autonomy. Counseling must be voluntary, respectful, and free of pressure or manipulation.
5.Ignoring cultural beliefs compromises trust and effectiveness. Cultural sensitivity is critical to understanding patient values and ensuring method acceptability and adherence.
Take home points
- Contraceptive counseling must assess medical history for safe method selection.
- Patient preferences guide method choice and support autonomy.
- Written materials enhance understanding and informed decision-making.
- Cultural beliefs must be respected to ensure effective counseling.
Exams on Family Planning
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Family Planning Fundamentals
- Hormonal Contraception
- Intrauterine Contraception
- Barrier Methods And Spermicides
- Fertility Awareness–based Methods (Fabms)
- Emergency Contraception
- Permanent Contraception
- Special Populations And Medical Eligibility
- Contraceptive Counseling And Patient Education
- Practice Exercise 1
- Clinical Procedures And Complications
- Practice Excercise 2
- Case-based Nursing Management
- Practice Excercise 3
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
• Provide a rigorous, scientifically accurate compendium of modern contraceptive methods, including mechanisms of action, indications, contraindications, effectiveness, side-effect profiles, and practical clinical management.
• Apply WHO/CDC Medical Eligibility Criteria (MEC) to individualized contraceptive selection across diverse clinical scenarios (e.g., postpartum lactation, adolescents, VTE risk, migraines with aura, chronic liver disease).
• Master counseling frameworks that operationalize shared decision-making, motivational interviewing, confidentiality standards, and culturally responsive education.
• Execute safe initiation (“Quick Start”), follow-up, troubleshooting, and complication management for hormonal, intrauterine, barrier, FABMs, emergency, and permanent contraception.
• Integrate dual-protection strategies to reduce unintended pregnancy and sexually transmitted infection (STI) transmission, including partner counseling and referral.
• Prepare for high-stakes examinations and real-world clinical practice via embedded Nursing Insights, case-based pearls, and targeted practice questions.
Introduction
Family planning is a cornerstone of reproductive health, enabling individuals and couples to achieve desired birth spacing and family size while minimizing adverse obstetric and neonatal outcomes. Contraceptive care encompasses biomedical selection of methods, longitudinal safety surveillance, anticipatory guidance regarding side effects, and patient-centered counseling rooted in autonomy and equity. For nurses, mastery of contraceptive pharmacology, device techniques, and the MEC framework is essential to deliver evidence-based, culturally safe care across the reproductive lifespan, including adolescence, the immediate postpartum period, and perimenopause.
Family Planning Fundamentals
1.1 Definitions and Epidemiology
• Family Planning: A comprehensive set of services that permits voluntary prevention, spacing, or timing of pregnancies via contraceptive methods, fertility awareness, or permanent sterilization.
• Unintended Pregnancy: A pregnancy that is mistimed or unwanted at conception; it correlates with delayed prenatal care, maternal morbidity, and adverse neonatal outcomes.
• Global and Regional Patterns:
➤ Contraceptive prevalence and method mix vary by geography, cultural norms, legal frameworks, and health system capacity.
➤ Long-acting reversible contraceptives (LARCs) have increased in uptake due to high effectiveness and minimal adherence burden.
• Public Health Impact:
➤ Effective family planning reduces maternal mortality, preterm birth, and low birth weight by optimizing interpregnancy intervals (ideal ≥18–24 months).
➤ Access barriers include cost, stock-outs, provider bias, restrictive policies, and misinformation.
Nursing Insights
• Always document the client’s reproductive intentions (e.g., “pregnant in the next year: yes/no/unsure”). This single question reframes counseling, aligns method tiers with intentions, and identifies those who would benefit from LARC or permanent options.
• Integrate dual protection counseling whenever STI risk is nonzero; recommend condoms in addition to the chosen contraceptive.
• Screen for intimate partner violence (IPV) and reproductive coercion; discuss discreet methods (e.g., implant, IUD, POPs) and provide safety resources.
1.2 Physiology of Fertility and Reproductive Anatomy
• Hypothalamic–Pituitary–Ovarian (HPO) Axis:
➤ Gonadotropin-releasing hormone (GnRH) pulsatility → pituitary secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
➤ Folliculogenesis culminates in an LH surge triggering ovulation; luteal progesterone stabilizes endometrium.
• Cervical Mucus Dynamics:
➤ Estrogen-dominant peri-ovulatory mucus becomes abundant, clear, and spinnbarkeit (stretchy), facilitating sperm transport.
➤ Progesterone-dominant luteal mucus is viscous and scant, impeding sperm passage.
• Sperm Transport and Capacitation:
➤ Sperm traverse cervical canal and uterus to the ampulla; capacitation enhances acrosomal reaction for fertilization.
• Implantation Window:
➤ Occurs ~6–10 days post-fertilization; endometrium requires synchronized receptivity (integrins, cytokines, pinopodes).
Nursing Insights
• Clients with irregular cycles may misidentify the fertile window; FABMs require reliable observation training or may be unsuitable.
• Lactation suppresses GnRH, but LAM efficacy requires strict criteria; partial breastfeeding or infant age >6 months markedly reduces protection.
1.3 Mechanisms of Contraception: Biological Targets
• Ovulation Inhibition:
➤ Combined hormonal contraceptives (CHCs) suppress LH surge via negative feedback.
➤ Some progestin-only methods (e.g., implant, DMPA) consistently inhibit ovulation.
• Cervical Mucus Viscosity:
➤ Progestins thicken mucus, reducing sperm penetration (key for POPs and LNG-IUDs).
• Endometrial Effects:
➤ Progestin exposure renders endometrium less receptive to implantation; LNG-IUDs cause glandular atrophy and decidualization.
• Sperm Toxicity/Immobilization:
➤ Copper ions create a spermicidal inflammatory milieu and impair motility (Cu-IUD).
• Mechanical Barrier:
➤ Condoms, diaphragms, caps, and sponges physically prevent sperm from entering the upper genital tract.
1.4 Effectiveness Metrics: Perfect Use vs Typical Use; Pearl Index and Failure Rates
• Perfect Use: Method used consistently and correctly every time.
• Typical Use: Reflects real-world adherence, user error, and discontinuation.
• Pearl Index (PI): Pregnancies per 100 woman-years; lower values indicate higher effectiveness.
• Tiered Counseling:
➤ Tier 1 (Highest efficacy): LARCs (implants, IUDs) and sterilization (failure rate <1%).
➤ Tier 2: CHCs and DMPA (typical failure ~4–7% for CHCs; lower with DMPA adherence).
➤ Tier 3: Barriers, spermicides, FABMs (higher typical-use failure).
Nursing Insights
• When discussing effectiveness, anchor with absolute numbers (“<1 pregnancy per 100 users in a year” for LARCs) and compare with condoms (typical use ~13–18 pregnancies per 100 users/year depending on source). This concreteness improves informed choices.
• Clarify that typical-use failure for user-dependent methods is driven by missed/late doses, ring/patch gaps, or incorrect barrier use; pair with adherence aids (alarms, apps, synchronized refills).
1.5 Determinants of Method Selection: MEC, Comorbidities, Age, Postpartum/Lactation, Medications, Cultural/Legal Factors
• Medical Eligibility Criteria (MEC):
➤ Categorizes safety (1 = no restriction; 4 = unacceptable risk).
➤ Absolute CHC contraindications include migraine with aura, current smoking ≥35 years with ≥15 cigarettes/day, VTE, certain thrombophilias, severe hypertension, ischemic heart disease, stroke, active hepatic disease, and breast cancer.
• Life Stage Considerations:
➤ Adolescents: Favor LARCs for high efficacy and privacy; address confidentiality and STI risk.
➤ Postpartum/Lactating: Avoid estrogen early postpartum due to VTE risk and potential effect on milk supply; POPs, implant, IUDs are preferred.
➤ Perimenopause: Consider VTE risk and comorbidities; non-estrogen options often preferred.
• Medication Interactions:
➤ Enzyme inducers (e.g., rifampin-class, certain anticonvulsants) reduce steroid levels; recommend Cu-IUD, LNG-IUD, or DMPA/implant depending on agent.
• Cultural/Religious and Legal Contexts:
➤ Respect beliefs while providing accurate, unbiased information and alternatives (e.g., FABMs).
• Health Equity:
➤ Proactively mitigate barriers (cost, transport, clinic hours); offer same-day initiation, long refills, and community outreach.
Nursing Insights
• Quick safety screen heuristic: “HEADACHE” mnemonic for CHC red flags: Hypertension, Embolism (VTE), Aura (migraine), Diabetes with vascular disease, Age ≥35 + heavy Cigarettes, Hepatopathy, Estrogen-sensitive malignancy.
• For clients on enzyme-inducing antiepileptics, document a medication–method plan (e.g., implant + condom backup or IUD) and liaise with neurology for possible regimen modification.
Hormonal Contraception
1.1 Combined Hormonal Methods (COCs, Transdermal Patch, Vaginal Ring)
• Mechanism: Ethinyl estradiol (or estradiol valerate) + progestin suppress GnRH/FSH/LH → ovulation inhibition; progestin thickens cervical mucus; endometrium becomes unreceptive.
• Formulations & Regimens:
➤ COCs: Monophasic (fixed doses) vs multiphasic; 21/7, 24/4, or extended/continuous cycles.
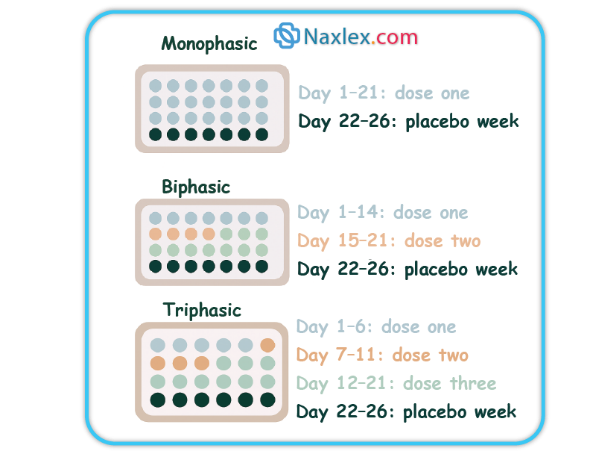
Weekly application x3 weeks then 1 patch-free week (or continuous); reduced efficacy possible at higher body weight for some products.
➤ Ring: Intravaginal device worn 3 weeks on/1 week off (or continuous).
• Noncontraceptive Benefits:
➤ Reduced dysmenorrhea, menorrhagia, and acne; cycle regulation; reduced risk of endometrial and ovarian cancers with long-term use.
• Contraindications (selected):
➤ Migraine with aura, smoking ≥35y with heavy use, VTE history, major thrombophilia, ischemic heart disease, stroke, severe hypertension, active hepatic disease, estrogen-sensitive cancers, early postpartum.
• Adverse Effects & Management:
➤ Breakthrough bleeding (optimize adherence, consider higher estrogen or different progestin).
➤ Nausea (take with food/at bedtime), breast tenderness, mild BP increase.
➤ Rare: VTE, stroke, MI in high-risk individuals.
• Initiation:
➤ Quick Start if reasonable certainty patient is not pregnant; backup x7 days unless starting within first 5 days of menses.
Nursing Insights
• For clients with migraine with aura, avoid all estrogen-containing methods; prioritize POPs, implant, IUDs, or DMPA.
• Patch adherence issues often stem from detachment; instruct on firm application to clean, dry skin and rotating sites; counsel on replacement if detachment >24 hours.
1.2 Progestin-Only Pills (POPs, “Minipill”)
• Mechanism: Primary—cervical mucus thickening; ovulation suppression in a subset depending on formulation.
• Use Pattern: Same time daily with a narrow window (often ≤3 hours for traditional norethindrone POPs); newer drospirenone POPs allow a slightly longer window per product labeling.

• Candidates: Lactating clients, estrogen contraindications, migraine with aura, smokers ≥35 years.
• Adverse Effects: Irregular spotting/bleeding, amenorrhea in some users.
• Missed Pill Protocol: If late beyond allowed window, take immediately and use backup for specified period (often 48 hours for norethindrone POPs).
Nursing Insights
• Counsel clients to set alarms and keep on-person backup condoms; a single late POP dose can reduce efficacy due to mucus thinning.
1.3 Injectable Progestin (Depot Medroxyprogesterone Acetate, DMPA)
• Dosing: 150 mg IM or 104 mg SC every 12–13 weeks.
• Mechanism: Consistent ovulation suppression, thickened cervical mucus, and endometrial atrophy.
• Benefits: Highly effective, privacy, reduction in dysmenorrhea and endometriosis-related pain; potential seizure threshold benefits.
• Adverse Effects:
➤ Menstrual changes: Irregular bleeding initially, progressing to amenorrhea in many users.
➤ Weight gain in some; delayed return to fertility (median ~9–10 months after last injection).
➤ Bone mineral density (BMD) loss—generally reversible; ensure calcium/vitamin D intake and weight-bearing exercise.
• Considerations:
➤ Good for those who cannot use estrogen or desire infrequent dosing; provide on-time appointment systems.
Nursing Insights
• At initiation, set next injection appointment before discharge and send calendar invites/text reminders. Discuss expected bleeding patterns proactively to reduce discontinuation.
1.4 Contraceptive Implant (Etonogestrel Subdermal Implant)
• Duration: Up to 3 years (some guidelines allow extended use in certain contexts).
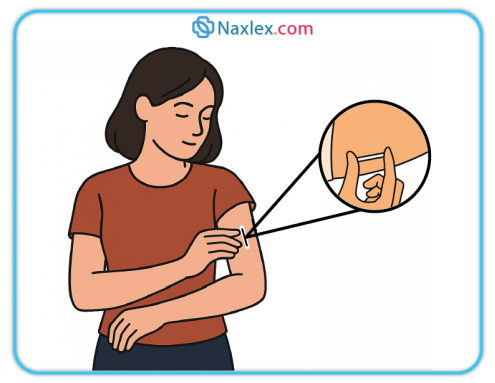
Inhibits ovulation and thickens cervical mucus.
• Effectiveness: >99% typical-use; rapid return to fertility on removal.
• Adverse Effects: Irregular bleeding patterns (spotting, amenorrhea, or prolonged bleeding), rare insertion/removal complications, potential bruising.
• Insertion/Removal: Office-based; confirm palpation post-insertion; maintain site dressing per protocol.
Nursing Insights
• For bothersome bleeding, offer short courses of NSAIDs, combined pills (if no contraindication), or tranexamic acid per local protocols; document shared decision and reassess.
1.5 Drug–Drug Interactions and Special Populations
• CYP3A inducers (e.g., rifampin, certain anticonvulsants, St. John’s wort) can reduce steroid levels, particularly impacting COCs, POPs, and emergency levonorgestrel; consider IUDs or DMPA which are less impacted.
• GI malabsorption (e.g., post-bariatric surgery) may reduce oral method effectiveness; prefer non-oral LARC.
• Obesity: Patch efficacy may be lower at higher body weight for some products; LARCs or IUDs avoid weight-based pharmacokinetic concerns.
1.6 Adverse Effects, Contraindications, and Management Algorithms
• Unscheduled Bleeding:
➤ First 3–6 months: expectant management; rule out pregnancy, STIs, and device malposition if severe/persistent.
➤ Targeted therapy: NSAIDs, short CHC course adjunct (if eligible), or method switch.
• Headache, Nausea, Breast Tenderness: Usually self-limited; supportive care; consider progestin type switch for mood/breast symptoms.
• Serious Events: Educate on ACHES warning for CHCs—Abdominal pain (severe), Chest pain/SOB, Headache (severe), Eye problems, Severe leg pain—seek urgent care.
Nursing Insights
• Use standardized bleeding diaries to track patterns and response to interventions; attach to EMR for continuity.
• When switching methods, avoid gaps: overlap or use backup to maintain protection.
Intrauterine Contraception
1.1 Copper IUD: Mechanism, Eligibility, Insertion, Adverse Effects
• Mechanism: Copper ions induce sterile endometrial inflammatory response that is spermicidal and prevents fertilization; may impair implantation.
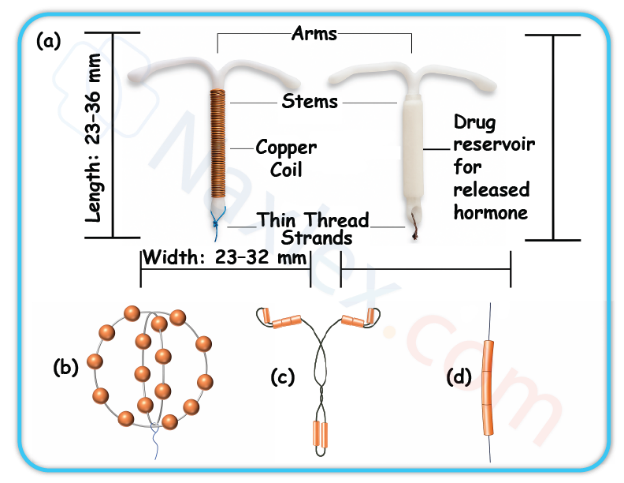
- Effectiveness: >99% with both perfect and typical use; immediate return to fertility on removal.
• Candidates: Desire hormone-free, long-acting, highly effective contraception; suitable as emergency contraception if placed within 5 days of unprotected intercourse.
• Adverse Effects: Heavier/longer menses, dysmenorrhea, especially in first cycles; rare perforation or expulsion.
• Insertion: Screen for pregnancy; STI screening per risk; use aseptic technique; counsel on cramping expectations; trim strings appropriately.
Nursing Insights
• Offer NSAIDs prophylactically before insertion to mitigate cramping; schedule follow-up or PRN visit for heavy bleeding counseling.
1.2 Levonorgestrel IUDs: Types, Doses, Amenorrhea, Noncontraceptive Benefits
• Mechanism: High local progestin levels → thick cervical mucus, endometrial decidualization/atrophy, variable ovulation suppression.
• Variants: Different LNG loads and durations (e.g., 52 mg for up to 5–8 years; lower-dose devices shorter duration per product).
• Benefits: Marked reduction in menstrual blood loss; treatment for heavy menstrual bleeding and dysmenorrhea; protective for endometrial hyperplasia in select contexts.
• Adverse Effects: Irregular bleeding initially, then lighter menses or amenorrhea; rare device complications as above.
Nursing Insights
• Normalize amenorrhea as a benign, expected outcome with LNG-IUDs; emphasize no buildup of blood occurs. Provide written aftercare instructions and when to return.
1.3 IUD Counseling, String Checks, Red Flags, and Complications
• String Check Education: Instruct how to palpate for strings monthly after menses; absence may indicate expulsion or retraction—seek evaluation.
• Red Flags (seek care): Pregnancy symptoms, severe pelvic pain/fever (possible PID), heavy bleeding unresponsive to OTC therapy, suspected expulsion (longer strings or device felt).
• Complications:
➤ Expulsion: Most common in first months; higher after immediate postpartum placement.
➤ Perforation: Rare; risk slightly increased during lactation and early postpartum.
➤ Pregnancy with IUD: If intrauterine pregnancy confirmed, remove IUD if strings visible to reduce adverse outcomes; if ectopic suspected, urgent evaluation.
1.4 Emergency Contraception with IUD
• Copper IUD provides the most effective EC when placed ≤120 hours after unprotected intercourse and offers ongoing contraception.
Nursing Insights
• If pregnancy occurs with IUD in situ, perform prompt location assessment (transvaginal ultrasound, hCG trend). Document counseling on risks and management choices, including continuation vs removal vs pregnancy options.
Barrier Methods And Spermicides
1.1 External (Male) and Internal (Female) Condoms
• External (Male) Condoms:
➤ Constructed of latex, polyurethane, or polyisoprene; a few available in lamb cecum (not protective against STIs).
➤ Mechanism: Physical barrier preventing semen from entering the vagina; latex/polyurethane types provide substantial protection against many STIs including HIV.
➤ Efficacy: Typical use ~82–87% (13–18 pregnancies per 100 women/year); perfect use ~98%.
➤ Use Considerations:
◆ Check expiration date and package integrity.
◆ Apply before any genital contact.
◆ Leave space at tip for semen collection; remove promptly after ejaculation, holding base to prevent slippage.
◆ Avoid oil-based lubricants with latex.
• Internal (Female) Condoms:
➤ Made from nitrile; inserted into vagina prior to intercourse; inner ring anchors near cervix, outer ring remains external.
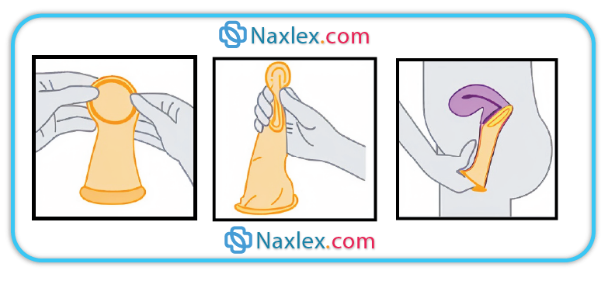
➤ Efficacy: Similar to male condoms with typical use.
➤ Advantages: Female-controlled, may be inserted up to 8 hours before intercourse, provides some protection against STIs.
Nursing Insights
• Demonstrate condom application on a model during counseling to ensure correct use—incorrect technique is a leading cause of barrier method failure.
• Always counsel to use a new condom for each act of intercourse and to store in a cool, dry place (avoid wallets or glove compartments where heat and friction degrade material).
1.2 Diaphragm, Cervical Cap, Contraceptive Sponge
• Diaphragm:
➤ Dome-shaped silicone cup used with spermicide; covers cervix to block sperm entry.
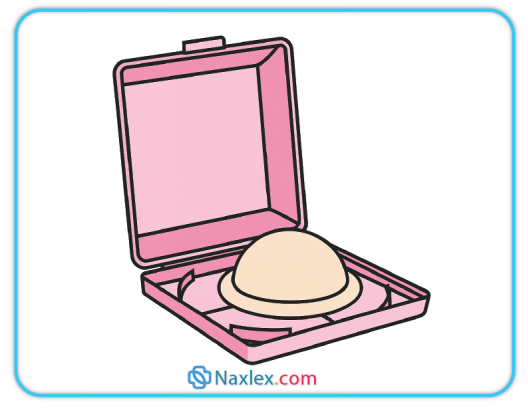
➤ Efficacy: Typical use ~88%; must remain in place ≥6 hours after intercourse but ≤24 hours.
➤ Fitting: Requires prescription and fitting by trained provider; must be refitted after childbirth or ≥10 lb weight change.
• Cervical Cap:
➤ Smaller silicone cup; fits tightly over cervix; used with spermicide.
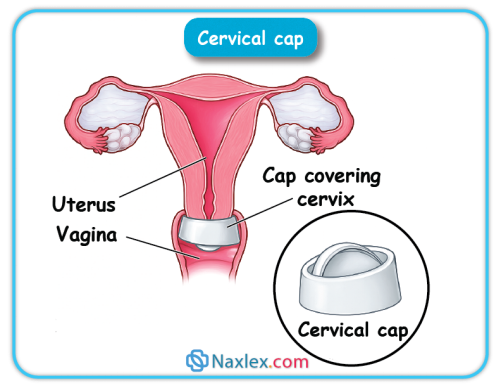
in place up to 48 hours; efficacy lower in parous women.
• Contraceptive Sponge:
➤ Polyurethane device containing nonoxynol-9 spermicide; moistened with water before use; provides up to 24 hours protection regardless of frequency of intercourse.
Nursing Insights
• For diaphragms and caps, emphasize reapplication of spermicide for repeat acts of intercourse without removal.
• Avoid use during menstruation or in women with recurrent urinary tract infections due to increased infection risk.
1.3 Spermicides and Lubricants
• Spermicides:
➤ Nonoxynol-9 most common; immobilizes and kills sperm; available as gels, foams, films, suppositories.
➤ Efficacy as sole method is low (~72% typical use); best used with barriers.
➤ Frequent use (>2/day) may irritate mucosa and increase HIV transmission risk in high-prevalence populations.
• Lubricants:
➤ Water-based and silicone-based safe with latex; oil-based degrade latex.
➤ Can enhance comfort and reduce condom breakage risk if appropriate type is chosen.
Fertility Awareness–based Methods (Fabms)
1.1 Calendar/Standard Days Method
• Based on menstrual cycle length; identifies fertile window (Day 8–19 for cycles 26–32 days).
• Requires daily charting; avoid unprotected intercourse during fertile window.
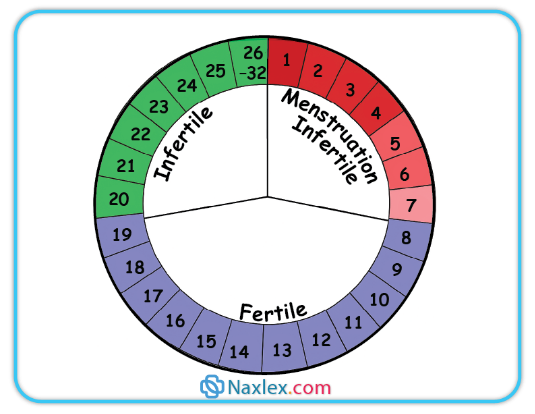
1.2 Cervical
Mucus (Billings) Method
• Daily assessment of mucus characteristics; ovulatory mucus is clear, stretchy (“spinnbarkeit”), slippery.
• Requires abstinence or barrier use during fertile mucus days.

1.2 Basal Body
Temperature (BBT) Method
• Daily temperature upon waking; slight rise (~0.3–0.5°C) after ovulation due to progesterone.
• Fertile window ends 3 days after temperature rise; sensitive to illness, alcohol, poor sleep.
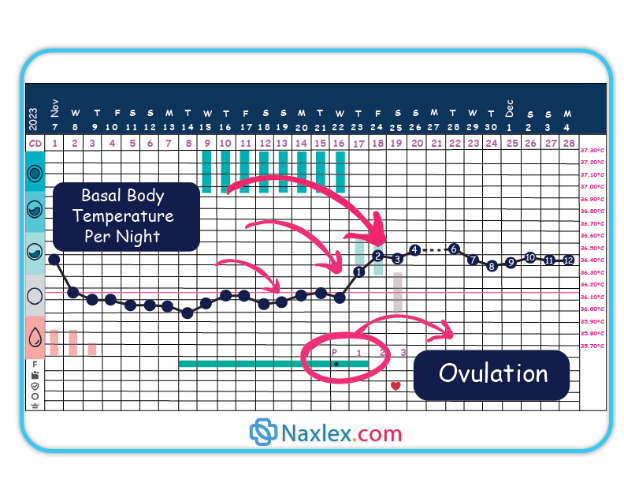
1.4 Symptothermal Method
• Combines BBT, cervical mucus, and other ovulation signs (e.g., mittelschmerz, cervical position).
• More effective than single-indicator methods.
1.5 Lactational Amenorrhea Method (LAM)
• Effective if:
➤ Infant <6 months old.
➤ Exclusive or near-exclusive breastfeeding on demand, day and night.
➤ Amenorrheic.
Nursing Insights
• FABMs require high motivation, consistent daily tracking, and partner cooperation; unsuitable for clients with irregular cycles.
• Illness, stress, or postpartum changes may alter fertility signs, leading to reduced reliability.
Emergency Contraception
1.1 Levonorgestrel Regimens
• Single-dose 1.5 mg or two doses of 0.75 mg 12 hours apart; available OTC in many settings.
• Most effective when taken within 72 hours but may have some efficacy up to 120 hours.
• Mechanism: Delays ovulation if not yet occurred.
Add ectopic pregnancy risk
1.2 Ulipristal Acetate
• Selective progesterone receptor modulator; effective up to 120 hours after unprotected intercourse; prescription required in many places.
• Superior efficacy to levonorgestrel in later part of 5-day window.
• Should not restart hormonal contraception until 5 days after use due to possible interaction.
1.3 Copper IUD as Emergency Contraception
• Most effective EC method; insert within 5 days of unprotected intercourse; provides ongoing contraception.
• Consider for clients at high risk of repeat unprotected sex and those wanting long-term contraception.
1.4 Counseling and Follow-Up After EC
• Warn about possible menstrual changes; advise pregnancy test if no withdrawal bleed within 3 weeks.
• Provide ongoing contraception initiation to prevent future unprotected episodes.
Nursing Insights
• EC does not terminate an established pregnancy—important for patient education to address misconceptions.
• Always use EC counseling as an opportunity to discuss and initiate a regular, reliable contraceptive method.
Permanent Contraception
1.1 Female Sterilization (Tubal Ligation/Salpingectomy)
• Mechanism: Occlusion, ligation, cauterization, or complete removal (salpingectomy) of the fallopian tubes to prevent sperm–oocyte meeting.
• Effectiveness: >99% in preventing pregnancy; failure rate ~0.5% in 10 years.
• Timing: Interval (nonpregnant state), postpartum (within 24–48 hours after delivery), or postabortion.
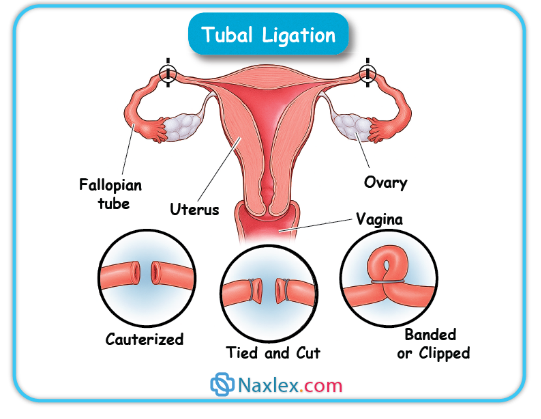
Advantages: Permanent, no ongoing maintenance, no hormonal exposure.
• Disadvantages: Requires surgery; carries anesthesia and surgical risks; regret possible, especially in women <30 years.
• Noncontraceptive Benefits: Bilateral salpingectomy may reduce ovarian cancer risk.
Nursing Insights
• Counsel on permanence—emphasize that reversal is not always possible or successful.
• Screen for ambivalence and external pressure; regret rates higher in younger patients and those with few children at time of procedure.
1.2 Male Sterilization (Vasectomy)
• Mechanism: Ligation or cauterization of vas deferens bilaterally to block sperm transport from testes to urethra.
• Effectiveness: >99% after azoospermia confirmed by semen analysis.
• Post-Procedure:
➤ Not immediately effective—backup contraception required until 1–2 semen analyses confirm no sperm (usually at 8–16 weeks or after 20 ejaculations).
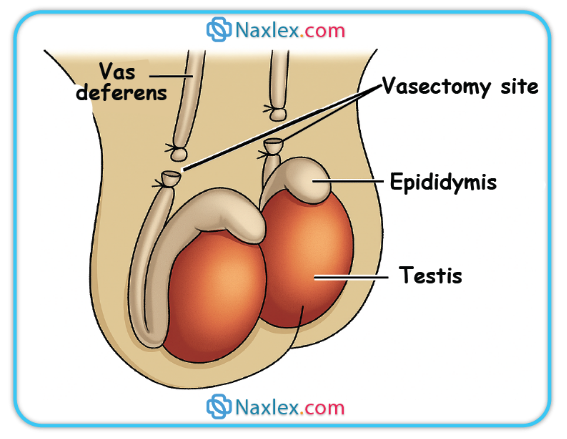
Advantages: Minor outpatient procedure; safer and less invasive than female sterilization.
• Disadvantages: Requires surgical access; small risk of chronic testicular pain; not protective against STIs.
Nursing Insights
• Many failures occur because couples stop using backup contraception before azoospermia is documented—schedule and emphasize follow-up semen analysis.
1.3 Regret, Failure, and Pre-Operative Counseling
• Regret Rates: Higher in those sterilized at a young age, during emotional distress, or under partner/family pressure.
• Failure: Rare, often due to technical error or recanalization.
• Pre-Operative Counseling:
➤ Discuss all reversible methods before sterilization.
➤ Obtain informed consent; document patient understanding and voluntary choice.
Special Populations And Medical Eligibility
1.1 Postpartum and Lactating Clients
• <21 days postpartum: CHCs contraindicated due to elevated VTE risk; progestin-only methods and non-hormonal methods are acceptable.
• Lactation: Estrogen can potentially decrease milk volume if started before lactation established; progestin-only and non-hormonal methods preferred.
1.2 Adolescents
• LARCs recommended as first-line by major organizations due to high efficacy and continuation rates.
• Emphasize confidentiality, STI prevention, and consent laws.
1.3 Perimenopause and ≥40 Years
• Fertility declines but persists; contraception recommended until menopause confirmed (12 months amenorrhea).
• CHCs may aid cycle regulation and vasomotor symptoms in healthy nonsmokers without contraindications.
1.4 Comorbidities
• Hypertension: Avoid CHCs in uncontrolled cases; progestin-only or non-hormonal preferred.
• VTE/Migraine with Aura: Avoid estrogen-containing methods.
• Liver Disease: Hormonal methods may be contraindicated in severe hepatic dysfunction.
• Diabetes: With vascular disease, avoid CHCs.
1.5 Enzyme-Inducing Medications
• Reduce efficacy of many hormonal methods except DMPA and IUDs.
• Counsel on backup methods or switching.
1.6 Cultural Sensitivity and Health Equity
• Assess beliefs, address myths respectfully, provide information in patient’s preferred language, and consider access barriers.
Nursing Insights
• Always cross-check patient’s health status against WHO/CDC Medical Eligibility Criteria before initiating a method.
• When working with adolescents, use developmentally appropriate language and ensure the encounter supports autonomy.
Contraceptive Counseling And Patient Education
1.1 Counseling Frameworks: Shared Decision-Making & Motivational Interviewing
• Explore patient values, preferences, reproductive goals.
• Provide unbiased, evidence-based information on all methods.
• Encourage patient participation and confirm understanding.
1.2 WHO/CDC MEC, Quick Start, and Follow-Up
• Use MEC to screen for contraindications.
• Quick Start method: Initiate contraception on day of visit if reasonably certain patient is not pregnant; backup needed for some methods.
• Schedule follow-up to assess satisfaction, side effects, and adherence.
1.3 Documentation, Informed Consent, Legal/Ethical Considerations
• Record counseling, method chosen, and patient’s consent.
• Be aware of laws regarding minors and contraception, spousal consent, and method-specific regulations.
1.4 Public Health Impact and Socioeconomic Benefits
• Reduces unintended pregnancies, maternal mortality, and abortion rates.
• Supports education and workforce participation.
Nursing Insights
• Always provide written materials and referral resources.
• Avoid coercive language—support patient autonomy.
• Be prepared to address myths (e.g., “IUDs cause infertility”) with factual information.
Clinical Procedures And Complications
1.1 Method Initiation Protocols and Timing
• Quick Start Protocol:
➤ Initiate contraception on the same day of the visit if reasonably certain the patient is not pregnant.
➤ Backup contraception required for some methods (e.g., CHCs, POPs) for a specified number of days unless initiated within first 5 days of menses.
• First-Day Start:
➤ Begin on day 1 of menstrual bleeding; immediate contraceptive protection for most hormonal methods.
• Sunday Start:
➤ Begin on the first Sunday after menstruation begins; designed to minimize weekend bleeding but requires backup for the first 7 days.
• Postpartum Start:
➤ Progestin-only methods and non-hormonal methods may be initiated immediately postpartum.
➤ CHCs delayed to ≥21 days postpartum if not breastfeeding, ≥42 days if breastfeeding and no VTE risk factors.
• Postabortion Start:
➤ Most methods can be initiated immediately following abortion or pregnancy loss, unless contraindications exist.
Nursing Insights
• For Quick Start, document last menstrual period, recent unprotected intercourse, and negative pregnancy test if performed; counsel on need for follow-up pregnancy test if there is any uncertainty.
• When counseling postpartum patients, ensure consideration of lactation impact and VTE risk timing.
1.2 Managing Side Effects and Complications
• Hormonal Methods:
➤ Breakthrough Bleeding: Often resolves after 3–6 months; may require dose adjustment or different progestin formulation.
➤ Nausea: Recommend taking with food or at bedtime.
➤ Weight Changes: Provide counseling on diet and exercise; assess for fluid retention.
➤ Mood Changes: Evaluate for history of mood disorders; consider progestin type change or non-hormonal method.
• IUD Complications:
➤ Expulsion: Educate on string check; most common in the first year.
➤ Perforation: Rare; usually occurs at insertion.
➤ Infection: Risk highest in first 20 days post-insertion; screen for STIs as indicated.
Nursing Insights
• Bleeding diaries are a practical tool to evaluate severity and impact of abnormal uterine bleeding on quality of life; adjust method based on pattern.
1.3 Suspected Pregnancy and Contraceptive Failure
• Assess Method Use: Check adherence, storage, timing, and any potential drug interactions.
• Testing: Confirm pregnancy with serum or urine hCG.
• Management:
➤ Hormonal Methods: Discontinue if pregnancy confirmed; no evidence of teratogenicity but unnecessary exposure avoided.
➤ IUD: If pregnant, remove IUD if strings visible to reduce risk of adverse outcomes.
1.4 STI Screening and Dual Protection Strategies
• Screening:
➤ Conduct based on risk assessment and CDC guidelines.
➤ Offer concurrent STI testing when initiating contraceptives.
• Dual Protection:
➤ Recommend condom use in addition to primary contraceptive for STI prevention, particularly in high-risk populations.
Nursing Insights
• Always emphasize that most contraceptive methods do not protect against STIs—condoms are essential for STI prevention in at-risk individuals.
Case-based Nursing Management
1.1 Adolescent First-Visit Contraception
• Scenario: 16-year-old seeking contraception, concerned about confidentiality.
• Approach: Assess sexual history, provide STI counseling, offer LARC as first-line, ensure privacy, clarify consent laws.
1.2 Postpartum, Lactation-Compatible Choices
• Scenario: 3 weeks postpartum, exclusively breastfeeding.
• Approach: Offer progestin-only pills, implant, or IUD; avoid CHCs until ≥6 weeks due to lactation and VTE risk.
1.3 Contraception with VTE/Migraine Risks
• Scenario: 30-year-old smoker with migraine with aura.
• Approach: Avoid estrogen-containing methods; recommend progestin-only or non-hormonal.
1.4 Irregular Cycles and PCOS
• Scenario: 25-year-old with oligomenorrhea and hyperandrogenism.
• Approach: CHCs for cycle regulation and androgen reduction if no contraindication; counsel on metabolic risk.
1.5 Postabortion Contraceptive Initiation
• Scenario: Client desires IUD after first-trimester abortion.
• Approach: Same-day IUD insertion if no infection; provide EC counseling for future prevention if indicated.
Nursing Insights
• Each scenario should be documented with method offered, rationale, patient preference, and informed consent.
• Always incorporate risk reduction for STIs in counseling, even if primary contraceptive method is non-barrier.
Summary
Family planning is an essential component of reproductive healthcare, enabling individuals and couples to achieve their desired timing and spacing of pregnancies while reducing unintended pregnancies and adverse maternal–infant outcomes. Contraceptive methods vary in mechanism, efficacy, reversibility, and suitability depending on patient-specific factors such as age, comorbidities, postpartum status, lactation, medication use, and cultural considerations.
Hormonal methods—including combined estrogen–progestin formulations (COCs, patch, ring) and progestin-only options (POPs, DMPA, implant)—primarily function by suppressing ovulation, thickening cervical mucus, and altering the endometrium. Non-hormonal intrauterine devices, particularly the copper IUD, act through a spermicidal inflammatory response. Levonorgestrel IUDs provide both high contraceptive efficacy and noncontraceptive benefits, such as menstrual reduction and treatment of heavy bleeding.
Barrier methods (male/female condoms, diaphragm, cervical cap, sponge) prevent sperm entry and may also provide STI protection, especially condoms. Fertility Awareness–Based Methods (FABMs) rely on recognition of fertile signs but require highly motivated, disciplined users. Emergency contraception options include levonorgestrel, ulipristal acetate, and copper IUD insertion—the latter being the most effective and longest-lasting solution.
Permanent methods (tubal ligation, vasectomy) offer highly effective contraception but require thorough counseling on irreversibility and follow-up, such as post-vasectomy semen analysis. Special populations—including adolescents, postpartum and lactating individuals, and those with medical comorbidities—require tailored method selection using the WHO/CDC Medical Eligibility Criteria to maximize safety and efficacy.
Effective contraceptive counseling hinges on shared decision-making, unbiased information delivery, cultural sensitivity, and informed consent. Nurses play a pivotal role in initiating, managing, and troubleshooting contraceptive methods, addressing side effects, reinforcing dual protection for STI prevention, and promoting health equity in reproductive care.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Family Planning
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


