Please set your exam date
Discomforts of Pregnancy
Study Questions
Practice Exercise 1
Which hormone is primarily responsible for nausea and vomiting in early pregnancy?
Explanation
Human chorionic gonadotropin (hCG)is a glycoprotein hormone produced by trophoblasts after implantation. It maintains the corpus luteum, stimulates progesteronesecretion, and peaks at 8–12 weeks gestation, reaching levels of 50,000–100,000 mIU/mL (normal non-pregnant <5 mIU/mL). High hCGconcentrations stimulate the chemoreceptor trigger zone, causing nauseaand vomiting. Elevated levels occur in molar pregnancy and multiple gestations.
Rationale for correct answers
2.hCG is the primary hormone responsible for nausea and vomiting in early pregnancy. Its peak around the end of the first trimester coincides with maximal morning sickness severity. Its stimulation of the chemoreceptor trigger zone and delayed gastric emptying explains the symptoms described.
Rationale for incorrect answers
1.Progesterone causes smooth muscle relaxation, decreased lower esophageal sphincter tone, and reduced gastrointestinal motility, which can contribute to bloating and constipation, not the primary mechanism for nausea and vomiting.
3.Estrogen is elevated in pregnancy and may have some role in enhancing sensitivity to odors, but its primary functions include uterine growth, increased blood flow, and breast tissue development. It does not directly stimulate the vomiting center.
4.Relaxin is secreted by the corpus luteum and placenta and functions mainly to relax pelvic ligaments and soften the cervix in preparation for delivery. It does not act on the gastrointestinal tract or central emetic pathways.
Take home points
- hCG is the main hormone responsible for nausea and vomiting in early pregnancy.
- Progesterone mainly causes constipation and reflux due to smooth muscle relaxation.
- Estrogen contributes to vascular changes and uterine growth, not emesis.
- Relaxin softens pelvic ligaments and cervix, unrelated to nausea.
A nurse is assessing a pregnant patient with nausea. Which tool is most appropriate for quantifying the severity of nausea and vomiting?
Explanation
Pregnancy-Unique Quantification of Emesis (PUQE) scoreis a validated tool developed specifically to assess the severity of nauseaand vomitingduring pregnancy. It measures 3 parameters: duration of nausea, number of vomiting episodes, and number of retching episodes over the past 24 hours. PUQE scores range from 3–15, with mild (≤6), moderate (7–12), and severe (≥13) classifications. This structured scoring allows objective monitoring of symptom severity and guides management, unlike nonspecific scales.
Rationale for correct answers
2.The PUQE score is the most appropriate and validated tool for quantifying the severity of nausea and vomiting in pregnancy. It assesses specific pregnancy-related gastrointestinal symptoms and provides a standardized classification that correlates with maternal and fetal outcomes.
Rationale for incorrect answers
1.The Visual Analog Scale (VAS) is useful for quantifying subjective symptom intensity, such as pain, but it is not specific to pregnancy-related nausea and vomiting. It does not capture frequency or duration of emesis, making it less clinically useful in this setting.
3.The McGill Pain Questionnaire is designed to evaluate qualitative and quantitative aspects of pain perception. It does not assess gastrointestinal symptoms or vomiting patterns and is inappropriate for pregnancy-associated nausea.
4.The Bristol Stool Chart is a tool used to classify stool form into 7 types to evaluate bowel habits and diagnose constipation or diarrhea. It has no role in assessing nausea or vomiting during pregnancy.
Take home points
- PUQE score is the validated tool for assessing nausea and vomiting severity in pregnancy.
- VAS is a general symptom intensity measure but not pregnancy-specific.
- McGill Pain Questionnaire evaluates pain, not emesis.
- Bristol Stool Chart is for stool consistency assessment, not nausea.
Which intervention would a nurse recommend to a pregnant client experiencing breast tenderness?
Explanation
Breast tenderness in pregnancyoccurs due to rising estrogen, increased progesterone, and elevated prolactin, which stimulate ductal and lobular-alveolar growth, leading to vascular engorgement and glandular hypertrophy. Normal serum estrogen in pregnancy rises from 200 pg/mL in early gestation to >10,000 pg/mL at term, while progesterone increases from 25 ng/mL to >150 ng/mL. Breast changesbegin as early as 6 weeks and include tenderness, areolar darkening, and Montgomery gland enlargement. Supportive measures, such as a well-fitting bra, help relieve discomfort without compromising circulation.
Rationale for correct answers
2.Wearing a supportive, well-fitting bra is the most effective non-pharmacological intervention for pregnancy-associated breast tenderness. It reduces strain on ligaments, decreases tissue movement, and minimizes discomfort caused by vascular congestion and hormonal stimulation.
Rationale for incorrect answers
1.Hot compresses are not recommended because they can increase vasodilation, worsen engorgement, and potentially elevate discomfort. They may also increase the risk of hyperthermia if applied excessively during pregnancy.
3.Avoiding physical activity is not a suitable intervention. Exercise is safe and beneficial in normal pregnancy, improving cardiovascular health and reducing complications. Limiting movement does not address the underlying cause of breast tenderness.
4.Limiting fluid intake is harmful, as adequate hydration is essential in pregnancy to maintain plasma volume, which normally expands by 40–50%. Reducing fluids does not relieve breast tenderness and increases risks of dehydration and hypotension.
Take home points
- Breast tenderness in pregnancy is primarily due to estrogen, progesterone, and prolactin effects.
- Supportive bras relieve discomfort by reducing tissue strain and engorgement.
- Hot compresses can worsen breast pain due to increased vasodilation.
- Fluid restriction is contraindicated in pregnancy and does not alleviate breast pain.
Urinary frequency in the first trimester is caused by:
Explanation
Urinary frequency in pregnancyoccurs due to early uterineenlargement and increased renalchanges that affect bladder capacity and function. By 6 weeks gestation, the uterus rises out of the pelvis, exerting pressureon the bladder, while renal plasma flow increases by 50–80% and glomerular filtration rate rises by 40–50% above the non-pregnant baseline of 90–120 mL/min/1.73 m². Increased filtrationalso contributes to physiologic glycosuria and mild polyuria. These adaptations are normal and help accommodate maternal and fetal metabolic demands.
Rationale for correct answers
2.Pressure from the enlarging uterus on the bladder is the main cause of urinary frequency in the first trimester. The uterus grows rapidly, and by 12 weeks gestation it is large enough to exert mechanical compression on the bladder, reducing capacity and increasing micturition episodes.
Rationale for incorrect answers
1.Decreased renal blood flow is not present in early pregnancy. Instead, renal plasma flow increases by 50–80% due to systemic vasodilation mediated by progesterone and relaxin. Increased perfusion, not decreased, characterizes renal physiology in early gestation.
3.Reduced glomerular filtration rate is not correct because GFR increases by 40–50% above baseline in pregnancy, reaching values around 150–180 mL/min/1.73 m². This rise leads to increased clearance of urea, creatinine, and electrolytes. Normal non-pregnant creatinine is 0.6–1.1 mg/dL, but in pregnancy levels drop to 0.4–0.8 mg/dL due to elevated GFR.
4.An increase in antidiuretic hormone does not occur in early pregnancy. Instead, there is a mild resetting of the osmotic threshold for thirst and ADH secretion, but baseline ADH concentrations remain unchanged. Plasma osmolality decreases by about 10 mmol/kg, yet this does not directly cause urinary frequency.
Take home points
- Urinary frequency in early pregnancy is primarily mechanical, due to uterine pressure on the bladder.
- Renal plasma flow and GFR increase significantly in pregnancy, not decrease.
- Normal creatinine levels are lower in pregnancy due to increased filtration.
- ADH secretion is unchanged; only the osmotic threshold for thirst is reset.
Which of the following interventions are appropriate for managing nausea and vomiting in pregnancy? Select all that apply.
Explanation
1.Consuming small, frequent meals helps by preventing gastric overdistension and reducing nausea. Empty stomachs and large meals worsen symptoms, so this dietary adjustment is first-line management.
2.Avoiding strong odors is effective because heightened olfactory sensitivity in pregnancy exacerbates nausea. Avoidance of triggers reduces vomiting episodes.
4.Using ginger-based remedies has proven antiemetic properties by modulating serotonin receptors in the gastrointestinal tract. Clinical studies show ginger reduces nausea severity without adverse fetal effects.
Rationale for incorrect answers
3.Eating large, high-fat meals worsens gastric emptying time, increases nausea, and is contraindicated. High-fat foods are harder to digest and increase reflux risk, which aggravates vomiting.
5.Limiting fluid intake is harmful, as dehydration worsens nausea and increases the risk of hypovolemia. Recommended strategy is sipping fluids between meals to maintain hydration and reduce gastric overfilling.
Take home points
- Nausea and vomiting in pregnancy are linked to high hCG and estrogen levels.
- Small, frequent meals and avoiding triggers reduce symptoms effectively.
- Ginger is safe and evidence-supported as a natural antiemetic.
- Large, fatty meals and fluid restriction worsen symptoms and are contraindicated.
Practice Exercise 2
Which physiological change contributes to heartburn in pregnancy?
Explanation
Heartburn in pregnancyoccurs due to hormonal and mechanical influences. Rising progesteronecauses smooth muscle relaxation, particularly of the lower esophageal sphincter (LES), reducing its resting pressure. Normal LES pressure is 10–30 mmHg, but in pregnancy it decreases significantly, allowing refluxof gastric contents. Additionally, uterineenlargement increases intra-abdominal pressure, exacerbating gastroesophageal reflux. Delayed gastric emptying also contributes, but the primary mechanism is LES relaxation.
Rationale for correct answers
3.Relaxation of the lower esophageal sphincter is the main cause of heartburn in pregnancy. Progesterone reduces LES tone, impairing the barrier between stomach and esophagus, which allows acid reflux and produces the burning sensation.
Rationale for incorrect answers
1.Increased lower esophageal sphincter tone does not occur in pregnancy. Instead, LES tone decreases, making reflux more likely. Increased tone would actually protect against heartburn.
2.Decreased intra-abdominal pressure is incorrect, as intra-abdominal pressure increases due to uterine expansion. This mechanical effect worsens reflux but is not the primary hormonal mechanism.
4.Accelerated gastric emptying does not occur; in fact, gastric emptying is slowed in pregnancy due to progesterone effects, further promoting reflux. Faster emptying would reduce reflux risk rather than increase it.
Take home points
- Heartburn in pregnancy is primarily due to progesterone-mediated LES relaxation.
- Normal LES pressure (10–30 mmHg) decreases significantly in pregnancy.
- Increased intra-abdominal pressure from the enlarging uterus worsens reflux.
- Delayed gastric emptying contributes but is secondary to LES relaxation.
A client with heartburn in the second trimester should be advised to:
Explanation
Heartburn in pregnancyis due to progesterone-mediated smooth muscle relaxation, reducing lower esophageal sphincter tone from its normal 10–30 mmHg and allowing gastric acid reflux. Uterineenlargement increases intra-abdominal pressure, worsening reflux, while delayed gastric emptyingfurther contributes. Symptoms are most pronounced in the 2nd and 3rd trimesters, with postprandial and recumbent positions being common triggers. Preventive strategies include dietary modifications, positional changes, and avoiding foods that decrease LES tone.
Rationale for correct answers
2.Avoiding lying down immediately after eating reduces reflux because gravity helps maintain gastric contents in the stomach. A minimum delay of 2–3 hours before reclining or sleeping is recommended to reduce heartburn episodes.
Rationale for incorrect answers
1.Eating large meals before bedtime worsens reflux by increasing gastric distension and acid production at a time when recumbency promotes reflux. Small, frequent meals are recommended instead.
3.Increasing intake of spicy and fatty foods aggravates reflux symptoms by further lowering LES tone and delaying gastric emptying, making this an inappropriate intervention.
4.Drinking carbonated beverages with meals increases gastric distension, promotes transient LES relaxations, and elevates reflux risk, worsening heartburn symptoms.
Take home points
- Heartburn in pregnancy is mainly caused by progesterone-mediated LES relaxation and increased intra-abdominal pressure.
- Patients should avoid lying down immediately after meals to reduce reflux.
- Small, frequent meals and avoidance of fatty/spicy foods are recommended.
- Carbonated beverages and large meals before bedtime worsen heartburn.
Which dietary recommendation is most effective for managing constipation?
Explanation
Constipation in pregnancyoccurs due to progesterone-induced smooth muscle relaxation, which slows intestinal transit, along with increased water absorption from stool. The enlarging uteruscompresses the bowel, worsening symptoms in later trimesters. Adequate fiberintake increases stool bulk and promotes colonic motility. Recommended daily fiber is 25–30 g, while normal adult fluid intake is 2–3 L/day to support bowel regularity. Constipation may also be aggravated by iron supplementation, so dietary adjustment is a first-line approach.
Rationale for correct answers
2.Increasing consumption of high-fiber foods such as fruits, vegetables, legumes, and whole grains improves constipation by enhancing stool bulk, stimulating peristalsis, and reducing colonic transit time. This is the most effective dietary recommendation.
Rationale for incorrect answers
1.Reducing fiber intake worsens constipation, as low-fiber diets decrease stool bulk and prolong colonic transit. This is the opposite of what is needed in management.
3.Avoiding hydration is harmful because dehydration leads to excessive water reabsorption from the colon, resulting in harder stools. Adequate hydration is essential for fiber to function effectively.
4.Limiting fruit intake removes an important source of soluble and insoluble fiber as well as natural sorbitol, which helps soften stools. Restricting fruits worsens constipation instead of improving it.
Take home points
- Constipation in pregnancy results from progesterone, uterine compression, and slowed intestinal transit.
- High-fiber diet (25–30 g/day) and hydration (2–3 L/day) are first-line measures.
- Reducing fiber or fluid intake worsens constipation.
- Fruits provide fiber and natural laxatives such as sorbitol, beneficial in constipation.
What is a recommended intervention for managing back pain in pregnancy?
Explanation
Back pain in pregnancyis caused by posturalchanges from uterine enlargement, increased lumbarlordosis, and hormonal effects of relaxinthat loosen ligaments and joints. The prevalence increases in the 2nd and 3rd trimesters. Normal relaxin levels rise from <100 pg/mL in non-pregnant women to >1,000 pg/mL in late pregnancy, leading to increased pelvicjoint mobility. Supportive devices such as maternity belts reduce spinal strain, improve posture, and relieve musculoskeletal discomfort without restricting mobility.
Rationale for correct answers
2.Use of a maternity belt provides external support to the lower back and abdomen, reducing lumbar strain, improving posture, and alleviating discomfort caused by ligament laxity and increased abdominal weight.
Rationale for incorrect answers
1.Prolonged standing worsens venous stasis, increases lumbar strain, and aggravates musculoskeletal pain. It should be avoided in women with pregnancy-associated back pain.
3.High-impact exercise, such as running or jumping, increases mechanical load on joints loosened by relaxin and worsens back pain. Safer alternatives include swimming, yoga, and walking.
4.Avoiding all physical activity is not recommended, as moderate exercise improves posture, strengthens core muscles, and relieves pain. Inactivity increases stiffness and worsens musculoskeletal discomfort.
Take home points
- Back pain in pregnancy results from postural changes, lumbar lordosis, and relaxin-mediated ligament laxity.
- Maternity belts relieve discomfort by supporting the abdomen and reducing spinal strain.
- Prolonged standing and high-impact exercise aggravate symptoms.
- Moderate physical activity improves pain control and functional mobility.
Which of the following factors contribute to heartburn in pregnancy? Select all that apply.
Explanation
Heartburn in pregnancyoccurs from hormonal and mechanical influences. Rising progesteronerelaxes smooth muscle, decreasing lower esophageal sphincterpressure from its normal 10–30 mmHg, allowing gastric reflux. Enlarging uterusincreases intra-abdominal pressure, further forcing gastric contents upward. Dietarytriggers such as spicy and fatty foods exacerbate symptoms by increasing gastric acid secretion and delaying emptying. Gastric emptying is normally slowed, not accelerated, in pregnancy. Preventive measures include dietary modification, upright posture after meals, and head elevation during sleep.
Rationale for correct answers
1.Relaxation of the lower esophageal sphincter is the primary physiological change due to progesterone, leading to decreased barrier pressure and increased reflux.
2.Increased intra-abdominal pressure from the enlarging uterus contributes mechanically to reflux, especially in the 2nd and 3rd trimesters.
4.Consumption of spicy foods worsens reflux by irritating the esophageal mucosa and stimulating gastric acid secretion, aggravating heartburn.
Rationale for incorrect answers
3.Accelerated gastric emptying does not occur; instead, gastric emptying is delayed in pregnancy due to progesterone, which increases reflux risk. Faster emptying would decrease reflux.
5.Elevated head position during sleep reduces nocturnal reflux by using gravity to keep gastric contents in the stomach, making it a management strategy rather than a contributing factor.
Take home points
- Heartburn in pregnancy is due to progesterone-induced LES relaxation and uterine pressure.
- LES pressure normally 10–30 mmHg decreases significantly in pregnancy.
- Spicy and fatty foods worsen reflux symptoms.
- Gastric emptying slows in pregnancy, contributing further to reflux.
Which of the following factors contribute to heartburn in pregnancy? Select all that apply.
Explanation
Heartburn in pregnancyoccurs from hormonal and mechanical influences. Rising progesteronerelaxes smooth muscle, decreasing lower esophageal sphincterpressure from its normal 10–30 mmHg, allowing gastric reflux. Enlarging uterusincreases intra-abdominal pressure, further forcing gastric contents upward. Dietarytriggers such as spicy and fatty foods exacerbate symptoms by increasing gastric acid secretion and delaying emptying. Gastric emptying is normally slowed, not accelerated, in pregnancy. Preventive measures include dietary modification, upright posture after meals, and head elevation during sleep.
Rationale for correct answers
1.Relaxation of the lower esophageal sphincter is the primary physiological change due to progesterone, leading to decreased barrier pressure and increased reflux.
2.Increased intra-abdominal pressure from the enlarging uterus contributes mechanically to reflux, especially in the 2nd and 3rd trimesters.
4.Consumption of spicy foods worsens reflux by irritating the esophageal mucosa and stimulating gastric acid secretion, aggravating heartburn.
Rationale for incorrect answers
3.Accelerated gastric emptying does not occur; instead, gastric emptying is delayed in pregnancy due to progesterone, which increases reflux risk. Faster emptying would decrease reflux.
5.Elevated head position during sleep reduces nocturnal reflux by using gravity to keep gastric contents in the stomach, making it a management strategy rather than a contributing factor.
Take home points
- Heartburn in pregnancy is due to progesterone-induced LES relaxation and uterine pressure.
- LES pressure normally 10–30 mmHg decreases significantly in pregnancy.
- Spicy and fatty foods worsen reflux symptoms.
- Gastric emptying slows in pregnancy, contributing further to reflux.
Practice Exercise 3
Leg cramps, particularly at night, are a common discomfort of pregnancy. What immediate action should the client take when experiencing a cramp?
Explanation
Leg cramps in pregnancyare frequent due to electrolyte imbalance, circulatory stasis, and increased uterine pressureon pelvic vessels. Hypocalcemia (serum calcium <8.5 mg/dL, normal 8.5–10.5 mg/dL) and hypomagnesemia (<1.7 mEq/L, normal 1.7–2.2 mEq/L) are contributors. Symptoms include sudden painful contractions, mostly at night. Correction involves dorsiflexion, stretching, adequate hydration, and replacement of calcium and magnesium.
Rationale for correct answers
3.Dorsiflexing the foot stretches the gastrocnemius muscle, immediately relieving muscle spasm by lengthening contracted fibers. It restores balance between calf muscles and relieves pain faster than massage or heat. Clinical guidelines recommend dorsiflexion as first-line management of acute cramp.
Rationale for incorrect answers
1.Vigorous massage may worsen the spasm by stimulating further contraction of muscle fibers. While gentle massage can aid recovery after stretching, it does not provide immediate relief of the acute cramp. It is not considered first-line action.
2.Applying a hot pack increases blood flow but does not rapidly relax the contracted muscle. Heat may help prevent recurrence but is too slow for immediate relief. Additionally, excessive heat use in pregnancy may cause thermal discomfort or risk of burns.
4.Elevating the leg without movement does not relieve the cramp because the muscle remains shortened and contracted. Elevation is useful for edema and venous return but ineffective for releasing an acute painful spasm.
Take home points
- Leg cramps in pregnancy are mainly due to electrolyte imbalance and venous stasis.
- Immediate management is dorsiflexion of the foot to stretch the calf.
- Heat, massage, and elevation may help afterward but are not first-line.
- Differentiation from deep vein thrombosis is essential, as DVT causes persistent pain, swelling, and warmth.
To prevent or alleviate varicose veins during pregnancy, a nurse would recommend:
Explanation
Varicose veins in pregnancyoccur due to venous stasis, increased blood volume, and hormonal relaxationof vessel walls from progesterone. Normal venous pressure in the legs is 60–90 mmHg standing, which increases in pregnancy, causing dilation and valve incompetence. Symptoms include visible tortuous veins, heaviness, and pain. Prevention includes leg elevation, compression therapy, and avoiding prolonged standing.
Rationale for correct answers
3.Wearing graduated compression stockings supports venous return by applying the greatest pressure at the ankle, gradually decreasing proximally. This reduces venous pooling, alleviates symptoms, and prevents progression of varicosities. Clinical guidelines recommend compression stockings as the most effective conservative measure.
Rationale for incorrect answers
1.Prolonged standing worsens venous stasis and increases hydrostatic pressure in the lower limbs. This promotes vein dilation and valve incompetence, aggravating varicosities instead of preventing them.
2.Avoiding leg elevation prevents blood from draining back toward the heart. Elevation above the level of the heart reduces venous pressure and edema, and thus is a recommended preventive measure. Not elevating the legs increases risk of symptom progression.
4.Crossing the legs frequently compresses venous return and obstructs circulation. This further increases venous pressure in the distal extremities, promoting pooling of blood and worsening of varicosities rather than alleviation.
Take home points
- Varicose veins in pregnancy result from venous stasis, increased blood volume, and progesterone-induced vessel relaxation.
- Graduated compression stockings are first-line prevention and management.
- Leg elevation and avoidance of prolonged standing help reduce venous pooling.
- Important differential is deep vein thrombosis, which requires urgent evaluation.
Which of the following interventions helps manage hemorrhoids during pregnancy?
Explanation
Hemorrhoids in pregnancydevelop due to increased venous pressure, constipation, and hormonal relaxationof vascular smooth muscle from progesterone. Normal bowel frequency is 3 times per day to 3 times per week, with stool water content of 70–75%. Constipation and straining raise rectal venous pressure, causing dilated hemorrhoidal veins. Symptoms include pain, itching, bleeding, and swelling. Management includes stool softeners, high-fiber diet (25–30 g/day), hydration (2–3 L/day), and local soothing measures.
Rationale for correct answers
3.Warm sitz baths promote relaxation of the anal sphincter, improve circulation, and provide symptomatic relief of pain and swelling. They are safe in pregnancy and recommended as a conservative, first-line measure for hemorrhoid management.
Rationale for incorrect answers
1.Straining during defecation increases intra-abdominal and rectal venous pressure, worsening hemorrhoidal congestion and pain. It also increases the risk of hemorrhoidal prolapse and bleeding.
2.Avoiding fluid intake leads to harder stools and constipation, aggravating hemorrhoids. Adequate hydration of 2–3 L/day is essential to soften stool and reduce straining.
4.Prolonged sitting increases perianal venous pressure and pooling, worsening hemorrhoid symptoms. It can also cause further irritation and swelling.
Take home points
- Hemorrhoids in pregnancy are due to venous congestion and constipation.
- Warm sitz baths are effective conservative therapy for pain relief.
- Adequate hydration, fiber intake, and avoidance of straining are essential preventive measures.
- Must differentiate hemorrhoids from anal fissures, which present with sharp pain and bright red bleeding.
Shortness of breath (dyspnea) in the third trimester is primarily caused by:
Explanation
Dyspnea in pregnancyis due to diaphragmatic elevation, increased oxygen demand, and maternal cardiorespiratory changes. In the third trimester, the diaphragm elevates by 4–5 cm because of uterine enlargement, reducing functional residual capacity from the normal 1800–2700 mL to as low as 1200 mL. Tidal volume rises from 450 mL to 600 mL, increasing minute ventilation by 30–40%. Symptoms include breathlessness, worsened on exertion or lying supine, but oxygenation remains normal. This is physiologic dyspnea, not pathology.
Rationale for correct answers
3.Elevation of the diaphragm by the enlarging uterus reduces lung volumes, especially functional residual capacity, making the woman feel short of breath. Despite this, tidal volume increases to compensate, maintaining normal oxygenation. This explains why dyspnea is common in late pregnancy but usually not pathological.
Rationale for incorrect answers
1.Oxygen consumption does not decrease in pregnancy; it actually increases by about 20% to meet maternal and fetal metabolic demands. A decrease in oxygen consumption would not explain dyspnea.
2.Significant lung damage is not a normal feature of pregnancy. Pathological lung damage may cause dyspnea, but in healthy pregnant women, respiratory mechanics, not disease, explain the symptom.
4.Reduced red blood cell count is not the main cause. Although physiologic anemia occurs due to hemodilution (plasma volume increases 40–50% vs. red blood cell mass 20–30%), it causes fatigue rather than the mechanical dyspnea seen in the third trimester.
Take home points
- Dyspnea in late pregnancy is primarily due to diaphragm elevation by the uterus.
- Tidal volume and minute ventilation increase to maintain oxygenation.
- Physiologic anemia causes fatigue, not true dyspnea.
- Important differential is pulmonary embolism, which causes sudden severe dyspnea with hypoxemia.
Which of the following are common management strategies for dependent edema in pregnancy? Select all that apply.
Explanation
Dependent edema in pregnancyresults from increased blood volume, venous stasis, and compression of the inferior vena cavaby the enlarging uterus. Plasma volume normally increases by 40–50% during pregnancy, and colloid osmotic pressure decreases from the normal 25 mmHg to about 22 mmHg, favoring fluid shift into interstitial tissues. Dependent edema is most pronounced in the lower extremities and worsens with prolonged standing. Management is conservative, aiming to improve venous return and reduce hydrostatic pressure.
Rationale for correct answers
1.Elevating legs and feet frequently decreases venous hydrostatic pressure, facilitates return of blood to the heart, and reduces pooling in the lower extremities, making it an effective measure.
2.Avoiding prolonged standing or sitting prevents venous stasis, which otherwise increases capillary hydrostatic pressure and promotes edema formation. Regular position changes are recommended.
4.Wearing support stockings provides external graduated compression, reducing venous pooling and edema formation, especially when used in the morning before edema develops.
5.Lying on the left side relieves pressure on the inferior vena cava, improving venous return and renal perfusion, thereby reducing fluid retention and lower extremity edema.
Rationale for incorrect answers
3.Limiting fluid intake significantly is inappropriate. Pregnant women require adequate hydration (2–3 L/day) to maintain plasma volume and amniotic fluid. Restricting fluids may worsen hemoconcentration, impair placental perfusion, and does not effectively treat dependent edema.
Take home points
- Dependent edema in pregnancy is due to venous stasis and increased plasma volume.
- Management is conservative with leg elevation, compression stockings, and avoiding prolonged standing.
- Adequate hydration must be maintained; fluid restriction is harmful.
- Differentiate from preeclampsia, where edema is associated with hypertension and proteinuria.
Comprehensive Questions
A pregnant patient reports persistent nausea and vomiting with weight loss. What condition should the nurse suspect?
Explanation
Hyperemesis gravidarumis severe nausea and vomitingin pregnancy leading to weight loss, electrolyte imbalance, and dehydration. Unlike normal morning sickness, it persists beyond the first trimester and interferes with nutrition. It is associated with elevated human chorionic gonadotropin(hCG) levels and more common in multiple gestation or molar pregnancy. Normal weight gain in pregnancy is 11.5–16 kg for women with BMI 18.5–24.9; weight loss instead of gain is abnormal. Laboratory findings include hypokalemia (<3.5 mEq/L), hyponatremia (<135 mEq/L), ketonuria, and metabolic alkalosis.
Rationale for correct answers
2.Hyperemesis gravidarum is suspected when nausea and vomiting are persistent, cause weight loss, and lead to dehydration or electrolyte disturbances. The presence of weight loss distinguishes it from physiologic morning sickness, making this the correct diagnosis.
Rationale for incorrect answers
1.Gastroesophageal reflux disease in pregnancy presents with heartburn, regurgitation, and epigastric discomfort due to relaxation of the lower esophageal sphincter. It does not cause severe persistent vomiting with weight loss.
3.Irritable bowel syndrome is characterized by abdominal pain, bloating, diarrhea, or constipation. It is not specific to pregnancy and does not present with persistent vomiting or weight loss.
4.Peptic ulcer disease causes epigastric pain, often related to meals, and may present with nausea. However, it does not typically cause severe persistent vomiting with maternal weight loss during pregnancy.
Take home points
- Hyperemesis gravidarum is defined by persistent vomiting with weight loss and electrolyte imbalance.
- Elevated hCG levels and multiple gestations increase risk.
- Differentiation from morning sickness is based on severity, persistence, and complications.
- Management includes hydration, electrolyte replacement, antiemetics, and nutritional support.
A nurse is educating a pregnant patient about heartburn prevention. Which recommendation is most effective?
Explanation
Heartburn in pregnancyis due to lower esophageal sphincter relaxation, progesterone effect, and gastric compressionby the enlarging uterus. Normal lower esophageal sphincter pressure is about 10–30 mmHg, but in pregnancy it decreases significantly, predisposing to gastroesophageal reflux. Gastric emptying time remains normal, but increased intra-abdominal pressure worsens reflux. Symptoms include burning retrosternal pain, regurgitation, and discomfort after meals or when lying down. Management includes postural modifications, dietary adjustments, and safe antacids if needed.
Rationale for correct answers
2.Elevating the head of the bed during sleep prevents reflux by using gravity to reduce upward flow of gastric contents into the esophagus. This is the most effective conservative strategy for heartburn prevention in pregnancy.
Rationale for incorrect answers
1.Lying down immediately after eating promotes reflux because gastric contents move more easily into the esophagus when supine. It worsens symptoms instead of preventing them.
3.Consuming large meals increases gastric distension and raises intra-abdominal pressure, predisposing to reflux. Smaller, more frequent meals are recommended instead.
4.Eating spicy foods stimulates gastric acid secretion and can irritate the esophagus, worsening heartburn. Avoiding spicy, fatty, and acidic foods helps reduce symptoms.
Take home points
- Heartburn in pregnancy is caused by progesterone-induced sphincter relaxation and uterine compression.
- Elevating the head of the bed is the most effective preventive strategy.
- Avoid lying down after meals, eating large meals, and irritating foods.
- Differentiate from peptic ulcer disease, which presents with localized epigastric pain related to meals.
What is a common cause of exacerbated fatigue in pregnancy?
Explanation
Iron deficiency anemia in pregnancyis the most common cause of excessive fatigue, due to hemodilution, increased iron demand, and reduced oxygen deliveryto tissues. Plasma volume increases by 40–50%, while red blood cell mass rises only 20–30%, causing physiologic anemia. Normal hemoglobin in pregnancy is ≥11 g/dL in the 1st and 3rd trimesters and ≥10.5 g/dL in the 2nd trimester; hematocrit should be ≥33%. Symptoms include pallor, fatigue, tachycardia, and decreased exercise tolerance. Severe cases increase maternal morbidity and risk of preterm birth.
Rationale for correct answers
2.Iron deficiency anemia reduces hemoglobin concentration and oxygen-carrying capacity of the blood, leading to tissue hypoxia. This is the most common pathological cause of persistent fatigue in pregnancy, beyond the normal physiologic tiredness.
Rationale for incorrect answers
1.Hyperthyroidism in pregnancy more often causes weight loss, palpitations, heat intolerance, and tremors, rather than isolated fatigue. It is much less common than anemia.
3.Elevated estrogen levels are normal in pregnancy and contribute to vascular changes and uterine growth. They do not directly cause severe fatigue.
4.Decreased progesterone levels are not typical in healthy pregnancy; instead, progesterone levels rise steadily. Low progesterone would threaten pregnancy but is not a cause of common fatigue.
Take home points
- Iron deficiency anemia is the leading cause of pathological fatigue in pregnancy.
- Hemoglobin <11 g/dL (1st/3rd trimester) or <10.5 g/dL (2nd trimester) defines anemia.
- Plasma volume expansion creates physiologic anemia, but iron deficiency worsens it.
Differentiate fatigue from thyroid disorders or depression in pregnancy.
Which hormone contributes to back pain by relaxing ligaments?
Explanation
Relaxin in pregnancyis a peptide hormone that causes ligamentous relaxation, increased pelvic mobility, and reduced joint stability, contributing to back and pelvic pain. It is secreted mainly by the corpus luteum, decidua, and placenta, with peak levels in the first trimester. Normal physiologic effects include softening of the cervix and widening of the pubic symphysis to prepare for delivery. Excessive ligamentous laxity, however, decreases spinal and pelvic support, leading to musculoskeletal discomfort.
Rationale for correct answers
3.Relaxin specifically loosens pelvic ligaments and soft tissues, reducing stability of the sacroiliac joints and lumbar spine. This directly contributes to the back pain commonly reported in pregnancy.
Rationale for incorrect answers
1.Estrogen promotes uterine growth, vascular proliferation, and breast development. While it supports connective tissue changes, it is not the primary cause of ligamentous relaxation leading to back pain.
2.Progesterone relaxes smooth muscle, reducing uterine contractility and gastrointestinal motility, but it does not significantly relax ligaments in the spine or pelvis.
4.hCG maintains the corpus luteum in early pregnancy and supports progesterone secretion. It does not affect ligaments or musculoskeletal support, so it is not a cause of back pain.
Take home points
- Relaxin is the hormone responsible for ligament relaxation and joint laxity in pregnancy.
- Ligamentous laxity contributes to back pain and pelvic instability.
- Estrogen and progesterone affect uterine and vascular changes, not ligamentous support.
- Back pain in pregnancy must be differentiated from pathologic causes such as urinary tract infection or disc disease.
Which medication is commonly used for severe heartburn in pregnancy?
Explanation
Severe heartburn in pregnancyis managed with acid-suppressing medicationsafter lifestyle modifications fail. Heartburn arises from lower esophageal sphincter relaxationdue to progesterone and mechanical pressure from the enlarging uterus. First-line management includes dietary adjustments, head elevation, and antacids. For persistent symptoms, H2 receptor antagonists such as ranitidineor famotidine are used. Gastric pH normally ranges 1.5–3.5, and acid suppression reduces reflux symptoms and esophageal irritation.
Rationale for correct answers
2.Ranitidine, an H2 receptor antagonist, reduces gastric acid secretion by blocking histamine action on parietal cells. It has historically been considered safe in pregnancy and commonly prescribed when antacids and lifestyle measures fail.
Rationale for incorrect answers
1.Ibuprofen is a nonsteroidal anti-inflammatory drug (NSAID) that inhibits prostaglandin synthesis. It can cause gastric irritation and is contraindicated in late pregnancy due to risk of premature ductus arteriosus closure and oligohydramnios.
3.Aspirin is also an NSAID with antiplatelet effects, increasing risk of gastrointestinal bleeding and fetal complications. It is not used for treating heartburn in pregnancy.
4.Acetaminophen is an analgesic and antipyretic, not an acid-suppressing drug. It does not affect gastric acid secretion and is therefore not effective for treating heartburn.
Take home points
- Severe heartburn in pregnancy is managed with H2 receptor antagonists when conservative measures fail.
- Ranitidine (historically) and famotidine are commonly used options.
- NSAIDs (ibuprofen, aspirin) are contraindicated in pregnancy for reflux.
- Acetaminophen relieves pain/fever but has no role in heartburn treatment.
Nausea and vomiting in the first trimester of pregnancy are primarily attributed to:
Explanation
Nausea and vomiting in early pregnancyare mainly due to elevated hCG, increased estrogen, and slowed gastrointestinal motility from progesterone. hCG peaks at 8–12 weeks (up to 100,000 mIU/mL, normal nonpregnant <5 mIU/mL), correlating with symptom severity. Estrogen contributes by delaying gastric emptying, while progesterone relaxes smooth muscle, reducing gastrointestinal peristalsis. Together, these changes cause queasiness, nausea, and occasional vomiting, known as morning sickness, which is physiological unless severe enough to cause dehydration or weight loss (hyperemesis gravidarum).
Rationale for correct answers
2.Elevated hCG, estrogen, and progesterone are the principal contributors to nausea and vomiting in the first trimester. Their hormonal effects explain the timing, severity, and natural improvement of symptoms after hCG levels plateau in the second trimester.
Rationale for incorrect answers
1.Decreased hCG does not cause nausea; rather, high circulating hCG correlates with symptom severity, especially in multiple gestation and molar pregnancy.
3.Gastrointestinal motility is not increased in pregnancy; progesterone actually decreases motility by relaxing smooth muscle, contributing to nausea, constipation, and bloating.
4.High maternal blood glucose is not a physiologic feature of early pregnancy and does not cause nausea. Gestational diabetes usually manifests later and presents differently (polyuria, polydipsia).
Take home points
- Nausea and vomiting in the first trimester are hormonally mediated by high hCG, estrogen, and progesterone.
- hCG peaks at 8–12 weeks, explaining timing of symptoms.
- Progesterone slows gastric emptying, adding to discomfort.
- Severe persistent vomiting suggests hyperemesis gravidarum, not normal morning sickness.
The backache commonly experienced in pregnancy is related to:
Explanation
Backache in pregnancyis mainly due to relaxin-induced ligament laxity, lumbar lordosis, and increased mechanical strainfrom fetal growth. Relaxin peaks in the first trimester and remains elevated, softening the pubic symphysis and sacroiliac joints to prepare for childbirth. This increased joint mobility reduces pelvic and spinal stability, predisposing to lumbosacral pain. Additionally, weight gain (11.5–16 kg normal for BMI 18.5–24.9) and shift of the center of gravity increase lordotic curvature, straining paraspinal muscles.
Rationale for correct answers
2.Relaxation of pelvic ligaments and joints due to relaxin decreases pelvic stability, contributing to lumbosacral and back pain in pregnancy. This hormonal effect, combined with postural changes, explains the musculoskeletal discomfort commonly reported.
Rationale for incorrect answers
1.Lumbar lordosis actually increases, not decreases, in pregnancy due to the anterior shift in center of gravity. This worsens back strain but is not decreased as stated.
3.Reduced maternal weight gain would lessen, not worsen, back strain. It is excessive weight gain that increases musculoskeletal discomfort.
4.Abdominal muscle strength decreases as the uterus enlarges, further reducing core support. Increased strength would help prevent backache, not cause it.
Take home points
- Pregnancy backache results from relaxin-induced ligamentous laxity and increased lumbar lordosis.
- Mechanical load from fetal growth and maternal weight gain exacerbates pain.
- Reduced abdominal muscle tone worsens postural instability.
- Important differentials include urinary tract infection and preterm labor, which can also present with back pain.
What is the primary management strategy for supine hypotensive syndrome?
Explanation
Supine hypotensive syndromeoccurs in late pregnancy due to compression of the inferior vena cava, decreased venous return, and reduced cardiac outputwhen the woman lies flat on her back. Normally, venous return maintains stroke volume and cardiac output at 4.5–6.5 L/min in pregnancy, but vena caval obstruction can decrease cardiac output by up to 25–30%. Symptoms include dizziness, pallor, hypotension (systolic <100 mmHg), tachycardia, and nausea. The condition is relieved by positional changes that restore venous return.
Rationale for correct answers
3.Turning the client to a side-lying position, preferably left lateral, relieves pressure on the inferior vena cava and restores venous return, cardiac output, and blood pressure. This is the primary and most immediate management strategy.
Rationale for incorrect answers
1.Elevating the legs may slightly improve venous return but does not resolve vena cava compression if the woman remains supine. It is not the primary management.
2.Administering intravenous fluids does not address the mechanical obstruction caused by the gravid uterus. Fluids may support blood volume but cannot restore venous return while the vena cava is compressed.
4.Encouraging the client to lie flat on her back worsens the condition, as the gravid uterus continues to obstruct vena caval flow, further decreasing cardiac output and exacerbating hypotension.
Take home points
- Supine hypotensive syndrome is due to inferior vena cava compression by the gravid uterus.
- Primary management is left lateral positioning to relieve pressure and restore venous return.
- IV fluids and leg elevation are supportive but ineffective without position change.
- Differentiate from hypovolemic shock, where hypotension is due to blood loss, not vena caval compression.
Braxton Hicks contractions are characterized by:
Explanation
Braxton Hicks contractionsare irregular uterine contractions, generally painless, that do not cause cervical change. They begin as early as the second trimester but are most noticeable in the third trimester. Uterine tone normally increases with pregnancy due to rising estrogen and oxytocin receptor sensitivity, but Braxton Hicks contractions remain non-progressive. They are sometimes referred to as “false labor” because, unlike true labor contractions, they do not lead to cervical effacement or dilation.
Rationale for correct answers
2.Irregular, often painless uterine contractions without cervical dilation or effacement are the hallmark of Braxton Hicks. They usually resolve with rest, hydration, or position change and are not considered true labor.
Rationale for incorrect answers
1.Regular, painful contractions that cause cervical dilation define true labor, not Braxton Hicks. True labor contractions progressively intensify and shorten in interval.
3.Braxton Hicks contractions improve, not worsen, with hydration and rest. Worsening with activity and persistence despite rest indicates true labor.
4.Braxton Hicks are not a sign of true labor. They are preparatory contractions and do not indicate imminent delivery.
Take home points
- Braxton Hicks contractions are irregular, mild, and non-progressive.
- They do not cause cervical dilation or effacement.
- True labor is characterized by regular, painful contractions with progressive cervical change.
- Hydration, rest, or position change relieves Braxton Hicks but not true labor.
What is a key difference between physiological edema of pregnancy and pathological edema that might indicate preeclampsia?
Explanation
Edema in pregnancycan be physiologicaldue to increased plasma volume, decreased colloid osmotic pressure, and uterine compressionof venous return, or pathological, as in preeclampsia. Plasma volume expands 40–50% and colloid osmotic pressure decreases from ~25 mmHg to ~22 mmHg, favoring dependent edema in legs and ankles. Physiological edema is gradual, dependent, and improves with rest or leg elevation. Pathological edema in preeclampsia is sudden, generalized (including face and hands), and associated with hypertension (≥140/90 mmHg after 20 weeks) and proteinuria (>300 mg/24h).
Rationale for correct answers
3.Physiological edema is dependent and improves with rest/elevation, while pathological edema in preeclampsia is sudden, generalized, and often resistant to postural changes. Its association with hypertension and proteinuria makes it clinically significant.
Rationale for incorrect answers
1.Physiological edema typically affects ankles and feet, not the face. Facial swelling is more concerning for preeclampsia.
2.Pathological edema is not localized to the ankles; it is usually generalized, involving face, hands, and sometimes entire body.
4.Pathological edema of preeclampsia occurs after 20 weeks, not in the first trimester. Early pregnancy edema is usually benign and physiologic.
Take home points
- Physiological edema is dependent, gradual, and resolves with rest and elevation.
- Pathological edema in preeclampsia is sudden, generalized, and associated with hypertension and proteinuria.
- Facial and hand swelling are red flags for preeclampsia.
- Differentiation is critical, as preeclampsia increases risk of maternal and fetal complications.
Which of the following interventions are effective for managing back pain in pregnancy? Select all that apply.
Explanation
Back pain in pregnancyarises from relaxin-induced ligament laxity, lumbar lordosis, and increased mechanical strainfrom fetal growth. Normal lumbar curvature increases as the uterus enlarges, shifting the center of gravity anteriorly. Relaxin loosens sacroiliac and pubic ligaments, decreasing joint stability. Risk is worsened by prolonged standing, poor posture, and reduced abdominal muscle tone. Management focuses on non-pharmacologic interventions to support the spine, relieve muscle strain, and improve posture.
Rationale for correct answers
1.Using a maternity belt supports the abdomen, redistributes weight, and reduces strain on lumbar muscles, effectively relieving back pain.
3.Practicing prenatal yoga improves posture, flexibility, and core strength, helping stabilize the spine and decrease musculoskeletal discomfort.
4.Applying heat therapy relaxes paraspinal muscles, reduces muscle spasm, and improves circulation, providing symptomatic relief for back pain.
Rationale for incorrect answers
2.Performing high-impact exercise increases mechanical strain and joint instability, worsening back pain. Safer options are low-impact activities such as swimming, walking, and prenatal yoga.
5.Prolonged standing aggravates venous stasis and lumbar strain, worsening discomfort instead of relieving it. Regular rest and position changes are recommended.
Take home points
- Back pain in pregnancy is caused by ligament laxity, lumbar lordosis, and increased load.
- Effective relief measures include maternity belts, prenatal yoga, and heat therapy.
- High-impact activity and prolonged standing worsen symptoms.
- Differential diagnoses include urinary tract infection and preterm labor, which can also present with back pain.
Which of the following are appropriate nursing assessments for constipation in pregnancy? Select all that apply.
Explanation
Constipation in pregnancyis due to progesterone-induced smooth muscle relaxation, reduced gastrointestinal motility, and increased water absorptionin the colon. Normal bowel frequency is 3 times per day to 3 times per week, with stool water content 70–75%. Constipation is worsened by iron supplements, low fiber intake (normal recommended 25–30 g/day), and dehydration (recommended fluid intake 2–3 L/day). Nursing assessment should focus on bowel habits, diet, and hydration status.
Rationale for correct answers
1.Evaluating bowel frequency and consistency identifies deviations from normal patterns and confirms constipation. Hard, infrequent stools suggest delayed colonic transit.
2.Assessing dietary fiber intake is essential since insufficient fiber reduces stool bulk and increases constipation risk. Recommended intake is 25–30 g/day.
4.Checking hydration status is important because inadequate fluid intake leads to excessive colonic water reabsorption, hardening stools. Adequate hydration softens stool and improves motility.
Rationale for incorrect answers
3.Monitoring respiratory rate is not relevant to constipation assessment. Respiratory changes in pregnancy are related to diaphragm elevation, not bowel habits.
5.Measuring blood glucose levels is related to screening for gestational diabetes, not constipation. Constipation is unrelated to glycemic status.
Take home points
- Constipation in pregnancy is due to progesterone, iron supplements, low fiber, and dehydration.
- Assessment should focus on stool frequency/consistency, fiber intake, and hydration status.
- Adequate hydration (2–3 L/day) and fiber (25–30 g/day) prevent constipation.
- Must differentiate constipation from bowel obstruction, which presents with pain, distension, and vomiting.
Which of the following are common discomforts typically experienced during the first trimester of pregnancy? Select all that apply.
Explanation
First trimester of pregnancyis characterized by profound hormonalchanges driven mainly by elevated estrogen, progesterone, and human chorionic gonadotropin (hCG). These hormones cause systemic effects including breast enlargement, fatigue, urinary frequency, and nausea/vomiting. Normal hCG rises rapidly, doubling every 48-72 hours, peaking at 100,000 mIU/mL around 9-10 weeks. Progesterone normally ranges from 11-90 ng/mL in the first trimester and promotes uterine relaxation but contributes to fatigue. Estrogen levels rise progressively, stimulating breast ductal growth and fluid retention. Increased renal plasma flow and glomerular filtration rate by about 50% explain urinary frequency.
Rationale for correct answers
1.Nausea and vomiting occur in the first trimester due to high hCG levels and rising estrogen, usually most pronounced between 6-12 weeks. The question stem asks about common discomforts, and this is one of the hallmark symptoms.
2.Breast tenderness is explained by estrogen-induced ductal proliferation and progesterone-driven lobular-alveolar development. Fluid retention and vascular engorgement during early pregnancy cause tenderness, making this a common early symptom.
4.Fatigue is due to elevated progesterone, increased basal metabolic rate, and demands of early embryonic development. Women often report significant tiredness even without physical exertion, making this a typical first-trimester discomfort.
5.Urinary frequency results from increased renal plasma flow and glomerular filtration rate, which peak early in pregnancy. The enlarging uterus also exerts pressure on the bladder, reinforcing this as a very common first-trimester symptom.
Rationale for incorrect answers
3.Leg cramps are not common in the first trimester but are more typical in the second and third trimesters. They result from altered calcium and magnesium metabolism, venous stasis from uterine compression of pelvic vessels, and increased neuromuscular excitability. They are not characteristic early discomforts.
Take home points
- First-trimester discomforts are mainly due to hormonal changes, not mechanical effects.
- Nausea/vomiting, breast tenderness, urinary frequency, and fatigue are characteristic early pregnancy symptoms.
- Leg cramps are more typical in later trimesters due to mechanical and metabolic changes.
- Understanding timing of symptoms helps differentiate normal discomforts from pathological conditions.
Which of the following are lifestyle modifications recommended for managing heartburn during pregnancy? Select all that apply.
Explanation
Heartburn in pregnancy(pyrosis) results from progesterone-induced relaxationof the lower esophageal sphincter, delayed gastric emptying, and mechanical pressurefrom the enlarging uterus. Gastric acid normally has a pH of 1.5–3.5, and disruption of esophageal sphincter tone allows reflux of this acidic content into the esophagus, producing burning retrosternal pain. Risk factors include large meals, lying supine after eating, fatty/spicy foods, and abdominal compression. Management emphasizes lifestyle and positional modifications.
Rationale for correct answers
1.Eating small, frequent meals prevents gastric overdistension, lowering reflux risk.
2.Avoiding spicy and fatty foods reduces gastric acid stimulation and delays gastric emptying, helping relieve symptoms.
4.Elevating the head of the bed during sleep decreases nocturnal reflux by using gravity to limit acid regurgitation.
5.Avoiding tight clothing around the abdomen reduces intra-abdominal pressure, lowering the chance of reflux.
Rationale for incorrect answers
3.Lying down immediately after eating worsens reflux because gravity no longer prevents acid regurgitation. Patients should wait at least 2–3 hours before lying down.
Take home points
- Heartburn in pregnancy is due to progesterone relaxation of the LES and uterine pressure.
- Small, frequent meals and avoidance of spicy/fatty foods help reduce reflux.
- Elevating the head of the bed prevents nocturnal symptoms.
- Tight abdominal clothing increases reflux risk and should be avoided.
Which of the following are "Best Practices" for nurses regarding the management of pregnancy discomforts? Select all that apply.
Explanation
Management of pregnancy discomfortsrelies on distinguishing physiological changesfrom signs of pathology, prioritizing non-pharmacological interventions, and setting realistic expectationsfor symptom progression. Normal discomforts arise from hormonal changes, mechanical uterine pressure, and metabolic adjustments, while pathological symptoms (e.g., hypertension ≥140/90 mmHg, proteinuria >300 mg/24h, vaginal bleeding) indicate complications. Nursing practice emphasizes safe symptom relief, patient education, and timely recognition of danger signs.
Rationale for correct answers
1.Differentiating between normal discomforts and warning signs ensures early recognition of conditions like preeclampsia, preterm labor, or gestational diabetes, preventing complications.
2.Emphasizing non-pharmacological interventions first (e.g., position changes, hydration, diet, exercise) minimizes fetal exposure to medications and provides safe symptom relief.
3.Providing realistic expectations helps patients cope with ongoing discomforts, such as backache, edema, or heartburn, and prevents unnecessary anxiety.
Rationale for incorrect answers
4.Encouraging self-diagnosis is unsafe because patients may misinterpret pathological symptoms (e.g., preeclampsia headache) as normal discomfort, delaying critical care.
5.Advising immediate hospitalization for any discomfort is unnecessary and impractical; most discomforts are benign and manageable at home unless accompanied by red-flag symptoms.
Take home points
- Nurses must differentiate physiological discomforts from pathological warning signs.
- Non-pharmacological management is first-line and safe in pregnancy.
- Patient education should set realistic expectations about persistent discomforts.
- Immediate medical attention is warranted only when red-flag symptoms appear.
Exams on Discomforts of Pregnancy
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
The objectives of these comprehensive nursing notes are to equip nursing students with a thorough understanding of the physiological and psychological discomforts experienced during pregnancy, enabling effective assessment, management, and patient education. By the end of this study, students will:
- Comprehensively describe the physiological mechanisms underlying common discomforts of pregnancy across all trimesters.
- Identify key assessment findings that differentiate normal pregnancy discomforts from potential complications requiring medical intervention.
- Apply evidence-based nursing interventions to alleviate discomforts and promote maternal well-being.
- Educate pregnant patients on non-pharmacological and pharmacological strategies to manage discomforts effectively.
- Recognize the importance of empathetic care and patient education in addressing psychological impacts of pregnancy discomforts.
Introduction
Pregnancy is a complex physiological state characterized by significant hormonal, anatomical, and metabolic changes that often result in discomforts affecting maternal quality of life. These discomforts, ranging from nausea and fatigue in the first trimester to edema and dyspnea in the third trimester, are primarily driven by hormonal fluctuations, uterine enlargement, and increased physiological demands. Nurses play a critical role in assessing these symptoms, differentiating normal physiological changes from pathological conditions, and implementing interventions to mitigate discomfort. These notes provide a detailed, scientific exploration of pregnancy discomforts, emphasizing evidence-based nursing care and patient education to prepare nursing students for clinical practice.
Nursing Insights: Nurses must understand the physiological basis of pregnancy discomforts to provide empathetic, evidence-based care. Comprehensive knowledge of these symptoms enables nurses to reassure patients, implement effective interventions, and identify warning signs of complications, ensuring optimal maternal and fetal outcomes.
Second Trimester Discomforts
The second trimester, spanning from 13 to 26 weeks of gestation, is characterized by continued hormonal and anatomical changes as the fetus grows rapidly. While some first-trimester discomforts, such as nausea, often subside, new symptoms emerge due to the enlarging uterus, increased intra-abdominal pressure, and persistent hormonal effects. Common second-trimester discomforts include heartburn, constipation, and back pain, each requiring targeted nursing assessment and interventions to promote maternal comfort and prevent complications.
1.1 Heartburn
Heartburn, or gastroesophageal reflux, is a prevalent discomfort in the second trimester, affecting approximately 30-50% of pregnant women. It results from physiological changes that impair esophageal function and increase acid reflux.

- Physiological Mechanisms:
- Progesterone-mediated relaxation of the lower esophageal sphincter (LES) reduces its tone, allowing gastric contents to reflux into the esophagus.
- Increased intra-abdominal pressure from the enlarging uterus compresses the stomach, promoting reflux.
- Delayed gastric emptying, driven by progesterone, prolongs acid exposure in the stomach, exacerbating reflux symptoms.
- Elevated estrogen levels enhance gastric acid secretion, contributing to esophageal irritation.
- Assessment:
- Assess the frequency, severity, and timing of heartburn, noting if symptoms occur postprandially or nocturnally.
- Evaluate for concerning symptoms, such as dysphagia, odynophagia, or weight loss, which may indicate esophagitis or other complications.
- Monitor dietary habits, identifying trigger foods (e.g., spicy, fatty, or acidic foods) that exacerbate symptoms.
- Assess for signs of dehydration or nutritional deficiencies if heartburn limits food intake.
- Nursing Interventions:
- Advise consuming small, frequent meals to reduce gastric distension and minimize reflux.
- Recommend avoiding trigger foods, including spicy, fatty, or citrus-based foods, and caffeine.
- Suggest elevating the head of the bed by 6-8 inches during sleep to prevent nocturnal reflux.
- Encourage upright positioning for at least 1-2 hours after meals to facilitate gastric emptying.
- Promote chewing gum to stimulate saliva production, which neutralizes gastric acid.
- Educate patients on safe antacids, such as calcium carbonate, under medical guidance for persistent symptoms.
- Pharmacological Considerations:
- Calcium carbonate antacids are safe and effective for mild heartburn relief in pregnancy.
- H2-receptor antagonists, such as ranitidine, may be prescribed for moderate to severe symptoms, per ACOG guidelines.
- Proton pump inhibitors (PPIs) may be considered for refractory cases but require medical supervision due to potential fetal risks.
Nursing Insights: Nurses must differentiate heartburn from pathological conditions, such as esophagitis or preeclampsia, by assessing for red flags like difficulty swallowing or severe epigastric pain. Patient education on lifestyle modifications, such as avoiding lying down immediately after meals, is critical to reducing symptom severity. Nurses should also monitor for psychological impacts, as chronic heartburn can lead to frustration or reduced quality of life.
1.2 Constipation
Constipation affects up to 40% of pregnant women in the second trimester due to hormonal and mechanical changes that slow gastrointestinal motility.

- Physiological Mechanisms:
- Progesterone-induced relaxation of gastrointestinal smooth muscle reduces peristalsis, leading to delayed colonic transit.
- Increased intra-abdominal pressure from the enlarging uterus compresses the intestines, further slowing motility.
- Iron supplements, commonly prescribed in pregnancy, can exacerbate constipation by altering gut motility.
- Increased water absorption in the colon, driven by hormonal changes, results in harder, less frequent stools.
- Assessment:
- Evaluate bowel movement frequency, consistency, and associated symptoms, such as straining or abdominal pain.
- Use the Bristol Stool Chart to assess stool type and identify constipation (Types 1-2 indicate hard, lumpy stools).
- Assess dietary fiber intake, hydration status, and physical activity levels, as these influence bowel function.
- Screen for complications, such as hemorrhoids or anal fissures, resulting from chronic straining.
- Nursing Interventions:
- Encourage increased consumption of high-fiber foods (e.g., fruits, vegetables, whole grains) to promote bowel motility.
- Advise adequate hydration (8-10 cups of water daily) to soften stools and facilitate passage.
- Recommend regular physical activity, such as walking or prenatal yoga, to stimulate peristalsis.
- Educate on safe stool softeners, such as docusate sodium, if dietary changes are insufficient, under medical guidance.
- Suggest natural remedies, like prune juice, to alleviate mild constipation.
- Pharmacological Considerations:
- Bulk-forming laxatives, such as psyllium, are safe and effective for constipation management in pregnancy.

- Osmotic laxatives, like lactulose, may be prescribed for persistent symptoms but require medical oversight.
- Stimulant laxatives should be avoided due to potential uterine stimulation and fetal risks.

- Stimulant laxatives should be avoided due to potential uterine stimulation and fetal risks.
- Bulk-forming laxatives, such as psyllium, are safe and effective for constipation management in pregnancy.
Nursing Insights: Nurses must assess for complications of constipation, such as hemorrhoids or rectal bleeding, and educate patients on preventive measures. Regular monitoring of bowel habits and early intervention can prevent progression to severe constipation or related complications. Nurses should also counsel patients on the side effects of iron supplements and suggest dietary adjustments to mitigate their impact.
1.3 Back Pain
Back pain, particularly in the lower back, is reported by 50-70% of pregnant women in the second trimester due to biomechanical and hormonal changes.

- Physiological Mechanisms:
- The enlarging uterus shifts the maternal center of gravity anteriorly, increasing lumbar lordosis and straining the lower back.
- Relaxin, a hormone that peaks in the second trimester, relaxes pelvic ligaments and joints, reducing spinal stability.
- Weakening of abdominal muscles due to uterine expansion contributes to poor posture and increased back strain.
- Increased maternal weight gain adds mechanical stress to the spine and supporting muscles.
- Assessment:
- Assess the location, intensity, and radiation of back pain using a pain scale (e.g., 0-10 Numeric Rating Scale).
- Evaluate for neurological symptoms, such as numbness, tingling, or weakness in the lower extremities, which may indicate sciatica or other complications.
- Monitor posture, gait, and activity levels to identify contributing factors, such as prolonged standing or improper lifting.
- Screen for red flags, such as severe pain unrelieved by rest or fever, which may suggest infection or disc herniation.
- Nursing Interventions:
- Educate on proper body mechanics, such as bending at the knees and avoiding heavy lifting, to reduce spinal strain.
- Recommend using a maternity support belt to stabilize the pelvis and lower back.
- Suggest prenatal yoga or stretching exercises to strengthen core muscles and improve flexibility.
- Advise applying heat therapy to relax tense muscles and alleviate discomfort.
- Encourage maintaining a neutral spine position during sitting and standing to minimize lordosis.
- Pharmacological Considerations:
- Acetaminophen is the preferred analgesic for back pain in pregnancy due to its safety profile.
- Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen, should be avoided due to potential fetal risks.
Nursing Insights: Nurses must differentiate physiological back pain from conditions like sciatica or preterm labor by assessing for neurological symptoms or uterine contractions. Patient education on posture and safe exercise is critical to preventing chronic pain and improving mobility. Nurses should also monitor for psychological impacts, as persistent pain can lead to anxiety or reduced physical activity, affecting overall maternal health.
Third Trimester Discomforts
The third trimester, spanning from 27 to 40 weeks of gestation, is marked by significant fetal growth and uterine expansion, leading to increased mechanical and physiological stress on the maternal body. Discomforts in this period, including leg cramps, varicose veins, hemorrhoids, edema, dyspnea, and Braxton Hicks contractions, arise from hormonal influences, increased venous pressure, and compression of maternal structures by the enlarging uterus. Nurses must assess these symptoms meticulously, provide targeted interventions, and educate patients to differentiate normal discomforts from potential complications.
1.1 Leg Cramps
Leg cramps, particularly nocturnal, affect approximately 30-50% of pregnant women in the third trimester, causing painful, involuntary muscle contractions, primarily in the calves.
- Physiological Mechanisms:
- Increased maternal weight and altered gait place additional strain on leg muscles, leading to fatigue and cramping.
- Reduced venous return due to uterine compression of pelvic veins causes fluid shifts, contributing to muscle irritability.
- Electrolyte imbalances, such as decreased magnesium or calcium levels, may exacerbate muscle spasms.
- Decreased circulation in the lower extremities, compounded by prolonged standing or sitting, increases cramp frequency.
- Assessment:
- Evaluate the frequency, duration, and severity of leg cramps, noting if they disrupt sleep or daily activities.
- Assess for contributing factors, such as dehydration, inadequate calcium/magnesium intake, or prolonged immobility.
- Screen for signs of deep vein thrombosis (DVT), such as unilateral swelling, redness, or warmth, which requires immediate referral.
- Nursing Interventions:
- Recommend dorsiflexion of the foot (pointing toes toward the head) during a cramp to relieve muscle tension.
- Encourage regular stretching exercises, such as calf stretches, to improve muscle flexibility and circulation.
- Advise adequate hydration and a diet rich in calcium (e.g., dairy) and magnesium (e.g., nuts, leafy greens).
- Suggest wearing supportive footwear and avoiding prolonged standing or sitting to enhance venous return.
- Promote gentle massage or warm compresses to relax affected muscles post-cramp.
- Pharmacological Considerations:
- Magnesium or calcium supplements may be prescribed under medical guidance if dietary intake is insufficient.
- Analgesics are generally not required, as cramps are transient and respond to non-pharmacological measures.
Nursing Insights: Nurses must differentiate leg cramps from DVT by assessing for unilateral symptoms or persistent pain, as DVT poses significant maternal risks, including pulmonary embolism. Patient education on immediate cramp relief techniques, such as dorsiflexion, empowers women to manage symptoms effectively, improving sleep quality and mobility.
1.2 Varicose Veins
Varicose veins, characterized by dilated, tortuous veins in the lower extremities, affect 20-40% of pregnant women in the third trimester due to increased venous pressure and hormonal changes.

- Physiological Mechanisms:
- Progesterone-mediated relaxation of venous smooth muscle reduces vascular tone, leading to venous dilation.
- Uterine compression of pelvic veins impairs venous return, increasing pressure in the lower extremities.
- Increased blood volume in pregnancy heightens venous distension, exacerbating varicosities.
- Genetic predisposition and prolonged standing further contribute to varicose vein development.
- Assessment:
- Inspect lower extremities for visible dilated veins, noting size, location, and associated discomfort.
- Assess for symptoms such as aching, heaviness, or itching in the affected areas.
- Evaluate for complications, such as superficial thrombophlebitis, indicated by localized redness or tenderness.
- Nursing Interventions:
- Recommend wearing graduated compression stockings to improve venous return and reduce swelling.
- Advise elevating legs above heart level when resting to decrease venous pressure.
- Encourage regular physical activity, such as walking, to promote circulation and prevent venous stasis.
- Educate patients to avoid crossing legs or wearing restrictive clothing that impairs circulation.
- Reassure patients that varicose veins often improve postpartum as hormonal and mechanical factors resolve.
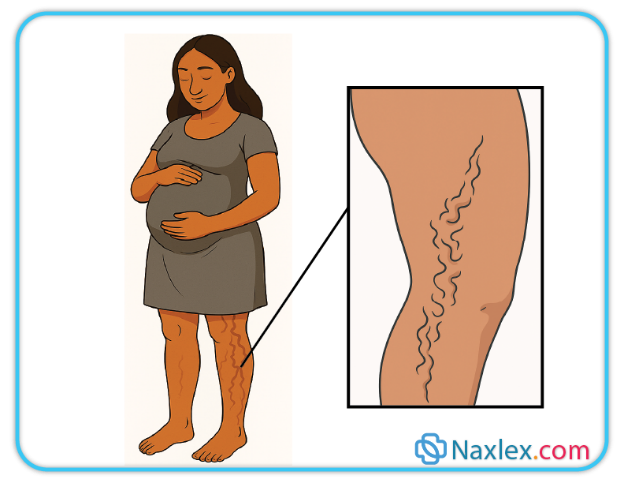
Nursing Insights: Nurses should monitor for signs of thrombophlebitis or DVT in patients with varicose veins, as pregnancy increases thrombotic risk. Educating patients on the use of compression stockings and leg elevation is critical to reducing discomfort and preventing progression of venous insufficiency.
1.3 Hemorrhoids
Hemorrhoids, swollen veins in the rectal or anal region, are reported by 25-35% of pregnant women in the third trimester, often exacerbated by constipation and increased venous pressure.
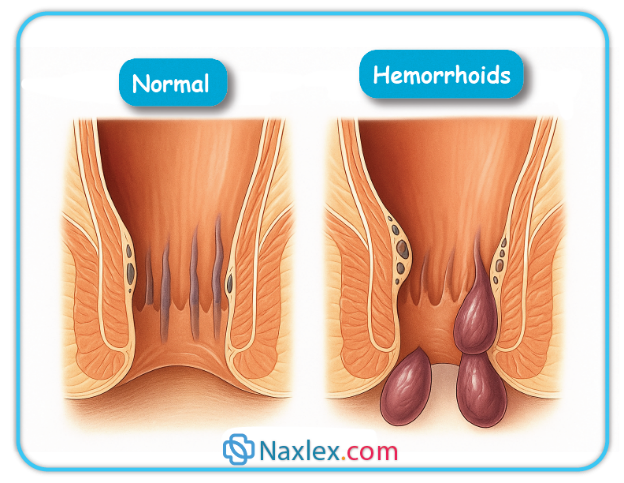
- Physiological Mechanisms:
- Increased intra-abdominal pressure from the enlarging uterus compresses pelvic veins, impairing venous return and causing hemorrhoidal engorgement.
- Progesterone-induced relaxation of venous smooth muscle contributes to venous dilation in the rectal area.
- Chronic constipation and straining during bowel movements increase pressure on rectal veins, promoting hemorrhoid formation.
- Increased blood volume in pregnancy exacerbates venous distension, worsening hemorrhoidal symptoms.
- Assessment:
- Assess for symptoms, including rectal pain, itching, bleeding during bowel movements, or a palpable mass.
- Evaluate bowel habits to identify constipation as a contributing factor.
- Screen for complications, such as thrombosis or severe bleeding, which require medical evaluation.
- Nursing Interventions:
- Recommend warm sitz baths for 10-15 minutes several times daily to reduce inflammation and pain.
- Advise increasing dietary fiber and fluid intake to prevent constipation and soften stools.
- Suggest topical over-the-counter hemorrhoid creams (e.g., witch hazel) under medical guidance to alleviate discomfort.
- Educate on proper perineal hygiene to prevent infection or irritation.
- Encourage side-lying positions to reduce pelvic pressure and improve venous return.
- Pharmacological Considerations:
- Topical hydrocortisone creams may be prescribed for severe inflammation but require medical oversight.
- Stool softeners, such as docusate sodium, are safe to prevent straining and reduce hemorrhoid exacerbation.
Nursing Insights: Nurses must educate patients on preventing constipation to reduce hemorrhoid risk, as straining significantly worsens symptoms. Monitoring for excessive bleeding or pain is crucial, as these may indicate thrombosed hemorrhoids requiring surgical intervention. Empathetic care is essential, as hemorrhoids can cause significant embarrassment and discomfort.
1.4 Edema
Dependent edema, characterized by swelling in the lower extremities, affects up to 80% of pregnant women in the third trimester due to increased venous pressure and fluid retention.

- Physiological Mechanisms:
- Uterine compression of pelvic veins increases venous pressure, impairing fluid return from the lower extremities.
- Increased blood volume and sodium retention elevate interstitial fluid, contributing to edema.
- Decreased colloid osmotic pressure due to hemodilution promotes fluid leakage into tissues.
- Prolonged standing or sitting exacerbates fluid accumulation in dependent areas.
- Assessment:
- Assess the extent and location of edema, typically in the ankles and feet, using a grading scale (1+ to 4+).
- Differentiate physiological edema from pathological edema (e.g., preeclampsia) by checking for sudden onset, facial swelling, or associated hypertension.
- Evaluate for symptoms such as pain or skin tightness, which may indicate severe edema or complications.
- Nursing Interventions:
- Recommend elevating legs above heart level when resting to promote venous return and reduce swelling.
- Advise wearing compression stockings to support venous circulation and prevent fluid accumulation.
- Encourage regular physical activity, such as walking, to enhance circulation and reduce stasis.
- Educate on maintaining adequate hydration to support renal function and prevent excessive sodium retention.
- Reassure patients that physiological edema typically resolves postpartum.

Nursing Insights: Nurses must differentiate physiological edema from preeclampsia by assessing for sudden, generalized swelling, headache, or visual changes. Patient education on leg elevation and compression stockings is critical to managing edema and improving comfort. Monitoring for skin integrity is also essential, as severe edema can lead to skin breakdown.
1.5 Dyspnea
Dyspnea, or shortness of breath, is reported by 60-70% of pregnant women in the third trimester due to mechanical and physiological changes affecting respiratory function.
- Physiological Mechanisms:
- Elevation of the diaphragm by the enlarging uterus reduces lung capacity and functional residual volume.
- Increased oxygen consumption and maternal metabolic rate heighten respiratory demand.
- Progesterone stimulates the respiratory center, increasing tidal volume and respiratory rate, which may be perceived as dyspnea.
- Mild physiological anemia reduces oxygen-carrying capacity, contributing to breathlessness.
- Assessment:
- Assess the severity, timing, and triggers of dyspnea, noting if it occurs at rest or with exertion.
- Monitor respiratory rate, oxygen saturation, and lung sounds to rule out pulmonary pathology.
- Screen for associated symptoms, such as chest pain or cyanosis, which may indicate serious conditions like pulmonary embolism.
- Nursing Interventions:
- Educate patients to maintain upright or semi-Fowler’s position to optimize lung expansion.
- Recommend paced breathing techniques to manage breathlessness during activity.
- Encourage light physical activity to improve cardiovascular fitness and respiratory efficiency.
- Reassure patients that dyspnea is often physiological and improves postpartum as the uterus descends.
- Advise avoiding overexertion and resting as needed to conserve energy.
Nursing Insights: Nurses must differentiate physiological dyspnea from pathological causes, such as pulmonary edema or embolism, by assessing for sudden onset or associated symptoms like chest pain. Patient reassurance and education on positioning are key to alleviating anxiety and improving respiratory comfort.
1.6 Braxton Hicks Contractions
Braxton Hicks contractions, irregular and often painless uterine contractions, occur in 50-60% of pregnant women in the third trimester, preparing the uterus for labor.

- Physiological Mechanisms:
- Increased uterine irritability due to stretching from fetal growth triggers sporadic contractions.
- Oxytocin sensitivity increases in the third trimester, contributing to uterine activity.
- Dehydration or physical activity may exacerbate the frequency or intensity of contractions.
- Unlike true labor, Braxton Hicks contractions do not cause cervical dilation or effacement.
- Assessment:
- Assess the frequency, duration, and intensity of contractions, noting if they are regular or painful.
- Differentiate Braxton Hicks from true labor by monitoring for cervical change or rupture of membranes.
- Evaluate hydration status, as dehydration can increase contraction frequency.
- Nursing Interventions:
- Educate patients to change positions, rest, or walk to alleviate contractions, as they often resolve with activity modification.
- Encourage adequate hydration to reduce uterine irritability.
- Reassure patients that Braxton Hicks contractions are normal and do not indicate labor onset.
- Advise monitoring for signs of true labor, such as regular, intensifying contractions or vaginal bleeding.
Nursing Insights: Nurses must teach patients to differentiate Braxton Hicks contractions from true labor by assessing contraction patterns and associated symptoms. Prompt reporting of regular, painful contractions or fluid leakage is critical to ensure timely evaluation for preterm labor.
Summary
The discomforts of pregnancy are primarily driven by hormonal, anatomical, and physiological changes that occur across the first, second, and third trimesters. In the first trimester, nausea and vomiting, fatigue, breast tenderness, and urinary frequency result from elevated levels of human chorionic gonadotropin (hCG), progesterone, and estrogen, coupled with early uterine growth. These symptoms often subside by the second trimester, where heartburn, constipation, and back pain emerge due to progesterone-mediated smooth muscle relaxation, increased intra-abdominal pressure, and biomechanical shifts such as altered center of gravity. In the third trimester, leg cramps, varicose veins, hemorrhoids, edema, dyspnea, and Braxton Hicks contractions arise from uterine compression, increased venous pressure, and heightened metabolic demands. Nurses play a pivotal role in assessing these discomforts, differentiating them from pathological conditions, and implementing evidence-based interventions to promote maternal comfort. Non-pharmacological strategies, such as dietary modifications, positional changes, and light physical activity, are prioritized to alleviate symptoms, while pharmacological options like antacids or stool softeners are used cautiously under medical guidance. Patient education is critical to empower women to manage discomforts and recognize warning signs, ensuring optimal maternal and fetal outcomes.
Nursing Insights: Nurses must integrate comprehensive assessment, empathetic care, and patient education to address pregnancy discomforts effectively. By understanding the physiological basis of each symptom, nurses can tailor interventions to individual patient needs, monitor for complications, and provide reassurance to reduce anxiety and enhance quality of life.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Discomforts of Pregnancy
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


