Please set your exam date
Healthcare Delivery Systems
Study Questions
Practice Exercise 1
After teaching a class about the various healthcare agencies and services, the instructor determines that the teaching was successful when the class identifies which of the following as a government agency?
Explanation
Healthcare agencies can be classified as private, nonprofit, for-profit, or government-run. Knowing which agencies are government-operated helps nurses understand funding sources, accountability, and the scope of services.
Rationale for correct answers:
B. Public Health Service: The U.S. Public Health Service is a federal government agency that provides leadership in public health and disease prevention.
Rationale for incorrect answers:
A. Alcoholics Anonymous: AA is a voluntary, private nonprofit organization, not a government agency.
C. Rural health center: While these centers may receive government funding, they are often privately operated or nonprofit organizations.
D. Ambulatory care center: These are typically privately owned, offering outpatient services.
A caregiver asks a nurse to explain respite care. How would the nurse respond?
Explanation
Respite care is designed to support family or informal caregivers by giving them temporary relief from caregiving duties, helping prevent burnout and improving the quality of care for the patient.
Rationale for correct answers:
A. “A service that allows time away for caregivers” This definition matches respite care’s purpose: temporary relief for caregivers.
Rationale for incorrect answers:
B. “A special service for the terminally ill and their family” This describes hospice care.
C. “Direct care provided to individuals in nursing homes” This could describe long-term or skilled nursing care, not respite services specifically.
D. “Living units for people without regular shelter” This refers to homeless shelters, unrelated to respite care.
Take home points:
- Respite care is temporary relief for caregivers, often in home or facility settings.
- It helps reduce caregiver stress and sustain long-term caregiving capacity
Which healthcare provider is a major source of health assessment and health education for children?
Explanation
Health assessment and education for children are essential for promoting wellness, detecting problems early, and establishing lifelong healthy habits. The provider’s role depends on accessibility, familiarity, and trust within the child’s daily environment.
Rationale for correct answers:
D. School nurse: Provides ongoing assessments, health screenings, and education directly where children spend much of their time.
Rationale for incorrect answers:
A. Hospital emergency department: EDs treat acute issues, not ongoing assessment or health education.
B. Community center: Can host programs, but not the primary or most consistent source of children’s health education.
C. Nurse practitioner: Plays a strong role in pediatric clinics but is not as consistently present in children’s daily environment as a school nurse.
Take home points:
- School nurses are key in routine health assessment and education for children.
- Integrating health services into daily school life improves prevention and early detection.
When reviewing information about the growth of healthcare services, which area would the nurse expect to find as the most rapidly growing area?
Explanation
Healthcare delivery has shifted significantly toward community and home-based models due to rising costs, technology improvements, and the desire to keep patients in familiar environments. Nurses need to be aware of trends to prepare for evolving practice demands.
Rationale for correct answers:
B. Home care: Advances in medical technology and insurance coverage have expanded home health services, making it the fastest-growing sector.
Rationale for incorrect answers:
A. Hospitals: Hospitals remain central but are not the fastest-growing area; inpatient admissions have declined in many places.
B. Nursing homes: While essential for long-term care, growth has been slower compared to home-based services.
D. Parish nursing: Parish nursing is a niche, community-based specialty and not the fastest-growing area overall.
Take home points:
- Home care is expanding rapidly due to patient preference and cost-effectiveness.
- Nurses should develop community and home health skills to meet this demand.
Which type of healthcare facility employs the largest percentage of RNs?
Explanation
Different healthcare settings employ varying numbers of nurses, but hospitals remain the largest employer of registered nurses due to the scope, complexity, and volume of patient care needs.
Rationale for correct answers:
C. Hospitals employ the majority of RNs due to 24/7 care demands and specialized services.
Rationale for incorrect answers:
A. Ambulatory care: Growing in size but does not surpass hospitals in RN employment.
B. Long-term care: Employs many nurses, especially LPNs/LVNs, but fewer RNs compared to hospitals.
D. Physician offices: These settings typically employ more medical assistants and fewer RNs.
Take home points:
- Hospitals remain the largest RN employers due to high-acuity care and staffing needs.
- Ambulatory and community care roles are growing but still smaller in RN workforce share.
A nurse is providing restorative care to a patient following an extended hospitalization for an acute illness. Which of the following is the most appropriate outcome for this patient’s restorative care?
Explanation
Restorative care helps patients regain maximum functional status and independence following illness or injury. Outcomes should be measurable, functional, and directly related to improving the patient’s daily living abilities
Rationale for correct answers:
A.Patient will be able to walk 200 feet without shortness of breath: This is a functional, measurable goal aimed at restoring mobility and endurance after illness.
Rationale for incorrect answers:
B. Wound will heal without signs of infection: This is an acute care outcome related to recovery, not a long-term functional restoration goal.
C. Patient will express concerns related to return to home: This is an emotional or psychosocial outcome, not a functional restorative goal.
D. Patient will identify strategies to improve sleep habits: This is health promotion but not directly tied to physical function restoration.
Take home points:
- Restorative care goals should focus on regaining independence and improving physical function.
- Measurable, specific outcomes help track functional progress over time.
Which of the following are examples of a nurse participating in primary care activities? Select all that apply
Explanation
Primary care focuses on health promotion, disease prevention, and early intervention. It is often the first point of contact for individuals in the healthcare system and includes patient education, screenings, and preventive services.
Rationale for correct answers:
A. Providing prenatal teaching on nutrition to a pregnant woman during the first trimester: This is preventive care, promoting maternal and fetal health early in pregnancy.
B. Assessing the nutritional status of older adults who come to the community center for lunch: Early assessment in a community setting helps identify risks before illness develops.
E. Teaching a class to parents at the local elementary school about the importance of immunizations: Immunization education is a primary prevention activity.
Rationale for incorrect answers:
C. Working with patients in a cardiac rehabilitation program: This is tertiary care, focusing on restoring health after a serious illness.
D. Providing home wound care to a patient: This is secondary or tertiary care, aimed at treatment and recovery rather than prevention.
Take home points:
- Primary care activities are preventive, educational, and community-focused.
- Differentiating between primary, secondary, and tertiary care is essential for correct nursing care planning.
Practice Exercise 2
A nurse is developing a presentation for a local community group about the knowledgeable healthcare consumer. Which technology would the nurse include as having the greatest effect on this area?
Explanation
Technology has transformed healthcare by increasing patient access to medical information, enabling remote services, and supporting informed decision-making. The most impactful technology in creating knowledgeable healthcare consumers is the one that allows broad, interactive access to credible resources.
Rationale for correct answers:
B. Computers, especially with internet access, allow consumers to research conditions, compare treatment options, and access online health portals, empowering informed healthcare decisions.
Rationale for incorrect answers:
A.Television: While health education programs exist, television is passive and limited compared to interactive technology.
C. Cell phones: While mobile health apps are valuable, their content and function often depend on computer-based internet platforms for depth of information.
D. Global positioning system (GPS) devices: GPS technology is not directly related to healthcare consumer education, though it can aid in locating facilities.
Take home points:
- Computers with internet access have revolutionized patient knowledge by providing immediate access to health resources.
- Digital literacy is now essential for effective healthcare navigation.
Private insurance most often is called a third-party payer, indicating which of the following?
Explanation
In healthcare financing, a third-party payer is an entity (often an insurance company) that pays for healthcare services on behalf of the insured person. Understanding this concept helps patients know their responsibilities, such as premiums, deductibles, and coverage limits.
Rationale for correct answers:
D. You pay a monthly premium, and the insurance company pays the bills: This is the essence of third-party payer systems - the insured pays premiums, and the insurance company pays the provider for covered services.
Rationale for incorrect answers:
A.You pay no monthly premium, paying for all healthcare costs yourself: This describes self-pay, not third-party payer insurance.
B. You belong to a preferred provider organization: A PPO is a type of insurance network, but the term "third-party payer" refers to the financial role of the insurer, not the network type.
C. You are at risk if your healthcare provider is not a part of the plan: While true for some insurance plans like HMOs or PPOs, this is not the definition of “third-party payer.”
Take home points:
- A third-party payer is an entity that reimburses healthcare costs for the insured person.
- Patients are still responsible for premiums, deductibles, and uncovered services.
Your newly employed friend is a part of the company’s HMO. You interpret that to mean the friend
Explanation
HMOs are a type of managed care organization where members receive services from a set network of providers. They are designed to lower costs and improve coordination but have specific restrictions on provider choice.
Rationale for correct answers:
C. Receives all healthcare from providers within the organization: HMOs contract with specific providers; members must receive most care within the network.
Rationale for incorrect answers:
A. Can have healthcare services from a provider of his choice: HMOs require members to use network providers except in emergencies.
B. Will be unable to have emergency care: Emergency care is covered, but usually requires follow-up within the HMO system.
D. Must pay an additional monthly premium: Premiums are part of the plan but are not "additional" beyond the agreed amount; some HMOs may even have lower premiums.
Take home points:
- HMO members must stay within the network for most services, with exceptions for emergencies.
- HMOs emphasize preventive care and cost control through contracted providers.
Which purpose best describes managed care as a framework for healthcare?
Explanation
Managed care is a healthcare delivery framework developed to address rising costs while ensuring quality. It involves structured systems for controlling spending and coordinating care to improve patient outcomes.
Rationale for correct answers:
A. A design to control the cost of care while maintaining the quality of care: This is the primary goal of managed care systems.
Rationale for incorrect answers:
B. Care coordination to maximize positive outcomes to contain costs: While related, this is more a description of case management, which is a component of managed care.
C. The delivery of services from initial contact through ongoing care: This describes continuity of care, which is a broader concept and not exclusive to managed care.
D. Based on a philosophy of ensuring death in comfort and dignity: This describes hospice care.
Take home points:
- Managed care focuses on cost control and quality maintenance through structured provider networks.
- It uses preventive services and coordinated care to reduce unnecessary expenses.
A nurse is preparing to discharge a 72-year-old client who was admitted for heart failure management. Which of the following are common barriers to effective discharge planning? Select all that apply
Explanation
Effective discharge planning is critical for ensuring that clients transition safely from the hospital to home or another care setting. However, this process can be disrupted by multiple barriers. Identifying and addressing these obstacles helps reduce hospital readmissions, improves health outcomes, and enhances patient satisfaction.
Rationale for correct answers:
A. Ineffective communication among providers: Poor communication between nurses, physicians, therapists, case managers, and other providers can lead to conflicting instructions, missed referrals, or incomplete discharge plans.
B. Lack of role clarity among health care team members: When team members are unsure of their responsibilities, tasks like medication reconciliation, education, and follow-up scheduling may be duplicated or missed, leading to fragmented discharge planning.
Rationale for incorrect answer:
C. Number of hospital beds to manage patient volume: While bed availability may affect admission and throughput, it is not a direct barrier to discharge planning. Discharge planning is more affected by the quality of coordination than by infrastructure like bed count.
D. Client’s long-term disabilities: Though long-term disabilities may require extensive planning, including home modifications, caregiver training, or access to outpatient services they are additional factors to consider, not barriers to discharge planning.
E. The client’s cultural background: Cultural factors can influence health beliefs, language comprehension, family involvement, and care preferences but are not traditional barriers to discharge planning.
Take home points:
- Effective discharge planning requires strong communication and clearly defined roles within the interdisciplinary team.
- Nurses must consider individual patient needs, including disabilities and cultural factors, to ensure a smooth and safe transition from hospital to home or rehab.
A nurse is educating student nurses about levels of prevention. Which activity does the nurse perform while providing tertiary care? Select all that apply
Explanation
Tertiary prevention focuses on managing and reducing complications of established diseases, restoring function, and improving quality of life for individuals with chronic conditions or disabilities.
Rationale for correct answers:
C. Inserting an indwelling catheter for a client on a medical-surgical unit: This manages complications of an existing condition- such as urinary retention, neurogenic bladder, or immobility due to a stroke or surgery. This intervention supports recovery and prevents secondary complications.
D. Performing endotracheal suctioning for a patient on a ventilator in the medical ICU: This is a highly specialized, supportive procedure for clients with serious health conditions. It helps prevent complications in patients already experiencing critical illness.
E. Working with patients in a cardiac rehabilitation program: Cardiac rehab is a classic example of tertiary prevention, aimed at maximizing recovery, restoring function, and preventing further cardiovascular events in clients after a heart attack or cardiac surgery.
Rationale for incorrect answers:
A. Conducting blood pressure screenings at a local food bank: This is an example of secondary prevention, which focuses on early detection and intervention to identify and manage diseases in the early stages.
B. Administering influenza vaccines for older adults at the local senior center: This is primary prevention, aimed at preventing disease before it occurs by promoting immunity and protecting against infectious illness.
Take home points:
- Tertiary prevention focuses on restoring health, managing chronic illness, and preventing complications.
- Nurses must distinguish between preventive screenings (secondary), vaccinations (primary), and treatment/supportive care (tertiary) to deliver appropriately targeted interventions.
A client is seeking to control health care costs for both preventive and illness care. Although no system guarantees exact out-of-pocket expenditures, the most prepaid and predictable client contribution would be seen with
Explanation
With rising health care costs, clients increasingly look for insurance options that offer predictability and affordability. While no plan can completely eliminate out-of-pocket expenses, some systems-particularly those based on prepaid models-allow clients to better manage and forecast their health care spending.
Rationale for correct answer:
D. A health maintenance organization (HMO): An HMO is a managed care plan that emphasizes prepaid, fixed payments (usually monthly premiums), which cover a broad range of services. HMOs provide the most predictable and limited out-of-pocket expenses compared to other models.
Rationale for incorrect answers:
A. Medicare: While Medicare offers comprehensive coverage for those over 65 and certain disabled individuals, it involves variable costs including premiums, deductibles, copays, and coinsurance.
B. An individual fee-for-service insurance: This model allows clients to see any provider and pay per service rendered, but it generally results in higher and less predictable out-of-pocket expenses, including deductibles and coinsurance.
C. A preferred provider organization (PPO): PPOs offer more flexibility than HMOs by allowing clients to see providers both in and out of the network without referrals, but this also means higher premiums and more variable cost-sharing.
Take home points:
- HMOs provide the most prepaid and predictable cost structure, making them ideal for clients who want to manage health care expenses proactively.
- Nurses should help clients evaluate health care plans based on coverage needs, financial predictability, and access to care.
Comprehensive Questions
A nurse is educating student nurses about levels of prevention. Which of the following is an example of a primary prevention activity?
Explanation
Primary prevention aims to prevent disease or injury before it occurs by reducing risk factors and enhancing resistance.
Rationale for correct answer:
C. Nutrition counseling for young adults with a strong family history of high cholesterol: This is primary prevention because it seeks to prevent the onset of hyperlipidemia and cardiovascular disease in people who are currently healthy but at risk due to family history.
Rationale for incorrect answers:
A. Antibiotic treatment of a suspected urinary tract infection: This is an example of secondary prevention, as it involves early treatment of a disease that has already developed to halt progression or complications. The goal is to cure or manage the infection.
B. Occupational therapy to assist a client in adapting his or her home environment following a stroke: This is tertiary prevention, aimed at helping the client recover and live optimally after a serious health event. It seeks to reduce disability and enhance function after the disease has occurred.
D. Removal of tonsils for a client with recurrent tonsillitis: This is also tertiary prevention, because it addresses a chronic or recurring condition and is intended to reduce further complications or suffering.
Take home points:
- Primary prevention focuses on health promotion and risk reduction before disease occurs.
- Distinguishing between primary, secondary, and tertiary prevention helps nurses select the most appropriate intervention based on the client’s health status and risk profile.
A community health nurse is providing orientation to a group of newly hired nursing staff. Which of the following statements is true regarding types of health care agencies?
Explanation
Health care services are delivered through a spectrum of facilities including hospitals, public health departments, outpatient clinics, and long-term care institutions. Each has a unique role in the health system based on the level of care provided, the population served, and the source of funding.
Rationale for correct answer:
B. Public health agencies are funded by governments to investigate and provide health programs. Public health agencies are primarily government-funded. Their focus is on population-level health, such as disease surveillance, health education, immunization programs, and sanitation initiatives.
Rationale for incorrect answers:
A. Hospitals provide only acute, inpatient services. While hospitals are well known for acute, inpatient care, they often provide outpatient services such as same-day surgery, diagnostic imaging, and physical therapy.
C. Surgery can only be performed inside a hospital setting. Many minor to moderate surgeries are safely performed in ambulatory surgery centers (ASCs) and outpatient clinics, which are licensed and equipped for such procedures without requiring hospital admission.
D. Skilled nursing, extended care, and long-term care facilities provide care for older adults whose insurance no longer covers hospital stays. These facilities provide care based on medical necessity, functional status, and rehabilitation needs, not just when insurance runs out.
Take home points:
- Public health agencies play a vital role in disease prevention, health promotion, and population surveillance.
- Nurses must understand the functions of different settings to properly guide clients and make referrals.
In most cases, clients must have a primary care provider in order to receive health insurance benefits. If a client is in need of a primary care provider, it is most appropriate for the nurse to recommend which of the following?
Explanation
Many health insurance plans, especially managed care plans like HMOs, require clients to have a designated primary care provider (PCP) to coordinate their care, authorize referrals, and manage health services. A PCP serves as the first point of contact in the health system and plays a key role in preventive care, diagnosis, and treatment of common conditions.
Rationale for correct answer:
A. A family practice physician is trained to provide comprehensive primary care to individuals of all ages. They diagnose and treat a wide range of acute and chronic conditions, provide health education, perform preventive screenings, and make referrals to specialists.
Rationale for incorrect answers:
B. A physical therapist is a rehabilitation specialist who helps clients improve physical function, mobility, and strength. While important in the care team, they do not diagnose, prescribe, or coordinate overall medical care, and are not recognized as PCPs.
C. A case manager/discharge planner typically works within hospitals or health systems to coordinate care, manage transitions, and arrange services after discharge. They are not licensed to serve as a client’s primary care provider.
D. While pharmacists are medication experts and play a critical role in client safety and education, they do not provide comprehensive medical care or serve as the main access point for health services like PCPs do.
Take home points:
- A primary care provider is essential in managing and coordinating a client’s overall health care.
- Nurses should guide clients to appropriate health professionals based on scope of practice.
- Only licensed providers like family physicians, internists, pediatricians, or nurse practitioners can fulfill the PCP role.
A nurse is aware that the most significant method for reducing the ongoing increase in the cost of health care in the United States includes controlling which of the following?
Explanation
Several factors contribute to these escalating costs, including administrative expenses, drug pricing, use of advanced technology, and lack of access to affordable preventive care. When individuals lack health insurance or have inadequate coverage, they often delay care or seek care through emergency departments, where treatment is more expensive and typically occurs after conditions have worsened.
Rationale for correct answer:
B. Numbers of uninsured and underinsured persons: Increasing insurance coverage can help shift care to more cost-effective preventive services and early interventions, ultimately reducing the financial burden on the health system.
Rationale for incorrect answers:
A. Number of children according to the family’s income: While population growth affects resource allocation, family planning based on income is a sensitive social and ethical issue, and not a central strategy for health care cost control.
C. Number of physicians and nurses nationwide: Increasing or decreasing the number of health care professionals does not directly control costs. In fact, shortages of providers can increase costs by causing delays in care and reducing access.
D. Competition among drug and medical equipment manufacturers: While competition can reduce costs in some markets, it is not the most significant factor. The lack of regulation in pricing and the influence of patents and monopolies often limit the effectiveness of competition.
Take home points:
- Improving access to health insurance is one of the most impactful strategies for reducing long-term health care costs.
- It promotes early, preventive care and reduces emergency care dependency.
A client asks the nurse, ‘‘Exactly what is an HMO?’’ The nurse’s response should include which of the following information? Select all that apply
Explanation
A Health Maintenance Organization (HMO) is a type of managed care insurance plan that delivers health care services for a prepaid, fixed fee. HMOs are designed to streamline care delivery, reduce unnecessary health care utilization, and promote cost-effectiveness by focusing on prevention, coordination, and efficiency.
Rationale for correct answers:
B. Many HMOs provide a continuum of care to individuals and families. HMOs typically offer comprehensive services, including preventive care, acute care, specialty services, and rehabilitation, ensuring a continuum of care under one system.
C. HMOs were established to control the costs of health care delivery. A major goal of HMOs is cost containment by promoting efficiency, minimizing unnecessary services, and requiring preauthorization and referrals to manage care effectively.
6. HMOs were intended to emphasize prevention rather than treatment of chronic conditions. HMOs emphasize preventive care such as immunizations, screenings, and health education to detect and manage health conditions before they become costly or chronic.
Rationale for incorrect answers:
A. HMOs are groups of federally financed insurance companies. HMOs are often private organizations (some are nonprofit, some for-profit) that may contract with Medicare or Medicaid, but they are not operated or funded by the federal government.
D. An HMO provides unlimited services to its members. HMOs do not provide unlimited services. Services are limited to what is covered under the plan, often requiring approval and network restrictions, and there may be caps or exclusions.
E. The HMO was developed as a type of fee-for-service reimbursement system. HMOs operate on a prepaid model, not fee-for-service. Providers are paid a fixed amount per enrollee, which incentivizes cost control and emphasizes preventive care over volume-based billing.
Take home points:
HMOs are designed to control health care costs by:
- using a prepaid model
- requiring clients to work within a network of providers coordinated by a primary care provider.
Preventive care and early intervention are foundational principles of HMO plans, helping to reduce long-term health care costs and improve client outcomes.
The nurse is aware that when working with a person from a vulnerable population, it is important to do which of the following?
Explanation
Vulnerable populations-such as individuals experiencing poverty, homelessness, mental illness, or those from minority ethnic or cultural backgrounds-face increased health risks and barriers to care. Nurses must provide culturally competent and patient-centered care.
Rationale for correct answers:
B. Learn about the person’s specific cultural practices. Learning about a client’s specific cultural beliefs and practices is a cornerstone of culturally competent care. This is especially important when working with vulnerable populations who may have experienced systemic inequities.
Rationale for incorrect answers:
A. Perform the nursing assessment as quickly as possible so the individual can return to the community. Rushing the assessment can lead to missed information, decreased trust, and a perception of insensitivity. Vulnerable clients often need more time and careful listening to feel safe and understood.
C. Focus only on the client’s verbal communication. Many clients from diverse cultural backgrounds, may rely heavily on nonverbal cues such as facial expressions, gestures, and body language. Focusing only on verbal communication can result in missed context and misinterpretation.
D. Refer the client to another nurse who is from the same cultural group as the client. While matching cultural backgrounds may enhance comfort in some cases, nurses are responsible for developing cultural competence themselves, not shifting care based on cultural similarity.
Take home points:
- Cultural awareness and sensitivity are essential when caring for clients from vulnerable populations.
- Learning about the client’s unique background promotes trust and therapeutic communication.
- Nurses must provide equitable care by developing their own cultural competence rather than relying on others.
The nurse who is working in a rehabilitation facility is providing which level of care?
Explanation
Health care is delivered in a system that includes primary, secondary, and tertiary care, each serving a different purpose in the continuum of care.
Rationale for correct answer:
C. Tertiary: Tertiary care involves specialized, long-term, or rehabilitative care provided after the initial illness or injury has been addressed. Rehabilitation facilities aim to restore optimal function and prevent complications following serious health events.
Rationale for incorrect answers:
A. Primary care focuses on health promotion, disease prevention, and early detection. It is typically provided in outpatient or community settings by general practitioners.
B. Secondary care refers to diagnosis and treatment of acute conditions, usually in hospitals or specialist clinics. This includes surgeries, hospitalizations, and emergency care.
D. Palliative care focuses on relief of symptoms and improving quality of life for clients with serious, chronic, or terminal illness, often without curative intent.
Take home points:
- Tertiary care includes rehabilitation services that focus on restoring health and functional ability after major illness or injury.
- Nurses should understand their role within each level of care to align their interventions with the goals of prevention, treatment, or recovery.
A nurse in a busy medical-surgical unit receives feedback from the hospital's patient satisfaction survey team. Which of the following nursing actions will adversely affect customer satisfaction of hospitalized clients? Select all that apply
Explanation
Patient satisfaction is a key measure of quality in health care and is often used in hospital performance evaluations and reimbursement models. Nursing care plays a major role in shaping patient experience, as nurses are often the primary point of contact during hospitalization.
Rationale for correct answers:
C. Implementing a routine schedule for every client: While routines help with efficiency, applying a one-size-fits-all approach may make clients feel overlooked or dehumanized.
E. Responding to a client’s call light after 15 minutes: Delayed responses to call lights are one of the most common causes of dissatisfaction among hospitalized clients. It may cause feelings of neglect, frustration, or anxiety, especially when clients need assistance for pain, toileting, or repositioning.
Rationale for incorrect answers:
A. Introducing self to client and family: This is a positive behavior that enhances patient satisfaction by building trust, rapport, and communication. It helps clients feel valued and respected.
B. Assessing pain level: Pain assessment is a fundamental nursing responsibility and directly affects client comfort and satisfaction. Consistent, proactive pain management is linked to higher satisfaction scores.
D. Documenting all care provided in a timely manner: Timely documentation is a professional standard that ensures continuity of care, legal compliance, and client safety.
Take home points:
- Delayed responses and impersonal routines are among the leading causes of poor client satisfaction.
- Nurses should strive to be prompt, attentive, and personalized in care delivery.
The school nurse has been following a 9-year-old student who has shown behavioral problems in class. The student acts out and does not follow teacher instructions. The nurse plans to meet with the student’s family to learn more about social determinants of health that might be affecting the student. Which of the following potential social determinants should the nurse assess? Select all that apply
Explanation
Social determinants of health (SDOH) are the non-medical factors that influence health outcomes, including the conditions in which people live, learn, work, and play. When a student exhibits behavioral issues, school nurses should assess underlying environmental, social, and economic factors that may contribute to or exacerbate the problem.
Rationale for correct answers:
B. The level of support parents offer when the student completes homework: Children with limited parental involvement may face academic stress, poor performance, or behavioral issues due to lack of guidance and encouragement.
C. The level of violence in the family’s neighborhood: Living in a high-crime or violent area can increase stress, anxiety, and behavioral issues in children, impacting both mental health and academic engagement.
E. The cultural values about education held by the family: Cultural beliefs and attitudes are part of social and community context, a domain of SDOH. Family views on education can shape a child’s motivation, behavior, and value placed on learning.
Rationale for incorrect answers:
A. The student’s seating placement in the classroom: This is an educational or environmental factor within the classroom, not a social determinant of health. While it may impact behavior or focus, it is not considered part of the broader social factors affecting health.
D. The age at which the child first began having behavioral problems: This is a clinical or developmental detail, not a social determinant. While important in assessment, it relates more to diagnostic timelines than to external social factors influencing health.
Take home points:
- Social determinants of health such as family involvement, neighborhood safety, and cultural attitudes can significantly affect a child’s behavior and school performance.
- Nurses must assess environmental and social factors when evaluating concerns in school-aged children.
A new graduate nurse is attending a forum on health care systems. Which of the following describe characteristics of an integrated health care system? Select all that apply
Explanation
An integrated health care system is designed to improve the quality, coordination, and cost-effectiveness of care across the entire continuum of services, including primary, specialty, acute, and long-term care.
Rationale for correct answers:
A. The focus is holistic: Integrated health systems address the whole person, including physical, emotional, social, and spiritual health. The aim is to improve outcomes and client satisfaction by treating more than just the disease.
C. The system coordinates a continuum of services: A key feature of integrated systems is coordination of services across settings-from preventive care to acute care to rehabilitation and long-term care-ensuring smooth transitions and improved outcomes.
E. Members of the health care team link electronically to use the EHR to share the client’s health care record. Electronic health records (EHRs) enable real-time communication and shared access to patient information among providers, improving coordination and safety in an integrated system.
Rationale for incorrect answers:
B. Participating hospitals follow the same model of health care delivery. While hospitals in an integrated system may collaborate and share resources, they may not necessarily follow the same delivery model. Variations exist based on location, specialization, and community needs.
D. The focus of health care providers is finding a cure for clients. While curing disease is part of care, integrated systems focus more broadly on prevention, chronic disease management, quality of life, and collaborative care, not just finding a cure.
Take home points:
- Integrated health care systems emphasize holistic, coordinated, and continuous care across various health care settings.
- Technology, such as shared electronic health records, plays a crucial role in enabling communication and collaboration within integrated care teams.
A nurse is assigned to care for an 82-year-old client who will be transferred from the hospital to a rehabilitation center. The client and her husband have selected the rehabilitation center closest to their home. The nurse learns that the client will be discharged in 3 days and decides to make the referral on the day of discharge. The nurse reviews the recommendations for physical therapy and applies the information to fall prevention strategies in the hospital. What discharge planning action by the nurse has not been addressed correctly?
Explanation
Discharge planning is a vital component of nursing care that should begin early in the hospitalization and involve collaboration with the client, family, and health care team. It ensures a safe, smooth transition from one level of care to another.
Rationale for correct answer:
B. Timing of referral: The referral should be made as early as possible once discharge needs are identified-not on the day of discharge. Delaying referrals can cause gaps in care coordination, insufficient preparation at the receiving facility, and delayed or unsafe transitions for the client.
Rationale for incorrect answers:
A. Patient and family involvement in referral: The nurse did involve the client and her husband in choosing the rehabilitation facility, which reflects appropriate patient and family engagement in the referral process.
C. Incorporation of referral discipline recommendations into plan of care: The nurse did apply physical therapy recommendations (e.g., for fall prevention), indicating that interdisciplinary input was correctly integrated into the current hospital care plan.
D. Determination of discharge date: The discharge date was already determined as 3 days from now, so that aspect of the discharge planning process was appropriately addressed.
Take home points:
- Timely referrals are essential for safe and effective discharge planning.
- Discharge planning should be interdisciplinary and proactive, involving the client, family, and care team.
A student nurse asks their preceptor what Magnet® status means. Which of the following statements is true regarding Magnet® status recognition for a hospital?
Explanation
Magnet® status is an internationally recognized designation awarded by the American Nurses Credentialing Center (ANCC) to health care organizations that demonstrate excellence in nursing services, innovation in professional nursing practice, and quality patient outcomes.
Rationale for correct answers:
D. Magnet® is a special designation for hospitals that achieve excellence in nursing practice. Magnet® designation is awarded to hospitals that meet high standards in nursing excellence, quality patient care, and innovations in professional nursing practice.
Rationale for incorrect answers:
A. Nursing is run by a Magnet® manager who makes decisions for the nursing units. Magnet® status does not involve a specific “Magnet manager.” Instead, it emphasizes shared governance where nurses at all levels are involved in decisions that affect their practice.
B. Nurses in Magnet® hospitals make all of the decisions on the clinical units. While nurses in Magnet® hospitals are highly involved in shared decision-making, they do not make all decisions independently.
C. Magnet® is a term that is used to describe hospitals that are able to hire the nurses they need. Magnet® status is not about staffing numbers, but rather about nursing quality, leadership, autonomy, and evidence-based practice.
Take home points:
- Magnet® status is a prestigious recognition that signifies excellence in nursing practice, leadership, and patient care quality.
- Hospitals with Magnet® status typically foster shared governance, evidence-based practice, and strong professional development, which benefits both nurses and clients.
Which activity performed by a nurse is related to maintaining competency in nursing practice?
Explanation
Maintaining competency in nursing is a professional responsibility that ensures safe, evidence-based, and high-quality patient care. Competency is developed and sustained through lifelong learning, self-assessment, and participation in professional development activities.
Rationale for correct answers:
D. Attending a review course in preparation for a certification examination: Formal review courses enhance knowledge and skills in a specialty, directly contributing to competency maintenance.
Rationale for incorrect answers:
A.Asking another nurse about how to change the settings on a medication pump: This shows initiative in learning a specific task but does not represent an ongoing or structured activity to maintain competency.
B. Regularly attending unit staff meetings: Staff meetings are important for communication but are not primarily designed to maintain clinical competency.
C. Participating as a member of the professional nursing council: While professional councils promote nursing practice, they focus more on governance and policy-making than on maintaining personal clinical competence.
Take home points:
- Ongoing education and skill refreshers are essential for clinical competency.
- Certification review courses prepare nurses for advanced proficiency in specialized practice areas.
A nurse newly hired at a community hospital learns about intentional hourly rounding during orientation. Which of the following are known evidence-based outcomes from intentional rounding? Select all that apply
Explanation
Intentional hourly rounding is a proactive nursing practice where staff check on patients at scheduled intervals to address needs before they arise. Research shows it improves safety, satisfaction, and efficiency by anticipating and meeting patient needs consistently.
Rationale for correct answers:
B.Improved patient satisfaction: Patients feel more cared for when their needs are met proactively.
C. Reduction in patient falls: Frequent checks allow nurses to address toileting and mobility needs, reducing fall risk.
E.Reduction in patient use of nurse call system: Patients call less often because needs are anticipated and addressed during rounds.
Rationale for incorrect answers:
A.Reduction in nurse staffing requirements: Rounding is not aimed at reducing staff; it is a care quality and safety strategy.
D. Increased costs: In fact, rounding can reduce costs by preventing complications and improving efficiency.
Take home points:
- Hourly rounding improves patient satisfaction, safety, and efficiency.
- Outcomes include fewer falls, fewer call lights, and improved experience.
A group of students are reviewing information about hospitals in preparation for a quiz the next day. Which of the following, if identified by the students as associated with a hospital, demonstrates the need for additional study?
Explanation
Hospitals provide a wide range of services, both inpatient and outpatient, and are central to acute care delivery. Understanding their scope helps differentiate them from community-based or faith-based services
Rationale for correct answers:
D. Parish nursing activities: Parish nursing is typically based in faith communities, not hospitals, although collaboration may occur.
Rationale for incorrect answers:
A. Provision of acute care: Hospitals are designed for managing acute illnesses, injuries, and urgent conditions.
B. Inpatient services: Hospital stays for surgery, medical treatment, or intensive monitoring are core functions.
C. Outpatient services: Many hospitals now offer outpatient clinics, diagnostic services, and same-day procedures.
Take-home points:
- Hospitals deliver acute, inpatient, and outpatient services.
- Parish nursing is community and faith-based, not a hospital core service.
Exams on Healthcare Delivery Systems
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Differentiate health care services based on primary, secondary, and tertiary disease prevention categories.
- Describe the functions and purposes of the health care agencies.
- Identify the roles of various health care professionals.
- Describe the factors that affect health care delivery.
- Describe frameworks for the delivery of nursing care.
- Compare various systems of payment for health care services.
- Summarize the importance of discharge planning.
Introduction
A health care system is the totality of services offered by all health disciplines.
The services provided by a health care system are commonly categorized according to type and level.
Types Of Healthcare Services
Health care services are often described in terms of how they are correlated with levels of disease prevention:
- primary prevention
- secondary prevention
- tertiary prevention
1) Primary Prevention:
Primary prevention programs address areas such as adequate and proper nutrition, weight control and exercise, and stress reduction.
- Health promotion activities emphasize the important role clients play in maintaining their own health and encourage them to maintain the highest level of wellness they can achieve.
- Illness prevention programs may be directed at the client or the community and involve such practices as providing immunizations, smoking cessation campaigns and environmental programs.
2) Secondary prevention:
Involves:
- Early detection of disease: This is accomplished through routine screening of the population and focused screening of those at increased risk of developing certain conditions.
- Diagnosis and treatment of illness.
3) Tertiary prevention:
The goal of tertiary prevention is to help people move to their previous level of health (i.e., to their previous capabilities) or to the highest level they are capable of given their current health status.
Includes:
- Rehabilitative care and Health Restoration emphasizes the importance of assisting clients to function adequately in the physical, mental, social, economic, and vocational areas of their lives.
- Palliative care- providing comfort and treatment for symptoms for people who cannot be returned to health.
Types Of Health Care Agencies And Services
Health care agencies and services in the United States are both varied and numerous.
|
SETTING |
SERVICES PROVIDED |
NURSE’S ROLES/RESPONSIBILITIES |
|
Home health agencies |
Acute and restorative |
Educator • Caregiver • Provides skilled nursing care • Coordinates health promotion activities |
|
Hospices |
Care of individuals with terminal illnesses • Improving the quality of end-of-life (EOL) care |
Caregiver • Counselor • Advocate • Plans and coordinates care • Promotes comfort measures • Provides pain control • Supports grieving families |
|
Outpatient settings (clinics, ambulatory treatment centers) |
Treatment of illness (acute and chronic) • Diagnostic testing • Noncomplex surgical procedures |
Traditional Role: • Checks vital signs • Assists with diagnostic tests • Prepares client for examination Expanded Role: • Provides teaching and counseling • Performs physical examination • In some settings, advanced practice registered nurses (APRNs) are the primary care providers |
|
Hospitals |
Diagnosis and treatment of illnesses • Acute inpatient services • Emergency care • Ambulatory care services • Critical (intensive) care • Rehabilitative care • Surgical interventions • Diagnostic procedures |
•Caregiver • Client educator • Provides ongoing assessment • Coordinates care and collaborates with other health care providers • Maintains client safety • Initiates discharge planning |
|
Extended care (long-term care) facilities (e.g., nursing homes, skilled nursing facilities) |
• Intermediate and long-term care for people with chronic illnesses or those who are unable to care for themselves • Restorative care until client is ready for discharge to home |
Caregiver • Educator • Advocate • Provides teaching and counseling • Plans and coordinates care • Administers medications, treatments, and other therapeutic modalities |
|
Community nursing centers |
Direct access to professional nursing services |
Caregiver • Treats client’s responses to health problems • Promotes health and wellness |
|
Rural primary care hospitals (RPCHs) |
Stabilize clients until they are physiologically able to be transferred to more skilled facilities |
Caregiver • Educator • Advocate • Performs assessments and provides emergency care |
|
Industrial clinics |
Maintain health and safety of workers |
Caregiver • Educator • Coordinates health promotion activities • Provides education for safety • Provides urgent care as needed • Maintains health records • Conducts ongoing screenings • Provides preventive services (e.g., tuberculosis testing) |
|
Schools |
School-based clinics are federally funded providers of physical and mental health services in elementary and secondary schools |
Caregiver • Educator • Advocate • Coordinates health promotion and disease prevention activities • Treats minor illnesses • Provides health education |
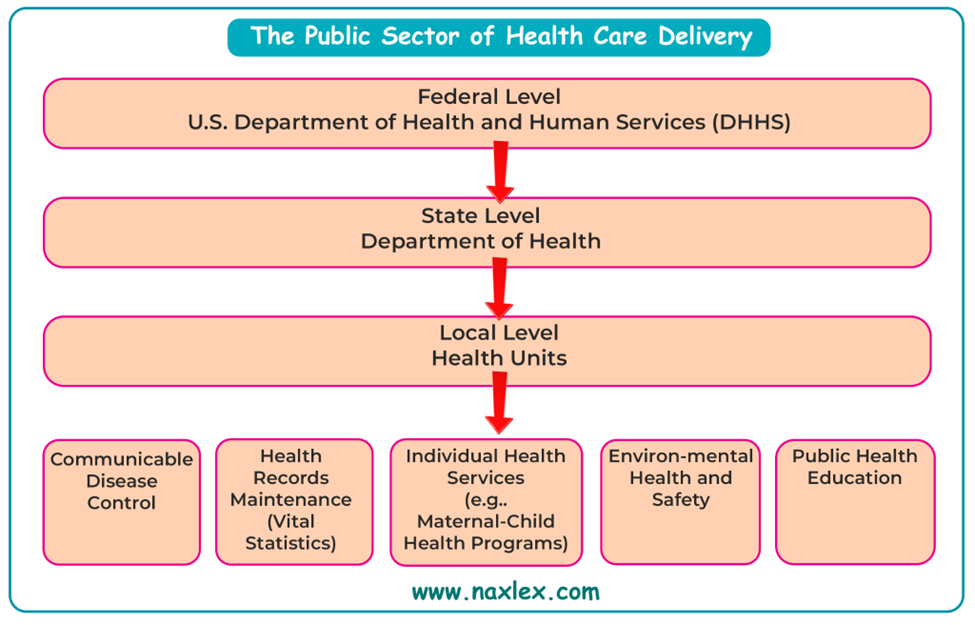
Public health
Government (official) agencies are established at the local, state, and federal levels to provide public health services.
Health agencies at the state, county, or city level vary according to the needs of the area. Their funds, usually generated from taxes, are administered by elected or appointed officials.
The Public Health Service (PHS) of the U.S. Department of Health and Human Services is an official agency at the federal level.
Functions:
- conducting research
- providing training in the health field
- assisting communities in planning and developing health facilities
- assisting states and local communities through financing and provision of trained personnel
Other institutions at the national level:
- National Institutes of Health (NIH)
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- The Centers for Disease Control and Prevention (CDC)
- Food and Drug Administration (FDA)
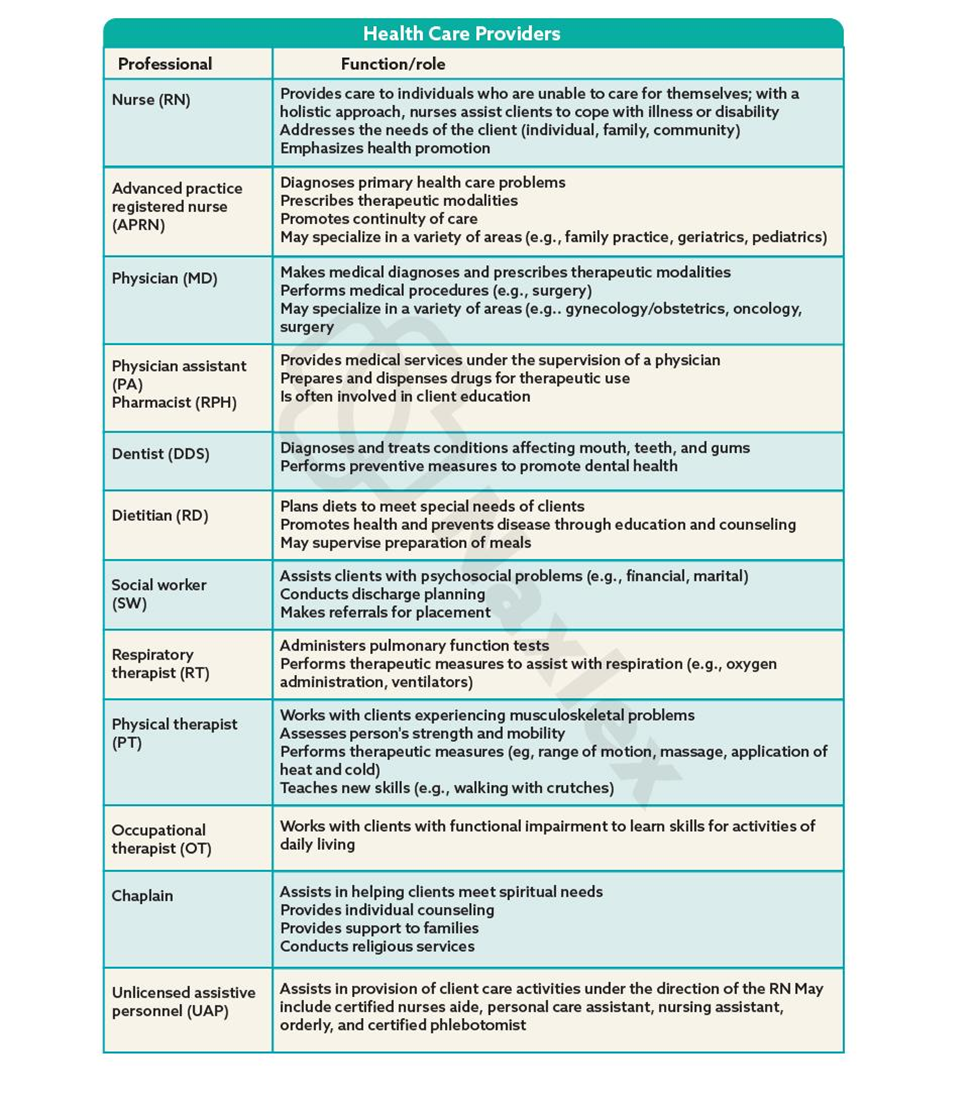
Health Care Providers
Health care services are delivered by a multidisciplinary team.
Because nurses work with other care providers on an ongoing basis, it is necessary to understand the role of each provider.
Nurses coordinate the care provided by the multidisciplinary team.
Factors Affecting Health Care Delivery
A number of factors affect the ability of the health care delivery system to meet the needs of the population.
Include:
- the increasing number of older adults
- advances in knowledge and technology, economics
- increased emphasis on women’s health
- uneven distribution of health services
- access to health insurance
- health care for the homeless and poor
- HIPAA
- demographic changes.
Frameworks For Care
A number of configurations for the delivery of nursing care support continuity of care and cost effectiveness. Some configurations are more suited for inpatient (hospital and long-term care) settings, whereas others are better suited to community or ambulatory settings.
Include:
1. Managed care:
Managed care describes a health care system whose goals are to provide cost-effective, quality care that focuses on decreased costs and improved outcomes for groups of clients.
Managed care denotes an emphasis on cost controls, customer satisfaction, health promotion, and preventive services.
2. Case management:
Case managers may be referred to as discharge planners; may be a nurse, social worker, or other appropriate professional
Case management involves multidisciplinary teams that assume collaborative responsibility for planning, assessing needs, and coordinating, implementing, and evaluating care for groups of clients from preadmission to discharge or transfer and recuperation.
3. Differentiated practice:
Differentiated practice is a system in which the best possible use of nursing personnel is based on their educational preparation and resultant skill sets.
Consist of specific job descriptions for nurses according to their education or training, for example, LVN, associate degree RN, BSN RN, MSN RN, or APRN. Requires the delineation of roles between both licensed nursing personnel and UAP.
4. Case method:
Also referred to as total care.
One nurse is assigned to and is responsible for the comprehensive care of a group of clients during an 8- or 12-hour shift. A client has consistent contact with one nurse during a shift but may have different nurses on other shifts.
5. Functional method:
The functional nursing method focuses on the jobs to be completed.
Personnel with less preparation than the professional nurse perform less complex care requirements.
6. Team nursing:
Team nursing is the delivery of nursing care to individual clients by a group of providers led by a professional nurse.
A nursing team consists of RNs, LPNs, and UAPs. This team is responsible for providing coordinated nursing care to a set of clients for a specific period of time, for example, one shift.
7. Primary nursing:
Primary nursing is a system in which one nurse is responsible for overseeing the total care of a number of hospitalized clients 24 hours a day, 7 days a week, even if he or she does not deliver all of the care personally.
Financing Health Care
Patient Protection and Affordable Care Act (ACA)
Comprehensive U.S. health care reform signed by President Obama in 2010.
Key features:
|
Key Feature |
Description |
|
Individual Mandate |
Most Americans are required to have insurance. Individuals will be fined if they do not have health insurance. |
|
Employer Mandate |
Employers must provide insurance if eligible |
|
Medicaid Expansion |
Expanded eligibility for low-income individuals |
|
Health Exchanges |
Marketplaces for individuals/small businesses (SHOP) |
|
Private Insurance Reforms |
Covers preexisting conditions and extends coverage for young adults |
|
Patient-Centered Outcomes Research Institute established |
Studies effectiveness of treatments |
|
Public Health Council established |
Coordinates wellness and prevention efforts |
Payment Sources in the United States
Public insurance programs:
|
Program |
Key Features |
|
Medicare |
For people ≥65 years or with disabilities |
|
- Part A |
Hospital, hospice, home care |
|
- Part B |
Outpatient/physician services (voluntary) |
|
- Part D |
Prescription drugs (voluntary) |
|
Medicaid |
Federal/state program for low-income individuals; each state defines coverage |
|
CHIP |
Children’s health insurance program- Covers low-income children not eligible for Medicaid |
|
WIC |
Women, infants, and children program- Nutritional support for low-income pregnant women and children ≤5 yrs |
|
SSI |
Supplemental Security Income- Financial aid to blind/disabled individuals, often used for health expenses |
Nursing insight
Prospective payment system:
This legislation limits the amount paid to hospitals that are reimbursed by Medicare. Reimbursement is made according to a classification system known as diagnosis-related groups (DRGs). The system has categories that establish pretreatment diagnosis billing categories.
Under this system, the hospital is paid a predetermined amount for clients with a specific diagnosis
Controls Medicare hospital costs.
No extra payment for preventable hospital-acquired conditions (e.g., pressure ulcers, retained surgical objects)
Health insurance types:
Private Insurance
Often covers 80% of service costs; consumer pays premiums, copays, deductibles
With private insurance health plans, the insurance company reimburses the health care provider a fee for each service provided (fee-for-service).
The term third-party reimbursement refers to the insurance company that pays the client’s (first party) bill to the provider (second party).
Types:
- For-Profit: e.g., Aetna, Metropolitan Life
- Not-For-Profit e.g., Blue Shield
Group Insurance Plans
|
Plan Type |
Key Characteristics |
|
HMO (Health Maintenance Organization) |
Emphasizes prevention; requires PCP; reduced but limited services |
|
ACO (Accountable Care Organization) |
Links payment to quality & cost control; often used by Medicare |
|
PPO (Preferred Provider Organization) |
Offers provider choice; higher cost than HMO |
|
PPA (Preferred Provider Arrangement) |
Contracted with individual providers; can be limited/unlimited |
|
IPA (Independent Practice Association) |
Fixed payment to IPA; services in private offices |
|
PHO (Physician/Hospital Organization) |
Collaboration between hospitals & physicians; part of integrated delivery systems (IDS) |
Discharge Planning
Discharge planning is a coordinated, interprofessional process that develops a plan for continuing care after a patient leaves a health care agency.
Discharge planning with coordination of services must begin the moment a patient is admitted to a hospital. Involves:
- Determining the appropriate post-hospital destination for a patient.
- Identifying a patient’s needs for a smooth and safe transition from the acute care hospital/post–acute care agency to the patient’s discharge destination.
- Early mobility protocols, health education, and new medication regimens.
Teach-back is an evidence-based health literacy intervention that promotes patient engagement, patient safety, adherence, and quality.
Comprehensive discharge instruction ensures that patients know what to do when they get home, how to perform care activities, and what to do when problems develop.
Discharge Planning Models:
Coleman’s “care transitions program”: Emphasizes the role of a transition coach in managing/facilitating the discharge of a patient to home or to a rehabilitation center. Model is based on four pillars:
(1) medication self-management
(2) patient-centered record
(3) follow-up
(4) indicators of worsening medical conditions.
Naylor’s “transitional care model”: Emphasizes comprehensive discharge planning and follow-up for older adults who are chronically ill.
Model contains six key components:
(1) in-hospital assessment and development of the discharge care plan by a transitional care nurse/advanced practice nurse/gerontological nurse
(2) discharge preparation by an interprofessional care team
(3) patient participation (communication between nursing staff and the patient) regarding the process, the decision making, the discharge planning, and the discharge education.
(4) continuity of care and communication among health care providers.
(5) predischarge assessment
(6) post-discharge follow-up.
High-intensity care model (grace model): The interprofessional team is headed by both a nurse practitioner and a social worker. Other team members include a pharmacist, geriatric specialist, and mental health provider. This team works in tandem to support the primary care physician and, following best practice protocols, to fully address a patient’s health conditions.
Referrals:
Tips for making a successful referral include the following:
- Engage the patient and family caregiver in the referral process, including selecting the care provider.
- Explain the reason for the referral, the service to be provided, and how the service will be provided.
- Make the referral as soon as possible.
- Give the care provider receiving the referral as much information as possible about the patient.
- The care provider, such as a physical therapist, social worker, dietitian, or radiologist, will make recommendations for the patient’s care.
- Learn these recommendations and incorporate them into the treatment plan as soon as possible.
Summary
- Health care delivery services can be categorized by the type of service: primary, secondary or tertiary.
- The role of the nurse in providing care to clients will vary depending on the employment setting, the nurse’s credentials, and the needs of the client.
- In the United States, health care is financed largely through government agencies and private organizations that provide health care insurance, prepaid plans, and federally funded programs.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Healthcare Delivery Systems
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


