Please set your exam date
Drug Action Across The Life Span
Study Questions
Practice Exercise 1
The nurse is reviewing factors that influence pharmacokinetics in the neonatal patient. Which factors puts the neonatal patient at risk with regard to drug therapy? Select all that apply
Explanation
Neonatal patients have immature organ systems, altered body composition, and different enzyme activity compared to adults. These developmental differences significantly affect pharmacokinetics—how the body absorbs, distributes, metabolizes, and excretes drugs—placing neonates at higher risk for drug accumulation and adverse effects.
Rationale for correct answers:
C. Immature renal function
Reduced glomerular filtration, tubular secretion, and reabsorption lead to slower elimination of drugs, increasing the risk of accumulation and toxicity.
D. Reduced first-pass elimination in the liver
Liver enzyme systems are immature in neonates, leading to reduced drug metabolism and prolonged drug effects.
E. Decreased protein-binding of medications
Lower plasma albumin levels and immature protein-binding capacity increase the amount of free (active) drug in circulation, heightening the risk of toxicity.
Rationale for incorrect answers:
A. Higher gastric pH
Neonates do have a higher gastric pH, but while this can influence drug absorption, it is not the main reason for increased risk of drug toxicity compared to organ immaturity and protein-binding differences.
B. Increased peristalsis in the GI tract
Neonates typically have slower gastric emptying and peristalsis, not increased, which can delay drug absorption.
Take-home points:
- Immature renal and hepatic function in neonates prolongs drug clearance.
- Reduced protein binding increases the active drug fraction in the blood.
- Neonatal pharmacokinetics requires cautious dosing and close monitoring for adverse effects.
The physiologic differences in the pediatric patient compared with the adult patient affect the amount of drug needed to produce a therapeutic effect. The nurse is aware that one of the main differences is that infants have which of these factors?
Explanation
Infants have a markedly different body composition compared to adults, which alters drug distribution. One of the most important differences is a much higher total body water percentage, which impacts the volume of distribution for water-soluble drugs and influences dosing requirements.
Rationale for correct answer:
D. Water composition of approximately 75%
Infants have a total body water content of about 70–80%, significantly higher than adults. This increases the distribution volume for water-soluble drugs, often requiring a larger mg/kg dose to achieve therapeutic plasma concentrations.
Rationale for incorrect answers:
A. Increased protein in circulation
Infants actually have lower plasma protein levels (e.g., albumin), reducing protein-binding capacity and increasing the free active drug in circulation.
B. Fat composition lower than 0.001%
This is incorrect; infants have a lower proportion of body fat than adults, but not nearly as low as 0.001%. Body fat typically makes up around 10–15% in newborns.
C. More muscular body composition
Infants have less developed muscle mass, which can affect intramuscular drug absorption and distribution, but this is not the primary difference influencing therapeutic dosing.
Take-home points:
- Infants have higher total body water and lower fat stores than adults.
- Water-soluble drugs may require higher mg/kg doses in neonates.
- Lower protein-binding capacity increases the proportion of free active drug in circulation.
A pregnant patient who is at 32 weeks’ gestation has a cold and calls the office to ask about taking an over-thecounter medication that is rated as pregnancy category. Which answer by the nurse is correct?
Explanation
The U.S. FDA pregnancy categories (now replaced by the Pregnancy and Lactation Labeling Rule, but still commonly tested) classified Category A medications as having no demonstrated risk to the fetus in controlled human studies. These are the safest drugs for use during pregnancy, although non-drug measures are always preferred when possible.
Rationale for correct answer:
D. “Studies indicate that there is no risk to the human fetus, so it is okay to take this medication as directed if you need it.”
This matches Category A, which is supported by well-controlled human studies showing no harm to the fetus.
Rationale for incorrect answers:
A. “This drug causes problems in the human fetus, so you should not take this medication.”
This statement would apply to Category X or some Category D drugs, not Category A.
B. “This drug may cause problems in the human fetus, but nothing has been proven in clinical trials. It is best not to take this medication.”
This describes the uncertainty of Category C drugs, not Category A.
C. “This drug has not caused problems in animals, but no testing has been done in humans. It is probably safe to take.”
This is consistent with Category B, where animal studies show no risk but human data is lacking.
Take-home points:
- Category A: controlled human studies show no fetal risk.
- Category B: animal studies show no risk, but human data lacking.
- Category C/D/X: increasing levels of known or potential fetal risk.
- Even safe drugs in pregnancy should be taken only when necessary.
The nurse is preparing to give an oral dose of acetaminophen (Tylenol) to a child who weighs 12 kg. The dose is 15 mg/kg. How many milligrams will the nurse administer for this dose?
Explanation
Rationale for correct answer:
To calculate the total dose, the child's weight in kilograms correlates to the prescribed dose per kilogram in that:
Child's weight: 12 kg
Dose: 15 mg/kg
Calculation:
The dose is the multiplication factor, where 15 milligrams of acetaminophen is administered for every kilogram of body weight.
15mg/kg x 12kg = 180.
For a child who weighs 12kg , 180 mg will suffice.
The final calculated dose is therefore, 180 milligrams (mg).
- Weight-Based Dosing is Crucial
- The core formula is: Patient's Weight (in kg) x Dose (in mg/kg) = Total Dose (in mg).
- Pay close attention to the units
A nurse caring for a pregnant client in her second trimester. She expects which of the following in the drug excretion?
Explanation
During pregnancy, especially in the second trimester, physiological changes occur that significantly affect pharmacokinetics. One major change is the increase in renal plasma flow and glomerular filtration rate (GFR), which accelerates renal drug clearance. This is important for drugs that are primarily excreted unchanged by the kidneys.
Rationale for correct answer:
B. Increased glomerular filtration rate – Correct. Pregnancy increases cardiac output and renal perfusion, leading to a ~50% rise in GFR by mid-pregnancy. This enhances drug excretion for renally cleared medications, sometimes requiring dosage adjustments.
Rationale for incorrect answers:
A. Decreased renal blood flow – Pregnancy increases, not decreases, renal blood flow due to cardiovascular adaptations that enhance perfusion to support maternal and fetal needs.
C. No change from pre-pregnancy values – Drug excretion changes substantially during pregnancy; assuming no change would ignore the documented increase in GFR.
D. Complete cessation of drug clearance via kidneys – This never occurs under normal pregnancy physiology; instead, clearance usually increases.
Take-home points:
- GFR increases during pregnancy, especially in the second trimester, enhancing renal drug clearance.
- Drugs eliminated mainly by the kidneys may require dose or frequency adjustments to maintain therapeutic levels.
- Monitoring drug efficacy is crucial, as subtherapeutic effects can occur if clearance is accelerated.
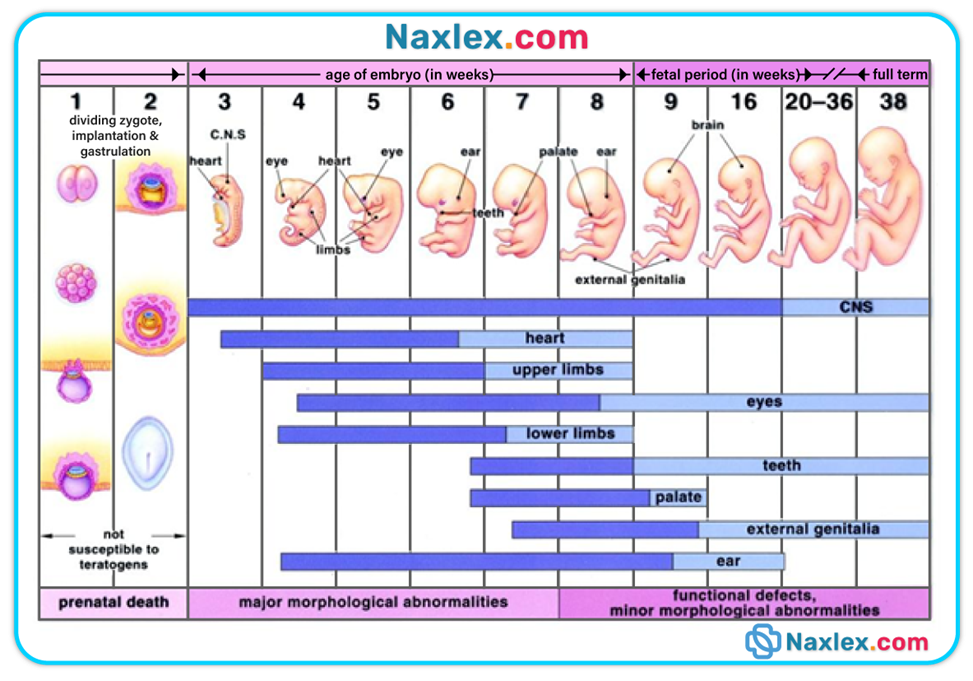
The critical window for organogenesis, when teratogens most often cause structural defects, occurs during:
Explanation
The embryonic period (weeks 3–8 after conception) is the critical window for organogenesis, where all major body structures and organ systems are formed. Exposure to teratogens during this stage can cause permanent, often severe structural abnormalities because cells are rapidly dividing, differentiating, and migrating. Nursing care for pregnant patients must include medication safety screening, thorough maternal education on environmental hazards, and timely prenatal care to reduce teratogenic exposure during this high-risk phase.
Rationale for correct answer:
B. Weeks 3–8 post-conception – This is the peak vulnerability period. During this embryonic stage, critical organ systems (heart, brain, limbs, facial structures, neural tube) are forming. Teratogenic damage here often results in irreversible structural malformations, such as congenital heart defects, cleft lip/palate, or limb deformities. The earlier in this window the exposure occurs, the more severe the impact.
Rationale for incorrect answers:
A. Weeks 1–2 post-conception – This pre-embryonic stage follows fertilization and ends with implantation. Teratogen exposure here usually leads to an all-or-none effect: either the embryo survives with no damage or it results in early pregnancy loss. Major malformations are uncommon at this stage.
C. Weeks 9–40 post-conception – The fetal period is focused on growth, maturation, and refinement of function. Teratogens here are more likely to cause functional deficits (e.g., cognitive impairment, hearing loss) or mild structural changes, but not major malformations.
D. The postpartum period – At this point, organogenesis has been completed. Teratogens no longer cause developmental defects, but some drugs can still harm the infant through lactation exposure, potentially causing toxicity or developmental delays.
Take-home points:
- The highest teratogenic risk is during weeks 3–8.
- Counseling and screening should begin before conception when possible.
- Pregnant patients should avoid known teratogens (e.g., isotretinoin, certain anticonvulsants, alcohol, tobacco, some infections) during early pregnancy.
For a neonate, which IM injection site is recommended due to its muscle development and safety?
Explanation
In neonates, intramuscular (IM) injections must be given in a site with adequate muscle mass, good vascular supply, and minimal risk of injury to major nerves or blood vessels. The vastus lateralis, located on the anterolateral thigh, is the preferred site because it is well-developed even in newborns, has fewer major nerves nearby, and ensures consistent absorption of medications. Other sites such as the deltoid, dorsogluteal, and ventrogluteal are either underdeveloped in neonates or carry a higher risk of complications. Safe site selection is essential to prevent injury and ensure proper drug delivery.
Rationale for correct answer:
B. Vastus lateralis – This is the most recommended IM injection site for neonates due to its relatively large muscle mass, easy accessibility, and safety profile. It allows reliable absorption and minimizes the risk of injuring major nerves or vessels.
Rationale for incorrect answers:
A. Deltoid – In neonates, the deltoid muscle is underdeveloped and too small to accommodate most IM doses safely. Using this site increases the risk of poor absorption and nerve injury.
C. Dorsogluteal – Not recommended for neonates because it poses a significant risk of sciatic nerve injury and has less predictable absorption due to variable fat distribution in infants.
D. Ventrogluteal – Although a safe site in older children and adults, it is not the first choice in neonates due to limited muscle development in this area during the early months of life.
Take-home points:
- The vastus lateralis is the safest and most reliable IM injection site in neonates.
- Deltoid and ventrogluteal sites may be considered only as the child grows and develops more muscle mass.
- Avoid the dorsogluteal site in neonates due to the high risk of sciatic nerve injury.
A nurse is teaching medication administration to caregivers of toddler. The nurse should emphasize:
Explanation
When administering medications to toddlers, it is important to use techniques that encourage compliance, maintain safety, and ensure accurate dosing. Masking unpleasant tastes with a small amount of a favorite food or liquid can help improve acceptance without requiring the child to consume a large volume, which could result in incomplete ingestion of the medication. Caregivers should be taught safe medication handling practices, avoiding techniques that risk dose inaccuracy, drug-food interactions, or loss of therapeutic effect.
Rationale for correct answer:
B. Using minimal volumes of food or liquid to mask taste – This is the preferred approach as it allows the child to consume the entire dose without excess fluid and reduces the chance of medication being left behind. It also helps maintain therapeutic effectiveness.
Rationale for incorrect answers:
A. Mixing drugs into a full bottle of milk – This is not recommended because the child may not finish the bottle, leading to partial dosing and reduced effectiveness of the medication.
C. Letting the child take medicine unsupervised to build trust – Unsafe for toddlers due to the risk of overdose, spills, and non-compliance. Medication should always be administered under adult supervision.
D. Crushing tablets without consulting a pharmacist – This may alter drug absorption, destroy protective coatings, or change drug effectiveness. Always confirm with a pharmacist before altering medication form.
Take-home points:
- Use a small amount of food or liquid to mask unpleasant medication taste in toddlers.
- Avoid large volumes of food or drink that may not be fully consumed.
- Medications should always be given under adult supervision and in the correct form.
Practice Exercise 2
Which nursing action(s) would be essential when monitoring drug therapy in the geriatric patient? Select all that apply
Explanation
Older adults experience significant physiological changes that affect how drugs are absorbed, distributed, metabolized, and excreted. Polypharmacy, multiple comorbidities, and age-related organ function decline increase their vulnerability to adverse drug reactions and drug–drug interactions. Nurses play a crucial role in carefully monitoring therapy, ensuring that doses remain therapeutic without causing harm. population.
Rationale for correct answers:
- Monitoring renal and liver function – Renal and hepatic function decline with age, leading to reduced drug clearance and increased risk of accumulation. Routine assessment of creatinine clearance, liver enzymes, and other relevant labs helps determine if dosage adjustments are needed to prevent toxicity.
- Monitoring for drug interactions – Older adults often take multiple prescription and over-the-counter drugs. Drug–drug and drug–food interactions are more common and can significantly alter therapeutic effects or cause harm, making vigilant monitoring essential.
- Completing a thorough drug history, including over-the-counter and alternative therapies – Many older patients use herbal remedies, vitamins, or supplements alongside prescribed medications. Without a complete list, dangerous interactions can be overlooked, so obtaining a detailed history is critical for safe prescribing and monitoring.
- Inquiring about the ability to pay for medications – While financial concerns are important for medication adherence, this action does not directly monitor the physiological safety of drug therapy. It is more related to socioeconomic support and access to care rather than drug monitoring itself.
- Educating the patient and caregivers about all drugs and potential complications – Knowledge empowers patients to recognize early warning signs of adverse reactions and understand proper administration. Caregiver education ensures that medication schedules are followed accurately and complications are reported promptly.
Take-home points:
- Renal and hepatic monitoring is essential in geriatrics to prevent drug toxicity.
- Drug interaction checks and a full medication history reduce adverse event risk.
- Education for patients and caregivers improves safety and adherence in long-term therapy.
While teaching a 76-year-old patient about the adverse effects of his medications, the nurse encourages him to keep a journal of the adverse effects he experiences. This intervention is important for the older adult patient because of which alterations in pharmacokinetics?
Explanation
In older adults, the way the body processes medications changes due to age-related alterations in pharmacokinetics. These changes can influence absorption, distribution, metabolism, and excretion, often increasing the likelihood of adverse effects or toxicity. Metabolism—especially in the liver—tends to slow with age due to reduced hepatic blood flow and diminished enzyme activity.
Rationale for correct answer:
C. Decreased blood flow to the liver, resulting in altered metabolism – Hepatic blood flow decreases by up to 40% with age, slowing the metabolism of many drugs, particularly those with a high first-pass effect. Slower metabolism means drugs remain in circulation longer, increasing the risk of adverse effects. Tracking these effects in a journal helps providers adjust doses more safely.
Rationale for incorrect answers:
A. Increased renal excretion of protein-bound drugs – Aging is typically associated with decreased, not increased, renal function. Slower elimination can lead to higher drug levels in the blood, but the concern is drug accumulation, not increased excretion.
B. More alkaline gastric pH, resulting in more adverse effects – Older adults often have a less acidic stomach environment, which can alter drug dissolution and absorption. while this may influence the onset or extent of absorption, it is not the primary reason why journaling adverse effects is emphasized for this population.
D. Less adipose tissue to store fat-soluble drugs – In older adults, there is typically more adipose tissue compared to lean muscle mass, not less. Increased fat stores can prolong the half-life of fat-soluble drugs, but this is unrelated to why the nurse emphasizes journaling adverse effects in this scenario.
Take-home points:
- Hepatic metabolism slows with age due to reduced blood flow and enzyme activity.
- Adverse effect journaling helps detect drug accumulation and patterns of toxicity.
- Medication teaching in older adults must address age-related pharmacokinetic changes for safer drug therapy.
When the nurse is reviewing a list of medications taken by an 88-year-old patient, the patient says, “I get dizzy when I stand up.” She also states that she has nearly fainted “a time or two” in the afternoons. Her systolic blood pressure drops 15 points when she stands up. Which type of medication may be responsible for these effects?
Explanation
Older adults are more susceptible to postural (orthostatic) hypotension, a condition in which blood pressure drops significantly upon standing, leading to dizziness, lightheadedness, or even fainting. This occurs due to age-related cardiovascular changes and the influence of certain medications. Antihypertensives, which lower blood pressure, can exacerbate this effect by reducing the body’s ability to rapidly compensate for position changes.
Rationale for correct answer:
D. Antihypertensives – Many antihypertensive agents, such as alpha-blockers, beta-blockers, and diuretics, can impair the body's compensatory mechanisms for maintaining blood pressure when standing. In older adults, reduced baroreceptor sensitivity compounds the problem, leading to orthostatic hypotension and an increased risk of falls.
Rationale for incorrect answers:
A. Nonsteroidal antiinflammatory drugs (NSAIDs) – NSAIDs primarily affect the gastrointestinal tract and kidneys, and while they can contribute to fluid retention or increase blood pressure, they are not a common cause of sudden drops in blood pressure upon standing.
B. Cardiac glycosides – Drugs like digoxin can cause dizziness or vision changes due to bradycardia or toxicity, but they do not directly cause orthostatic hypotension. If dizziness is related to these medications, it is usually due to altered heart rate or rhythm, not a positional drop in blood pressure.
C. Anticoagulants – These drugs reduce clotting ability and increase bleeding risk but have no direct effect on blood pressure regulation. Dizziness in patients on anticoagulants may result from anemia due to bleeding, but not from position changes causing hypotension.
Take-home points:
- Antihypertensives can cause orthostatic hypotension, especially in older adults.
- Age-related changes in baroreceptor sensitivity increase fall risk with these medications.
- Medication reviews in the elderly should include assessment for dizziness, near-syncope, and blood pressure changes with position.
The nurse is preparing to administer an injection to a preschool-age child. Which approaches are appropriate for this age group? Select all that apply
Explanation
Preschool-age children (ages 3–5) are in Piaget’s preoperational stage of cognitive development, characterized by magical thinking, egocentrism, and limited understanding of cause-and-effect. When preparing for a medical procedure like an injection, the nurse’s approach must be brief, concrete, and supportive to match the child’s developmental level. Overly detailed explanations or attempts to involve the child in decision-making may cause more anxiety. Comfort measures, reassurance, and framing the experience in familiar or imaginative terms help reduce fear and improve cooperation.
Rationale for correct answers:
B. Provide a brief, concrete explanation about the injection – Preschoolers benefit from simple, specific instructions like “This will feel like a quick pinch,” rather than abstract or complex explanations. This helps them process what will happen without becoming overwhelmed.
D. Make use of magical thinking – Preschoolers often engage in fantasy play and magical thinking; the nurse can use this to reduce fear. For example, explaining that the medicine is “superhero juice” that will help their body be strong can make the experience less threatening.
E. Provide comfort measures after the injection – Giving a hug, praise, or a small reward after the procedure helps reinforce positive coping and provides emotional security, which is crucial for preschoolers after a stressful event.
Rationale for incorrect answers:
A. Explain to the child in advance about the injection – Giving detailed explanations far in advance is not appropriate for preschoolers, as it can increase anxiety and anticipation. Their limited time concept means they may fixate on the upcoming event and become more fearful.
C. Encourage participation in the procedure – Involving preschoolers in decision-making (e.g., choosing the injection site) is not developmentally appropriate, as it may create feelings of responsibility or guilt. They are better supported through distraction and reassurance rather than active participation in the medical decision.
Take-home points:
- Preschoolers need brief, concrete explanations rather than detailed or abstract information.
- Magical thinking can be an effective coping tool during medical procedures.
- Comfort measures after procedures promote emotional security and trust in healthcare providers.
An 82-year-old patient is admitted to the hospital after an episode of confusion at home. The nurse is assessing the current medications he is taking at home. Which method is the best way to assess his home medications?
Explanation
In older adults, obtaining an accurate medication history is essential to avoid medication errors, drug interactions, or duplications. Age-related cognitive changes, acute confusion, or memory impairment can make verbal reports unreliable. Reviewing the actual medication containers provides the nurse with precise information about drug names, dosages, frequencies, and prescribing providers, which is critical for ensuring patient safety and proper reconciliation.
Rationale for correct answer:
C. Ask the patient's wife to bring his medications to the hospital in their original containers – This is the most accurate method because original labels show the exact drug names, strengths, dosage forms, and prescribing information, allowing the nurse to verify and reconcile medications safely.
Rationale for incorrect answers:
A. Ask the patient what medications he takes at home – Older adults experiencing confusion may have unreliable recall of medication details, increasing the risk of omissions or inaccuracies.
B. Ask the patient's wife what medications he takes at home – While family members can provide helpful information, they may not know exact dosages, strengths, or updated medication changes, leading to incomplete data.
D. Contact the patient's pharmacy for a list of the patient's current medications – A pharmacy list can be useful but may not reflect over-the-counter drugs, herbal supplements, or prescriptions filled at other pharmacies.
Take-home points:
- Direct inspection of medication containers ensures accurate medication reconciliation.
- Elderly patients with confusion may not provide reliable medication histories.
- Original labels reveal important details about drug names, doses, and prescribers, reducing the risk of medication errors.
The nurse understands that when counseling an adolescent on new medication therapy, which approach best supports safe and effective use?
Explanation
When counseling adolescents on new medication therapy, the nurse should use an approach that respects privacy, supports autonomy, and encourages active participation. Adolescents are developing a stronger sense of identity and independence, so they respond better when they are treated as responsible partners in their care. Explaining medication purpose, expected effects, and possible side effects in a clear, age-appropriate manner fosters trust, increases understanding, and improves adherence to the prescribed regimen.
Rationale for correct answer:
D. Respect privacy and autonomy while explaining medication effects – Best choice because it meets the adolescent’s developmental needs, ensures they understand how and why to take the medication, and fosters responsibility and adherence through trust and respect.
Rationale for incorrect answers:
A. Speak only to the parents about the medication plan – This approach ignores the adolescent’s need for involvement and control over their health decisions, which can result in resistance or poor adherence.
B. Provide minimal details to avoid overwhelming the patient – Limiting information deprives the adolescent of the knowledge necessary to manage their own health safely and can create confusion or mistrust.
C. Give a written schedule without further discussion – Written instructions alone cannot address questions, correct misconceptions, or ensure understanding. Interactive discussion is essential for safe use.
Take-Home Points:
- Involve adolescents directly in medication discussions to promote adherence and understanding.
- Balance privacy with education by providing honest, age-appropriate explanations.
- Interactive communication is more effective than written or parent-only instruction.
Which of the following pharmacokinetic change in older adults can lead to prolonged sedation from benzodiazepines?
Explanation
In older adults, age-related changes in body composition and organ function can significantly affect pharmacokinetics—the way drugs are absorbed, distributed, metabolized, and excreted. Benzodiazepines are highly lipid-soluble drugs, meaning they are stored in fat tissue. As adults age, they tend to have increased body fat stores and reduced lean body mass, leading to a larger reservoir for lipid-soluble medications.
Rationale for correct answer:
D. Increased fat stores – Best choice because the increased fat content in older adults acts as a storage depot for lipid-soluble drugs like benzodiazepines, slowing their release and metabolism, thereby extending sedative effects and increasing fall risk.
Rationale for incorrect answers:
A. Increased total body water – Older adults typically have decreased, not increased, total body water, which primarily affects water-soluble drugs rather than lipid-soluble drugs like benzodiazepines.
B. Increased plasma albumin levels – Plasma albumin levels often decrease with age or chronic illness, especially affecting protein-bound drugs. Higher albumin levels are uncommon in older adults and would not explain prolonged sedation.
C. Increased renal clearance – Renal clearance usually declines with aging due to reduced glomerular filtration rate. Even if renal clearance increased, benzodiazepines are metabolized mainly by the liver, not eliminated unchanged by the kidneys.
Take-Home Points:
- Older adults have increased fat stores and decreased lean body mass, altering drug distribution.
- Lipid-soluble drugs like benzodiazepines remain longer in the body, causing prolonged effects.
- Drug therapy in older adults requires careful dose adjustment and monitoring to prevent toxicity.
Comprehensive Questions
A 16-year-old adolescent is 6 weeks pregnant. The pregnancy has exacerbated her acne. She asks the nurse if she can resume taking her isotretinoin (Accutane) prescription, a category X drug. What is the most appropriate response by the nurse?
Explanation
Understanding the risks of pregnancy category X drugs is essential when caring for pregnant clients. Isotretinoin (Accutane) is a potent teratogen that can cause serious fetal malformations if taken during pregnancy. Nurses play a critical role in ensuring client education, promoting effective contraception, and preventing harmful drug exposure during the prenatal period.
Rationale for correct answer:
C. “Accutane is known to cause birth defects and should never be taken during pregnancy”:
Isotretinoin is a category X drug, meaning the risks of fetal abnormalities outweigh any benefit. The nurse must emphasize its contraindication and the serious risks of teratogenicity.
Rationale for incorrect answers:
A. “Since you have a prescription for Accutane, it is safe to resume using it”:
Having a previous prescription does not ensure current safety. Isotretinoin is contraindicated in pregnancy due to its teratogenic effects, and resuming it could cause severe fetal harm.
B. “You should check with your health care provider at your next visit”:
Delaying guidance puts the fetus at risk. Immediate education is necessary because continued or resumed use of isotretinoin could cause irreversible developmental defects.
D. “You should reduce the Accutane dosage by half during pregnancy”:
Reducing the dose does not eliminate the risk of teratogenicity. Even small amounts of isotretinoin can cause severe birth defects, so it must be completely avoided during pregnancy.
Take-home points:
- Isotretinoin is a pregnancy category X drug and is absolutely contraindicated during pregnancy.
- Even small doses of isotretinoin can cause severe fetal abnormalities due to its teratogenic effects.
- Immediate client education is essential to prevent fetal harm from high-risk medications during pregnancy.
To reduce the effect of a prescribed medication on the infant of a breast-feeding mother, how should the nurse teach the mother to take the medication?
Explanation
When administering medications to breastfeeding mothers, timing can significantly reduce drug exposure to the infant. To minimize infant absorption, it is best to take the medication immediately after breastfeeding. This allows the drug concentration in breast milk to decrease before the next feeding, helping to ensure infant safety while maintaining therapeutic benefit for the mother.
Rationale for correct answer:
D. Immediately after breast-feeding:
Taking the medication right after breastfeeding allows time for drug levels in the mother’s bloodstream—and consequently in her milk—to decline before the next feed. This minimizes the amount of drug the infant receives.
Rationale for incorrect answers:
A. At night:
Taking the medication at night does not consistently reduce the drug level in breast milk unless coordinated with feeding times. Drug transfer to milk is influenced more by timing relative to breastfeeding than by the time of day.
B. Immediately before the next feeding:
Taking medication just before breastfeeding allows peak drug levels to pass into breast milk during the feeding, increasing infant exposure. This timing should be avoided when minimizing transfer to the baby.
C. In divided doses at regular intervals around the clock:
While regular dosing maintains steady therapeutic levels in the mother, it can lead to continuous exposure in the infant through breast milk. This approach may be appropriate for safety but doesn’t minimize infant drug exposure.
Take-home points:
- Administering medication immediately after breastfeeding helps reduce infant drug exposure.
- Breastfeeding timing impacts how much drug passes into breast milk, not just time of day.
- Peak drug levels in breast milk should be avoided during feeding to protect the infant.
An older adult client has arthritis in her hands and takes several prescription drugs. Which statement by this client requires further assessment by the nurse?
Explanation
Older adults often manage multiple medications and may unintentionally place young children at risk if drugs are not stored safely. Medications should be kept in childproof containers and placed out of reach. Nurses must promptly provide education on safe medication storage to prevent accidental pediatric exposure.
Rationale for correct answer:
C. “I care for my 2-year-old grandson twice a week”:
This raises safety concerns, especially if medications are within reach. Older adults may unintentionally expose young children to harmful drugs if proper storage isn't ensured, requiring immediate assessment and education.
Rationale for incorrect answers:
A. “My pharmacist puts my pills in screw-top bottles to make it easier for me to take them”:
This shows that medication packaging is being adapted to her needs, which is a positive step in maintaining medication adherence despite limited hand dexterity.
B. “I fill my prescriptions once per month”:
Refilling medications monthly is common and suggests she is maintaining a routine. It does not indicate any immediate risk or need for further evaluation.
D. “My arthritis medicine helps my stiff hands”:
This reflects that the medication is achieving its intended therapeutic effect, and there are no red flags indicating a problem that needs further assessment.
Take-home points:
- Older adults caring for young children must be assessed for safe medication storage practices.
- Routine medication refills and effectiveness do not typically require further assessment.
- Medications in accessible areas can pose serious harm to toddlers in multi-generational homes.
A nurse is administering a liquid medication to a 15-month-old child. What is the most appropriate approach to medication administration by the nurse? Select all that apply.
Explanation
Administering medications to young children, such as a 15-month-old, requires strategies that promote safety and cooperation. The nurse should ensure the child is sitting upright to reduce the risk of aspiration and should use age-appropriate choices, like offering a preferred cup, to enhance acceptance and reduce resistance during medication administration. These techniques help build trust and support medication adherence in pediatric clients.
Rationale for correct answers:
D. Sit the child up, hold the medicine cup to her lips, and kindly instruct her to drink:
Sitting the child upright supports safe swallowing and reduces the risk of aspiration. Clear, gentle instructions provide guidance and reassurance during medication administration.
E. Offer the child a choice of cup in which to take the medicine:
Giving the toddler a simple choice (like selecting a cup) promotes a sense of control and cooperation while still ensuring the medication is taken.
Rationale for incorrect answers:
A. Tell the child that the medication tastes just like candy:
Misleading the child about the taste can reduce trust and increase future resistance to medications, especially if the taste is unpleasant. Honest, age-appropriate explanations are more effective.
B. Mix the medication in 8 oz of orange juice:
Mixing medication in a large volume risks the child not consuming the full dose. Also, combining meds with juice may alter taste or stability, potentially decreasing effectiveness.
C. Ask the child if she would like to take her medication now:
Giving a toddler the option to refuse can lead to noncompliance. Offering limited choices within the framework of taking the medication is more developmentally appropriate.
Take-home points:
- Always sit young children upright during medication administration to reduce aspiration risk.
- Offering toddlers limited choices, such as selecting a cup, increases cooperation without allowing refusal.
- Avoid misleading statements and large fluid volumes when giving liquid medications to toddlers.
The nurse is preparing to give an oral medication to a 6-month-old infant. How should this drug be administered?
Explanation
Administering oral medications to infants requires careful technique to ensure safety and effectiveness. Placing the medicine dropper in the inner cheek helps prevent choking and allows the infant time to swallow gradually, reducing the risk of aspiration. This method supports safe and comfortable medication delivery in young patients.
Rationale for correct answer:
C. By placing the medicine dropper in the inner cheek, allowing time for the infant to swallow:
This method helps control the flow of medication and prevents gagging or choking. The inner cheek route allows the infant to swallow safely and gradually, reducing the chance of spitting it out.
Rationale for incorrect answers:
A. By placing the medication in the next bottle of formula:
Mixing medication with formula can result in incomplete dosing if the infant doesn't finish the bottle. It also risks altering the formula’s taste, potentially causing feeding aversion.
B. By mixing the medication with juice in a bottle:
Juice is generally not recommended for infants under 1 year, and using it for medication delivery carries the same risk of incomplete dosing if the bottle isn’t finished.
D. By placing the medication toward the back of the mouth to avoid having the infant immediately spit out the medication:
Placing medication too far back in the mouth increases the risk of choking or aspiration. The safest and most effective route is along the inner cheek.
Take-home points:
- Administer oral medications to infants by placing the dropper in the inner cheek to prevent aspiration.
- Avoid mixing medication in formula or juice, as incomplete intake may result in an ineffective dose.
- Placing medicine toward the back of the mouth increases choking risk and should be avoided.
To reduce the chance of duplicate medication order for the older adult returning home after surgery, what actions should the nurse take? Select all that apply.
Explanation
Preventing duplicate medication orders in older adults after surgery is essential to ensure safe medication use and avoid adverse drug events. Taking a thorough medication history, including all OTC and prescription drugs, and performing medication reconciliation before discharge helps identify overlaps or omissions in therapy. These practices promote continuity of care and protect against medication-related complications.
Rationale for correct answers:
C. Take a medication history, including all OTC and prescription medications and a pharmacy history with each client visit:
Gathering a complete medication and pharmacy history helps identify overlapping or duplicate drugs, especially when multiple providers or pharmacies are involved in the patient’s care.
E. Perform a medication reconciliation before sending the client home:
Medication reconciliation compares hospital and home medication lists to detect duplications, omissions, or changes. It is essential for preventing errors during care transitions.
Rationale for incorrect answers:
A. Call in all prescriptions to the client’s pharmacies rather than relying on paper copies of prescriptions:
Calling prescriptions may help with legibility and pharmacy coordination, but it does not eliminate the risk of duplicate medications unless a complete medication review is performed.
B. Give all prescriptions to the client’s family member:
Providing prescriptions to a family member may support adherence, but it does not address the potential for duplication or medication overlap without a formal review process.
D. Work with the client’s health care provider to limit the number of prescriptions:
While reducing polypharmacy is beneficial, limiting prescriptions alone does not ensure duplication is avoided unless a reconciliation process verifies current therapy.
Take-home points:
- Always perform a medication reconciliation before discharge to prevent duplicate or omitted prescriptions.
- A complete medication and pharmacy history is vital to identify potential overlaps or errors in medication regimens.
- Relying solely on verbal orders or family involvement is not sufficient to prevent medication duplication.
A client who has been asked to participate in a study asks the nurse what the term placebo means. What would be an appropriate response by the nurse?
Explanation
Understanding the concept of a placebo is important when educating clients participating in clinical research. A placebo is a substance with no active medicinal ingredients, often used in studies to evaluate the true effectiveness of a new drug by comparison. Placebos help distinguish between a drug’s real therapeutic effects and psychological responses unrelated to the medication.
Rationale for correct answer:
C. “The term placebo refers to a dosage form that has no active ingredients; these are frequently used in studies to determine the effect of a new medication”:
A placebo is an inactive substance given to compare outcomes in clinical trials. It helps researchers assess a drug’s true effects by comparing results with participants who receive no active treatment.
Rationale for incorrect answers:
A. “The word placebo refers to the type of abnormal response that may occur when taking medications”:
This confuses placebo with adverse drug reactions or unpredictable drug responses. A placebo does not produce pharmacologic effects and is not inherently linked to abnormal responses.
B. “That term means the body has built up a resistance to a drug and that more of the drug is needed to get the same response”:
This describes drug tolerance, not placebo. Tolerance involves the body requiring increasing amounts of a drug to achieve the same therapeutic effect, which differs from placebo use.
D. “The word placebo comes from Latin and means ‘I will harm”:
The Latin origin of “placebo” is “I shall please,” not “I will harm.” Placebos are used ethically in controlled studies, not intended to cause harm.
Take-home points:
- A placebo is an inactive substance used in clinical trials to compare effects against active treatment.
- Placebos do not contain active ingredients and are used to evaluate the true effect of a medication.
- Misunderstanding placebo as tolerance or side effects reflects a need for client education during research participation.
Why is it important for the nurse to understand the difference between drug dependence and drug accumulation?
Explanation
Understanding the difference between drug dependence and drug accumulation is essential for safe medication management. Drug dependence involves a physical or psychological need for a substance after prolonged use, often associated with addictive drugs. In contrast, drug accumulation occurs when the body cannot metabolize or excrete a drug efficiently, leading to elevated plasma levels and potential overdose. Recognizing both concepts helps prevent adverse effects and supports appropriate therapeutic monitoring.
Rationale for correct answer:
D. Drug dependence can be the result of taking addictive substances for a prolonged time, and drug accumulation can result in drug overdose:
Drug dependence involves a physical or psychological need for a substance, often after chronic use. Drug accumulation occurs when repeated doses are given faster than the body can eliminate the drug, which can lead to toxicity or overdose. Understanding both helps nurses monitor for signs and educate patients effectively.
Rationale for incorrect answers:
A. Drug accumulation can be detected more easily than drug dependence:
Both drug accumulation and dependence require clinical observation, but detection depends on context, monitoring, and assessment. One is not inherently easier to detect than the other.
B. Drug accumulation may result in drug toxicity, and drug dependence can result in cell mutation:
While drug accumulation can lead to toxicity, dependence does not cause cell mutation. Cell mutation is typically associated with carcinogenic substances, not with dependency.
C. Drug dependence can be prevented, and drug accumulation is inevitable:
Drug accumulation is not inevitable; it can be avoided through proper dosing, renal/hepatic monitoring, and timing. Dependence may be reduced with appropriate prescribing and monitoring.
Take-home points:
- Drug dependence involves a psychological or physical need for a substance, often due to prolonged use.
- Drug accumulation occurs when the body cannot eliminate a drug efficiently, increasing the risk of overdose.
- Recognizing the difference between dependence and accumulation helps prevent toxicity and promotes safe medication practices.
The nurse knows that drug absorption in the elderly is affected by which of these physiologic factors? Select all that apply.
Explanation
Drug absorption in the elderly is influenced by age-related physiological changes that can alter how medications are processed in the body. Factors such as reduced cardiac output can decrease blood flow to the gastrointestinal tract, slowing absorption. A higher gastric pH may reduce the solubility of certain drugs, while decreased GI motility can delay the time it takes for medications to reach absorption sites.
Rationale for correct answers:
C. Reduced cardiac output:
Reduced cardiac output can decrease blood flow to the GI tract, slowing absorption due to less efficient drug transport into circulation after oral administration.
D. Higher gastric pH:
Aging can lead to reduced stomach acid production, increasing gastric pH. This affects the solubility and absorption of certain drugs, especially those needing an acidic environment for optimal absorption.
E. Decreased GI motility:
Slower gastrointestinal motility can delay drug absorption by prolonging the time it takes for a drug to reach its site of absorption or altering the absorption pattern altogether.
Rationale for incorrect answers:
A. Changes in albumin levels:
Albumin affects drug distribution and protein binding, not absorption. Low albumin may influence free drug levels in plasma but does not significantly impact how drugs are absorbed in the GI tract.
B. Increased filtration capacity of the kidneys:
Kidney filtration relates to drug excretion, not absorption. In the elderly, renal function typically declines rather than increases, affecting elimination rather than how the drug enters the bloodstream.
Take-home points:
- Reduced cardiac output in the elderly can impair GI blood flow, slowing the absorption of orally administered medications.
- Higher gastric pH due to decreased stomach acid affects drug solubility and delays absorption for pH-dependent drugs.
- Decreased GI motility prolongs drug transit time, potentially altering the rate and extent of drug absorption.
A client was discussing with the nurse the idea that in the future we will be able to determine which drug will be effective depending on a person’s genetic makeup. Which term does this refer to?
Explanation
Pharmacogenetics is the study of how a person's genetic makeup influences their response to medications. Variations in genes can affect drug metabolism, efficacy, and the risk of adverse effects. Understanding pharmacogenetics helps guide individualized therapy, ensuring safer and more effective medication use across diverse patient populations.
Rationale for correct answer:
B. Pharmacogenetics:
This is the study of how genetic differences influence individual responses to drugs, including efficacy and side effects. It enables personalized medicine by predicting which drugs are most effective based on a person's genetic profile.
Rationale for incorrect answers:
A. Polymorphisms:
These are variations in DNA sequences that may influence how individuals respond to medications. While relevant, the term refers to the variations themselves, not the broader study of drug response based on genetics.
C. Genome coding:
This term refers to the mapping and interpretation of genetic sequences but does not specifically address drug response or personalized therapy.
D. Pharmacokinetics:
Pharmacokinetics involves how the body absorbs, distributes, metabolizes, and excretes drugs. It does not focus on genetic influences but on the general behavior of drugs in the body.
Take-home points:
- Pharmacogenetics focuses on how genetic differences affect individual drug responses, guiding personalized therapy.
- Polymorphisms are gene variations that may impact drug metabolism but are not the same as pharmacogenetics.
- Pharmacokinetics explains the movement of drugs in the body but does not account for genetic variability in drug response.
The nurse caring for an elderly client understands that when giving medications there are aging factors that affect how the drug will work.
Indicate with an X the factors that influence drug actions related to aging.
Explanation
As individuals age, several physiologic changes impact how drugs are absorbed, distributed, metabolized, and excreted. Factors such as reduced renal function, decreased hepatic metabolism, and lower serum albumin levels can alter a drug’s action in older adults. Recognizing these age-related changes is essential for ensuring safe and effective medication management.
Rationale for correct answer:
Genetics, smoking, diet, gender, other medications and diseases
These factors influence all phases of pharmacokinetics by altering enzyme function, gut health, protein binding, and organ performance. They can affect how drugs are absorbed, distributed, metabolized, or excreted, leading to variability in drug response.
Albumin levels diminish
Older adults often have lower serum albumin, which affects protein binding of drugs. Reduced binding increases the free active drug in circulation, influencing drug distribution and potentially enhancing drug effects or toxicity.
Decreased renal blood flow
Aging reduces renal perfusion and glomerular filtration rate, impairing the kidneys’ ability to excrete drugs. This can lead to drug accumulation and an increased risk of toxicity, especially with renally-excreted medications.
Muscle inactivity and changes in muscle mass
Loss of lean body mass and increased fat content in the elderly alters the volume of distribution. Lipophilic drugs may accumulate in fat stores, while hydrophilic drugs may have less tissue for distribution, affecting both onset and duration of action.
Take-home points:
- Aging reduces renal and hepatic function, increasing the risk of drug accumulation and toxicity.
- Lower albumin levels in older adults can lead to higher active drug levels in the bloodstream.
- Changes in body composition and lifestyle factors significantly impact how drugs are absorbed, distributed, and metabolized in the elderly.
While discussing with a mother the importance of administering furosemide orally to an infant with a cardiac abnormality, the nurse would recognize the need for further explanation if the mother makes which statement?
Explanation
Infants typically cannot swallow tablets safely due to their undeveloped swallowing reflexes and risk of aspiration. For this reason, medications are often given in liquid form using droppers or oral syringes, ensuring safer and more accurate administration. Understanding appropriate medication forms for infants is essential for safe pediatric care. Incorrect medication form can lead to choking, ineffective dosing, or refusal of treatment.
Rationale for correct answer:
B. “My baby will have no problem taking this tablet.”
Infants typically cannot swallow tablets safely. Oral medications for infants are usually in liquid form to ensure proper dosing and administration. This statement indicates a misunderstanding and requires correction.
Rationale for incorrect answers:
A. “I know that my baby needs this drug every day at approximately the same time.”
This reflects appropriate understanding of maintaining consistent drug levels through scheduled dosing, which is essential for managing fluid balance in infants with cardiac issues.
C. “I will check to make sure that the furosemide is working by monitoring the number of wet diapers.”
Monitoring urine output is a practical and important way to assess diuretic effectiveness in infants. Fewer wet diapers may indicate that the medication is not working effectively.
D. “I understand that my baby will continue to grow even while taking this drug.”
This shows understanding that while diuretics manage fluid overload, they do not interfere with normal growth if used appropriately and monitored regularly.
Take-home points:
- Infants cannot safely swallow tablets and should be given medications in liquid form.
- Furosemide effectiveness in infants can be monitored by tracking the number of wet diapers.
- Consistency in medication timing supports optimal therapeutic effect in pediatric cardiac care.
A pregnant woman asked a nurse at the obstetrician’s clinic how she could determine which drug was safe to take during pregnancy. What would be an appropriate response by the nurse?
Explanation
Medication safety during pregnancy is a critical consideration due to the potential effects on fetal development. Because few well-controlled studies exist on drug use in pregnancy, it is essential for pregnant individuals to consult their primary healthcare provider or pharmacist before taking any prescription or over-the-counter medications. This guidance helps minimize fetal risk while ensuring maternal health needs are appropriately addressed.
Rationale for correct answer:
B. “Because there are few studies done to determine the safe use of drugs during pregnancy, it is advisable to ask your primary healthcare provider or pharmacist regarding taking prescription and over-the-counter drugs.”
This is the safest and most accurate guidance. Because of limited clinical trials in pregnant populations, consulting a healthcare provider ensures that only drugs with a favorable risk-benefit profile are used.
Rationale for incorrect answers:
A. “Because there are few studies done to determine the safe use of drugs during pregnancy, it is okay to keep taking what was previously prescribed by your primary healthcare provider.”
This assumes that previously prescribed medications are automatically safe during pregnancy, which may not be true. Drug safety must be reassessed due to potential fetal risks.
C. “You are not to take any drugs during pregnancy.”
While minimizing drug use is ideal, some medications are necessary for maternal and fetal health. A blanket statement like this may prevent essential treatment.
D. “It would be fine to take over-the-counter drugs, since they never cause any issues.”
Many over-the-counter drugs can harm a developing fetus. Safety depends on the drug, trimester, and maternal condition. This advice could lead to misuse.
Take-home points:
- Pregnant individuals should consult a healthcare provider before taking any medication.
- Limited research on drug safety during pregnancy makes professional guidance essential.
- Over-the-counter medications are not automatically safe for use in pregnancy.
An expecting mother asks the nurse if it would be okay for her to take some cold medicine. What would be an appropriate response by the nurse?
Explanation
Medication use during pregnancy must be approached with caution due to the limited research on fetal safety. When an expecting mother inquires about taking cold medicine, it is important to explain that there are not many studies confirming the safety of various drugs during pregnancy. This uncertainty highlights the need to consult a healthcare provider before using any medication.
Rationale for correct answer:
A. “There are not a lot of studies done with regard to how safe medications are to take during pregnancy.”
This is the most appropriate response because clinical drug trials in pregnant women are limited due to ethical concerns. The nurse should promote caution and advise consultation with a healthcare provider before taking any medication during pregnancy.
Rationale for incorrect answers:
B. “I am sure it is safe to take, no problem.”
This is inappropriate and potentially unsafe. Safety cannot be assumed for any medication during pregnancy without evaluating the specific drug, gestational age, and maternal/fetal health status.
C. “I believe the cold medication is contraindicated for pregnant women.”
Stating that all cold medications are contraindicated is overly broad and inaccurate. Some may be safe while others are not, depending on their active ingredients and the trimester of pregnancy.
D. “Animal studies have revealed no evidence of harm to the fetus using these drugs.”
Animal studies do not guarantee safety in humans. Drugs deemed safe in animals may still pose risks during human pregnancy, so further clinical guidance is always necessary.
Take-home points:
- Medication safety in pregnancy is unclear due to limited human studies.
- Pregnant individuals should consult a healthcare provider before taking cold medicine.
- Animal studies do not reliably predict drug safety in human pregnancy.
The nurse recognized there are gender considerations to keep in mind with regard to drug actions.
Choose the most likely options for the information missing from the sentence below by selecting from the lists of options provided.
The gender considerations to keep in mind with regard to drug actions are that
Explanation
Answer:
The gender considerations to keep in mind with regard to drug actions are that women have greater proportion of body fat will affect distribution and that women have slower gastric emptying time will affect absorption, as well as that women have more active cytochrome P450 enzymes will affect metabolism.
Gender differences can significantly influence how drugs are processed in the body. Women generally have a greater proportion of body fat, which can alter drug distribution, especially for fat-soluble medications. Additionally, slower gastric emptying time in women can affect drug absorption, and more active cytochrome P450 enzymes may lead to faster or altered drug metabolism. These differences highlight the importance of considering gender when evaluating drug response and dosing.
Rationale for correct answer:
Women have greater proportion of body fat → distribution
Fat-soluble drugs distribute more widely and persist longer in individuals with higher body fat, which can influence the drug's duration and effectiveness in women.
Women have slower gastric emptying time → absorption
Slower gastric emptying can delay the time it takes for drugs to reach the small intestine, affecting the rate and possibly the extent of drug absorption.
Women have more active cytochrome P450 enzymes → metabolism
Cytochrome P450 enzymes are responsible for drug metabolism. Increased enzyme activity can lead to faster metabolism and potentially reduced efficacy or duration of action of some medications in women.
Take-home points:
- Women’s higher body fat percentage can influence the distribution of fat-soluble drugs.
- Slower gastric emptying in women may delay or alter drug absorption.
- More active cytochrome P450 enzymes in women can change the rate of drug metabolism.
Exams on Drug Action Across The Life Span
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Pharmacotherapy During Pregnancy
- Pharmacotherapy During Lactation
- Pediatric Pharmacotherapy
- Practice Exercise 1
- Pharmacotherapy Of Adolescents
- Pharmacotherapy In Young And Middle Adulthood
- Pharmacotherapy In Older Adults (65 And Over)
- Communicating With Patients With Sensory Impairments
- Practice Exercise 2
- Summary
- Nursing Insights
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Explain age-related pharmacokinetics.
- Identify teratogenic drug risks in pregnancy.
- Describe safe drug use during lactation.
- Outline pediatric medication administration principles.
- Discuss adolescent-specific pharmacologic concerns.
- Differentiate adult and older adult drug considerations.
- Recognize the impact of polypharmacy and organ decline.
- Apply communication strategies for sensory impairments.
Introduction
- Human growth and development stages—from infancy to old age—affect how drugs are absorbed, distributed, metabolized, and excreted.
Human development causes predictable physiological and anatomic changes (for example, changing body water and fat percentages, organ maturation, and declining organ function) that alter drug handling; a nurse who understands these changes can anticipate differences in drug onset, intensity, duration, and clearance across life stages. - Pharmacokinetics:
- Absorption: Absorption is affected by gastrointestinal motility, digestive enzyme activity, splanchnic blood flow, and gastric pH, and these variables change substantially with age and physiologic state; for example, neonates have higher gastric pH and delayed gastric emptying, whereas older adults often have slower motility and reduced blood flow.
- Distribution: Distribution depends on body composition (percentage of body fat and total body water), plasma protein levels (mainly albumin), and tissue perfusion; neonates’ higher total body water and lower fat stores change the distribution of hydrophilic versus lipophilic drugs compared with adults, and older adults’ increased fat and decreased water alter drug reservoirs and plasma concentrations.
- Metabolism: The liver is the principal organ for biotransformation, and enzyme activity varies with age and disease; neonates have immature hepatic enzyme systems, children may have increased metabolic rates for some enzymes, and older adults commonly have decreased hepatic blood flow and phase I enzyme activity.
- Excretion: The kidneys are the primary route for elimination of many drugs; neonatal renal function is immature and gradually matures over months, while aging causes declining glomerular filtration and tubular function that increases the risk for accumulation and toxicity if doses are not adjusted.
Pharmacotherapy During Pregnancy
- Pregnancy introduces many physiological changes that impact drug pharmacokinetics and pharmacodynamics.
Nurses must weigh maternal therapeutic needs against fetal risks: the growing uterus, altered circulatory dynamics, and hormonal shifts change drug absorption, distribution, metabolism, and excretion, and the placenta allows some drugs to reach the fetus while blocking or metabolizing others.

Physiological Changes Affecting Drug Therapy:
-
- Absorption: Progesterone-related smooth muscle relaxation and the growing uterus slow gastric emptying, which can delay the absorption of oral medications; increased gastric pH may reduce the solubility of some weak acids and thus alter their absorption.
- Distribution: Maternal plasma volume increases substantially during pregnancy (dilutional effect), which often reduces plasma drug concentrations for hydrophilic drugs; decreased plasma protein concentrations lead to a higher free (active) fraction of drugs, and increased adipose tissue during pregnancy alters distribution of lipophilic medications.
- Metabolism: Hepatic enzyme activity changes during pregnancy: some cytochrome P450 enzymes are induced (increasing clearance of drugs like some anticonvulsants), while others may be inhibited; these changes can necessitate dose adjustments for drugs with narrow therapeutic windows.
- Excretion: Renal blood flow and glomerular filtration rate increase—particularly in the second and third trimesters—leading to enhanced renal clearance of many drugs and, in some cases, the need for higher or more frequent dosing.
Teratogenic Risk Periods:
-
- Preimplantation (Weeks 1–2): The embryo is not yet attached to the uterine wall; teratogenic exposure during this "all-or-none" period typically either causes embryonic death or no effect because organogenesis has not yet begun.
- Embryonic Period (Weeks 3–8): This is the critical window of organogenesis; exposure to teratogens during these weeks can lead to major structural anomalies that are usually organ-specific depending on the timing of exposure.
- Fetal Period (Weeks 9–40): While the risk for gross structural defects declines, functional maturation continues, so teratogens may cause growth retardation, neurodevelopmental deficits, or impaired organ function rather than gross malformations; the thinning placental barrier later in pregnancy can increase fetal exposure to maternal drugs.
FDA Pregnancy Categories (classic A–X framework, for teaching):
-
- Category A: Well-controlled human studies show no fetal risk (e.g., prenatal vitamins with folic acid).
- Category B: Animal studies show no fetal risk but adequate human data are lacking, or animal studies show adverse effects that were not confirmed in human studies (e.g., many penicillins).
- Category C: Animal studies show adverse effects or no studies are available; drugs are used only if benefits justify potential risk (many SSRIs, some antihypertensives fall here depending on data).
- Category D: Positive evidence of fetal risk exists, but therapy may be given if benefits outweigh risks in serious conditions (e.g., certain anticonvulsants, ACE inhibitors in pregnancy are teratogenic in later trimesters).
- Category X: Contraindicated in pregnancy because studies in animals or humans demonstrate fetal abnormalities or evidence of fetal risk clearly outweighs any possible benefit (e.g., isotretinoin, thalidomide, warfarin).
Nursing insights in pregnancy:
-
- Ask all women of childbearing potential about pregnancy plans and possible pregnancy before prescribing or administering medications; ensure informed consent and counseling where appropriate.
- Prefer nonpharmacologic measures when feasible and safe; if drug therapy is necessary, choose agents with the best-known safety profile and monitor maternal and fetal effects carefully.
- Be familiar with pregnancy registries and consult obstetrics/pharmacy when prescribing drugs that are less well-studied in pregnancy.
- Educate pregnant patients about the risks of OTC, herbal, and recreational substances (e.g., alcohol, nicotine, cocaine) that can harm the fetus.
Pharmacotherapy During Lactation
- Breastfeeding mothers should use medications cautiously to protect infants from drug exposure through breast milk.
While many medications pass into breast milk in small amounts without causing harm, the nurse must evaluate the drug’s properties and the infant’s vulnerability (prematurity or organ immaturity increase risk).

Factors Affecting Drug Transfer into Breast Milk:
-
- Drug molecular size: Smaller molecules pass more readily into milk.
- Lipid solubility: Lipophilic drugs accumulate in milk fat and can reach higher milk concentrations.
- Protein binding: Highly protein-bound drugs are less likely to pass into milk; conversely, low protein binding increases transfer.
- Ionization and pH: Milk is slightly more acidic than plasma, so weakly basic drugs may become ion-trapped in milk.
- Half-life and active metabolites: Drugs with long half-lives or active metabolites pose higher risks because they can accumulate in the infant.
General Recommendations for Breastfeeding Mothers:
-
- Use medications only when essential and prefer alternatives with established safety in lactation.
- Give a dose immediately after breastfeeding (rather than before) or during the infant’s longest sleep interval to minimize drug concentration at the next feeding.
- Prefer drugs with short half-lives and high protein binding because they clear from the mother’s plasma more quickly and are less present in milk.
- Avoid drugs with long half-lives or active metabolites that could concentrate in the infant over time.
- Avoid herbal and OTC products unless they have known safety data for lactation and are recommended by the healthcare provider.
Examples of Drugs That Should Be Avoided or Used with Caution During Lactation:
-
- Codeine: Risk of severe neonatal respiratory depression and death in infants of mothers who are ultra-rapid metabolizers of codeine via CYP2D6, because higher morphine levels can accumulate in breast milk.
- Lithium: Crosses into milk and can cause T-wave changes and toxicity in the neonate, especially if the infant’s renal function is immature.
- Erythromycin (in neonates): Has been associated, rarely, with infantile hypertrophic pyloric stenosis.
- Valproic acid, phenytoin: Potential hematologic and hepatic effects in infants; caution and monitoring required.
- Indomethacin, naproxen (NSAIDs): Can affect neonatal platelet function and cause bleeding or other adverse effects.
- Dapsone, certain antifolates: Hemolytic anemia risk in G6PD-deficient infants or other specific conditions.

Nursing insights during lactation:
-
- Help mothers weigh maternal benefit against infant risk; consult lactation specialists and pharmacists for up-to-date milk-safety data.
- Teach timing strategies (dose after feed) and signs of infant adverse effects: excessive sleepiness, poor feeding, respiratory depression, jitteriness, rash, or poor weight gain.
- Encourage avoidance of alcohol, nicotine, and illicit drugs during breastfeeding.
- For high-risk medications, consider temporary cessation of breastfeeding (with support for milk expression) or switching to safer alternatives.
Pediatric Pharmacotherapy
- Children are not simply “small adults.”
Pediatric pharmacotherapy must consider organ immaturity, changing body composition, developmental behaviors, and the need for weight-based dosing. Dosing errors and formulation issues are common sources of adverse events in pediatrics, so careful calculation and administration technique are critical.
Age Groups (commonly used for dosing/management):
-
- Neonates: birth to 28 days — organ systems are immature and highly variable.
- Infants: 1 to 12 months — rapid physiologic changes and growth.
- Toddlers: 1 to 3 years — increased mobility and exploration; poisoning risk.
- Preschoolers: 3 to 5 years — growing understanding, still limited reasoning.
- School-age children: 6 to 12 years — increasing cooperation and ability to understand explanations.
-
- Oral medications should be directed to the inner cheek to reduce aspiration and allow the infant to swallow slowly; teaching caregivers correct technique reduces the risk of choking.
- IM injections should be administered in the vastus lateralis muscle because it is well-developed and avoids risk to major nerves; use the smallest safe needle and limit injected volume.
- IV access in neonates may require scalp or foot veins; those sites are often suitable for neonatal venipuncture and require meticulous antisepsis and securement.
- Rectal suppositories should be held in place briefly after insertion to allow for absorption; caregivers should be instructed to hold the buttocks together for several minutes.
- Pathophysiology: Neonatal gastric pH is higher (less acidic) and gastric emptying is slower, which affects absorption of certain drugs (e.g., acid-labile drugs may be absorbed better in neonates).
Toddlers
-
- High risk of accidental poisoning due to mouthing behavior; nurses must emphasize safe storage, child-resistant containers, and keeping medications out of reach.
- Mixing oral medications with a small amount of jam or syrup can mask taste and encourage full ingestion, but caregivers should avoid mixing medications with large volumes of milk or juice that the child might later avoid; always use minimal volumes to ensure the entire dose is consumed.
- Restraint for IM or IV procedures may be necessary; the parent’s comforting presence often improves cooperation, and the nurse should coach the parent on how to safely assist.
Preschoolers
-
- Use short, simple explanations and role-play to prepare preschoolers for procedures; allowing them to give a pill to a doll or to play-act the procedure reduces anxiety and improves cooperation.
- After walking for about a year, the ventrogluteal site may be used for IM injections because it is less painful and avoids the sciatic nerve; always assess muscle development before selecting the site.
School-age children:
-
- Offer limited choices (which medication first, which drink afterwards) to enhance the child’s sense of control and improve compliance.
- Chewable tablets or swallowing whole tablets become options for many school-aged children; provide technique coaching and supervised attempts when trying tablet swallowing.
Pediatric dosing principles:
-
- Dose calculations should be weight-based (mg/kg) and recalculated at each encounter; use the most current weight in kilograms and check decimal placement carefully.
- Consider age, organ maturity, and disease state when converting adult doses; consult pediatric dosing references rather than relying solely on simple scaling formulas.
- Be cautious with excipients (alcohol, benzyl alcohol, propylene glycol) in neonatal formulations because neonates metabolize these substances poorly.
Pharmacotherapy Of Adolescents
- Adolescence (approximately ages 13–16 in this guide) is a period of rapid physiologic, psychological, and social change that affects pharmacotherapy.
Adolescents may self-medicate, be influenced by peers, or conceal medication misuse; they also experience hormonal fluctuations that can alter pharmacokinetics and pharmacodynamics for some agents.
Key considerations for adolescent care:
-
- Common therapeutic needs include acne treatments, hormonal contraceptives, medications for menstrual irregularities, sports injuries management, and mental health pharmacotherapies such as antidepressants or anxiolytics.
- Sexual health education is essential; nurses should provide evidence-based information about contraception, STI prevention, and the safe use of medications for sexual health.
- Screen for eating disorders and hidden medication use, including laxatives and appetite suppressants, as these behaviors can significantly affect drug absorption and electrolyte balance.
- Substance use and abuse (alcohol, tobacco, inhalants, stimulants, anabolic steroids) must be addressed with nonjudgmental screening and education about risks and drug interactions.
- Respect privacy and autonomy while understanding local laws regarding consent and confidentiality; involve adolescents in decision-making and explain medication effects in an adult-appropriate manner.
- Adherence issues: adolescents may have poor understanding despite claiming otherwise; the nurse should thoroughly explain dosing, side effects, and the rationale for therapy and check comprehension.
Pharmacotherapy In Young And Middle Adulthood
- Young adults (18–40 years) generally have optimal organ function and robust pharmacokinetic capacity, but they commonly use medications for contraception, short-term infections, or mental health, and they frequently use OTC and herbal products that can interact with prescription medications.
- Middle adults (40–65 years) begin to show increased prevalence of chronic conditions such as hypertension, diabetes, obesity, and hyperlipidemia; lifestyle interventions are often first-line, but pharmacotherapy becomes more common and may be lifelong.
Nursing priorities for these groups:
-
- Assess for OTC and herbal supplement use and counsel about potential interactions with prescribed drugs.

-
- Encourage preventive strategies (exercise, diet, smoking cessation) and stress management to reduce reliance on medications when lifestyle changes are appropriate.
- Screen for chronic disease development and support early pharmacologic intervention when indicated to prevent long-term complications.
Pharmacotherapy In Older Adults (65 And Over)
- Older adults face multiple pharmacologic challenges because age-related physiologic changes alter each phase of drug action, and polypharmacy increases the risk of adverse interactions.
Age-Related Pharmacokinetic Changes:
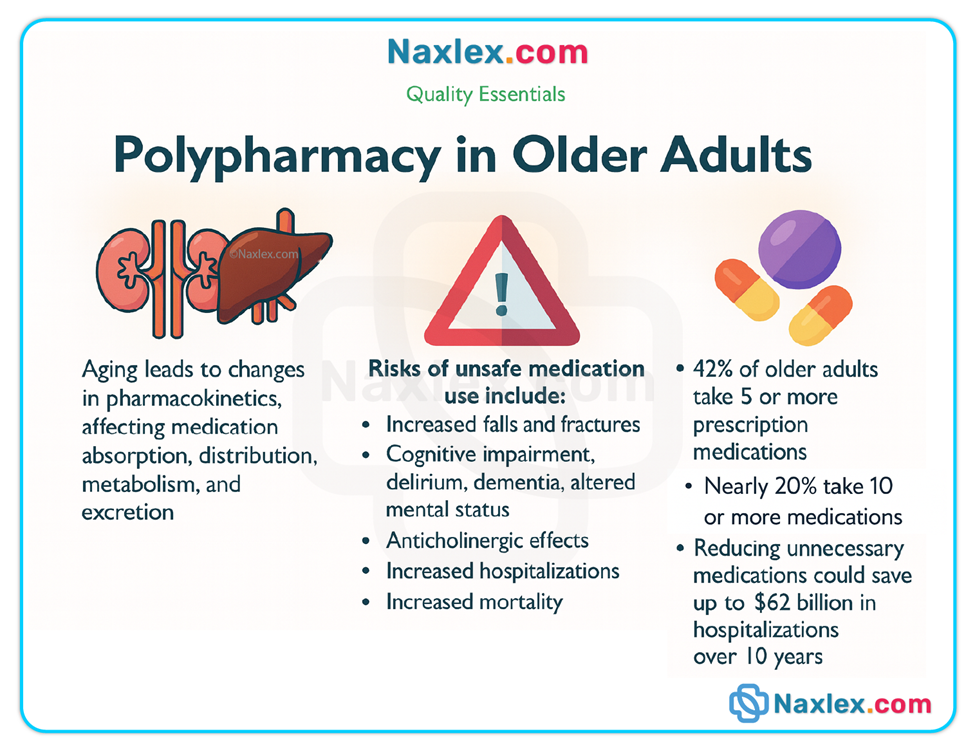
-
- Absorption: Gastric motility and splanchnic blood flow generally decrease with age, which can slow the rate (but usually not the extent) of absorption; drugs that require an acidic stomach for dissolution may dissolve more slowly.
- Distribution: Older adults typically have increased body fat and decreased total body water; lipophilic drugs (e.g., benzodiazepines, certain antidepressants) have a larger distribution and prolonged effects, whereas hydrophilic drugs reach higher plasma concentrations in a smaller aqueous volume. Reduced plasma albumin increases the free fraction of highly protein-bound drugs, increasing the risk of adverse effects.
- Metabolism: Hepatic mass and blood flow commonly decrease with age, reducing first-pass metabolism and phase I (oxidation/reduction) metabolic capacity; phase II (conjugation) reactions are often relatively preserved but individual variability exists, so half-lives may be prolonged.
- Excretion: Renal function declines with age—glomerular filtration rate and tubular secretion decrease—so drugs eliminated primarily by the kidneys (e.g., aminoglycosides, digoxin, many antidiabetics) require dose adjustments to avoid accumulation.
Polypharmacy:
-
- Older adults frequently take multiple medications prescribed by different providers, increasing the risk of drug–drug interactions, duplicate therapies, and adverse events. Regular medication reconciliation (especially at transitions of care) and deprescribing where appropriate reduce risk.

Clinical consequences & common adverse outcomes:
-
- Older adults are at increased risk for orthostatic hypotension, delirium, falls, bleeding, hypoglycemia, confusion, and drug accumulation due to impaired renal or hepatic function; these effects often present atypically and must be actively screened for.
Nursing insights for older adults:
-
- Start low and go slow—initiate therapy at lower doses and titrate slowly while monitoring for efficacy and adverse effects.
- Perform medication reconciliation at every care transition, and encourage the use of a single pharmacy to help identify interactions.
- Assess for ability to self-administer medications (vision, dexterity, cognition) and provide support tools (pill organizers, easy-open containers, large-print labels).
- Calculate creatinine clearance rather than relying solely on serum creatinine because reduced muscle mass can mask renal impairment; adjust drug dosing per renal function.
- Monitor labs and drug levels when using narrow therapeutic index drugs (e.g., warfarin, digoxin, certain anticonvulsants), and be vigilant for signs of toxicity.
Communicating With Patients With Sensory Impairments
Patients with Speech Impairments:
-
- Use simple yes/no questions, allow extended time for responses, and encourage written or drawn replies when possible.
- Validate understanding by paraphrasing the patient’s responses and watching nonverbal cues to ensure the message is accurate.
Patients with Visual Impairments:
-
- Provide clear, verbal step-by-step explanations of medication administration, ensure adequate lighting, offer tactile cues (e.g., pill boxes with different textures), and supply written materials in large print or audio formats as needed.
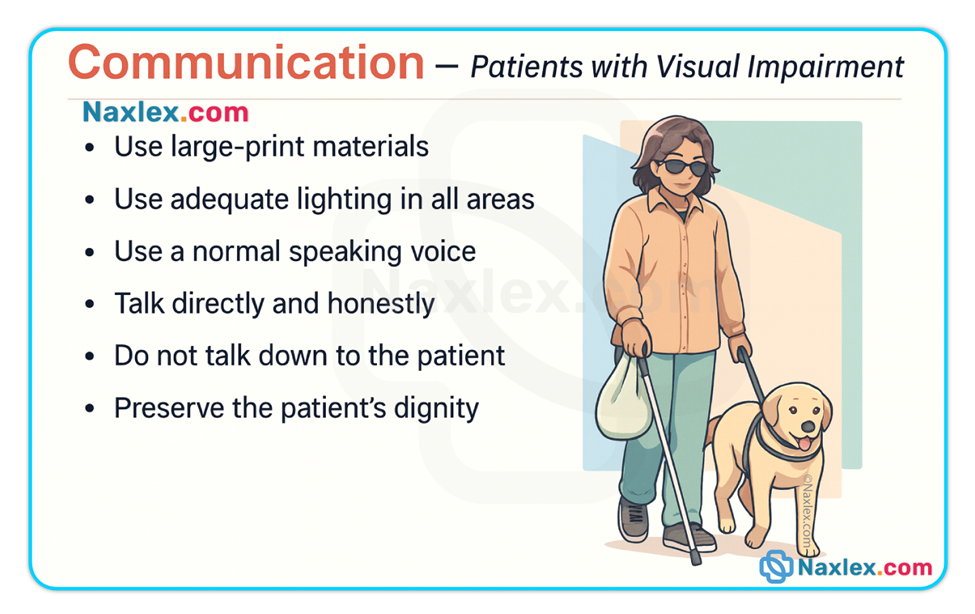
Patients with Hearing Impairments:
-
- Face the patient, speak clearly (without shouting), limit background noise, and use written instructions or sign language interpreters when available; document the best method of communication in the chart.
General communication tips:
-
- Always confirm comprehension using teach-back, document the communication method, and include family or caregivers as appropriate while respecting patient privacy and consent requirements.
Summary
- Drug pharmacokinetics and dynamics are strongly influenced by a patient’s age and developmental stage.
Because absorption, distribution, metabolism, and excretion change over the life span, dosing, route, formulation, monitoring, and patient education must be tailored for neonates, children, pregnant or lactating women, adolescents, adults, and older adults. - Each life stage requires unique approaches to medication administration, safety monitoring, and patient education.
For example, neonatal and infant dosing requires careful mg/kg calculations and attention to organ immaturity; pregnancy requires balancing maternal benefits and fetal risks and recognizing teratogenic windows; older adults require dose reduction and monitoring for drug accumulation and interactions. - Effective communication, family involvement, and individualized care plans help ensure safe and effective pharmacotherapy.
Nurses play a central role in educating patients and caregivers, performing accurate medication reconciliation, monitoring for adverse effects, and advocating for adjustments based on organ function, comorbidities, and social factors. - Monitoring for adverse effects is especially important in vulnerable groups such as neonates, pregnant individuals, and the elderly.
Use appropriate laboratory data, clinical observation, and drug level monitoring for narrow therapeutic index drugs to detect toxicity early. - Nurses play a vital role in preventing drug errors, managing polypharmacy, and advocating for patient-centered medication regimens.
By integrating life-span physiology, pharmacology principles, and clear communication strategies, nurses ensure safer and more effective pharmacotherapy for all patients.
Nursing Insights
- Verify patient identity, allergies, pregnancy status, and lactation status before administering medications.
- Calculate pediatric doses by weight (mg/kg) and cross-check with a second nurse or an approved dosing reference; double-check decimal placement.
- Confirm formulation and route — do not crush enteric-coated or extended-release tablets; use appropriate pediatric formulations when available.
- Assess organ function (renal: BUN/creatinine/CLcr; hepatic: AST/ALT/bilirubin) and adjust doses for impaired metabolism or excretion.
- Perform medication reconciliation at all care transitions and remove duplicates or unsafe combinations when possible.
- Educate patients and caregivers about timing with meals, expected side effects, signs of toxicity, and safe storage (especially for households with children).
- Monitor and document therapeutic response and adverse effects; obtain peak/trough levels as indicated for narrow therapeutic index drugs.
- Use teach-back and adapted communication for patients with sensory or speech impairments to confirm understanding.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drug Action Across The Life Span
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


