Please set your exam date
Seizures and Epilepsy
Study Questions
Practice Exercise 1
A patient is being evaluated for a diagnosis of epilepsy. Which of the following criteria, if present, would support this diagnosis?
Explanation
Epilepsy is a neurological disorder marked by recurrent seizures caused by abnormal electrical activity in the brain. It affects people of all ages and can vary in severity and type. Seizures may involve loss of awareness, convulsions, or subtle sensory disturbances. While it has many potential causes, including genetic factors, brain injury, and infections, epilepsy is often manageable with medication, lifestyle adjustments, and sometimes surgical intervention.
Rationale for correct answer:
B. The definition of epilepsy includes the occurrence of at least two unprovoked (or reflex) seizures occurring more than 24 hours apart. This criterion supports a diagnosis of epilepsy by demonstrating a persistent predisposition to generate epileptic seizures.
Rationale for incorrect answers:
A. A single provoked seizure due to a high fever is considered acute symptomatic and not epilepsy. Febrile seizures are often isolated and do not meet epilepsy diagnostic criteria.
C. While a brain tumor increases seizure risk, a single unprovoked seizure even with structural brain abnormality does not fulfill the standard definition unless recurrence risk is deemed high (>60%).
D. An abnormal EEG may suggest a predisposition to seizures, but a single seizure with such findings does not confirm epilepsy. EEG findings alone are not diagnostic without the appropriate clinical context.
Take pome points
- Epilepsy is typically diagnosed after two unprovoked seizures >24 hours apart.
- Provoked seizures (e.g., due to fever or intoxication) do not count toward the diagnosis.
- Diagnostic workup includes EEG and imaging, but clinical history is essential for confirmation.
A patient is brought to the emergency department after experiencing their first-ever generalized seizure. The seizure lasted for 45 seconds and resolved spontaneously. What is the nurse's highest priority action related to the diagnosis?
Explanation
In managing epilepsy, effective prioritization is essential to ensure safety, seizure control, and quality of life. The first priority is preventing injury during seizures through safety measures. Next is ensuring medication adherence to maintain therapeutic levels. Identifying and avoiding seizure triggers is crucial, along with providing education to patients and caregivers. Regular neurological evaluations and individualized care plans support long-term stability and well-being.
Rationale for correct answer:
C. A detailed history is the most important step after a first seizure. Understanding the context, characteristics, duration, triggers, and recovery phase of the event is essential to differentiate epileptic seizures from other causes (e.g., syncope, psychogenic non-epileptic seizures), and to guide further evaluation and management.
Rationale for incorrect answers:
A. Lumbar puncture is only indicated if there are signs of CNS infection (e.g., fever, nuchal rigidity, altered mental status), which are not present here.
B. Prophylactic anti-seizure medication is not routinely started after a first seizure unless the risk of recurrence is high (e.g., structural lesion, abnormal EEG).
D. It is premature to diagnose epilepsy or offer support group referrals after a single, unprovoked seizure, especially without further diagnostic confirmation.
Take pome points
- A detailed clinical history is the cornerstone of seizure evaluation.
- Not all first seizures are due to epilepsy—thorough assessment is needed.
- Immediate treatment or labeling the patient with epilepsy is not appropriate without supporting evidence.
Practice Exercise 2
A 75-year-old patient with a history of hypertension and atrial fibrillation is admitted to the hospital after a new-onset focal seizure. The nurse recognizes which of the following is the most likely underlying risk factor?
Explanation
A focal seizure is a type of epileptic seizure that begins in a specific area of the brain. It may cause symptoms such as muscle twitching, unusual sensations, or altered consciousness, depending on the affected region. Focal seizures are classified as either focal aware (consciousness retained) or focal impaired awareness. Diagnosis involves EEG and neuroimaging, and treatment includes antiseizure medications, lifestyle changes, and sometimes surgery for drug-resistant cases.
Rationale for correct answer:
C. In elderly patients, ischemic stroke is one of the most common causes of new-onset focal seizures. The presence of atrial fibrillation and hypertension places this patient at high risk for embolic or thrombotic strokes, which can lead to seizure activity due to acute cortical irritation or chronic gliosis.
Rationale for incorrect answers:
A. TBI from 30 years ago is a remote insult; while old injuries can be associated with seizures, they are a far less likely cause than a recent vascular event in an elderly patient.
B. Cerebral palsy is a childhood condition that may include seizures but is not a new risk factor for late-onset seizures in an elderly person without a diagnosis.
D. Febrile seizures in childhood are typically benign and do not significantly increase the long-term risk of adult-onset epilepsy unless associated with other neurological issues.
Take pome points
- Ischemic stroke is a leading cause of late-onset epilepsy in older adults.
- Risk factors such as atrial fibrillation and hypertension elevate the stroke risk and therefore secondary seizure risk.
- Seizures from remote childhood conditions are less likely to be causative in elderly-onset seizures.
A nurse is teaching a community group about post-traumatic epilepsy (PTE). The nurse should include which of the following as significant risk factors for developing PTE?
Explanation
Post-traumatic epilepsy (PTE) is a form of epilepsy that develops following a traumatic brain injury (TBI). It is caused by structural brain damage that disrupts normal electrical activity, leading to recurrent seizures. PTE may occur weeks to years after the injury and is more likely with severe or penetrating head trauma. Management involves antiseizure medications, monitoring for seizure activity, and rehabilitation to support cognitive and physical recovery.
Rationale for correct answer:
B. The severity of TBI is the most consistent predictor of post-traumatic epilepsy. Moderate to severe TBIs, especially those involving cortical damage, hemorrhage, or penetrating injuries, are strongly associated with a higher risk of late-onset seizures and epilepsy.
Rationale for incorrect answers:
A. Skull fracture alone does not always increase PTE risk unless it is associated with brain contusion, hemorrhage, or penetrating injury.
C. While location can affect seizure type, the severity of injury plays a more significant role in predicting whether epilepsy will occur. No specific lobe alone universally predicts PTE.
D. Post-traumatic amnesia >24 hours is a marker of injury severity, but not an independent predictor of epilepsy. It's used in classification but not as a direct risk factor alone.
Take pome points
- PTE risk increases with moderate to severe TBIs.
- Skull fracture and amnesia are indirect indicators but not primary determinants.
- Education on TBI severity is essential when discussing seizure risk after trauma.
Practice Exercise 3
A nurse is observing a patient who suddenly stops talking, stares blankly into space, and makes a few small chewing motions with their mouth. The patient does not respond when the nurse calls their name. After about 30 seconds, the patient blinks, looks at the nurse, and appears unaware of what just happened. This is a classic presentation of which type of seizure?
Explanation
A focal impaired awareness seizure is a type of focal seizure where the person experiences altered consciousness or impaired awareness during the event. It originates in one part of the brain, often the temporal lobe, and may cause automatisms like lip-smacking, wandering, or repetitive movements. Afterward, the person may feel confused or fatigued. Diagnosis includes EEG and imaging, and treatment involves antiseizure medications or, in some cases, surgical intervention.
Rationale for correct answer:
D. Focal impaired awareness seizures originate in one hemisphere and involve altered consciousness. The presence of automatisms such as chewing motions, blank staring, and post-event confusion strongly supports this diagnosis, especially when the patient has no memory of the event.
Rationale for incorrect answers:
A. Tonic-clonic seizures are generalized and involve full-body stiffening and jerking, typically accompanied by a post-ictal phase but not focal automatisms alone.
B. Atonic seizures cause sudden loss of muscle tone and collapse, without automatisms or a staring phase.
C. Absence seizures are usually brief (under 10 seconds), occur mainly in children, and do not typically include automatisms or prolonged unresponsiveness.
Take pome points
• Focal impaired awareness seizures often involve behavioral automatisms and impaired awareness.
• They are more common in adults and typically last 30 seconds to 2 minutes.
• Absence and atonic seizures differ in age group, duration, and motor features.
A patient is experiencing a tonic-clonic seizure. Which of the following clinical manifestations would the nurse expect to observe during this event? Select all that apply
Explanation
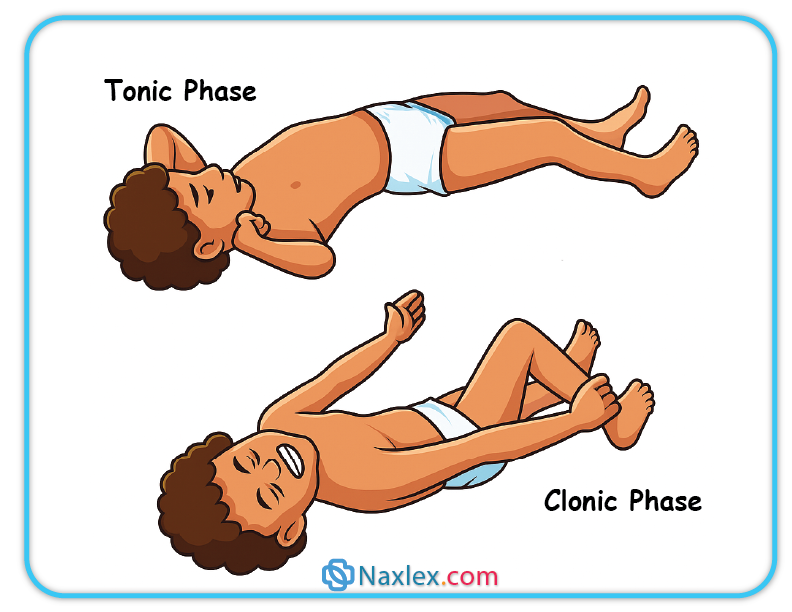
A tonic-clonic seizure, previously known as a grand mal seizure, is a type of generalized seizure that affects the entire brain. It begins with a tonic phase, causing muscle stiffening, followed by a clonic phase of rhythmic jerking. The person often loses consciousness and may experience incontinence or tongue biting. Afterward, a postictal state of confusion and fatigue follows. Management includes antiseizure medications, safety precautions, and regular neurological monitoring.
Rationale for correct answers:
B. The clonic phase of a tonic-clonic seizure includes rhythmic jerking of the limbs, which may last from seconds to minutes.
C. The tonic phase involves initial muscle stiffening, often with a cry or fall, as muscles contract forcefully.
E. A post-ictal period is common following tonic-clonic seizures and is characterized by drowsiness, confusion, and headache due to cerebral recovery.
Rationale for incorrect answers:
A. Sudden loss of tone is a hallmark of atonic seizures, not tonic-clonic ones, which progress through stiffening and jerking phases.
D. Brief shock-like jerks are typical of myoclonic seizures, not tonic-clonic seizures which involve sustained and patterned movements.
Take pome points
• Tonic-clonic seizures progress through tonic (stiffening) and clonic (jerking) phases.
• The post-ictal state is essential for diagnosis and patient monitoring.
• Recognizing the pattern helps in prompt and appropriate response.
Practice Exercise 4
A nurse is preparing to care for a patient with a new-onset seizure. The patient is stable and alert. Which diagnostic step is the highest priority for the nurse to facilitate?
Explanation
In managing epilepsy, effective prioritization is essential to ensure safety, seizure control, and quality of life. The first priority is preventing injury during seizures through safety measures. Next is ensuring medication adherence to maintain therapeutic levels. Identifying and avoiding seizure triggers is crucial, along with providing education to patients and caregivers. Regular neurological evaluations and individualized care plans support long-term stability and well-being.
Rationale for correct answer:
C. A detailed history is the most critical first step in evaluating a new-onset seizure. Information about what occurred before, during, and after the seizure helps differentiate epileptic seizures from mimics (e.g., syncope or psychogenic events) and guides further diagnostic testing.
Rationale for incorrect answers:
A. An anti-seizure medication is not urgently needed in a patient who is stable and not actively seizing, especially after a single event.
B. While a CT scan may be indicated, it is not the immediate priority if the patient is stable. The scan may follow history-taking, particularly if trauma or structural lesions are suspected.
D. Long-term video-EEG monitoring is generally reserved for complex or unclear seizure cases and is not appropriate for initial evaluation.
Take pome points
• History-taking is foundational in seizure evaluation and influences all subsequent diagnostic steps.
• Immediate medication or imaging is not required unless the patient is unstable or at risk.
• Early identification of seizure features supports appropriate diagnostic direction.
A nurse is reviewing a patient's diagnostic workup for recurrent seizures. Which of the following are primary purposes for ordering a brain MRI?
Explanation
Imaging in seizures is essential for identifying structural brain abnormalities that may cause or contribute to epilepsy. The most commonly used modalities are MRI and CT scans. MRI is preferred for its high sensitivity in detecting lesions, tumors, scarring, or vascular malformations. Imaging helps guide treatment decisions, especially in new-onset seizures or focal seizures, and is crucial in planning for surgical intervention in drug-resistant epilepsy cases.
Rationale for correct answers:
B. MRI is used to detect structural abnormalities such as tumors, malformations, or cortical scarring that may be the underlying cause of epilepsy. Identifying such causes is critical for treatment planning.
D. MRI can reveal surgically treatable conditions like mesial temporal sclerosis, tumors, or vascular malformations, which may offer curative options in refractory epilepsy.
Rationale for incorrect answers:
A. Epilepsy is a clinical diagnosis; imaging helps identify underlying causes but does not alone confirm the condition.
C. Electrical activity is assessed through EEG, not MRI, which provides anatomical—not functional—data.
Take pome points
• Brain MRI is essential in epilepsy workup to detect underlying structural causes.
• MRI findings may influence medical versus surgical treatment strategies.
• EEG complements MRI by evaluating brain function, not structure.
A nurse is educating a patient and family about atonic seizures. Which of the following statements indicates an accurate understanding of this type of seizure?
Explanation
Atonic seizures, also known as drop attacks, involve a sudden and brief loss of muscle tone, which can result in the person collapsing or falling unexpectedly. These seizures typically last less than 15 seconds and do not always involve loss of consciousness. Because of the risk of injury from falls, helmets may be recommended for safety.
Rationale for Correct Answer:
B. Atonic seizures are characterized by a sudden loss of muscle tone, often leading to falls
This is the hallmark feature of atonic seizures. The sudden loss of postural control is what differentiates them from other seizure types.
Rationale for Incorrect Answers:
A. Atonic seizures typically involve rhythmic jerking of the extremities
This describes clonic seizures, not atonic seizures.
C. Atonic seizures usually begin with an aura and progress to loss of consciousness
Auras are more common in focal seizures, and loss of consciousness is variable in atonic seizures.
D. Atonic seizures cause stiffening of the body followed by limb jerking
This is characteristic of tonic-clonic seizures, not atonic seizures.
Take home points
- Atonic seizures involve sudden muscle tone loss, often leading to falls.
- Patients may require protective gear to prevent injury.
- These seizures are brief and may or may not involve altered consciousness.
- Differentiation from other seizure types is crucial for accurate diagnosis and safety planning.
Practice Exercise 5
A patient suddenly begins to have a tonic-clonic seizure while sitting in a chair. Which nursing action is appropriate?
Explanation
In managing epilepsy, effective prioritization is essential to ensure safety, seizure control, and quality of life. The first priority is preventing injury during seizures through safety measures. Next is ensuring medication adherence to maintain therapeutic levels. Identifying and avoiding seizure triggers is crucial, along with providing education to patients and caregivers. Regular neurological evaluations and individualized care plans support long-term stability and well-being.
Rationale for correct answer:
A. Timing the seizure is essential because it provides critical information on the seizure’s duration, which helps determine if further intervention (such as pharmacologic treatment for status epilepticus) is needed. Monitoring the time also guides the evaluation of therapeutic response and supports timely communication with the health care team.
Rationale for incorrect answers:
B. Turning the patient onto their side, while helpful for maintaining airway post-seizure, is not the highest priority during the seizure.
C. Restraining a patient during a tonic-clonic seizure increases the risk of injury to both the patient and the nurse and is not recommended.
D. Placing a tongue blade in the patient’s mouth is contraindicated as it can cause dental or soft tissue injury and obstruct the airway.
Take pome points
• Timing the seizure provides vital data for clinical decision-making.
• Airway maintenance is important, but interventions like repositioning should be done when safe.
• Avoid actions that increase risk of harm during active convulsions.
A nurse is educating a patient about long-term management of their epilepsy with anti-seizure drugs (ASDs). Which of the following statements should the nurse include in the teaching plan? Select all that apply
Explanation
Client education in epilepsy is vital for promoting seizure control, safety, and treatment adherence. Clients should understand their medication regimen, recognize potential seizure triggers, and implement lifestyle modifications such as stress reduction and adequate sleep. Education should cover first aid for seizures, when to seek emergency care, and the importance of regular follow-up. Empowering clients with knowledge enhances self-management and improves overall quality of life.
Rationale for correct answers:
B. Taking the medication at the same time every day maintains a consistent therapeutic level in the bloodstream, which is crucial for preventing breakthrough seizures.
C. Regular blood level monitoring is important to ensure that the drug concentration stays within the therapeutic range and minimizes toxicity.
E. Missing a dose can lower the drug levels, significantly increasing the risk of breakthrough seizures, which is why adherence to the regimen is critical.
Rationale for incorrect answers:
A. ASDs must be taken consistently regardless of perceived seizure activity; waiting for a prodrome undermines the therapeutic regimen and could lead to uncontrolled seizures.
D. Stopping the medication abruptly, even in the face of side effects, can precipitate withdrawal seizures and should only be done under medical supervision.
Take pome points
• Consistency in medication timing is essential for effective seizure control.
• Regular monitoring helps balance efficacy and safety in long-term ASD therapy.
• Adherence to the prescribed regimen significantly reduces the risk of breakthrough seizures.
A nurse is providing discharge instructions to a female client who has a prescription for phenytoin (Dilantin). Which of the following information should the nurse include?
Explanation
Phenytoin (Dilantin) is an antiepileptic drug used to control seizures. It has a narrow therapeutic index, meaning small changes in dosage or blood levels can result in toxicity or loss of seizure control. Therefore, taking the medication at the same time every day is critical to maintain stable blood levels and optimize seizure management.
Rationale for Correct Answer:
C. Take the medication at the same time every day: Maintaining a consistent dosing schedule is essential for drugs like phenytoin, which require stable serum levels. Irregular intake can lead to breakthrough seizures or toxicity.
Rationale for Incorrect Answers:
A. Consider taking oral contraceptives when on this medication: Phenytoin reduces the effectiveness of hormonal contraceptives. Women should be advised to use non-hormonal methods or consult their provider for alternatives.
B. Watch for receding gums when taking the medication: While gingival hyperplasia is a known side effect of phenytoin, it is not the most critical discharge teaching point. The priority here is medication adherence and timing.
D. Provide a urine sample to determine therapeutic levels of the medication: Phenytoin levels are monitored through blood tests, not urine. Blood testing ensures the dose remains within the therapeutic range (typically 10–20 mcg/mL).
Take home points
- Consistency in dosing time is crucial for phenytoin’s effectiveness.
- Phenytoin lowers the efficacy of hormonal contraceptives.
- Monitor phenytoin levels using blood, not urine.
- Be aware of side effects like gingival hyperplasia, but prioritize adherence.
A nurse is completing discharge teaching to a client who has seizures and received a vagal nerve stimulator to decrease seizure activity. Which of the following information should the nurse include in the teaching?
Explanation
Clients with a vagal nerve stimulator (VNS) can use a magnet to activate the device manually when they sense a seizure aura. This manual activation can help abort or lessen the severity of a seizure. VNS is used in clients with refractory epilepsy who do not respond adequately to medication.
Rationale for Correct Answer:
C. Place a magnet over the implantable device when an aura occurs: Patients are taught to swipe a magnet (provided by the manufacturer) over the implanted device when they feel a seizure coming. This action stimulates the vagus nerve, potentially interrupting the seizure.
Rationale for Incorrect Answers:
A. The use of a microwave to heat food is permitted: While technically not harmful, this is not the most relevant teaching point during discharge about the VNS device. Microwaves do not interfere with VNS function, but this option lacks priority relevance.
B. Inform a provider to order only a MRI when a scan is needed: MRIs are generally contraindicated or require caution in patients with VNS. If needed, MRI safety protocols must be followed strictly, and not all MRI sites are safe depending on the magnet strength. This makes the statement inaccurate as written.
D. The use of ultrasound diathermy for pain management is recommended: Ultrasound diathermy is contraindicated in clients with implanted electrical devices like a VNS. It may interfere with the stimulator or cause tissue damage, making this answer incorrect and potentially dangerous.
Take home points
- Vagal nerve stimulators can be activated manually with a magnet at the onset of an aura.
- MRI and diathermy require special precautions or are contraindicated in patients with VNS.
- Teaching should focus on how to use the device effectively and avoid sources of interference or harm.
Practice Exercise 6
A patient's seizure has lasted for 6 minutes without stopping. The nurse recognizes that this is a medical emergency requiring immediate intervention to prevent brain damage. This condition is known as:
Explanation
Status epilepticus is a medical emergency characterized by a seizure lasting more than 5 minutes or repeated seizures without full recovery of consciousness between them. It can be life-threatening and may result in brain damage if not treated promptly. Common causes include medication nonadherence, stroke, and head trauma. Immediate management involves benzodiazepines, followed by antiseizure medications, airway support, and identifying the underlying cause to prevent recurrence.
Rationale for correct answer:
C. Status epilepticus is defined as a seizure lasting longer than 5 minutes or recurrent seizures without full recovery of consciousness in between. It is a neurological emergency because prolonged seizure activity can lead to permanent brain injury, systemic complications, and even death if not treated promptly.
Rationale for incorrect answers:
A. Atony refers to loss of muscle tone, not a prolonged seizure state.
B. Focal impaired awareness seizures typically last 30 seconds to 2 minutes and do not meet the duration criteria for status epilepticus.
D. Post-ictal amnesia is a period of confusion or memory loss following a seizure, not a continuous seizure condition.
Take pome points
• Seizures lasting longer than 5 minutes are considered status epilepticus.
• Immediate intervention is needed to prevent neuronal damage and complications.
• Nurses must recognize and escalate care rapidly when seizure duration exceeds 5 minutes.
The nurse is providing education to a patient with a new diagnosis of epilepsy about the potential complications. Which of the following psychosocial issues should the nurse discuss? Select all that apply
Explanation
Epilepsy complications can impact both physical health and quality of life. Common risks include injuries during seizures, status epilepticus, and sudden unexpected death in epilepsy (SUDEP). Long-term complications may involve cognitive impairment, depression, and social stigma. Poorly controlled seizures can interfere with education, employment, and independence. Effective management focuses on seizure control, medication adherence, and addressing psychosocial needs to minimize complications and improve outcomes.
Rationale for correct answers:
A. Depression and anxiety are common in people with epilepsy due to neurological changes, medication effects, and psychosocial stressors, and should be regularly assessed and addressed.
C. Social isolation and stigma often result from misunderstanding of epilepsy and fear of seizures occurring in public, which can negatively impact self-esteem and relationships.
D. SUDEP is a rare but serious complication that patients and families should be informed about, especially if seizures are uncontrolled or frequent.
E. Employment challenges and driving restrictions due to safety concerns can significantly affect quality of life and independence in people with epilepsy.
Rationale for incorrect answer:
B. While joining a support group is a helpful strategy, it is an intervention, not a psychosocial complication of epilepsy.
Take home points
• Epilepsy can have significant emotional, social, and occupational consequences.
• Education should include both medical and psychosocial risks to promote holistic care.
• Nurses play a vital role in reducing stigma and supporting self-management strategies
Comprehensive Questions
The nurse is preparing to admit a newly diagnosed patient experiencing tonic-clonic seizures.
What could the nurse delegate to unlicensed assistive personnel (UAP)?
Explanation
In clients experiencing tonic-clonic seizures, the nurse must ensure that emergency equipment is readily available to maintain airway safety during and after a seizure. Tasks that are non-complex, do not require clinical judgment, and are part of basic supportive care can be safely delegated to UAPs. The nurse should retain responsibilities involving assessment, education, and decision-making.
Rationale for correct answer:
C. Obtain the suction equipment from the supply cabinet: This is a straightforward, non-clinical task that a UAP can perform. Having suction equipment at the bedside is essential in case the client vomits or has excessive secretions during or after a seizure.
Rationale for incorrect answers:
A. Complete the admission assessment: This involves data collection and interpretation, which are nursing responsibilities and cannot be delegated to a UAP.
B. Explain the call system to the patient: Teaching and verifying understanding fall under the nurse’s role. UAPs should not be assigned tasks involving patient education.
D. Place a padded tongue blade on the wall above the patient’s bed: This reflects an outdated and unsafe practice. Nothing should be inserted into the mouth during a seizure, and padded tongue blades are not used in modern seizure precautions.
Take pome points
- Delegate non-clinical, routine tasks like equipment retrieval to UAPs.
- The RN retains responsibility for assessment, education, and clinical decision-making.
- Padded tongue blades are no longer used in seizure precautions due to safety concerns.
How do generalized seizures differ from focal seizures?
Explanation
Generalized seizures differ from focal seizures in that they involve bilateral, synchronous epileptic discharges that affect the entire brain from the onset. In contrast, focal seizures (also called partial seizures) begin in one hemisphere and may either remain localized or progress to a bilateral tonic-clonic seizure. Generalized seizures often result in loss of consciousness and involve motor or non-motor symptoms such as tonic-clonic movements or absence episodes.
Rationale for correct answer:
D. Generalized seizures have bilateral synchronous epileptic discharges affecting the whole brain at onset of the seizure: This is the defining feature of generalized seizures. They involve simultaneous discharge of neurons across both hemispheres from the beginning of the event, leading to loss of consciousness and global motor involvement.
Rationale for incorrect answers:
A. Focal seizures are confined to one side of the brain and remain focal in nature: While focal seizures begin in one hemisphere, they may spread and become generalized, so this statement is only partially true and not the key distinction.
B. Generalized seizures result in loss of consciousness whereas focal seizures do not: Some focal seizures do impair consciousness (focal impaired awareness seizures), so this is an oversimplification.
C. Generalized seizures result in temporary residual deficits during the postictal phase: Postictal deficits (e.g., Todd's paralysis) are more often associated with focal seizures, not generalized ones.
Take pome points
- Generalized seizures begin with bilateral brain involvement and typically cause loss of consciousness.
- Focal seizures originate in one hemisphere and may or may not affect awareness.
- The key distinguishing feature is the site and pattern of onset—generalized seizures are bilateral at onset, while focal ones are unilateral.
Which type of seizure occurs in children, is also known as a petit mal seizure, and consists of a staring spell that lasts for a few seconds?
Explanation
Typical absence seizures, formerly called petit mal seizures, are most commonly seen in children and are characterized by brief episodes of staring and loss of awareness lasting only a few seconds. These seizures often go unrecognized because they are subtle, involve no convulsions, and may occur multiple times a day. The child typically resumes normal activity immediately afterward, with no postictal confusion.
Rationale for correct answer:
C. Typical absence: This type of seizure fits the description exactly—occurs in children, lasts a few seconds, and involves a sudden lapse in consciousness with a blank stare. The child may stop speaking or doing an activity momentarily and then continue as if nothing happened. It's classically described as "daydreaming" and is easily missed without EEG monitoring.
Rationale for incorrect answers:
A. Atonic: These seizures involve sudden loss of muscle tone, leading to falls or head drops. They do not primarily involve staring spells.
B. Simple focal: These seizures involve localized brain activity and do not cause a loss of consciousness. Staring is not a typical feature.
D. Atypical absence: These may also involve staring but are longer in duration, have more pronounced changes in tone, and typically occur in children with developmental delays or cognitive impairments. The onset and resolution are less abrupt than in typical absence seizures.
Take pome points
- Typical absence seizures are brief, involve staring spells, and occur mostly in children.
- They were previously called petit mal seizures.
- They differ from atonic, focal, and atypical absence seizures in duration, symptoms, and population affected.
The patient is diagnosed with complex focal seizures. Which characteristics are related to complex focal seizures? Select all that apply
Explanation
Complex focal seizures (also known as focal impaired awareness seizures) originate in one hemisphere of the brain and are associated with altered consciousness. They may involve automatisms such as lip smacking, picking at clothing, or repetitive gestures. Additionally, patients may experience distorted sensory perceptions, including changes in memory, emotions, or sensations. These seizures often affect the temporal lobe, a region linked to emotion and sensory integration.
Rationale for correct answers:
C. Psychomotor seizures with repetitive behaviors and lip smacking: These are classic signs of automatisms seen in complex focal seizures.
D. Altered memory, sexual sensations, and distortions of visual or auditory sensations: These are typical of temporal lobe involvement, common in complex focal seizures.
F. Often involves behavioral, emotional, and cognitive functions with altered consciousness: Complex focal seizures frequently disrupt cognitive and emotional functions due to impaired consciousness.
Rationale for incorrect answers:
A. Formerly known as grand mal seizure: This refers to generalized tonic-clonic seizures, not complex focal seizures.
B. Often accompanied by incontinence or tongue or cheek biting: These signs are more common in generalized tonic-clonic seizures, not focal seizures.
E. Loss of consciousness and stiffening of the body with subsequent jerking of extremities: This describes a tonic-clonic seizure, which is generalized, not focal in origin.
Take pome points
- Complex focal seizures involve altered consciousness and may include automatisms.
- They often affect the temporal lobe, leading to emotional and sensory disturbances.
- Unlike generalized seizures, they start in one hemisphere and may not involve full-body convulsions.
Which type of seizure is most likely to cause death for the patient?
Explanation
Tonic-clonic status epilepticus is a life-threatening neurologic emergency characterized by a prolonged tonic-clonic seizure lasting more than 5 minutes, or repeated seizures without full recovery of consciousness between episodes. This condition can lead to permanent brain damage, respiratory failure, metabolic disturbances, and death if not treated promptly. Immediate intervention with benzodiazepines and other anticonvulsants is critical to reduce morbidity and mortality.
Rationale for correct answer:
D. Tonic-clonic status epilepticus: This is the most dangerous seizure type and requires emergency treatment. Prolonged seizure activity can cause hypoxia, acidosis, hyperthermia, and systemic complications that may be fatal if not addressed urgently.
Rationale for incorrect answers:
A. Subclinical seizures: These are seizures without outward physical manifestations, often seen on EEG. While clinically important, they are not immediately life-threatening.
B. Myoclonic seizures: These involve brief, shock-like muscle jerks and are usually not fatal, though they may occur in epilepsy syndromes with serious outcomes.
C. Psychogenic seizures: Also called pseudoseizures, these are non-epileptic events typically related to psychological factors. They do not cause physiologic brain damage or death.
Take pome points
- Tonic-clonic status epilepticus is the most dangerous seizure type and can be fatal without prompt intervention.
- Emergency management includes airway protection, benzodiazepines, and IV antiepileptics.
- Other seizure types may require monitoring but are less likely to cause death.
A patient admitted to the hospital following a generalized tonic-clonic seizure asks the nurse what caused the seizure. What is the best response by the nurse?
Explanation
The best response offers a clear, factual, and general explanation about how seizures occur without making assumptions or sounding dismissive. Seizures result from sudden, abnormal electrical discharges in the brain, which may be triggered by factors such as fever, trauma, electrolyte imbalances, or idiopathic causes. Providing this information helps educate the patient while remaining open to further diagnostic evaluation.
Rationale for correct answer:
C. “In seizures, some type of trigger causes sudden, abnormal bursts of electrical brain activity.” This answer explains the basic pathophysiology of seizures in a simple and accurate way. It is informative, nonjudgmental, and appropriate for a patient unfamiliar with the condition. It opens the door for further discussion and education based on the patient’s needs.
Rationale for incorrect answers:
A. “So many factors can cause epilepsy that it is impossible to say what caused your seizure.”
While partially true, this response is vague and dismissive, and may increase anxiety without offering useful information.
B. “Epilepsy is an inherited disorder. Does anyone else in your family have a seizure disorder?” This suggests a narrow cause (genetic) and may lead to unnecessary concern. Not all epilepsy is inherited.
D. “Scar tissue in the brain alters the chemical balance, creating uncontrolled electrical discharges.” This describes one potential cause (post-traumatic or post-surgical epilepsy), but it’s too specific and may not apply to this patient’s situation.
Take pome points
- Seizures result from abnormal electrical activity in the brain and can have various causes.
- Nurses should provide clear, simple explanations to help educate and reassure the patient.
- Avoid giving overly specific or dismissive answers that may confuse or distress the patient.
A patient with a seizure disorder is being evaluated for surgical treatment of the seizures. The nurse recognizes that what is one of the requirements for surgical treatment?
Explanation
Before surgical treatment for epilepsy is considered, patients must undergo an adequate trial of antiepileptic drug (AED) therapy usually involving two or more appropriate medications without achieving satisfactory seizure control. Surgery is often reserved for medication-refractory epilepsy, especially when seizures originate from a single, well-defined area of the brain that can be safely resected.
Rationale for correct answer:
B. An adequate trial of drug therapy that had unsatisfactory results: This is the primary prerequisite for epilepsy surgery. Only patients who fail to achieve seizure control despite optimal medical therapy are considered for surgical intervention. This step ensures that surgery is reserved for those with medically intractable epilepsy.
Rationale for incorrect answers:
A. Identification of scar tissue that is able to be removed: While identifying a resectable focus (such as a lesion or scar tissue) is important, it is not the initial requirement. The failure of drug therapy comes first.
C. Development of toxic syndromes from long-term use of antiseizure drugs: This may prompt a change in medication but is not a direct indication for surgery.
D. The presence of symptoms of cerebral degeneration from repeated seizures: While chronic seizures can cause neurologic decline, cerebral degeneration is not a requirement or a typical indication for surgery. Surgical treatment aims to prevent further damage.
Take pome points
- Surgery is considered in drug-resistant epilepsy, after a failed trial of adequate drug therapy.
- Candidates must have seizures localized to one resectable brain area.
- Surgery aims to improve seizure control and quality of life when medications are ineffective.
The nurse teaches the patient taking antiseizure drugs that this method is most commonly used to measure compliance and monitor for toxicity:
Explanation
Blood testing for drug levels is the most reliable and commonly used method to assess patient compliance and monitor for potential toxicity of antiseizure medications. Most antiepileptic drugs (AEDs) have defined therapeutic serum concentration ranges, and maintaining levels within this range helps ensure efficacy while minimizing adverse effects. Drug levels also help clinicians adjust doses as needed and detect noncompliance, overuse, or drug interactions.
Rationale for correct answer:
C. Blood testing for drug levels: Monitoring serum levels of AEDs allows for assessment of both therapeutic effectiveness and potential toxicity. It helps ensure that patients are taking the medication consistently and provides a quantitative measure for dose adjustments.
Rationale for incorrect answers:
A. A daily seizure log: While helpful in tracking seizure frequency and medication effects, it is subjective and does not assess drug levels or toxicity directly.
B. Urine testing for drug levels: Urine levels are less reliable for monitoring therapeutic ranges and are not typically used for routine management of epilepsy.
D. Monthly electroencephalography (EEG): EEG measures electrical brain activity and can detect seizure patterns but is not used to monitor medication compliance or toxicity.
Take pome points
- Blood level monitoring is the standard for assessing AED compliance and toxicity.
- Therapeutic drug ranges help guide dosing and reduce side effects.
- Seizure logs and EEGs are useful tools but do not replace blood level monitoring for this purpose.
When teaching a patient with a seizure disorder about the medication regimen, what is most important for the nurse to emphasize?
Explanation
The most critical teaching point for patients on antiseizure medications is that they should never stop the medication abruptly, as this can lead to rebound seizures, which may be more frequent, intense, and difficult to control. Abrupt withdrawal can even lead to status epilepticus, a life-threatening condition. Patients should be instructed to take their medications exactly as prescribed and consult their healthcare provider before making any changes.
Rationale for correct answer:
C. Stopping the medication abruptly may increase the intensity and frequency of seizures: This is a life-saving teaching point. Sudden withdrawal from antiepileptic drugs can lead to serious complications, including status epilepticus. Gradual tapering under medical supervision is essential if discontinuation is necessary.
Rationale for incorrect answers:
A. The patient should increase the dosage of the medication if stress is increased: Patients should never self-adjust their medication dose. This can cause toxicity or inadequate control. Any changes must be directed by a healthcare provider.
B. Most over-the-counter and prescription drugs are safe to take with antiseizure drugs: Many drug interactions can occur with AEDs. Patients should be advised to consult their provider before taking any new medications.
D. If gingival hypertrophy occurs, the drug should be stopped and the health care provider notified: Gingival hyperplasia is a known side effect of phenytoin, but the drug should not be stopped abruptly. Good oral hygiene and provider notification are appropriate, but discontinuation should be physician-directed.
Take pome points
- Abrupt discontinuation of antiseizure medication can lead to severe rebound seizures or status epilepticus.
- Patients should be taught to take medications consistently and as prescribed.
- Medication adjustments or additions must be approved by the healthcare provider to avoid interactions or complications.
The nurse finds a patient in bed having a generalized tonic-clonic seizure. During the seizure activity, what actions should the nurse take? Select all that apply
Explanation
During a generalized tonic-clonic seizure, the nurse’s priority is to maintain airway patency, prevent injury, and provide supportive care. This includes loosening restrictive clothing, turning the patient to the side to reduce aspiration risk, and protecting the head from trauma. It is essential not to insert objects into the mouth or restrain the patient, as these actions can cause more harm than good.
Rationale for correct answers:
A. Loosen restrictive clothing: Helps improve airflow and reduces the risk of choking or aspiration.
B. Turn the patient to the side: Promotes drainage of secretions or vomit and reduces risk of aspiration during the postictal phase.
C. Protect the patient’s head from injury: Use a pillow, rolled towel, or hands to cushion the head and prevent trauma during convulsions.
Rationale for incorrect answers:
D. Place a padded tongue blade between the patient’s teeth: This is an outdated and dangerous practice. Inserting anything into the mouth during a seizure can lead to broken teeth, aspiration, or airway obstruction.
E. Restrain the patient’s extremities to prevent soft tissue and bone injury: Restraints should not be used during a seizure, as they can lead to musculoskeletal injury or worsen the seizure.
Take pome points
- During a seizure, focus on airway protection, injury prevention, and supportive positioning.
- Do not insert objects into the mouth or restrain the patient.
- Turning the patient to the side and protecting the head are safe and effective interventions.
Following a generalized tonic-clonic seizure, the patient is tired and sleepy. What care should the nurse provide?
Explanation
After a generalized tonic-clonic seizure, it is common for the patient to enter a postictal state characterized by fatigue, confusion, headache, or drowsiness. The appropriate nursing action is to allow the patient to rest while ensuring a safe environment and monitoring for airway patency and recovery. Forcing stimulation or unnecessary suctioning can be harmful or distressing unless clinically indicated.
Rationale for correct answer:
B. Allow the patient to sleep as long as he feels sleepy: Rest is part of the normal recovery process after a seizure. The postictal phase may last minutes to hours. Allowing uninterrupted rest helps the brain recover from the seizure activity.
Rationale for incorrect answers:
A. Suction the patient before allowing him to rest: Suctioning should only be performed if there is evidence of airway obstruction, excess secretions, or vomiting. Routine suctioning without need is unnecessary and invasive.
C. Stimulate the patient to increase his level of consciousness: Stimulating a postictal patient is inappropriate and may increase agitation or confusion. The brain needs time to recover naturally.
D. Check the patient’s level of consciousness every 15 minutes for an hour: Frequent checks may disrupt needed rest. While initial monitoring is important, once the patient is stable and breathing well, letting them rest is the priority.
Take pome points
- The postictal phase includes fatigue and drowsiness—rest is therapeutic and expected.
- Do not perform invasive interventions like suctioning unless indicated.
- Unnecessary stimulation may delay recovery and increase confusion.
- Ensure the patient is in a safe position (on the side) and allow uninterrupted rest.
During the diagnosis and long-term management of a seizure disorder, what should the nurse recognize as one of the major needs of the patient?
Explanation
One of the major psychosocial challenges faced by individuals with epilepsy is coping with societal stigma and negative attitudes. Despite advances in treatment and understanding of seizure disorders, many people with epilepsy still experience discrimination, isolation, or misunderstanding in personal, educational, and professional settings. Addressing these emotional and social concerns is a critical part of holistic nursing care and patient support.
Rationale for correct answer:
B. Coping with the effects of negative social attitudes toward epilepsy: This is a well-documented concern for people with seizure disorders. Fear of having a seizure in public and the misconceptions about epilepsy can cause anxiety, low self-esteem, and reduced quality of life. Support, education, and advocacy are key roles of the nurse in helping patients navigate these challenges.
Rationale for incorrect answers:
A. Managing the complicated drug regimen of seizure control: While medication adherence is important, most seizure regimens are not overly complex. Psychosocial issues often present a greater long-term challenge than drug management.
C. Adjusting to the very restricted lifestyle required by a diagnosis of epilepsy: Although some activity modifications (e.g., avoiding swimming alone, driving restrictions) may be necessary, many patients can lead full and active lives with proper control. The idea of a “very restricted lifestyle” is inaccurate and outdated.
D. Learning to minimize the effect of the condition in order to obtain employment: Employment concerns are valid, but this choice emphasizes concealment rather than support and adaptation. Addressing stigma directly is a more holistic and empowering approach.
Take pome points
- Stigma and social isolation remain significant issues for people with epilepsy.
- Nurses play a vital role in supporting emotional health, promoting self-advocacy, and providing education to reduce stigma.
- Holistic care involves addressing both medical and psychosocial needs.
A nurse is assessing a client who has a seizure disorder. The client reports he thinks he is about to have a seizure. Which of the following actions should the nurse implement? Select all that apply
Explanation
When a patient indicates a seizure is imminent, the nurse must take preventive safety measures to minimize injury. These actions aim to create a safe environment and ensure dignity, while avoiding harmful interventions like restraint.
Rationale for correct answers:
A. Provide privacy: This maintains the patient’s dignity during and after the seizure, especially if in a public or shared area.
B. Ease the client to the floor if standing: This prevents falls and injuries if the seizure begins while the patient is upright.
C. Move furniture away from the client: Clearing the area reduces the risk of the patient striking nearby objects during the seizure.
D. Loosen the client’s clothing: Loosening tight clothing, especially around the neck, supports airway patency and comfort.
E. Protect the client’s head with padding: Placing a pillow, folded towel, or similar soft item under the head can reduce the risk of head trauma during convulsions.
Rationale for incorrect answer:
F. Restrain the client: Never restrain a patient during a seizure. This can cause musculoskeletal injury, increased agitation, or soft tissue damage. The priority is to allow the seizure to occur safely without interference.
Take pome points
- Always prioritize safety and dignity before and during seizure activity.
- Use protective measures such as easing the patient to the floor, removing hazards, and padding the head.
- Do not restrain or insert anything into the patient's mouth during a seizure.
A nurse is caring for a client who just experienced a generalized seizure. Which of the following actions should the nurse perform first?
Explanation
After a generalized seizure, the nurse’s first priority is maintaining a patent airway and ensuring the client’s safety. Positioning the client on their side helps prevent aspiration by allowing secretions to drain and keeping the tongue from obstructing the airway.
Rationale for correct answer:
A. Keep the client in a side-lying position: This action supports airway clearance, promotes ventilation, and helps prevent aspiration of saliva, blood, or emesis. It is the most immediate and critical step following a seizure.
Rationale for incorrect answers:
B. Monitor the client’s vital signs: While important for ongoing assessment, vital signs should be taken after airway and positioning needs are addressed.
C. Reorient the client to the environment: Reorientation is necessary once the client regains full consciousness, but it is not the immediate priority.
D. Check the client for injuries: This should be done after ensuring the client is safe and stable, especially after the airway has been secured.
Take pome points
- The side-lying position is critical post-seizure to protect the airway and prevent aspiration.
- Airway, breathing, and circulation (ABCs) always guide priority nursing actions.
- Secondary assessments like vital signs and injury checks should follow stabilization.
A nurse is reviewing trigger factors that can cause seizures with a client who has a new diagnosis of generalized seizures. Which of the following information should the nurse include in this review? Select all that apply
Explanation
Clients with generalized seizures must be aware of common seizure triggers, which include sleep deprivation, stimulants like caffeine, flashing lights, and hyperventilation or hypoventilation. Aerobic exercise is generally safe and beneficial unless specifically contraindicated. However, aerosol hairsprays are not known to be protective or recommended and may even irritate the respiratory tract in some individuals.
Rationale for correct answers:
A. Overwhelming fatigue should be avoided: Fatigue and sleep deprivation are common seizure triggers. Clients should maintain a regular sleep schedule.
B. Caffeinated products should be removed from the diet: Caffeine can increase neuronal excitability and lower the seizure threshold. Reducing or eliminating it is often recommended.
C. Looking at flashing lights should be limited: Photostimulation, like flashing or flickering lights, can trigger seizures, especially in clients with photosensitive epilepsy.
D. Aerobic exercise may be performed: Regular moderate aerobic activity can improve overall health and reduce seizure frequency. It should be encouraged unless it poses a personal risk.
E. Episodes of hypoventilation should be limited: Breathing irregularities like hyperventilation or hypoventilation can provoke seizures, especially in children or individuals with generalized epilepsy.
Rationale for incorrect answer:
D. Aerobic exercise may be performed: The nurse should instruct the client to decrease physical activity, which may help to avoid triggering a seizure.
E. Episodes of hypoventilation should be limited: The nurse should instruct the client to limit excess hyperventilation, which may trigger a seizure by stimulating abnormal electrical neuron activity.
F. Use of aerosol hairspray is recommended: Aerosol products are not seizure-preventative and could be harmful if inhaled excessively or in enclosed spaces.
Take home points
- Seizure triggers include fatigue, caffeine, flashing lights, and abnormal breathing patterns.
- Aerobic exercise is generally safe and encouraged.
- Avoid unnecessary aerosol exposures—they are not protective and could be irritating.
Exams on Seizures and Epilepsy
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Differentiate between the terms "seizure" and "epilepsy."
- Identify key risk factors associated with the development of seizures and epilepsy.
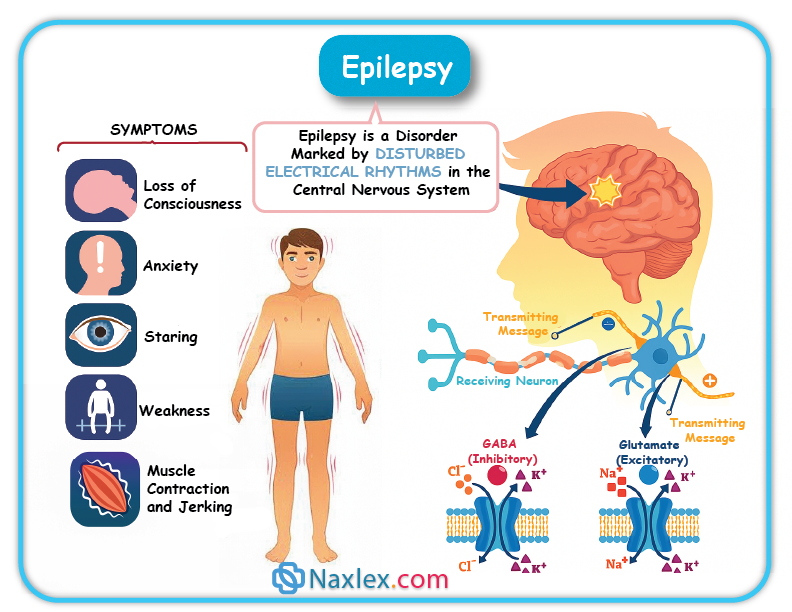
- Describe the pathophysiology of a seizure.
- Distinguish between different classifications of seizures, including focal and generalized seizures.
- Recognize the clinical manifestations of various seizure types.
- Explain the diagnostic procedures used to confirm a seizure disorder.
- Outline the nursing and collaborative management of a patient experiencing a seizure.
- Develop an appropriate nursing care plan for a patient with epilepsy, including health promotion and patient education.
- Discuss the pharmacological and surgical treatment options for epilepsy.
Introduction
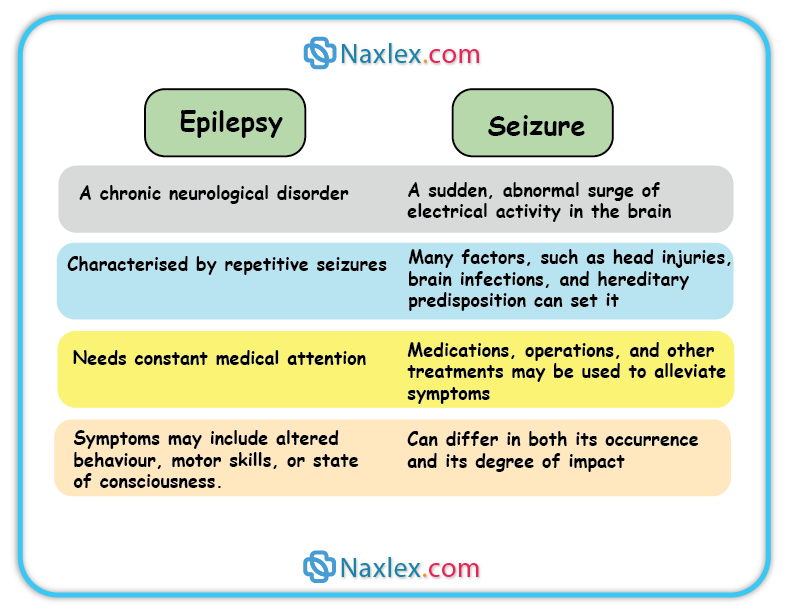
A seizure is a sudden, uncontrolled electrical disturbance in the brain. It is the clinical manifestation of abnormal, synchronous electrical activity in neurons. Seizures are not a disease in themselves but rather a symptom of an underlying neurological problem.
Epilepsy is a chronic neurological disorder characterized by recurrent, unprovoked seizures. A person is diagnosed with epilepsy after having at least two unprovoked seizures more than 24 hours apart, or one unprovoked seizure with a high probability of having more.
The distinction is crucial: a single seizure may be caused by a temporary condition, whereas epilepsy implies a long-term condition that requires ongoing management.
Risk Factors
Risk factors for seizures and epilepsy can be categorized into those that increase the likelihood of a first seizure and those that contribute to the development of chronic epilepsy.
 Genetic Factors:
Genetic Factors:
- A family history of seizures or epilepsy.
- Genetic mutations that affect brain development or function (e.g., Dravet syndrome).
Brain Injury and Pathology:
- Stroke: Ischemic or hemorrhagic strokes are a leading cause of new-onset seizures, especially in older adults.
- Brain Tumors: Both benign and malignant tumors can irritate brain tissue, leading to seizures.
- Traumatic Brain Injury (TBI): The risk of developing epilepsy increases with the severity of the TBI. Post-traumatic epilepsy can occur months or even years after the initial injury.
- Infections: Meningitis, encephalitis, and viral or parasitic infections (e.g., neurocysticercosis) that cause brain inflammation or damage.
- Congenital Abnormalities: Developmental brain malformations.
Metabolic and Systemic Conditions:
- Electrolyte Imbalances: Severe hyponatremia or hypocalcemia.
- Hypoglycemia: Critically low blood sugar levels.
- High Fever: Particularly in infants and young children, leading to febrile seizures.
- Toxins: Exposure to lead, carbon monoxide, or other toxic substances.
- Drug or Alcohol Withdrawal: Abrupt cessation of alcohol, benzodiazepines, or barbiturates can trigger seizures.
Other Factors:
- Cerebral Palsy: Seizures are a common comorbidity in individuals with cerebral palsy.
- Alzheimer's Disease: There is an increased incidence of seizures in people with Alzheimer's, particularly in advanced stages.
Clinical Manifestations
The clinical manifestations of a seizure depend on the type of seizure and the area of the brain where the abnormal electrical activity originates. The International League Against Epilepsy (ILAE) classifies seizures into two main categories: focal onset and generalized onset.
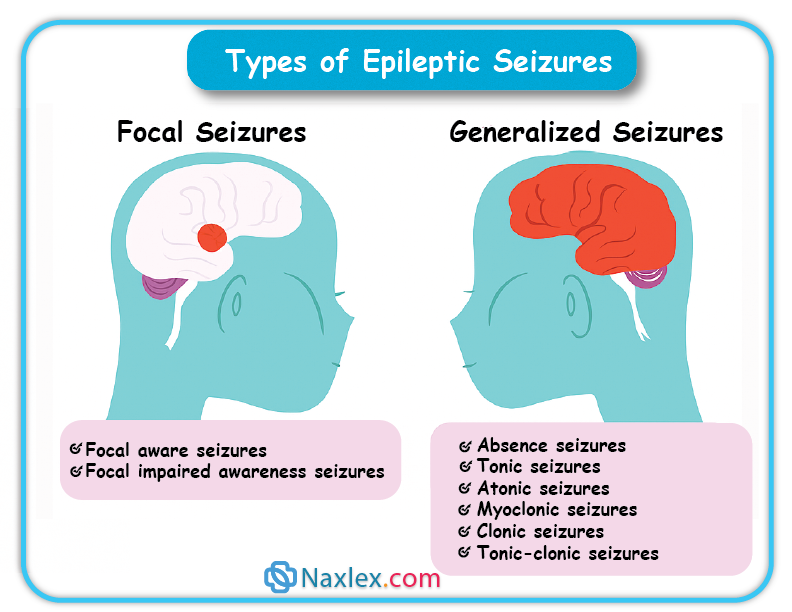 Focal-Onset Seizures (Partial Seizures)
Focal-Onset Seizures (Partial Seizures)
These seizures originate in one hemisphere of the brain. The manifestations reflect the function of the brain area affected.
Focal Aware Seizures (Simple Partial Seizures)
-
- The patient remains conscious and aware.
- Symptoms are often brief and can include:
- Motor symptoms: Jerking of a limb (e.g., finger, hand), muscle stiffness, or head turning.
- Sensory symptoms: Numbness, tingling, auditory or visual hallucinations (e.g., seeing flashing lights), or strange smells (e.g., burning rubber).
- Autonomic symptoms: Feeling of a rising sensation in the stomach (epigastric aura), pallor, sweating, or flushing.
Focal Impaired Awareness Seizures (Complex Partial Seizures)
-
- The patient's consciousness is impaired, and they may appear to be "zoning out" or "daydreaming."
- Often preceded by a focal aware seizure (aura).
- Characterized by automatisms, which are repetitive, purposeless behaviors. Examples include:
- Lip-smacking or chewing.
- Picking at clothing.
- Wandering or fumbling with objects.
- Inability to respond to verbal commands.
- The patient will not remember the event (post-ictal amnesia).
Generalized-Onset Seizures
These seizures involve both sides of the brain from the beginning. Consciousness is typically lost or impaired.
Tonic-Clonic Seizures (Grand Mal)
-
- The most common type.
- Tonic Phase (10-20 seconds): Stiffening of the body, including the arms and legs. The patient may let out a cry or scream as air is forced out of the lungs. The patient loses consciousness and falls to the ground.
- Clonic Phase (30-40 seconds): Rhythmic jerking of the extremities. The patient may bite their tongue or cheek and have frothy saliva.
- Post-ictal Phase: The patient is often confused, drowsy, and may have a headache and muscle soreness. They have no memory of the seizure.
 Absence Seizures (Petit Mal)
Absence Seizures (Petit Mal)
-
- Most common in children.
- Brief (3-30 seconds), sudden loss of consciousness.
- The patient stares into space and appears to be "daydreaming."
- Eyelid fluttering or minor facial movements may occur.
- The patient returns to a normal state immediately after the seizure and is unaware that it occurred.
Myoclonic Seizures
-
- Brief, shock-like jerks of the muscles.
- Can affect one part of the body or the entire body.
- Consciousness is not usually impaired.
Atonic Seizures (Drop Attacks)
-
- Sudden, brief loss of muscle tone.
- The patient suddenly goes limp and falls to the ground, often resulting in head injuries.
- Consciousness is briefly impaired.
Diagnostics
The diagnostic workup includes a combination of subjective and objective data.
- Health History:
- Detailed description of the seizure event (e.g., what happened before, during, and after).
- Information from witnesses is critical to differentiate between seizure types.
- Past medical history, including head trauma, infections, family history of seizures, and any relevant comorbidities.
- Electroencephalogram (EEG):
- The most important diagnostic tool for seizures.
- Measures and records the electrical activity of the brain.
- An abnormal EEG may show spike-and-wave discharges or other patterns consistent with seizures.
- Note: A normal EEG does not rule out epilepsy, as the brain's electrical activity may be normal between seizures.
- Neuroimaging:
- Magnetic Resonance Imaging (MRI): The gold standard for detecting structural abnormalities in the brain, such as tumors, vascular lesions, or congenital malformations, that may be causing the seizures.
- Computed Tomography (CT) Scan: Can be used to rule out acute causes of a seizure, such as a hemorrhage or brain tumor, especially in an emergency setting.
- Blood Tests:
- Complete blood count (CBC), serum electrolytes, blood glucose, and liver and kidney function tests to rule out metabolic disorders or systemic diseases as the cause.
- Toxicology screening to check for drug or alcohol use.
- Lumbar Puncture:
- May be performed if a central nervous system infection (e.g., meningitis, encephalitis) is suspected.
Management
Effective management of seizures and epilepsy involves both immediate care during a seizure event and long-term collaborative care to prevent future seizures and improve quality of life.
Acute Management of a Seizure
The primary goal is to ensure patient safety and prevent injury.
- During the Seizure:
- Ensure Airway and Safety:
- Loosen clothing around the neck.
- Turn the patient to their side (recovery position) to prevent aspiration.
- Do NOT restrain the patient.
- Do NOT put anything in the patient’s mouth.
- Protect the head from injury by placing a soft object (e.g., a folded jacket) under it.
- Monitor and Time: Note the time the seizure began and how long it lasts. Observe the characteristics of the seizure (e.g., where it started, body parts involved, eye movements).
- Ensure Airway and Safety:
- After the Seizure (Post-Ictal Phase):
- Keep the patient on their side.
- Perform a neurological assessment (level of consciousness, vital signs, pupil response).
- Reorient the patient as they regain consciousness.
- Document all details of the seizure and the patient’s response.
Long-Term Collaborative Management
Pharmacological Therapy:
- Anti-Seizure Drugs (ASDs) or Anti-Epileptic Drugs (AEDs):
- The primary treatment for epilepsy. The goal is to control seizures with minimal side effects.
- Therapy typically begins with a single drug (monotherapy), which is titrated to achieve a therapeutic level. If this is ineffective, a second drug may be added or substituted.
- Key Principles:
- Adherence: Patients must take their medication consistently as prescribed. Missed doses are a common cause of breakthrough seizures.
- Serum Drug Levels: Regular monitoring of drug levels may be necessary to ensure the dose is therapeutic and not toxic.
- Common Medications:
- Phenytoin (Dilantin): Can cause gingival hyperplasia, hirsutism, and requires careful monitoring of serum levels.
- Carbamazepine (Tegretol): Can cause bone marrow suppression.
- Levetiracetam (Keppra): Less drug-drug interactions, but can cause mood changes.
- Valproate (Depakote): Broad-spectrum, but can cause liver toxicity and is teratogenic.
Surgical Therapy
- An option for patients with medically refractory epilepsy (seizures that do not respond to medication).
- Anterior Temporal Lobe Resection: The most common surgical procedure. Removes the seizure focus.
- Vagal Nerve Stimulation (VNS): An implanted device that sends electrical impulses to the vagus nerve to reduce seizure frequency and intensity.
Other Therapies
- Ketogenic Diet: A high-fat, low-carbohydrate, and adequate-protein diet that forces the body to use fat for energy. Used primarily in children with difficult-to-control epilepsy.
Nursing Management & Education
- Promote Safety:
- Advise the patient to avoid triggers (e.g., fatigue, alcohol, stress).
- Caution the patient about driving and operating heavy machinery until seizures are well-controlled.
- Patient Education:
- Teach the patient and family about the importance of medication adherence and the potential side effects.
- Advise them on what to do during a seizure (seizure first aid).
- Encourage the use of a medical alert bracelet.
Complications
Complications of seizures and epilepsy can be severe, impacting both physical health and quality of life.
Acute Complications
- Status Epilepticus:
- A medical emergency defined as a seizure lasting more than 5 minutes or repeated seizures without a return to consciousness.
- This condition requires immediate intervention to prevent irreversible brain damage, respiratory failure, and death.
- Emergency Management: Administration of rapid-acting benzodiazepines (e.g., lorazepam, diazepam) to stop the seizure, followed by a long-acting AED (e.g., phenytoin, levetiracetam).
- Injury:
- Physical injuries are common during the seizure due to a fall or violent muscle contractions.
- Common injuries include head trauma, lacerations, burns, and fractures.
Chronic Complications
- Psychosocial Issues:
- Depression and Anxiety: The unpredictable nature of seizures and the stigma associated with epilepsy can lead to significant psychological distress.
- Social Isolation: Patients may avoid social situations out of fear of having a seizure or feeling embarrassed.
- Discrimination: Stigma can lead to discrimination in school or the workplace.
- Cognitive Dysfunction:
- Frequent seizures and the long-term use of AEDs can lead to memory loss, difficulty concentrating, and other cognitive impairments.
- Sudden Unexpected Death in Epilepsy (SUDEP):
- The most serious complication.
- Defined as the sudden, unexplained death of a patient with epilepsy.
- The cause is not fully understood but may be related to respiratory failure or cardiac dysrhythmias during or after a seizure.
Summary
- A seizure is a temporary electrical disturbance in the brain, while epilepsy is a chronic disorder of recurrent unprovoked seizures.
- Risk factors include genetic factors, brain injuries, tumors, infections, and metabolic disorders.
- Clinical manifestations are classified as either focal (originating in one side of the brain) or generalized (affecting both sides).
- Diagnosis is primarily based on a detailed history, an EEG, and an MRI.
- Acute management prioritizes patient safety, while long-term management involves anti-seizure medications and, in some cases, surgery.
- Serious complications include status epilepticus, physical injury, and Sudden Unexpected Death in Epilepsy (SUDEP).
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Seizures and Epilepsy
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


