Please set your exam date
Obsessive-Compulsive and Related Disorders
Study Questions
Practice Exercise 1
Which nursing diagnosis reflects the intrapersonal theory of the etiology of obsessive-compulsive disorder?
Explanation
Intrapersonal theoryof obsessive-compulsive disorder (OCD) emphasizes internal psychological conflict, particularly the role of unconscious processes and personality structures. Rooted in psychodynamicmodels, this theory suggests that OCD symptoms arise from unresolved internal conflicts between the id, ego, and superego. The superego, representing moral conscience, may become excessively punitive, leading to guilt and anxiety. This theory contrasts with biological or behavioral models by focusing on internal drives and defense mechanisms.
Rationale for correct answers
1.A punitivesuperego reflects intrapsychic conflict where excessive guilt and moral rigidity drive compulsive behaviors. This aligns with intrapersonal theory, which centers on internal psychological structures and unconscious defense mechanisms.
Rationale for incorrect answers
2.Avoidanceis a behavioral concept, not intrapersonal. It reflects external coping strategies rather than internal psychological conflict, making it inconsistent with intrapersonal theory.
3.Serotoninimbalance is a biological explanation. It involves neurochemical dysfunction rather than internal psychological dynamics, thus not fitting the intrapersonal framework.
4.Conditioningis a behavioral theory mechanism. It explains OCD through learned associations, not through unconscious intrapsychic processes, making it incompatible with intrapersonal theory.
Take Home Points
- Intrapersonal theory attributes OCD to internal psychological conflict, especially involving the superego.
- Behavioral and biological models focus on external stimuli and neurochemical imbalances, respectively.
- OCD symptoms may symbolically express unresolved unconscious guilt or anxiety.
- Differentiating OCD etiology requires understanding psychodynamic, behavioral, and biological frameworks.
A nurse is admitting a client diagnosed with obsessive-compulsive disorder (OCD) who has ordering issues. Which intervention should the nurse delegate to ancillary staff?
Explanation
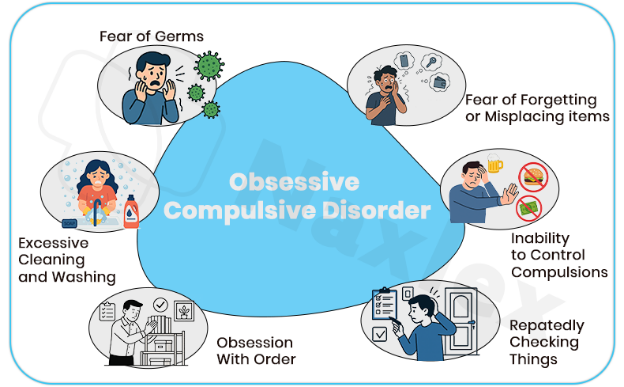
Obsessive-compulsive disorder (OCD)is a chronic psychiatric condition characterized by intrusive thoughts(obsessions) and repetitive behaviors(compulsions) performed to reduce anxiety. In clients with ordering compulsions, the need for symmetry and precise arrangement can dominate behavior, often interfering with basic tasks. These rituals are driven by distress and not pleasure and disrupting them can escalate anxiety. OCD is classified under its own diagnostic category in DSM-5, separate from anxiety disorders.
Rationale for correct answers
1.Assisting with storing belongings is a task-orientedactivity that can be delegated to ancillary staff, provided it’s done in a way that respects the client’s compulsive ordering needs. This intervention supports physiological comfortand reduces anxiety without requiring clinical judgment.
Rationale for incorrect answers
2.Admission notification involves gathering psychosocial history and identifying support systems, which requires clinical assessment and is outside the scope of ancillary staff.
3.Rules orientation involves therapeutic communication and behavioral expectations, which must be tailored to the client’s psychiatric condition and requires nursing judgment.
4.Encouragement to talk about anxiety is a psychosocial intervention requiring therapeutic communication skills and awareness of the client’s mental status, which ancillary staff are not trained to provide.
Take Home Points
- OCD with ordering compulsions involves distressing rituals that must be respected to avoid escalating anxiety.
- Ancillary staff can assist with non-clinical tasks that support physiological comfort, such as organizing belongings.
- Interventions involving psychosocial assessment or therapeutic communication must be performed by licensed nurses.
- Differentiating OCD from generalized anxiety disorder is essential; OCD involves specific compulsions tied to intrusive thoughts.
Which approach should a nurse use when working with an individual diagnosed with obsessive-compulsive disorder?
Explanation
Obsessive-compulsive disorder (OCD)is a psychiatric condition marked by intrusive thoughtsand compulsive behaviorsaimed at reducing anxiety. These rituals are ego-dystonic, meaning the individual recognizes them as irrational but feels compelled to perform them. Confrontation or disruption of these behaviors can escalate distress. Nursing care must prioritize emotional safety, therapeutic alliance, and gradual behavioral modification. SSRIs and cognitive-behavioral therapy are first-line treatments. Respecting the client’s autonomy and minimizing anxiety are essential, especially during acute phases.
Rationale for correct answers
3.A calm and nonconfrontationalapproach fosters trust and reduces anxiety, allowing the nurse to support the client’s coping mechanisms without escalating compulsive behavior.
Rationale for incorrect answers
1.Autocratic behavior may provoke resistance and worsen anxiety, undermining therapeutic rapport and increasing compulsive responses.
2.Confrontational tactics can trigger defensive reactions and intensify obsessive-compulsive symptoms, making treatment less effective.
4.Hurried interactions disregard the client’s need for control and predictability, increasing distress and impairing communication.
Take Home Points
- OCD requires a calm, nonjudgmental approach to reduce anxiety and support behavioral change.
- Confrontation or authoritarian behavior can worsen compulsions and damage therapeutic rapport.
- Nursing care should focus on emotional safety and gradual exposure-based interventions.
- OCD must be differentiated from personality disorders; compulsions are ego-dystonic and anxiety-driven.
Which of the following statements are correct regarding obsessive-compulsive disorder (OCD)? Select all that apply.
Explanation
Obsessive-compulsive disorderis a chronic psychiatric condition marked by persistent intrusive thoughts and repetitive behaviors aimed at reducing distress. It can significantly impair functioning, often accompanied by anxiety and sleep disturbances, and is assessed using validated scales to monitor severity and treatment progress.
Rationale for correct answers
1.Obsessions are intrusive, unwanted thoughts, while compulsions are repetitiveactions aimed at reducing the anxiety provoked by these thoughts.
3.Sleep problems occur due to heightened arousaland mental preoccupation with intrusive thoughts, making it difficult for patients to fall or stay asleep.
5.Structured tools such as the Yale-Brown Obsessive Compulsive Scale are used to measuresymptom severity and guide treatment decisions.
Rationale for incorrect answers
2.While rare cases may occur in young children, onset before age 5 is extremely uncommon, with typical onset in late childhood or adolescence.
4.Schizophrenia is not a common comorbidity; OCD is more often associated with anxiety or depression, not primary psychotic disorders.
6.Suicide risk in OCD is elevated compared to the general population, but generally lower than in severe depressionwithout comorbid conditions.
Take Home Points
- OCD involves intrusive thoughts (obsessions) and repetitive behaviors (compulsions) performed to reduce anxiety.
- Sleep disturbances are common due to persistent mental preoccupation.
- Standardized tools like the Yale-Brown Obsessive Compulsive Scale help track symptom severity.
- Onset typically occurs in late childhood or adolescence, with earlier onset being rare.
Which of the following statements explains the etiology of obsessive-compulsive disorder (OCD) from a biological theory perspective?
Explanation
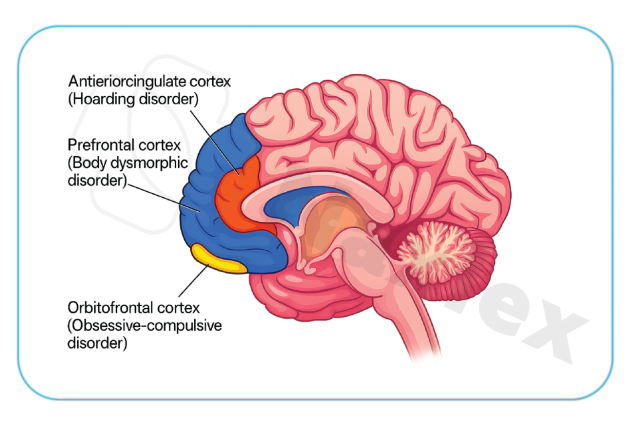
Obsessive-compulsive disorder (OCD)is a chronic psychiatric condition marked by intrusive thoughts (obsessions) and repetitive behaviors (compulsions). It is strongly linked to neurobiologicaldysfunction, particularly involving the cortico-striato-thalamo-cortical circuit, which regulates decision-making and behavioral inhibition. Abnormalities in serotonintransmission and structural changes in the orbitofrontal cortex, anterior cingulate cortex, and basal ganglia are consistently observed in affected individuals. SSRIs remain the first-line pharmacologic treatment due to their modulation of serotonin pathways.
Rationale for correct answers
4.Structural and functional abnormalitiesin the orbitofrontal cortex, anterior cingulate cortex, and basal ganglia disrupt inhibitory control and decision-making, contributing to compulsive behaviors. Neuroimaging consistently shows hyperactivity in these regions, supporting a biological etiology.
Rationale for incorrect answers
1.The term egostems from psychodynamic theory, not biological models. It reflects personality structure rather than neurochemical or anatomical dysfunction, making it irrelevant to biological etiology.
2.A conditionedresponse aligns with behavioral theory, not biological. While trauma may exacerbate symptoms, it does not explain the neurobiological underpinnings of OCD.
3.The analsadistic phase is a Freudian concept from psychosexual development theory. It lacks empirical support and does not reflect current biological understanding of OCD.
Take Home Points
- OCD is primarily linked to dysfunction in cortico-striato-thalamo-cortical circuits and serotonin imbalance.
- Neuroimaging reveals hyperactivity in orbitofrontal cortex and basal ganglia in OCD patients.
- SSRIs are effective due to their action on serotonin pathways, confirming biological involvement.
- OCD must be differentiated from trauma-related disorders and personality disorders based on etiology and symptom patterns.
Practice Exercise 3
Interventions for a client with OCD would include: Select all that apply.
Explanation
Obsessive-compulsive disorderis a chronic psychiatric disorder involving intrusive, recurrent thoughts and repetitive behaviors aimed at reducing distress. Treatment combines cognitive-behavioral therapyand medication, with a focus on gradually reducing compulsions while improving tolerance to anxiety.
Rationale for correct answers
1.Encouraging emotional expression allows the client to process obsessive thoughts and associated distress, which can reduce internalpressure and aid in symptom control.
4.Collaborative planning to limit rituals supports gradual exposurewhile respecting the client’s readiness, reducing resistance and promoting adherence to interventions.
5.Relaxation techniques lower physiologicalarousal, helping the client manage anxiety and resist compulsions during exposure and response prevention therapy.
6.Tolerating anxious feelings builds resilience, reinforcing that discomfort is temporary and manageable without engaging in compulsive behaviors.
Rationale for incorrect answers
2.Avoiding obsessive thinking reinforces the obsession by increasing its salience, making it more persistent rather than diminishing it.
3.Abruptly interrupting rituals without preparation may escalate distress, potentially worsening anxiety and resistance to therapy.
Take Home Points
- OCD management focuses on anxiety tolerance, not avoidance or abrupt elimination of symptoms.
- Gradual reduction of compulsions is more effective than sudden interruption of rituals.
- Relaxation and emotional expression complement exposure and response prevention strategies.
- Collaboration with the client enhances treatment adherence and reduces resistance.
The client with OCD has counting and checking rituals that prolong attempts to perform activities of daily living and get ready for activities of the day. The nurse knows that interrupting the client’s ritual to assist in faster task completion will likely result in:
Explanation
Obsessive-compulsive disorderis a chronic mental health condition involving intrusive, unwanted thoughts (obsessions) and repetitive actions or mental acts (compulsions) performed to reduce distress. Disrupting these rituals without preparation can trigger a physiologicalstress response and exacerbate anxiety symptoms, as compulsions temporarily relieve distress caused by obsessions.
Rationale for correct answers
1.Interrupting rituals prematurely can cause an acute spike in anxietybecause the compulsive act is a coping mechanism to neutralize obsessive distress.
Rationale for incorrect answers
2.Gratitude is unlikely since interference may be perceived as intrusive, leading to resentmentrather than appreciation during heightened anxiety.
3.Relief is improbable because stopping rituals before completion leaves obsessions unresolved, increasing tensionrather than decreasing it.
4.Although depression can coexist with OCD, sudden ritual interruption does not directly cause suicidality; this risk requires broader assessment over time.
Take Home Points
- OCD rituals function as maladaptive coping mechanisms to reduce anxiety from obsessions.
- Sudden interference in rituals can intensify anxiety and distress rather than alleviate it.
- Effective interventions include gradual exposure with response prevention rather than abrupt interruption.
- OCD must be differentiated from anxiety disorders and psychotic disorders, as management strategies differ significantly.
Clients with OCD often have exposure/response prevention therapy. Which of the following statements by the client would indicate positive outcomes for this therapy?
Explanation
Obsessive-compulsive disorderis characterized by persistent, intrusive thoughts (obsessions) and repetitive behaviors or mental acts (compulsions) performed to reduce distress. The goalof exposure and response prevention therapy is to help patients face anxiety-provoking triggers without engaging in compulsive rituals, ultimately improving tolerance to discomfort and reducing symptom severity.
Rationale for correct answers
2.Successful therapy involves exposure to feared stimuli while resisting compulsions, leading to improved toleranceof the anxiety rather than complete elimination of anxiety.
Rationale for incorrect answers
1.Avoidance of obsessive thoughts is unrealistic, as therapy focuses on acceptanceand management rather than suppression of intrusive thoughts.
3.Complete absence of anxiety is not the goal; some residualanxiety is expected even with significant improvement.
4.Immediate loss of compulsion is unlikely; reduction occurs gradually, and therapy targets the ability to resist rather than instantly remove urges.
Take Home Points
- ERP therapy teaches patients to face obsessions without performing compulsions, focusing on anxiety tolerance rather than total removal.
- Complete elimination of anxiety or obsessive thoughts is not a realistic short-term goal of OCD treatment.
- Avoidance behaviors can worsen OCD symptoms by reinforcing anxiety rather than reducing it.
- Improvement is measured by functional gains and reduced ritual frequency, not just symptom disappearance.
Which of the following would be an appropriate intervention for a client with OCD who has a ritual of excessive, constant cleaning?
Explanation
Obsessive-compulsive disorder (OCD)is a chronic psychiatric condition marked by intrusive obsessionsand repetitive compulsions. In contamination-related OCD, individuals experience intense fear of germs or illness, leading to excessive cleaning rituals. These behaviors temporarily relieve anxiety but reinforce maladaptive patterns. Treatment focuses on exposure and response prevention (ERP), cognitive restructuring, and behavioral interventions that reduce ritual dependency and promote adaptive coping.
Rationale for correct answers
1.A structured daily schedule provides predictabilityand reduces idle time that could trigger compulsive cleaning. It supports behavioral activation and helps redirect attention toward goal-oriented tasks, minimizing ritual reinforcement.
Rationale for incorrect answers
2.Daily intense psychotherapy may overwhelm the client and increase distress, especially without gradual exposure. OCD treatment requires paced interventions like ERP, not high-frequency sessions that risk emotional exhaustion.
3.Distraction alone is a compulsionsubstitute and reinforces avoidance. While it may reduce anxiety temporarily, it fails to address the underlying obsession and does not promote habituation or cognitive restructuring.
4.Imposing negative consequences fosters shame, which exacerbates OCD symptoms. Punitive approaches are contraindicated and may worsen compulsive behaviors by increasing anxiety and reinforcing the obsession-compulsion cycle.
Take Home Points
- Structured schedules reduce compulsive behaviors by promoting routine and minimizing idle time.
- ERP is the gold-standard treatment for OCD, focusing on exposure without ritual engagement.
- Distraction techniques may offer temporary relief but are not substitutes for evidence-based therapy.
A client with OCD is admitted to the hospital due to ritualistic hand washing that occupies several hours each day. The skin on the client’s hands is red and cracked, with evidence of minor bleeding. The goal for this client is:
Explanation
Obsessive-compulsive disorderis a mental health condition marked by obsessions(intrusive, unwanted thoughts) and compulsions(repetitive behaviors) performed to reduce anxiety. Sudden removal of compulsions often worsens anxiety; instead, a gradual approach with exposure and response prevention is preferred. The goal is to reduce ritual time while building tolerance to anxiety triggers, improving function and daily living.
Rationale for correct answer
1.Reducing the time spent on compulsive hand washing is a realistic and measurable goal that decreases impairment without overwhelming the client’s ability to cope.
Rationale for incorrect answers
2.Abrupt elimination of compulsions can cause significant anxietyspikes, risking noncompliance and worsening symptoms.
3.Switching to a milder soap addresses skin irritation but does not treat the underlying compulsionor improve time management.
4.Good skin care supports comfort and prevents infection but fails to address behavioral controlover the excessive hand washing.
Take Home Points
- OCD treatment prioritizes gradual reduction of compulsions rather than immediate elimination.
- Hand washing rituals in OCD can cause skin breakdown requiring supportive care.
- Exposure and response prevention therapy is the behavioral treatment of choice.
- Sudden removal of compulsions can worsen anxiety and hinder recovery.
Comprehensive Questions
Which of the following characteristics describe the obsessional thoughts experienced by clients with OCD? Select all that apply.
Explanation
Obsessive-compulsive disorderinvolves persistent, intrusive thoughts or urges (obsessions) and repetitive actions or mental rituals (compulsions) performed to reduce distress. Obsessions are ego-dystonic, meaning they conflict with the person’s values or desires, and they provoke anxiety that fuels compulsive behaviors.
Rationale for correct answers
1.Obsessional thoughts are intrusive, occurring suddenly and disrupting normal thinking patterns without the person’s intent or control.
3.They are recurrent, repeatedly appearing in the person’s mind despite efforts to dismiss them, often leading to significant distress.
4.These thoughts are uncontrollable, arising involuntarily and persisting despite conscious attempts to suppress or replace them.
5.They are unwanted, causing discomfort because they are inconsistent with the individual’s beliefs, values, or desired mental state.
Rationale for incorrect answers
2.They are rarely realistic; most obsessions involve exaggerated, illogical fears or unlikely scenarios rather than accurate assessments of reality.
6.They are not voluntary, as the person does not willingly initiate them and often wishes to avoid or eliminate them.
Take Home Points
- Obsessions in OCD are intrusive, recurrent, uncontrollable, and unwanted thoughts that cause significant distress.
- They are ego-dystonic and differ from normal worries by their irrational and exaggerated nature.
- OCD requires differentiation from psychotic disorders, where intrusive thoughts may align with fixed false beliefs.
- Effective management involves cognitive-behavioral therapy with exposure and response prevention and, in some cases, pharmacologic treatment.
A client newly admitted to an inpatient psychiatric unit is diagnosed with obsessive-compulsive disorder. Which behavioral symptom would the nurse expect to assess?
Explanation
Obsessive-compulsive disorder (OCD)is a psychiatric condition characterized by persistent obsessionsand repetitive compulsionsperformed to alleviate anxiety. Behavioral symptoms often manifest as ritualistic actions, such as excessive hand washing, checking, or ordering. These compulsions are not connected in a realistic way to the feared event but are driven by internal distress. The DSM-5 outlines that compulsions must be time-consuming or cause significant impairment. Behavioral symptoms are observable and often interfere with daily functioning, distinguishing them from emotional or physiological responses.
Rationale for correct answers
1.Excessive hand washingis a classic behavioral compulsion in OCD, typically performed to neutralize obsessive fears of contamination. It reflects the repetitive, ritualistic nature of compulsions aimed at reducing anxiety.
Rationale for incorrect answers
2.Anxietyrating is a subjective emotional report, not a behavioral symptom. It reflects internal distress but does not demonstrate the compulsive actions characteristic of OCD.
3.Breathingtechniques are adaptive coping strategies, not compulsive behaviors. They are voluntary and therapeutic, unlike the involuntary rituals seen in OCD.
4.Diaphoresisand tachycardia are physiological symptoms of anxiety, not behavioral manifestations. They may occur in panic or generalized anxiety but are not specific to OCD compulsions.
Take Home Points
- Behavioral symptoms in OCD are repetitive actions performed to reduce distress from obsessions.
- Excessive hand washing is a hallmark compulsion, especially in contamination-related OCD.
- Emotional and physiological symptoms may accompany OCD but are not diagnostic behavioral features.
- OCD must be differentiated from anxiety disorders based on the presence of compulsive rituals.
A client newly admitted to an inpatient psychiatric unit is diagnosed with obsessive-compulsive disorder. Which correctly stated nursing diagnosis takes priority?
Explanation
Obsessive-compulsive disorder (OCD)is a psychiatric condition marked by intrusive obsessionsand repetitive compulsionsthat interfere with functioning. The compulsions are performed to reduce the anxiety triggered by the obsessions, creating a cycle of distress and temporary relief. The priority in nursing care is to address the anxiety, which drives the compulsive behaviors and impairs the patient’s ability to engage in daily activities. Managing anxiety is essential to reduce ritualistic actions and improve coping capacity.
Rationale for correct answers
1.Ritualistic behaviors are driven by obsessivethoughts that provoke intense anxiety. Addressing anxiety is the priority because it underlies the compulsions and impairs functioning.
Rationale for incorrect answers
2.Powerlessnessmay be present, but it is secondary to anxiety. The compulsions stem from an attempt to regain control, not a passive sense of helplessness.
3.Fearrelated to trauma is characteristic of PTSD, not OCD. OCD is driven by internal obsessions, not external traumatic stimuli.
4.Isolationmay occur due to embarrassment or time spent on rituals, but it is not the primary concern. Anxiety must be addressed first to reduce avoidance behaviors.
Take Home Points
- Anxiety is the driving force behind compulsions in OCD and must be prioritized in nursing care.
- Ritualistic behaviors are coping mechanisms for obsessive thoughts, not voluntary habits.
- OCD differs from PTSD in that it is not triggered by external trauma but by internal obsessions.
- Addressing anxiety can reduce social withdrawal and improve participation in therapeutic activities.
The nurse on the inpatient psychiatric unit should include which of the following interventions when working with a newly admitted client diagnosed with obsessive-compulsive disorder? Select all that apply.
Explanation
Obsessive-compulsive disorderis a chronic anxiety disorder characterized by persistent, intrusive obsessions and repetitive compulsions intended to reduce distress. It is associated with dysregulation in cortico-striato-thalamo-cortical circuits, often beginning in adolescence. Treatment involves exposureand response prevention therapy alongside pharmacologic interventions such as SSRIs. Symptom management requires a structured, collaborative care plan, respecting safety and physiologicalneeds while gradually reducing maladaptive behaviors.
Rationale for correct answers
1.Evaluating prior copingstrategies helps identify ineffective behaviors and informs tailored interventions to reduce anxiety without reinforcing compulsions.
2.Allowing completion of rituals initially prevents panicescalation, creating trust before initiating gradual exposure and response prevention.
3.Collaborative limit setting fosters autonomyand reduces defensiveness, allowing gradual modification of compulsions without overwhelming the client.
5.Exploring feelings around symptoms builds insightinto triggers and maintains therapeutic alliance, aiding motivation for behavioral change.
Rationale for incorrect answers
4.Directly confronting the impact of compulsions early can increase defensiveness, heighten anxiety, and hinder rapport before trust is established.
Take Home Points
- OCD involves obsessions and compulsions maintained by anxiety-reduction reinforcement.
- Initial care should respect rituals to build trust before gradual exposure therapy.
- Collaborative limit setting and emotional exploration enhance adherence to treatment.
- Early confrontation of impairments may harm rapport; timing is critical in psychiatric nursing care.
A nurse is developing a care plan for a client with an obsessive-compulsive behavior disorder. Which nursing intervention will most likely increase the client’s anxiety?
Explanation
Obsessive-compulsive disorder (OCD)is a chronic psychiatric condition marked by intrusive obsessionsand repetitive compulsionsthat aim to reduce anxiety. These compulsions are often rigid and time-consuming, and any disruption to them can provoke significant distress. The disorder is ego-dystonic, meaning the individual recognizes the irrationality of their behaviors but feels compelled to perform them. Treatment involves gradual exposure and response prevention, often supported by SSRIs and cognitive behavioral therapy.
Rationale for correct answers
2.Limiting ritualistic acts abruptly increases anxiety by disrupting the client’s primary coping mechanism. Without gradual desensitization, this approach risks emotional destabilization and noncompliance.
Rationale for incorrect answers
1.Understanding the nature of anxiety is therapeutic and promotes insight. It does not provoke anxiety but rather supports cognitive restructuring.
3.Involving the client in care planning enhances autonomy and reduces anxiety. Collaborative approaches foster trust and therapeutic engagement.
4.Nonjudgmental environments reduce shame and stigma. They are essential for building rapport and do not contribute to increased anxiety.
Take Home Points
- OCD rituals serve as maladaptive coping mechanisms that temporarily relieve anxiety but reinforce obsessive thought patterns.
- Abrupt restriction of compulsions without client preparation can escalate anxiety and hinder therapeutic progress.
- Effective care planning for OCD requires gradual exposure and response prevention, not immediate behavioral suppression.
- OCD must be differentiated from obsessive-compulsive personality disorder, which lacks the ego-dystonic nature and ritualistic distress.
Hospitalization or day-treatment centers are often indicated for the treatment of a client with an obsessive-compulsive disorder because these settings:
Explanation
Obsessive-compulsive disorderis a chronic condition involving intrusive, unwanted thoughts (obsessions) and repetitive actions (compulsions) that reduce distress. Neurobiological factors include hyperactivity in orbitofrontal cortex circuits and altered serotonin transmission. In severe cases, structured environments can reduce triggers, support therapy, and promote functional improvement while maintaining safety and stability. Treatment often combines cognitive-behavioral therapy and SSRIs, with emphasis on exposure and responseprevention.
Rationale for correct answers
4.A neutral environment minimizes emotional stimulationand external stressors, allowing the client to address internal conflicts and practice adaptive coping without excessive triggering.
Rationale for incorrect answers
1.Abrupt prevention of rituals can escalate distress, potentially worsening symptoms and damaging trust before gradual exposure techniques are implemented.
2.Excessive staff control may reinforce dependencerather than promoting the client’s self-regulation and active participation in therapeutic activities.
3.Minimal decision-making may temporarily lower anxiety but can impair autonomy, which is essential for long-term recovery and self-management.
Take Home Points
- OCD symptoms are maintained by anxiety-reducing behaviors that require gradual modification, not abrupt cessation.
- Neutral, structured environments help reduce external triggers while supporting therapy engagement.
- Overcontrol or avoidance of decisions may undermine autonomy and coping skills.
- Treatment success relies on trust, gradual exposure, and balanced support in a therapeutic setting.
What should a nurse include in the initial plan of care for a client with the long-standing, obsessive-compulsive behavior of hand washing?
Explanation
Obsessive-compulsive disorderinvolves persistent obsessions and compulsions driven by anxiety, often reinforced through temporary relief after the ritual. Long-standing compulsions like repetitive hand washing may be linked to contamination fears or other intrusive thoughts. Identifying the underlying purposeof the compulsion allows for targeted interventions and supports the development of exposure and responseprevention strategies. Understanding triggers is essential for addressing both psychological distress and related physicalconsequences, such as skin damage.
Rationale for correct answers
1.Determining the underlying functionof the ritual helps guide individualized interventions and ensures therapy addresses the specific anxiety or intrusive thought driving the compulsion.
Rationale for incorrect answers
2.Immediate time restriction without assessment can heighten anxietyand provoke resistance, worsening the compulsive cycle before trust and readiness are established.
3.Symptom substitution ignores the underlying obsession, risking a shift to another compulsion without resolving the core anxiety.
4.Rigid activity scheduling may offer some distractionbut does not directly address the cause or meaning of the compulsive behavior.
Take Home Points
- Understanding the purpose of a compulsion is critical before modifying or restricting it.
- Abrupt limitation of rituals can worsen anxiety and hinder rapport.
- Substitution techniques may mask but not resolve the underlying obsession.
- Effective OCD management integrates assessment, gradual exposure, and anxiety regulation strategies.
A client with a history of obsessive-compulsive behaviors has a marked decrease in symptoms and expresses a wish to obtain a part-time job. On the day of a job interview the client arrives at the mental health center displaying signs of anxiety. What is the nurse’s best response to the client’s behavior?
Explanation
Obsessive-compulsive disordercan significantly impair functioning, but with symptom reduction, gradual reintegration into normal roles is encouraged. Stressful events like job interviews may temporarily heighten anxietyas part of exposure to feared situations. Supportive interventions focus on validating the client’s experience, maintaining forward progress, and providing practicalcoping strategies. Encouraging adaptive problem-solving helps sustain recovery while avoiding reinforcement of avoidance behaviors.
Rationale for correct answers
4.Validates the emotional experienceand offers a concrete coping option, supporting both autonomy and progression toward the client’s vocational goal.
Rationale for incorrect answers
1.Pressuring exposure without acknowledging feelingscan increase resistance and diminish trust, risking relapse into avoidance patterns.
2.Suggesting the client is not readyreinforces avoidance and undermines progress made in symptom management.
3.Misinterpreting the anxiety as lack of motivationinvalidates the client's efforts and may damage therapeutic rapport.
Take Home Points
- Anxiety may spike temporarily during exposure to real-life challenges in OCD recovery.
- Validating feelings encourages trust and self-efficacy.
- Avoidance reinforcement can hinder functional reintegration.
- Supportive, practical solutions help bridge the gap between therapy and real-world functioning.
Which is the best nursing intervention during the working phase of the therapeutic relationship to meet the needs of individuals who demonstrate obsessive-compulsive behavior?
Explanation
Obsessive-compulsive disorderis a chronic mental health condition involving intrusive thoughts(obsessions) and repetitive acts (compulsions) performed to reduce anxiety. Symptoms often intensify under stress, and compulsions can significantly impair social and occupational functioning. Management focuses on anxiety reduction, gradual exposure, and response preventionwhile maintaining therapeutic rapport. Interventions require a balance between respecting the patient’s coping mechanisms and promoting healthy behavior change.
Rationale for correct answers
4.Supporting rituals initially allows the patient to maintain a sense of control, which reduces acute anxiety, while setting realistic limits prevents the compulsion from dominating daily functioning. This balance fosters trust during the working phase, making gradual modification more acceptable.
Rationale for incorrect answers
1.Restricting movements can abruptly remove a coping mechanism, triggering heightened distressand potentially causing the patient to withdraw from therapeutic engagement.
2.Calling attention to the behavior in a critical manner can increase shame, leading to resistance and decreased openness in the therapeutic relationship.
3.Simply keeping the patient busy may provide temporary distraction, but it fails to address the underlying anxiety and the compulsive drive sustaining the behavior.
Take Home Points
- OCD involves obsessions and compulsions that temporarily relieve anxiety but reinforce the cycle of symptoms.
- Supportive limits help reduce compulsions without causing defensive withdrawal.
- Abrupt restriction of rituals can worsen anxiety and damage trust.
- Effective management combines therapeutic rapport with gradual exposure and response prevention.
A nurse is caring for a client with an obsessive-compulsive personality disorder that involves rituals. What should the nurse conclude about the ritual?
Explanation
Obsessive-compulsive personality disorderis characterized by a pervasive preoccupation with orderliness, perfectionism, and control, often at the expense of flexibility and efficiency. In cases involving ritualistic behavior, these actions serve to reduce underlying anxiety, even when the behavior seems unreasonable to others. The compulsion is not simply a habit but a psychologically necessary act to relieve mental discomfort caused by intrusive or rigid thought patterns.
Rationale for correct answers
4.Rituals, though illogicalto observers, function as an essential coping mechanism for controlling anxiety or distress, making them psychologically necessary to the individual’s functioning at that moment.
Rationale for incorrect answers
1.While rituals may seem uselessfrom an outsider’s view, they have a clear anxiety-reducing function for the individual and are not purposeless to them.
2.Ritualistic acts are not usually performed after prolonged urging; they are initiated by an internal drive or compulsion to alleviate discomfort.
3.The behavior may look willing, but it is driven by an internal compulsion rather than free choice or genuine desire.
Take Home Points
- Obsessive-compulsive personality disorder involves inflexible patterns of behavior aimed at maintaining control and order.
- Ritualistic acts serve a psychological purpose in reducing anxiety, even if they appear unreasonable.
- Compulsions are internally driven, not externally encouraged.
- Understanding the function of rituals is key to forming effective therapeutic interventions.
A nursing assistant interrupts the performance of a ritual by a client with obsessive-compulsive disorder. What is the most likely client reaction?
Explanation
Obsessive-compulsive disorderis an anxiety disorder marked by intrusive obsessionsand repetitive compulsions performed to prevent or reduce distress. These rituals are strongly linked to relief from mounting anxiety. If they are interrupted, the discomfort escalates rapidly, often resulting in intense emotional distress rather than calm acceptance. The interruption disrupts the individual’s coping mechanism, triggering heightened physiological arousal and emotional reactivity.
Rationale for correct answers
1.Stopping a ritual abruptly increases anxiety, as the act serves to neutralize distress caused by obsessive thoughts, leaving the individual without their main coping strategy.
Rationale for incorrect answers
2.While frustration can occur, sustained hostilityis less likely; the primary response is heightened anxiety, not prolonged antagonistic feelings.
3.Aggressionis uncommon unless anxiety becomes extreme and the person feels threatened, making it a less predictable primary reaction.
4.Withdrawalis unlikely immediately after interruption; the person typically experiences an acute anxiety spike before any retreat from interaction.
Take Home Points
- OCD rituals function as coping tools to reduce distress from intrusive thoughts.
- Interrupting rituals removes the individual’s immediate anxiety control mechanism.
- The most immediate reaction is a surge in anxiety rather than aggression or withdrawal.
- Managing OCD requires balancing therapeutic limits with strategies that minimize distress spikes.
Research indicates that the symptoms of OCD:
Explanation
Obsessive-compulsive disorderis a neuropsychiatric condition involving intrusive thoughts and repetitive behaviors linked to dysfunction in cortico-striato-thalamo-cortical circuits. Research shows hyperactivityin the orbitofrontal cortex, anterior cingulate cortex, and caudate nucleus, leading to heightened error detection and overestimation of threat. This hyperactivity drives compulsive rituals, reinforcing maladaptive neural pathways through repeated performance of compulsions.
Rationale for correct answers
3.The orbitofrontal cortexshows hypermetabolism in OCD, causing excessive concern with potential danger and intrusive checking or cleaning behaviors.
Rationale for incorrect answers
1.OCD differs from panic disorder; panic involves sudden autonomicsurges, whereas OCD has persistent intrusive thoughts with ritualized responses.
2.Low stress hormone levels do not cause OCD; dysregulation involves serotoninand glutamate systems alongside abnormal cortical activity.
4.Viewing triggering stimuli without therapy usually worsens symptoms; reduction requires controlled exposure with response prevention, not passive viewing.
Take Home Points
- OCD involves hyperactivity in cortico-striatal circuits, especially the orbitofrontal cortex.
- Dysfunction leads to heightened threat perception and compulsive rituals.
- Neurotransmitter imbalances, particularly serotonin and glutamate, are implicated.
- Treatment often combines exposure and response prevention with pharmacotherapy.
Which of the following is the drug of choice in OCD?
Explanation
Obsessive-compulsive disorderresponds best to pharmacologic agents that enhance serotoninneurotransmission. Selective serotonin reuptake inhibitors (SSRIs) are first-line therapy because they increase synaptic serotonin and normalize activity in overactive cortical-subcortical pathways. Compared to older antidepressants, SSRIs have better tolerability and lower toxicity in overdose, making them safer for long-term management.
Rationale for correct answers
1.Fluoxetine, an SSRI, effectively reduces intrusive thoughts and compulsions by enhancing serotonergic activity in the cortico-striatal circuitry.
Rationale for incorrect answers
2.Imipramine, a tricyclic antidepressant, is mainly used in depressionand enuresis, not first-line for OCD due to more side effects.
3.Alprazolam, a benzodiazepine, targets acute anxietybut does not address the intrusive thought-compulsion cycle in OCD.
4.Chlorpromazine, a typical antipsychotic, is for psychosis, not OCD, and can cause significant extrapyramidal and sedative effects.
Take Home Points
- SSRIs are first-line pharmacotherapy for OCD.
- Fluoxetine, sertraline, and fluvoxamine are commonly prescribed.
- Tricyclic clomipramine is effective but has more adverse effects.
- Therapy is most effective when combined with cognitive behavioral interventions.
Which of the following is the treatment of choice for OCD?
Explanation
Obsessive-compulsive disorder (OCD)is a chronic psychiatric condition involving intrusive, recurrent obsessions and repetitive compulsions that interfere with functioning. It is linked to serotonin dysregulationand hyperactivity in cortico-striato-thalamo-cortical circuits. First-line treatment includes pharmacotherapy with SSRIs and structured psychotherapy aimed at gradually confronting feared stimuli while preventing compulsive rituals. Behavioral therapyinterventions target maladaptive responses through systematic, controlled exposure.
Rationale for correct answers
1.This approach systematically exposes the individual to feared triggers while preventing compulsive responses, leading to habituationand reduced anxiety over time.
Rationale for incorrect answers
2.Flooding uses intense exposure without gradual buildup, which can cause overwhelming distressand poor adherence, making it unsuitable for most OCD patients.
3.Psychoanalysis focuses on unconscious conflicts and past experiences but lacks evidence for effectively targeting the core symptomsof OCD.
4.Modeling demonstrates desired behaviors for imitation, which is useful in some learning contexts but insufficient to reduce compulsive ritualsin OCD.
Take Home Points
- OCD involves dysfunction in cortico-striatal-thalamo-cortical pathways and serotonin dysregulation.
- Exposure and response prevention is the gold-standard behavioral therapy for OCD.
- SSRIs like fluoxetine, sertraline, and fluvoxamine are first-line pharmacologic treatments.
- Differentiating OCD from generalized anxiety disorder or psychotic disorders is essential for proper treatment planning.
The concept of PANDAS is related to which of the following conditions:
Explanation
Pediatric autoimmune neuropsychiatric disorders associated with streptococcal infections (PANDAS)is a post-infectious syndrome where group A β-hemolytic Streptococcus triggers autoimmune neuroinflammationaffecting basal ganglia circuits. This results in sudden-onset obsessive-compulsive symptoms and/or motor tics in children. Pathogenesis involves molecular mimicrywith antibodies cross-reacting with neuronal tissue, leading to abrupt behavioral changes. Diagnosis is clinical, and management may involve antibiotics, psychiatric intervention, and immune-modulatingtherapies in severe cases.
Rationale for correct answers
1.The abrupt onset of obsessive-compulsive symptoms following streptococcal infection aligns with autoimmunepathophysiology involving basal ganglia, making this the defining feature of the disorder.
Rationale for incorrect answers
2.Schizophrenia involves chronic psychosis and disorganized thought, not acute postinfectiousonset related to group A streptococcal immune responses.
3.Autism spectrum disorder is a developmental neurobehavioralcondition present from early childhood and unrelated to infectious autoimmune triggers.
4.Depression is a mood disorder with persistent sadness, unrelated to acute autoimmune mechanismsfollowing bacterial infection.
Take Home Points
- PANDAS presents with sudden-onset OCD or tics following group A streptococcal infection.
- Pathophysiology involves autoimmune cross-reactivity against basal ganglia neurons.
- Diagnosis is clinical and requires temporal relation to infection and neuropsychiatric symptom onset.
- Differential diagnosis includes Tourette syndrome, autoimmune encephalitis, and primary OCD.
The basic pathology in Pediatric Autoimmune Neuropsychiatric Disorders associated with Streptococcus (PANDAS) causing OCD in children is development of antibodies against:
Explanation
Pediatric Autoimmune Neuropsychiatric Disorders associated with Streptococcus (PANDAS)is a condition where autoantibodiestarget neuronal tissue following a Group A Streptococcal infection. These antibodies cross-react with brain structures, particularly the basal ganglia, leading to abrupt onset of obsessive-compulsive behaviors and motor tics. The basal ganglia regulate motor control, behavior, and emotion, making them central to the neuropsychiatric symptoms seen in PANDAS. The pathophysiology involves molecular mimicry, where streptococcal antigens resemble neuronal proteins, triggering an autoimmune response.
Rationale for correct answers
1.The basal gangliaare the primary target of autoantibodies in PANDAS, leading to dysfunction in motor and behavioral regulation. This explains the sudden onset of OCD and tics.
Rationale for incorrect answers
2.The hippocampus is involved in memory and spatial navigation, not typically affected in PANDAS. Autoantibody targeting here would not explain OCD or motor tics.
3.The cingulate cortex modulates emotion and decision-making, but it is not the primary site of autoimmune attack in PANDAS. Its involvement is secondary, if at all.
4.The mammillary bodies are linked to memory consolidation and are not implicated in the autoimmune pathology of PANDAS. Their dysfunction does not produce OCD-like symptoms.
Take Home Points
- PANDAS is triggered by Group A Streptococcal infection leading to autoimmune attack on basal ganglia.
- Symptoms include abrupt onset of OCD, motor tics, and emotional dysregulation.
- Differentiation from Tourette syndrome and Sydenham chorea is essential due to overlapping features.
- Treatment may involve antibiotics, immunomodulatory therapy, and psychiatric support.
Exams on Obsessive-Compulsive and Related Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Overview Of Oc And Related Disorders (Ocrds)
- Obsessions
- Compulsions
- Practice Exercise 1
- Compulsive Behavior Patterns
- Related Disorders
- Practice Exercise 2
- Assessment In Nursing Practice
- Nursing Diagnoses And Planning
- Interventions And Treatments
- Practice Exercise 3
- Complications, Prognosis, And Patient Education
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define Obsessive-Compulsive Disorder (OCD) and its core components, including obsessions, compulsions, and related behavioral patterns, based on established diagnostic frameworks.
- Identify epidemiological trends, etiological factors, and neurobiological underpinnings of OCD and associated disorders.
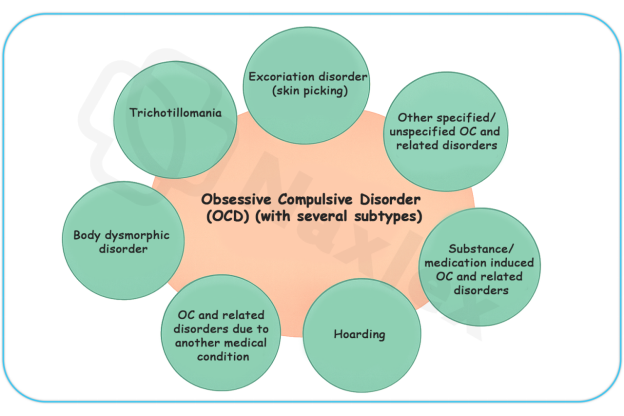
- Differentiate OCD from related disorders like body dysmorphic disorder, hoarding disorder, trichotillomania, and excoriation disorder, focusing on clinical features.
- Apply nursing assessment techniques, including screening tools and cultural considerations, to evaluate patients with these conditions.
- Formulate appropriate nursing diagnoses, plan interventions, and evaluate outcomes using evidence-based treatments like pharmacotherapy and cognitive-behavioral therapy.
- Recognize complications, prognostic indicators, and patient education strategies to promote holistic care and recovery.
- Integrate key nursing insights to enhance clinical decision-making and prepare for nursing examinations on mental health topics.
Introduction
- Obsessive-compulsive and related disorders involve persistent, intrusive thoughts and repetitive behaviors significantly impairing daily functioning.
- These disorders are classified together due to shared features of repetitive, unwanted mental or behavioral activities aimed at reducing distress.
- OCD affects millions globally and often co-occurs with anxiety, depression, or other psychiatric conditions.
- Nurses play a critical role in early identification, therapeutic alliance building, medication management, and supporting behavioral therapies.
Overview Of Oc And Related Disorders (Ocrds)
- OCD is a chronic psychiatric condition characterized by recurrent obsessions and compulsions causing marked distress and functional impairment.
- Related disorders share phenomenological similarities but differ in focus, such as appearance in body dysmorphic disorder or hair-pulling in trichotillomania.
- Dysregulation in cortico-striato-thalamo-cortical circuits, with genetic, environmental, and neurochemical influences, underpins these disorders.
- Prevalence of OCD is approximately 1-3% globally, highlighting the need for nursing proficiency in recognition and management.
1.1 Definition and Diagnostic Features
- OCD is defined by the presence of obsessions, compulsions, or both, which are time-consuming (more than one hour per day) and not attributable to another medical condition or substance use.
- Diagnostic features include recognition by the individual that obsessions or compulsions are excessive, though insight may vary.
- Related disorders involve repetitive behaviors directed toward specific foci, such as perceived defects in body dysmorphic disorder.
- Obsessions are recurrent, persistent thoughts, urges, or images that are intrusive and unwanted, causing anxiety or distress.
- Compulsions are repetitive behaviors or mental acts performed in response to obsessions or rigid rules.
- Disorders must cause clinically significant distress or impairment, not better explained by other mental disorders like schizophrenia.
Nursing Insights
- Nurses must recognize that poor insight in OCD (belief that obsessions are realistic) occurs in 25-30% of cases, associated with worse prognosis, guiding tailored interventions and predicting treatment adherence.
1.2 Epidemiology
- OCD has a lifetime prevalence of 2-3%, with onset typically in late adolescence or early adulthood, though childhood onset occurs.
- Females are slightly more affected than males in adulthood; males predominate in pediatric cases.
- Related disorders’ prevalence: body dysmorphic disorder (1-2%), hoarding disorder (2-6%), trichotillomania (1-2%), excoriation disorder (1-5%).
- Cultural factors influence presentation; religious obsessions are common in devout populations.
- Comorbidity is high, with 75% of OCD patients having at least one additional axis I disorder, such as depression or anxiety.
- Risk is elevated in first-degree relatives, with heritability estimates of 40-50% for OCD.
- Socioeconomic factors, urban living, and stressful life events correlate with higher incidence.
- Global studies show consistent core symptoms but variations in content based on cultural norms.
1.3 Etiology and Risk Factors
- Etiology involves genetic, neurobiological, environmental, and psychological factors.
- Genetic factors include candidate genes like serotonin transporter (SLC6A4) and glutamate systems (SLC1A1).
- Neurobiologically, hyperactivity in orbitofrontal cortex, anterior cingulate cortex, and basal ganglia is implicated, shown by functional MRI.
- Environmental risks include perinatal complications, streptococcal infections (PANDAS), and trauma.
- Psychological models, like cognitive appraisal theory, suggest misinterpretation of intrusive thoughts contributes to symptom maintenance.
- Twin studies show 80-87% concordance in monozygotic twins versus 47-50% in dizygotic, supporting heritability.
- Serotonin dysregulation is central, evidenced by SSRI efficacy; dopamine and glutamate also play roles.
- Childhood abuse increases risk by 2-3 times; infections like group A streptococcus can precipitate acute onset in children.
- Protective factors include strong social support and cognitive resilience.
Obsessions
- Obsessions are involuntary mental intrusions provoking anxiety and compelling behavioral responses.
- They arise from dysfunctional beliefs where neutral thoughts are appraised as threatening, leading to amygdala activation and distress.
- Obsessions must be time-consuming and not pleasurable, distinguishing them from ruminations in other disorders.
1.1 Characteristics
- Obsessions are recurrent, persistent thoughts, impulses, or images intruding into consciousness, causing marked anxiety or distress.
- Characteristics include intrusiveness, resistance to suppression, and association with specific themes.
- Individuals attempt to ignore or neutralize obsessions with compulsions, providing temporary relief.
- Persistence: Obsessions recur despite efforts to dismiss, escalating under stress.
- Distress induction: Trigger physiological responses like increased heart rate and cortisol levels.
- Insight variability: Most recognize obsessions as irrational, but poor insight leads to acting as if true.
- Obsessions differ from worries in generalized anxiety disorder by being more image-based and less reality-oriented, vital for differential diagnosis.
1.2 Common Themes
- Common themes include contamination fears, doubts about actions, aggressive or sexual impulses, religious scrupulosity, and symmetry needs.
- Themes are culturally influenced; contamination may involve germs or moral “dirtiness.”
- 90% of OCD patients report multiple themes, with contamination being most prevalent (45-60%).
- Contamination: Fear of dirt, germs, or chemicals leading to avoidance.
- Harm: Intrusive thoughts of harming others or self, despite no intent.
- Symmetry/order: Need for things to be “just right,” linked to perfectionism.
- Forbidden thoughts: Taboo sexual, religious, or blasphemous content causing guilt.
- Contamination obsessions surged during the COVID-19 pandemic, increasing OCD prevalence; nurses screen for exacerbation in public health crises.
1.3 Neurobiological Basis
- Obsessions involve aberrant functioning in the fear circuitry, particularly the orbitofrontal-subcortical loop.
- PET scans reveal hypermetabolism in the caudate nucleus during obsessive states, normalized post-treatment.
- Serotonergic deficits contribute, as low 5-HT levels correlate with symptom severity.
- Glutamatergic hyperactivity in the prefrontal cortex amplifies intrusive thoughts.
- Circuitry dysfunction: Overactivation of cortico-basal ganglia-thalamic loop leads to failure in thought suppression.
- Neurotransmitter roles: Serotonin modulates anxiety; dopamine influences reward in compulsion reinforcement.
- Genetic links: Polymorphisms in COMT and MAOA genes affect catecholamine metabolism, predisposing to obsessional thinking.
Compulsions
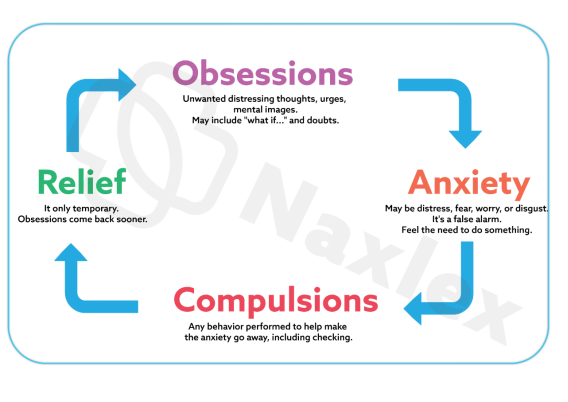
- Compulsions are repetitive, purposeful behaviors or mental acts performed in response to obsessions to reduce distress or prevent dreaded events.
- They are not realistically connected to the feared outcome and are excessive.
- Neurologically, compulsions reinforce the obsessive cycle via negative reinforcement, strengthening striatal pathways.
1.1 Purpose of compulsions
- Compulsions are stereotyped responses driven by rigid rules or to neutralize obsessions, often consuming significant time.
- Their purpose is anxiety reduction, but relief is short-lived, perpetuating a vicious cycle.
- Compulsions must be recognized as excessive in most cases.
- Behavioral vs. mental: Physical acts like hand-washing versus covert counting or praying.
- Time consumption: Often exceed one hour daily, impacting productivity.
- Resistance: Attempts to resist increase anxiety, leading to surrender.
- Compulsions provide temporary relief but maintain the disorder, key for explaining exposure therapy rationale.
1.2 Examples of Compulsive Behaviors
- Examples include checking, cleaning/washing, ordering/arranging, hoarding, and mental rituals like repeating phrases.
- Checking compulsions occur in 30% of cases, often linked to doubt obsessions.
- Behaviors can lead to physical harm, such as skin damage from washing.
- Checking: Repeated verification to prevent harm, e.g., ensuring stove is off.
- Washing/cleaning: Ritualistic hand-washing to remove contaminants.
- Counting/repeating: Mental or verbal repetition to “undo” bad thoughts.
Arranging: Aligning objects symmetrically for completeness.
Compulsive Behavior Patterns
- Compulsive behavior patterns are structured, ritualistic sequences evolving into complex routines.
- They are driven by the need to achieve a “just right” feeling, often overt or covert.
- They reflect habit formation in the basal ganglia, where actions become automatized.
1.1 Rituals and Their Impact
- Rituals are elaborate, rule-bound sequences, such as washing hands a specific number of times or following a precise path.
- Impact includes time loss, social isolation, and physical consequences like dermatitis from cleaning.
- Long-term, rituals erode self-efficacy and exacerbate depression.
- Complexity escalation: Rituals become more intricate, increasing impairment.
- Functional interference: Daily activities like work or relationships suffer.
- Emotional toll: Guilt and frustration arise from irrationality awareness.
- Documenting ritual details is crucial, as abrupt interruption causes panic; gradual exposure is key in care plans.
1.2 Differentiation from Other Behaviors
- Compulsions are distinguished from tics (involuntary, as in Tourette’s), stereotypies (in autism), or addictions (pleasure-seeking).
- Compulsions are ego-dystonic and anxiety-driven, unlike habitual behaviors lacking distress.
- Vs. tics: Tics are sudden, non-rhythmic; compulsions are purposeful.
- Vs. impulsivity: In ADHD, actions are spontaneous; compulsions are ritualized.
- Vs. normal rituals: Cultural rituals lack distress; OCD rituals impair functioning.
1.3 Cycle of Obsessions and Compulsions
- The cycle begins with an obsession triggering anxiety, followed by compulsion for relief, reinforcing via operant conditioning.
- Breaking this requires therapeutic disruption, as in CBT.
- Trigger: External cue or spontaneous thought.
- Anxiety spike: Physiological arousal.
- Compulsion: Temporary neutralization.
- Reinforcement: Short-term relief perpetuates cycle.
- The obsession-compulsion cycle is maintained by avoidance, guiding nurses to reinforce ERP therapy tolerance.
Related Disorders
- Related disorders are grouped with OCD due to overlapping phenomenology, genetics, and treatment responses.
- They involve repetitive behaviors focusing on body-focused or accumulation issues.
1.1 Body Dysmorphic Disorder
- Body dysmorphic disorder (BDD) involves preoccupation with perceived flaws in appearance that are minor or unobservable.
- Definition: Persistent preoccupation with defects, causing distress or impairment.
- Criteria require repetitive behaviors (e.g., mirror checking) or mental acts (e.g., comparing), not explained by eating disorders, with specifiers for muscle dysmorphia or insight.
- Preoccupation time: At least one hour daily.
- Behaviors: Camouflaging, seeking reassurance, excessive grooming.
- Distress: Leads to social withdrawal or suicidal ideation in 80% of cases.
- Clinical features include high comorbidity with depression (60%) and OCD (30%), with adolescent onset.
- Assessment evaluates delusion-like beliefs and suicide risk (25% attempt rate).
- Common foci: Skin, hair, nose; muscle concerns in males.
- Neurobiology: Visual processing abnormalities in fusiform gyrus.
- Cultural variations: Higher in cosmetic surgery seekers.
- Treatments include SSRIs and CBT focused on appearance beliefs; nurses monitor for dermatological self-harm.
- BDD is underdiagnosed; nurses screen with questions like “Do you worry excessively about your appearance?” to prevent cosmetic procedure traps.
1.2 Hoarding Disorder
- Hoarding disorder entails difficulty discarding possessions, leading to cluttered living spaces and impairment.
- Definition: Accumulation due to perceived need to save items, with distress at discarding.
- Criteria include clutter compromising living areas, not due to other conditions like dementia, with specifiers for acquisition or insight.
- Accumulation: Items of little value, like newspapers or trash.
- Distress: Emotional attachment or fear of needing items.
- Impairment: Health hazards from clutter, e.g., fire risks.
- Features: Onset in teens, worsening with age; 50% have comorbid depression.
- Assessment uses Hoarding Rating Scale, evaluating safety and functionality.
- Demographics: More common in older adults, equal in genders.
- Neurobiology: Frontal lobe deficits in decision-making.
- Complications: Social isolation, eviction risks.
- Treatments include CBT with motivational interviewing; SSRIs are less effective.
- Nursing interventions focus on harm reduction, like organizing sessions.
- Differentiate hoarding from collecting: Hoarding causes distress and clutter; nurses assess home safety for fall risks.
1.3 Trichotillomania (Hair-Pulling Disorder)
- Trichotillomania involves recurrent hair-pulling resulting in hair loss, with failed stop attempts.
- Definition: Repetitive pulling from scalp, eyebrows, or other areas, causing noticeable loss.
- Criteria require tension before pulling or relief after, not due to medical conditions, causing distress.
- Sites: Scalp (75%), eyebrows, eyelashes.
- Behaviors: Automatic (unaware) vs. focused (intentional).
- Prevalence: 1-2%, females predominant.
- Features: Onset in childhood, comorbid with excoriation (50%).
- Assessment examines bald patches and rules out alopecia.
- Psychological: Triggered by stress; may involve eating pulled hair (trichophagia).
- Neurobiology: Reward pathway involvement, similar to addictions.
- Complications: Infections, gastrointestinal issues from ingestion.
- Treatments include habit reversal training and SSRIs; nurses monitor for infections.
- Trichotillomania is body-focused; nurses educate on stress management to avoid misdiagnosis as self-harm.
1.4 Excoriation (Skin-Picking) Disorder
- Excoriation disorder features recurrent skin-picking causing lesions, with unsuccessful stop attempts.
- Definition: Repetitive picking at skin, causing damage.
- Criteria include distress or impairment, not substance-induced, not explained by other disorders.
- Sites: Face, arms, hands.
- Triggers: Boredom, anxiety.
- Duration: Episodes last minutes to hours.
- Features: Comorbid with OCD (40%), females more affected.
- Assessment involves dermatological exam and infection risk evaluation.
- Patterns: Automatic or focused picking.
- Neurobiology: Dopaminergic reinforcement.
- Scarring: Permanent damage common.
- Treatments include CBT, N-acetylcysteine for glutamate modulation; nurses apply wound care.
- Excoriation often co-occurs with acne; nurses promote barrier methods like gloves for habit breaking.
1.5 Substance/Medication-Induced Obsessive-Compulsive and Related Disorder
- Involves OCD-like symptoms from substance intoxication, withdrawal, or medication side effects, like stimulants or corticosteroids.
- Symptoms resolve upon cessation; nurses monitor for underlying vulnerabilities.
- Common agents: Amphetamines induce compulsions; antipsychotics may worsen.
- Assessment: Temporal link to substance use.
1.6 Obsessive-Compulsive and Related Disorder Due to Another Medical Condition
- Symptoms arise from medical issues like brain injury or Sydenham’s chorea.
- Nursing focuses on treating the primary condition.
- Examples: Post-stroke OCD from basal ganglia lesions.
- Diagnosis: Evidence of etiological medical factor.
1.7 Other Specified Obsessive-Compulsive and Related Disorder
- For presentations not meeting full criteria, like body odor concerns (olfactory reference syndrome).
- Subthreshold symptoms with impairment.
1.8 Unspecified Obsessive-Compulsive and Related Disorder
- Used when full criteria are unmet due to insufficient information.
- Temporary diagnosis in emergencies.
- In related disorders, poor insight in BDD predicts cosmetic surgery seeking; nurses advocate for psychiatric evaluation first.
Assessment In Nursing Practice
- Nursing assessment is systematic, incorporating biopsychosocial elements to inform care.
- Begins with building rapport to reduce stigma.
1.1 Screening Tools and Instruments
- Screening uses validated tools like Yale-Brown Obsessive Compulsive Scale (Y-BOCS) for severity, scoring obsessions and compulsions from 0-40.
- Other instruments include Obsessive-Compulsive Inventory (OCI) and Hoarding Rating Scale.
- Y-BOCS: Gold standard, assesses time, interference, distress.
- BDD-YBOCS: Adapted for body dysmorphic disorder.
- Interpretation: Scores >16 indicate moderate OCD needing intervention.
- Use Y-BOCS for initial and follow-up assessments; a 25-35% reduction indicates response, guiding medication adjustments.
1.2 Comprehensive Nursing Assessment
- Covers history, symptom details, functional impact, and comorbidities.
- Physical exam checks for compulsion-related injuries.
- Symptom inquiry: Frequency, triggers, relief methods.
- Mental status: Insight, mood, suicidality.
- Family history: Genetic risks.
1.3 Cultural and Developmental Considerations
- Cultural norms influence symptom expression; e.g., religious obsessions in conservative groups.
- Developmental stages affect presentation: children show more compulsions, elderly more hoarding.
- Cultural sensitivity: Avoid pathologizing cultural rituals.
- Age-specific: Pediatric assessments use play therapy.
Nursing Insights
- In nursing school exams, emphasize that OCD onset peaks bimodally (childhood and early adulthood); nurses screen adolescents during routine health visits, as early intervention reduces suicide risk, elevated 10-fold in untreated OCD.
Nursing Diagnoses And Planning
- Nursing diagnoses are derived from assessment data using frameworks like NANDA-I.
1.1 Common Nursing Diagnoses
- Common diagnoses include Anxiety related to obsessive thoughts, Ineffective Coping due to compulsions, and Impaired Social Interaction from avoidance.
- Anxiety: Evidenced by physiological symptoms.
- Disturbed Thought Processes: From intrusive obsessions.
- Risk for Injury: From skin-picking or hoarding clutter.
1.2 Goal Setting and Outcome Criteria
- Goals are SMART: e.g., Reduce compulsion time by 50% in 4 weeks.
- Outcomes measured by self-reports and scales.
- Short-term: Verbalize understanding of cycle.
- Long-term: Resume occupational functioning.
Interventions And Treatments
- Interventions combine pharmacological, psychotherapeutic, and nursing strategies for symptom reduction and quality of life improvement.
1.1 Pharmacological Interventions
- First-line: SSRIs like fluoxetine (20-80 mg/day), with 40-60% response rate.
- Clomipramine for refractory cases; augmentation with antipsychotics like risperidone.
- Mechanism: Increase serotonin availability.
- Side effects: Sexual dysfunction, weight gain; nurses monitor adherence.
- Onset: 8-12 weeks for full effect.
1.2 Psychotherapeutic Interventions
- Cognitive-behavioral therapy (CBT) challenges dysfunctional beliefs; effective in 70% of cases.
- Cognitive restructuring: Reframe obsessions as harmless.
- Mindfulness: Acceptance and commitment therapy variants.
1.3 Exposure and Response Prevention Therapy
- ERP involves gradual exposure to obsessions without compulsions, habituating to anxiety; 60-85% efficacy.
- Hierarchy building: Rank fears from least to most.
- Sessions: Weekly, with homework.
- Nursing role: Support during distress.
- ERP is superior to medication alone; nurses reinforce homework compliance, as dropout rates are 20-30%.
1.4 Nursing-Specific Interventions
- Nurses provide education, monitor medications, and facilitate support groups.
- Therapeutic communication validates distress without reassurance-seeking.
- Milieu therapy: Structured environments to limit rituals.
- Behavioral contracts: Agree on ritual reduction.
1.5 Multidisciplinary Collaboration
Involves psychiatrists, therapists, social workers; nurses coordinate care.
Complications, Prognosis, And Patient Education
- Complications arise from untreated symptoms; prognosis improves with early intervention.
- Education empowers self-management.
1.1 Potential Complications
- Include chronic depression (50% comorbidity), substance abuse, and physical issues like infections from picking or malnutrition in hoarding.
- Suicidality: 10-17% attempt rate in OCD.
- Occupational loss: Unemployment in 20-30%.
- Family strain: Caregiver burden high.
1.2 Prognostic Factors
- Good prognosis with early treatment, good insight, and no comorbidities.
- Poor prognosis in chronic cases; hoarding subtype has worst outcome.
- Response predictors: Family support, therapy adherence.
- Recovery rates: 50% achieve remission with treatment.
1.3 Patient and Family Education Strategies
- Education covers disorder nature, treatment rationale, and relapse prevention.
- Use teach-back methods.
- Topics: Cycle breaking, medication facts.
- Resources: OCD Foundation materials.
- Family involvement: Avoid enabling compulsions.
- Educate on relapse signs like ritual return; schedule follow-ups, as 30% relapse post-treatment.
Nursing Insights
- A key point for nurses is the biopsychosocial model in OCD etiology; assess for streptococcal history in pediatric cases to rule out PANDAS, potentially altering treatment to immunological interventions.
Summary
- OCD and related disorders involve intrusive obsessions and repetitive compulsions or behaviors, rooted in neurobiological dysregulation.
- Key components include obsessions (intrusive thoughts), compulsions (repetitive acts), and compulsive patterns (ritualized sequences).
- Related disorders like body dysmorphic disorder, hoarding disorder, trichotillomania, and excoriation disorder require tailored assessments.
- Nursing involves screening with Y-BOCS, diagnosing Anxiety, and implementing SSRIs, CBT, and ERP.
- Complications like suicidality require vigilant monitoring; prognosis improves with multidisciplinary care and education.
- These concepts equip nurses for scientific, compassionate care using biopsychosocial approaches.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Obsessive-Compulsive and Related Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


