Please set your exam date
Drugs Used for Seizure Disorders
Study Questions
Practice Exercise 1
The nurse witnesses a patient’s seizure involving generalized contraction of the body followed by jerkiness of the arms and legs. The nurse reports that this is which type of seizure?
Explanation
A tonic-clonic seizure, previously known as a “grand mal” seizure, is the most recognized form of generalized seizure. It typically begins with a tonic phase, where the body stiffens due to sustained muscle contraction, followed by a clonic phase, in which the arms and legs exhibit rhythmic jerking movements. The seizure usually lasts one to three minutes and may be followed by a postictal phase of confusion, fatigue, or headache.
Rationale for correct answer:
C. Tonic-clonic seizures involve a sudden loss of consciousness with an initial tonic phase, characterized by generalized stiffening of muscles, often accompanied by a cry or groan and possible tongue biting. This is followed by the clonic phase, where the limbs jerk rhythmically, and breathing may be irregular.
Rationale for incorrect answers:
A. Myoclonic seizures are brief, shock-like jerks of a muscle or group of muscles. They are usually much shorter in duration and do not involve the prolonged tonic or clonic phases observed here.
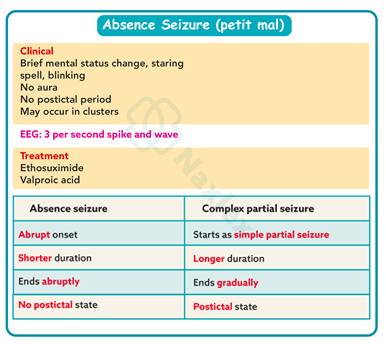
B. Petit mal seizures, also called absence seizures, are brief episodes of staring, lasting only seconds, without tonic or clonic motor activity. They are common in children and would not involve generalized stiffening and jerking.
D. Psychomotor seizures, now more commonly termed focal impaired-awareness seizures, typically arise from the temporal lobe. They involve automatisms such as lip-smacking, picking at clothes, or wandering behavior, not generalized tonic-clonic movements.
Take-home points:
• Tonic-clonic seizures feature a tonic phase of stiffening followed by a clonic phase of jerking.
• Other seizure types, such as myoclonic, absence, or focal seizures, present with different motor or behavioral patterns.
• Accurate observation and reporting of seizure characteristics are essential for diagnosis and treatment planning.
Anticonvulsants fall into several major classes, including:
Explanation
Anticonvulsants are grouped into several major classes according to their mechanism of action. These include hydantoins, barbiturates, benzodiazepines, valproates, and succinimides. Succinimides are particularly significant for the treatment of absence (petit mal) seizures, where other drug classes are less effective.
Rationale for correct answer:
C. Succinimides, such as ethosuximide (Zarontin), reduce calcium influx in thalamic neurons, which is central to the abnormal neuronal firing seen in absence seizures. They remain first-line therapy for this seizure type.
Rationale for incorrect answers:
A. Anticholinergics are not anticonvulsants; they are used in conditions like Parkinson’s disease to reduce tremors and rigidity.
B. Fluoroquinolones are a class of antibiotics. In fact, they may lower the seizure threshold, increasing the risk of seizures.
D. Dopaminergics are also unrelated to seizure treatment. They are used to increase dopamine activity in Parkinson’s disease but have no role in epilepsy management.
Take-home points:
• Succinimides are a key anticonvulsant class, especially for absence seizures.
• Other major classes include hydantoins, barbiturates, benzodiazepines, and valproates.
• Anticholinergics, fluoroquinolones, and dopaminergics are not anticonvulsants.
A patient was recently diagnosed with epilepsy by a healthcare provider after having experienced multiple episodes of convulsions accompanied by loss of consciousness.
The nurse witnesses the patient from the scenario with epilepsy as the patient suddenly had spasms of his arms and legs, falling to the floor. The patient initially lost consciousness and was quite groggy when he woke up. Which type of seizure will be documented by the nurse?
Explanation
A tonic-clonic seizure is the most recognizable type of generalized seizure and is often what people associate with the term “epileptic fit.” It begins with a tonic phase, characterized by sudden muscle stiffening and loss of consciousness, followed by a clonic phase involving rhythmic jerking movements of the arms and legs.
Rationale for correct answer:
A. The description of sudden spasms of the arms and legs, collapse, loss of consciousness, and grogginess upon awakening aligns with a tonic-clonic seizure. This type of seizure typically involves both hemispheres of the brain and has a classic postictal state, which differentiates it from other seizure types.
Rationale for incorrect answers:
B. An atonic seizure involves sudden loss of muscle tone, leading to a fall, but without the characteristic jerking movements described here. It usually lasts only seconds, and the recovery period is shorter.
C. A focal simple motor seizure may cause localized muscle twitching or jerking but does not result in loss of consciousness.
D. An absence seizure is brief, typically lasting 5–20 seconds, with sudden staring spells or lapses in awareness, but without convulsions, collapse, or postictal grogginess.
Take-home points:
• Tonic-clonic seizures involve stiffening, rhythmic jerking, loss of consciousness, and postictal confusion.
• Atonic seizures cause sudden loss of muscle tone without convulsions.
• Absence seizures present as brief lapses in awareness without postictal symptoms.
An infant is brought to the emergency department with observable twitching of the extremities and a temperature of 104.2°F as reported by his parents. The nurse will need to attend the infant.
Click to indicate the appropriate (necessary) action to take, or the not appropriate action (could be harmful).
Explanation
Infants with high fevers are at risk of developing febrile seizures, which may present with twitching of the extremities, loss of consciousness, or altered responsiveness. In the emergency setting, the nurse’s priority is to maintain airway patency, ensure safety, assess vital signs, and administer prescribed therapy while monitoring the infant’s response.
Rationale for correct answers:
Taking the infant’s vital signs is essential to monitor the severity of fever and overall physiological status.
Administering antiepileptic drugs as ordered is appropriate to control seizure activity.
Assessing the airway is crucial because infants are at high risk for airway obstruction during seizures.
Monitoring the response to therapy ensures the medication is effective and guides further treatment.
Protecting the infant from injury prevents harm from sudden movements during seizures, and having emergency equipment available ensures immediate intervention if the seizure escalates.
Rationale for incorrect answers:
Leaving the infant and mother for privacy is inappropriate during active seizure activity as continuous observation is needed to ensure safety.
Restraining the infant and tightly swaddling can cause injury, restrict movement, and worsen seizure-related trauma.
Take-home points:
• Active seizure management in infants requires airway protection, injury prevention, and continuous monitoring.
• Antiepileptic drugs should be administered as prescribed, but safety and observation take priority.
• Never leave a seizing infant unattended, and avoid restraining them during a seizure.
When caring for a patient with epilepsy who is hospitalized and is recovering from a seizure, what are the expected assessments/ interventions by the nurse during the postictal time? Select all that apply
Explanation
The postictal phase follows a seizure and is marked by confusion, fatigue, drowsiness, or temporary neurological deficits such as weakness or speech changes. Nursing care during this period is focused on maintaining airway safety, preventing injury, and assessing neurological recovery.
Rationale for correct answers:
A. Placing oxygen and suction equipment at the bedside is essential because patients may have compromised airway clearance due to secretions, decreased consciousness, or hypoventilation. Preparedness ensures immediate intervention if respiratory distress occurs.
B. Determining whether any bodily harm occurred during the seizure is critical because seizures often involve loss of motor control, falls, or biting of the tongue. Postictal assessment ensures that injuries such as lacerations, fractures, or head trauma are promptly identified and treated.
C. Evaluating weakness, speech changes, and memory loss is important since these are common postictal findings. Documenting these helps in distinguishing seizure-related deficits from possible complications such as stroke or prolonged neurological impairment.
E. Turning the patient on their side helps maintain a patent airway by allowing saliva and secretions to drain from the mouth, reducing the risk of aspiration. This is a standard nursing intervention in seizure care.
Rationale for incorrect answer:
D. Encouraging oral hygiene and brushing teeth is not appropriate immediately after a seizure, especially during the postictal period when the patient is fatigued, confused, and possibly at risk of aspiration. Oral care can be performed later when the patient is stable and fully alert.
Take-home points:
• Postictal nursing care focuses on airway management, injury assessment, and neurological monitoring.
• Side positioning prevents aspiration and supports airway safety.
• Oral hygiene is not a priority immediately after a seizure and should be delayed until the patient has fully recovered.
Practice Exercise 2
Phenytoin has been prescribed for a patient with seizures. The nurse should include which appropriate nursing intervention in the plan of care?
Explanation
Phenytoin (Dilantin) is an anticonvulsant used to control generalized tonic-clonic and partial seizures. While effective, it has a narrow therapeutic index and multiple adverse effects that require close monitoring. One of the most serious complications is blood dyscrasias, such as leukopenia, thrombocytopenia, or agranulocytosis, which can be detected early through routine CBC monitoring.
Rationale for correct answer:
B. Monitoring CBC levels is essential because phenytoin can cause suppression of bone marrow, leading to potentially life-threatening blood dyscrasias. Detecting abnormalities early allows for timely intervention to prevent severe infections, bleeding, or anemia. This makes regular blood work one of the most important nursing responsibilities in patients receiving phenytoin therapy.
Rationale for incorrect answers:
A. Reporting an abnormal phenytoin level of 18 mcg/mL would not be necessary, as this level falls within the therapeutic range of 10–20 mcg/mL. Reporting would only be indicated if levels were below 10 (risk of seizures) or above 20 (risk of toxicity).
C. Encouraging vigorous tooth brushing is not appropriate because phenytoin is associated with gingival hyperplasia. Patients should instead be taught gentle oral hygiene with a soft-bristled toothbrush and regular dental visits to minimize gum irritation and overgrowth.
D. Stopping the drug immediately when urine turns pinkish-red or reddish-brown is not appropriate because this is a harmless side effect of phenytoin. Discontinuation should never be sudden, as it may precipitate status epilepticus. Patients should be reassured that urine discoloration is expected and benign.
Take-home points:
• Monitor CBC regularly to detect blood dyscrasias early in patients taking phenytoin.
• Phenytoin levels between 10–20 mcg/mL are therapeutic—values within this range do not require reporting.
• Educate patients on gentle oral care and reassure them about harmless urine discoloration.
When administering phenytoin, the nurse realizes more teaching is needed if the patient makes which statement?
Explanation
Phenytoin (Dilantin) is an anticonvulsant used to manage tonic-clonic and partial seizures. It has strict administration guidelines because its absorption can be altered by food, antacids, and enteral feedings. Nurses must ensure patients understand how to take the medication correctly to maintain stable therapeutic levels and reduce the risk of breakthrough seizures or toxicity.
Rationale for correct answer:
C. Taking phenytoin 1 hour before meals is not recommended. Phenytoin should generally be taken with or immediately after meals to minimize gastrointestinal irritation and promote steady absorption. Taking it on an empty stomach increases the likelihood of stomach upset and inconsistent drug absorption.
Rationale for incorrect answers:
A. “I must shake the oral suspension very well before pouring it in the dose cup.” This reflects proper knowledge. Phenytoin suspension must be shaken to ensure even distribution of the drug because it can settle, leading to inaccurate dosing if not mixed.
B. “I cannot drink alcoholic beverages when taking phenytoin.” This statement is appropriate because alcohol can alter phenytoin levels, either raising toxicity risk with acute intake or lowering seizure control with chronic use. Avoiding alcohol is an important safety precaution.
D. “I will need to get periodic dental checkups.” This is accurate since phenytoin commonly causes gingival hyperplasia, and regular dental visits combined with good oral hygiene help reduce complications.
Take-home points:
• Phenytoin should be taken with food to improve absorption and minimize GI upset.
• Alcohol interacts with phenytoin and must be avoided to maintain safe drug levels.
• Regular dental care is essential due to the risk of gingival hyperplasia.
The nurse should monitor the patient receiving phenytoin for which adverse effect?
Explanation
Phenytoin (Dilantin) is widely used to treat generalized tonic-clonic and partial seizures, but it carries a risk of several serious adverse effects. One of the most concerning complications is blood dyscrasias, which can manifest as thrombocytopenia. When platelet counts drop, the patient may experience easy bruising, petechiae, or nosebleeds, all of which require prompt monitoring and intervention.
Rationale for correct answer:
B. Nosebleeds can indicate thrombocytopenia or another blood disorder associated with phenytoin use. Because bleeding tendencies are an early sign of hematologic toxicity, the nurse must closely monitor for epistaxis, unusual bruising, or bleeding gums and report these findings immediately.
Rationale for incorrect answers:
A. Psychosis is not a common adverse effect of phenytoin. While phenytoin can cause confusion or mood changes at toxic levels, psychosis is not typically associated with its use.
C. Hypertension is not linked to phenytoin therapy. If anything, phenytoin toxicity may cause hypotension, particularly when administered intravenously too rapidly.
D. Gum erosion is not a known adverse effect of phenytoin. Instead, the drug is associated with gingival hyperplasia, or overgrowth of gum tissue, not erosion or breakdown.
Take-home points:
• Nosebleeds may signal thrombocytopenia, a serious adverse effect of phenytoin.
• Phenytoin toxicity does not cause hypertension but may lead to hypotension if given IV too quickly.
• Oral complications are related to gingival hyperplasia, not gum erosion.
An 8-year-old boy is evaluated and diagnosed with absence seizures. He is started on ethosuximide (Zarontin). Which information should the nurse provide the parents?
Explanation
Ethosuximide (Zarontin) is the first-line medication for absence seizures, especially in children. It works by blocking T-type calcium channels in thalamic neurons, thereby reducing the abnormal neuronal activity that causes petit mal seizures. Although it is generally well tolerated, ethosuximide can have long-term effects on growth and development, so close monitoring is important during therapy.
Rationale for correct answer:
B. Monitoring height and weight is essential because ethosuximide therapy in children may affect appetite, gastrointestinal tolerance, and overall growth patterns. Regular tracking ensures that the child is developing normally and that the medication is not causing growth suppression or nutritional compromise.
Rationale for incorrect answers:
A. After-school sports activities will need to be stopped is not true. Ethosuximide helps control seizures so that children can continue a normal lifestyle, including participation in sports, once seizures are well managed. Physical activity does not increase seizure risk.
C. Fractures may occur, so increase the amount of vitamin D and calcium-rich foods in the diet is more relevant to long-term therapy with enzyme-inducing anticonvulsants such as phenytoin, carbamazepine, or phenobarbital, which can affect bone metabolism. Ethosuximide is not typically associated with osteoporosis or fracture risk.
D. Avoid dehydration with activities and increase fluid intake is not a key teaching point for ethosuximide. While maintaining hydration is always healthy, ethosuximide does not cause significant dehydration or renal effects that require special fluid precautions.
Take-home points:
• Ethosuximide is the first-line drug for absence seizures in children.
• Growth monitoring through height and weight checks is essential during therapy.
• Children can continue normal activities, including sports, once seizures are controlled.
A client has been taking phenytoin (Dilantin) for control of generalized seizures, tonic–clonic type. The client is admitted to the medical unit with symptoms of nystagmus, confusion, and ataxia. What change in the phenytoin dosage does the nurse anticipate will be made based on these symptoms?
Explanation
Phenytoin (Dilantin) is an anticonvulsant used to manage generalized tonic–clonic seizures. It has a narrow therapeutic index, with the recommended serum range being 10–20 mcg/mL. Toxicity can occur quickly if levels rise above this range, and classic symptoms of phenytoin toxicity include nystagmus, confusion, and ataxia.
Rationale for correct answer:
B. Decreasing the dosage is the expected change because the client is exhibiting clear signs of phenytoin toxicity. Reducing the dose will help bring serum drug levels back into the therapeutic range, alleviating CNS side effects while maintaining seizure control. The healthcare provider may also order phenytoin levels to confirm toxicity and adjust the dosage accordingly.
Rationale for incorrect answers:
A. Increasing the dosage would be unsafe since the patient is already experiencing toxicity. Higher doses would worsen CNS depression and put the client at risk of life-threatening complications.
C. Leaving the dosage unchanged and considering these symptoms unrelated would be inappropriate because the symptoms strongly match phenytoin toxicity and cannot be ignored.
D. Keeping the dosage the same and adding another antiseizure medication is not correct at this stage. The priority is to address toxicity by lowering the dose, not by adding additional medications.
Take-home points:
• Nystagmus, ataxia, and confusion are hallmark signs of phenytoin toxicity.
• The therapeutic serum range is 10–20 mcg/mL; levels above this increase risk of adverse effects.
• Dosage reduction is the appropriate intervention to resolve toxicity while maintaining seizure control.
Practice Exercise 3
A nurse is reviewing a new prescription for oxcarbazepine (Trileptal) with a female client who has partial seizures. Which of the following statements by the nurse are appropriate? Select all that apply
Explanation
Oxcarbazepine (Trileptal) is an anticonvulsant commonly prescribed for partial seizures. It stabilizes neuronal membranes by blocking voltage-sensitive sodium channels, which helps reduce abnormal electrical activity in the brain. While effective, the medication has several important safety considerations related to electrolyte balance, drug interactions, central nervous system effects, and hypersensitivity reactions.
Rationale for correct answers:
A. “Use caution if given a prescription for a diuretic medication.” This teaching is appropriate because oxcarbazepine can cause hyponatremia, and concurrent use with diuretics increases this risk. Nurses must reinforce the importance of monitoring for symptoms such as nausea, confusion, or muscle weakness.
B. “Consider using an alternate form of contraception.” This is correct because oxcarbazepine can decrease the effectiveness of oral contraceptives through hepatic enzyme induction. Women of childbearing age should be counseled to use non-hormonal or additional barrier methods of contraception.
D. “Avoid driving until you see how the medication affects you.” This teaching is accurate since oxcarbazepine can cause CNS side effects such as dizziness, drowsiness, and blurred vision. These effects can impair reaction times, making it unsafe to drive or operate heavy machinery until the client knows how they respond to the drug.
E. “Notify your provider if you develop a skin rash.” This is appropriate because oxcarbazepine carries a risk of serious dermatologic reactions such as Stevens-Johnson syndrome or toxic epidermal necrolysis. Any rash, especially in the early weeks of therapy, should be reported immediately.
Rationale for incorrect answer:
C. “Chew gum to increase saliva production.” This statement is not appropriate because oxcarbazepine does not commonly cause dry mouth. Instead, its side effect profile is more focused on CNS depression, hyponatremia, and skin reactions.
Take-home points:
• Oxcarbazepine can cause hyponatremia—use caution with diuretics.
• It decreases the effectiveness of oral contraceptives—advise alternate contraception.
• CNS effects and skin rash are key safety concerns requiring patient education.
The nurse is administering valproic acid (Depakote) to a patient. The nurse checks the laboratory values and finds a serum range for valproic acid of 200 mcg/ml. What should the nurse do?
Explanation
Valproic acid (Depakote) is a broad-spectrum anticonvulsant used to manage generalized and partial seizures, as well as bipolar disorder and migraine prophylaxis. The therapeutic serum range is 50–100 mcg/mL. Levels significantly above this range place the patient at risk for toxicity, which can lead to CNS depression, hepatotoxicity, pancreatitis, and life-threatening complications.
Rationale for correct answer:
D. Holding the medication and notifying the health care provider is the safest course of action when the serum level is 200 mcg/mL. This value is well above the therapeutic range, indicating toxic accumulation. Administering another dose could worsen toxicity, so the nurse must stop the medication and immediately inform the provider for further evaluation, dosage adjustment or supportive care.
Rationale for incorrect answers:
A. Increasing the daily dose to get the patient’s level to a therapeutic range is inappropriate because the serum level is already too high, not too low. Giving more of the drug would worsen toxicity.
B. Holding the morning dose but giving the other scheduled dosages for the day would still place the patient at risk because the serum level is critically elevated. The drug should not be given again until the provider evaluates and adjusts therapy.
C. Asking the patient if he is having any adverse effects from the medication may help assess symptoms but does not address the dangerously high level. Even in the absence of symptoms, the serum concentration is toxic and requires immediate intervention.
Take-home points:
• Valproic acid has a therapeutic range of 50–100 mcg/mL; 200 mcg/mL is toxic.
• The nurse should hold the drug and notify the provider when serum levels are critically elevated.
• Toxic levels can lead to severe CNS and hepatic complications, making early intervention essential.
The nurse is caring for a 72-year-old client taking gabapentin (Neurontin) for a seizure disorder. Because of this client’s age, the nurse would establish which nursing diagnosis related to the drug’s common adverse effects?
Explanation
Gabapentin (Neurontin) is an anticonvulsant often used for seizure disorders and neuropathic pain. In older adults, it requires close monitoring because age-related pharmacokinetic changes increase the risk of central nervous system side effects, particularly dizziness, drowsiness, and impaired coordination. These effects greatly heighten the likelihood of falls in the elderly, making fall prevention a key nursing priority.
Rationale for correct answer:
D. Risk for Falls is the most appropriate nursing diagnosis for a 72-year-old client on gabapentin. Older adults are especially vulnerable to gabapentin’s adverse effects of ataxia, dizziness, sedation, and visual disturbances, all of which impair balance and mobility. This places them at higher risk for falls, fractures, and subsequent complications, which can be severe in geriatric patients.
Rationale for incorrect answers:
A. Risk for Deficient Fluid Volume is not associated with gabapentin use. The drug does not cause significant fluid loss, dehydration, or diuresis.
B. Risk for Impaired Verbal Communication is not relevant, since gabapentin does not typically affect speech or language function. While it may cause mild confusion in some patients, communication impairment is not a primary concern.
C. Risk for Constipation is not a common adverse effect of gabapentin. Constipation may occur with some other anticonvulsants or opioids, but it is not a hallmark issue for this drug.
Take-home points:
• Gabapentin in older adults increases fall risk due to dizziness, sedation, and ataxia.
• Fall prevention interventions, such as assistance with ambulation and safety education, are critical.
• Other potential issues like constipation or fluid imbalance are not major concerns with gabapentin.
Teaching for a client receiving carbamazepine (Tegretol) should include instructions that the client should immediately report which symptom?
Explanation
Carbamazepine (Tegretol) is an anticonvulsant used for partial and generalized seizures, trigeminal neuralgia, and mood stabilization. While effective, it carries significant risks, particularly hematologic toxicity and serious dermatologic reactions. The most urgent of these is Stevens–Johnson syndrome (SJS) or toxic epidermal necrolysis (TEN), both of which may begin as a blister-like rash. Immediate recognition and discontinuation of the drug are crucial to prevent life-threatening complications.
Rationale for correct answer:
D. Blister-like rash requires urgent reporting because it can signal the onset of Stevens–Johnson syndrome or TEN. These conditions involve widespread skin detachment and mucous membrane involvement and are medical emergencies. Early discontinuation of carbamazepine can be lifesaving.
Rationale for incorrect answers:
A. Leg cramping may be uncomfortable but is not a serious or life-threatening adverse effect of carbamazepine.
B. Blurred vision can occur due to dose-related CNS effects such as diplopia or dizziness, but this is not as urgent as a blister-like rash.
C. Lethargy may also result from CNS depression associated with carbamazepine, but it does not demand the same immediate intervention as a severe dermatologic reaction.
Take-home points:
• Carbamazepine can cause life-threatening skin reactions like SJS/TEN, signaled by blister-like rash.
• Any rash in a patient taking carbamazepine must be reported immediately.
• Other side effects such as blurred vision, lethargy, or mild muscle issues are less urgent but still warrant monitoring.
The nurse is preparing to administer phenobarbital. The order reads: “Give phenobarbital, IV, 2 mg/kg/day at 0900.” The patient weighs 253 pounds. How many milligrams will the patient receive for each dose?
Explanation
A critical part of the nurses’s role involves medication administration. Accurate dosage calculation is a fundamental skill that ensures patient safety and therapeutic efficacy. By carefully converting units and following the healthcare provider's orders, nurses prevent medication errors and this contributes to positive patient outcomes.
Rationale for correct answer:
The step-by-step calculation to determine the phenobarbital dose is as follows:
Step 1: Convert Patient Weight from Pounds to Kilograms
The medication order is based on the patient's weight in kilograms, so you must first convert the patient's weight from pounds (lbs) to kilograms (kg). The conversion factor is 1kg=2.2lbs.
253lbs÷2.2lbs/kg=115kg
Step 2: Calculate the Total Daily Dose
Next, multiply the patient's weight in kilograms by the ordered dose of phenobarbital (2mg/kg/day) to find the total daily dose in milligrams (mg).
115kg×2mg/kg/day=230mg/day
Step 3: Determine the Dose Per Administration
The order specifies to give the medication once daily, so the total daily dose is the same as the dose for each administration.
The patient will receive 230 mg of phenobarbital for each dose.
Take-home points:
- Unit Conversion is essential: 1kg=2.2lbs.
- Double-Check the Calculation
- The basic formula for dosage calculation is: Dose=PatientWeight(kg)×DoseperWeight(mg/kg)
Comprehensive Questions
A nurse is preparing to administer medication to a client who has absence seizures. Which of the following medications are appropriate for the nurse to administer? Select all that apply
Explanation
Absence seizures are brief episodes of impaired consciousness caused by abnormal electrical activity in the brain, most common in children. The goal of therapy is to suppress the abnormal neuronal firing while minimizing side effects. Ethosuximide, valproic acid, and lamotrigine are the preferred medications for absence seizures because they specifically target the mechanisms involved in this seizure type.
Rationale for correct answers:
B. Ethosuximide (Zarontin) is considered the first-line treatment for absence seizures. It works by reducing calcium influx through T-type calcium channels in thalamic neurons, which play a key role in generating absence seizure activity. Its effectiveness and relatively favorable side effect profile make it the gold standard for treating absence seizures.
E. Valproic acid (Depakote) is another highly effective agent for absence seizures. In addition to blocking sodium channels, it increases brain levels of GABA, the main inhibitory neurotransmitter, which reduces seizure activity. It is often used when a client has both absence seizures and other seizure types, such as generalized tonic-clonic seizures, because of its broad-spectrum activity.
F. Lamotrigine (Lamictal) is also appropriate for absence seizures. It works mainly by inhibiting sodium channels and stabilizing neuronal membranes. While not always first-line, lamotrigine is considered an acceptable alternative or adjunct for absence seizures, especially when ethosuximide or valproic acid are not tolerated.
Rationale for incorrect answers:
A. Phenytoin (Dilantin) is not effective for absence seizures and may even worsen seizure control in these patients. It is primarily used for generalized tonic-clonic and partial seizures.
C. Gabapentin (Neurontin) is not indicated for absence seizures. It is more commonly used for partial seizures and neuropathic pain rather than generalized seizure types.
D. Carbamazepine (Tegretol) can actually exacerbate absence seizures, making it inappropriate for this condition. It is more effective in treating partial and generalized tonic-clonic seizures.
Take-home points:
• Ethosuximide is the first-line treatment for absence seizures.
• Valproic acid and lamotrigine are also effective options, particularly when mixed seizure types are present.
• Phenytoin, gabapentin, and carbamazepine are not suitable for absence seizures and may worsen them.
A patient is having absence (petit mal) seizures. Which of the following does the nurse expect to be prescribed for this type of seizures? Select all that apply
Explanation
Absence (petit mal) seizures are brief episodes of impaired consciousness, often seen in children, that involve staring spells without major motor involvement. The goal of treatment is to suppress the abnormal thalamic neuronal activity responsible for these seizures. Valproic acid, clonazepam, and ethosuximide are effective agents because they specifically target the neuronal pathways involved in absence seizures, while other common anticonvulsants may worsen them.
Rationale for correct answers:
C. Valproic acid (Depakote) is highly effective in controlling absence seizures. It works by increasing brain levels of GABA and blocking sodium channels, thereby stabilizing neuronal firing. It is especially useful in patients who have absence seizures along with other generalized seizure types, making it a broad-spectrum option.
D. Clonazepam (Klonopin), a benzodiazepine, can also be prescribed for absence seizures. It enhances GABA-mediated inhibition in the central nervous system, reducing seizure activity. While effective, it is often used as an adjunct or second-line option due to the potential for tolerance and sedation.
E. Ethosuximide (Zarontin) is considered the first-line therapy for absence seizures. It specifically reduces abnormal thalamic activity by blocking T-type calcium channels, which are central to the pathophysiology of petit mal seizures.
Rationale for incorrect answers:
A. Phenytoin (Dilantin) is not effective in absence seizures and can actually worsen seizure frequency. Its use is reserved for tonic-clonic and partial seizures.
B. Phenobarbital (Luminal) is more effective for generalized tonic-clonic and focal seizures. It does not adequately control absence seizures and is rarely prescribed for this type.
Take-home points:
• Ethosuximide is the first-line drug for absence seizures.
• Valproic acid and clonazepam are also effective, particularly for patients with multiple seizure types.
• Phenytoin and phenobarbital are not suitable and may worsen absence seizures.
A patient is admitted to the emergency department with status epilepticus. Which drug should the nurse most likely prepare to administer to this patient? Select all that apply
Explanation
Status epilepticus is a neurological emergency characterized by continuous seizure activity lasting more than five minutes or recurrent seizures without recovery in between. It requires rapid intervention to stop seizures and prevent permanent brain injury. The first-line treatment is the immediate administration of intravenous benzodiazepines such as diazepam or midazolam, which act quickly to enhance GABA activity and suppress abnormal neuronal firing.
Rationale for correct answers:
A. Diazepam (Valium) is commonly used in emergency settings because it has a rapid onset of action when given IV or rectally. It enhances GABA activity, producing quick CNS depression that terminates seizure activity. However, its effect is relatively short-lived, so it is usually followed by a longer-acting anticonvulsant for sustained seizure control.
B. Midazolam (Versed) is another benzodiazepine frequently used for status epilepticus. It can be given IV, IM, or intranasally, making it useful when IV access is difficult. Like diazepam, it provides fast seizure control but also requires follow-up with maintenance therapy due to its shorter duration of action.
Rationale for incorrect answers:
C. Gabapentin (Neurontin) is not appropriate for status epilepticus because it is used primarily for partial seizures and neuropathic pain. Its onset of action is too slow for emergency seizure management.
D. Levetiracetam (Keppra) is often used as a maintenance or adjunct therapy for seizure control but is not first-line for acute status epilepticus. It may be administered later for ongoing prevention after the emergency is stabilized.
E. Topiramate (Topamax) is an anticonvulsant effective for partial and generalized seizures, but it is not used in emergencies. Its oral formulation and slower onset of action make it unsuitable for immediate management of status epilepticus.
Take-home points:
• Benzodiazepines such as diazepam and midazolam are the drugs of choice for status epilepticus.
• These drugs act rapidly by enhancing GABA-mediated inhibition in the CNS.
• Other anticonvulsants like gabapentin, levetiracetam, and topiramate are used for long-term seizure control, not acute emergencies.
The nurse is providing education for a 12-year-old client with partial seizures currently prescribed valproic acid (Depakene). The nurse will teach the client and the parents to immediately report which symptom?
Explanation
Valproic acid (Depakene) is a broad-spectrum anticonvulsant used for partial and generalized seizures. While generally effective, it carries a risk of serious hepatotoxicity and pancreatitis, both of which can be life-threatening if not detected early. Nurses must ensure that families understand which symptoms indicate urgent complications requiring immediate medical attention.
Rationale for correct answer:
A. Increasing or severe abdominal pain should be reported immediately because it may signal acute pancreatitis, a rare but dangerous adverse effect of valproic acid. Other associated symptoms may include nausea, vomiting, and anorexia. Prompt recognition and treatment are critical since pancreatitis can rapidly progress and lead to severe morbidity or death if unaddressed.
Rationale for incorrect answers:
B. Decreased or foul taste in the mouth can occasionally occur with valproic acid but is a benign side effect that does not require urgent intervention. It may be bothersome but is not life-threatening.
C. Pruritus and dry skin are not common or severe adverse effects of valproic acid. Mild rashes may occur but are not typically significant unless accompanied by systemic symptoms.
D. Bone and joint pain is not a key adverse effect of valproic acid. Concerns about bone health are more relevant to other long-term antiepileptic drugs such as phenytoin or carbamazepine, which affect vitamin D metabolism.
Take-home points:
• Severe abdominal pain with valproic acid may indicate pancreatitis and requires immediate reporting.
• Other mild side effects, such as taste changes or skin dryness, are not medical emergencies.
• Family education is essential to ensure early recognition of serious complications.
Which of the following medications may be used to treat partial seizures? Select all that apply
Explanation
Partial seizures (also called focal seizures) originate in a specific area of the brain and may remain localized or spread to become generalized. The primary medications for treating partial seizures are those that stabilize neuronal membranes and reduce abnormal electrical activity.
Rationale for correct answers:
A. Phenytoin (Dilantin) is appropriate because it works by blocking sodium channels, thereby decreasing neuronal excitability. It has long been used for partial seizures as well as generalized tonic–clonic seizures.
B. Valproic acid (Depakene) is effective for a broad spectrum of seizures, including partial seizures, generalized seizures, and absence seizures. Its mechanism includes increasing GABA levels and stabilizing neuronal firing.
D. Carbamazepine (Tegretol) is a first-line drug for partial seizures. Like phenytoin, it reduces repetitive firing of neurons through sodium channel blockade, making it highly effective in focal epilepsy.
Rationale for incorrect answers:
C. Diazepam (Valium) is primarily used as a short-term agent for status epilepticus or acute seizure control due to its rapid onset. It is not used as a maintenance therapy for partial seizures.
E. Ethosuximide (Zarontin) is used specifically for absence seizures. It works by reducing calcium currents in thalamic neurons, but it has no role in treating partial seizures.
Take-home points:
• Phenytoin, valproic acid, and carbamazepine are effective long-term therapies for partial seizures.
• Diazepam is reserved for acute seizure emergencies, not maintenance therapy.
• Ethosuximide is limited to absence seizures and not effective for partial seizures.
The nurse is preparing to give medications. Which is an appropriate nursing action for intravenous (IV) phenytoin (Dilantin)? Select all that apply
Explanation
Phenytoin (Dilantin) is an anticonvulsant commonly given intravenously when rapid seizure control is required, such as in status epilepticus. Because of its chemical properties, special precautions are necessary during IV administration to prevent complications such as precipitation, phlebitis, or cardiovascular collapse.
Rationale for correct answers:
B. Administer in normal saline solutions is appropriate because phenytoin is incompatible with dextrose-containing solutions. When mixed with dextrose, phenytoin precipitates, making the solution unsafe for administration. Normal saline is the only suitable diluent.
D. Use a filter for IV infusions is correct because phenytoin can crystallize or precipitate in solution. Using an in-line filter prevents the infusion of particulate matter into the bloodstream, which could cause phlebitis or emboli.
Rationale for incorrect answers:
A. Give IV doses via rapid IV push is unsafe. Phenytoin must be administered slowly (generally no faster than 50 mg/min in adults) to avoid severe cardiovascular effects such as hypotension and arrhythmias. Rapid IV push greatly increases these risks.
C. Administer in dextrose solutions is contraindicated because phenytoin is incompatible with glucose-containing solutions, leading to precipitation and loss of drug potency.
E. Ensure continuous infusion of the drug is not recommended. Phenytoin is typically given as intermittent dosing, not continuous infusion, to maintain therapeutic levels while reducing the risk of adverse effects.
Take-home points:
• Phenytoin should always be diluted in normal saline, never dextrose.
• An in-line filter must be used to prevent precipitation from entering circulation.
• Avoid rapid IV push or continuous infusion to reduce risk of cardiovascular complications.
The nurse is reviewing the drugs currently taken by a patient who will be starting drug therapy with carbamazepine (Tegretol). Which drug may raise a concern for interactions?
Explanation
Carbamazepine (Tegretol) is an anticonvulsant used for partial and generalized seizures, trigeminal neuralgia, and sometimes bipolar disorder. It is a potent inducer of hepatic enzymes, meaning it speeds up the metabolism of many drugs. This property creates significant drug–drug interaction risks, especially with medications metabolized by the liver.
Rationale for correct answer:
B. Acetaminophen (Tylenol) raises concern when taken with carbamazepine because both drugs are hepatotoxic. Using them together increases the risk of liver damage. In addition, carbamazepine accelerates the metabolism of acetaminophen, which can lead to toxic metabolites and heighten the potential for hepatotoxicity.
Rationale for incorrect answers:
A. Digoxin (Lanoxin) is not primarily affected by carbamazepine’s hepatic enzyme–inducing effect, and the interaction risk is low. Digoxin levels are more commonly influenced by renal function and electrolyte imbalances.
C. Diazepam (Valium) can be metabolized more quickly in the presence of carbamazepine, leading to reduced therapeutic effect. While this is an interaction, it is not as clinically concerning as the risk of hepatotoxicity with acetaminophen.
D. Pantoprazole (Protonix) is a proton pump inhibitor and has no significant interaction with carbamazepine, as it is not primarily metabolized by the same liver enzyme pathways.
Take-home points:
• Carbamazepine induces liver enzymes, increasing the risk of hepatotoxicity with acetaminophen.
• Drug interactions with carbamazepine are common and require careful monitoring.
• Liver function tests should be closely monitored when carbamazepine is combined with other hepatotoxic drugs.
Which response would the nurse expect to find in a patient with a phenytoin (Dilantin) level of 25 mcg/mL?
Explanation
Phenytoin (Dilantin) is a widely used anticonvulsant for generalized tonic–clonic and partial seizures. The usual therapeutic serum range is 10–20 mcg/mL. Levels above this range indicate toxicity, which can cause serious neurologic side effects. Nurses must be able to recognize these signs promptly to prevent harm.
Rationale for correct answer:
A. Ataxia is expected at a phenytoin level of 25 mcg/mL because this value is above the therapeutic range and into the toxic range. Neurological toxicity is the hallmark of phenytoin overdose, with symptoms such as nystagmus, slurred speech, confusion, and ataxia.
Rationale for incorrect answers:
B. Hypertension is not a typical finding with phenytoin toxicity. Instead, rapid IV administration of phenytoin can cause hypotension and arrhythmias, but hypertension is not expected with high serum levels.
C. Seizures are unlikely when the level is 25 mcg/mL because this is above the therapeutic range. Seizures usually occur when the phenytoin level is too low, not too high.
D. No unusual response; this level is therapeutic is incorrect because 25 mcg/mL exceeds the therapeutic range. At this level, the patient is at risk for toxicity rather than seizure control alone.
Take-home points:
• Therapeutic serum range for phenytoin is 10–20 mcg/mL; levels above 20 suggest toxicity.
• Ataxia, nystagmus, and confusion are common signs of phenytoin overdose.
• Seizures occur with subtherapeutic levels, while neurologic toxicity occurs with supratherapeutic levels.
The nurse is assessing a newly admitted patient who has a history of seizures. During the assessment, the patient has a generalized seizure that does not stop for several minutes. The nurse expects that which drug will be ordered for this condition?
Explanation
A seizure lasting several minutes without stopping indicates status epilepticus, a life-threatening emergency requiring immediate treatment to prevent brain injury and death. The priority in this situation is to stop the seizure quickly using a drug that acts rapidly on the central nervous system.
Rationale for correct answer:
D. Diazepam (Valium) is the drug of choice for acute management of status epilepticus because it is a benzodiazepine with rapid onset of action. It enhances the effects of GABA, the brain’s major inhibitory neurotransmitter, quickly calming abnormal electrical activity. Diazepam can be administered intravenously, allowing fast seizure control.
Rationale for incorrect answers:
A. Valproic acid (Depakote) is effective for generalized and partial seizures but is not the first-line treatment for status epilepticus. It has a slower onset of action compared to benzodiazepines and is not suitable in an acute emergency setting.
B. Gabapentin (Neurontin) is primarily used for partial seizures and neuropathic pain. It does not act quickly enough to stop prolonged seizures and is not indicated for status epilepticus.
C. Carbamazepine (Tegretol) is used for partial and generalized tonic–clonic seizures but is not effective in managing acute, ongoing seizures. Like valproic acid, it is used for maintenance therapy, not emergency intervention.
Take-home points:
• Diazepam is the first-line drug for status epilepticus due to its rapid CNS action.
• Maintenance drugs like valproic acid and carbamazepine are not useful in emergencies.
• Prompt recognition and treatment of status epilepticus are critical to prevent permanent brain damage.
The nurse is administering an antiepileptic drug and will follow which guidelines? Select all that apply
Explanation
Antiepileptic drugs (AEDs) are prescribed to control seizure activity by stabilizing neuronal firing and preventing abnormal electrical discharges. Safe and effective management requires strict adherence to dosing schedules, ongoing monitoring for side effects, and coordination with the prescriber if problems arise.
Rationale for correct answers:
A. Monitor the patient for drowsiness is essential because many AEDs cause central nervous system depression. Sedation, dizziness, and fatigue are common adverse effects, especially when therapy is first started or doses are adjusted.
C. Give the medication at the same time every day is critical to maintain stable blood drug levels, which help prevent seizure activity. Irregular dosing increases the risk of subtherapeutic levels and breakthrough seizures.
E. Notify the prescriber if the patient is unable to take the medication is vital because abrupt discontinuation of AEDs can lead to status epilepticus, a medical emergency. If a dose is missed or the patient cannot tolerate oral administration, alternative routes or adjustments should be discussed with the provider immediately.
Rationale for incorrect answers:
B. Medications may be stopped if seizure activity disappears is incorrect because AEDs must never be stopped abruptly, even if seizures appear controlled. Seizure disorders are typically chronic, and stopping therapy suddenly increases the risk of rebound seizures or status epilepticus.
D. Give the medication on an empty stomach is not required for most AEDs. In fact, many are better tolerated when taken with food to reduce gastric irritation or nausea.
Take-home points:
• AEDs must be taken consistently at the same time each day to maintain therapeutic levels.
• Do not stop antiepileptic medications suddenly, even if seizures appear controlled.
• Report inability to take the drug immediately to prevent breakthrough seizures or status epilepticus.
The nurse is providing education for a patient who will be taking an antiepileptic drug for the first time. Which statement by the patient indicates that further teaching is indicated?
Explanation
Antiepileptic drugs are prescribed to reduce or prevent seizures, but they do not cure the underlying condition. Because seizures can still occur even when drug levels are therapeutic, patient safety education is essential. Nurses must correct misconceptions about lifestyle adjustments, especially regarding driving and activity restrictions.
Rationale for correct answer:
D. “I can drive to work again once my drug levels are normal.” indicates a misunderstanding. Even with therapeutic drug levels, patients may still be at risk for seizures. Driving restrictions are based on seizure control, not just medication levels. Most regions require patients to be seizure-free for a specific period (commonly 6–12 months) before resuming driving. This statement shows the need for further teaching.
Rationale for incorrect answers:
A. “I will take the medicine at the same time every day.” demonstrates proper understanding. Consistency in timing ensures stable serum drug concentrations and reduces the risk of breakthrough seizures.
B. “I will check with my doctor before taking any over-the-counter drugs.” is correct because many OTC medications can interact with AEDs, either reducing effectiveness or increasing toxicity.
C. “I will keep the appointments to check my bloodwork.” is also appropriate. Monitoring drug levels, liver function, and blood counts is crucial to ensure safety and effectiveness of AED therapy.
Take-home points:
• Driving restrictions depend on seizure control, not just therapeutic blood levels.
• AEDs must be taken consistently and monitored with regular lab tests.
• Patients should consult their provider before using OTC drugs due to potential interactions.
A 15-year-old patient has a tonic-clonic seizure disorder and is prescribed phenytoin. Which term best describes the absorption rate of oral phenytoin?
Explanation
Phenytoin is a first-line antiepileptic drug commonly used for tonic–clonic and partial seizures. Its absorption and metabolism are unique compared to many other medications, and this has important implications for dosing, monitoring, and therapeutic drug levels.
Rationale for correct answer:
B. Slow absorption best describes oral phenytoin. After ingestion, phenytoin is absorbed gradually in the gastrointestinal tract. Because of this slow absorption and its nonlinear (zero-order) kinetics, small changes in dose can cause disproportionate increases in serum drug levels, making careful monitoring essential.
Rationale for incorrect answers:
A. Rapid absorption is not correct because phenytoin does not enter the bloodstream quickly. Unlike benzodiazepines, which act rapidly in acute seizure management, phenytoin requires time to build therapeutic levels.
C. Erratic absorption is not the best description. While food and formulations can slightly affect absorption, phenytoin is generally absorbed consistently, just at a slow rate.
D. Moderate absorption does not accurately describe phenytoin’s pharmacokinetics. The defining feature is slow and prolonged absorption, not moderate or variable.
Take-home points:
• Oral phenytoin is absorbed slowly, requiring careful dose adjustments.
• Nonlinear kinetics mean small dose changes can cause large shifts in serum levels.
• Therapeutic monitoring is essential, with a target range of 10–20 mcg/mL.
An 11-year-old patient develops myoclonic seizures. Which potential adverse reaction makes it unlikely that valproate will be prescribed for this patient?
Explanation
Valproate (valproic acid, Depakote) is a broad-spectrum antiepileptic drug effective against multiple seizure types, including myoclonic, absence, and generalized tonic–clonic seizures. However, its use in children raises special safety concerns because of the risk of serious organ toxicity.
Rationale for correct answer:
A. Liver toxicity is the primary adverse reaction that makes valproate less favorable in children, especially those younger than 2 years. Valproate has been linked to fatal hepatotoxicity, and children are at higher risk due to immature liver enzyme systems. For this reason, liver function must be monitored closely.
Rationale for incorrect answers:
B. CNS sedation can occur with many antiepileptics, including valproate, but it is usually mild to moderate and manageable. Sedation does not pose the same life-threatening risk as hepatotoxicity.
C. Respiratory depression is not a typical adverse effect of valproate. This reaction is more associated with benzodiazepines or barbiturates, especially when given intravenously or in overdose.
D. Hyperthermia is not a known complication of valproate. In fact, valproate is not associated with temperature dysregulation.
Take-home points:
• Hepatotoxicity is the most serious adverse effect of valproate, particularly in children.
• Liver function monitoring is mandatory during therapy.
• Other adverse effects like sedation are usually manageable, but hepatotoxicity may be fatal
Barbiturate anticonvulsants are effective in treating all of these seizure types except:
Explanation
Barbiturate anticonvulsants, such as phenobarbital, act by enhancing the effect of GABA, the brain’s primary inhibitory neurotransmitter. This increases the threshold for neuronal firing and helps control abnormal electrical activity. They are effective for a wide range of seizures, particularly tonic–clonic and partial seizures, as well as for febrile seizures in children.
Rationale for correct answer:
D. Absence seizures are not treated with barbiturates. The drug of choice is ethosuximide, a succinimide, or alternatively valproic acid. Barbiturates do not target the thalamic calcium channel mechanisms responsible for absence seizures and therefore provide no benefit.
Rationale for incorrect answers:
A. Partial seizures can be managed with barbiturates because of their general CNS depressant and GABA-enhancing effects.
B. Tonic–clonic seizures respond well to phenobarbital, making it one of the oldest and most reliable treatments for generalized seizures.
C. Febrile seizures in children can be treated with barbiturates such as phenobarbital when recurrent or severe, although they are not first-line anymore due to sedation and cognitive side effects.
Take-home points:
• Barbiturates are effective for partial, tonic–clonic, and febrile seizures.
• They are not effective for absence seizures; ethosuximide or valproic acid is preferred.
• Phenobarbital is one of the oldest anticonvulsants still in use, but its sedative and dependence potential limit long-term use.
Exams on Drugs Used for Seizure Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
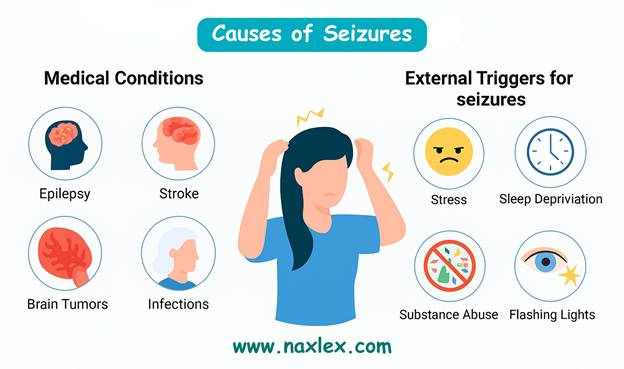
- Compare and contrast the terms seizures, convulsions, and epilepsy.
- Recognize possible causes and risk factors of seizures.
- Relate signs and symptoms to the major types of seizures.
- Categorize drugs used in the treatment of seizure disorders based on their classification and mechanism of action.
- Explain the general principles and goals of antiepileptic drug therapy.
- For each drug class, identify representative examples and explain their mechanism of action, primary uses, and important adverse effects.
- Describe the nurse’s role in the pharmacologic management of seizures, including both acute seizures and long-term epilepsy.
- Explain the importance of patient education and drug compliance in the management of seizure disorders.
- Recognize important safety considerations and monitoring parameters in antiepileptic therapy.
- Apply the nursing process in the care of patients receiving antiepileptic medications.
Introduction
Seizure disorders
Seizures are episodes of abnormal, excessive, and synchronous neuronal activity in the brain. They can present in various forms, ranging from brief lapses of consciousness to severe convulsions with loss of motor control. Understanding seizure disorders is essential for safe and effective pharmacologic management.
Seizures
Seizures result from a sudden disturbance in the electrical activity of the brain. The disturbance can be localized to one area of the brain or involve both hemispheres.
Seizures can occur in anyone, but epilepsy is diagnosed when a person experiences recurrent, un-provoked seizure.
Key Features of Seizures:
- Sudden onset and abrupt termination.
- Loss or alteration of consciousness in many types.
- Motor, sensory, autonomic, or psychic symptoms may occur.
- Postictal phase: period of confusion, fatigue, or drowsiness after the seizure.
Epilepsy
Epilepsy is a chronic neurologic disorder characterized by a predisposition to recurrent seizures. The causes can be idiopathic (genetic), structural (brain injury, tumor, stroke), metabolic, infectious, or unknown.
Important Points About Epilepsy:
- Seizure frequency can vary widely—from multiple times per day to a few episodes per year.
- Management requires a comprehensive approach, including pharmacotherapy, lifestyle modifications, and patient education.
- Anti-seizure medications (also called anticonvulsants or antiepileptic drugs) are tailored to the type of seizure, patient age, comorbidities, and potential drug interactions.

Classification of Seizures
Seizures are classified based on onset, symptoms, and EEG findings.
-
Focal (Partial) Onset Seizures:
- Originate in a localized area of the brain.
- May remain localized (simple) or spread to involve the whole brain (secondary generalized).
- Can present with motor, sensory, autonomic, or psychic symptoms.
- Generalized Onset Seizures:
- Involve both cerebral hemispheres from the onset.
- May be convulsive or nonconvulsive.
- Unknown Onset Seizures:
- When the origin is not clearly identified, often due to insufficient observation or EEG data.
Descriptions of seizures
Generalized Convulsive Seizures
Tonic-Clonic Seizures (Grand Mal):
- Involve loss of consciousness, tonic stiffening, and clonic rhythmic jerking.
- Usually last 1–3 minutes; postictal confusion is common.
- May cause tongue biting, incontinence, and fatigue.
Atonic or Akinetic Seizures:
- Sudden loss of muscle tone, leading to collapse.
- Often called “drop attacks”; risk of injury is high.
Myoclonic Seizures:
- Sudden, brief jerks of muscles or groups of muscles.
- May occur in clusters, typically in the morning.
- Consciousness is usually preserved.
Generalized Nonconvulsive Seizures
Absence (Petit Mal) Seizures:
-
Brief loss of consciousness lasting a few seconds.
- May include eye fluttering or subtle motor activity (lip-smacking, hand movements).
- Typically occurs in children and can interfere with learning.
Focal (Localized) Seizures
Simple Focal Seizures:
- Affect one area of the brain, usually preserve consciousness.
- May cause motor, sensory, or autonomic symptoms.
Complex Focal Seizures:
- Impair consciousness.
- Often include repetitive movements (lip-smacking, picking at clothes).
- May progress to generalized tonic-clonic seizures.
Nursing insights for antiepileptic therapy
Nursing care for patients with seizures focuses on monitoring, safety, patient education, and evaluating therapeutic response.
Baseline Assessment:
- Complete health history: liver, kidney, cardiovascular, neurological disease, and pregnancy status.
- Detailed drug history, including prescriptions, OTC medications, and herbal supplements.
- Seizure history: type, frequency, duration, triggers, prodromal warnings, and postictal period.
- Baseline vital signs, weight, and laboratory values (CBC, electrolytes, liver and kidney function).
- Assess development and school performance in children.
Ongoing Assessment:
- Monitor therapeutic effects: decrease in seizure frequency, duration, and severity.
- Periodically check drug levels for medications with narrow therapeutic windows (e.g., phenytoin, valproic acid).
- Observe for adverse effects: CNS depression, ataxia, vision changes, skin reactions, bruising, or bleeding.
- Monitor growth and development in pediatric patients.
Patient and Family Education:
- Keep a seizure diary: record date, time, duration, type, triggers, and postictal symptoms.
- Avoid abrupt discontinuation to prevent status epilepticus or rebound seizures.
- Emphasize safe environment: avoid heights, swimming alone, and driving until seizures are controlled.
- Advise medication adherence, same brand when possible, and take with food if GI upset occurs.
- Educate about drug interactions: alcohol, other CNS depressants, and certain herbal supplements.
- Provide guidance on pregnancy and contraception: many antiepileptic drugs are teratogenic.
Safety Measures:
- Pad bed rails and provide fall precautions for high-risk patients.
- Ensure IV access for rapid administration during status epilepticus.
- Observe respiratory and cardiovascular status, particularly for benzodiazepines and barbiturates.
Lifestyle Considerations:
- Encourage adequate sleep, balanced diet, hydration, and stress management.
- Limit caffeine and nicotine, as they may reduce medication efficacy.
- Promote regular dental care for patients on hydantoins or phenytoin-like drugs due to gingival hyperplasia.
Evaluation of Outcomes:
- Patient experiences therapeutic effect: reduced seizure frequency and severity.
- Patient demonstrates understanding of medications, including dose, timing, adverse effects, and reporting requirements.
- Patient maintains safety at home, school, and work, avoiding activities that could lead to injury.
Classification of Antiepileptic Drugs
Antiepileptic Drug Classes
Benzodiazepines
Here are the main benzodiazepines used:
- Diazepam (Valium):
- Widely used for status epilepticus (IV, rectal gel formulations).
- Rapid onset but relatively short duration of anticonvulsant action.
- Lorazepam (Ativan):
- Preferred IV benzodiazepine for status epilepticus because it has a longer duration of action in the CNS than diazepam.
- Often first-line in emergency settings.
- Midazolam (Versed):
- Used IV or intranasally in acute seizure emergencies, especially in children or when IV access is difficult.
- Short-acting but very effective for rapid seizure control.
- Clonazepam (Klonopin):
- Used as an adjunct for absence seizures, myoclonic seizures, and Lennox–Gastaut syndrome.
- Taken orally for long-term management, though tolerance can develop.
- Clobazam (Onfi):
- Specifically approved for Lennox–Gastaut syndrome.
- Has fewer sedative effects than some other benzodiazepines, making it useful for long-term adjunctive therapy.
Actions:
- Enhance GABAergic inhibition in the CNS, which increases the effect of gamma-aminobutyric acid (GABA), the primary inhibitory neurotransmitter in the brain. This suppresses excessive neuronal firing and stabilizes overactive neuronal circuits.
- Stabilize hyperexcitable neurons and prevent seizure propagation across different areas of the brain, which helps limit the duration and intensity of seizures.
- Provide rapid anticonvulsant effects, which is especially valuable during acute seizure events such as status epilepticus.
- Can also produce muscle relaxation by reducing excessive motor neuron activity in skeletal muscles.
Uses:
- First-line therapy for status epilepticus, particularly via intravenous (IV) administration in emergency settings due to rapid onset of action.
- Adjunct therapy for partial and generalized seizures, helping patients whose seizures are not fully controlled by other antiepileptic drugs.
- Occasionally used to manage anxiety, agitation, and muscle spasms in seizure patients, improving overall comfort and reducing seizure triggers related to stress.
- Can be used pre-procedurally to minimize seizure risk during surgery or diagnostic procedures in epileptic patients.
Therapeutic Outcomes:
- Termination of ongoing seizures and prevention of prolonged seizure activity, especially in life-threatening status epilepticus.
- Reduced frequency and severity of seizures when used adjunctively with other antiepileptic medications.
- Improved patient safety and reduced risk of seizure-related injuries, such as falls or head trauma.
- Enhanced quality of life by reducing seizure burden and associated complications.
Nursing Insights:
- Monitor respiratory and cardiovascular status, especially during IV administration, because benzodiazepines can depress breathing and lower blood pressure.
- Observe for sedation, dizziness, and ataxia, which may affect patient mobility and increase the risk of falls.
- Educate patients and caregivers to avoid driving, operating machinery, alcohol, or other CNS depressants while on therapy.
- Emphasize the importance of gradual tapering to prevent rebound seizures, withdrawal symptoms, and potential dependence.
- Assess liver function and overall metabolic status in long-term therapy, as some benzodiazepines are metabolized hepatically.
- Encourage seizure diaries to track frequency, triggers, and any side effects to guide therapy adjustments.
Common Adverse Effects:
- CNS effects: drowsiness, fatigue, dizziness, ataxia, cognitive slowing.
- Cardiovascular: hypotension, rarely bradycardia.
- Paradoxical reactions: agitation, hyperactivity, or aggression, especially in children and older adults.
- Dependence and tolerance: with long-term use, requiring careful monitoring and tapering.
Drug Interactions:
- CNS depressants (opioids, alcohol, antihistamines, sedative hypnotics) can enhance sedation and respiratory depression.
- Enzyme-inducing anticonvulsants (phenytoin, carbamazepine) may alter metabolism and reduce effectiveness of some benzodiazepines.
- Some benzodiazepines can interact with oral contraceptives, antifungals, or macrolide antibiotics, altering drug levels and effectiveness.
Hydantoins (phenytoin, fosphenytoin)
Actions:
- Desensitizes sodium channels in neurons, preventing repetitive, high-frequency firing that contributes to seizure activity.
- Stabilizes neuronal membranes, reducing the spread of abnormal electrical discharges.
- Also exhibits antidysrhythmic properties, similar to lidocaine, making it occasionally useful in certain cardiac conditions.
- Slows the recovery of sodium channels from inactivation, which limits the likelihood of recurrent neuronal firing.
Uses:
- Management of tonic-clonic seizures (grand mal) and partial seizures.
- Digitalis-induced cardiac dysrhythmias (unlabeled use), leveraging its membrane-stabilizing effects.
- Occasionally used as adjunct therapy for certain neurologic conditions with hyperexcitable neuronal activity.
Therapeutic Outcomes:
- Decreased frequency of seizures, reducing seizure severity and preventing injury.
- Stabilized cardiac rhythm in dysrhythmias, improving cardiac output and patient safety.
- Enhanced patient quality of life due to better seizure control.
Nursing Insights:
- Monitor serum drug levels regularly (therapeutic: 10–20 mcg/mL) to maintain efficacy and avoid toxicity.
- Assess oral hygiene, as phenytoin may cause gingival hyperplasia; provide guidance on dental care.
- Monitor vital signs, CNS function, and skin for signs of rash or Stevens–Johnson syndrome.
- Educate patient to take medication exactly as prescribed, avoid abrupt discontinuation, and report any unusual bruising, bleeding, or infections.
- Evaluate liver and kidney function, as these organs metabolize and excrete the drug.
- Encourage patient to wear medical alert identification in case of severe reactions.
Common Adverse Effects:
- CNS: dizziness, headache, confusion, nystagmus, ataxia.
- Cardiovascular: bradycardia, hypotension, ventricular dysrhythmias.
- Hematologic: agranulocytosis, aplastic anemia.
- Dermatologic: rash, Stevens–Johnson syndrome, toxic epidermal necrolysis.
- Connective tissue: lupus-like reactions, hirsutism, hypertrichosis, coarsening of facial features with long-term use.
Drug Interactions:
- Reduces effectiveness of oral contraceptives, doxycycline, furosemide.
- Interacts with glucocorticoids, H2 blockers, antitubercular drugs.
- Herbal interactions: Ginkgo may reduce anticonvulsant efficacy; herbal laxatives may increase potassium loss and alter electrolyte balance.
- Co-administration with other CNS depressants may exacerbate drowsiness and sedation.
Succinimides (ethosuximide, methsuximide)
Actions:
- Suppress calcium influx in thalamic neurons, which reduces the likelihood of abnormal firing that leads to absence seizures.
- Increase seizure threshold, making it more difficult for neurons to fire excessively.
- Stabilizes abnormal neural circuits specifically responsible for non-convulsive, generalized absence seizures.
Uses:
- First-line therapy for absence (petit mal) seizures, especially in children and adolescents.
- Occasionally used as adjunctive therapy in patients with multiple seizure types who do not respond fully to other antiepileptics.
Therapeutic Outcomes:
- Reduced frequency of absence seizures, which often manifest as brief lapses in consciousness multiple times per day.
- Improved daily functioning and school or work performance by minimizing seizure interruptions.
- Reduced risk of injury and long-term cognitive or developmental effects in pediatric patients.
Nursing Insights:
- Monitor CBC for blood dyscrasias, including anemia or leukopenia.
- Observe for CNS depression, ataxia, dizziness, and fatigue.
- Educate patient to avoid abrupt discontinuation, as sudden withdrawal can precipitate seizures.
- Provide guidance on adherence, dosing schedules, and potential side effects.
- Encourage parents and caregivers to maintain seizure logs for accurate dose titration and monitoring.
Common Adverse Effects:
- CNS: drowsiness, dizziness, ataxia, headache.
- Gastrointestinal: epigastric distress, nausea, vomiting, anorexia.
- Hematologic: agranulocytosis, pancytopenia, aplastic anemia.
- May also cause mild rash or photosensitivity in some patients.
Drug Interactions:
- Ethosuximide may increase phenytoin levels, requiring dose adjustments.
- Valproic acid can alter ethosuximide serum concentrations, increasing risk of toxicity.
- Herbal supplements, such as Ginkgo, may reduce effectiveness.
- Co-administration with other CNS depressants may intensify sedation.
Other Antiepileptic Drugs
Carbamazepine (Tegretol)
Actions:
- Desensitizes sodium channels in hyperactive neurons, reducing repetitive firing and stabilizing neuronal membranes.
- Limits neuronal excitability and seizure spread across the CNS.
- Produces antimanic and mood-stabilizing effects, making it useful for bipolar disorder management.
- Reduces abnormal discharge in partial and generalized tonic-clonic seizures, providing broad-spectrum seizure control.
Uses:
- Tonic-clonic seizures and partial seizures as monotherapy or adjunct therapy.
- Bipolar disorder, especially for acute manic or mixed episodes.
- Trigeminal neuralgia, leveraging its ability to stabilize hyperactive neuronal pathways.
- Occasionally used in off-label management of neuropathic pain.
Therapeutic Outcomes:
- Reduced seizure frequency and intensity, improving patient safety.
- Mood stabilization in bipolar disorder, decreasing manic episodes and emotional lability.
- Prevention of trigeminal neuralgia attacks, improving quality of life.
Nursing Insights:
- Monitor CBC, liver function, and sodium levels due to risk of hyponatremia and bone marrow suppression.
- Assess for neurologic symptoms, including dizziness, drowsiness, and ataxia.
- Educate patients on avoiding abrupt discontinuation, which can precipitate status epilepticus.
- Encourage reporting of rashes, fever, or sore throat, as these may indicate serious dermatologic or hematologic reactions.
- Advise women of childbearing age to discuss pregnancy planning due to teratogenic potential.
Common Adverse Effects:
- CNS: dizziness, drowsiness, headache, blurred vision.
- Hematologic: leukopenia, anemia, thrombocytopenia in rare cases.
- Dermatologic: rash, Stevens–Johnson syndrome, photosensitivity.
- Electrolyte disturbances: hyponatremia may manifest as confusion, seizures, or edema.
Drug Interactions:
- Strong hepatic enzyme inducer: decreases effectiveness of oral contraceptives, warfarin, and other medications metabolized by CYP450.
- CNS depressants may increase sedation.
- Alcohol can exacerbate CNS effects.
Oxcarbazepine (Trileptal)
Actions:
- Structurally related to carbamazepine; blocks sodium channels, stabilizing hyperactive neurons.
- Reduces excessive neuronal firing in partial and generalized seizures.
- Slightly better tolerated than carbamazepine with fewer drug-drug interactions.
Uses:
- Partial seizures in adults and children over 4 years.
- Occasionally adjunctive therapy for tonic-clonic seizures.
- Off-label use for bipolar disorder in some patients.
Therapeutic Outcomes:
- Decreased seizure frequency with improved tolerability compared to carbamazepine.
- Maintains functional independence in daily activities.
Nursing Insights:
- Monitor sodium levels due to risk of hyponatremia, especially in elderly or those on diuretics.
- Educate patients on signs of rash or allergic reaction, as severe skin reactions can occur.
- Monitor CNS side effects including dizziness, headache, or somnolence.
- Encourage adherence to dosing schedules for consistent therapeutic effect.
Common Adverse Effects:
- Dizziness, headache, drowsiness, and fatigue.
- Hyponatremia leading to confusion or seizures.
- Dermatologic: rash, rare cases of Stevens–Johnson syndrome.
Drug Interactions:
- May reduce effectiveness of oral contraceptives.
- Additive CNS depression with other sedatives or alcohol.
Valproic Acid / Divalproex (Depakene / Depakote)
Actions:
- Blocks sodium channels, suppresses calcium influx, and enhances GABAergic inhibition, reducing neuronal hyperexcitability.
- Works across multiple seizure types due to broad-spectrum anticonvulsant effects.
- Exhibits mood-stabilizing properties via modulation of neurotransmitters.

Uses:
- Absence, myoclonic, partial, and tonic-clonic seizures.
- Bipolar disorder, particularly acute mania or mixed episodes.
- Migraine prophylaxis to reduce headache frequency.
Therapeutic Outcomes:
- Broad seizure control, improving safety and quality of life.
- Mood stabilization in bipolar disorder.
- Reduced migraine frequency and severity.
Nursing Insights:
- Monitor liver function tests, CBC, and pancreatic enzymes due to risk of hepatotoxicity and pancreatitis.
- Educate patients on pregnancy risks; category D drug associated with spina bifida.
- Teach symptom monitoring for abdominal pain, jaundice, or unusual bleeding.
- Avoid abrupt discontinuation to prevent seizure recurrence.
- Advise avoiding alcohol and CNS depressants to minimize additive sedation.
Common Adverse Effects:
- CNS: sedation, dizziness, ataxia, headache, tremor.
- Gastrointestinal: nausea, vomiting, abdominal pain.
- Hepatic: hepatotoxicity, especially in children under 2 years.
- Hematologic: thrombocytopenia, bone marrow suppression.
- Weight gain, hair loss, tremor, pancreatitis (rare).
Drug Interactions:
- Increases serum levels of phenytoin and phenobarbital.
- Interaction with aspirin, warfarin, alcohol, CNS depressants.
- Lamotrigine, phenytoin, and rifampin may lower valproic acid levels, reducing efficacy.
Lamotrigine (Lamictal)
Actions:
- Blocks sodium channels and inhibits glutamate release, reducing excitatory neurotransmission.
- Stabilizes neuronal membranes and prevents seizure propagation.
- Acts on multiple seizure types, making it versatile.
Uses:
- Partial, tonic-clonic, and absence seizures.
- Bipolar disorder maintenance therapy, particularly for depressive episodes.
- Occasionally adjunctive for mixed seizure types.
Therapeutic Outcomes:
- Reduced seizure frequency and severity.
- Improved mood stabilization in bipolar disorder.
- Better overall cognitive and functional performance due to seizure control.
Nursing Insights:
- Monitor for rash; may indicate Stevens–Johnson syndrome, which requires urgent discontinuation.
- Educate patient on dose titration, as rapid dose escalation increases risk of severe rash.
- Monitor for CNS effects: dizziness, headache, blurred vision.
- Review concomitant medications, especially enzyme inducers or inhibitors.
Common Adverse Effects:
- Dizziness, headache, blurred vision, somnolence.
- Severe rash (Stevens–Johnson syndrome, toxic epidermal necrolysis).
- Nausea, vomiting, ataxia.
Drug Interactions:
- Hepatic enzyme inducers (phenytoin, carbamazepine) lower lamotrigine levels.
- Valproic acid increases lamotrigine levels, requiring lower dosing.
- Rifampin reduces lamotrigine levels.
Levetiracetam (Keppra)
Actions:
- Modulates synaptic neurotransmitter release, stabilizing neuronal activity.
- Reduces neuronal excitability without directly acting on sodium channels or GABA receptors.
- Broad-spectrum efficacy with minimal drug interactions, making it suitable for polytherapy.
Uses:
- Adjunct therapy for partial seizures in adults and children.
- Occasionally used for generalized tonic-clonic seizures in refractory cases.
Therapeutic Outcomes:
- Reduced seizure frequency with good tolerability.
- Minimal CNS cognitive impairment compared to older antiepileptics.
Nursing Insights:
- Monitor behavioral changes including irritability, mood swings, or aggression.
- Educate patient on CNS side effects, including drowsiness and dizziness.
- Encourage adherence and consistent timing to maintain therapeutic levels.
Common Adverse Effects:
- Drowsiness, fatigue, dizziness.
- Mood changes, irritability, depression in some patients.
- Rare cases of severe allergic reactions or multi-organ effects.
Drug Interactions:
- Minimal interactions; safe for polytherapy.
- Caution with other CNS depressants to avoid additive sedation.
Gabapentin (Neurontin)
Actions:
- Modulates voltage-gated calcium channels, reducing the release of excitatory neurotransmitters like glutamate.
- Enhances GABA activity indirectly, promoting neuronal stabilization.
- Does not significantly affect sodium channels, making it distinct from traditional antiepileptics.
Uses:
- Partial seizures as adjunct therapy in adults and children.
- Neuropathic pain, including postherpetic neuralgia and diabetic neuropathy.
- Occasionally used off-label for anxiety disorders or restless leg syndrome.
Therapeutic Outcomes:
- Reduction in seizure frequency and severity.
- Relief of neuropathic pain, improving sleep and quality of life.
- Minimal cognitive impairment compared to older antiepileptics.
Nursing Insights:
- Monitor for CNS effects, including drowsiness, dizziness, and ataxia.
- Adjust dose in patients with renal impairment to prevent toxicity.
- Educate patients to avoid abrupt discontinuation, which may increase seizure risk.
- Encourage adherence to consistent dosing schedules to maintain steady-state levels.
Common Adverse Effects:
- CNS: drowsiness, dizziness, fatigue, ataxia.
- Peripheral edema may occur, especially in older adults.
- Gastrointestinal: mild nausea or vomiting.
Drug Interactions:
- Few clinically significant interactions, making it safer for combination therapy.
- Additive CNS depression may occur with alcohol or sedatives.
Pregabalin (Lyrica)
Actions:
- Binds to voltage-gated calcium channels, reducing excitatory neurotransmitter release.
- Stabilizes hyperactive neurons, decreasing seizure propagation.
- Also modulates pain pathways in the CNS, making it effective for neuropathic pain.
Uses:
- Adjunct therapy for partial-onset seizures in adults.
- Neuropathic pain from diabetic neuropathy or postherpetic neuralgia.
- Occasionally used for fibromyalgia and generalized anxiety disorder.
Therapeutic Outcomes:
- Reduced seizure frequency in combination therapy.
- Alleviation of neuropathic pain, improving patient mobility and daily function.
- Decreased anxiety symptoms in off-label use.
Nursing Insights:
- Monitor for CNS depression, especially when combined with other sedatives.
- Educate patients about gradual tapering to prevent withdrawal seizures or insomnia.
- Monitor for weight gain and peripheral edema in long-term use.
- Encourage adherence to dosing schedule for consistent therapeutic effect.
Common Adverse Effects:
- CNS: dizziness, somnolence, blurred vision.
- Weight gain and peripheral edema may occur.
- Occasional dry mouth or mild gastrointestinal upset.
Drug Interactions:
- Additive CNS depression when combined with opioids, benzodiazepines, or alcohol.
- Minimal interactions with other antiepileptic medications.
Topiramate (Topamax)
Actions:
- Blocks sodium channels and inhibits glutamate activity, reducing excitatory neurotransmission.
- Enhances GABA-mediated inhibition, increasing seizure threshold.
- Exhibits mild carbonic anhydrase inhibition, which can lead to metabolic acidosis in rare cases.
Uses:
- Partial and generalized tonic-clonic seizures in adults and children.
- Migraine prophylaxis, reducing the frequency and severity of attacks.
- Occasionally used off-label for bipolar disorder, weight reduction, or binge eating disorders.
Therapeutic Outcomes:
- Decreased seizure frequency and severity.
- Reduction in migraine attacks and improved quality of life.
- Minimal cognitive impact when monitored closely.
Nursing Insights:
- Monitor cognitive effects, including attention and memory deficits.
- Ensure adequate hydration to prevent kidney stones.
- Assess for weight loss or appetite changes during therapy.
- Educate patients on gradual titration and adherence, avoiding abrupt discontinuation.
- Monitor for signs of metabolic acidosis, especially in patients with kidney disease.
Common Adverse Effects:
- Cognitive impairment, memory difficulties, confusion.
- Weight loss, anorexia, dizziness.
- Kidney stones due to carbonic anhydrase inhibition.
- Paresthesia or tingling sensations in extremities.
Drug Interactions:
- May reduce effectiveness of oral contraceptives.
- Additive CNS depression with other sedatives.
- Metabolism may be altered when combined with other enzyme-inducing antiepileptics.
Phenobarbital
Actions:
- Enhances GABA-mediated chloride influx, suppressing CNS excitability.
- Increases seizure threshold and prevents abnormal electrical activity.
- Long-acting barbiturate with both anticonvulsant and sedative properties.
Uses:
- Partial and generalized tonic-clonic seizures.
- Occasionally used for status epilepticus if benzodiazepines are ineffective.
- Rarely used for sedation in critically ill patients.
Therapeutic Outcomes:
- Reduced frequency and severity of seizures.
- Stabilization of neuronal activity with minimal breakthrough seizures when used correctly.
- Sedation and improved sleep in select patients.
Nursing Insights:
- Monitor CNS and respiratory status, especially with IV administration.
- Assess for dependence and tolerance with long-term therapy.
- Educate patients to avoid abrupt discontinuation to prevent rebound seizures.
- Monitor liver function and CBC periodically.
- Teach patients about sedation and impaired coordination, avoiding driving until effects are known.
Common Adverse Effects:
- Sedation, drowsiness, cognitive impairment.
- Respiratory depression in high doses or IV administration.
- Osteoporosis and vitamin D deficiency with long-term therapy.
- Risk of tolerance, dependence, and withdrawal seizures.
Drug Interactions:
- Induces hepatic enzymes, reducing efficacy of oral contraceptives, warfarin, and other drugs.
- Additive CNS depression with alcohol, benzodiazepines, or opioids.
- Interactions with other antiepileptic drugs may require dosage adjustments.
Zonisamide (Zonegran)
Actions:
- Blocks sodium and T-type calcium channels, stabilizing hyperexcitable neurons.
- Reduces glutamate release, preventing abnormal neuronal firing.
- Weak carbonic anhydrase inhibition may contribute to metabolic effects.
Uses:
- Adjunct therapy for partial-onset seizures in adults.
- Occasionally used off-label for generalized seizures in refractory cases.
- May have mood-stabilizing or neuroprotective properties under investigation.
Therapeutic Outcomes:
- Reduced frequency and severity of seizures in adults.
- Maintains cognitive function due to generally mild CNS side effects.
- Improved quality of life through better seizure control.
Nursing Insights:
- Monitor renal function and sulfonamide allergies.
- Educate patients about CNS effects, including drowsiness, dizziness, and impaired cognition.
- Monitor for rash, which may indicate serious dermatologic reactions.
- Encourage adequate hydration to prevent kidney stones.
- Taper gradually if discontinuation is necessary.
Common Adverse Effects:
- Drowsiness, cognitive impairment, dizziness.
- Kidney stones, rash, anorexia, weight loss.
- Rare metabolic acidosis due to carbonic anhydrase inhibition.
Drug Interactions:
- CNS depressants may increase sedation.
- Hepatic enzyme inducers (e.g., carbamazepine) may reduce zonisamide levels.
- Caution with other sulfonamide-containing drugs.
Summary
Seizure disorders: Neurological conditions with abnormal, excessive, synchronous neuronal activity.
Epilepsy: Chronic disorder with recurrent, unprovoked seizures.
Seizure classification:
- Focal seizures – simple (consciousness preserved) or complex (consciousness impaired).
- Generalized seizures – tonic-clonic, myoclonic, atonic, absence.
- Unknown onset seizures.
Pharmacologic goals: Reduce seizure frequency/severity, prevent complications, improve quality of life.
Drug Classes:
- Benzodiazepines – rapid seizure control in emergencies (status epilepticus); enhance GABA; risk of sedation & respiratory depression.
- Hydantoins (Phenytoin) – sodium channel stabilizers; effective for tonic-clonic/partial seizures; require serum monitoring; adverse effects include gingival hyperplasia & dermatologic reactions.
- Succinimides (Ethosuximide) – first-line for absence seizures; suppress thalamic calcium influx; GI & CNS side effects.
- Carbamazepine / Oxcarbazepine – sodium channel blockers; used in tonic-clonic & partial seizures, bipolar disorder, trigeminal neuralgia; risks: hyponatremia, serious rashes.
- Valproic acid / Divalproex – broad-spectrum efficacy; also used in bipolar disorder & migraine prophylaxis; risks: hepatotoxicity, pancreatitis, teratogenicity.
- Newer agents (Lamotrigine, Levetiracetam, Gabapentin, Pregabalin, Topiramate, Zonisamide) – diverse mechanisms, fewer interactions, generally better tolerability.
- Phenobarbital – barbiturate enhancing GABA activity; effective for tonic-clonic seizures; limited by sedation, dependence, hepatic enzyme induction.
Nursing insights:
- Perform baseline and ongoing assessments.
- Monitor drug levels, organ function, and adverse effects.
- Reinforce patient adherence and gradual tapering.
- Educate on safety measures, lifestyle modifications, and injury prevention.
- Support patients and families in chronic management.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drugs Used for Seizure Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


