Please set your exam date
Introduction To Mental Health Nursing
Study Questions
Practice Exercise
Which phase of the nurse–patient relationship is characterized by establishing trust and defining the nurse’s role?
Explanation
Nurse–patient relationship: This therapeutic bond is foundational in healthcare, fostering trust, communication, and collaboration to enhance patient outcomes. It progresses through distinct phases, each with specific goals. Trust is critical for effective care, enabling patients to share sensitive information. Respect and empathy strengthen this bond, aligning with physiological and safety needs.
Rationale for correct answers
B. The orientation phase involves initial interactions where nurses establish trust and clarify their role. This sets the foundation for collaboration, addressing the patient’s immediate needs and expectations.
Rationale for incorrect answers
A. The working phase focuses on implementing care plans, not primarily on establishing trust or defining roles.
C. The termination phase centers on concluding the relationship, reviewing progress, not initiating trust.
D. The evaluation phase is not a standard phase; it may occur within others but does not focus on trust-building.
Take Home Points
- The nurse–patient relationship is critical for patient cooperation and improved health outcomes.
- Trust is established primarily in the orientation phase through active listening and role clarification.
- Each phase—pre-interaction, orientation, working, termination—has unique goals for therapeutic progress.
- Missteps in trust-building can hinder communication, distinguishing this relationship from casual interactions.
A client expresses intent to harm another person. What is the nurse’s immediate legal responsibility?
Explanation
Duty to warn is a legal and ethical obligation requiring mental health professionals to break confidentiality when a client poses a credible threat to another person. This protects public safety and involves notifying both law enforcement and the potential victim. It stems from Tarasoff case precedent and is recognized in many jurisdictions. Breaching confidentiality in this context is legally permissible and prioritized over privacy to prevent harm.
Rationale for correct answers
C. The nurse must act on the legal duty to protect others from foreseeable harm by alerting authorities and warning the threatened individual when a client makes a credible threat. This immediate action prioritizes safety over confidentiality.
Rationale for incorrect answers
A. Strictly maintaining confidentiality disregards the safety exception in cases of imminent harm to others, placing both the potential victim and the nurse at legal risk.
B. Solely documenting the statement fails to prevent danger, as it does not involve active steps to warn or protect the intended victim.
D. Administering medication addresses possible agitation but does not fulfill the legal obligation to protect third parties from credible threats of harm.
Take Home Points
- The duty to warn overrides confidentiality when a client poses a serious, credible threat to another person.
- Legal precedent from the Tarasoff case guides mental health professionals in balancing privacy with public safety.
- Warning includes notifying law enforcement and, if possible, directly informing the potential victim.
- Simply documenting or treating symptoms is insufficient without active protective measures when harm is imminent.
List two environmental safety measures in an acute psychiatric setting.
Explanation
Environmental safety in acute psychiatric settings involves structured measures to prevent self-harm or violence toward others. These interventions address physical surroundings, staff vigilance, and removal of hazards. High-risk items, unsafe structures, and inadequate observation can significantly increase injury potential, making proactive management essential.
Rationale for correct answers
A. Removing sharp objects and securing other potential weapons prevents impulsive acts of harm in high-acuity psychiatric units where patients may experience sudden agitation or psychosis.
Rationale for incorrect answers
B. Locking patients in rooms increases risk by restricting supervision, escalating agitation, and violating patient rights and therapeutic environment principles.
C. Turning off lights during the day disrupts orientation, increases confusion, and may worsen mood or psychotic symptoms in vulnerable patients.
D. Allowing unrestricted visitors introduces uncontrolled variables, increasing the chance of contraband entry or unsafe interactions that could jeopardize patient or staff safety.
Take Home Points
- Environmental safety in psychiatric care prioritizes preventing access to dangerous objects and reducing opportunities for harm.
- Continuous observation and structured environmental checks help mitigate impulsive or premeditated unsafe acts.
- Safety protocols should balance patient protection with therapeutic rights and dignity.
- Limiting environmental hazards reduces injury risk while supporting a stable, recovery-oriented setting.
Practice Exercise 2
Define primary prevention in mental health.
Explanation
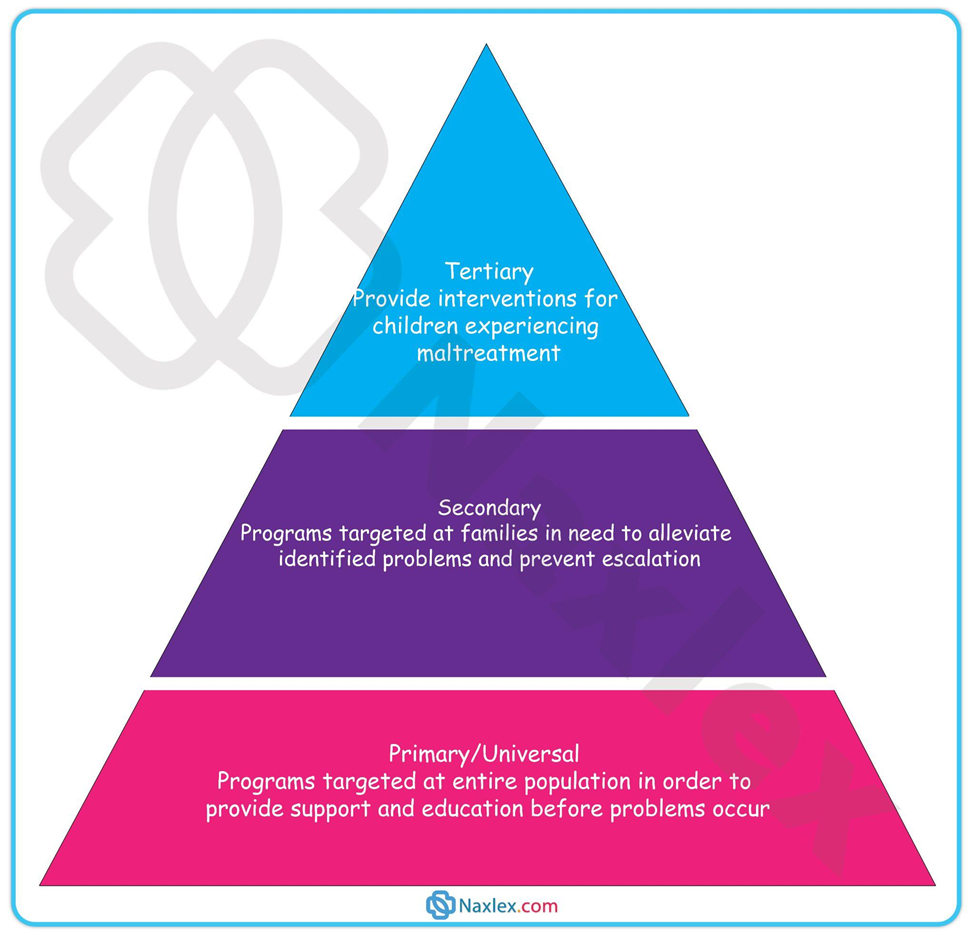
Primary prevention in mental health focuses on preventing the onset of illness before symptoms occur by reducing risk factors and enhancing protective factors. It targets healthy or at-risk populations through education, policy, and community interventions to maintain well-being.
Rationale for correct answers
B. Public education on stress management equips individuals with coping strategies, reducing the likelihood of developing mental health disorders before symptoms emerge.
Rationale for incorrect answers
A. Screening detects existing conditions at an early stage, making it secondary prevention rather than prevention before onset.
C. Rehabilitation addresses disability and functional restoration after illness has occurred, which is a component of tertiary prevention.
D. Administering antidepressants treats an existing disorder, falling under secondary or tertiary prevention depending on stage of illness.
Take Home Points
- Primary prevention aims to stop mental illness before it begins.
- Strategies include education, early life skill-building, and community awareness campaigns.
- Secondary prevention focuses on early detection and intervention.
- Tertiary prevention reduces disability and supports recovery after illness onset.
Give an example of a secondary prevention strategy for mental illness.
Explanation
Secondary prevention in mental health involves early detection and prompt intervention to halt progression of a disorder and minimize complications. It targets individuals at high risk or with early symptoms, aiming to restore functioning quickly and prevent chronicity.
Rationale for correct answers
D. Prescribing prophylactic medication to prevent anxiety progression addresses symptoms in their early phase, preventing further development or recurrence.
Rationale for incorrect answers
A. Stress-reduction workshops are primary prevention, aiming to prevent illness before it occurs in the general population.
B. Hospitalizing after a suicide attempt is tertiary prevention, as it addresses acute management after harm has occurred.
C. Job skills training supports rehabilitation, making it a tertiary prevention measure for those with established chronic illness.
Take Home Points
- Secondary prevention targets early symptom recognition and rapid intervention.
- Examples include mental health screening and initiating early pharmacologic or psychotherapeutic treatment.
- Primary prevention aims to stop illness before it starts.
- Tertiary prevention focuses on recovery, rehabilitation, and reducing disability after illness onset.
What is the primary goal of tertiary prevention?
Explanation
Tertiary prevention in mental health focuses on reducing disability and maximizing quality of life after an illness is established. It includes rehabilitation, relapse prevention, and support services to optimize functioning and promote community reintegration.
Rationale for correct answers
B. The aim is to improve daily functioning and reduce long-term disability through therapy, medication adherence, and psychosocial interventions.
Rationale for incorrect answers
A. Preventing onset is a primary prevention goal, occurring before disease develops.
C. Screening for early detection is secondary prevention, not focused on established illness.
D. Eliminating environmental risk factors is part of primary prevention strategies to avoid initial disease development.
Take Home Points
- Tertiary prevention starts after diagnosis and treatment have begun.
- Its focus is on rehabilitation, relapse prevention, and improving quality of life.
- Primary prevention addresses risk reduction before illness onset.
- Secondary prevention detects and treats illness early to halt progression.
Practice Exercise 3
What is the primary goal of crisis intervention?
Explanation
Crisis intervention is an immediate, short-term approach aimed at restoring stability and functioning in individuals facing acute psychological distress. It focuses on safety, problem-solving, and preventing further harm rather than long-term therapy.
Rationale for correct answers
B. The main goal is rapid stabilization to prevent deterioration and reduce the risk of lasting psychological effects.
Rationale for incorrect answers
A. Long-term psychotherapy is a rehabilitative process, not the immediate focus during an acute crisis.
C. Diagnostic assessment may occur later but is not the immediate aim of crisis intervention.
D. Immediate psychopharmacology may be used as an adjunct, but stabilization is the primary objective.
Take Home Points
- Crisis intervention focuses on immediate stabilization and safety.
- It is short-term and problem-focused, not meant for long-term therapy.
- The aim is to restore baseline functioning and prevent further harm.
- Medical or psychiatric treatment may be included, but only as part of a stabilization plan.
Which of the following is an example of maladaptive coping?
Explanation
Maladaptive coping refers to behavioral or cognitive strategies that temporarily reduce stress but ultimately worsen functioning or create additional problems. These behaviors often avoid addressing the root cause and can lead to harm over time.
Rationale for correct answers
C. Substance abuse provides temporary relief but increases risk for health problems, addiction, and worsening of the original stressor.
Rationale for incorrect answers
A. Problem-solving is an adaptive strategy that directly addresses and resolves the cause of stress.
B. Seeking social support promotes emotional relief and can improve coping outcomes.
D. Positive reframing encourages resilience by helping individuals view challenges from a more constructive perspective.
Take Home Points
- Maladaptive coping worsens stress or functioning over time.
- Examples include avoidance, denial, aggression, and substance abuse.
- Adaptive coping strategies improve problem resolution and emotional well-being.
- Choosing adaptive responses reduces the likelihood of long-term psychological or physical harm.
Which of the following is a therapeutic communication technique?
Explanation
Rationale for the Correct Answer
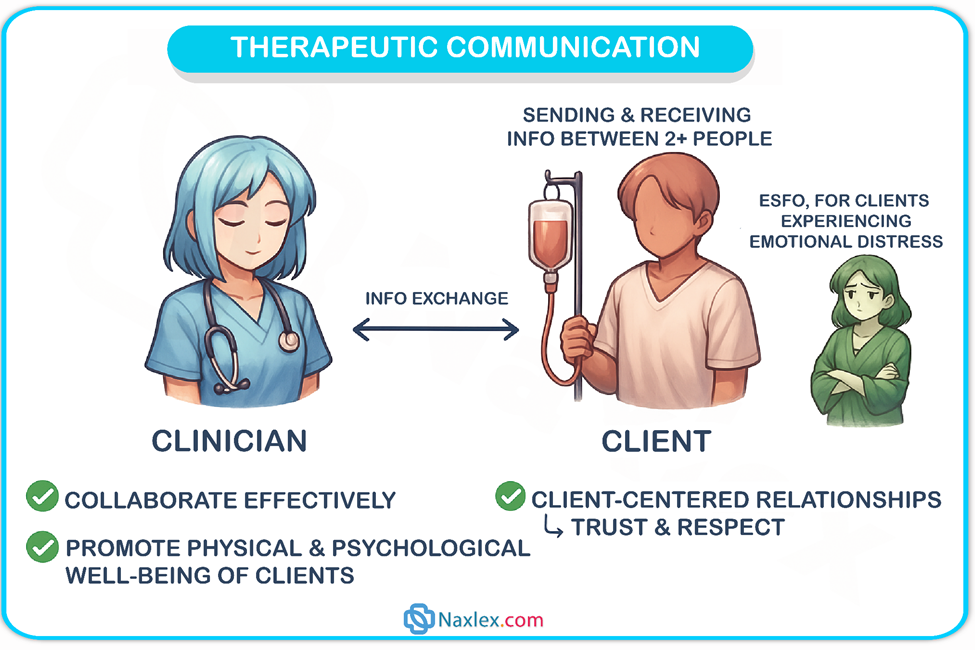
Reflectingis a therapeutic approach in which the practitioner rephrases or repeats the patient's feelings or remarks. This encourages the patient to elaborate further by demonstrating that they are being understood and listened. The patient develops awareness of their own feelings and thoughts.
Clarifying involves asking open-ended questionsto ensure that the patient's words are understood correctly. This reduces miscommunication and shows sincere interest, which fosters rapport and trust.
Rationale for Incorrect Answers
Giving advice and probing questions: Giving advice can be harmful as it takes away the patient's autonomy and suggests that the healthcare provider knows what's best for them, which can discourage the patient from solving problems on their own. Probing questions can make a patient feel questioned and defensive.
Using clichés and offering reassurance: Using phrases such as "It's going to be okay" can sound condescending and inauthentic, invalidating the patient's emotions. Offering false reassurance can end a conversation and give them the impression that their concerns are not being taken seriously.
Interrupting and redirecting the conversation: Interrupting a patient can harm rapport because it conveys a lack of interest and respect. Redirecting the conversation away from the patient's concerns invalidates their feelings and stops them from freely expressing themselves.
Comprehensive Questions
A client who is involuntarily committed to an inpatient psychiatric unit loses which of the following rights?
Explanation
Involuntary Commitment occurs when an individual is admitted to a psychiatric facility against their will due to concerns about their safety or the safety of others. This process is legally regulated and requires a court order. While the client retains most civil rights, the right to freedom is restricted, meaning they cannot leave the facility voluntarily. The commitment is based on medical and legal assessments of their mental state and potential risk.
Rationale for correct answers
A. Involuntary commitment legally restricts a person's ability to leave the facility, as their freedom is curtailed for safety reasons. This is the primary right affected by the commitment process.
Rationale for incorrect answers
B. Clients generally retain the right to refuse treatment, including medications, unless they are deemed unable to make informed decisions due to their mental state or a court order mandates treatment.
C. The ability to sign legal documents is not automatically revoked. Clients may still engage in legal matters unless a separate legal determination, such as guardianship, restricts this right.
D. While involuntarily committed, clients do not lose all rights. They retain rights such as humane treatment, access to legal counsel, and the ability to refuse certain interventions unless legally overridden.
Take Home Points
- Involuntary commitment primarily restricts freedom of movement, requiring a court order for hospitalization.
- Clients generally retain the right to refuse treatment, unless legally mandated.
- Signing legal documents remains possible unless a separate legal restriction applies.
- Patients maintain fundamental civil rights, including humane treatment and legal representation.
A nurse notices a physician beginning a physical examination of a disoriented client without closing the curtain or obtaining consent. What is the nurse's best response?
Explanation
Patient Privacy is a fundamental principle in healthcare, ensuring dignity and respect during medical procedures. Disoriented clients may be unable to advocate for themselves, making it the nurse’s responsibility to maintain confidentiality and uphold ethical standards. Closing the curtain and ensuring proper draping protects the client’s modesty and aligns with professional guidelines.
Rationale for correct answers
B. Closing the curtain and draping the client maintains privacy and dignity, preventing unnecessary exposure. This action is immediate and directly addresses the physician’s oversight without escalating the situation.
Rationale for incorrect answers
A. Notifying the charge nurse does not provide immediate protection for the client. While reporting concerns is important, the priority is ensuring privacy at the moment.
C. A disoriented client may not be able to make an informed decision about their comfort level. The nurse must proactively safeguard their dignity rather than relying on their response.
D. Saying nothing allows the breach of privacy to continue, failing to uphold ethical nursing responsibilities.
Take Home Points
- Nurses must actively protect patient privacy during examinations.
- Disoriented clients require advocacy to ensure ethical care.
- Immediate action, such as closing the curtain, is preferred over delayed reporting.
- Maintaining dignity is a core nursing responsibility in all patient interactions.
A client is scheduled for electroconvulsive therapy (ECT). Which action by the nurse ensures the client’s right to informed consent?
Explanation
Informed Consent is a legal and ethical process ensuring that a client understands a medical procedure before agreeing to it. Electroconvulsive therapy (ECT) requires thorough explanation of risks, benefits, and alternatives. The nurse plays a critical role in verifying comprehension and ensuring voluntary consent.
Rationale for correct answers
C. Witnessing the client’s signature and confirming their understanding ensures that consent is truly informed. The nurse must assess comprehension and clarify any concerns before the client signs. This includes ensuring the client is aware of potential side effects, expected outcomes, and alternative treatments. If confusion arises, further discussion is necessary before proceeding.
Rationale for incorrect answers
A. While explaining the procedure is important, it does not guarantee full understanding or voluntary consent. The nurse must verify comprehension, as simply providing information does not ensure the client grasps the risks, benefits, and alternatives. Misconceptions or unanswered questions can lead to uninformed decisions.
B. Pressuring the client to sign quickly undermines informed consent, which requires adequate time for discussion and decision-making. Rushing the process increases the risk of ethical and legal violations. Clients must be given the opportunity to ask questions, consider their options, and make an informed choice without coercion.
D. Delegating the responsibility entirely to the physician does not fulfill the nurse’s duty to advocate for the client’s understanding and autonomy. While physicians provide detailed explanations, nurses ensure comprehension and voluntary decision-making. Ignoring this responsibility can result in uninformed consent, which is legally and ethically unacceptable.
Take Home Points
- Informed consent ensures clients understand procedures before agreeing.
- Nurses must verify comprehension and witness voluntary consent.
- Clients should never be rushed or pressured into signing.
A nurse sees a former psychiatric inpatient client at a grocery store. Which of the following actions maintain client confidentiality? Select all that apply
Explanation
Client Confidentiality
Client confidentiality in mental health care ensures protection of personal health information, safeguarding patient privacy and trust. It involves strict adherence to legal standards, like HIPAA, which restrict sharing identifiable data without consent. Breaches can harm therapeutic relationships and carry legal consequences. Nurses must avoid disclosing patient status or details in public settings. Confidentiality supports patient autonomy and encourages open communication in treatment. Unauthorized disclosure risks stigma and discrimination, particularly in mental health contexts.
Rationale for Correct Answers
A. Avoiding eye contact and walking away prevents unintentional acknowledgment of the client’s health history, protecting confidentiality in a public setting.
B. Making eye contact and responding only if the client initiates interaction respects privacy while allowing natural social engagement without disclosing sensitive information.
Rationale for Incorrect Answers
C. Approaching and greeting the client by name risks implying familiarity from a healthcare context, potentially breaching confidentiality by signaling prior hospitalization to others nearby.
D. Informing the cashier about the client’s recent hospitalization directly violates confidentiality by disclosing protected health information without consent, contravening legal and ethical standards.
E. Asking the client if they need assistance may suggest a professional relationship, potentially compromising confidentiality by implying prior healthcare interactions in a public setting.
Take Home Points
- Client confidentiality is critical in mental health to maintain trust and comply with legal standards like HIPAA.
- Nurses must avoid actions that imply or disclose a client’s health history in public settings.
- Respecting patient autonomy involves minimal interaction unless initiated by the client.
- Breaches in confidentiality can lead to stigma, legal issues, and damaged therapeutic relationships.
A client's home was destroyed by a tornado. She has minor injuries but is experiencing disabling anxiety. What is the best nursing intervention?
Explanation
Anxiety is a common human experience, characterized by feelings of unease, worry, or fear. While often a normal reaction to stress, it can become disabling when intense and persistent, significantly impacting daily functioning. It involves physiological responses like increased heart rate and muscle tension, and cognitive symptoms such as racing thoughts. Understanding anxiety is crucial for effective nursing interventions.
Rationale for correct answers
C. Identifying community resources directly addresses the client's immediate and long-term needs stemming from the tornado's destruction and disabling anxiety, aligning with Maslow's hierarchy by assisting with safety and security needs.
Rationale for incorrect answers
A. Encouraging the client to focus on being lucky minimizes her current distress and invalidates her feelings of loss and anxiety, which is not therapeutic and can hinder emotional processing.
B. Discussing the stages of grief, while relevant to loss, is not the most immediate or direct intervention for disabling anxiety caused by an acute traumatic event and the loss of her home; immediate practical support is prioritized.
D. Suggesting she find a new home with a storm shelter, while a practical consideration for the future, is premature and dismissive of her current acute anxiety and the immediate need for support in the aftermath of trauma.
Take Home Points
- Prioritize immediate safety and security needs for clients experiencing trauma, aligning with Maslow's hierarchy.
- Emotional validation is crucial; avoid minimizing a client's feelings, even if well-intentioned.
- Practical support and connection to resources are often the most effective initial interventions for acute distress following a traumatic event.
- A holistic approach considers both the psychological impact of trauma and the tangible needs arising from it.
A psychiatric client tells the nurse, “Please don’t tell anyone about my sexual abuse.” What is the best nursing response?
Explanation
Confidentiality in psychiatric care Confidentiality is a fundamental principle in psychiatric nursing, ensuring that sensitive patient information is protected while balancing ethical and legal obligations. In cases of sexual abuse disclosure, nurses must adhere to mandatory reporting laws and institutional policies. While patient autonomy is respected, healthcare providers must share relevant information with the treatment team to ensure appropriate care and intervention. Trauma-informed care emphasizes validating the patient's experience while maintaining professional boundaries.
Rationale for correct answers
B. Sharing information with the treatment team ensures coordinated care while maintaining professional confidentiality. Nurses are obligated to disclose abuse-related information to appropriate healthcare professionals to facilitate intervention and support.
Rationale for incorrect answers
A. Absolute confidentiality is not appropriate in cases of abuse disclosure, as healthcare providers have a duty to report and address safety concerns.
C. Asking why the patient does not want the team to know may feel intrusive and could discourage further disclosure. A supportive approach is preferred.
D. While discussing feelings is important, it does not address the ethical obligation to ensure proper intervention and support.
Take Home Points
- Confidentiality in psychiatric care must balance patient autonomy with ethical and legal responsibilities.
- Sexual abuse disclosures require trauma-informed responses and appropriate reporting.
- Nurses must communicate professional confidentiality limits while ensuring patient trust.
- Supportive, non-judgmental responses encourage further disclosure and therapeutic engagement.
A nurse is assessing a client in the psychiatric unit. Which of the following are tasks of the orientation phase of the nurse-client relationship? Select all that apply
Explanation
The nurse-client relationship is a therapeutic alliance built on trust and collaboration, designed to promote healing and growth. It progresses through distinct phases: orientation, working, and termination. Each phase involves specific tasks crucial for achieving positive client outcomes and maintaining professional boundaries.
Rationale for correct answers
A. Establishing a contract for intervention is a primary task of the orientation phase. This involves setting mutual goals, discussing roles, responsibilities, and the parameters of the therapeutic relationship, including confidentiality and time frames.
B. Identifying the client’s strengths and limitations is integral to the initial assessment during the orientation phase. This helps the nurse understand the client's current state, resources, and areas needing support, informing the development of a tailored plan of care.
E. The formulation of nursing diagnostic statements occurs in the orientation phase. This is a crucial step that involves analyzing assessment data collected from the client to identify actual or potential health problems, forming the basis for subsequent planning and intervention.
Rationale for incorrect answers
C. Problem-solving situational crises is typically a task performed during the working phase of the nurse-client relationship. In this phase, the client and nurse actively collaborate to address the client's identified problems and develop coping strategies.
D. Promoting client’s insight and perception of reality is a core activity that takes place during the working phase. This involves exploring the client's thoughts, feelings, and behaviors, and helping them to understand their patterns and develop healthier responses. The orientation phase focuses on establishing the foundation for such work.
Take Home Points
- The orientation phase establishes the foundation for the therapeutic nurse-client relationship through trust building and goal setting.
- Key activities in the orientation phase include assessment, contracting, and the development of nursing diagnoses.
- Interventions like problem-solving and promoting insight are characteristic of the working phase.
- A clear understanding of each phase's tasks is essential for effective psychiatric nursing practice.
A nurse observes bruises on a child visiting a client on the psychiatric unit. What is the nurse’s legal responsibility?
Explanation
Mandatory reporting in child abuse Child abuse requires immediate intervention to prevent further harm. Healthcare professionals, including nurses, are legally obligated to report suspicions of abuse. Delayed action increases risk to the child. Reporting ensures timely protection, appropriate support, and legal compliance in safeguarding vulnerable individuals.
Rationale for correct answers
C. Reporting suspected child abuse is a nurse's legal duty, ensuring swift protective action. Child protective services conduct investigations to assess safety, preventing ongoing harm. Failure to report could result in neglecting the child's welfare and potential legal repercussions for the healthcare provider.
Rationale for incorrect answers
A. Directly asking the child may not yield accurate information due to fear or coercion, limiting the effectiveness of disclosure. Nurses must rely on professional observation and mandated reporting rather than attempting personal interrogation, which may further distress the child.
B. Informing the physician and documenting findings support care coordination but do not fulfill the mandated reporting obligation. Without direct notification to child protective services, intervention may be delayed, increasing risk to the child and failing legal responsibilities.
D. Waiting for repeated incidents can lead to prolonged abuse and worsen harm. Nurses must act immediately upon suspicion, prioritizing the child's safety over observational delays. Hesitation to report violates ethical duties and legal requirements in child protection protocols.
Take Home Points
- Nurses are legally obligated to report suspected child abuse promptly to child protective services.
- Delayed reporting increases risk to the child and may have legal consequences.
- Documenting and notifying the physician support care but do not replace mandatory reporting.
- Immediate action ensures protection, intervention, and prevention of ongoing abuse.
A nurse brings a client’s morning medications, and the client says, “Just tell my wife. She gives me all my pills.” Which of the following responses by the nurse appropriately address the client’s request? Select all that apply
Explanation
Patient education in medication management Medication education is essential for patient autonomy, ensuring individuals understand their prescribed treatments. While caregivers play a supportive role, the patient must also be informed to prevent medication errors and ensure adherence. Involving family members can enhance compliance and safety.
Rationale for correct answers
C. Including the wife in medication education fosters shared responsibility while ensuring the patient remains informed. This approach supports adherence and allows both individuals to ask questions, improving understanding and safety.
E. Encouraging the patient to learn about their medications while involving their wife ensures comprehensive education. This strategy balances autonomy with caregiver support, reducing reliance on a single individual for medication management.
Rationale for incorrect answers
A. While emphasizing patient responsibility is important, this response may come across as confrontational rather than supportive, potentially discouraging engagement in medication education.
B. Providing a written list for the wife assumes she will always be available, neglecting the need for direct patient education. The patient must also understand their medications for independent management.
D. Simply affirming the patient's reliance on their wife does not address the importance of personal medication knowledge, missing an opportunity for education and empowerment.
Take Home Points
- Patients must understand their medications to ensure adherence and prevent errors.
- Involving caregivers in education supports compliance but should not replace patient learning.
- Nurses should encourage autonomy while providing supportive teaching strategies.
Medication education improves safety, reduces dependence, and enhances treatment outcomes.
A client reports continued but improving insomnia, anorexia, and crying spells following the death of the client’s spouse 1 month ago. Which is the most appropriate nursing diagnosis that a nurse should establish for the client?
Explanation
Impaired adjustment refers to a maladaptive reaction to a significant life change or stressor, such as loss or trauma. It is marked by emotional or behavioral symptoms that impair social functioning, last up to 3 months, and are not due to another mental disorder. Symptoms include depressed mood, anxiety, or disturbances in conduct but do not meet full criteria for major depressive disorder. It often occurs following a clearly identifiable stressor and usually resolves as the individual adapts or the stressor is removed. Diagnosis requires distress out of proportion to the stressor's severity but with a maintained level of some day-to-day functioning.
Rationale for correct answers
A. Emotional distress and functional ability are key here. The client exhibits emotional symptoms like insomnia, anorexia, and crying, but the improvement over time and presence of some coping indicate partial adaptation, consistent with impaired adjustment. The timeframe of one month fits diagnostic criteria, and the symptoms don’t yet qualify as major depressive disorder or pathological grief.
Rationale for incorrect answers
B. Ineffective coping is incorrect because the client is showing signs of improving symptoms, which implies some coping strategies are working. This diagnosis is more appropriate when no coping mechanisms are evident or distress is escalating.
C. Dysfunctional grieving is incorrect because the client’s response is within normal expectations for acute grief. There is no evidence of prolonged, delayed, or distorted grief processes which are necessary for this diagnosis.
D. Family processes interrupted is not appropriate as there is no information suggesting family role disruption, dysfunction, or strain in family dynamics. The issue is focused solely on the individual’s emotional response to personal loss.
Take Home Points
- Impaired adjustment includes emotional or behavioral symptoms that occur within 3 months of a stressor and cause functional impairment without meeting criteria for another disorder.
- It differs from major depression and pathological grief due to shorter duration and the absence of severe functional impairment.
- Normal grief is expected within the first 2 months post-loss and should show signs of gradual improvement.
- Always differentiate grief, depression, and adjustment disorders based on duration, severity, and functional impact.
A nurse is caring for a client with dementia. Which intervention takes top priority?
Explanation
Dementia is a progressive neurocognitive disorder that affects memory, judgment, and executive function, leading to impairment in daily functioning and increased vulnerability to environmental hazards. Safety is a top priority because clients with dementia may wander, fall, or engage in unsafe behaviors due to poor cognition and limited insight. Early stages involve memory loss and confusion, while advanced stages include severe disorientation, incontinence, and dependency. The risk of injury and inability to recognize danger make environmental safety a primary concern in care planning.
Rationale for correct answers
D. Safety risks and impaired judgment are dominant in dementia care. The client’s decreased ability to assess risk makes them prone to falls, ingestion of harmful substances, and wandering. A secure environment prevents injury and supports autonomy within safe limits.
Rationale for incorrect answers
A. While nutrition is important, it is not the most immediate concern. A client cannot safely eat or be fed unless the environment prevents choking, distraction, or injury first. Safety enables all other care aspects to be effective.
B. Rest and sleep are important but not urgent unless affected by agitation or behavioral issues. Lack of sleep does not immediately endanger the client like falls or elopement might. Rest becomes a priority after safety is established.
C. Hygiene and skin care are essential but do not surpass the need for a secure environment. Incontinence care reduces infection risk and discomfort but does not address immediate injury potential from environmental hazards.
Take Home Points
- Ensuring environmental safety is the first priority in dementia care due to the high risk of injury from wandering and poor judgment.
- Clients with dementia may not perceive danger or communicate needs effectively, increasing reliance on structured safe surroundings.
- Nutritional needs, hygiene, and sleep are important but become secondary to injury prevention.
- Dementia must be differentiated from delirium, which has acute onset and fluctuating levels of consciousness.
A nurse is establishing a therapeutic relationship with a client. Which of the following best describes this type of relationship in mental health nursing?
Explanation
A therapeutic relationship in mental health nursing is a professional alliance designed to support client well-being, promote healing, and encourage growth. It is built on trust, empathy, and clear boundaries. The relationship fosters emotional safety and collaboration, enabling patients to explore thoughts and behaviors in a nonjudgmental space. The nurse must remain objective, maintain confidentiality, and apply purposeful communication techniques. Unlike social relationships, this interaction is goal-directed, time-limited, and centered on the client’s needs and progress in treatment.
Rationale for correct answers
B. Collaborative and growth-oriented, this type of relationship centers on the client’s well-being. It facilitates emotional healing, builds insight, and empowers the patient, all while maintaining clear boundaries and therapeutic intent.
Rationale for incorrect answers
A. Becoming close friends with a client crosses professional boundaries. It compromises objectivity and may hinder the ability to provide appropriate care due to emotional involvement.
C. While emotional needs are acknowledged in mental health care, social interaction is not the goal. A therapeutic relationship is structured and focused on clinical outcomes, not casual emotional support.
D. A relationship focused on the nurse’s goals is self-serving and violates the ethical principles of nursing care. The therapeutic relationship must prioritize the client's needs, not the providers.
Take Home Points
- A therapeutic relationship is structured, professional, and goal-directed toward the client’s mental health needs.
- It differs from social relationships by maintaining boundaries, objectivity, and clinical focus.
- Emotional safety, empathy, and trust are foundational elements enabling healing and behavior change.
- It is essential to distinguish therapeutic relationships from friendships or self-serving interactions to uphold ethical standards.
A nursing student submits clinical paperwork using a client’s full name. Which of the following is the instructor’s priority response?
Explanation
Confidentiality is the legal and ethical obligation of nurses to protect client health information. It is mandated under the Health Insurance Portability and Accountability Act (HIPAA). Nurses must ensure that all identifiable health data are protected. This includes names, contact details, diagnosis, and treatment records. Breaches may occur via clinical paperwork, discussions in public spaces, or digital records. Even unintentional disclosure violates professional standards. Maintaining privacy preserves trust and promotes psychological safety in therapeutic relationships.
Rationale for correct answers
B. Maintain confidentiality is a priority in any healthcare setting. Using a client's full name in student paperwork is a direct breach of protected health information. The instructor must immediately correct this to prevent recurrence and reinforce legal compliance.
Rationale for incorrect answers
A. Reinforcing documentation is important, but it does not address the immediate breach of confidentiality, which takes precedence. Legal and ethical obligations must be corrected first.
C. Client competency does not negate the need for privacy. Even incompetent clients are fully protected under privacy laws and ethical practice standards.
D. Explaining HIPAA after class delays corrective action. The breach has already occurred and must be addressed immediately to prevent further risk and ensure learning is timely and effective.
Take Home Points
- All healthcare providers must protect identifiable patient information under HIPAA.
- Clinical paperwork used for academic purposes must omit names and other identifiers.
- Instructors are responsible for immediate correction of confidentiality breaches.
- Client competency status does not reduce the need for privacy protections.
A nurse is using seclusion for a violent client. Which of the following practices are appropriate? Select all that apply
Explanation
Seclusion is the involuntary confinement of a person alone in a designated area to prevent imminent harm. It requires continuous monitoring, regular reassessment, and removal once the threat subsides. Policy mandates no deprivation of basic needs and emphasizes trauma-informed, least-restrictive care.
Rationale for correct answers
A. Documenting the client’s behavior every 15 minutes ensures continuous monitoring and legal compliance with regulatory standards requiring frequent observation. The frequency reflects best practice in high-risk situations.
B. Discontinuing seclusion as soon as the client is calm aligns with the principle of the least restrictive intervention and seclusion should end immediately once the risk no longer exists.
Rationale for incorrect answers
C. Keeping the client for the full order regardless of behavior overrides the requirement to terminate seclusion early when safe, and violates the least restrictive mandate.
D. Allowing visitors during seclusion increases risk and violates seclusion protocols which require patient isolation to maintain safety and control.
E. Restricting food and water constitutes deprivation and is unethical and illegal; patients must have access to basic physiological needs throughout seclusion per Maslow and legal standards.
Take Home Points
- Seclusion is an emergency measure requiring continuous monitoring and frequent reassessment until the patient is calm.
- Orders must be reviewed and ended promptly when the risk decreases—use the least restrictive intervention.
- Never withhold food, water, or basic needs, and do not allow visitors during seclusion.
- Documentation must include behavior, interventions, timing, and reassessment to ensure safety and compliance.
A nurse is assessing five clients in the psychiatric unit. Which clients are legally able to give informed consent for treatment? Select all that apply
Explanation
Informed consent capacity refers to a person’s ability to understand, appreciate, reason about, and communicate treatment decisions. It requires intact orientation, cognitive functioning, and absence of legal incapacity, ensuring the individual can make autonomous health decisions.
Rationale for correct answers
C. A client with psychosis who is oriented and cooperative demonstrates intact capacity domains—understanding, appreciation, reasoning, and expression—so can legally consent to treatment despite psychiatric symptoms.
E. An adult with no cognitive impairments who clearly understands treatment meets all legal criteria—including competence, disclosure, absence of coercion—thus is fully capable of informed consent.
Rationale for incorrect answers
A. A 17-year-old minor generally cannot provide legal consent unless mature-minor or emancipation status applies, which isn’t indicated, so lacks legal authority independently.
B. A client declared incompetent by court lacks legal capacity explicitly and cannot provide informed consent for treatment under any circumstances until restored.
D. An unconscious trauma patient cannot understand or communicate information, and implied consent applies only in emergencies—not for ongoing psychiatric or elective treatments.
Take Home Points
- Capacity is task-specific and must be assessed in current context, especially in psychosis.
- Adults are presumed capable; legal incompetence must be court determined.
- Minors generally require guardian consent unless legally emancipated or judged mature.
- Unconscious or incapacitated patients cannot provide consent; implied consent applies only for emergencies.
Exams on Introduction To Mental Health Nursing
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
By the end of this lecture, the student nurse will be able to:
- Define mental health nursing and explain its scope of practice.
- Identify the legal and ethical responsibilities of a mental health nurse.
- Demonstrate knowledge of safe and effective care practices within psychiatric settings.
- Explain the role of health promotion, maintenance, and rehabilitation in mental health nursing.
- Discuss psychosocial integrity principles, including therapeutic communication and coping support.
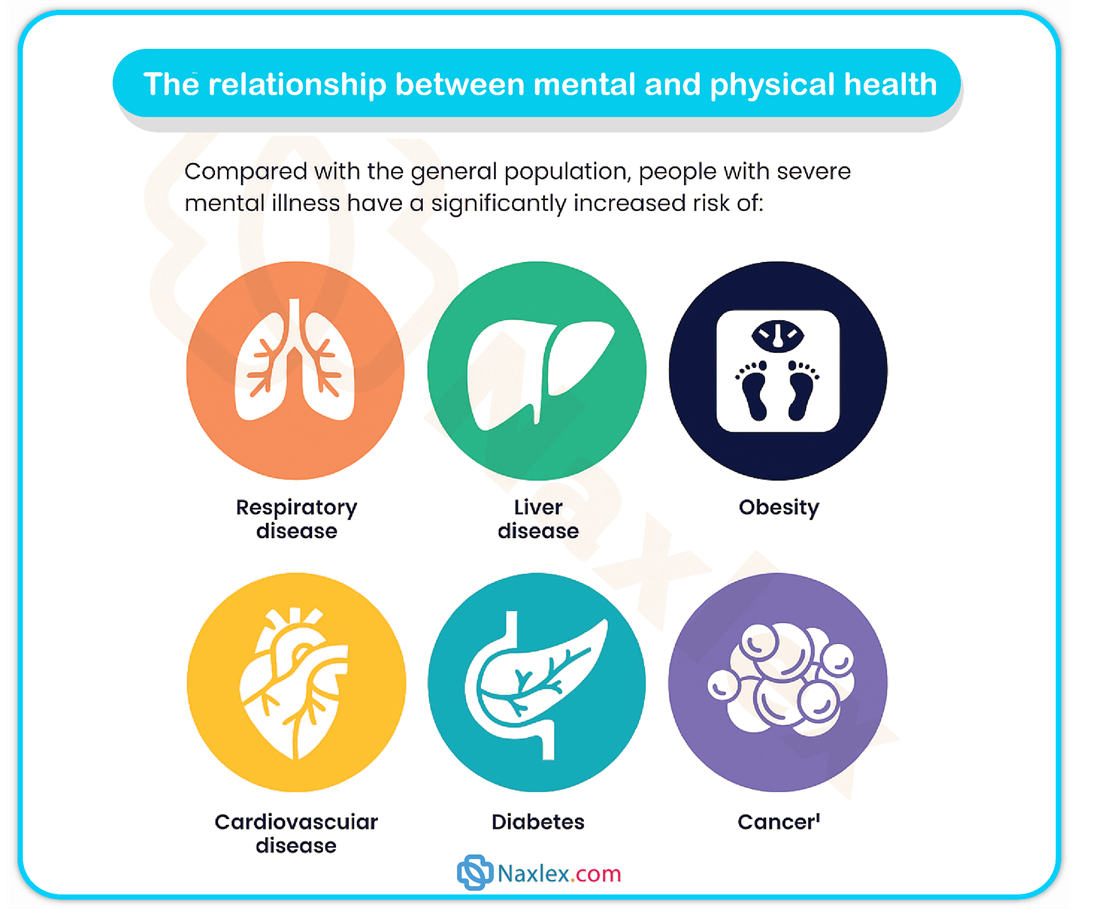
- Understand the relationship between mental health disorders and physiological health.
- Apply evidence-based nursing interventions for clients with mental health needs.
Introduction
- Mental health nursing, also referred to as psychiatric–mental health nursing, is a specialized area of nursing practice focused on the promotion of mental well-being, the prevention of mental disorders, and the therapeutic management of patients experiencing psychiatric conditions.
- It involves integrating biological, psychological, and social sciences to deliver holistic care to individuals, families, and communities.
- The nurse in this field utilizes the nursing process—assessment, diagnosis, planning, implementation, and evaluation—in conjunction with therapeutic use of self to foster recovery, optimize functioning, and enhance quality of life for clients with mental health needs.
- Psychiatric nursing is grounded in the principles of safety, evidence-based practice, cultural competence, patient advocacy, and legal-ethical accountability.
- It requires proficiency in communication, crisis intervention, psychopharmacology, and the management of comorbid physical and mental conditions.
Safe and Effective Care Environment
- The safe and effective care environment in mental health nursing is characterized by structured therapeutic settings, ethical and legal adherence, and comprehensive safety measures to prevent harm to clients, staff, and the public.
1.1 Therapeutic Nurse–Patient Relationship
- The therapeutic relationship is the foundation of psychiatric nursing practice.
- It is characterized by purposeful, goal-directed, and professional interactions that promote client insight, emotional expression, and problem-solving.
- The phases of the nurse–patient relationship include:
- Orientation Phase: Establishing rapport, defining roles, and identifying client needs.
- Working Phase: Facilitating behavioral change, exploring stressors, and reinforcing coping skills.
- Termination Phase: Reviewing progress, reinforcing adaptive coping, and ensuring continuity of care.
- Boundaries must be maintained at all times to prevent role blurring and countertransference.
Nursing Insights
- Always maintain professional boundaries; over-involvement or under-involvement impairs therapeutic outcomes.
- Use active listening, empathy, and unconditional positive regard to build trust.
- Recognize that the therapeutic use of self is a deliberate and skillful intervention.
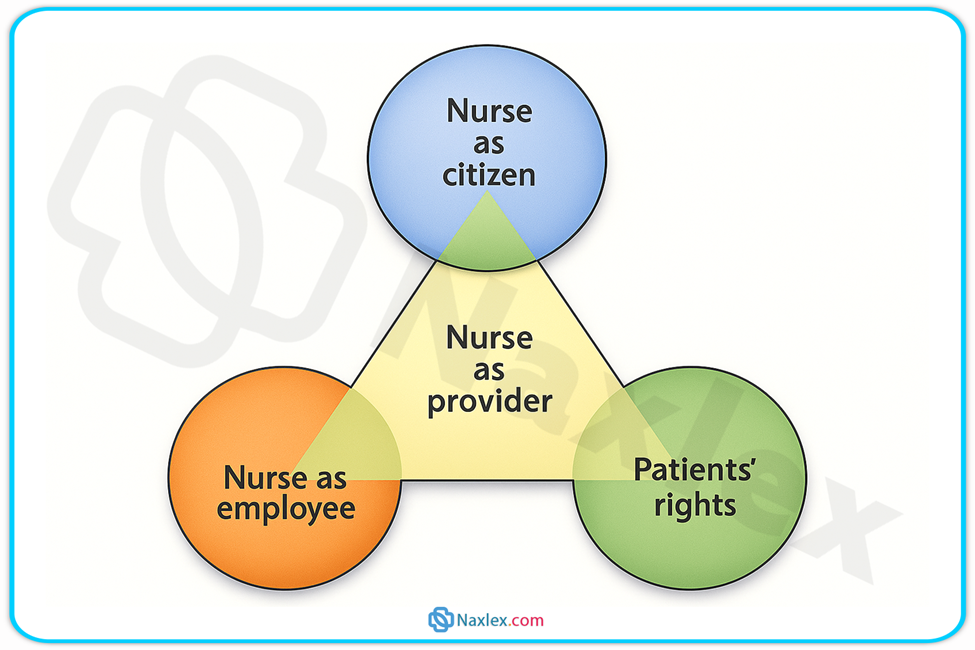
1.2 Legal and Ethical Considerations in Mental Health Nursing
- Autonomy: Respecting the patient’s right to make decisions about their care.
- Beneficence: Acting in the best interest of the client.
- Nonmaleficence: Avoiding harm.
- Justice: Fair treatment of all clients.
- Fidelity: Maintaining loyalty and commitments.
- Veracity: Providing truthful information.
- Legal aspects include:
- Involuntary admission criteria and patient rights.
- Confidentiality under HIPAA regulations.
- Duty to warn (Tarasoff ruling).
1.3 Safety Management in Psychiatric Care Settings
- Environmental safety measures include removing potential weapons, securing sharps, and maintaining observation levels.
- Suicide prevention protocols include risk assessment tools and continuous monitoring when indicated.
- Aggression management involves de-escalation techniques, staff training, and as a last resort, safe restraint use.
Health Promotion and Maintenance
Health promotion in mental health nursing focuses on enhancing psychological well-being and preventing psychiatric disorders through education, early intervention, and lifestyle modifications.
1.1 Primary Prevention in Mental Health
- Strategies aimed at preventing the onset of mental illness:
- Public education on stress management and healthy coping.
- Parenting programs to prevent childhood trauma.
- Community-based mental wellness campaigns.
1.2 Secondary Prevention and Early Identification of Mental Disorders
- Early screening for depression, anxiety, and substance use in primary care.
- Crisis intervention for individuals experiencing acute psychological distress.
- Prompt referral to psychiatric services to reduce morbidity.
1.3 Tertiary Prevention and Rehabilitation in Mental Health
- Focus on minimizing disability and restoring functioning in individuals with chronic mental illness.
- Includes vocational training, social skills development, and supported housing.
Nursing Insights
- Prevention is most effective when tailored to developmental stage, cultural background, and community resources.
- Nurses are frontline advocates for screening and early detection in both hospital and community settings.
Psychosocial Integrity
This domain addresses the nurse’s role in assisting clients to cope with life stressors, adapt to change, and maintain interpersonal relationships.
1.1 Communication Techniques in Mental Health Nursing
- Therapeutic communication includes active listening, reflecting, clarifying, and summarizing.
- Avoid non-therapeutic techniques such as giving advice, false reassurance, or changing the subject.
1.2 Coping Mechanisms and Stress Adaptation
- Adaptive coping: problem-solving, seeking social support, positive reframing.
- Maladaptive coping: substance abuse, aggression, withdrawal.
1.3 Crisis Intervention Strategies
- Aimed at stabilizing the client’s condition and preventing long-term psychological harm.
- Involves establishing safety, providing emotional support, and mobilizing resources.
Physiological Integrity
Mental disorders often have physiological manifestations and require integrated care.
1.1 Psychopharmacology Principles in Mental Health Care
- Classes include antidepressants, antipsychotics, mood stabilizers, anxiolytics.
- Nurses must monitor for therapeutic effects and side effects, including extrapyramidal symptoms, serotonin syndrome, and metabolic changes.
1.2 Physiological Effects of Mental Disorders on Body Systems
- Chronic stress can lead to hypertension, immune suppression, and gastrointestinal disturbances.
- Depression is associated with increased cardiovascular morbidity.
1.3 Nursing Management of Patients with Comorbid Psychiatric and Medical Conditions
- Requires coordination between medical and psychiatric teams.
- Monitoring for drug–drug interactions is critical.
Summary
Mental health nursing integrates scientific knowledge, therapeutic communication, legal–ethical principles, and safety measures to promote the psychological and physical well-being of individuals.
It requires mastery of prevention strategies, psychosocial interventions, and the physiological implications of mental illness, ensuring comprehensive and compassionate care delivery.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Introduction To Mental Health Nursing
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


