Please set your exam date
Middle and Inner Ear Disorders
Study Questions
Practice Exercise 1
What characteristics describe the care of a patient with chronic otitis media? Select all that apply
Explanation
Chronic otitis media is a persistent infection of the middle ear, often associated with eustachian tube dysfunction and recurrent effusion. Management may include surgical procedures such as myringotomy with tympanostomy tube insertion to facilitate drainage and prevent complications. Patients require careful education on ear protection and monitoring for reinfection.
Rationale for correct answers:
3. Impairment of the eustachian tube is most commonly associated with effusion: Chronic otitis media is often related to poor eustachian tube function, which leads to accumulation of fluid and recurrent infections.
5. The patient who has had a myringotomy with placement of a tympanostomy tube should be instructed to avoid getting water in the ear: Water entry can introduce pathogens into the middle ear, increasing risk of infection; ear protection is essential.
Rationale for incorrect answers:
1. It is most commonly treated with antibiotics: Chronic otitis media typically requires surgical management or long-term strategies rather than repeated antibiotic therapy, which is more applicable to acute otitis media.
2. It is an infection in the inner ear that may lead to headaches: Chronic otitis media affects the middle ear, not the inner ear; inner ear infections (labyrinthitis) are distinct and present differently.
4. Formation of an acoustic neuroma may destroy the structures of the middle ear or invade the dura of the brain: Acoustic neuromas are benign tumors of the vestibulocochlear nerve, unrelated to chronic otitis media.
Take home points:
- Chronic otitis media is linked to eustachian tube dysfunction and recurrent effusion.
- Surgical intervention (e.g., tympanostomy tubes) is common for management.
- Patient education includes avoiding water exposure in the ear after tube placement.
- Antibiotics are not the mainstay for chronic cases, unlike acute otitis media
While caring for a patient with otosclerosis, which finding would the nurse expect in the patient’s history and physical?
Explanation
Otosclerosis is a hereditary disorder of the bony labyrinth of the ear, where abnormal bone remodeling leads to fixation of the stapes, causing conductive hearing loss. It commonly presents in early to middle adulthood and has a significant genetic predisposition. Surgical treatment (stapedectomy or stapedotomy) can improve hearing, but immediate consistent restoration is not always expected.
Rationale for correct answer:
- A strong family history of the disease: Otosclerosis often follows an autosomal dominant inheritance pattern, making family history a key expected finding in a patient’s history.
Rationale for incorrect answers:
2. Symptoms of sensorineural hearing loss: Otosclerosis primarily causes conductive hearing loss due to stapes fixation, not sensorineural hearing loss.
3. A positive Rinne test and lateralization to the good or better ear on Weber testing: In conductive hearing loss (otosclerosis), Rinne is typically negative (bone conduction > air conduction), and Weber lateralizes to the affected ear, not the good ear.
4. An immediate and consistent improvement in hearing at the time of surgical treatment: Postoperative results vary; while many patients experience hearing improvement, it is not always immediate or guaranteed.
Take home points:
- Otosclerosis is an inherited cause of conductive hearing loss.
- Family history is a significant diagnostic clue.
- Rinne test negative and Weber lateralizing to the affected ear are expected in conductive hearing loss.
- Surgery (stapedectomy/stapedotomy) can help but does not always result in immediate or perfect improvement.
What characteristics of hearing loss are associated with conductive loss? Select all that apply
Explanation
Conductive hearing loss occurs when there is an obstruction or dysfunction in the external or middle ear that prevents sound waves from reaching the inner ear. This can result from infections, structural problems, or mechanical obstructions such as cerumen impaction. Patients often report improved hearing in noisy environments because external sounds can mask background noise.
Rationale for correct answers:
3. Related to otitis media: Middle ear infections interfere with sound conduction, making otitis media a common cause of conductive hearing loss.
5. Hears best in noisy environment: People with conductive hearing loss often hear better in noisy surroundings because the loss is mechanical rather than neural, so background noise may enhance speech perception.
6. May be caused by impacted cerumen: Blockage of the ear canal by wax prevents sound waves from reaching the tympanic membrane, leading to conductive loss.
Rationale for incorrect answers:
1. Presbycusis: This is age-related, progressive sensorineural hearing loss, not conductive.
2. Speaks softly: Patients with sensorineural hearing loss often speak loudly because they cannot hear themselves clearly; conductive loss patients usually speak at a normal level.
4. Result of ototoxic drugs: Ototoxicity damages the cochlea or auditory nerve, leading to sensorineural hearing loss, not conductive loss.
Take home points:
- Conductive hearing loss originates from problems in the outer or middle ear (e.g., wax, infection, structural issues).
- Common causes: otitis media, impacted cerumen, otosclerosis.
- Patients may hear better in noisy environments.
- Differentiated from sensorineural loss (e.g., presbycusis, ototoxicity) by cause and clinical findings.
The nurse suspects a patient has presbycusis when she says she has
Explanation
Presbycusis is an age-related, progressive sensorineural hearing loss caused by degeneration of the cochlea, auditory nerve, or inner ear structures. It typically begins with difficulty hearing high-pitched sounds and progresses to challenges with speech discrimination.
Rationale for correct answer:
4. A decrease in the ability to hear high-pitched sounds: This is the hallmark of presbycusis. It occurs because the high-frequency hair cells in the cochlea are most susceptible to age-related degeneration. Patients may initially report trouble hearing doorbells, telephones, or voices of women and children.
Rationale for incorrect answers:
- Ringing in the ears: This refers to tinnitus, which can accompany presbycusis but is not the defining feature. Many other conditions such as noise exposure, medications, or vascular problems can also cause tinnitus, so it is not specific to age-related hearing loss.
- A sensation of fullness in the ears: This is more typical of conductive hearing problems, such as otitis media or cerumen impaction. In presbycusis, there is no obstruction in the outer or middle ear, so fullness is not an expected finding.
- Difficulty understanding the meaning of words: This symptom reflects reduced speech discrimination, which may occur in advanced presbycusis. However, it develops later in the condition rather than being the earliest or primary characteristic.
Take home points:
- Presbycusis = age-related sensorineural hearing loss.
- The earliest and most specific symptom is inability to hear high-pitched sounds.
- Progression may lead to poor speech discrimination and communication difficulties.
- Differentiate from conductive causes, which present with fullness, wax, or infection.
A client receives a prescription for sodium fluoride for otosclerosis and asks a nurse what the medication will do for his ears. Which response by the nurse is correct?
Explanation
Otosclerosis is a hereditary condition where abnormal bone remodeling leads to fixation of the stapes bone, producing conductive hearing loss. Sodium fluoride may be prescribed to help slow the disease process by stabilizing the abnormal bone turnover. Although surgery is the main treatment, medication can sometimes be used as an adjunct.
Rationale for correct answer:
- “The medication prevents the breakdown of bone cells and hardens the bone in the ear.”: Sodium fluoride helps to inhibit further bone resorption and promotes calcification, which can stabilize the abnormal growth. This effect may slow the progression of otosclerosis, although it does not reverse existing hearing loss.
Rationale for incorrect answers:
2. “The medication causes the breakdown of bone cells and softens the bone in the ear.”: Sodium fluoride does not cause breakdown of bone cells or softening; in fact, its role is the opposite—slowing bone remodeling and hardening the abnormal bone. Softening of bone would worsen hearing rather than improve it.
3. “The medication blocks the effect of histamine and dries the fluid in the ear.”: Antihistamines act in this way, but sodium fluoride is not an antihistamine and does not affect fluid balance in the ear. This choice confuses otosclerosis with inner ear conditions like Ménière’s disease.
4. “The medication causes the production of histamine and increases the fluid in the ear.”: Sodium fluoride has no relation to histamine production or fluid accumulation. An increase in inner ear fluid would worsen hearing symptoms, not improve them.
Take home points:
- Otosclerosis involves abnormal bone growth around the stapes, causing conductive hearing loss.
- Sodium fluoride helps slow bone resorption and promotes calcification, stabilizing disease progression.
- Surgery (stapedectomy or stapedotomy) remains the definitive treatment.
- Distinguish from inner ear fluid problems (e.g., Ménière’s), which involve histamine and fluid balance, not abnormal bone remodeling.
Practice Exercise 2
What makes up the triad of symptoms that occur with inner ear problems? Select all that apply
Explanation
Inner ear disorders, such as Ménière’s disease, often present with a characteristic triad of symptoms: vertigo, tinnitus, and sensorineural hearing loss. These result from abnormal fluid accumulation (endolymphatic hydrops) in the inner ear, which affects both balance and hearing. Nausea may occur secondarily due to vertigo, but it is not part of the classic triad.
Rationale for correct answers:
1. Vertigo: Inner ear problems, especially Ménière’s disease, commonly cause spinning sensations due to disturbances in the vestibular system. This vertigo is often sudden, severe, and disabling, lasting from minutes to hours.
3. Tinnitus: A hallmark symptom of inner ear disorders is tinnitus, or ringing in the ears. This occurs because of abnormal stimulation or damage to the cochlear hair cells, leading to perception of sound without external input.
4. Sensorineural hearing loss: Inner ear damage affects the cochlea or auditory nerve, leading to sensorineural loss. In Ménière’s disease, hearing loss often begins intermittently but may progress to permanent loss over time.
Rationale for incorrect answers:
2. Nausea: While nausea and vomiting often accompany vertigo, they are secondary effects of the balance disturbance rather than a core part of the triad. They are common symptoms but not diagnostic criteria.
5. Inflammation of the ear canal: This describes otitis externa (swimmer’s ear), which affects the outer ear, not the inner ear. It causes localized pain, swelling, and discharge but not the triad associated with inner ear disorders.
Take home points:
- Classic triad of inner ear disorders (e.g., Ménière’s): vertigo, tinnitus, and sensorineural hearing loss.
- Nausea and vomiting may occur, but they are secondary to vertigo.
- Differentiate from outer ear problems (pain, inflammation, discharge) and middle ear conditions (conductive hearing loss, effusion).
An appropriate nursing intervention for the patient during an acute attack of Meniere disease includes providing
Explanation
Ménière disease is an inner ear disorder characterized by recurrent episodes of vertigo, tinnitus, and sensorineural hearing loss. During an acute attack, patients experience severe spinning sensations, nausea, and imbalance, making rest and environmental control critical. The priority nursing intervention is to provide a calm setting that minimizes sensory stimulation.
Rationale for correct answer:
2. A quiet, darkened room: Patients with acute Ménière attacks are extremely sensitive to motion, light, and noise, which can worsen vertigo and nausea. A quiet, darkened environment helps reduce sensory input and allows the vestibular system to stabilize.
Rationale for incorrect answers:
1. Frequent repositioning: Moving the patient frequently will worsen vertigo and increase nausea. The patient should be kept as still as possible until symptoms subside.
3. A television for diversion: Visual stimulation, such as watching television, can aggravate dizziness and nausea during an acute attack, making it inappropriate.
4. Padded side rails on the bed: While useful for seizure precautions, side rails do not address the underlying issue of vertigo in Ménière disease. The priority intervention is reducing environmental stimuli.
Take home points:
- Acute Ménière attacks require quiet, darkened rooms to minimize sensory input.
- Movement, light, and noise can worsen vertigo and nausea.
- Safety is important, but environmental control is the first priority intervention.
What knowledge guides the nurse in providing care for a patient with an acoustic neuroma?
Explanation
An acoustic neuroma is a benign tumor that arises from the vestibulocochlear nerve (cranial nerve VIII). Because of its location, it can compress nearby nerves, especially the cochlear and vestibular branches, leading to progressive hearing loss, tinnitus, and balance problems. Early recognition and intervention are important to preserve hearing and vestibular function while also preventing complications like facial nerve damage or brainstem compression.
Rationale for correct answer:
3. Early diagnosis and treatment of the tumor can preserve hearing and vestibular function: Detecting the neuroma in its early stages allows for treatment before significant nerve compression occurs. This can prevent permanent sensorineural hearing loss and reduce the risk of balance disturbances.
Rationale for incorrect answers:
1. Widespread metastasis usually occurs before symptoms of the tumor are noticed: Acoustic neuromas are benign, non-metastatic tumors. The symptoms result from local compression, not spread to other body sites.
2. Facial nerve function will be sacrificed during surgical treatment to preserve hearing: The goal of surgery is to remove the tumor while preserving both hearing and facial nerve function. Sacrificing the facial nerve is not an expected or planned outcome.
4. Treatment is usually delayed until hearing loss is significant because a neuroma is a benign tumor: Even though the tumor is benign, delaying treatment risks irreversible hearing loss, facial nerve damage, or brainstem compression. Early intervention improves prognosis.
Take home points:
- Acoustic neuroma = benign tumor of the vestibulocochlear nerve.
- Early diagnosis and treatment are essential to preserve hearing and balance function.
- Symptoms include unilateral hearing loss, tinnitus, and disequilibrium.
- Untreated growth can cause compression of the facial nerve and even the brainstem, leading to serious complications.
What characteristics of hearing loss are associated with sensorineural loss? Select all that apply
Explanation
Sensorineural hearing loss results from damage to the inner ear structures (cochlea, hair cells) or auditory nerve pathways. It is often irreversible and caused by conditions such as noise trauma, aging (presbycusis), Ménière disease, or ototoxic medications. Conductive causes, such as otitis media and otosclerosis, are not part of sensorineural loss.
Rationale for correct answers:
3. Caused by noise trauma: Prolonged exposure to loud sounds damages the delicate hair cells in the cochlea, leading to permanent sensorineural hearing loss. This is a common preventable cause of hearing loss in younger and working-age adults.
5. Associated with Ménière disease: Ménière disease is an inner ear disorder caused by abnormal fluid buildup that damages cochlear and vestibular structures. Over time, this leads to progressive sensorineural hearing loss, tinnitus, and vertigo.
Rationale for incorrect answers:
1. Hearing aid is helpful: While hearing aids can amplify sounds, they cannot correct distortion caused by nerve or cochlear damage. They are more effective in conductive loss, though some benefit may still occur in mild-to-moderate sensorineural loss.
2. Related to otitis media: Otitis media is a middle ear infection that interferes with sound conduction, causing conductive hearing loss, not sensorineural. Once treated, hearing usually improves unless chronic damage occurs.
4. Linked with otosclerosis: Otosclerosis involves abnormal bone growth in the middle ear that immobilizes the stapes. This results in conductive hearing loss, though in rare advanced cases it can extend to the cochlea (mixed hearing loss).
Take home points:
- Sensorineural loss = damage to the inner ear or auditory nerve.
- Major causes: noise trauma, Ménière disease, presbycusis, ototoxicity.
- Conductive causes include otitis media and otosclerosis, not sensorineural.
- Hearing aids may help somewhat, but they cannot restore lost nerve function.
What indicates sensorineural hearing loss? Select all that apply
Explanation
Sensorineural hearing loss results from damage to the inner ear (cochlea, hair cells) or the auditory nerve pathways. Tuning fork tests such as Rinne and Weber help differentiate between sensorineural and conductive loss. In sensorineural loss, air conduction remains better than bone conduction (positive Rinne), but sound lateralizes to the good ear on Weber testing.
Rationale for correct answers:
1. Positive Rinne test: In sensorineural loss, air conduction remains better than bone conduction because the pathway through the outer and middle ear is intact. This results in a positive Rinne test, even though overall hearing is reduced.
4. Weber lateralization to good ear: In Weber testing, sound localizes to the unaffected ear because the damaged inner ear cannot perceive the vibration as well. This helps differentiate sensorineural loss from conductive loss, which lateralizes to the impaired ear.
6. Inner ear or nerve pathway pathology: Sensorineural hearing loss originates from damage to the cochlea, auditory nerve, or central auditory pathways. Causes include presbycusis, noise trauma, Ménière disease, and ototoxic drugs.
Rationale for incorrect answers:
2. Negative Rinne test: A negative Rinne (bone conduction > air conduction) indicates conductive hearing loss, not sensorineural. It reflects impaired sound transmission through the outer or middle ear.
3. Weber lateralization to impaired ear: Lateralization to the impaired ear occurs in conductive loss, where background noise is reduced, making the vibration more noticeable. It does not occur in sensorineural loss.
5. External or middle ear pathology: Pathology in the outer or middle ear causes conductive loss, not sensorineural. Sensorineural loss always involves the inner ear or auditory nerve.
Take home points:
- Sensorineural hearing loss = positive Rinne, Weber to good ear, inner ear/nerve pathology.
- Conductive hearing loss = negative Rinne, Weber to impaired ear, outer/middle ear pathology.
- Tuning fork tests are key bedside tools to distinguish between conductive and sensorineural loss.
Practice Exercise 3
When teaching a patient to use a hearing aid, where does the nurse encourage the patient to initially use the aid?
Explanation
Hearing aids are devices that amplify sound to help patients with hearing loss, but initial use requires adaptation. Patients often need time to adjust to amplified sounds, recognize speech, and learn to fine-tune tone and volume. A quiet, controlled environment is best for this learning process, before progressing to more complex listening situations.
Rationale for correct answer:
3. In a quiet, controlled environment to experiment with tone and volume: Beginning in a quiet setting allows the patient to gradually adjust to amplified sounds without overwhelming background noise. This helps them become comfortable with volume adjustments and builds confidence before using the aid in challenging environments.
Rationale for incorrect answers:
1. Outdoors, where sounds are distinct: Outdoor settings include unpredictable sounds such as wind, traffic, or birds, which can be overwhelming for new hearing aid users. This can make adaptation frustrating and less successful.
2. At social functions, where simultaneous conversations take place: Social gatherings present too much competing background noise, which is especially difficult for someone just learning to use a hearing aid. This can discourage use rather than promote adjustment.
4. In public areas such as malls or stores, where others will not notice its use: Public areas have a variety of unpredictable noises, making them poor initial learning environments. The priority is not hiding the hearing aid but ensuring effective adaptation in a controlled setting.
Take home points:
- Hearing aid teaching begins in a quiet, controlled environment to help patients adapt comfortably.
- Gradual progression to noisier and more complex environments increases success.
- Early overwhelming environments may lead to frustration and discourage consistent use.
The nurse identifies a nursing diagnosis of risk for injury for a patient following a stapedectomy based on what knowledge about this surgery?
Explanation
Stapedectomy is a surgical procedure performed to improve hearing in patients with otosclerosis by replacing the stapes bone. Because the procedure directly involves the middle and inner ear structures, labyrinth stimulation may occur, leading to postoperative vertigo and imbalance. This makes the patient at high risk for falls or other injuries during the recovery period.
Rationale for correct answer:
2. Stimulation of the labyrinth during surgery may cause vertigo and loss of balance: Vertigo and imbalance are common after stapedectomy due to disturbance of the vestibular apparatus. These symptoms increase fall risk, making safety precautions and assistance with ambulation essential.
Rationale for incorrect answers:
1. Nystagmus may result from perilymph disturbances caused by surgery: While nystagmus can occur, it is usually transient and does not directly increase the risk of injury as much as vertigo and imbalance do. The major safety concern is dizziness and instability.
3. Blowing the nose or coughing may precipitate dislodgement of the tympanic graft: This is true regarding graft protection, but it does not directly explain the risk for injury diagnosis. It is more related to risk for impaired healing.
4. Postoperative tinnitus may decrease the patient’s awareness of environmental hazards: Tinnitus is bothersome but does not significantly impair safety or balance compared to vertigo. It is not the primary risk factor for injury.
Take home points:
- After stapedectomy, patients are at high risk for injury due to vertigo and imbalance.
- Safety interventions include assistance with ambulation, avoiding sudden movements, and fall precautions.
- Patient teaching should emphasize avoiding actions that increase pressure in the ear, but priority remains injury prevention.
When does caloric testing indicate disease of the vestibular system of the ear?
Explanation
Caloric testing is a diagnostic procedure used to evaluate the function of the vestibular system by irrigating the ear canal with warm or cold water and observing eye movements (nystagmus). A normal response is the development of nystagmus, which demonstrates intact vestibular function. Absence of nystagmus indicates abnormal vestibular function and is consistent with disease or dysfunction of the vestibular apparatus or nerve.
Rationale for correct answer:
2. No nystagmus is elicited with application of water in the external ear: The absence of nystagmus during caloric testing is abnormal and strongly suggests vestibular dysfunction. This means the labyrinth or vestibular nerve is not responding properly to stimulation, which helps in diagnosing inner ear disease.
Rationale for incorrect answers:
1. Hearing is improved with irrigation of the external ear canal: Improvement in hearing after irrigation usually indicates removal of impacted cerumen, which is unrelated to vestibular system function. This finding does not diagnose inner ear disease.
3. The patient experiences intolerable pain with irrigation of the external ear: Pain suggests an inflamed or infected external ear canal (otitis externa) but has nothing to do with the vestibular system’s integrity. It is not the purpose of caloric testing.
4. Irrigation of the external ear with water produces nystagmus opposite the side of instillation: Nystagmus is the normal expected response, indicating intact vestibular function. This would not point to disease, but rather to a healthy vestibular system.
Take home points:
- Normal caloric testing = nystagmus is elicited.
- Abnormal caloric testing = absence of nystagmus, which indicates vestibular dysfunction.
- The test helps distinguish inner ear and vestibular nerve disorders from other causes of dizziness or balance problems.
Results of an audiometry indicate that a patient has a 10-dB hearing loss at 8000 Hz. What is the most appropriate action by the nurse?
Explanation
Audiometry measures hearing sensitivity across different frequencies. A 10-dB loss at 8000 Hz represents a very mild, high-frequency hearing loss, which usually does not require aggressive interventions such as hearing aids or lip-reading. At this stage, the nurse should focus on effective, clear communication, and reassurance by speaking normally without exaggerating volume or speed.
Rationale for correct answer:
2. Speak at a normal speed and volume with the patient: A 10-dB loss is minimal and not likely to significantly impact daily communication. The best approach is to maintain normal speech patterns to avoid drawing unnecessary attention or creating anxiety about the minor hearing change.
Rationale for incorrect answers:
1. Encourage the patient to start learning to lip-read: Lip-reading is typically recommended for patients with moderate-to-severe hearing loss. It is unnecessary and premature for a very mild high-frequency deficit.
3. Avoid words in conversation that have many high-pitched consonants: Although consonant sounds may be harder to hear in advanced high-frequency loss, avoiding such words is not a realistic or appropriate strategy for such a minimal loss.
4. Discuss the advantages and disadvantages of various hearing aids with the patient: A 10-dB hearing loss does not warrant the use of a hearing aid, as it is within the range of normal conversational hearing. This would not be appropriate at this stage.
Take home points:
- A 10-dB hearing loss at high frequencies is minimal and usually requires no treatment.
- Nurses should speak normally without raising their voice unnecessarily.
- Interventions like lip-reading training or hearing aids are reserved for more significant hearing losses.
What accurately describes an assessment of the ear?
Explanation
Ear assessment requires knowledge of normal tympanic membrane landmarks. The umbo, handle of malleus, and cone of light are expected findings and help the nurse distinguish a healthy eardrum from pathological changes. Recognizing these landmarks is essential for detecting abnormalities such as infection, fluid, or perforation.
Rationale for correct answer:
- Major landmarks of the tympanic membrane include the umbo, handle of malleus, and cone of light: These structures are normal anatomical features that should be visible on otoscopic exam. Their presence helps confirm that the tympanic membrane is intact and healthy.
Rationale for incorrect answers:
2. The presence of a retracted eardrum on otoscopic examination is indicative of positive pressure in the middle ear: A retracted eardrum actually indicates negative pressure due to eustachian tube dysfunction, not positive pressure.
3. In chronic otitis media, the nurse would expect to find a lack of landmarks and a bulging eardrum on otoscopic examination: A bulging tympanic membrane is more typical of acute otitis media. Chronic otitis media usually shows scarring, perforation, or thickening, not acute bulging.
4. To straighten the ear canal in an adult before insertion of the otoscope, the nurse grasps the auricle and pulls downward and backward: For adults, the auricle should be pulled upward and backward. Downward and backward is correct for children under 3 years of age.
Take home points:
- Normal tympanic membrane landmarks include the umbo, handle of malleus, and cone of light.
- Retracted tympanic membrane = negative middle ear pressure, not positive.
- Bulging tympanic membrane = acute otitis media, while chronic cases show scarring or perforation.
- For otoscope insertion: pull the auricle up and back in adults, down and back in children <3 years.
Comprehensive Questions
A nurse is performing an otoscopic examination of a client. Which of the following is an unexpected finding?
Explanation
An otoscopic exam assesses for normal tympanic membrane appearance and external canal condition. A pearly gray TM with visible landmarks is expected, and minor flaky skin may be normal in the external canal. However, black cerumen partially occluding the TM is unexpected, as it may interfere with assessment and hearing, requiring removal.
Rationale for correct answer:
4. Black cerumen partially occluding the TM: Cerumen should normally be light yellow to brown and not obstruct the view of the TM. Black or impacted cerumen is considered abnormal, as it may signal excessive buildup, fungal infection, or hinder visualization of ear structures.
Rationale for incorrect answers:
- Pearly, gray tympanic membrane (TM): This is the normal color and appearance of a healthy eardrum, showing no infection or fluid behind the TM.
- Malleus visible behind the TM: The malleus is a normal landmark visible on otoscopic exam and helps confirm proper identification of the TM.
- Flaky skin in the external canal near the TM: Small amounts of flaky skin can be normal, especially in clients with dry skin or after healing of mild irritation. It is not necessarily pathological.
Take home points:
- Normal TM = pearly gray, translucent, with visible malleus and cone of light.
- Black or obstructing cerumen = abnormal finding that may require removal for proper exam.
- Flaky skin in canal can be a benign finding, but persistent inflammation or scaling may need follow-up.
A nurse in a clinic is caring for a client who has been experiencing mild to moderate vertigo due to benign paroxysmal vertigo for several weeks. Which of the following actions should the nurse recommend to help control the vertigo? Select all that apply
Explanation
Benign paroxysmal positional vertigo (BPPV) is a vestibular disorder caused by displacement of calcium carbonate crystals (otoconia) into the semicircular canals of the inner ear. This condition leads to brief episodes of vertigo that are triggered by changes in head position. Patients often describe dizziness, imbalance, or a spinning sensation that interferes with daily activities. Nursing care focuses on lifestyle modifications, movement precautions, and avoidance of risk factors that may worsen vestibular symptoms. Proper teaching helps patients minimize the frequency and severity of vertigo episodes and promotes overall safety.
Rationale for correct answers:
2. Move head slowly when changing positions: Rapid movements worsen vertigo by shifting otoliths in the semicircular canals. Slow, deliberate head movements minimize dizziness and reduce the risk of falls.
4. Plan evenly spaced daily fluid intake: Adequate hydration helps stabilize inner ear fluid balance, which can reduce vertigo symptoms. Even fluid intake throughout the day prevents sudden fluid shifts that may worsen dizziness.
5. Avoid smoking: Nicotine impairs circulation to the inner ear, which may intensify vestibular symptoms. Avoiding smoking supports vestibular health and reduces the risk of worsening vertigo.
Rationale for incorrect answers:
1. Reduce exposure to bright lighting: While helpful in migraine-related dizziness, light sensitivity does not affect BPPV. The vertigo stems from inner ear positional changes, not visual triggers.
3. Avoid fruits high in potassium: Potassium has no effect on BPPV symptoms and does not require restriction. On the contrary, potassium-rich foods support cardiovascular and neuromuscular health.
Take home points:
- BPPV results from displacement of crystals in the inner ear, leading to position-related vertigo.
- Patients should move slowly, maintain hydration, and avoid smoking to control symptoms.
- Bright light exposure and potassium intake are not linked to BPPV symptom management.
A nurse is caring for a client who has suspected Ménière’s disease. Which of the following is an expected finding?
Explanation
Ménière’s disease is a chronic disorder of the inner ear caused by an imbalance of endolymphatic fluid. It is characterized by a triad of symptoms: vertigo, tinnitus, and sensorineural hearing loss. In the early stages, hearing loss typically occurs in only one ear and may fluctuate, but it often progresses with time. Patients may also experience a sensation of fullness or pressure in the affected ear, which further supports the diagnosis. Early recognition of these hallmark symptoms is crucial for proper management and patient safety.
Rationale for correct answer:
4. Unilateral hearing loss: This is a classic finding in Ménière’s disease, usually accompanied by vertigo and tinnitus. The progressive, one-sided sensorineural loss helps differentiate it from external or middle ear pathologies.
Rationale for incorrect answers:
- Presence of a purulent lesion in the external ear canal: This finding is typical of external otitis, not Ménière’s disease. Ménière’s involves the inner ear, not the external canal.
- Recent history of plane travel: Barotrauma from pressure changes may affect the middle ear, but it is not associated with Ménière’s disease, which is an inner ear condition.
- Bulging, red bilateral tympanic membranes: This is consistent with acute otitis media, a middle ear infection, not an inner ear fluid disorder like Ménière’s.
Take home points:
- Ménière’s disease presents with vertigo, tinnitus, and progressive unilateral hearing loss.
- The disorder results from an endolymphatic fluid imbalance within the inner ear.
- Differentiation from external and middle ear conditions is key for accurate diagnosis and management.
A nurse is reviewing the health record of a client who has a middle ear disorder. Which of the following are expected findings? Select all that apply
Explanation
Middle ear disorders are often linked to blockage of the eustachian tube, which impairs drainage and ventilation. Enlarged adenoids or a history of recurrent upper respiratory infections are key risk factors. The resulting fluid accumulation or infection leads to characteristic symptoms such as hearing loss, pressure, or discomfort in the ear. Identifying these associated factors helps the nurse anticipate complications and plan effective interventions.
Rationale for correct answers:
- Enlarged adenoids: Enlarged adenoids can obstruct the eustachian tube, preventing normal drainage of middle ear secretions. This makes patients more susceptible to infections and effusions.
- Report of recent colds: Recurrent colds or upper respiratory infections increase the risk of middle ear disorders. The inflammation and congestion impair eustachian tube function, leading to middle ear fluid buildup.
Rationale for incorrect answers:
3. Discontinued prescription for furosemide 6 months ago: Furosemide is associated with sensorineural hearing loss due to ototoxicity, not middle ear disorders. Past use would not cause middle ear pathology.
4. Light reflexes visible on otoscopic exam at 5 and 7 o’clock: A normal light reflex indicates a healthy tympanic membrane. In middle ear disorders, the reflex is often absent or distorted due to fluid or infection.
5. Report of frequent ingestion of ibuprofen: Ibuprofen may contribute to sensorineural hearing changes when used in excess but does not cause middle ear disorders.
Take home points:
- Enlarged adenoids and recent colds are common risk factors for middle ear pathology.
- Middle ear issues are linked to eustachian tube dysfunction and fluid accumulation.
- Ototoxic medications and a normal otoscopic exam do not point to middle ear disorders.
A nurse is completing discharge teaching to a client following a stapedectomy. Which of the following statements by the client indicates understanding of the teaching?
Explanation
After a stapedectomy, clients must follow careful discharge instructions to prevent infection, protect the surgical site, and promote healing. One important teaching point is to keep the ear dry to avoid complications. Hearing improvement is often gradual rather than immediate, and activity restrictions are necessary to allow proper recovery of the middle ear.
Rationale for correct answer:
2. “I will cover my ear when washing my hair.”: This statement reflects correct understanding. Protecting the ear from water prevents infection and ensures the surgical site heals properly.
Rationale for incorrect answers:
1. “I am glad I’ll be able to return to my position as an airplane pilot right away.”: Air travel and high altitudes are contraindicated during the recovery phase due to pressure changes that can affect the ear.
3. “I will remove the dressing behind my ear in 7 days.”: The dressing should only be removed by a healthcare provider, not by the patient, to avoid disrupting the surgical site.
4. “I can expect my hearing to return in 24 hours.”: Hearing improvement after stapedectomy is gradual and may take several weeks. Immediate full recovery of hearing is not expected.
Take home points:
- Clients should keep the ear dry to prevent infection after stapedectomy.
- Air travel, heavy lifting, and straining are restricted during recovery.
- Hearing improvement is progressive, not immediate.
During an assessment of hearing, the nurse would expect to find a normal finding of
Explanation
A hearing assessment helps determine the client’s ability to detect sound conduction through air and bone, and whether sound is perceived equally in both ears. A normal finding on the Weber test is when the tone is heard equally in both ears, indicating no lateralization. Abnormal findings include absent cone of light, fluid behind the tympanic membrane, or discoloration of the tympanic membrane.
Rationale for correct answer:
3. Midline tone heard equally in both ears. This is the expected finding during the Weber test. It indicates that sound conduction is normal and there is no sensorineural or conductive hearing loss.
Rationale for incorrect answers:
1. Absent cone of light. The cone of light should normally be visible on otoscopic examination; its absence suggests middle ear pathology.
2. Bluish purple tympanic membrane. A healthy tympanic membrane should be pearly gray; discoloration indicates abnormality such as trauma or infection.
4. Fluid level at hairline in the tympanum. The presence of fluid suggests otitis media with effusion or another middle ear disorder.
Take home points:
- Normal Weber test finding: tone heard equally in both ears.
- A healthy tympanic membrane is pearly gray with a visible cone of light.
- Fluid or discoloration of the tympanic membrane indicates pathology.
Age-related changes in the auditory system commonly include (select all that apply)
Explanation
As people age, changes in the auditory system can affect both the external and inner ear structures, leading to hearing impairment. The cerumen often becomes drier and harder, which may obstruct the canal. Auditory nerve degeneration contributes to presbycusis, a sensorineural hearing loss associated with aging. Additionally, atrophy of the tympanic membrane reduces sound conduction efficiency. While tinnitus may occur, it is not universal, and hearing high-pitched sounds usually becomes more difficult, not easier.
Rationale for correct answers:
1. Drier cerumen. Aging causes cerumen to become thicker and drier, which may accumulate and impair hearing.
3. Auditory nerve degeneration. Degeneration of the cochlear nerve and hair cells contributes to presbycusis, the most common age-related hearing loss.
4. Atrophy of the tympanic membrane. The eardrum becomes thinner and less elastic with age, reducing its ability to transmit sound effectively.
Rationale for incorrect answers:
2. Tinnitus in both ears. While tinnitus can occur with age, it is not a universal or expected change and may be linked to pathology rather than normal aging.
5. Greater ability to hear high-pitched sounds. Aging decreases the ability to hear high-frequency sounds; it does not improve it.
Take home points:
- Normal aging changes: drier cerumen, auditory nerve degeneration, and tympanic membrane atrophy.
- Presbycusis is linked with difficulty hearing high-pitched sounds.
- Tinnitus may occur with aging but is not considered a normal or universal finding.
Before injecting fluorescein for angiography, it is important for the nurse to (select all that apply)
Explanation
Fluorescein angiography is a diagnostic procedure used to visualize blood vessels in the retina and choroid. Because the injection of fluorescein dye can cause certain expected side effects, the nurse must prepare both the patient and the environment to ensure comfort and safety. Having an emesis basin is important since nausea and vomiting are common after injection. Patients should also be informed that their skin may temporarily turn yellow and urine may appear bright yellow, which are normal and harmless effects of the dye. Topical anesthetics are not required, fatigue is not a contraindication, and fluorescein is not iodine-based, so iodine allergy is not a concern.
Rationale for correct answers:
1. Obtain an emesis basin. Nausea and vomiting are common side effects of fluorescein injection, so being prepared with an emesis basin is important for patient comfort.
4. Inform patient that skin may turn yellow. Temporary yellowing of the skin and bright yellow urine are normal effects of fluorescein and should be explained to prevent unnecessary alarm.
Rationale for incorrect answers:
2. Ask if the patient is fatigued. Fatigue does not affect the safety or effectiveness of fluorescein angiography.
3. Administer a topical anesthetic. Fluorescein is given intravenously, so a topical anesthetic is not needed.
5. Assess for allergies to iodine-based contrast media. Fluorescein does not contain iodine, so iodine allergy is irrelevant.
Take home points:
- Nausea/vomiting and yellow discoloration of skin/urine are common after fluorescein angiography.
- Iodine allergy is not a concern because fluorescein dye is not iodine-based.
- Patient education before the test is essential to reduce anxiety and ensure cooperation.
A client arrives at the emergency department after an insect has entered the ear. Which of the following solutions would the nurse instill into the client’s ear to smother the insect?
Explanation
When an insect enters the ear, the goal is to smother and immobilize it before attempting removal, as movement of the insect can cause severe pain, anxiety, and potential damage to the ear canal or tympanic membrane. Mineral oil or sometimes lidocaine is instilled into the ear to suffocate the insect and allow it to be removed safely. Carbamide peroxide and triethanolamine are cerumenolytics used to soften earwax, while hot water is unsafe and can cause burns or further trauma.
Rationale for correct answer:
3. Mineral oil. Safe and effective in smothering the insect, immobilizing it, and reducing discomfort so it can be removed without injury.
Rationale for incorrect answers:
1. Carbamide peroxide. Used for earwax removal, not effective for insects.
2. Hot water. Unsafe and may burn or damage the ear canal/tympanic membrane.
4. Triethanolamine. Another cerumenolytic, not intended for insect removal.
Take home points:
- Mineral oil or lidocaine is the agent of choice to smother an insect in the ear.
- Do not use hot water or cerumenolytics in this situation.
- The priority is to immobilize the insect before removal to prevent trauma and pain.
For a client with Ménière’s disease, which medication is most appropriate to administer during an acute attack?
Explanation
When an insect enters the ear, the priority is to smother and immobilize it before attempting removal, since movement can worsen pain, anxiety, or damage to the tympanic membrane. Mineral oil or sometimes lidocaine is instilled into the canal to suffocate the insect and make it easier and safer to extract. Cerumenolytics and hot water are not appropriate and may cause additional harm.
Rationale for correct answer:
3. Mineral oil. Mineral oil is the safest and most effective method to immobilize an insect in the ear canal. It suffocates the insect, reduces its movement, and minimizes trauma to the delicate ear structures. This allows for controlled and less painful removal of the foreign body.
Rationale for incorrect answers:
1. Carbamide peroxide. This agent is a cerumenolytic that softens and dissolves earwax. It has no effect on insects and may cause irritation if instilled when a foreign body is present.
2. Hot water. Introducing hot water into the ear canal is dangerous, as it can cause burns and further damage to the tympanic membrane. Additionally, it does not effectively immobilize the insect, making removal more difficult.
4. Triethanolamine. Like carbamide peroxide, triethanolamine is used for cerumen management and has no role in treating an insect in the ear. Using it in this situation may increase discomfort and fails to address the underlying issue.
Take home points:
- Mineral oil or lidocaine are first-line agents to immobilize an insect in the ear.
- Avoid hot water and cerumenolytics, as they can cause harm or are ineffective.
- The main goal is to immobilize the insect before removal to prevent pain and injury.
Which is the best evidence that the antibiotic the nurse is administering for the treatment of acute otitis media is having a therapeutic effect?
Explanation
When treating acute otitis media with antibiotics, the most reliable evidence of therapeutic effect is relief of ear discomfort, since pain is the hallmark symptom of the condition. Symptom relief usually occurs as the infection and inflammation resolve. Other findings, such as drainage or external warmth, are not dependable indicators of treatment effectiveness.
Rationale for correct answer:
- Ear discomfort is relieved. Pain relief directly reflects reduction of infection and inflammation in the middle ear. This is the clearest clinical evidence that antibiotics are working. Improvement in pain typically occurs before other changes, making it the best therapeutic marker.
Rationale for incorrect answers:
2. Ear drainage is thin and watery. Drainage often signals tympanic membrane rupture or ongoing infection rather than improvement, so it is not a positive therapeutic indicator.
3. Ringing sounds within the ear stop. Tinnitus is not a primary feature of acute otitis media and is not a reliable way to evaluate antibiotic effectiveness.
4. The ear feels less warm to the touch. Warmth is not a valid or consistent measure of improvement; resolution of pain is far more clinically significant.
Take home points:
- Pain relief is the best evidence of effective antibiotic therapy in acute otitis media.
- Drainage, tinnitus, or ear warmth are not dependable signs of resolution.
- Monitoring patient-reported symptom relief is key in evaluating treatment success.
The nurse helps the team leader plan interventions to promote effective communication with the client with otosclerosis. Which is the most appropriate nursing order to include in the care plan of this client?
Explanation
In otosclerosis, conductive hearing loss occurs due to abnormal bone growth in the middle ear, which reduces the ability to hear sound vibrations. The most effective communication strategy is to face the client while speaking, as this allows the individual to use lip-reading and visual cues to better understand the message. Other techniques, such as raising pitch or speaking into the ear, are not helpful and may even reduce comprehension.
Rationale for correct answer:
2. Face the client when speaking to him or her. Facing the client promotes better understanding because it enhances the use of lip-reading and facial expressions. This method provides a clear line of sight and optimizes communication without straining the client.
Rationale for incorrect answers:
1. Drop voice at the end of each sentence. Lowering the voice makes speech harder to hear and understand, which further complicates communication for clients with hearing loss.
3. Raise pitch of voice one octave higher. High-pitched sounds are often more difficult for people with hearing impairments to detect, so this strategy is ineffective.
4. Speak directly into the client’s ear. Speaking into the ear can distort sound and is considered disrespectful; it also does not promote visual cues that aid comprehension.
Take home points:
- Always face clients with hearing impairment when speaking.
- Avoid raising voice pitch or dropping sentences, as these reduce clarity.
- Visual cues are as important as verbal sound in promoting effective communication.
What is the organ of balance and equilibrium?
Explanation
The semicircular canals are the primary organ of balance and equilibrium in the inner ear. They detect angular movements of the head through fluid shifts and hair cell stimulation, which send signals to the brain to help maintain posture and coordination. Other structures of the ear, such as the cochlea and Organ of Corti, are essential for hearing but not balance.
Rationale for correct answer:
4. Semicircular canals. These structures contain endolymph and specialized hair cells that detect rotational movements. They work together with the vestibule and vestibular nerve to maintain balance and spatial orientation.
Rationale for incorrect answers:
- Cochlea. The cochlea is the organ of hearing, responsible for converting sound waves into nerve impulses, but it does not play a role in balance.
- Ossicular chain. The ossicles (malleus, incus, stapes) amplify sound vibrations to the inner ear but are not involved in equilibrium.
- Organ of Corti. Located within the cochlea, this structure contains sensory hair cells for hearing, not balance.
Take home points:
- The semicircular canals are responsible for detecting head movements and maintaining equilibrium.
- The cochlea and Organ of Corti are strictly auditory structures.
- The ossicular chain amplifies sound but does not contribute to balance.
How does the eustachian tube assist the auditory system?
Explanation
The eustachian tube plays a vital role in the auditory system by allowing for the equalization of pressure between the middle ear and the external environment. This equalization ensures proper vibration of the tympanic membrane and prevents damage or discomfort from pressure changes, such as during altitude shifts. It also helps with drainage of secretions from the middle ear into the nasopharynx.
Rationale for correct answer:
3. Allows for equalization of pressure in the middle ear. The eustachian tube maintains balance in air pressure on both sides of the tympanic membrane, which is essential for accurate sound conduction and comfort. This function also reduces the risk of barotrauma.
Rationale for incorrect answers:
1. Transmits sound stimuli to the brain. This is the role of the auditory nerve, not the eustachian tube.
2. Sets bones of the middle ear in motion. This function is carried out by the tympanic membrane and ossicles (malleus, incus, stapes).
4. Transmits stimuli from the semicircular canals to the brain. This is performed by the vestibular nerve as part of the balance system, not the eustachian tube.
Take home points:
- The eustachian tube equalizes middle ear pressure with atmospheric pressure.
- It prevents barotrauma and maintains optimal tympanic membrane vibration.
- It does not transmit sound or balance signals—that role belongs to the auditory and vestibular nerves.
Which changes of aging can impair hearing in the older adult? Select all that apply
Explanation
With aging, changes in the auditory system can impair hearing due to alterations in the external, middle, and inner ear structures. In the external ear, cerumen becomes drier and more difficult to expel, and excessive hair growth can obstruct the canal. In the middle ear, atrophy of the tympanic membrane reduces its ability to vibrate effectively. In the inner ear, neuron degeneration within the auditory nerve and central pathways leads to sensorineural hearing loss.
Rationale for correct answers:
1. Atrophy of eardrum (middle ear). Thinning and loss of elasticity in the tympanic membrane decreases its ability to transmit sound vibrations effectively, contributing to conductive hearing changes.
2. Increased hair growth (external ear). Excess hair can trap cerumen and debris, obstructing the external canal and impeding sound conduction.
3. Increased production of and dryness of cerumen (external ear). Dry, hardened cerumen can build up and block the ear canal, which interferes with sound wave transmission.
6. Neuron degeneration in auditory nerve and central pathways (inner ear). This is a hallmark of presbycusis (age-related hearing loss), leading to difficulty distinguishing speech, especially in noisy environments.
Rationale for incorrect answers:
4. Increased vestibular apparatus in semicircular canals. No such change occurs with aging; instead, vestibular function may decline, but the apparatus does not increase.
5. Decreased cochlear efficiency from increased blood supply. Aging is associated with reduced blood supply to the cochlea, not increased. This reduction contributes to sensorineural hearing loss.
Take home points:
- Age-related hearing loss (presbycusis) results from both conductive and sensorineural changes.
- Key changes include tympanic membrane atrophy, cerumen impaction from dryness/hair growth, and auditory nerve degeneration.
- Misconceptions such as increased cochlear blood supply or enlargement of vestibular structures are incorrect.
Exams on Middle and Inner Ear Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Identify the key anatomical structures and functions of the middle and inner ear.
- Describe the pathophysiology, risk factors, and clinical manifestations of common middle and inner ear disorders.
- Differentiate between various ear disorders based on subjective and objective data.
- Explain key diagnostic procedures and the associated nursing actions and client education.
- Formulate a nursing care plan that includes appropriate medications, safety precautions, and patient education for each disorder.
- Recognize common ototoxic medications and implement appropriate nursing
Anatomy And Physiology Of The Ear
The ear is a complex sensory organ divided into three main sections: the outer, middle, and inner ear. While the outer ear collects sound, the middle ear and inner ear are crucial for both hearing and balance. The middle ear is an air-filled cavity containing the three smallest bones in the body, the ossicles (malleus, incus, and stapes), which amplify and transmit sound vibrations from the tympanic membrane to the oval window. The inner ear is a delicate, fluid-filled labyrinth within the temporal bone. It contains the cochlea, responsible for converting sound waves into electrical signals for the brain, and the vestibular system (semicircular canals, saccule, and utricle), which is essential for maintaining balance and equilibrium.
Changes Related to Aging
With age, the tympanic membrane can thicken and lose elasticity, and the movement of the ossicles can become limited. There can also be a loss of sensory "hair" cells in the organ of Corti in the inner ear. These changes contribute to many of the hearing and balance problems seen in older adults.
Middle Ear Disorders
Acute Otitis Media (AOM)
Acute otitis media (AOM) is a common infectious process of the middle ear. It is frequently a complication of a respiratory infection, such as the common cold or influenza. The Eustachian tube, which connects the middle ear to the nasopharynx, becomes obstructed, trapping fluid that can become infected. This is especially common in children due to the shorter, straighter, and more horizontal Eustachian tube.
Risk Factors
- Recurrent colds and otitis media
- Enlarged adenoids
- Trauma to the ear
- Changes in air pressure (e.g., scuba diving, flying)
Clinical Manifestations
- Pain (Otalgia): The most prominent symptom is a sudden, sharp, and severe ear pain, often described as a throbbing sensation.
- Fever and Malaise: Patients may present with a high fever and general feeling of being unwell.
- Hearing Loss: A temporary conductive hearing loss occurs due to the fluid and pressure buildup.
- Tympanic Membrane: On otoscopic examination, the nurse will note a red, bulging, and inflamed tympanic membrane. Fluid and/or bubbles may be visible behind the eardrum. If the eardrum perforates, a purulent or bloody drainage (otorrhea) may be observed.
- Vertigo: Less commonly, patients may experience dizziness or a spinning sensation.
Pathophysiology
The inflammatory response from a respiratory infection causes swelling and obstruction of the Eustachian tube. This prevents air from entering the middle ear, leading to a negative pressure that pulls fluid from the surrounding mucosa into the middle ear space. This fluid provides an ideal medium for the proliferation of bacteria or viruses. The resulting buildup of infected fluid increases pressure on the tympanic membrane, causing significant pain and, if left untreated, can lead to perforation.
Otosclerosis
Otosclerosis is a hereditary disease that involves abnormal bone remodeling in the middle ear. It primarily affects the stapes, causing it to become fixated in the oval window and preventing sound from being transmitted to the inner ear. The disease is more common in women and can be accelerated by pregnancy.
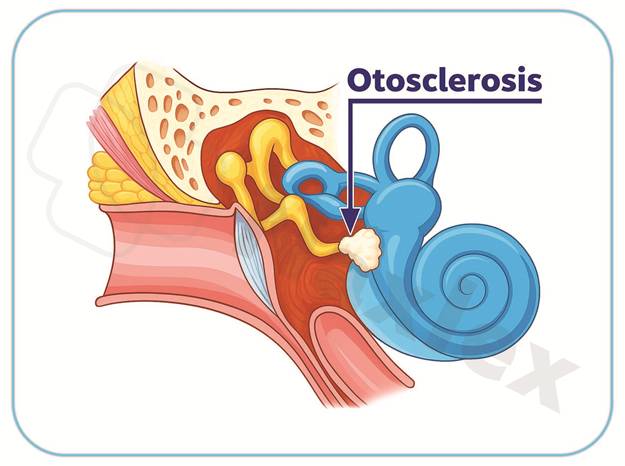
Pathophysiology
The process involves both bone resorption and new, spongy bone formation, creating an otosclerotic lesion. This new bone growth gradually hardens and immobilizes the stapes footplate at its attachment to the oval window. This fixation results in a progressive conductive hearing loss.
Clinical Manifestations
- Progressive Conductive Hearing Loss: The most common symptom. The hearing loss is typically bilateral and asymmetrical. A key finding is paracusis willisii, where the patient hears better in noisy environments because others unconsciously speak louder.
- Tinnitus: A persistent ringing, buzzing, or roaring sound in the ear may be present.
- Dizziness or Balance Issues: While less common, vertigo can occur in advanced cases.
Inner Ear Disorders
Ménière's Disease
Ménière's disease is a chronic and progressive inner ear disorder characterized by a classic triad of symptoms. It is believed to be caused by an excess of endolymphatic fluid, leading to increased pressure within the inner ear labyrinth.
Risk Factors
- Viral or bacterial infection
- Damage due to ototoxic medications
Pathophysiology
The exact etiology is unknown, but it is theorized to be related to either an overproduction or a decreased reabsorption of endolymphatic fluid. This buildup of fluid causes hydrops, or distention of the inner ear. This increased pressure can cause the membranes to rupture, mixing the endolymph with perilymph. The altered fluid composition disrupts the hair cells' function in the cochlea and vestibular system, resulting in the characteristic symptoms.
Clinical Manifestations
- Classic Triad: The hallmarks of Ménière's disease are:
- Episodic Vertigo: A sudden, often debilitating sensation of spinning that can last from minutes to hours. This is the most incapacitating symptom.
- Fluctuating Sensorineural Hearing Loss: Hearing loss in the affected ear that can worsen during an attack and may become permanent over time.
- Tinnitus: A persistent roaring, buzzing, or hissing sound in the affected ear.
- Aural Fullness: Patients often report a feeling of pressure or congestion in the affected ear.
- Nausea and Vomiting: Accompanying the severe vertigo, these can contribute to dehydration and exhaustion.
- Nystagmus: Rapid, involuntary eye movements.
- Alterations in Balance: Due to the inner ear's role in the vestibular system.
Benign Paroxysmal Positional Vertigo (BPPV)
Benign Paroxysmal Positional Vertigo (BPPV) is the most common cause of vertigo. It is caused by the displacement of tiny calcium carbonate crystals, called otoconia, from their normal location in the utricle into one of the semicircular canals.
Pathophysiology
The otoconia are responsible for sensing linear movement. When they become dislodged and float into the semicircular canals, they act as tiny rocks. With specific head movements (e.g., looking up, rolling over in bed), the gravity-dependent movement of these crystals sends an erroneous signal to the brain that the head is spinning.
Clinical Manifestations
- Brief, Sudden Vertigo: The sensation of spinning is intense but brief, typically lasting less than 60 seconds. It is always triggered by a change in head position.
- Nystagmus: Rapid, involuntary eye movements often accompany the vertigo.
- Nausea: Nausea can occur due to the vestibular disturbance.
Acoustic Neuroma (Vestibular Schwannoma)
An acoustic neuroma is a benign, slow-growing tumor that arises from the Schwann cells of the vestibular nerve (cranial nerve VIII). As the tumor enlarges, it compresses the vestibular, cochlear, and eventually, other nearby cranial nerves.
Pathophysiology
The tumor grows slowly, typically over years. As it expands, it exerts pressure on the vestibular nerve, causing balance issues. Because the cochlear nerve is directly adjacent, it is also compressed, leading to hearing loss. In later stages, the tumor can compress the trigeminal nerve (facial sensation) and the facial nerve, causing facial numbness and weakness.
Clinical Manifestations
- Unilateral Sensorineural Hearing Loss: This is a common early symptom and is usually insidious and progressive.
- Tinnitus: A persistent ringing in the affected ear.
- Dizziness and Balance Issues: Unsteadiness and vertigo are common as the tumor presses on the vestibular nerve.
- Facial Numbness/Weakness: As the tumor grows, the patient may experience tingling, numbness, or weakness on one side of the face.
Common Otic Problems
Impacted Cerumen (Ear Wax)
Cerumen (ear wax) is a normal, protective secretion of the ear canal. However, it can become impacted and obstruct the ear canal, causing symptoms.
Pathophysiology
Due to factors like excessive secretion, narrow canals, or improper cleaning (e.g., with cotton swabs), cerumen can become impacted, forming a plug.
Clinical Manifestations
- Feeling of Fullness: A sensation of fullness or pressure in the ear.
- Hearing Loss: A temporary, mild conductive hearing loss.
- Pain: Can be present if the impaction presses on the tympanic membrane.
- Itching or Dizziness: The impacted cerumen can cause an itchy sensation or mild dizziness.
Diagnostic Studies
- Otoscopic Examination: The nurse will visualize a plug of cerumen partially or completely blocking the ear canal.
Collaborative and Nursing Management
- Patient Education: Teach the patient about proper ear hygiene and advise them to avoid using cotton swabs.
- Manual Removal: A trained nurse can remove soft cerumen with an ear curette.
- Irrigation: If the eardrum is intact, a gentle warm water irrigation can be used to flush out the cerumen.
- Cerumenolytic Agents: Ear drops like mineral oil or hydrogen peroxide can be used to soften hard wax before removal.
External Otitis (Swimmer's Ear)
External otitis is an infection or inflammation of the external auditory canal. It is often caused by retained moisture in the ear, which creates a favorable environment for bacterial or fungal growth.
Pathophysiology
Commonly caused by Pseudomonas aeruginosa or Staphylococcus aureus. Moisture in the ear canal, trauma from foreign objects (e.g., cotton swabs), or exposure to contaminated water can break down the skin's natural protective barrier, allowing pathogens to enter and cause inflammation.
Clinical Manifestations
- Pain: The most common symptom is pain, which can be severe and is often worsened by moving the auricle or tragus.
- Swelling: The ear canal may be swollen, red, and tender.
- Drainage: A foul-smelling, purulent, or watery discharge may be present.
- Hearing Loss: A temporary conductive hearing loss can occur if the canal is swollen shut
Diagnostic Procedures
Otoscopy
An otoscope is used to examine the external auditory canal and the tympanic membrane (TM).
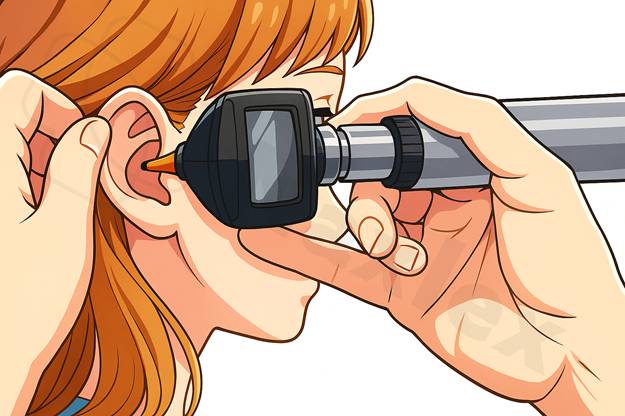
- Nursing Actions:
- For adults, pull the auricle up and back to straighten the ear canal.
- For children, pull the auricle down and back.
- Note the TM should be a pearly gray color and intact.
- The light reflex should be visible from the center of the TM anteriorly (5 o'clock for the right ear, 7 o'clock for the left ear).
- In the presence of infection, the TM becomes inflamed and may bulge, displacing the light reflex.
- Avoid touching the lining of the ear canal, as it is very sensitive.
- Client Education: Inform the client that a firm pull on the ear may be needed to visualize the eardrum.
Tympanometry
This test measures the mobility of the TM and middle ear structures, helping to diagnose middle ear disorders.
Electronystagmography (ENG)
ENG determines the type of nystagmus (involuntary eye movement) by stimulating the acoustic nerve.
- Nursing Actions:
- During the procedure, ask the client simple questions to ensure they remain alert.
- After the procedure, keep the client on bed rest and NPO until vertigo subsides.
- Client Education:
- The client must fast and restrict caffeine, alcohol, sedatives, and antihistamines 24 hours before the test.
- This test is not performed on clients with a pacemaker.
Caloric Testing
This can be done with or concurrently with ENG. Water (warmer or cooler than body temperature) is instilled in the ear to induce nystagmus. The eye's response is diagnostic of vestibular disorders. The same client preparation and restrictions for ENG apply.
Management
General Nursing Care
-
Monitor functional ability and balance. Implement fall risk precautions as needed.
- Evaluate the client's home environment for safety and fall risks.
- Encourage the client to rise slowly and use assistive devices as needed.
- Check the hearing of clients on ototoxic medications for more than 5 days. These include:
- Antibiotics (e.g., gentamicin, amikacin)
- Diuretics (e.g., furosemide)
- NSAIDs (e.g., aspirin, ibuprofen)
- Chemotherapeutic agents (e.g., cisplatin)
- Administer antivertigo and antiemetic medications as needed.
Medications
-
Meclizine (Antivert): An antihistamine with anticholinergic effects used to treat vertigo.
- Nursing Considerations: Observe for sedation. Restrict use in clients with closed-angle glaucoma.
- Antiemetics: Used to treat nausea and vomiting associated with vertigo.
- Nursing Considerations: Observe for postural hypotension and tachycardia.
- Diphenhydramine (Benadryl) and Dimenhydrinate (Dramamine): Antihistamines that treat vertigo and nausea.
- Nursing Considerations: Observe for urinary retention and sedation.
- Scopolamine (Transderm Scop): An anticholinergic that treats nausea.
- Nursing Considerations: Observe for urinary retention and sedation. Contraindicated in clients with angle-closure glaucoma.
- Diazepam (Valium): A benzodiazepine with antivertigo effects.
- Nursing Considerations: Observe for sedation. Restrict use in clients with closed-angle glaucoma. Use the smallest effective dose for older adults to prevent oversedation.
Vertigo-Reducing Activities and Client Education
-
Avoid caffeine and alcohol.
- Rest in a quiet, darkened room when vertigo is severe.
- Use assistive devices (cane, walker) for safe ambulation.
- Maintain a safe, clutter-free environment.
- Take a diuretic if prescribed to decrease fluid in the semicircular canals.
- Decrease intake of salt and sodium-containing foods (e.g., processed meats, MSG).
Surgical Interventions
Stapedectomy
A surgical procedure where the stapes is removed and replaced with a prosthesis to treat otosclerosis.
- Nursing Actions: Assess the client for facial nerve damage and manage postoperative vertigo, nausea, and vomiting.
- Client Education: Hearing may initially be worse but will improve. Avoid straining, coughing, sneezing with a closed mouth, and air travel. Keep the ear covered when washing hair and prevent water from entering the ear.
Labyrinthectomy
A surgical treatment for vertigo that involves the removal of the labyrinthine portion of the inner ear.
- Nursing Actions: The client will have severe nausea and vertigo postoperatively. Take safety precautions and administer antiemetics.
- Client Education: Inform the client that hearing loss is to be expected in the affected ear.
Cochlear Implant
An electronic device for clients with sensorineural hearing loss. It consists of an external microphone and processor that send electrical impulses to a receiver and electrodes attached to the auditory nerve.
- Nursing Actions: Follow standard pre-, intra-, and postoperative surgery guidelines.
- Client Education: The unit is not turned on immediately after surgery. Two to six weeks later, the external unit is applied and programmed. Instruct the client on infection prevention and the need to avoid MRIs.
Summary
- The middle and inner ears are essential for hearing and balance but are vulnerable to various disorders.
- Middle ear disorders (e.g., Acute Otitis Media, Serous Otitis Media) are often inflammatory, leading to pain and conductive hearing loss.
- Inner ear disorders (e.g., Ménière’s disease, BPPV) are primarily associated with tinnitus, sensorineural hearing loss, and vertigo.
- A key nursing role involves educating patients on managing symptoms, preventing complications, and ensuring safety, especially for those with balance issues.
- Diagnostic procedures and appropriate medication administration are crucial for effective treatment.
- Surgical interventions (e.g., stapedectomy, cochlear implants) may provide definitive management and require careful preoperative and postoperative nursing care.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Middle and Inner Ear Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


