Please set your exam date
Parkinson’s Disease
Study Questions
Practice Exercise 1
The classic triad of manifestations associated with Parkinson’s disease is tremor, rigidity, and bradykinesia. What is a consequence related to rigidity?
Explanation
Parkinson’s disease is a neurodegenerative disorder characterized by the classic triad of tremor, rigidity, and bradykinesia. Each of these symptoms contributes to distinct physical impairments that affect mobility, coordination, and quality of life. Rigidity refers to increased muscle tone that results in resistance to movement and leads to various muscular symptoms. One of the most common consequences of rigidity is muscle soreness and pain.
Rationale for correct answer:
D. Muscle soreness and pain: Muscle rigidity causes sustained contraction of muscles, leading to discomfort and pain. This is a direct effect of the increased muscle tone that characterizes rigidity in Parkinson’s disease.
Rationale for incorrect answers:
A. Shuffling gait: This is a result of bradykinesia, which causes slowness of movement and difficulty initiating steps. It is not directly caused by rigidity.
B. Impaired handwriting: This is known as micrographia and is linked to bradykinesia affecting fine motor control. Rigidity is not the primary cause of this symptom.
C. Lack of postural stability: Postural instability arises from impaired balance and reflexes. It is not a consequence of rigidity but of other motor deficits in Parkinson’s disease.
Take home points
- Rigidity causes muscle tightness, soreness, and pain in clients with Parkinson’s disease.
- Bradykinesia and postural instability contribute to gait changes, micrographia, and balance difficulties.
- Understanding the source of each symptom helps guide patient education and symptom management.
Which of the following clinical manifestations is most characteristic of early-stage Parkinson’s disease?
Explanation
Parkinson’s disease typically begins with subtle motor symptoms that gradually worsen over time. One of the most characteristic early signs is a resting tremor, often starting on one side of the body, particularly in one hand. This tremor may be described as a “pill-rolling” movement of the fingers and is most noticeable when the limb is at rest. Early identification of these signs can support prompt diagnosis and treatment.
Rationale for correct answer:
B. Resting tremor of one hand: A unilateral resting tremor is one of the earliest and most recognizable signs of Parkinson’s disease. It typically starts on one side and progresses gradually to involve other areas.
Rationale for incorrect answers:
A. Severe muscle atrophy: Muscle atrophy is not an early feature of Parkinson’s disease. It may occur later due to inactivity but is not a primary manifestation of the disease.
C. Complete loss of facial expression: Reduced facial expression, known as hypomimia, can occur in later stages. However, a complete loss is not typical in the early phase.
D. Bilateral rigidity of all extremities: Rigidity generally begins unilaterally, like tremor, and progresses over time. Bilateral involvement of all extremities is more common in advanced stages.
Take home points
- Resting tremor, especially of one hand, is a hallmark of early-stage Parkinson’s disease.
- Muscle atrophy and bilateral rigidity are more likely in later stages due to disease progression.
- Recognizing early motor signs can facilitate earlier diagnosis and management.
A nurse is assessing a client with suspected Parkinson’s disease. Which of the following signs would the nurse expect to find? Select all that apply
Explanation
Parkinson’s disease presents with progressive motor symptoms due to dopaminergic neuron degeneration in the brain. The hallmark signs include resting tremor, rigidity, bradykinesia, and postural instability. During physical assessment, the nurse should look for features such as a pill-rolling tremor, cogwheel rigidity, and a shuffling gait, which are classic indicators of the disease. These signs help distinguish Parkinson’s from other neurological conditions like cerebellar disorders.
Rationale for correct answers:
A. Pill-rolling tremor: This resting tremor, typically seen in the hands, is one of the earliest and most recognizable symptoms of Parkinson’s disease. It appears as rhythmic movement of the thumb and fingers, as if rolling a pill.
C. Cogwheel rigidity: This type of rigidity presents as a ratchety resistance during passive movement of limbs. It reflects both muscle stiffness and tremor, hallmark features of Parkinson’s disease.
D. Shuffling gait: Parkinson’s disease often causes a distinctive walk with short, hesitant steps and reduced arm swing. This gait disturbance is associated with bradykinesia and postural instability.
Rationale for incorrect answers:
B. Hyperreflexia: Hyperreflexia is more characteristic of upper motor neuron lesions, not Parkinson’s disease. Clients with Parkinson’s typically have normal or reduced reflexes.
E. Intention tremor: Intention tremors occur during purposeful movement and are associated with cerebellar disorders. Parkinson’s tremors occur at rest and usually diminish with voluntary activity.
Take home points
- Classic signs of Parkinson’s disease include pill-rolling tremor, cogwheel rigidity, and shuffling gait.
- Hyperreflexia and intention tremor are not typical findings in Parkinson’s and suggest alternative diagnoses.
- Accurate assessment of motor symptoms is essential for early diagnosis and effective management.
Practice Exercise 2
Which of the following findings is most commonly used to support the clinical diagnosis of Parkinson’s disease?
Explanation
Parkinson’s disease is a clinical diagnosis, meaning it is based on the presence of key motor symptoms rather than lab or imaging findings. The combination of resting tremor, cogwheel rigidity, and bradykinesia forms the classic triad used by clinicians to identify the condition. These signs are typically observed during physical examination. While imaging and lab tests may help rule out other causes, they do not confirm Parkinson’s disease.
Rationale for correct answer:
A. Presence of tremor at rest, cogwheel rigidity, and bradykinesia: These hallmark motor symptoms are essential for diagnosing Parkinson’s disease. The diagnosis is primarily based on clinical observation of these features over time.
Rationale for incorrect answers:
B. Abnormal findings on brain MRI: Brain imaging is usually normal in Parkinson’s disease. MRI is primarily used to exclude other neurological conditions, not to confirm this diagnosis.
C. Elevated serum dopamine levels: There is no reliable blood test for dopamine levels that supports diagnosis. In fact, dopamine levels are decreased in the brain, not elevated in the serum.
D. Positive family history and recent infection: While genetic factors may increase risk, a positive family history and infection are not diagnostic criteria. Parkinson’s disease is rarely triggered directly by infection.
Take home points
- Diagnosis of Parkinson’s disease is based on clinical signs, especially resting tremor, cogwheel rigidity, and bradykinesia.
- MRI and lab tests are used to rule out other conditions, not confirm Parkinson’s.
- No specific blood test or imaging definitively diagnoses the disease—clinical evaluation is key.
A newly diagnosed patient with Parkinson’s disease is started on carbidopa-levodopa. What should the nurse include in the teaching about this medication?
Explanation
Carbidopa-levodopa is a cornerstone medication in the treatment of Parkinson’s disease and works by replenishing dopamine levels in the brain. While it is effective, it can cause side effects, including orthostatic hypotension, which increases the risk of falls. Nurses should educate clients to change positions slowly to prevent dizziness or fainting. Proper medication education helps reduce complications and supports long-term adherence.
Rationale for correct answer:
C. "Change positions slowly to reduce the risk of dizziness.": Carbidopa-levodopa commonly causes orthostatic hypotension, especially when starting treatment. Teaching clients to rise slowly helps reduce fall risk and improves safety.
Rationale for incorrect answers:
A. "Take the medication on a full stomach to increase absorption.": Taking carbidopa-levodopa with high-protein meals can impair absorption. It is usually recommended to take it on an empty stomach or with a small snack if nausea occurs.
B. "You may notice improvement immediately after the first dose.": Therapeutic effects may take days or weeks to become noticeable. Immediate improvement after the first dose is unlikely.
D. "Stop the drug if involuntary movements improve suddenly.": The medication should never be stopped abruptly without consulting a provider. Sudden withdrawal can lead to severe side effects, including neuroleptic malignant-like syndrome.
Take home points
- Carbidopa-levodopa may cause orthostatic hypotension—clients should be advised to rise slowly.
- Avoid taking the medication with high-protein meals, which may impair absorption.
- Do not stop the medication suddenly, and therapeutic effects often take time to appear.
Which of the following is the most appropriate intervention to help manage bradykinesia in a client with Parkinson’s disease?
Explanation
Bradykinesia is a core feature of Parkinson’s disease and refers to slowness in initiating and executing movement. It can make starting voluntary movements like walking or standing very difficult. One effective strategy is to encourage rhythmic or repetitive motions, such as rocking side to side, to help initiate movement. This technique can improve mobility and reduce the risk of falls.
Rationale for correct answer:
B. Encourage rocking side to side before standing: Rhythmic movements help overcome freezing episodes and assist in initiating motion. This technique improves momentum and supports safer transfers.
Rationale for incorrect answers:
A. Use an alternating air pressure mattress: This intervention is for pressure ulcer prevention and has no effect on bradykinesia. It does not support movement initiation or motor control.
C. Offer frequent snacks between meals: While important for maintaining nutrition, this does not address the motor symptoms of Parkinson’s. It is not an intervention for bradykinesia.
D. Apply heat packs to the legs before walking: Heat may provide muscle relaxation but does not directly improve bradykinesia or facilitate movement. It is not a primary intervention for mobility challenges in Parkinson’s disease.
Take home points
- Bradykinesia causes slowness of movement and can be addressed with rhythmic strategies like rocking side to side.
- Interventions should focus on mobility facilitation, not just comfort or skin care.
- Safe movement techniques help reduce the risk of falls and freezing episodes.
Practice Exercise 3
A 65-year-old woman was just diagnosed with Parkinson’s disease. The priority nursing intervention is:
Explanation
Parkinson’s disease is a progressive neurological disorder that increases the risk of falls due to gait disturbances, postural instability, and bradykinesia. In newly diagnosed clients, the nurse’s priority intervention should focus on ensuring home safety to prevent injury. This includes assessing the environment for fall hazards and promoting safety adaptations. Addressing safety needs early helps protect the client’s independence and well-being.
Rationale for correct answer:
B. Evaluating the home for environmental safety: Clients with Parkinson’s are at increased risk for falls due to impaired balance and movement. Assessing and modifying the home environment is essential to prevent injuries and promote safe mobility.
Rationale for incorrect answers:
A. Searching the Internet for educational videos: While education is important, it is not the priority at the time of diagnosis. Immediate focus should be on safety and risk prevention.
C. Promoting physical exercise and a well-balanced diet: These are essential for long-term management but are not the most urgent concern at the initial stage. Safety comes first to prevent injury while physical routines are established.
D. Designing an exercise program to strengthen and stretch specific muscles: This is more appropriate after an initial assessment and once the client is stabilized. Early interventions should prioritize environmental and safety needs.
Take home points
- Safety assessment is the priority in early Parkinson’s care due to fall risk.
- Other interventions like education and exercise are important but follow safety evaluation.
- Nurses should assess for environmental hazards and support home modifications to enhance independence.
A nurse is teaching a client newly diagnosed with Parkinson’s disease about management and treatment options. Which of the following statements should the nurse include? Select all that apply
Explanation
Parkinson’s disease (PD) is a chronic, progressive neurological disorder that affects movement, typically treated with a combination of pharmacologic, surgical, and rehabilitative strategies. Management aims to control motor symptoms, maintain function, and enhance quality of life. Medications like levodopa are mainstays of treatment, while supportive therapies such as physical and occupational therapy can improve daily function. In advanced cases, surgical interventions may be considered.
Rationale for correct answers:
A. Levodopa can help improve movement by replenishing dopamine in the brain: Levodopa is the gold-standard medication that converts to dopamine in the brain, helping reduce motor symptoms.
C. Occupational therapy may help with tasks such as dressing or feeding: OT assists patients in maintaining independence with ADLs despite tremors or rigidity.
E. Deep brain stimulation may be considered if medications are not effective: This surgical treatment can reduce motor complications when pharmacologic management is insufficient.
Rationale for incorrect answers:
B. "You should avoid all physical activity to reduce fatigue": Physical activity is encouraged in PD to maintain mobility and muscle strength.
D. "A high-protein meal will improve your medication's absorption": High-protein meals can interfere with levodopa absorption and should be timed carefully.
Take home points
- Levodopa is the cornerstone of Parkinson’s treatment.
- Therapies such as physical and occupational therapy are vital.
- Deep brain stimulation is a viable option for patients with advanced symptoms.
A client with Parkinson’s disease is prescribed carbidopa-levodopa. Which instruction should the nurse include in the medication teaching?
Explanation
Carbidopa-levodopa is a combination medication commonly prescribed to treat motor symptoms of Parkinson’s disease. It works by increasing the amount of dopamine available in the brain. However, long-term use may result in motor complications such as dyskinesias or wearing-off effects. Patient education is essential to ensure safe administration and early recognition of adverse effects.
Rationale for correct answer:
B. Report any uncontrolled movements of the face, eyelids, or limbs: These may indicate dyskinesias, a common side effect of long-term levodopa use, requiring dosage adjustment.
Rationale for incorrect answers:
A. Avoid driving for 2 hours after each dose due to sedation: Sedation is not a typical or predictable effect; driving precautions are based on individual response.
C. Stop taking the medication if symptoms improve significantly: Stopping levodopa abruptly can worsen symptoms and cause serious side effects.
D. Take this medication only at bedtime to prevent daytime drowsiness: It should be taken regularly during the day to control symptoms, not limited to bedtime.
Take home points
- Educate clients on timing, effects, and side effects of carbidopa-levodopa.
- Monitor for dyskinesias and wearing-off effects.
- Never abruptly stop dopaminergic medications without medical supervision.
Comprehensive Questions
A patient with a tremor is being evaluated for Parkinson’s disease. The nurse explains to the patient that Parkinson’s disease can be confirmed by:
Explanation
Parkinson’s disease is primarily a clinical diagnosis, as there are no definitive laboratory or imaging tests that confirm it. One of the most reliable indicators is a positive response to dopaminergic therapy, particularly to levodopa, which supports the diagnosis. Improvement in symptoms such as tremor, rigidity, and bradykinesia following treatment is considered diagnostic evidence. This therapeutic response helps distinguish Parkinson’s from other movement disorders.
Rationale for correct answer:
B. Relief of symptoms with administration of dopaminergic agents: A noticeable improvement in motor symptoms after starting levodopa therapy supports the diagnosis of Parkinson’s disease. This clinical response is often used as confirmation when diagnostic uncertainty exists.
Rationale for incorrect answers:
A. CT and MRI scans: Imaging studies are typically normal in Parkinson’s and are used only to rule out other causes. They do not confirm the diagnosis.
C. The presence of tremors that increase during voluntary movement: This describes an intention tremor, which is more characteristic of cerebellar disorders, not Parkinson’s. Parkinson’s tremors occur at rest and decrease with voluntary motion.
D. Cerebral angiogram that reveals the presence of cerebral atherosclerosis: A cerebral angiogram assesses blood vessels, not neurodegenerative changes. It is not used to diagnose Parkinson’s disease.
Take home points
- Parkinson’s disease is confirmed by clinical symptoms and response to dopaminergic medication.
- Levodopa responsiveness strongly supports the diagnosis.
- Imaging and angiograms may rule out other conditions but do not confirm Parkinson’s.
- Resting tremor, not intention tremor, is typical of Parkinson’s disease.
Which observation of the patient made by the nurse is most indicative of Parkinson’s disease?
Explanation
Parkinson’s disease is a neurodegenerative disorder that primarily affects motor function, leading to bradykinesia, rigidity, and postural instability. One of the most characteristic early signs is difficulty initiating movement, especially from a seated position or when starting to walk. This phenomenon, sometimes called "freezing", reflects the hallmark slowness and impaired coordination of voluntary movements. Recognizing this early can aid in timely diagnosis and intervention.
Rationale for correct answer:
C. Difficulty rising from a chair and beginning to walk: This is a classic sign of bradykinesia, one of the core motor symptoms of Parkinson’s disease. Clients often struggle with movement initiation due to reduced dopamine activity in the basal ganglia.
Rationale for incorrect answers:
A. Large, embellished handwriting: Parkinson’s typically causes micrographia, or abnormally small, cramped handwriting. Large, decorative writing is not characteristic of the disease.
B. Weakness of one leg resulting in a limping walk: Parkinson’s does not usually cause true muscle weakness; gait changes are due to bradykinesia and rigidity rather than unilateral weakness.
D. Onset of muscle spasms occurring with voluntary movement: This description is more consistent with spasticity or dystonia, not Parkinson’s. Muscle rigidity in Parkinson’s is usually continuous and not limited to voluntary motion.
Take home points
- Bradykinesia leads to difficulty initiating movement, such as rising from a chair.
- Micrographia, not large handwriting, is a common symptom.
- Gait changes in Parkinson’s are related to rigidity and bradykinesia, not muscle weakness.
- Early recognition of motor symptoms helps guide timely diagnosis and treatment.
A patient with Parkinson’s disease is started on levodopa. What should the nurse explain about this drug?
Explanation
Levodopa is the most effective medication for managing Parkinson’s disease symptoms, particularly bradykinesia and rigidity. It works by serving as a dopamine precursor, which crosses the blood-brain barrier and is then converted to dopamine within the brain. This helps restore dopaminergic activity in areas of the brain that are affected by neuronal loss. Nurses must provide accurate medication education to improve understanding and promote adherence.
Rationale for correct answer:
C. It is a precursor of dopamine that is converted to dopamine in the brain: Levodopa is taken up by neurons and enzymatically converted into dopamine to replenish deficient levels. This directly improves motor symptoms in Parkinson’s disease.
Rationale for incorrect answers:
A. It stimulates dopamine receptors in the basal ganglia: This describes the action of dopamine agonists, not levodopa. Levodopa requires conversion into dopamine before exerting its effects.
B. It promotes the release of dopamine from brain neurons: Levodopa increases dopamine by being converted into it, not by causing release from existing stores. Parkinson’s involves loss of dopamine-producing neurons, limiting natural release.
D. It prevents the excessive breakdown of dopamine in the peripheral tissues: This is the role of carbidopa, which is often combined with levodopa. Carbidopa allows more levodopa to reach the brain by preventing premature breakdown.
Take home points
- Levodopa is converted to dopamine in the brain and directly replenishes dopamine levels.
- It is usually combined with carbidopa to enhance effectiveness and reduce side effects.
- Understanding how the drug works supports patient education and medication adherence.
To reduce the risk for falls in the patient with Parkinson’s disease, what should the nurse teach the patient to do?
Explanation
Parkinson’s disease is associated with bradykinesia, rigidity, and a shuffling gait, which increase the risk of falls. One effective strategy to improve gait safety is to teach the client to consciously lift the toes when stepping, which helps prevent tripping and improves step clearance. This technique helps counteract the typical dragging of the feet seen in Parkinson’s. Reinforcing safe walking practices is an essential part of fall prevention in these clients.
Rationale for correct answer:
C. Consciously lift the toes when stepping: Parkinson’s patients often have a shuffling gait and reduced foot clearance, increasing fall risk. Intentionally lifting the toes promotes safer ambulation and reduces the chance of tripping.
Rationale for incorrect answers:
A. Use an elevated toilet seat: While helpful for ease of transfers, it does not directly reduce fall risk during walking. It is more related to comfort and mobility at rest.
B. Use a walker or cane for support: Assistive devices can help, but correct gait mechanics—like lifting the toes—are still essential. Devices alone are not sufficient without proper walking technique.
D. Rock side to side to initiate leg movements: This technique helps with freezing of gait, but it is not primarily for fall prevention during regular walking. It is used to overcome hesitation in movement, not to address toe dragging.
Take home points
- Toe dragging contributes to falls in Parkinson’s disease.
- Teaching patients to consciously lift their toes helps improve gait safety.
- Fall prevention requires a combination of safe techniques and assistive devices, with proper gait training as a foundation.
To ensure the safety of a client with Parkinson’s disease using a wheeled walker, it is best for the nurse to remind the client to do which of the following?
Explanation
Clients with Parkinson’s disease are at high risk for falls due to stooped posture, bradykinesia, and impaired balance. Teaching clients to stand straight with the head up improves posture, visual orientation, and center of gravity, all of which help maintain safe mobility. This intervention enhances walker use effectiveness and reduces the risk of tripping or falling forward. It also helps counteract the characteristic forward-flexed stance seen in Parkinson’s.
Rationale for correct answer:
D. Stand straight with the head up: Good posture improves balance and visibility of the walking path. It helps align the body properly for safer and more effective walker use.
Rationale for incorrect answers:
A. Maintain a constant pace of walking: Clients with Parkinson’s often experience freezing or shuffling, making consistent pacing difficult. Emphasizing posture is more effective for preventing falls.
B. Keep the walker a full arm’s length in front: This places the walker too far ahead and increases fall risk. The walker should remain close enough to provide stable support.
C. Pick up the walker when taking a step: Wheeled walkers are designed to glide; lifting them can destabilize the client. This can lead to imbalance and a greater risk of falling.
Take home points
- Clients with Parkinson’s disease should be reminded to maintain an upright posture and look ahead when walking.
- Proper posture improves balance and makes walker use safer and more effective.
- Walkers should be used as designed—close to the body and not lifted during steps.
A client with Parkinson’s disease has difficulty swallowing. To promote adequate nutrition and reduce the risk for aspiration, which of the following nursing measures are appropriate? Select all that apply
Explanation
Clients with Parkinson’s disease often experience dysphagia, or difficulty swallowing, due to impaired muscle coordination and bradykinesia affecting the throat and esophageal muscles. This increases the risk for aspiration, choking, and inadequate nutritional intake. Nursing interventions should focus on promoting safe swallowing techniques, proper positioning, and modified diets to reduce complications. Providing adequate time for meals also allows for safer and more effective eating.
Rationale for correct answers:
A. Modify the texture and consistency of food: Soft or thickened foods are easier to control and swallow, reducing the risk of choking or aspiration. Texture modification is a standard dysphagia intervention.
B. Have the client flex the chin when swallowing: The chin-tuck maneuver helps close the airway during swallowing and directs food safely into the esophagus. It is an effective technique for preventing aspiration.
D. Position the client in a sitting position: Upright positioning during meals uses gravity to assist in swallowing and reduces the chance of aspiration. It is a key safety measure for clients with dysphagia.
E. Allow ample time for consuming meals: Bradykinesia slows the eating process, so rushing increases risk. Providing extra time allows for careful, deliberate swallowing.
Rationale for incorrect answer:
C. Encourage frequent sips of liquid while eating: Thin liquids are often more difficult to control and can increase aspiration risk. Liquids should be thickened if needed, as determined by a swallowing evaluation.
Take home points
- Dysphagia in Parkinson’s increases risk for aspiration and malnutrition.
- Use texture-modified diets, chin-tuck, upright positioning, and allow sufficient time for meals.
- Avoid thin liquids unless cleared by a speech-language pathologist.
- Safe feeding practices help preserve nutrition, hydration, and client safety.
A nurse is assessing a client for manifestations of Parkinson’s disease. Which of the following are expected findings? Select all that apply
Explanation
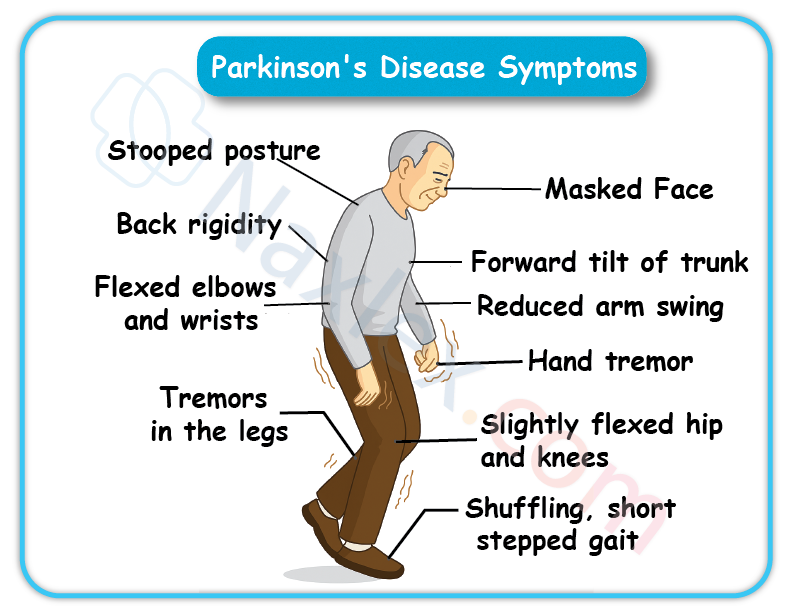
Parkinson’s disease is a progressive neurodegenerative disorder that affects motor function due to the loss of dopaminergic neurons in the brain. Common symptoms include resting tremors, muscle rigidity, bradykinesia, and postural instability. Patients often show a shuffling gait, masked facial expressions, and autonomic symptoms such as drooling. Recognizing these classic manifestations aids early diagnosis and supports effective nursing care.
Rationale for correct answers:
B. Pill-rolling tremor of the fingers: This is a hallmark sign of Parkinson’s and typically begins unilaterally at rest. It reflects the disease’s effect on fine motor control.
C. Shuffling gait: Patients walk with small, hesitant steps due to bradykinesia and muscle rigidity. This increases the risk of falls and is commonly seen in later stages.
D. Drooling: Impaired swallowing and reduced automatic movements contribute to drooling. It is a result of autonomic dysfunction and bradykinesia.
F. Lack of facial expressions: Also known as "masked facies," this results from rigidity and bradykinesia of facial muscles. It leads to reduced expressiveness and is a common symptom.
Rationale for incorrect answers:
A. Decreased vision: Parkinson’s may affect eye movement but does not typically cause vision loss. Vision changes are not core symptoms of the disease.
E. Bilateral ankle edema: Edema is not a direct manifestation of Parkinson’s. It may be related to immobility or medications but is not diagnostic.
Take home points
- Classic signs of Parkinson’s include resting tremor, shuffling gait, drooling, and masked facies.
- Symptoms result from dopamine deficiency affecting motor control and autonomic function.
- Early recognition of these symptoms supports prompt diagnosis and symptom management.
A nurse is caring for a client who has Parkinson’s disease and displays signs of bradykinesia. Which of the following is an appropriate action by the nurse?
Explanation
Bradykinesia, a hallmark symptom of Parkinson’s disease, refers to the slowness of movement and affects both physical and verbal responses. Clients often require additional time to complete tasks, including speaking, due to impaired motor planning and execution.
Allowing extra time promotes accurate communication and supports the client’s autonomy and dignity. It also helps reduce frustration and allows the nurse to more accurately assess the client’s abilities.
Rationale for correct answer:
A. Allow client extra time for verbal responses to questions: Bradykinesia slows down the ability to initiate and execute verbal responses. Giving more time respects the client’s cognitive integrity while accommodating motor delays.
Rationale for incorrect answers:
B. Complete passive range-of-motion exercises: This is more appropriate for preventing contractures in immobile clients, not specifically for addressing bradykinesia. Bradykinesia requires supportive pacing, not passive exercises alone.
C. Provide an alternate form of communication: This may be necessary in cases of speech loss or advanced disease, but is not the most appropriate first response to bradykinesia. Clients with bradykinesia can still communicate, just more slowly.
D. Assist with hygiene as needed: While important in overall care, this action does not directly address the communication difficulties caused by bradykinesia.
Take home points
- Bradykinesia causes slowness of both movement and speech.
- Nurses should allow extra time for clients to respond to promote effective communication and patient dignity.
- Supportive pacing is more appropriate than immediately replacing or bypassing the client’s own efforts.
Exams on Parkinson’s Disease
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Definition And Overview
- Etiology
- Pathophysiology Of Parkinson’s Disease
- Clinical Manifestations
- Practice Exercise 1
- Diagnostic Process And Evaluation
- Practice Exercise 2
- Nursing Care Plan
- Complications And Prognosis
- Patient And Family Education And Support
- Practice Exercise 3
- Summary
- Comprehensive Questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define Parkinson’s disease and describe its underlying pathophysiology, including the role of dopamine and basal ganglia dysfunction.
- Identify the cardinal motor symptoms of Parkinson’s disease: bradykinesia, resting tremor, rigidity, and postural instability.
- Describe common non-motor symptoms of Parkinson’s disease, including cognitive changes, mood disturbances, sleep disorders, and autonomic dysfunction.
- List the risk factors for developing Parkinson’s disease, including age, sex, environmental exposures, and genetic predisposition.
- Explain the clinical diagnosis process, including history-taking, physical exam findings, and the role of response to dopaminergic therapy.
- Differentiate Parkinson’s disease from similar disorders, such as essential tremor, Parkinson-plus syndromes, and normal pressure hydrocephalus.
- Outline pharmacologic treatment options, including levodopa-carbidopa, dopamine agonists, MAO-B inhibitors, and their side effects.
- Describe non-pharmacologic management strategies, including physical therapy, occupational therapy, nutrition, and patient/family education.
Definition And Overview
Parkinson's disease (PD) is a progressive neurodegenerative disorder characterized by bradykinesia (slow movement) and at least one of the following: resting tremor or rigidity. Non-motor symptoms like loss of smell, sleep issues (e.g., REM behavior disorder), depression, drooling, and constipation often precede motor symptoms. Pathologically, PD involves the loss of dopamine-producing neurons in the substantia nigra and the presence of Lewy bodies (abnormal alpha-synuclein protein aggregates). This broad symptom profile highlights PD as a complex systemic disorder.
Etiology
Most PD cases are idiopathic, resulting from a complex interplay of genetics and environment.
Genetic Factors:
- GBA (GBA1): Most common (5-10% of PD); a risk factor, not causative. Associated with earlier onset, faster dementia progression, greater motor difficulties.
- PRKN (Parkin): Most common cause of young-onset PD (<50). Associated with early bradykinesia/rigidity, less dementia, good levodopa response.
- PINK1: Associated with early bradykinesia/rigidity, less non-motor symptoms, slow progression, good levodopa response.
Environmental Risk Factors:
- Pesticides/Herbicides (e.g., paraquat, rotenone).
- Solvents (e.g., trichloroethylene).
- Polychlorinated Biphenyls (PCBs).
- MPTP (synthetic neurotoxin).
- Heavy Metals (e.g., manganese, lead).
- Head Injury (with altered consciousness).
Protective Factors:
- Caffeine consumption.
- Higher uric acid levels.
- Regular NSAID use.
- Cigarette smoking.
- Statin use.
- Higher Vitamin D levels.
- Increased physical activity earlier in life.
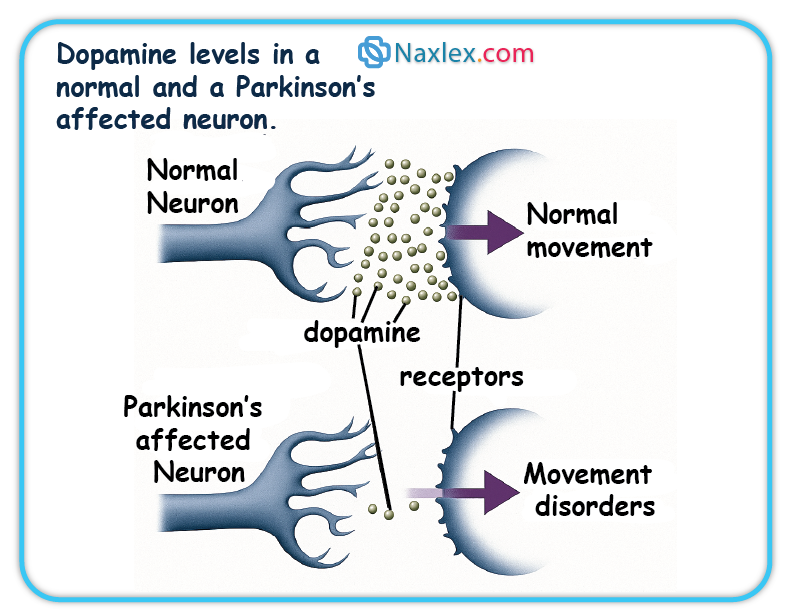
Pathophysiology Of Parkinson’s Disease
Neurotransmitter Imbalance
PD's core mechanism is the progressive death of dopamine-producing neurons in the substantia nigra. This dopamine deficiency impairs nerve cell communication, leading to motor symptoms. The brain may compensate with high glutamate levels. Treatment aims to restore dopamine activity.
 Alpha-Synuclein Aggregation and Lewy Bodies
Alpha-Synuclein Aggregation and Lewy Bodies
Lewy bodies (LB) and Lewy neurites (LN) are abnormal protein aggregates in neurons, primarily composed of misfolded alpha-synuclein. These misfolded proteins aggregate into filaments, forming LBs, which disrupt cell function and contribute to neuronal death. Early oligomeric forms of alpha-synuclein are thought to be most neurotoxic. LBs are found in various brain regions, correlating with both motor and non-motor symptoms.
Basal Ganglia Dysfunction
PD is a disorder of the basal ganglia, brain nuclei vital for movement control. Loss of dopaminergic neurons in the substantia nigra reduces dopamine in the striatum, disrupting basal ganglia circuitry. This imbalance leads to overactivity in some pathways and underactivity in others, causing bradykinesia, rigidity, and tremor.
Clinical Manifestations
PD symptoms are motor and non-motor, often starting insidiously and asymmetrically.
Motor Symptoms (TRAP)
- Tremor: Often initial, resting tremor (e.g., "pill-rolling"), diminishes with action.
- Rigidity: Increased muscle stiffness, resistance to passive movement ("lead pipe" or "cogwheel"), reduced arm swing.
- Akinesia (Slowness of Movement): Core feature; difficulty initiating/executing movements, slow daily tasks, reduced reaction time, micrographia (small handwriting).
- Postural (Gait) Disturbance: Later symptom; flexed posture, shuffling steps (festination), reduced arm swing, "freezing of gait," turning "en bloc."
Non-Motor Symptoms
Often precede motor symptoms and impact quality of life.
- Loss of smell (anosmia).
- Sleep dysfunction (e.g., REM behavior disorder, daytime sleepiness).
- Mood disorders (depression, anxiety, apathy).
- Excess salivation (drooling).
- Constipation.
- Autonomic dysfunction (orthostatic hypotension, dysphagia, urinary issues, sexual dysfunction).
- Dementia (cognitive decline in advanced stages).
 Stages of Parkinson's Disease (Hoehn and Yahr Scale)
Stages of Parkinson's Disease (Hoehn and Yahr Scale)
- Stage 0: No signs.
- Stage 1: Unilateral involvement.
- Stage 1.5: Unilateral plus axial involvement.
- Stage 2: Bilateral disease, no balance impairment.
- Stage 2.5: Mild bilateral, recovers on pull test.
- Stage 3: Mild to moderate bilateral, some postural instability, physically independent.
- Stage 4: Severe disability, still walks/stands unassisted.
- Stage 5: Wheelchair-bound or bedridden unless aided.
Diagnostic Process And Evaluation
Diagnosis is primarily clinical, based on history and neurological exam.
Clinical Diagnosis
Based on bradykinesia plus resting tremor or rigidity, often with asymmetric onset.
Exclusion of Other Conditions
Rule out drug-induced parkinsonism (e.g., from antipsychotics), other alpha-synucleinopathies (Lewy body dementia, multiple system atrophy), tauopathies (progressive supranuclear palsy), and other conditions (essential tremor, Huntington chorea, normal pressure hydrocephalus).
Role of Imaging Studies
- MRI: Excludes other conditions (stroke, tumors, hydrocephalus).
- DaTscan (Dopamine Transporter Scan): Identifies loss of dopaminergic neurons in striatum. Useful to distinguish PD from essential tremor, drug-induced parkinsonism, and vascular parkinsonism when clinical diagnosis is unclear. Cannot distinguish PD from other parkinsonian syndromes (PSP, CBD, MSA). Not for monitoring progression.
Response to Levodopa Treatment
A clear, sustained positive response to levodopa strongly supports a PD diagnosis.
Rating Scales
- Unified Parkinson Disease Rating Scale (UPDRS): Comprehensive assessment of motor and non-motor symptoms.
- Hoehn and Yahr Staging: Global measure of disease progression.
Pharmacological Management
Pharmacology is key for symptom control, not cure. Most patients need combination therapy. Response may weaken over time. Adherence is crucial; abrupt stopping can be dangerous.
Drug Classes, Mechanisms, Side Effects, and Nursing Implications
Levodopa/Carbidopa
- Mechanism: Levodopa (dopamine precursor) crosses BBB, converts to dopamine. Carbidopa prevents peripheral breakdown, increasing brain availability and reducing GI side effects. Most effective for bradykinesia, rigidity, tremor.
- Side Effects: Nausea/vomiting, dizziness, postural hypotension, headache, daytime sleepiness, confusion, hallucinations, dyskinesias, "on-off" episodes. Harmless dark urine/sweat. Possible melanoma risk.
- Nursing Implications: Start low, full effect up to 6 months. Monitor "on-off" and dyskinesias. Assess for orthostatic hypotension, psychosis. Avoid high-protein foods. Do not stop abruptly (risk of parkinsonism hyperpyrexia syndrome). Avoid alcohol, reserpine, pyridoxine (B6), phenothiazine.
Dopamine Agonists
- Mechanism: Directly stimulate dopamine receptors, mimicking dopamine. Used early to delay levodopa, or as adjuncts for motor fluctuations.
- Side Effects: Hallucinations, delusions, confusion, drowsiness, sudden sleep attacks, impulsive behaviors, nausea/vomiting, dry mouth, orthostatic hypotension.
- Nursing Implications: Start low, titrate gradually. Monitor for hallucinations, confusion, impulsive behaviors (especially in elderly). Advise against driving if sudden sleepiness occurs. Do not stop abruptly (risk of withdrawal syndrome).
MAO-B Inhibitors
- Mechanism: Block MAO-B enzyme, increasing dopamine availability in brain. Used alone in early PD or as add-on to levodopa to reduce "off" time.
- Side Effects: Heartburn, nausea, dry mouth, dizziness, insomnia, headaches, confusion, hallucinations. May worsen dyskinesia. Risk of hypertensive crisis with tyramine-rich foods or certain antidepressants.
- Nursing Implications: Full effect in 2-3 weeks. Monitor for dyskinesia (may need levodopa dose reduction). Avoid certain antidepressants, decongestants. Educate on tyramine-rich foods.
COMT Inhibitors
- Mechanism: Block COMT enzyme, preventing levodopa breakdown in periphery, extending levodopa's half-life and "on" time. Always used with levodopa.
- Side Effects: Diarrhea, dyskinesia (may worsen), confusion, hallucinations, dizziness, falls. Harmless reddish-orange urine. Tolcapone has rare liver damage risk (requires monitoring).
- Nursing Implications: Always take with levodopa. Levodopa dose may need reduction. Monitor for dyskinesia, diarrhea. For tolcapone, strict liver function monitoring. Avoid iron supplements concurrently with entacapone.
Anticholinergics
- Mechanism: Block acetylcholine, reducing tremor and rigidity. Minimal effect on bradykinesia/postural instability. Can reduce drooling.
- Side Effects: Cognitive deficits, confusion, memory impairment, sedation, delirium, hallucinations (especially in elderly). Dry mouth, blurred vision, constipation, urinary retention.
- Nursing Implications: Used for younger patients, primarily for tremor/dystonia; avoid in those over 70. Start low, titrate gradually. Monitor for cognitive side effects. Manage dry mouth, constipation, urinary retention. Contraindicated in narrow-angle glaucoma, myasthenia gravis, severe ulcerative colitis.
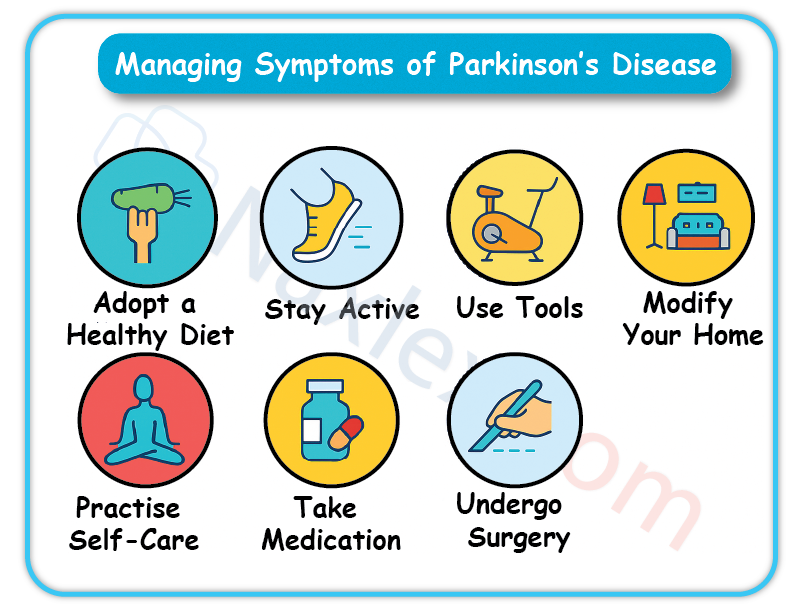
VI. Non-Pharmacological Management and Surgical Interventions
Holistic management includes therapies and, for select patients, surgery.
Therapies
- Physical Therapy (PT): Improves gait, balance, strength, flexibility. Includes cardiorespiratory, resistance, flexibility, gait/balance training. Teaches movement strategies (rocking, large steps, arm swing).
- Occupational Therapy (OT): Maximizes fine motor skills, adapts ADLs, provides adaptive equipment.
- Speech Therapy: Addresses communication (dysarthria, hypophonia) and swallowing (dysphagia). Teaches facial/tongue exercises, voice amplification, safe swallowing.
- Complementary Therapies: Yoga, Tai Chi, Qigong, acupuncture, massage, art/music therapy, meditation. May help with symptoms and well-being.
Surgical Interventions
For advanced motor complications not controlled by medication.
Deep Brain Stimulation (DBS)
- Description: Electrodes implanted in specific brain areas (STN, GPi) connected to a chest neurostimulator. Delivers continuous electrical impulses to modulate abnormal brain activity. Does not damage brain tissue.
- Indications: Disabling tremors, significant motor fluctuations ("on-off"), medication-induced dyskinesias, good levodopa response but with side effects. PD symptoms for at least 4 years.
- Benefits: Significant symptom reduction, reduced medication dosages, decreased dyskinesia. Benefits last at least 5 years. Reversible and adjustable.
- Risks/Complications: Small risk of infection, stroke, bleeding, seizure. Post-op: reduced speech clarity, subtle word-finding issues, cognitive decline (if pre-existing).
- Nursing Care:
- Pre-op: Stop blood thinners, withhold movement disorder meds after midnight before surgery. NPO. Skin cleansing. Cognitive assessment.
- Post-op: Wound care (clean/dry, remove dressings day 3, gentle showering). Pain management (taper opioids). Activity restrictions (no heavy lifting, strenuous activity, driving for 2 weeks). Patient education: carry ID card, inform airport security, avoid large magnetic fields/heat therapy/electrocautery. DBS activated 3-4 weeks post-op.
Focused Ultrasound (FUS)
- Description: Non-invasive. Focused ultrasound beams create precise thermal lesions in brain targets (thalamus for tremor, globus pallidus for dyskinesia/rigidity) to disrupt abnormal circuits. No incision or implants.
- Indications: Tremor-dominated PD, Parkinson's dyskinesia, mobility, rigidity, slow initiation of movement. Currently unilateral, bilateral studies ongoing.
- Benefits: Non-invasive, avoids implant risks. Single procedure, no battery/wire maintenance. Potential for future drug delivery by opening blood-brain barrier.
- Risks/Complications: Sensory disturbances (numbness/tingling, temporary or permanent in 10-15%). Gait disturbance/imbalance (common temporarily, permanent in up to 10%). Minor: headache, pain, dizziness during procedure. Very low risk of stroke, infection, seizures.
- Nursing Care: Pre-procedure preparation. Monitor comfort/vitals during. Post-procedure: monitor side effects, educate on temporary symptoms, safety precautions for unsteadiness.
Nursing Care Plan
Holistic, patient-centered care with interprofessional collaboration. Goals: optimize motor function, enhance quality of life, maintain independence, promote stability, empower patients/caregivers.
Mobility
- Assessment: Motor function (tremors, gait, balance), ADL independence, fine motor skills, weakness, fatigue, stiffness.
- Interventions: PT referral. Assistive devices. Teach movement techniques (rocking to initiate, large steps, arm swing, lifting feet, visual cues for freezing, holding objects for tremor, warm baths for rigidity). Proper posture (firm mattress, prone positioning). Energy conservation. Avoid rushing.
Safety
- Fall Prevention: Remove hazards (rugs, clutter). Home modifications (grab bars, elevated toilets, chair lifts). Low-heeled shoes. Monitor gait/balance, especially during "off" periods.
- Medication Safety: Educate on dosage, route, action, side effects. Monitor for side effects (impaired balance, dizziness, sleepiness). Educate on drug-drug/drug-food interactions. Stress never stopping meds abruptly.
Nutrition
- Assessment: Swallowing function (dysphagia, aspiration risk), weight changes, constipation.
- Interventions: Dietitian collaboration (thickened liquids, pureed foods). Small, frequent, nutrient-dense meals. Increase fluids/fiber for constipation. Limit Vitamin B6 foods (can block levodopa).
Communication
- Assessment: Speech patterns (slurred, soft, monotone), ability to express.
- Interventions: Speech therapy referral. Encourage deep breaths, diaphragmatic speech. Suggest communication aids (amplifiers, boards). Allow ample response time.
Elimination
- Assessment: Constipation, urinary retention.
- Interventions: Increase fiber/fluids, encourage mobility for constipation. Monitor for urinary retention, discuss management.
Psychosocial Well-being
- Assessment: Emotional well-being (depression, anxiety, mood swings), cognitive function (memory, attention), caregiver strain.
- Interventions: Mental health professional referral. Support groups for patients/families. Patient/caregiver education on disease management, coping. Promote independence.
Complications And Prognosis
PD is chronic and progressive; symptoms worsen over time. Not directly fatal, but complications increase morbidity/mortality.
Complications
- Depression and Dementia: Common, especially in advanced stages; increased confusion, hallucinations, agitation.
- Laryngeal Dysfunction and Aspiration Pneumonia: Dysphagia leads to aspiration, major cause of illness/death. Weak cough reflex.
- Autonomic Dysfunction: Orthostatic hypotension (falls risk), urinary retention, erectile dysfunction.
- Falls: Increased risk due to balance problems, gait issues, orthostatic hypotension. Leading cause of ER visits/hospitalizations.
- Pressure Ulcers: Due to immobility; risk of infection/sepsis.
- Kyphosis: Flexed posture can lead to spinal curvature, cardiopulmonary impairment.
- Other Infections and Frailty: Increased susceptibility to infections, reduced resilience to new medical problems. Hospitalization risks (medication disruption, increased immobility, UTIs).
Disease Progression and Long-Term Prognosis
PD is progressive, but progression rate varies. No way to predict individual course. Advanced PD (longer duration, higher Hoehn and Yahr stage, cognitive dysfunction, hallucinations, comorbidities) linked to increased mortality risk. Patients typically succumb to complications (pneumonia, sepsis from ulcers, fall complications) on top of increasing disability/frailty. Proactive management minimizes risks.
Patient And Family Education And Support
Empowering patients and families is crucial for active participation and coping.
Medication Adherence
- Importance of Schedule: Strict adherence for consistent symptom control.
- Reporting Side Effects: Promptly report new/bothersome symptoms.
- Never Stop Abruptly: Risk of severe complications.
- Interactions: Educate on food/drug interactions (protein, tyramine, B6, other meds, OTCs, supplements). Use single pharmacy.
Lifestyle Modifications
- Exercise: Only intervention potentially slowing progression. Regular cardio, resistance, flexibility, balance training.
- Diet and Nutrition: Manage constipation (fiber/fluids), optimize medication absorption (avoid high-protein with levodopa). Small, frequent meals.
- Sleep Hygiene: Promote good practices for sleep dysfunction.
Coping Strategies
- Mental Health Support: Encourage professional help for depression, anxiety.
- Support Groups: Provide emotional support, shared experiences, coping strategies.
- Adaptive Strategies: Guidance on adapting daily living as disease evolves.
Summary
- Parkinson's disease is a complex, progressive neurodegenerative disorder.
- It is defined by both motor symptoms (e.g., tremor, rigidity, bradykinesia) and non-motor symptoms (e.g., depression, sleep disturbances, autonomic dysfunction).
- The disease stems from dopaminergic neuron loss in the substantia nigra and alpha-synuclein protein aggregation.
- Diagnosis is clinical, often supported by neuroimaging and a positive response to levodopa therapy.
- Pharmacological treatments (e.g., levodopa, dopamine agonists) and non-pharmacological therapies (e.g., physical and occupational therapy) are essential for symptom control.
- Surgical options, such as deep brain stimulation, may be considered in advanced cases
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Parkinson’s Disease
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now