Please set your exam date
Drugs Used for Sedation and Sleep
Study Questions
Practice Exercise 1
A hospitalized patient is complaining of having difficulty sleeping. Which action will the nurse take first to address this problem?
Explanation
When a patient in the hospital reports difficulty sleeping, the nurse’s first priority is to implement nonpharmacologic interventions, such as providing a quiet and restful environment. These measures are safe, cost-effective, and address common hospital-related barriers to sleep, such as noise and interruptions. Medication or alternative remedies are considered only after basic environmental and comfort measures are attempted.
Rationale for correct answer:
D. Provide an environment that is restful, and reduce loud noises
Creating a quiet, calm environment is the safest and most immediate intervention to help the patient sleep. Reducing noise, dimming lights, and minimizing interruptions can significantly improve sleep quality, especially in the hospital setting where environmental disturbances are common.
Rationales for incorrect answers:
A. Administer a sedative-hypnotic drug if ordered
This should not be the first step. Pharmacologic interventions are considered only after non-drug measures fail due to potential adverse effects and risks such as dependence or oversedation.
B. Offer tea made with the herbal preparation valerian
Herbal remedies may promote relaxation but are not the initial intervention in the hospital. Additionally, herbal supplements may interact with prescribed medications and are generally not given without provider approval.
C. Encourage the patient to exercise by walking up and down the halls a few times if tolerated
Exercising before bedtime is not recommended, as it may increase stimulation and make it harder to fall asleep. Physical activity is best encouraged earlier in the day.
Take-home points:
- Always implement nonpharmacologic sleep measures first in hospitalized patients.
- A quiet, restful environment is the priority intervention.
- Pharmacologic or herbal sleep aids are secondary and require provider oversight.
Patient scenario:
A patient who recently lost their job and is experiencing bouts of insomnia called the nurse line to discuss options for better sleep.
A patient was discussing a recent development of nightmares and restlessness since the discontinuation of triazolam (Halcion) with the nurse, who recognized the symptoms of which sleep disorder?
Explanation
Triazolam (Halcion) is a short-acting benzodiazepine used for insomnia. When discontinued suddenly, it can cause rebound phenomena, including nightmares, restlessness, and worsened sleep disturbances. This occurs because the body, previously reliant on the drug for sedation, reacts with heightened arousal when it is removed. Recognizing rebound sleep is critical to prevent unnecessary re-dosing and to guide safe tapering strategies.
Rationale for correct answer:
A. Rebound sleep
Rebound sleep refers to the return of insomnia symptoms—often worse than before treatment—after abrupt discontinuation of a sedative-hypnotic drug like triazolam. It is characterized by vivid dreams, nightmares, increased wakefulness, and restlessness. This effect is particularly common with short-acting benzodiazepines.
Rationales for incorrect answers:
B. Terminal insomnia
Terminal insomnia involves waking up too early and being unable to fall back asleep. While problematic, it is not typically associated with vivid nightmares after medication withdrawal.
C. Transient insomnia
Transient insomnia is short-term insomnia related to stress, changes in environment, or situational factors. It does not explain the nightmares and restlessness after stopping triazolam.
D. Initial insomnia
Initial insomnia refers to difficulty falling asleep at the start of the night. It does not match the clinical picture of nightmares and increased restlessness after stopping a sleep medication.
Take-home points:
- Rebound sleep occurs when insomnia symptoms worsen after abrupt discontinuation of sedative-hypnotics.
- Short-acting benzodiazepines like triazolam are especially prone to causing rebound insomnia and nightmares.
- Gradual tapering and patient education are essential to prevent withdrawal-related sleep disturbances.
The nurse is reviewing an order for a sleep aid for a patient in the scenario who is complaining of insomnia. The nurse understands that a sedative is different from a hypnotic in which manner?
Explanation
Sedatives and hypnotics are both CNS depressants, but they differ in the degree of depression they cause. Sedatives produce relaxation and decrease anxiety without necessarily causing sleep, while hypnotics are stronger agents that induce and maintain sleep. Understanding this distinction allows nurses to anticipate the intended therapeutic outcome and monitor patients appropriately.
Rationale for correct answer:
B. The sedative causes feelings of relaxation and rest, and the hypnotic agent produces sleep.
This is the key distinction. Sedatives calm the patient and reduce restlessness, making it easier to relax, whereas hypnotics are designed to promote the onset and maintenance of sleep. Both act on similar pathways in the brain, but the dosage and intensity of effect differ.
Rationales for incorrect answers:
A. The sedative causes feelings of relaxation and rest, and the hypnotic agent causes feelings of restlessness and anxiety.
Hypnotics are not intended to increase restlessness or anxiety—they promote sleep.
C. The hypnotic agent produces sleep, and the sedative causes no hangover effect.
Both sedatives and hypnotics can cause residual drowsiness or a “hangover effect,” especially in older adults. The difference lies in sedation versus sleep induction, not adverse effects.
D. The hypnotic agent causes feelings of relaxation and rest, and the sedative produces sleep.
This reverses the definitions. Sedatives relax without always producing sleep, while hypnotics directly promote sleep.
Take-home points:
- Sedatives promote relaxation and reduce restlessness but do not necessarily cause sleep.
- Hypnotics induce sleep and are used for short-term management of insomnia.
- Both classes can cause CNS depression and residual drowsiness, requiring close monitoring for safety.
The patient in the scenario came to the clinic complaining of not being able to get a good night’s sleep for the past month, as he finds that he frequently awakens throughout the night, then will fall asleep again. The nurse recognizes this condition as which sleep disorder?
Explanation
Intermittent insomnia is characterized by frequent awakenings during the night with difficulty maintaining sleep, even though the patient may eventually fall back asleep. It can be caused by stress, medical conditions, medications, or environmental disturbances. Recognizing the specific type of insomnia helps the nurse plan targeted interventions to improve sleep quality.
Rationale for correct answer:
B. Intermittent insomnia
This form of insomnia involves repeated awakenings throughout the night, which can lead to daytime fatigue, impaired concentration, and mood disturbances. Unlike initial insomnia (difficulty falling asleep) or terminal insomnia (early morning awakening), intermittent insomnia specifically affects the maintenance of sleep.
Rationales for incorrect answers:
A. Initial insomnia
Initial insomnia refers to difficulty falling asleep at the beginning of the night, not frequent nighttime awakenings.
C. Terminal insomnia
Terminal insomnia involves waking too early in the morning and being unable to return to sleep, which is not described in this scenario.
D. Transient insomnia
Transient insomnia is short-term, usually lasting a few days and often related to stress or environmental changes. A duration of one month exceeds the typical definition of transient insomnia.
Take-home points:
- Intermittent insomnia involves frequent nighttime awakenings with difficulty maintaining sleep.
- Correctly identifying the type of insomnia guides appropriate interventions.
- Causes may include stress, medications, or medical conditions, and management should address underlying factors.
Practice Exercise 2
A nurse in a provider’s office is providing instructions to a client who has a new prescription for lorazepam (Ativan). The nurse should inform the client that which of the following are adverse effects of lorazepam? Select all that apply
Explanation
When educating clients about lorazepam (Ativan), it is important to stress that this benzodiazepine acts on the central nervous system (CNS) to enhance the inhibitory effects of GABA. While effective for anxiety, seizures, and sedation, lorazepam may produce adverse effects such as incoordination, euphoria, and amnesia. Clients must be taught these risks to ensure safety and reduce chances of misuse or dependence.
Rationale for correct answer:
A. Incoordination:
Lorazepam causes CNS depression, which can impair motor control, balance, and coordination. This increases the risk of falls and accidents, especially in older adults.
B. Euphoria:
Some clients experience a sense of euphoria, which contributes to lorazepam’s potential for misuse and dependence. This reinforces the need for close monitoring and short-term prescribing.
E. Amnesia:
Lorazepam can cause anterograde amnesia, where new memories are impaired after the drug is taken. This effect is especially noted when the drug is used for sedation or preoperative purposes.
Rationales for incorrect answers:
C. Pruritus:
Itching is not a common or expected adverse effect of lorazepam. While possible with some medications, it is not typically associated with benzodiazepines.
D. Flatus:
Increased intestinal gas is unrelated to lorazepam’s pharmacologic action and is not considered an adverse effect of this medication.
Take-home points:
• Lorazepam can cause incoordination, euphoria, and amnesia due to CNS effects.
• Clients should be counseled on safety precautions such as avoiding driving or operating heavy machinery.
• Benzodiazepines carry a risk for misuse and dependence, so therapy should be closely monitored and time-limited.
A nurse is caring for a client who is receiving moderate sedation with diazepam (Valium) IV. The client is over-sedated. Which of the following medications should the nurse anticipate administering to this client?
Explanation
When caring for a client receiving moderate sedation with diazepam (Valium), the nurse must be alert for signs of over-sedation or respiratory depression. Diazepam is a benzodiazepine, and the specific antidote for benzodiazepine overdose is flumazenil (Romazicon). Flumazenil is a benzodiazepine receptor antagonist that rapidly reverses sedation and restores protective reflexes, making it the drug of choice in this situation.
Rationale for correct answer:
C. Flumazenil (Romazicon):
Flumazenil works by competitively binding to benzodiazepine receptor sites, thereby reversing their sedative, hypnotic, and respiratory-depressant effects. It acts quickly, usually within minutes, and is administered intravenously. The nurse should anticipate giving this medication when a client receiving diazepam becomes overly sedated. Because flumazenil has a shorter half-life than many benzodiazepines, clients require close monitoring for resedation and recurrence of symptoms after initial reversal.
Rationales for incorrect answers:
A. Ketamine (Ketalar):
This is a dissociative anesthetic, not an antidote. Administering ketamine would worsen sedation rather than reverse it.
B. Naltrexone (ReVia):
Naltrexone is an opioid antagonist used to treat opioid and alcohol dependence. It does not affect benzodiazepine receptors and would have no benefit in reversing diazepam sedation.
D. Fluvoxamine (Luvox):
This is a selective serotonin reuptake inhibitor (SSRI) used to treat depression and obsessive-compulsive disorder. It has no role in reversing benzodiazepine overdose.
Take-home points:
• Flumazenil is the antidote for benzodiazepine overdose and over-sedation.
• Clients require close monitoring after reversal due to the risk of resedation as flumazenil wears off.
• Other agents such as ketamine, naltrexone, and fluvoxamine have no effect on benzodiazepine-induced sedation.
A patient taking lorazepam (Ativan) asks the nurse how this drug works. The nurse should respond by stating that it is a benzodiazepine that acts by which mechanism?
Explanation
When teaching a client about lorazepam (Ativan), it is important to emphasize that it is a benzodiazepine, which works by enhancing the effect of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). By binding to GABA receptors, lorazepam increases GABA’s calming effect on the central nervous system, producing anxiolytic, sedative, muscle-relaxant, and anticonvulsant effects.
Rationale for correct answer:
C. Increasing the action of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA) to GABA receptors:
Lorazepam and other benzodiazepines do not directly stimulate GABA receptors but potentiate GABA’s natural inhibitory effect. By increasing the frequency of chloride channel opening at the receptor site, these drugs enhance neuronal hyperpolarization, leading to reduced excitability of the CNS. This mechanism provides therapeutic benefits in anxiety, seizure control, muscle relaxation, and sedation.
Rationales for incorrect answers:
A. Depressing the central nervous system (CNS), leading to a loss of consciousness:
This describes the effect of general anesthetics, not lorazepam. While lorazepam causes sedation, it does not routinely induce complete loss of consciousness at therapeutic doses.
B. Depressing the CNS, including the motor and sensory activities:
This explanation aligns more with barbiturates or high-dose anesthetics that cause widespread CNS suppression. Lorazepam acts selectively by potentiating GABA, not by indiscriminate CNS depression.
D. Creating an epidural block by placement of the local anesthetic in the outer covering of the spinal cord:
This is the mechanism of local anesthetics used in regional anesthesia, not benzodiazepines. Lorazepam has no role in creating nerve blocks or spinal anesthesia.
Take-home points:
• Lorazepam works by enhancing the inhibitory effects of GABA at its receptors.
• Its clinical uses include treating anxiety, seizures, muscle spasms, and insomnia.
• It is different from general anesthetics and local anesthetics, which act through broader CNS depression or nerve conduction blockade.
A patient is taking triazolam (Halcion). Which instructions about this drug are important for the nurse to include?
Explanation
Triazolam (Halcion) is a short-acting benzodiazepine prescribed for short-term management of insomnia. It enhances the effects of GABA, promoting sedation and sleep onset. Client teaching must emphasize safety precautions, especially avoiding substances like alcohol and tobacco, which can alter the drug’s effects and increase the risk of complications.
Rationale for correct answer:
D. Avoid alcohol and smoking while taking this drug.
Alcohol has a synergistic depressant effect when combined with triazolam, greatly increasing the risk of respiratory depression, excessive sedation, and impaired coordination. Smoking induces hepatic enzymes that can increase drug metabolism, lowering its effectiveness. Teaching the client to avoid both alcohol and smoking ensures optimal therapeutic effect and safety.
Rationales for incorrect answers:
A. It may be used as a barbiturate for only 4 weeks.
Triazolam is a benzodiazepine, not a barbiturate. Additionally, treatment duration is usually limited to 7–10 days, not 4 weeks, due to risks of dependence and rebound insomnia.
B. Use as a nonbenzodiazepine to reduce anxiety.
Triazolam is classified as a benzodiazepine, not a nonbenzodiazepine. While it has anxiolytic effects, its main therapeutic role is in treating insomnia, not general anxiety management.
C. This drug does not lead to vivid dreams or nightmares.
Triazolam can actually cause vivid dreams, nightmares, or abnormal sleep behaviors (such as sleepwalking or sleep-driving) in some clients, particularly with prolonged use or higher doses.
Take-home points:
- Triazolam is a short-acting benzodiazepine used for short-term treatment of insomnia.
- Clients must avoid alcohol and smoking due to risks of excessive sedation or reduced effectiveness.
- Potential side effects include vivid dreams, nightmares, and abnormal sleep behaviors.
Practice Exercise 3
Zolpidem (Ambien) has been ordered for a client for the treatment of insomnia. What information will the nurse provide for this client? Select all that apply
Explanation
Zolpidem (Ambien) is a non-benzodiazepine hypnotic prescribed for the short-term management of insomnia. It has a rapid onset of action, which means it should be taken immediately before bedtime. The drug can cause residual sedation or a “hangover” effect the following day, particularly in sensitive clients. In addition, zolpidem carries a risk of additive CNS depression if combined with alcohol or other sedating medications, which can lead to dangerous respiratory or cognitive impairment.
Rationale for correct answer:
A. Be cautious when performing morning activities because it may cause a significant “hangover” effect with drowsiness and dizziness.
Zolpidem can cause next-day sedation, dizziness, and impaired coordination, which is why clients must use caution when driving or performing activities that require alertness the following morning. This residual effect is an adverse reaction and can increase the risk of falls and accidents.
C. Take the drug immediately before going to bed; it has a quick onset of action.
Zolpidem has a rapid onset (within 15–30 minutes) and a short half-life, making it effective for initiating sleep quickly. For maximum effectiveness and safety, clients should only take the medication when they are ready to sleep and can remain in bed for at least 7–8 hours
E. Alcohol and other drugs that cause CNS depression (e.g., antihistamines) should be avoided while taking this.
Zolpidem exerts its effects by enhancing GABA-mediated CNS depression. Combining it with alcohol, opioids, benzodiazepines, or sedating antihistamines can result in additive respiratory depression, excessive sedation, confusion, or even coma.
Rationales for incorrect answers:
B. Take the drug with food; this enhances the absorption for quicker effects.
Food actually delays the absorption of zolpidem, leading to a slower onset of action. Clients should take the drug on an empty stomach to ensure rapid effectiveness in promoting sleep.
D. If the insomnia is long-lasting, this drug may safely be used for up to one year.
Zolpidem is intended for short-term use only (typically 7–10 days) because of risks such as dependence, tolerance, and rebound insomnia. Long-term use is generally avoided unless under very specific medical supervision.
Take-home points:
- Zolpidem should be taken immediately before bedtime due to its rapid onset.
- Residual morning drowsiness is common—clients must be cautious with driving or activities requiring alertness.
- Alcohol and other CNS depressants must be strictly avoided to prevent dangerous sedation.
A nurse is providing instructions to a female client who has a new prescription for zolpidem (Ambien). Which of the following instructions should the nurse include?
Explanation
When teaching a female client about zolpidem (Ambien), it is important to highlight that this drug is a sedative-hypnotic used for the short-term management of insomnia. Zolpidem is classified as pregnancy category C, meaning potential risks to the fetus cannot be ruled out. Therefore, women of childbearing age should be instructed to notify their provider if they plan to become pregnant while taking zolpidem to ensure safe management.
Rationale for correct answer:
A. Notify the provider if you plan to become pregnant:
Zolpidem may cause fetal harm when administered during pregnancy. Clients planning pregnancy or who become pregnant must consult their provider to evaluate whether the drug should be discontinued or replaced with a safer alternative.
Rationales for incorrect answers:
B. Take the medication 1 hr before you plan to go to sleep:
Zolpidem has a rapid onset of action and should be taken immediately before bedtime, not 1 hour earlier. Taking it too soon may lead to unnecessary drowsiness before the client is ready for sleep.
C. Allow at least 6 hr for sleep when taking zolpidem:
The correct recommendation is to allow at least 8 hr of sleep time after taking zolpidem. If the client awakens earlier, there may be residual drowsiness, dizziness, or impaired alertness.
D. To increase the effectiveness of zolpidem, take it with a bedtime snack:
Food, especially a high-fat meal, delays the absorption of zolpidem and reduces its effectiveness in promoting sleep onset. It should be taken on an empty stomach for optimal effect.
Take-home points:
• Zolpidem is contraindicated in pregnancy, so women should notify their provider if planning to conceive.
• The drug should be taken immediately before bedtime, with at least 8 hr available for sleep.
• Clients should avoid taking zolpidem with food, as it delays absorption and reduces effectiveness.
A patient is taking zolpidem (Ambien) for insomnia. The nurse prepares a care plan that includes monitoring of the patient for side effects/adverse reactions of this drug. Which is a side effect of zolpidem?
Explanation
When caring for a client taking zolpidem (Ambien) for insomnia, it is important to recognize the potential side effects and adverse reactions associated with this sedative-hypnotic. Although generally well tolerated, zolpidem may cause headache, dizziness, and daytime drowsiness. Monitoring for these effects helps ensure client safety and appropriate management of therapy.
Rationale for correct answer:
B. Headache:
Headache is a common side effect of zolpidem due to its central nervous system activity. Other mild side effects may include dizziness, nausea, or next-day drowsiness. Clients should be informed about these possible effects and encouraged to report persistent or severe headaches to their healthcare provider.
Rationales for incorrect answers:
A. Insomnia:
Zolpidem is prescribed to treat insomnia, not cause it. While rebound insomnia can occur if the drug is discontinued abruptly after long-term use, insomnia itself is not considered a direct side effect during therapy.
C. Laryngospasm:
Laryngospasm is not associated with zolpidem use. This adverse effect is more commonly related to anesthetic agents rather than hypnotics like zolpidem.
D. Blood dyscrasias:
Zolpidem does not cause hematologic adverse effects such as anemia, leukopenia, or thrombocytopenia. Blood dyscrasias are more likely linked to other classes of drugs, such as certain antipsychotics or chemotherapy agents.
Take-home points:
• Headache is a common side effect of zolpidem and should be monitored in clients taking the drug.
• Zolpidem is effective for short-term insomnia treatment but carries risks of dizziness, drowsiness, and dependence.
• Rebound insomnia may occur if abruptly discontinued, reinforcing the need for careful tapering and patient education.
A nurse is teaching a patient about zolpidem. Which is important for the nurse to include in the teaching of this drug?
Explanation
Zolpidem is a sedative-hypnotic commonly used for short-term treatment of insomnia. While it is effective in improving sleep onset and maintenance, it carries a risk of psychological dependence with prolonged or inappropriate use. Clients need education on safe use, potential adverse effects, and the importance of adhering to prescribed dosing and duration.
Rationale for correct answer:
B. It may lead to psychological dependence.
Zolpidem, though structurally different from benzodiazepines, acts on the GABA-A receptor complex and can cause dependence when used beyond the recommended period or at higher-than-prescribed doses. Psychological dependence means the client may feel unable to sleep without the drug, which can create problematic reliance.
Rationales for incorrect answers:
A. The maximum dose is 20 mg/d.
The recommended maximum dose for zolpidem is typically 10 mg once daily at bedtime for adults, and often lower (5 mg) for older adults or those with hepatic impairment. A 20 mg/day dose would exceed safety limits and increase the risk of adverse effects such as next-day drowsiness, confusion, and impaired coordination.
C. For older adults, the dose is 15 mg at bedtime.
Older adults are more sensitive to zolpidem, so they are prescribed lower doses (commonly 5 mg at bedtime) to reduce the risk of excessive sedation, falls, and confusion. A 15 mg dose would be unsafe and contraindicated.
D. The drug should only be used for 21 days or less.
While zolpidem is recommended for short-term use, usually no longer than 7–10 days, the statement of “21 days or less” is misleading and not consistent with prescribing guidelines. Prolonged use increases the risk of dependence, rebound insomnia, and withdrawal symptoms.
Take-home points:
- Zolpidem can cause psychological dependence if misused or used long-term.
- The safe maximum dose is 10 mg at bedtime for adults, and lower (5 mg) for older adults.
- Use is intended for short-term management of insomnia, typically no longer than 7–10 days.
Practice Exercise 4
A nurse is teaching a client who has a new prescription for ramelteon (Rozerem) about the medication. The nurse should instruct the client to avoid which of the following foods while taking this medication?
Explanation
When teaching a client about ramelteon (Rozerem), it is important to emphasize that this drug is a melatonin receptor agonist used for insomnia. Unlike benzodiazepines, it has a lower risk of dependence, but its metabolism is strongly affected by grapefruit juice, which inhibits the CYP450 enzyme system in the liver. This can lead to increased blood levels of the drug, raising the risk of excessive sedation and adverse effects.
Rationale for correct answer:
B. Grapefruit juice:
Grapefruit juice inhibits the cytochrome P450 (CYP1A2 and CYP3A4) enzymes responsible for metabolizing ramelteon. When metabolism is inhibited, serum levels of ramelteon rise, increasing the likelihood of prolonged sedation, dizziness, and impaired daytime function. To ensure safe therapy and reduce risk of adverse effects, clients should avoid grapefruit juice entirely while on this medication.
Rationales for incorrect answers:
A.Eggs:
There is no interaction between ramelteon and eggs. Clients can safely consume eggs while taking this medication.
C. Whole-grain bread:
Whole-grain bread does not affect the metabolism or absorption of ramelteon. It is not restricted in the client’s diet.
D. Chicken:
Chicken does not interact with ramelteon and is safe to consume. No dietary precautions are necessary regarding this food.
Take-home points:
• Ramelteon is a melatonin receptor agonist used for insomnia with a low risk of dependence.
• Grapefruit juice should be avoided because it inhibits metabolism and increases drug levels.
• Dietary interactions are specific—most common foods like eggs, bread, or chicken are safe.
The nurse is preparing to administer suvorexant (Belsomra) for sleep. The nurse will need to include which teaching about this drug? Select all that apply
Explanation
Suvorexant (Belsomra) is an orexin receptor antagonist used for insomnia. Patient teaching should cover timing of administration (about 30 minutes before bedtime) and the risk of daytime somnolence and complex/unconscious nighttime behaviors (sleepwalking, sleep-driving). Advise precautions to promote safety and avoid additive CNS depressants.
Rationale for correct answers:
A. This drug needs to be taken approximately 30 minutes before bedtime.
Suvorexant’s onset of action aligns with taking it about 30 minutes before intended sleep, so the drug’s peak effect coincides with sleep initiation. Taking it too early reduces nighttime benefit and can produce excessive daytime sedation; taking it with a high-fat meal delays absorption and slows onset. Patients should only take suvorexant when they can allow at least 7 hours for sleep.
C. The patient needs to be cautioned about the high incidence of daytime somnolence and unconscious nighttime behaviors that may occur.
Suvorexant can cause next-day drowsiness and has been associated with complex sleep-related behaviors (e.g., sleepwalking, sleep-driving, eating while not fully awake). Counseling should include avoiding driving or operating machinery until the patient knows how the drug affects them, and reporting any unusual nighttime behaviors immediately. Alcohol and other CNS depressants increase these risks.
Rationales for incorrect answers:
B. It needs to be taken 2 hours before bedtime because of its slow onset.
Onset is much faster than 2 hours; recommending a 2-hour lead time would unnecessarily increase daytime sedation and reduce the medication’s usefulness for sleep onset.
D. This drug is less likely to interact with alcohol.
Alcohol has additive CNS-depressant effects with suvorexant and increases the risk of severe drowsiness and unsafe behaviors; patients should avoid alcohol while taking the medication.
E. This drug is available over the counter.
Suvorexant is a prescription medication because of its sedation risks and potential for complex sleep behaviors; it is not available OTC.
Take-home points:
- Take about 30 minutes before bedtime and only when able to get ≥7 hours of sleep.
- Beware of next-day somnolence and complex sleep behaviors; avoid driving until you know how it affects you.
- Avoid alcohol and other CNS depressants; suvorexant is prescription-only.
A nurse is providing education to a client who has mild insomnia and wishes to use valerian root instead of prescription medication. Which statements by the nurse are appropriate? Select all that apply
Explanation
Valerian root is an herbal supplement commonly used for mild insomnia, but it carries potential interactions and contraindications. Clients must be educated about risks when combining valerian with other central nervous system depressants, particularly benzodiazepines, as additive sedation can occur. Additionally, valerian is processed by the liver, so clients with hepatic disease should avoid its use.
Rationale for correct answer:
A. “Avoid combining valerian with benzodiazepines.”
Valerian enhances GABAergic activity, which can potentiate the sedative effects of benzodiazepines. This may lead to excessive drowsiness, dizziness, or respiratory depression. Clients must be warned against concurrent use with other sedatives to prevent dangerous additive CNS depression.
B. “Do not use valerian if you have liver disease.”
Valerian undergoes hepatic metabolism, and there have been rare reports of hepatotoxicity. Clients with pre-existing liver disease may be at increased risk of liver injury or complications, making avoidance essential.
Rationales for incorrect answers:
C. “Valerian is safe for use during breastfeeding.”
There is insufficient evidence to confirm the safety of valerian during lactation, and potential sedative effects could impact the infant. Nursing mothers should avoid valerian unless advised by a healthcare provider.
D. “You can stop valerian abruptly after regular use.”
Although valerian is not highly addictive, gradual tapering is recommended after prolonged use to reduce the risk of rebound insomnia or withdrawal-like symptoms. Abrupt discontinuation may worsen sleep disturbances.
E. “Valerian works quickly within minutes for acute insomnia.”
Valerian typically requires several days to weeks of consistent use to achieve maximal effect. It is not effective for immediate or acute insomnia, and clients should have realistic expectations regarding onset of action.
Take-home points:
• Valerian should not be combined with benzodiazepines or other sedatives due to additive CNS depression.
• Clients with liver disease should avoid valerian because of potential hepatotoxicity.
• Valerian requires regular use for several days to weeks and is not a rapid-onset solution for insomnia.
Comprehensive Questions
Education given to clients about the use of all drugs to treat insomnia should include an emphasis on what important issue?
Explanation
When educating clients about drugs used to treat insomnia, the nurse should emphasize the importance of short-term use and the risks associated with prolonged therapy. While these medications may be effective initially, long-term use increases the risk of tolerance, dependence, adverse effects, and rebound insomnia upon discontinuation.
Rationale for correct answer:
D. Long-term use may increase the risk of adverse effects, create a “sleep debt,” and cause rebound insomnia when stopped:
Chronic use of insomnia medications, including benzodiazepines and non-benzodiazepine hypnotics, can lead to tolerance (reduced effectiveness over time), physical dependence, and withdrawal symptoms if stopped abruptly. Rebound insomnia is common, where sleep problems worsen after discontinuation. In addition, long-term use increases risks such as daytime drowsiness, impaired cognition, falls, and drug interactions.
Rationales for incorrect answers:
A. They will be required long-term to achieve lasting effects:
This is incorrect because long-term use is not recommended. The goal is to use medications temporarily while addressing underlying causes of insomnia.
B. They require frequent blood counts to avoid adverse effects:
Most insomnia medications do not require blood count monitoring. This teaching point applies more to drugs with hematologic risks, such as certain anticonvulsants or clozapine, not sleep aids.
C. They are among the safest drugs available and have few adverse effects:
This is misleading. While many insomnia drugs are generally safe when used short term, they carry risks such as sedation, falls, confusion, dependence, and withdrawal when used inappropriately or for extended periods.
Take-home points:
• Insomnia medications should be used short term due to risks of dependence, tolerance, and rebound insomnia.
• Clients must be educated about combining medications with nonpharmacologic interventions for lasting benefits.
• Long-term use increases adverse effects, making patient teaching about safe use essential.
A patient is to receive conscious sedation for a minor surgical procedure. Which drug administration should the nurse expect? Select all that apply
Explanation
Conscious sedation, also called moderate sedation, is used during minor surgical or diagnostic procedures to ensure the client remains relaxed, drowsy, and cooperative while maintaining protective reflexes and the ability to respond to verbal commands. The drugs of choice are typically short-acting sedatives and anesthetics which provide effective sedation without prolonging recovery.
Rationale for correct answer:
A. Propofol (Diprivan) to sustain natural sleep
Propofol is a short-acting anesthetic commonly used for conscious sedation because it induces a sleep-like state while allowing rapid recovery once the infusion stops. It provides excellent control during minor procedures and has a predictable duration of action, making it ideal for outpatient settings.
C. Midazolam (Versed) to promote sedation and following of commands
Midazolam, a benzodiazepine, is frequently used in conscious sedation because it produces anxiolysis, amnesia, and moderate sedation. Clients remain able to follow commands while being comfortable and relaxed. Its rapid onset and short half-life make it safe and effective for minor surgical procedures.
Rationales for incorrect answers:
B. Lidocaine (Xylocaine) to provide local anesthesia
Lidocaine is a local anesthetic, not a sedative. While it may be used to numb the surgical area, it does not cause sedation or amnesia, and therefore is not considered a primary drug for conscious sedation.
D. Ketamine (Ketalar) for rapid induction and prolonged duration of action
Ketamine produces dissociative anesthesia rather than conscious sedation. It can cause hallucinations, agitation, and emergence reactions, making it less favorable for minor procedures requiring moderate sedation.
E. Phenobarbital (Luminal) for short-acting duration of sleep
Phenobarbital is a barbiturate with long-acting sedative properties, but it is rarely used for conscious sedation because of its prolonged duration, narrow therapeutic index, and high risk of respiratory depression.
Take-home points:
• Conscious sedation requires short-acting sedatives.
• Clients under conscious sedation remain responsive to verbal stimuli and maintain protective reflexes.
• Local anesthetics and long-acting sedatives are not primary choices for conscious sedation.
A patient has been admitted to the emergency department because of an overdose of an oral benzodiazepine. He is very drowsy but still responsive. The nurse will prepare for which immediate intervention?
Explanation
Benzodiazepine overdose can cause excessive sedation, respiratory depression, and impaired consciousness. In cases where the patient is still responsive but overly drowsy, the priority is to administer a specific antagonist to reverse the drug’s effects while monitoring airway and vital signs.
Rationale for correct answer:
B. Administration of flumazenil.
Flumazenil is a benzodiazepine receptor antagonist that rapidly reverses the sedative effects of benzodiazepines. It restores alertness and improves respiratory function without reversing analgesia. In an overdose situation where the client is drowsy but arousable, flumazenil is the drug of choice. However, careful monitoring is required because flumazenil may precipitate seizures in clients with benzodiazepine dependence or mixed overdoses.
Rationales for incorrect answers:
A. Hemodialysis to remove the medication.
Hemodialysis is not effective in benzodiazepine overdose because benzodiazepines are highly protein-bound and lipid-soluble, which prevents efficient removal from circulation.
C. Administration of naloxone.
Naloxone is an opioid antagonist, not effective for benzodiazepine overdose. It would be indicated only if opioid co-ingestion were suspected.
D. Intubation and mechanical ventilation.
Although airway protection is always a priority, this intervention is reserved for cases of severe respiratory depression or unresponsiveness. Since this client is still responsive, immediate intubation is unnecessary at this stage.
Take-home points:
- Flumazenil is the antidote for benzodiazepine overdose, reversing sedation and respiratory depression.
- Naloxone is only effective for opioid overdose, not benzodiazepines.
- Hemodialysis is ineffective in benzodiazepine overdose due to protein binding and lipid solubility.
An older adult has been given a benzodiazepine for sleep induction, but the night nurse noted that the patient was awake most of the night, watching television and reading in bed. The nurse documents that the patient has had which type of reaction to the medication?
Explanation
Benzodiazepines are often prescribed for short-term treatment of insomnia due to their sedative and hypnotic effects. However, in some cases, especially in older adults, these drugs can produce the opposite of the intended response, resulting in increased alertness, agitation, or restlessness instead of sedation.
Rationale for correct answer:
C. Paradoxical.
A paradoxical reaction occurs when a drug produces an effect opposite to what is expected. Instead of sedation, some clients—most commonly older adults—experience insomnia, agitation, or heightened alertness after benzodiazepine administration. Recognizing this helps the nurse identify an abnormal but known drug response and report it promptly for medication reassessment.
Rationales for incorrect answers:
A. Allergic.
An allergic reaction would present with signs such as rash, itching, swelling, or respiratory distress, not with being alert or awake after receiving a sedative.
B. Teratogenic.
A teratogenic reaction involves fetal harm during pregnancy. This term does not apply to an older adult patient receiving medication for sleep.
D. Idiopathic.
Idiopathic refers to a reaction or condition with no identifiable cause. In this case, the cause is identifiable—the paradoxical effect of the benzodiazepine—so this label would not be accurate.
Take-home points:
- Older adults are at higher risk for paradoxical reactions to benzodiazepines, resulting in agitation or wakefulness.
- A paradoxical reaction is the opposite of the intended therapeutic effect.
- Recognition of paradoxical effects is critical for timely intervention and medication adjustment.
Which considerations are important for the nurse to remember when administering a benzodiazepine as a sedative-hypnotic drug? Select all that apply
Explanation
Benzodiazepines are effective sedative-hypnotics but require careful administration because of their risk for tolerance, dependence, and residual effects. Nurses must focus on timing of administration and monitoring for next-day drowsiness to maintain patient safety.
Rationales for correct answers:
C. The dose needs to be given approximately 1 hour before the patient's bedtime
Benzodiazepines should be administered close to bedtime to allow the onset of action to coincide with the patient’s intended sleep period. Giving the drug too early or too late may disrupt the intended effect.
E. The patient needs to be evaluated for the drowsiness that may occur the morning after a benzodiazepine is taken
A common adverse effect is residual sedation or “hangover effect,” which can impair alertness, coordination, and increase fall risk. Nurses must monitor and educate patients about this risk.
Rationales for incorrect answers:
A. These drugs are intended for long-term management of insomnia
This is not correct. Benzodiazepines are recommended only for short-term use due to the risks of tolerance, dependence, and withdrawal.
B. The drugs can be administered safely with other central nervous system depressants for insomnia
Combining benzodiazepines with alcohol, opioids, or other CNS depressants can cause dangerous additive effects such as severe sedation, respiratory depression, or death.
D. The drug is used as a first choice for treatment of sleeplessness
Nonpharmacologic sleep measures and non-benzodiazepine medications are preferred as first-line interventions. Benzodiazepines are generally reserved for cases where other options fail.
Take-home points:
- Benzodiazepines should be given about 1 hour before bedtime.
- Nurses must monitor for next-day drowsiness and fall risk.
- These drugs are intended for short-term use only due to dependence and tolerance.
A patient is to receive diazepam 4 mg IV push as a “now” order for sedation. The medication is available for injection with a concentration of 5 mg/mL. How many milliliters will the nurse give for this dosage?
Explanation
A patient has been prescribed diazepam 4 mg IV push for sedation. To administer this safely, the nurse must calculate the correct volume of the medication. Accurate dosage calculation is essential in IV therapy to ensure therapeutic effectiveness while preventing potential overdose or adverse effects.
Rationale for correct answer:
The problem requires determining the volume (in milliliters) of a medication solution needed to deliver a specific dose, given its concentration.
1. Identify the Known Values
- Desired Dose (D): 4mg
- Available Concentration (H): 5mg per 1mL
- Available Amount (A): 5mg
- Volume to Administer (V): 1mL
2. Use the Dosage Calculation Formula
The most common formula for this type of calculation is:
Volumetogive=AvailableAmount(H)DesiredDose(D)×Volume(V)
3. Substitute the Values into the Formula
Volumetogive=5mg4mg×1mL
4. Perform the Calculation
Volumetogive=0.8×1mL
Volumetogive=0.8mL
= The nurse will give 0.8mL of the diazepam injection.
Take-home points:
- Always use the formula: Volume to give = (Desired Dose ÷ Available Dose) × Volume, when calculating IV medication volumes.
- Verify the concentration of the solution before performing calculations to avoid medication errors.
- Administer exactly the calculated volume (in this case, 0.8 mL) to ensure safe and effective sedation.
The nurse is reviewing the prescriptions for a patient who will be discharged to home after being hospitalized for a hysterectomy. The patient asked for a sleeping pill, and the surgeon wrote a prescription for Ambien, 10 mg at bedtime as needed for sleep. What is the nurse's priority action at this time?
Explanation
Ambien (zolpidem) is a sedative-hypnotic prescribed for insomnia. While 10 mg is the standard maximum dose for adults, women should not receive more than 5 mg at bedtime because they metabolize zolpidem more slowly, leading to higher morning blood levels and increased risk of next-day drowsiness, impaired alertness, and accidents. Therefore, the nurse’s priority action is to question the prescription for safety.
Rationale for correct answer:
C. Contact the prescriber to question the dose of the Ambien.
FDA guidelines recommend a maximum of 5 mg nightly for women because of slower clearance and risk of impaired psychomotor performance the following day. The nurse must advocate for patient safety by clarifying this order with the provider before discharge.
Rationales for incorrect answers:
A. Review the potential adverse effects with the patient.
While important, patient teaching should occur after the prescription is confirmed to be safe. Providing education about an incorrect or unsafe dose does not address the immediate safety concern.
B. Suggest that the patient try drinking a glass of wine at bedtime.
This is unsafe and inappropriate. Combining alcohol with zolpidem increases the risk of severe CNS depression, respiratory depression, and accidents.
D. Assist the patient to find a pharmacy to fill the prescription on her way home.
Helping the patient fill the prescription without verifying the dose may promote unsafe medication use and put the patient at risk.
Take-home points:
- Women should not receive more than 5 mg of zolpidem nightly.
- Nurses must question potentially unsafe medication orders before discharge.
- Patient education and support come after prescription safety is ensured.
A patient who has been receiving benzodiazepines for several years was told by the nurse that this may cause which condition as a complication?
Explanation
Benzodiazepines are widely used for anxiety, insomnia, and other conditions, but long-term use can lead to dependence. When the drug is discontinued abruptly after extended use, the patient may experience withdrawal symptoms ranging from anxiety and insomnia to severe complications like tremors, agitation, and seizures. Nurses play a key role in educating patients on the importance of tapering these medications gradually.
Rationale for correct answer:
C. Withdrawal symptoms if the drug is discontinued rapidly
Long-term benzodiazepine use causes the body to adapt, and sudden cessation can trigger withdrawal syndrome. Symptoms include rebound anxiety, irritability, restlessness, insomnia, muscle tension, and in severe cases, seizures. This is why gradual tapering under medical supervision is the safest way to discontinue the drug.
Rationales for incorrect answers:
A. Symptoms of renal impairment
Benzodiazepines are primarily metabolized in the liver, not the kidneys. Renal impairment is not a common complication of long-term benzodiazepine use.
B. A rush of morning energy with repeated usage
Instead of increased morning energy, benzodiazepines can cause residual drowsiness, fatigue, or cognitive impairment, especially with prolonged use.
D. Seizures during the time that the drug is being administered
Seizures are not a complication of benzodiazepine use itself. In fact, benzodiazepines are often used to prevent or treat seizures. Seizures are more likely during withdrawal, not during active therapy.
Take-home points:
- Long-term benzodiazepine use can lead to physical dependence.
- Abrupt discontinuation may cause withdrawal symptoms, including seizures.
- Benzodiazepines must be tapered gradually under supervision to prevent complications.
The nurse is making rounds at 2 am on the unit during the night shift and notes that one of the older patients is awake. The nurse reviews the patient’s bedtime medication and sees that 5 mg of zolpidem (Ambien) was administered at 9 pm. What interventions are appropriate for the nurse to do next? Select all that apply
Explanation
Zolpidem (Ambien) is a sedative-hypnotic used for short-term management of insomnia. Older adults are prescribed lower doses (5 mg) due to slower clearance and increased sensitivity. Even so, patients may still have difficulty sleeping or show paradoxical symptoms such as agitation. The nurse must combine safe pharmacologic interventions with nonpharmacologic comfort and safety measures to promote rest.
Rationales for correct answers:
A. Repeat the dose if ordered.
If there is a valid prescription allowing a repeated dose, the nurse may administer it while ensuring it does not exceed the maximum safe dosage. This must be verified before giving an additional dose.
B. Provide patient comfort measures (e.g., back rub, quiet room).
Nonpharmacologic interventions such as reducing noise, dimming lights, and offering comfort measures can help enhance rest and improve the effectiveness of sleep aids.
C. Determine what the patient normally does at home when unable to sleep.
Asking about the patient’s home routine respects individual sleep habits and may identify strategies that help the patient fall asleep more effectively.
E. Assess for paradoxical symptoms.
Older adults may develop paradoxical reactions to zolpidem, such as increased restlessness, agitation, or confusion instead of sedation. Monitoring for these effects ensures patient safety.
F. Provide safety measures.
Sedative-hypnotics increase the risk of falls, confusion, and nighttime wandering, especially in older adults. Safety measures such as keeping the bed in a low position and ensuring the call light is within reach are essential.
Rationales for incorrect answers:
D. Keep the patient awake to prevent rebound sleep.
This is inappropriate. Forcing a patient to stay awake is unsafe and does not prevent rebound sleep; instead, it worsens sleep deprivation and agitation.
G. Turn all the lights on to keep the patient from falling asleep.
This is counterproductive. Bright lights stimulate wakefulness and prevent the patient from resting, increasing insomnia.
Take-home points:
- Zolpidem should be paired with comfort and safety measures to promote sleep in older adults.
- Nurses must assess for paradoxical reactions when sedatives are ineffective.
- Individual sleep routines should be considered alongside medication for best outcomes.
The nurse was discussing the difference between temazepam (Restoril) and zolpidem (Ambien) with a patient requesting drug therapy for sleep disturbance. Which of the following statements are appropriate? Select all that apply
Explanation
Temazepam (Restoril) is a benzodiazepine, while zolpidem (Ambien) is a nonbenzodiazepine sedative-hypnotic. Both are used for insomnia, but they differ in structure, mechanism, and adverse effect profiles. Patient teaching should emphasize short-term use, proper tapering of benzodiazepines, and available formulations.
Rationales for correct answers:
A. “When you take Restoril, it can cause rebound insomnia if you abruptly stop taking it without tapering the drug.”
Abrupt discontinuation of benzodiazepines like temazepam can lead to rebound insomnia, where sleep disturbances return worse than baseline. Gradual tapering is recommended to avoid this complication.
C. “Ambien is also available in a sublingual tablet form, which disintegrates in seconds.”
Zolpidem is available in sublingual formulations (e.g., Intermezzo) for rapid onset, particularly for patients who wake during the night. This provides an alternative to oral tablets and allows more flexible dosing.
E. “Ambien is used for short-term treatment of insomnia.”
Zolpidem is intended for short-term management, generally 7–10 days, to reduce the risk of dependence, tolerance, and next-day sedation.
Rationales for incorrect answers:
B. “There is no difference between these drugs; you can take them without any worries.”
Temazepam and zolpidem differ in drug class, mechanism, and risks, including dependence potential, tapering needs, and next-day sedation.
D. “The side effect of morning drowsiness is only caused by Restoril, not Ambien.”
Morning drowsiness can occur with both drugs, especially in older adults or if zolpidem is taken too close to waking.
Take-home points:
- Temazepam requires tapering to prevent rebound insomnia.
- Zolpidem is short-acting and available in sublingual form for rapid sleep onset.
- Both drugs carry a risk of next-day sedation and should be used short-term.
The nurse taking care of a patient who was admitted for an overdose of lorazepam (Ativan) knows which antidote will be used?
Explanation
Lorazepam is a benzodiazepine, and in cases of overdose, patients may experience excessive sedation, respiratory depression, and CNS depression. Flumazenil is a specific benzodiazepine antagonist that reverses these effects by competitively inhibiting benzodiazepine binding at the GABA-A receptor. Nurses must monitor closely for reversal of sedation and potential withdrawal or seizures after administration.
Rationale for correct answer:
C. Flumazenil
Flumazenil rapidly reverses benzodiazepine-induced sedation by blocking benzodiazepine activity at GABA-A receptors. It is used cautiously because it can precipitate withdrawal seizures in patients with long-term benzodiazepine use. Continuous monitoring of vital signs, airway, and neurological status is required.
Rationales for incorrect answers:
A. Fluvoxamine
Fluvoxamine is a selective serotonin reuptake inhibitor (SSRI) used for obsessive-compulsive disorder; it does not reverse benzodiazepine overdose.
B. Temazepam (Restoril)
Temazepam is a benzodiazepine hypnotic. Administering another benzodiazepine would worsen CNS depression, not reverse it.
D. Selegiline (Zelapar)
Selegiline is a MAO-B inhibitor used for Parkinson’s disease and depression; it has no role in benzodiazepine overdose.
Take-home points:
- Flumazenil is the antidote for benzodiazepine overdose.
- Monitor for seizures and withdrawal symptoms after administration.
- Supportive care, including airway and vital sign monitoring, is essential during reversal.
The nurse is monitoring laboratory results for a patient who has been taking quazepam (Doral) for several years. The following laboratory values on the patient’s chart are considered elevated; indicate with an X the ones that would alert the nurse to possible hepatotoxicity or blood dyscrasias.
Explanation
The nurse is monitoring a patient who has been taking quazepam (Doral), a long-acting benzodiazepine, for several years. Chronic use of certain medications can sometimes contribute to hepatotoxicity or blood dyscrasias. Careful monitoring of laboratory values helps identify the early signs of liver injury or hematologic complications. This allows prompt nursing interventions to prevent serious adverse effects.
Rationale for correct answers:
- AST (aspartate aminotransferase): Elevated AST is a marker of hepatocellular injury. Long-term use of medications metabolized by the liver, including quazepam, can increase AST levels, indicating potential liver toxicity.
- ALP (alkaline phosphatase): Elevated ALP may indicate cholestasis or liver dysfunction, which can occur with prolonged drug therapy. Monitoring this value helps detect liver injury early.
- ALT (alanine aminotransferase): ALT is another sensitive marker of hepatocellular damage. Persistent elevations suggest hepatotoxicity, requiring evaluation of medication effects on liver function.
- Platelets: A low platelet count indicates thrombocytopenia, which is a type of blood dyscrasia. Long-term medication use may suppress bone marrow, so monitoring is important.
- WBC (white blood cells): Abnormal WBC levels suggest leukopenia or other hematologic issues, which can result from drug-induced bone marrow suppression. Monitoring helps prevent infection risk.
- PT/INR (prothrombin time/international normalized ratio): Prolonged PT/INR reflects impaired liver synthesis of clotting factors, which can result from hepatotoxicity. This value is critical for assessing liver function. Clinically, this also represents a blood dyscrasia, because the patient becomes predisposed to excessive bleeding or hemorrhage even from minor injuries or invasive procedures.
Take-home points:
- Regular monitoring of liver function tests is essential for patients on long-term benzodiazepines.
- Monitor hematologic parameters to detect blood dyscrasias early.
- Early identification of abnormal lab values allows timely intervention, such as adjusting or discontinuing the medication, to prevent serious complications.
It is important for the nurse teaching the patient regarding secobarbital (Seconal) to include which information about the drug?
Explanation
When teaching a client about secobarbital (Seconal), it is essential to emphasize that this drug is a short-acting barbiturate used primarily for sedation and preoperative anesthesia. Because of its short duration of action, secobarbital may cause the client to fall asleep quickly but awaken early in the morning, which limits its effectiveness for maintaining sleep throughout the night.
Rationale for correct answer:
A.It is a short-acting drug that may cause one to awaken early in the morning:
Secobarbital is a short-acting barbiturate with a duration of about 3–4 hours. While it is effective for sleep induction, its short half-life means clients may experience early morning awakening and incomplete rest. This characteristic differentiates it from intermediate- and long-acting barbiturates.
Rationales for incorrect answers:
B. It is an intermediate-acting drug that frequently causes REM rebound:
Secobarbital is not intermediate-acting; it is short-acting. While REM rebound can occur with withdrawal from barbiturates, this is not the defining feature of secobarbital.
C. It is an intermediate-acting drug that frequently causes a hangover effect:
The “hangover effect” of residual drowsiness and impaired alertness is more typical of intermediate-acting barbiturates, not short-acting ones like secobarbital.
D. It is a long-acting drug that is frequently associated with dependence:
While barbiturates in general carry a high risk of dependence, secobarbital is not classified as a long-acting drug. Long-acting barbiturates, such as phenobarbital, are used more for seizure control than for insomnia.
Take-home points:
• Secobarbital is a short-acting barbiturate that can cause early morning awakening.
• Short-acting sedatives help induce sleep but are less effective at maintaining it.
• All barbiturates carry risks of dependence, tolerance, and withdrawal, requiring careful use.
A patient received spinal anesthesia. Which is most important for the nurse to monitor?
Explanation
When caring for a client who has received spinal anesthesia, the nurse’s priority is to monitor for hypotension and headaches, which are the most common and significant complications. Spinal anesthesia works by blocking nerve conduction in the spinal cord, leading to sensory, motor, and autonomic blockade. The autonomic block can cause vasodilation and hypotension, while leakage of cerebrospinal fluid (CSF) at the puncture site can result in a post-dural puncture headache.
Rationale for correct answer:
C. Hypotension and headaches:
Spinal anesthesia causes sympathetic nervous system blockade, leading to vasodilation, decreased venous return, and hypotension. This drop in blood pressure can compromise tissue perfusion and must be treated promptly, often with IV fluids or vasopressors. Additionally, a post-spinal headache may occur due to CSF leakage at the puncture site, which can be severe and persistent.
Rationales for incorrect answers:
A. Loss of consciousness:
Spinal anesthesia produces regional nerve blockade, not general anesthesia. Clients remain awake and conscious unless sedation is given separately.
B. Hangover effects and dependence:
These are associated with sedative-hypnotics such as barbiturates or benzodiazepines, not with spinal anesthesia.
D. Excitement or delirium:
Excitement or delirium may occur with certain general anesthetics but is not typical of spinal anesthesia, which does not act on higher brain centers directly.
Take-home points:
• The nurse must closely monitor for hypotension and post-spinal headaches after spinal anesthesia.
• Spinal anesthesia blocks autonomic, sensory, and motor function, but clients remain conscious.
• Prompt recognition and treatment of complications ensure client safety and stable recovery.
The nurse will monitor the patient who is taking a muscle relaxant for which adverse effect?
Explanation
Muscle relaxants act primarily on the central nervous system, producing generalized CNS depression rather than directly relaxing skeletal muscle fibers. This can manifest as drowsiness, dizziness, fatigue, confusion, and decreased alertness. Because of this effect, patients should be cautioned about activities requiring mental alertness, such as driving or operating heavy machinery.
Rationale for correct answer:
A. CNS depression
This is the most significant and common adverse effect of centrally acting muscle relaxants. Sedation and impaired coordination are frequent, and risk increases when combined with alcohol, opioids, or other CNS depressants.
Rationales for incorrect answers:
B. Hypertension
Muscle relaxants are not associated with causing hypertension. Some may even lower blood pressure slightly due to CNS effects.
C. Peripheral edema
Edema is not a typical adverse effect of this drug class.
D. Blurred vision
Visual disturbances are not characteristic adverse effects of muscle relaxants; CNS depression is the main concern.
Take-home points:
- CNS depression is the key adverse effect of muscle relaxants.
- Teach patients to avoid alcohol, opioids, and hazardous activities until drug effects are known.
- Sedation and dizziness are common and should be closely monitored.
A client is admitted to undergo a surgical procedure. The nurse should be aware that which of the following preexisting conditions may be a contraindication for the use of ketamine (Ketalar) as an intravenous anesthetic for this client?
Explanation
When selecting anesthetic agents, the nurse must consider the client’s medical history, potential contraindications, and the drug’s adverse effects. Ketamine (Ketalar) is a dissociative anesthetic known to cause hallucinations, confusion, and vivid dreams during emergence from anesthesia. Therefore, clients with psychiatric disorders such as schizophrenia are at increased risk of exacerbation of symptoms.
Rationale for correct answer:
D. Schizophrenia:
Ketamine is contraindicated in clients with schizophrenia or other psychotic disorders because it can worsen symptoms by stimulating the central nervous system. It acts as an NMDA receptor antagonist, which disrupts glutamate pathways and may trigger hallucinations, agitation, and psychosis. Since schizophrenia already involves disturbances in perception, thought processes, and reality testing, ketamine increases the risk of postoperative delirium or exacerbation of psychotic symptoms.
Rationales for incorrect answers:
A. Peptic ulcer disease:
Ketamine does not directly worsen peptic ulcer disease. Although it can increase secretions, this is not a contraindication. Other anesthetics, not ketamine, pose higher risks for gastrointestinal issues.
B. Breast cancer:
There is no direct contraindication between ketamine use and a history of breast cancer. Anesthetic considerations for cancer patients usually focus on prior treatments (chemotherapy, radiation) and their systemic effects, not ketamine itself.
C. Diabetes mellitus:
Diabetes requires careful monitoring of blood glucose and wound healing, but ketamine does not have specific adverse interactions with diabetes. Other anesthetic choices may need adjustment due to comorbidities, but ketamine is not contraindicated.
Take-home points:
• Ketamine may worsen psychiatric disorders such as schizophrenia by inducing hallucinations and psychosis.
• Medical history must always be reviewed before selecting anesthetic agents.
• Safe anesthetic management requires stailoring drug choice to the client’s preexisting conditions.
Exams on Drugs Used for Sedation and Sleep
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Explain the stages and functions of sleep and classify the types and duration of insomnia.
- Apply non-pharmacologic interventions, including sleep hygiene and behavioral strategies, to improve sleep quality.
- Describe the mechanisms of action and dose-dependent effects of sedative and hypnotic agents on the CNS.
- Identify the pharmacology, clinical uses, adverse effects, interactions, contraindications, and nursing considerations for benzodiazepines.
- Identify the mechanisms, indications, adverse effects, and safety monitoring of nonbenzodiazepine hypnotics such as Z-drugs and trazodone.
- Understand the pharmacology, therapeutic uses, adverse effects, and nursing considerations of antihistamines, tricyclic antidepressants, melatonin receptor agonists, orexin receptor antagonists, and herbal sedatives.
- Implement comprehensive nursing management including patient education, monitoring for adverse effects and tapering schedules.
- Evaluate the therapeutic effectiveness for all sedative-hypnotic agents.
Introduction
Overview of Sleep:
-
Sleep is a biologic and physiologic process essential for maintaining neurological, cognitive, and emotional health. It supports tissue repair, immune system function, hormonal regulation, learning, and memory consolidation.
- Adequate sleep enhances problem-solving, attention, and mood stability. Chronic sleep disturbances can increase risks of cardiovascular disease, metabolic syndrome, depression, and impaired cognition.
- Sleep occurs in cycles: non-REM (N1–N3) and REM sleep. Non-REM promotes physical restoration, while REM is critical for emotional regulation and memory consolidation. Disruption of these cycles contributes to insomnia and daytime dysfunction.
Definition of Insomnia:
-
Insomnia is characterized by difficulty falling asleep, difficulty staying asleep, or early awakening, despite adequate opportunity to sleep. It can significantly impair daily functioning, concentration, and quality of life.
- Insomnia may be primary (not linked to other disorders) or secondary (associated with medical, psychiatric, or environmental causes).
Types of Insomnia:
-
Initial Insomnia
- Difficulty initiating sleep; patient lies awake for prolonged periods.
- Often associated with stress, anxiety, depression, stimulants (caffeine, nicotine), or environmental factors.
- Teach relaxation techniques, avoid stimulating activities before bedtime, and consider short-acting sedative-hypnotics if non-pharmacologic measures fail.
- Intermittent Insomnia
- Multiple awakenings during the night, resulting in fragmented sleep.
- Common in chronic pain, restless leg syndrome, sleep apnea, or medication side effects.
- Identify underlying cause (pain management, adjusting medications). Encourage sleep environment modifications such as white noise or blackout curtains.
- Terminal Insomnia
- Early morning awakening without ability to return to sleep.
- Frequently occurs in depression, age-related circadian changes, or chronic illness.
- Evaluate for depression or circadian rhythm disorders. Consider medications with longer duration if pharmacologic therapy is indicated.
Duration-Based Classification of Insomnia:
- Transient Insomnia
- Lasts 1–2 nights. Often due to acute stress, travel (jet lag), environmental changes, or illness.
- Usually self-limiting; pharmacologic intervention is rarely required.
- Encourage sleep hygiene, relaxation, and temporary environmental adjustments.
- Short-Term Insomnia
- Less than 3 weeks; may require short-term pharmacologic management.
- Commonly caused by stress, situational changes, or temporary medical conditions.
- Assess for contributing factors and teach coping strategies. Short-acting sedative-hypnotics may be considered, with close monitoring for next-day drowsiness and dependence.
- Chronic Insomnia
- Persists longer than 3 weeks.
- Often associated with psychiatric disorders, chronic pain, medications, or underlying medical conditions.
- Comprehensive evaluation is needed; management may include cognitive-behavioral therapy, long-term pharmacotherapy, and lifestyle interventions.
Rebound Insomnia:
- Temporary worsening of sleep quality after abrupt discontinuation of sedative-hypnotics, particularly benzodiazepines and nonbenzodiazepine receptor agonists.
- Educate patients on gradual tapering to avoid rebound effects and withdrawal symptoms. Monitor for agitation, anxiety, and insomnia recurrence.
Non-Pharmacologic Nursing Interventions (Sleep Hygiene):
-
Maintain a consistent sleep-wake schedule, even on weekends.
- Limit caffeine, nicotine, and alcohol, especially in the evening.
- Ensure a quiet, cool, and dark sleep environment.
- Encourage relaxation techniques: deep breathing, meditation, progressive muscle relaxation, guided imagery, or warm baths.
- Avoid heavy meals or vigorous exercise within 2–3 hours of bedtime.
- Promote daytime physical activity to increase sleep drive at night.
- Reduce screen time from TVs, phones, or tablets at least 1 hour before bedtime.
- Consider cognitive-behavioral strategies for stress or anxiety that interfere with sleep.
Nursing Insights:
-
Assess baseline sleep patterns: total sleep time, number of awakenings, and perceived sleep quality.
- Identify contributing factors: caffeine intake, medication effects, chronic illness, psychological stressors.
- Evaluate for comorbidities that affect sleep, e.g., chronic pain, depression, heart failure, or COPD.
- Document sleep diary for 1–2 weeks to identify patterns before pharmacologic intervention.
- Educate patients on the difference between sedative and hypnotic medications: sedatives reduce anxiety, hypnotics induce sleep.

Sedative-hypnotic Therapy
Overview of Sedative-Hypnotics:
- Sedative-hypnotics are CNS depressants that are widely used in the management of anxiety, insomnia, procedural sedation, and anesthesia induction.
- Sedatives: Calm the central nervous system (CNS) and reduce anxiety or agitation at low doses without necessarily inducing sleep.
- Hypnotics: At higher doses, these medications induce sleep and are primarily used for insomnia management.
- Many medications are dose-dependent, acting as sedatives at lower doses and hypnotics at higher doses.
Major Classes:
-
Benzodiazepines (BZDs) – Enhance GABA activity → sedation, anxiolysis, muscle relaxation, anticonvulsant effects.
- Nonbenzodiazepine Sedative-Hypnotics (Benzodiazepine-like receptor agonists) – Selectively act on GABA-BZ receptors, primarily for sleep.
- Barbiturates – Less commonly used due to high tolerance, dependence, and respiratory depression risk.
- Melatonin receptor agonists – Regulate circadian rhythm.
- Orexin receptor antagonists – Reduce wakefulness and promote sleep maintenance.
- Antihistamines and Tricyclic Antidepressants – Provide mild sedation, especially for short-term insomnia.
- Herbal agents (e.g., Valerian) – Mild CNS depressants with fewer regulatory controls.
- Intravenous Anesthetics – Nonopioid and opioid agents used for anesthesia or procedural sedation.
Therapeutic Uses:
-
Anxiety disorders – BZDs are commonly prescribed for generalized anxiety and panic attacks.
- Insomnia – Short-acting agents for sleep-onset insomnia, long-acting agents for sleep-maintenance insomnia.
- Seizure disorders – Some BZDs have anticonvulsant properties (e.g., lorazepam, diazepam).
- Muscle spasm – Sedation and muscle relaxation can relieve spasticity.
- Alcohol withdrawal – BZDs help prevent seizures and agitation.
- Induction of anesthesia / procedural sedation – IV BZDs (midazolam) and IV anesthetics (propofol) used in surgical or procedural settings.
Evaluation of Effectiveness:
-
Therapeutic goals depend on indication:
- Improved sleep onset, maintenance, and daytime alertness.
- Relief of anxiety, panic attacks, or muscle spasm.
- Successful procedural sedation or induction of anesthesia.
- Prevention of seizures or withdrawal complications.
Benzodiazepines (BZDs)
Overview of Benzodiazepines:
- Mechanism of Action: Enhance GABA-A receptor activity, increasing chloride influx → hyperpolarization → CNS depression. Produces sedation, anxiolysis, anticonvulsant effects, muscle relaxation, and reduction in sleep latency.
- Pharmacokinetics: Lipophilic → rapidly crosses the blood-brain barrier. Metabolized in the liver (CYP450). Elimination varies by half-life; long-acting agents may accumulate, especially in elderly or hepatic impairment.
- Therapeutic Uses: Anxiety disorders, insomnia, seizure disorders, muscle spasms, alcohol withdrawal, pre-anesthesia sedation, panic disorder.
1. Estazolam
Pharmacology:
- Intermediate-acting BZD; enhances GABA inhibitory neurotransmission.
- Reduces sleep latency and increases total sleep time.
Uses:
- Short-term treatment of insomnia, particularly sleep maintenance issues.
Adverse Effects:
- Drowsiness, dizziness, headache, anterograde amnesia, mild hypotension, fatigue.
Contraindications / Precautions:
- Pregnancy Risk Category X, severe respiratory depression, sleep apnea, liver disease.
- Caution in elderly (risk of falls, confusion) and history of substance use disorder.
Interactions:
- Additive CNS depression with alcohol, opioids, barbiturates.
- CYP3A4 inhibitors (e.g., ketoconazole, erythromycin) can increase plasma levels → toxicity.
Clinical pearls:
- Administer 30–60 minutes before bedtime.
- Assess fall risk, cognition, and history of substance abuse.
- Educate patient to avoid alcohol or CNS depressants.
- Monitor for tolerance and dependence.
- In overdose: supportive care; Flumazenil can be used cautiously.
Clinical Tip:
- Ideal for short-term insomnia management; monitor elderly closely for next-day sedation and confusion.
2. Flurazepam
Pharmacology:
- Long-acting BZD; prolongs sleep duration by increasing total sleep time and reducing nighttime awakenings.
Uses:
- Long-term insomnia therapy, particularly sleep maintenance insomnia.
Adverse Effects:
- Daytime sedation, dizziness, lethargy, impaired psychomotor function, mild respiratory depression.
Contraindications / Precautions:
- Pregnancy Category X. Avoid in sleep apnea, respiratory depression.
- Elderly patients prone to drug accumulation → next-day drowsiness.
Interactions:
- Additive CNS depression with alcohol, opioids, barbiturates.
- Drugs that inhibit CYP3A4 may increase plasma concentration → toxicity.
Clinical pearls:
- Monitor hepatic function (long-term use).
- Educate patients about next-day drowsiness and to avoid driving.
- Encourage sleep hygiene measures alongside pharmacotherapy.
Clinical Tip:
- Due to long half-life, avoid routine use in elderly; better suited for younger adults needing sleep maintenance therapy.
3. Lorazepam
Pharmacology:
- Intermediate-acting BZD; enhances GABA-A activity. Provides sedation, anxiolysis, and anticonvulsant effects.
Uses:
- Anxiety, insomnia, pre-anesthesia sedation, acute seizure management, alcohol withdrawal.
Adverse Effects:
- Sedation, ataxia, dizziness, hypotension, paradoxical agitation, respiratory depression (especially IV).
Contraindications / Precautions:
- Pregnancy Category D. Avoid in severe respiratory insufficiency, sleep apnea.
- Use caution in renal/hepatic impairment, elderly.
Interactions:
- Additive CNS depression with alcohol, opioids.
- Caution with other CYP3A4 substrates/inhibitors.
Clinical pearls:
- Assess vital signs, fall risk, and baseline cognition.
- Flumazenil is the antidote for overdose.
- Monitor elderly for paradoxical reactions.
- Administer orally, IV, or IM depending on clinical scenario.
Clinical Tip:
- Preferred for IM administration when IV access is not available. Useful for procedural sedation or rapid anxiolysis.
4. Midazolam
Pharmacology:
- Short-acting BZD; rapid onset due to high lipophilicity.
- Produces sedation, amnesia, anxiolysis; used primarily for procedural sedation or induction of anesthesia.
Uses:
- Procedural sedation, ICU sedation, induction of anesthesia, short-term insomnia in hospital settings.
Adverse Effects:
- Respiratory depression, hypotension, paradoxical reactions, temporary amnesia.
Contraindications / Precautions:
- Pregnancy Category D. Avoid in severe respiratory disease, glaucoma, acute alcohol intoxication, status asthmaticus.
Interactions:
- Additive CNS depression with alcohol, opioids, barbiturates.
- CYP3A4 inhibitors may prolong sedative effects.
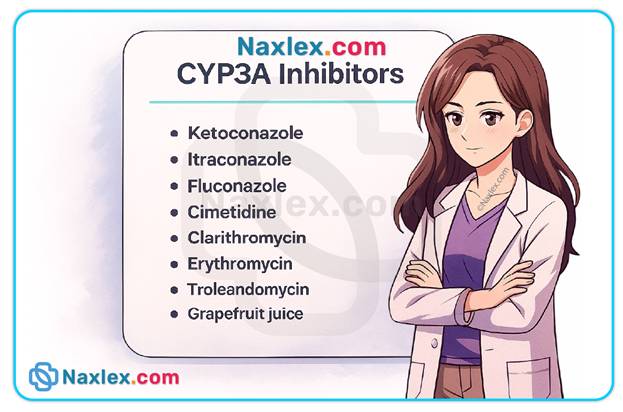
Clinical pearls:
- Continuous cardiorespiratory monitoring during IV administration.
- Ensure resuscitation equipment is available.
- Educate patient about temporary amnesia post-procedure.
Clinical Tip:
- Ideal for short procedures requiring sedation; rapid onset and short duration allow quick recovery.
5. Quazepam
Pharmacology:
- Long-acting BZD; specifically indicated for sleep maintenance insomnia.
Uses:
- Sleep maintenance insomnia; reduces nighttime awakenings.
Adverse Effects:
- Daytime drowsiness, dizziness, headache, confusion (particularly in elderly).
Contraindications / Precautions:
- Pregnancy Category X, sleep apnea, severe respiratory depression.
- Avoid in elderly or those with hepatic impairment.
Interactions:
- Additive CNS depression with alcohol or other CNS depressants.
- CYP3A4 inhibitors increase plasma concentration.
Clinical pearls:
- Monitor falls and daytime sedation, especially in older adults.
- Educate patients about tolerance and dependence risks.
- Assess liver function for prolonged therapy.
Clinical Tip:
- Suitable for patients with frequent nighttime awakenings, but use with caution in elderly due to long half-life.
6. Temazepam
Pharmacology:
- Intermediate-acting BZD; enhances GABA → sleep induction.
Uses:
- Short-term insomnia therapy; effective for sleep onset and early awakenings.
Adverse Effects:
- Drowsiness, fatigue, dizziness, paradoxical reactions, mild hypotension.
Contraindications / Precautions:
- Pregnancy Category X. Avoid in severe respiratory disorders, sleep apnea.
- Caution in elderly, renal or hepatic impairment.
Interactions:
- Additive CNS depression with alcohol, opioids, or other sedatives.
Clinical pearls:
- Administer 30–60 minutes before bedtime.
- Educate on dependence and rebound insomnia.
- Monitor renal/hepatic function for long-term use.
Clinical Tip:
- One of the safest BZDs for short-term insomnia; minimal next-day sedation if taken at proper dose.
7. Triazolam
Pharmacology:
- Short-acting BZD; rapid onset, primarily for sleep-onset insomnia.
Uses:
- Sleep-onset insomnia; often used for patients who have difficulty falling asleep.
Adverse Effects:
- Amnesia, dizziness, headache, rebound insomnia, paradoxical reactions.
Contraindications / Precautions:
- Pregnancy Category X. Avoid in sleep apnea, respiratory depression, elderly, and severe hepatic impairment.
Interactions:
- Additive CNS depression with alcohol, opioids, barbiturates.
- CYP3A4 inhibitors increase risk of toxicity.
Clinical pearls:
- Administer immediately before bedtime, ensuring 7–8 hours of sleep opportunity.
- Avoid abrupt discontinuation → risk of rebound insomnia.
- Monitor elderly for falls, confusion, memory impairment.
Clinical Tip:
- Rapid onset makes it ideal for patients with difficulty falling asleep, but short half-life can lead to early awakening; educate patient on timing.
Nursing Insights for Benzodiazepines:
-
Safety first: Assess cognition, fall risk, respiratory status, and baseline liver/renal function.
- Taper gradually: Avoid abrupt discontinuation to prevent rebound insomnia and withdrawal.
- Flumazenil: Antidote for BZD overdose (IV only); monitor closely for seizures and resedation.
- Elderly caution: Higher sensitivity → start low, go slow; monitor for confusion and daytime sedation.
- Patient education: Avoid alcohol and other CNS depressants; take at prescribed time; ensure sufficient sleep opportunity.
- Monitor effectiveness: Improvement in sleep latency, total sleep time, and daytime alertness.
Nonbenzodiazepine Sedative-hypnotics
Overview:
- Often called “Benzodiazepine-like receptor agonists” or “Z-drugs”, they act selectively at the GABA-A receptor complex.
- Produce sedation without significant anxiolytic, muscle relaxant, or anticonvulsant effects typical of benzodiazepines.
- Lower risk of tolerance, dependence, and next-day sedation compared to BZDs.
- Mainly used for insomnia—both sleep-onset and sleep-maintenance.
General:
- Administer immediately before bedtime with at least 7–8 hours of planned sleep.
- Monitor for complex sleep behaviors (sleepwalking, sleep-driving, cooking, or phone use while asleep).
- Avoid alcohol or other CNS depressants.
- Use cautiously in elderly or patients with renal/hepatic impairment.
1. Eszopiclone (Lunesta)
Pharmacology:
- Binds selectively to GABA-A receptor subtypes (α1, α2, α3, α5), enhancing inhibitory neurotransmission.
- Reduces sleep latency and increases total sleep time; helps maintain sleep throughout the night.
Uses:
- Long-term management of sleep-onset and sleep-maintenance insomnia.
Adverse Effects:
- Bitter aftertaste, headache, dizziness, somnolence, mild memory impairment.
- Rare: complex sleep behaviors, hallucinations.
Contraindications / Precautions:
- Pregnancy Category C; caution in breastfeeding.
- Avoid in severe hepatic impairment or severe respiratory disease.
- Use cautiously in elderly (risk of falls, confusion).
Interactions:
- Additive CNS depression with alcohol, opioids, or other sedatives.
- CYP3A4 inhibitors (ketoconazole, clarithromycin) can increase plasma levels → toxicity.
Clinical pearls:
- Administer immediately before bedtime.
- Educate patient to avoid driving or operating machinery after use.
- Monitor for next-day sedation, confusion, or unusual sleep behaviors.
- Encourage sleep hygiene practices alongside pharmacotherapy.
Tips:
- Only non-BZD hypnotic approved for long-term use (>6 months) with lower risk of tolerance.
2. Zaleplon (Sonata)
Pharmacology:
- Ultra-short-acting GABA-A receptor agonist.
- Primarily reduces sleep latency; minimal effect on sleep maintenance.
Uses:
- Sleep-onset insomnia.
- Useful for middle-of-the-night awakenings if at least 4 hours of sleep are planned.
Adverse Effects:
- Headache, mild drowsiness, dizziness, nausea.
- Rare: complex sleep behaviors (sleep-driving, sleep-eating).
Contraindications / Precautions:
- Pregnancy Category C; contraindicated in breastfeeding.
- Caution in elderly, hepatic or renal impairment.
Interactions:
- Additive CNS depression with alcohol, opioids, barbiturates.
- CYP3A4 inhibitors can increase plasma concentration → increased sedation.
Clinical pearls:
- Administer immediately before bedtime or middle-of-night dose only if 4+ hours of sleep remain.
- Educate patient on avoiding alcohol or other CNS depressants.
- Monitor elderly for falls, dizziness, confusion.
Tips:
- Best choice for patients who need to fall asleep quickly but do not have issues staying asleep.
3. Zolpidem (Ambien)
Pharmacology:
- Selective GABA-A α1 receptor agonist; promotes sleep initiation and maintenance.
- Short-acting but newer extended-release formulations provide longer sleep duration.
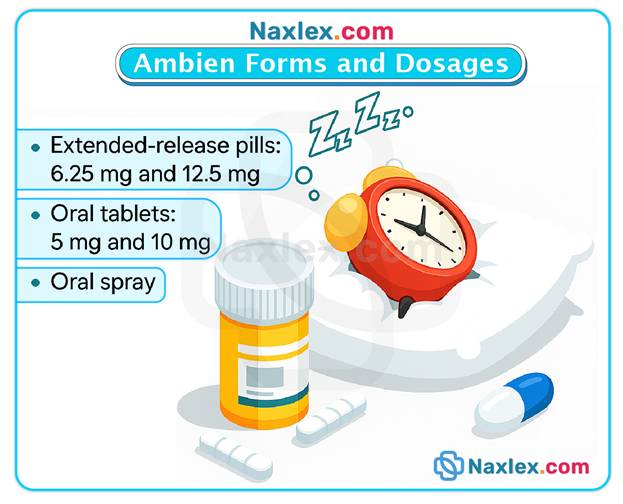
Uses:
- Sleep-onset insomnia; extended-release forms for sleep-maintenance insomnia.
Adverse Effects:
- Daytime drowsiness, dizziness, headache, amnesia, complex sleep behaviors (sleep-driving, sleep-eating).
- Rare: hallucinations, depression exacerbation.
Contraindications / Precautions:
- Pregnancy Category C; avoid breastfeeding.
- Severe hepatic impairment, respiratory insufficiency, sleep apnea.
- Elderly: start at low doses due to risk of next-day sedation.
Interactions:
- CNS depressants (alcohol, opioids, barbiturates) → additive sedation.
- CYP3A4 inhibitors can increase risk of toxicity.
Clinical pearls:
- Administer immediately before bedtime.
- Educate patient on sleep behaviors without awareness.
- Monitor for morning grogginess and dizziness, especially in elderly.
- Avoid driving or operating machinery the next day if residual sedation persists.
Tips:
- Consider low-dose extended-release for patients with frequent nighttime awakenings.
- Educate about risk of complex sleep behaviors, particularly with alcohol or sedatives.
4. Trazodone (Oleptro)
Pharmacology:
- Atypical antidepressant with sedative properties at low doses; serotonin receptor antagonist and reuptake inhibitor.
- Blocks H1 histamine and α1-adrenergic receptors → sedation.
Uses:
- Off-label management of insomnia, especially sleep-maintenance insomnia.
- Sometimes used in patients with depression and concurrent insomnia.
Adverse Effects:
- Sedation, dizziness, orthostatic hypotension, dry mouth, nausea.
- Rare: priapism, arrhythmias, serotonin syndrome (if combined with other serotonergic agents).
Contraindications / Precautions:
- Pregnancy Category C; avoid breastfeeding.
- Caution in cardiovascular disease, elderly, and patients taking other serotonergic drugs.
Interactions:
- CNS depressants → additive sedation.
- MAO inhibitors → risk of serotonin syndrome.
- CYP3A4 inhibitors may increase plasma concentration.
Clinical pearls:
- Administer 30–60 minutes before bedtime.
- Monitor blood pressure, cardiac status, and mental status.
- Educate patients to rise slowly from bed to avoid orthostatic hypotension.
- Use caution with concurrent antidepressants or CNS depressants.
Tips:
- Useful in patients with comorbid depression and insomnia.
- May be preferred over BZDs in elderly due to lower risk of dependence.
Nursing Insights:
-
Administration timing: Immediately before bedtime; ensure at least 7–8 hours of planned sleep.
- Monitor complex sleep behaviors: Sleep-driving, sleep-eating, or sleep-cooking can occur.
- Avoid CNS depressants: Alcohol, opioids, or other sedatives increase risk of respiratory depression and sedation.
- Elderly caution: Start with lower doses; monitor for falls, confusion, and next-day sedation.
- Effectiveness evaluation: Improvement in sleep latency, total sleep duration, and reduced nighttime awakenings.
- Patient education: Maintain sleep hygiene, avoid abrupt discontinuation, report unusual sleep behaviors.
Other Sedative-hypnotic Agents
1. Antihistamines
Common Agents: Diphenhydramine, Doxylamine
Pharmacology:
- H1 receptor antagonists → block central histamine receptors in the CNS → sedation.
- Often available over-the-counter; can cause anticholinergic effects.
Uses:
- Mild or transient insomnia.
- Short-term adjunct therapy for sleep disturbances.
- Occasionally used for allergic conditions, motion sickness, or cold symptoms.
Adverse Effects:
- Daytime sedation, dry mouth, constipation, urinary retention, blurred vision.
- Paradoxical excitation may occur in children or elderly.
Contraindications / Precautions:
- Narrow-angle glaucoma, BPH, asthma exacerbations.
- Pregnancy Category B (Diphenhydramine) and C (Doxylamine).
- Elderly: increased risk of confusion, falls, and anticholinergic toxicity.
Interactions:
- Additive CNS depression with alcohol, opioids, barbiturates, or benzodiazepines.
- Anticholinergic drugs may worsen constipation, urinary retention, or dry mouth.
Clinical pearls:
- Administer 30–60 minutes before bedtime.
- Educate patient to avoid alcohol and CNS depressants.
- Encourage hydration and fiber intake to minimize constipation.
- Monitor elderly for confusion, dizziness, and falls.
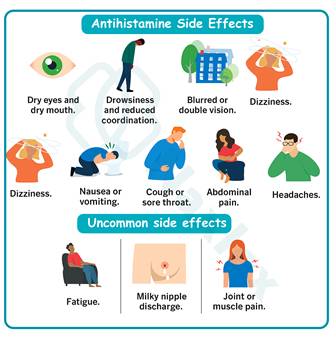
Clinical Tips:
- Useful for short-term, situational insomnia.
- Avoid chronic use due to anticholinergic side effects and tolerance development.
2. Tricyclic Antidepressant (TCA)
Agent: Doxepin
Pharmacology:
- At low doses, H1 histamine receptor antagonism → sedation.
- At higher doses, inhibits serotonin and norepinephrine reuptake → antidepressant effect.
Uses:
- Sleep-maintenance insomnia.
- Insomnia in patients with comorbid depression.
- Occasionally used for chronic pain syndromes (off-label).
Adverse Effects:
- Drowsiness, dry mouth, constipation, urinary retention.
- Rare: cardiac conduction abnormalities, orthostatic hypotension, blurred vision.
Contraindications / Precautions:
- Recent myocardial infarction, arrhythmias, severe heart block.
- Pregnancy Category C; avoid breastfeeding.
- Caution in elderly, renal/hepatic impairment, or glaucoma.
Interactions:
- CNS depressants → additive sedation.
- MAO inhibitors → risk of hypertensive crisis.
- Alcohol → increased sedation.
Clinical pearls:
- Administer 30 minutes before bedtime.
- Monitor blood pressure, heart rate, ECG in patients with cardiac disease.
- Educate about morning grogginess; caution with driving.
- Encourage hydration and fiber intake to prevent constipation.
Tips:
- Low-dose doxepin is effective for sleep maintenance without significant antidepressant effects.
- Often preferred in elderly due to lower risk of dependence compared to BZDs.
3. Melatonin Receptor Agonists
Agents: Melatonin, Ramelteon, Tasimelteon
Pharmacology:
- Bind to MT1 and MT2 receptors in the suprachiasmatic nucleus → regulate circadian rhythm.
- Do not cause generalized CNS depression; low risk of tolerance and dependence.
Uses:
- Sleep-onset insomnia.
- Circadian rhythm disorders (shift work disorder, jet lag).
- Non-24-hour sleep-wake disorder (tasimelteon).
Adverse Effects:
- Dizziness, headache, fatigue, mild hormonal changes (decreased libido, menstrual irregularities).
- Rare: vivid dreams or next-day grogginess.
Contraindications / Precautions:
- Pregnancy and lactation (use with caution).
- Severe liver disease, depression, sleep apnea, or COPD.
- Elderly: monitor for drowsiness and dizziness.
Interactions:
- CNS depressants → additive sedation.
- High-fat meals or grapefruit juice → altered absorption (ramelteon).
- Fluvoxamine → increases ramelteon levels.
Clinical pearls:
- Administer 30 minutes before bedtime on an empty stomach.
- Educate patients to avoid alcohol and other CNS depressants.
- Evaluate effectiveness by improvement in sleep onset.
- Monitor for hormonal changes or unusual side effects.
Tips:
- Preferred for patients at risk for dependence or with sleep-onset difficulties.
- Ideal for elderly or those with mild insomnia.
4. Orexin Receptor Antagonists
Agents: Lemborexant, Suvorexant
Pharmacology:
- Block orexin neuropeptides (OX1R, OX2R) → decrease wakefulness and promote sleep initiation and maintenance.
- Novel mechanism: unlike BZDs, do not act directly on GABA receptors.
Uses:
- Insomnia characterized by difficulty staying asleep or sleep-maintenance insomnia.
Adverse Effects:
- Somnolence, headache, fatigue.
- Complex sleep behaviors (sleep-driving, sleep-eating).
- Rare: abnormal dreams, next-day drowsiness.
Contraindications / Precautions:
- Pregnancy and lactation: insufficient safety data.
- Hepatic impairment: avoid or reduce dose.
- Caution in elderly and patients with respiratory insufficiency.
Interactions:
- CNS depressants (alcohol, opioids) → additive sedation.
- CYP3A4 inhibitors (ketoconazole, itraconazole) → increased plasma levels.
Clinical pearls:
- Administer immediately before bedtime.
- Ensure patient has 7–8 hours available for sleep.
- Educate about next-day drowsiness and avoiding driving or operating machinery.
- Monitor for complex sleep behaviors.
Tips:
- Especially useful for patients who have difficulty staying asleep.
- Offers a non-GABAergic alternative to traditional hypnotics, reducing risk of dependence.
5. Herbal Medicine: Valerian
Pharmacology:
- Increases GABA availability in the CNS → mild sedative effect.
- Mechanism not fully understood; thought to modulate GABA metabolism and receptor activity.
Uses:
- Mild insomnia or adjunct therapy for sleep initiation.
- Often used by patients preferring natural remedies.
Adverse Effects:
- Headache, dizziness, gastrointestinal upset, mild daytime sedation.
- Rare: paradoxical excitation, hepatotoxicity (rare).
Contraindications / Precautions:
- Pregnancy and breastfeeding: safety not established.
- Avoid in patients with liver disease.
- Caution when combined with CNS depressants.
Interactions:
- Additive sedation with benzodiazepines, non-BZD hypnotics, opioids, or alcohol.
- May interact with anticonvulsants or anticoagulants.
Clinical pearls:
- Advise patients to avoid abrupt discontinuation.
- Monitor for drowsiness, dizziness, and GI upset.
- Encourage consistent sleep hygiene alongside herbal therapy.
- Educate about potential drug-herb interactions.
Tips:
- Often suitable for patients with mild insomnia or those wishing to avoid prescription hypnotics.
- Effects may take several days to become noticeable; not suitable for acute insomnia.
Nursing insights
-
Assess baseline sleep patterns, cognitive function, fall risk, comorbidities, and current medications.
- Implement non-pharmacologic sleep hygiene measures before pharmacologic therapy.
- Educate patients about:
- Proper timing and duration of medication use.
- Avoiding alcohol and other CNS depressants.
- Risks of complex sleep behaviors and daytime sedation.
- Monitor for adverse effects, tolerance, dependence, rebound insomnia, and interactions.
- Evaluate effectiveness: improvement in sleep onset, sleep maintenance, total sleep time, and daytime alertness.
IV Anesthetics – Nonopioid and Opioid Agents
-
Nonopioid IV anesthetics:
- Propofol: Rapid onset and short duration; used for induction and maintenance of anesthesia and procedural sedation; can cause hypotension, respiratory depression, and pain at injection site.
- Etomidate: Hemodynamically stable induction agent; preferred in patients with cardiovascular compromise; may cause adrenal suppression with prolonged use.
- Ketamine: Dissociative anesthesia; provides analgesia and sedation; preserves airway reflexes; may cause hallucinations or emergence delirium.
- Midazolam (IV): Short-acting benzodiazepine; used for procedural sedation and induction; produces amnesia, anxiolysis, and sedation; risk of respiratory depression.
- Opioid IV anesthetics:
- Fentanyl: Potent opioid; used for analgesia during anesthesia and procedural sedation; risk of respiratory depression, bradycardia, hypotension, and chest wall rigidity at high doses.
- Morphine: Less commonly used IV for anesthesia; mainly analgesic; may cause hypotension, respiratory depression, and histamine release.
- Remifentanil: Ultra-short-acting opioid; rapid onset/offset; used in procedural anesthesia; requires careful monitoring for respiratory depression and hypotension.
Nursing Insights
-
Continuous monitoring of vital signs, oxygen saturation, and level of consciousness during and after administration.
- Resuscitation equipment must be immediately available.
- Monitor for adverse effects: hypotension, bradycardia, respiratory depression, arrhythmias, or paradoxical reactions.
- Educate patients regarding temporary amnesia, sedation, and recovery period.
- Titrate doses carefully, especially in elderly, critically ill, or hemodynamically unstable patients.
Summary
1. Sleep Overview
- Sleep is essential for neurological, cognitive, emotional, and physical health.
- Occurs in cycles: non-REM (physical restoration) and REM (memory & emotional regulation).
- Chronic sleep disturbances → cardiovascular, metabolic, cognitive, and mood disorders.
2. Insomnia
- Difficulty falling asleep, staying asleep, or early awakening despite adequate opportunity.
- Types:
- Initial insomnia: difficulty initiating sleep.
- Intermittent insomnia: fragmented sleep, multiple awakenings.
- Terminal insomnia: early awakening, cannot return to sleep.
- Duration:
- Transient: 1–2 nights, often stress-related.
- Short-term: <3 weeks, may need short-term meds.
- Chronic: >3 weeks, often with medical or psychiatric causes.
- Rebound insomnia: worsened sleep after abrupt sedative-hypnotic discontinuation; taper gradually.
3. Non-Pharmacologic Interventions (Sleep Hygiene)
- Maintain consistent sleep-wake schedule.
- Avoid caffeine, nicotine, alcohol in the evening.
- Ensure quiet, cool, dark environment.
- Encourage relaxation techniques: deep breathing, meditation, guided imagery, warm baths.
- Avoid heavy meals or vigorous exercise 2–3 hours before bedtime.
- Reduce screen time before bed; promote daytime activity.
- Use cognitive-behavioral strategies for stress or anxiety.
4. Sedative-Hypnotic Therapy
- CNS depressants used for anxiety, insomnia, procedural sedation, anesthesia induction.
- Sedatives: calm CNS, reduce anxiety; Hypnotics: induce sleep at higher doses.
- Dose-dependent: low doses → sedation, high doses → hypnotic effect.
5. Major Drug Classes
- Benzodiazepines (BZDs): sedation, anxiolysis, muscle relaxation, anticonvulsant.
- Nonbenzodiazepine hypnotics (Z-drugs): selective GABA-A agonists; lower dependence.
- Barbiturates: less used; high tolerance/dependence risk.
- Melatonin receptor agonists: regulate circadian rhythm.
- Orexin receptor antagonists: reduce wakefulness, promote sleep.
- Antihistamines & TCAs: mild sedation, short-term insomnia.
- Herbal agents (Valerian): mild CNS depressants.
- IV anesthetics: procedural sedation or anesthesia induction.
6. Therapeutic Uses
- Anxiety disorders, insomnia (onset vs maintenance), seizure disorders, muscle spasm, alcohol withdrawal, procedural sedation/anesthesia.
7. Adverse Effects / Nursing Considerations
- CNS depression: monitor safety, advise no driving.
- Anterograde amnesia: monitor memory.
- Paradoxical reactions: monitor behavior.
- Respiratory depression (high dose/IV): monitor vital signs.
- Dependence/withdrawal: taper gradually.
- Acute toxicity: supportive care; Flumazenil for BZD overdose.
8. Benzodiazepines
- Enhance GABA-A → CNS depression; used for anxiety, insomnia, seizures, muscle spasm, alcohol withdrawal, pre-anesthesia.
- Short-, intermediate-, and long-acting options.
- Elderly: start low, go slow; monitor for confusion, falls, next-day sedation.
9. Nonbenzodiazepine Hypnotics (Z-Drugs & Trazodone)
- Selective GABA-A agonists; less anxiolytic/muscle relaxant effect than BZDs.
- Eszopiclone, Zaleplon, Zolpidem: sleep-onset and/or maintenance insomnia.
- Trazodone: off-label insomnia, especially with depression; lower dependence risk.
- Nursing: administer before bedtime, monitor for complex sleep behaviors, avoid CNS depressants.
10. Other Sedative-Hypnotic Agents
- Antihistamines: mild sedation; caution in elderly and anticholinergic-sensitive patients.
- TCAs (Doxepin): low-dose sedation for sleep maintenance; monitor cardiac status.
- Melatonin agonists: regulate circadian rhythm; low dependence risk.
- Orexin receptor antagonists: reduce wakefulness; avoid CNS depressants.
- Herbal (Valerian): mild insomnia; monitor for additive sedation, liver effects.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drugs Used for Sedation and Sleep
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


