Please set your exam date
The Male Reproductive System
Study Questions
Practice Questions 1
Which structure is responsible for producing male gametes?
Explanation
Testesare paired male gonads responsible for both spermatogenesisand hormone secretion. The process of spermatogenesis occurs in the seminiferous tubules, where germ cells develop into mature spermatozoa over approximately 64 days. Sertoli cells support sperm development, while Leydig cells secrete testosterone (normal serum total testosterone in adult males: 300–1,000 ng/dL). Sperm production requires normal scrotal temperature (~35–36 °C), adequate luteinizing hormone (1.24–7.8 IU/L), and follicle-stimulating hormone (1.5–12.4 IU/L).
Rationale for correct answers
B.The testes contain seminiferous tubules, which directly produce male gametes (spermatozoa) through spermatogenesis. The question asks specifically about the structure producing male gametes, making testes the direct and scientifically correct choice.
Rationale for incorrect answers
A.The epididymis does not produce gametes; it functions as the site for sperm maturation and storage after spermatogenesis has already occurred in the testes. Sperm in the epididymis gain motility but are not formed there.
C.The prostate gland produces prostatic fluid, which contributes to seminal fluid composition, enhancing sperm motility and longevity. It has no role in the actual production of male gametes.
D.The seminal vesicles secrete fructose-rich fluid that provides an energy source for sperm. This structure is accessory to reproduction but does not produce spermatozoa.
Take home points
- Testes are the primary male gonads producing spermatozoa and testosterone.
- Epididymis stores and matures sperm but does not create them.
- Accessory glands contribute to semen composition, not gamete formation.
- Spermatogenesis requires optimal hormonal levels and scrotal temperature.
During penile erection, which physiological process occurs?
Explanation
Penile erectionis a neurovascular event primarily mediated by parasympathetic stimulationthrough the pelvic splanchnic nerves (S2–S4). Parasympathetic activity releases nitric oxide, activating guanylyl cyclase in smooth muscle cells and increasing cyclic guanosine monophosphate (cGMP), leading to vasodilationof penile arterioles. This increases blood flow into the corpora cavernosa while compressing venous outflow. Normal resting systolic blood pressure (90–120 mmHg) supports the hemodynamic changes. Sympathetic activity (T11–L2) primarily mediates detumescence and ejaculation rather than erection.
Rationale for correct answers
B.Parasympathetic activation via S2–S4 induces nitric oxide release, causing smooth muscle relaxation and vasodilation in penile erectile tissue, allowing engorgement with blood. This process is the primary mechanism of erection.
Rationale for incorrect answers
A.Sympathetic-induced vasoconstriction reduces arterial inflow, leading to detumescence. This is opposite to the mechanism required for initiating and maintaining penile erection.
C.Testosterone production is not suppressed during erection; instead, it remains essential for maintaining libido and normal erectile function. Hormonal suppression is unrelated to the acute hemodynamic process.
D.Urethral sphincter contraction occurs during ejaculation to prevent retrograde flow of semen into the bladder. It is not part of the mechanism initiating penile erection.
Take home points
- Penile erection is mediated by parasympathetic stimulation (S2–S4).
- Nitric oxide release causes smooth muscle relaxation and vasodilation.
- Sympathetic activity mediates ejaculation and detumescence.
- Testosterone is necessary for libido and erectile function but not acutely suppressed in erection.
Select all functions of the scrotum.
Explanation
Scrotumis an external cutaneous sachousing the testes and associated structures. Its primary functions are protectionof the testes from mechanical trauma and temperature regulationto maintain optimal spermatogenesis at 35–36 °C, slightly below core body temperature (37 °C). Temperature control occurs via the dartos and cremaster muscles, which alter scrotal surface area and testicular position. The scrotum does not directly produce hormones or store sperm, as these functions are performed by the testes and epididymis respectively.
Rationale for correct answers
A.The scrotum encases the testes within a protective sac of skin, connective tissue, and muscle layers, reducing the risk of direct mechanical injury.
C.The scrotum regulates temperature through contraction/relaxation of the dartos and cremaster muscles, ensuring an optimal testicular environment for spermatogenesis.
Rationale for incorrect answers
B.Testosterone production is a function of Leydig cells located within the testes, not the scrotum. The scrotum only houses the testes and aids in their protection and cooling.
D.Sperm maturation occurs in the epididymis, where sperm acquire motility and fertilizing capacity, not in the scrotum.
E.Mature sperm are stored in the epididymis, particularly in its tail, not in the scrotum itself.
Take home points
- The scrotum protects the testes from mechanical trauma.
- Temperature regulation by the scrotum is essential for normal spermatogenesis.
- Hormone production is a testicular function, not scrotal.
- Sperm maturation and storage occur in the epididymis, not the scrotum.
Which muscle contracts to elevate the testes in response to cold?
Explanation
Cremaster muscleis a thin skeletal musclelayer derived from the internal oblique muscle, innervated by the genital branch of the genitofemoral nerve (L1–L2). It responds to temperature changesand tactile stimulation, contracting to elevate the testestoward the body to conserve heat when ambient temperature drops. This action helps maintain testicular temperature at 35–36 °C, crucial for spermatogenesis. The cremasteric reflex can be elicited by stroking the medial thigh, causing ipsilateral testicular elevation.
Rationale for correct answers
B.The cremaster muscle elevates the testes toward the body during cold exposure, reducing heat loss and maintaining the optimal temperature for sperm production.
Rationale for incorrect answers
A.The dartos muscle is a smooth muscle in the scrotal wall that wrinkles the skin to reduce surface area and limit heat loss but does not elevate the testes.
C.The bulbospongiosus muscle surrounds the bulb of the penis and aids in ejaculation and expulsion of urine, not thermoregulation of testes.
D.The ischiocavernosus muscle compresses the crus of the penis during erection to maintain rigidity, unrelated to testicular elevation or temperature control.
Take home points
- Cremaster muscle contraction elevates testes during cold to conserve heat.
- Dartos muscle wrinkles scrotal skin to reduce heat loss.
- Both muscles work together to regulate testicular temperature for spermatogenesis.
- Optimal sperm production occurs at 35–36 °C.
The glans penis is:
Explanation
Glans penisis the expanded distal endof the corpus spongiosum, forming the sensitive, bulbous tip of the penis. It is covered by stratified squamous epithelium, normally protected by the prepuce in uncircumcised males. The glans contains numerous sensory nerve endings(especially from the dorsal nerve of the penis), making it highly sensitive to tactile stimuli. It also surrounds the external urethral orifice, facilitating semen and urine passage. The corpus spongiosum maintains patency of the urethra during erection by preventing its compression.
Rationale for correct answers
B.The glans penis is anatomically the terminal, enlarged portion of the corpus spongiosum. Its structure and location match the definition exactly.
Rationale for incorrect answers
A.The attached base of the penis is called the root, composed of the bulb and crura, not the glans.
C.The outer covering of the penile shaft is skin and superficial fascia, not the glans penis.
D.The erectile tissue surrounding the urethra is the entire corpus spongiosum, not just the glans. The glans is only its distal expansion.
Take home points
- The glans penis is the distal expansion of the corpus spongiosum.
- It contains numerous sensory nerve endings for sexual sensation.
- The corpus spongiosum surrounds and protects the urethra during erection.
- The root is the fixed base of the penis, not the glans.
Select all functions of the epididymis.
Explanation
Epididymisis a highly coiled ductsituated on the posterior aspect of each testis, connecting the efferent ductules to the vas deferens. It plays a crucial role in sperm maturation, acquiring motility and fertilizing capacity over 10–14 days. It also serves as a storage sitefor mature sperm and reabsorbs unused or defective spermatozoa. The epididymal environment maintains sperm at ~35–36 °C, optimal for viability. It does not produce testosterone or initiate spermatogenesis, which occur in Leydig cells and seminiferous tubules respectively.
Rationale for correct answers
A.The epididymis provides the environment for sperm to mature, gaining motility and the ability to fertilize.
C.Mature sperm are stored in the tail of the epididymis until ejaculation.
E.The epididymis reabsorbs sperm not ejaculated, preventing accumulation and maintaining optimal conditions for new sperm.
Rationale for incorrect answers
B.Testosterone secretion occurs in Leydig cells of the testes under LH stimulation, not in the epididymis.
D.Spermatogenesis takes place in the seminiferous tubules of the testes, not in the epididymis. The epididymis only handles post-testicular sperm handling.
Take home points
- The epididymis matures, stores, and recycles sperm.
- Spermatogenesis occurs in seminiferous tubules, not in the epididymis.
- Testosterone is produced by Leydig cells, not the epididymis.
- Sperm gain motility and fertilization capacity in the epididymis.
Practice Excercise 2
Which cells produce testosterone in the testes?
Explanation
Leydig cellsare interstitial endocrine cellslocated between the seminiferous tubules of the testes. They produce testosteronein response to luteinizing hormone(LH) from the anterior pituitary. Normal serum total testosterone levels in adult males range from 300–1,000 ng/dL. Testosterone is essential for development of male secondary sexual characteristics, maintenance of spermatogenesis, libido, and anabolic functions. LH secretion is regulated by gonadotropin-releasing hormone (GnRH) from the hypothalamus via negative feedback from circulating testosterone levels.
Rationale for correct answers
B.Leydig cells synthesize and secrete testosterone under LH stimulation. They are located in the interstitial space, separate from the seminiferous tubules where spermatogenesis occurs.
Rationale for incorrect answers
A.Sertoli cells are found within seminiferous tubules and support spermatogenesis by nourishing developing sperm and producing androgen-binding protein, not testosterone.
C.Spermatogonia are germ cells that undergo mitotic and meiotic divisions to produce spermatozoa, not steroid hormones.
D.Myoid cells are contractile cells surrounding seminiferous tubules, aiding movement of sperm and testicular fluid, but they do not produce hormones.
Take home points
- Leydig cells are the testosterone-producing cells of the testes.
- LH stimulates Leydig cells to secrete testosterone.
- Sertoli cells support spermatogenesis but do not produce testosterone.
- Spermatogonia are precursors of sperm, not hormone producers.
The seminal vesicle fluid contains which nutrient that fuels sperm motility?
Explanation
Seminal vesicle fluidis an alkaline secretion constituting about 60–70% of semen volume, rich in fructose, prostaglandins, and clotting proteins. Fructoseserves as the primary energy substrate for sperm motility by entering glycolysis within sperm cells. Normal seminal plasma fructose concentration is approximately 11–15 mmol/L. The alkaline pH (7.2–8.0) neutralizes vaginal acidity, enhancing sperm survival. Prostaglandins promote cervical mucus thinning and induce reverse peristalsis in the female reproductive tract to aid sperm transport.
Rationale for correct answers
B.Fructose in seminal vesicle fluid is the main nutrient metabolized by spermatozoa to generate ATP for motility and fertilization capability.
Rationale for incorrect answers
A.Glucose is not the predominant sugar in seminal vesicle fluid; while sperm can metabolize glucose, seminal vesicles specifically secrete fructose as their carbohydrate source.
C.Galactose is not a major component of seminal plasma; it is not secreted by seminal vesicles and has no primary role in fueling sperm.
D.Citrate is present in prostatic fluid, functioning mainly as a pH buffer and nutrient, but is not the main motility fuel in seminal vesicle secretion.
Take home points
- Seminal vesicles secrete fructose as the primary sperm energy source.
- Fructose concentration in seminal fluid can be a marker of seminal vesicle function.
- Prostatic fluid contains citrate, not fructose.
- Alkalinity of seminal fluid helps sperm survive in acidic vaginal environment.
Which male structure secretes PSA?
Explanation
Prostate glandis a fibromuscular exocrine glandencircling the proximal urethra, located inferior to the bladder. It secretes a slightly acidic fluid (pH 6.5–6.7) containing prostate-specific antigen(PSA), citrate, and proteolytic enzymes. PSA is a serine protease that liquefies semen by breaking down seminogelin, aiding sperm motility. Normal serum PSA in healthy adult males is ≤4.0 ng/mL. PSA levels can rise in benign prostatic hyperplasia, prostatitis, and prostate cancer, making it a useful but non-specific screening marker.
Rationale for correct answers
A.The prostate gland secretes PSA into seminal fluid to facilitate semen liquefaction after ejaculation, enhancing sperm motility.
Rationale for incorrect answers
B.The bulbourethral glands (Cowper’s glands) secrete pre-ejaculatory alkaline mucus to neutralize acidic urine residues in the urethra, not PSA.
C.The seminal vesicles secrete alkaline fluid rich in fructose and prostaglandins, but they do not produce PSA.
D.The epididymis functions in sperm maturation, storage, and reabsorption of unused sperm, with no secretory role in PSA production.
Take home points
- PSA is secreted by the prostate gland into seminal fluid.
- PSA liquefies semen for improved sperm motility.
- Serum PSA is a non-specific marker for prostate disorders.
- Seminal vesicles and bulbourethral glands do not secrete PSA.
The bulbourethral glands primarily function to:
Explanation
Bulbourethral glands(Cowper’s glands) are paired exocrine glandslocated in the urogenital diaphragm, each draining into the proximal spongy urethra. They secrete an alkaline mucus-like pre-ejaculatory fluidthat neutralizes acidic urine residues in the urethra and lubricates the urethral lining. This secretion protects sperm during ejaculation by preventing acid-mediated damage and facilitating smooth passage. The alkaline pH (~7.4–8.0) of the secretion contributes to optimizing conditions for sperm viability during ejaculation.
Rationale for correct answers
B.The bulbourethral glands release alkaline mucus prior to ejaculation to neutralize urethral acidity and lubricate the passage for sperm.
Rationale for incorrect answers
A.Sperm are produced in the seminiferous tubules of the testes, not in bulbourethral glands.
C.Storage of mature sperm occurs in the tail of the epididymis, not in the bulbourethral glands.
D.Liquefaction of semen after ejaculation is mediated by PSA and other proteolytic enzymes from the prostate gland, not by bulbourethral glands.
Take home points
- Bulbourethral glands secrete alkaline mucus before ejaculation.
- Function is to neutralize urethral acidity and provide lubrication.
- Sperm production and storage occur in the testes and epididymis respectively.
- Prostate gland, not bulbourethral glands, liquefies semen post-ejaculation.
Practice Questions 3
Which hormone stimulates Leydig cells to produce testosterone?
Explanation
Luteinizing hormone(LH) is a glycoprotein hormonesecreted by the anterior pituitary in response to gonadotropin-releasing hormone(GnRH) from the hypothalamus. In males, LH specifically stimulates Leydig cellsin the interstitial tissue of the testes to produce and secrete testosterone. Normal adult male LH levels range from 1.24–7.8 IU/L, and testosterone levels range from 300–1,000 ng/dL. LH binding to Leydig cell receptors activates the cAMP–protein kinase A pathway, increasing cholesterol transport into mitochondria for steroidogenesis.
Rationale for correct answers
B.LH directly stimulates Leydig cells to synthesize testosterone, which supports spermatogenesis and male secondary sexual characteristics.
Rationale for incorrect answers
A.Follicle-stimulating hormone (FSH) acts on Sertoli cells to support spermatogenesis and produce androgen-binding protein, not testosterone.
C.GnRH from the hypothalamus regulates the anterior pituitary release of LH and FSH but does not act directly on Leydig cells.
D.Inhibin, produced by Sertoli cells, selectively inhibits FSH secretion from the anterior pituitary, with no role in testosterone synthesis.
Take home points
- LH is the direct stimulator of testosterone production by Leydig cells.
- FSH acts on Sertoli cells for spermatogenesis, not testosterone secretion.
- GnRH controls pituitary release of LH and FSH.
- Inhibin regulates FSH via negative feedback but not testosterone synthesis.
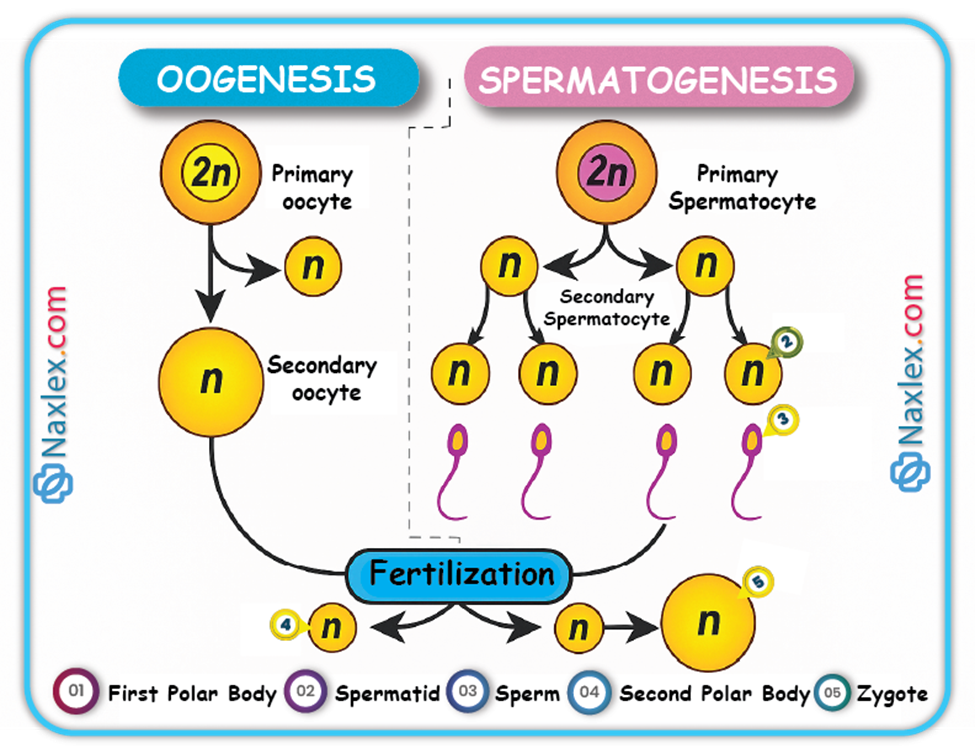
Select all correct steps in spermatogenesis.
Explanation
Spermatogenesisis the processby which diploidspermatogonia develop into haploidmature spermatozoa within the seminiferous tubules of the testes. It begins at puberty under the influence of FSH and testosterone and proceeds in three main phases: mitotic proliferation, meiotic division, and spermiogenesis. Normal sperm count is 15–259 million/mL, with motility ≥40% and morphology ≥4% normal forms. The entire process takes about 64 days.
Rationale for correct answers
A.Mitosis of spermatogonia produces primary spermatocytes, maintaining the germ cell pool and initiating spermatogenesis.
B.Formation of spermatids occurs after meiosis II, producing haploid cells ready for morphological maturation into spermatozoa.
D.Meiosis I reduces chromosome number from diploid to haploid, while meiosis II separates sister chromatids, essential for genetic diversity.
Rationale for incorrect answers
C.Ovulation is the release of an oocyte from the ovary in females and is not part of spermatogenesis.
E.Fertilization is the fusion of a sperm cell with an oocyte to form a zygote, occurring after spermatogenesis is complete.
Take home points
- Spermatogenesis occurs in seminiferous tubules and takes ~64 days.
- Involves mitosis, meiosis I & II, and spermiogenesis.
- Produces haploid spermatids that mature into spermatozoa.
- Ovulation and fertilization are not part of spermatogenesis.
Which hormone provides negative feedback to inhibit FSH secretion?
Explanation
Inhibinis a glycoprotein hormonesecreted by Sertoli cellsof the testes in males and granulosa cells of the ovaries in females. In males, inhibin selectively suppresses follicle-stimulating hormone(FSH) secretion from the anterior pituitary without significantly affecting LH. Normal adult male inhibin B levels range from 80–400 pg/mL. Its secretion is stimulated by high sperm production, providing a regulatory loop to maintain optimal spermatogenesis.
Rationale for correct answers
B.Inhibin acts directly on the anterior pituitary to reduce FSH release, thus controlling Sertoli cell stimulation and spermatogenesis rate.
Rationale for incorrect answers
A.Testosterone primarily inhibits GnRH and LH secretion via negative feedback to the hypothalamus and pituitary, not selective FSH suppression.
C.LH stimulates Leydig cells to produce testosterone and is not a negative feedback hormone.
D.GnRH stimulates the release of both FSH and LH and is not involved in negative feedback inhibition.
Take home points
- Inhibin selectively inhibits FSH secretion from the anterior pituitary.
- Sertoli cells produce inhibin in response to active spermatogenesis.
- Testosterone mainly inhibits GnRH and LH, not FSH specifically.
- Negative feedback maintains hormonal balance in spermatogenesis.
Spermiogenesis refers to:
Explanation
Spermiogenesisis the final stageof spermatogenesisin which haploidspermatids undergo morphological changes to become mature, motile spermatozoa. It does not involve cell division but structural remodeling, including condensation of nuclear chromatin, formation of the acrosome, development of the flagellum, and shedding of excess cytoplasm. Normal human sperm have a head length of ~5 µm and a flagellum length of ~50 µm, optimized for motility and fertilization.
Rationale for correct answers
B.Spermiogenesis transforms non-motile spermatids into structurally mature spermatozoa with specialized morphology for fertilization, without changing chromosome number.
Rationale for incorrect answers
A.Division of spermatogonia occurs in the mitotic phase of spermatogenesis, before meiosis, not during spermiogenesis.
C.Release of sperm into the epididymis is spermiation, which follows spermiogenesis but is a distinct process.
D.Fusion of sperm with the ovum is fertilization, occurring in the female reproductive tract after ejaculation.
Take home points
- Spermiogenesis is morphological maturation of spermatids into spermatozoa.
- No further cell division occurs during spermiogenesis.
- Distinct from spermiation, which is the release of sperm into the lumen.
- Structural adaptations optimize sperm for motility and fertilization.
Which structure is the site of spermatogenesis?
Explanation
Seminiferous tubulesare highly coiled structures within the testes where spermatogenesisoccurs. They contain Sertoli cellsfor structural and nutritional support and germ cellsat various developmental stages. Normal adult males have ~500–1,000 seminiferous tubules per testis, each ~150–300 µm in diameter. Spermatogenesis involves mitosis, meiosis, and spermiogenesis, taking about 64 days in humans.
Rationale for correct answers
B.Seminiferous tubules are the exclusive site of sperm production, containing the complete microenvironment for germ cell development under hormonal regulation by FSH and testosterone.
Rationale for incorrect answers
A.The rete testis is a network of channels that collect sperm from seminiferous tubules and transport them to the efferent ductules; no spermatogenesis occurs here.
C.The vas deferens transports mature sperm from the epididymis to the ejaculatory ducts during ejaculation; it is not a site of sperm production.
D.The epididymis stores and matures sperm but does not produce them.
Take home points
- Seminiferous tubules are the only site of spermatogenesis.
- Sertoli cells support germ cell development and secrete inhibin.
- Spermatogenesis requires FSH, testosterone, and proper temperature regulation.
- Other male reproductive structures transport or mature sperm but do not produce them.
Comprehensive Questions
A nurse is reviewing the male reproductive physiology with a group of adolescent clients. Which of the following best describes the process of spermatogenesis?
Explanation
Spermatogenesis is the process through which mature sperm cells (spermatozoa) are formed from spermatogonial stem cells in the seminiferous tubules of the testes. It involves mitosis, meiosis, and spermiogenesis. Initiated by follicle-stimulating hormone (FSH) and testosterone, spermatogenesis starts at puberty and continues throughout life. The entire process takes approximately 64 to 74 days. Normal sperm concentration ranges from 15 to 259 million/mL, with a total motility above 40% considered normal.
Rationale for correct answers
D. The entire process of sperm formation is termed spermatogenesis. It encompasses the mitotic division of spermatogonia, meiotic division of spermatocytes, and the morphological transformation of spermatids into spermatozoa. The question asked what best describes the full process, and this choice covers all stages comprehensively.
Rationale for incorrect answers
A. This choice describes only the first phase of spermatogenesis—mitotic division of spermatogonia to form primary spermatocytes. It does not include meiosis or spermiogenesis, hence it is incomplete and does not capture the entire process.
B. Division of spermatocytes to form secondary spermatocytes refers specifically to meiosis I, where primary spermatocytes divide. This is just a middle phase of spermatogenesis and not the entire process, thus making it an incomplete representation.
C. Structural changes of spermatids is called spermiogenesis, a late phase in spermatogenesis. While important, it is just one step and does not include the earlier mitotic or meiotic divisions, so it cannot define spermatogenesis as a whole.
Take home points
- Spermatogenesis is the complete process of sperm production from stem cells to mature spermatozoa.
- It includes mitosis, meiosis, and spermiogenesis occurring in the seminiferous tubules.
- Hormones involved include FSH and testosterone.
- It differs from spermiogenesis, which only involves morphological maturation of spermatids.
A nurse is teaching a male adolescent client about reproductive system function. Which of the following statements by the nurse accurately reflects the primary function of the scrotum?
Explanation
Scrotal thermoregulation ensures proper spermatogenesis, which requires temperatures approximately 2°C to 4°C (3E.6°F to 39.2°F) below core body temperature. The scrotum, a cutaneous outpouching of the anterior abdominal wall, protects the testes and maintains optimal testicular temperature via the dartos and cremaster muscles. Impaired temperature regulation can reduce sperm motility, increase DNA fragmentation, and compromise fertility. Normal testicular volume is between 12 to 30 mL per testis, and optimal semen pH ranges from 7.2 to 8.0.
Rationale for correct answers
B. The scrotum’s main function is to maintain the testes at a temperature lower than core body temperature to facilitate optimal spermatogenesis. The dartos muscle contracts to reduce surface area during cold, and the cremaster muscle elevates the testes, bringing them closer to the body, helping maintain thermoregulation within the ideal range.
Rationale for incorrect answers
A. Sperm are not stored in the scrotum. Instead, mature sperm are stored and matured in the epididymis, which lies along the posterior aspect of the testis. The scrotum itself does not serve as a storage site.
C. The scrotum does not play a role in sperm deposition. That function is carried out by the penis during ejaculation. The scrotum is a protective and thermoregulatory structure, not one involved in reproductive tract entry.
D. Spermatogenesis occurs within the seminiferous tubules of the testes, which are housed inside the scrotum, but the scrotum itself does not initiate or carry out spermatogenesis. Its role is to maintain the correct environment for the testes, not to perform the process.
Take home points
- The scrotum’s primary function is to regulate testicular temperature for effective spermatogenesis.
- Spermatogenesis occurs in the seminiferous tubules of the testes, not in the scrotum.
- Sperm maturation and storage occur in the epididymis, not the scrotum.
- Temperature elevation impairs sperm production and quality.
A nurse is educating a male client about the function of his reproductive system. Which of the following cells are primarily responsible for the production of testosterone?
Explanation
Testosterone production is regulated by luteinizing hormone (LH) acting on Leydig cells located in the interstitial tissue of the testes. These endocrine cells secrete testosterone, which is essential for spermatogenesis, development of secondary sexual characteristics, and libido. Normal serum testosterone levels in adult males range from 300 to 1000 ng/dL. Peak levels occur in early morning hours and decline with age. Testosterone exerts negative feedback on the hypothalamic-pituitary-gonadal axis, reducing both LH and follicle-stimulating hormone (FSH).
Rationale for correct answers
C. Leydig cells are the interstitial endocrine cells of the testes responsible for testosterone synthesis. They respond to LH stimulation and produce testosterone, which is essential for the maintenance of spermatogenesis and male secondary sexual traits.
Rationale for incorrect answers
A. Sertoli cells are located within the seminiferous tubules and support the maturation of developing sperm. They produce inhibin and androgen-binding protein but do not produce testosterone. Their function is regulated primarily by FSH, not LH.
B. Spermatogenic cells are germ cells that undergo mitosis and meiosis to form mature spermatozoa. These cells are dependent on the hormonal support of testosterone but are not involved in hormone production themselves.
D. Efferent ductules are part of the male reproductive ductal system that transport sperm from the rete testis to the epididymis. They play no role in endocrine function or hormone production.
Take home points
- Leydig cells synthesize testosterone in response to LH.
- Sertoli cells support spermatogenesis and secrete inhibin.
- Spermatogenic cells undergo cellular division, not hormone production.
- Testosterone regulates libido, muscle mass, and spermatogenesis.
A client asks a nurse about the function of the fluid produced by the bulbourethral glands. Which of the following is the most accurate explanation?
Explanation
Bulbourethral gland secretion plays a critical role in urethral pH regulation and lubrication during sexual arousal. The Cowper’s glands, located inferior to the prostate, secrete a clear, mucous-like fluid that neutralizes acidic urine residue in the penile urethra and provides lubrication for sperm transport. This secretion precedes ejaculation and protects sperm from damage. Normal semen pH ranges from 7.2 to 8.0, and optimal sperm motility requires this alkaline environment.
Rationale for correct answers
B. The bulbourethral glands secrete a pre-ejaculate fluid that serves to neutralize residual acidic urine in the urethra, creating an alkaline path for sperm passage. This secretion also lubricates the penile urethra, reducing friction and aiding sperm viability during ejaculation.
Rationale for incorrect answers
A. Fructose is secreted by the seminal vesicles, not the bulbourethral glands. Seminal fluid provides an energy source for sperm via fructose, but this is unrelated to bulbourethral gland function.
C. Coagulation of semen is facilitated by fibrinogen-like proteins in seminal vesicle fluid. This process helps semen temporarily coagulate post-ejaculation, but the bulbourethral glands are not involved in this mechanism.
D. Prostate-specific antigen (PSA) is secreted by the prostate gland, not the bulbourethral glands. PSA helps liquefy semen after coagulation to enable sperm motility, which occurs post-ejaculation.
Take home points
- Bulbourethral gland fluid neutralizes urethral acidity and provides lubrication.
- Fructose in semen comes from seminal vesicles, not bulbourethral glands.
- PSA is a prostate secretion, not from bulbourethral glands.
- Semen coagulation and liquefaction involve different glandular secretions.
A nurse is reviewing the components of semen analysis with a client. The nurse explains that the seminal vesicles contribute a significant amount of fluid to semen, which contains fructose. What is the primary purpose of fructose in semen?
Explanation
Sperm maturation occurs in the epididymis, a highly coiled duct located along the posterior aspect of each testis. Spermatozoa produced in the seminiferous tubules are non-motile and incapable of fertilization until they pass through the epididymis, where they undergo biochemical and structural changes over a period of approximately 12 to 21 days. Mature sperm gain progressive motility and fertilizing capacity. Normal sperm motility should be ≥40%, and normal transit time through the epididymis ranges between 2 to 14 days, depending on frequency of ejaculation.
Rationale for correct answers
B. The epididymis is the primary site for sperm maturation and acquisition of motility. Immature sperm enter the head of the epididymis from the rete testis and progressively mature as they transit through the body and tail. This process is critical for sperm to acquire the ability to swim and fertilize an ovum.
Rationale for incorrect answers
A. The vas deferens functions as a transport conduit, carrying mature sperm from the epididymis to the ejaculatory ducts. It does not contribute to sperm maturation or motility development but is crucial during ejaculation.
C. The seminal vesicles secrete fructose-rich fluid contributing to semen volume and energy supply but do not play a role in sperm storage or maturation. Their function is exocrine, contributing fluid post-sperm maturation.
D. The ejaculatory ducts are short ducts formed by the union of the vas deferens and seminal vesicles. They pass through the prostate and open into the urethra. Their role is purely conductive, with no involvement in sperm development or motility acquisition.
A nurse is teaching a group of nursing students about the process of spermatogenesis. Which of the following is the correct sequence of cell development in the seminiferous tubules?
Explanation
Spermatogenesis is the complex, multistep process by which diploid spermatogonia develop into mature haploid spermatozoa within the seminiferous tubules. This involves sequential mitotic, meiotic, and morphological changes. The process begins at puberty and is regulated by follicle-stimulating hormone (FSH) and testosterone. Normal sperm concentration ranges from 15 to 259 million/mL, and a complete spermatogenic cycle lasts approximately 64 to 74 days in humans.
Rationale for correct answers
B. Spermatogenesis starts with spermatogonia (2n), which divide mitotically to form primary spermatocytes (2n). These undergo meiosis I to form secondary spermatocytes (n), which then undergo meiosis II to form spermatids (n). Spermatids undergo spermiogenesis to become spermatozoa (n). This sequence accurately reflects normal germ cell development.
Rationale for incorrect answers
A. This sequence is completely reversed. Spermatids are late-stage cells that arise after secondary spermatocytes, and spermatogonia are the original stem cells. Spermatozoa are the final product and cannot come before early precursors like spermatogonia or primary spermatocytes.
C. This option presents an illogical and incorrect developmental order. Spermatogonia precede primary spermatocytes, and spermatids cannot arise before secondary spermatocytes. The order of cell types is out of physiological sequence.
D. This is a reverse sequence starting with the final cell type (spermatozoa) and moving backward to the stem cells (spermatogonia). It does not represent the developmental chronology of spermatogenesis within the seminiferous epithelium.
Take home points
- Spermatogonia are the stem cells initiating spermatogenesis.
- Primary and secondary spermatocytes result from meiotic division.
- Spermatids mature into spermatozoa through spermiogenesis.
- Spermatozoa are the final, motile cells capable of fertilization.
A nurse is educating a male client about the importance of scrotal temperature regulation for sperm production. Which of the following muscles is primarily responsible for pulling the testes closer to the body to conserve heat?
Explanation
Scrotal thermoregulation is vital for maintaining the optimal temperature required for normal spermatogenesis, which occurs 2°C to 4°C (3E.6°F to 39.2°F) below core body temperature. The cremaster muscle, a skeletal muscle derived from the internal oblique, elevates the testes in response to cold, physical stimulation, or threat. This action reduces heat loss, supporting sperm viability. Normal testicular volume is 12 to 30 mL, and normal semen motility requires temperatures below 35°C (95°F) to prevent DNA damage and impaired motility.
Rationale for correct answers
B. The cremaster muscle contracts reflexively to elevate the testes toward the abdominal wall in response to cold temperatures or tactile stimulation, conserving heat and optimizing the temperature for spermatogenesis. This reflex is especially active in cold environments and is essential for protecting sperm development.
Rationale for incorrect answers
A. The dartos muscle is a layer of smooth muscle in the scrotal wall that contracts to wrinkle the scrotal skin, reducing surface area and minimizing heat loss. However, it does not pull the testes upward toward the body like the cremaster muscle.
C. The bulbospongiosus muscle is a perineal muscle involved in emptying the urethra after urination and aiding ejaculation. It has no role in thermoregulation or testicular elevation.
D. The ischiocavernosus muscle compresses the crus of the penis and helps maintain erection. It is unrelated to testicular temperature regulation and has no influence on scrotal positioning.
Take home points
- The cremaster muscle elevates testes to conserve heat.
- Dartos muscle wrinkles the scrotum to reduce heat loss.
- Perineal muscles like bulbospongiosus are not involved in thermoregulation.
- Proper scrotal temperature is critical for healthy sperm production.
A nurse is teaching an anatomy class about the external male genitalia. Which of the following are components of the penis? Select all that apply
Explanation
Penile anatomy includes specialized erectile tissues, vascular structures, and sensory regions that function in urination, copulation, and ejaculation. The penis is composed of two corpora cavernosa and one corpus spongiosum, all enveloped in dense connective tissue. The glans penis, an extension of the corpus spongiosum, houses numerous sensory receptors. Normal penile erection involves vasodilation and blood filling of erectile tissues, with typical penile length in erect state ranging from 1B.9 to 1E.5 cm and penile arterial systolic velocity >30 cm/s indicating normal erectile function.
Rationale for correct answers
A. The corpora cavernosa are paired cylindrical erectile tissues located dorsolaterally in the penis. They are primarily responsible for penile rigidity during erection by engorging with blood via deep penile arteries.
C. The glans penis is the bulbous distal end of the penis, formed by the expansion of the corpus spongiosum. It is richly innervated and plays a key role in tactile sensation and sexual stimulation.
E. The corpus spongiosum is a single midline erectile structure surrounding the urethra. It prevents urethral compression during erection and expands distally to form the glans penis, contributing to both structure and function.
Rationale for incorrect answers
B. The rete testis is not a penile structure. It is a network of interconnecting tubules located in the mediastinum testis, responsible for collecting sperm from seminiferous tubules and transporting it to the epididymis. It has no structural or functional association with the penis.
D. The corpus luteum is a temporary endocrine structure formed from the ruptured ovarian follicle after ovulation in females. It secretes progesterone and estrogen. It is exclusive to the female reproductive system and unrelated to male genital anatomy.
Take home points
- The penis consists of corpora cavernosa, corpus spongiosum, and glans penis.
- Rete testis is located within the testes, not the penis.
- Corpus luteum is a female ovarian structure, not present in males.
- Erectile tissues are essential for penile rigidity and reproductive function.
A nurse is explaining the composition of semen to a client. Which of the following are components secreted by the prostate gland? Select all that apply
Explanation
Prostatic fluid composition is a critical component of semen, contributing to its biochemical environment and fertility function. The prostate gland secretes a milky, slightly acidic fluid (pH range: F.5–F.7) rich in proteolytic enzymes, citrate, and antimicrobial proteins. These substances aid in sperm motility, semen liquefaction, and infection prevention. Normal total semen pH ranges from 7.2 to 8.0, but prostatic fluid alone is slightly acidic, counterbalancing alkaline seminal vesicle secretions. It forms approximately 25% of semen volume and plays a crucial role in reproductive efficiency.
Rationale for correct answers
B. Citrate is a key metabolic intermediate in the prostatic fluid. It serves as a buffering agent and provides nutrients that support sperm metabolism and motility. Its concentration in prostatic fluid is high and is used clinically as a marker for prostate function.
D. Proteolytic enzymes, especially prostate-specific antigen (PSA), break down seminogelin and other coagulated proteins in semen. This promotes semen liquefaction after ejaculation, facilitating sperm motility. Normal PSA serum levels are <D.0 ng/mL; elevated levels suggest prostate pathology.
E. Seminalplasmin is an antimicrobial protein secreted by the prostate that inhibits bacterial growth in the male and female reproductive tracts. It contributes to the immune defense of semen and reduces the risk of ascending infections.
Rationale for incorrect answers
A. Fructose is not secreted by the prostate gland. It is produced by the seminal vesicles and functions as the primary energy source for sperm motility. It is an alkaline fluid component and helps balance the acidity of prostatic secretions.
C. Prostaglandins are produced by the seminal vesicles, not the prostate. They stimulate smooth muscle contractions in the female reproductive tract to help propel sperm toward the oocyte. They also contribute to inflammatory modulation in the reproductive system.
Take home points
- Prostatic fluid contains citrate, PSA, and seminalplasmin.
- Seminal vesicles produce fructose and prostaglandins.
- PSA aids in semen liquefaction by breaking down coagulated proteins.
- Seminalplasmin helps reduce microbial contamination of semen.
A nurse is providing an overview of the human reproductive system to a group of high school students. Which of the following are key functions of the reproductive system? Select all that apply
Explanation
Reproductive system function involves the generation and support of gametes, secretion of essential hormones, and coordination of structures for fertilization. The system includes gonads, ducts, accessory glands, and external genitalia, all of which coordinate to ensure gamete production, transport, and hormonal regulation. Major hormones such as testosterone in males (normal range: 300–1,000 ng/dL) and estrogen in females (estradiol normal range: 30–400 pg/mL, depending on phase) regulate secondary sexual characteristics, libido, and reproductive organ development.
Rationale for correct answers
B. The reproductive system's primary role includes the production of gametes: spermatozoa in males and ova in females. This function is performed by the testes and ovaries, respectively, through spermatogenesis and oogenesis.
C. Gametes must be transported and stored effectively to allow for fertilization. In males, sperm are transported through the vas deferens and stored temporarily in the epididymis. In females, ova travel via the fallopian tubes where fertilization occurs.
E. The reproductive system produces sex hormones such as testosterone, estrogen, and progesterone, which are essential for the development of secondary sexual characteristics like facial hair, breast development, voice changes, and body fat distribution.
Rationale for incorrect answers
A. Regulation of blood pressure is primarily governed by the renin-angiotensin-aldosterone system (RAAS), autonomic nervous system, and kidneys, not the reproductive system. While reproductive hormones can influence vascular tone indirectly, they are not central to blood pressure homeostasis.
D. Regulation of body temperature is the function of the hypothalamus in the brain, using mechanisms such as sweating, vasodilation, and shivering. The reproductive system is not directly responsible for thermoregulation, though testes rely on cooler temperatures (~2–4°C below body temp) for spermatogenesis.
Take home points
- The reproductive system produces, stores, and transports gametes.
- Sex hormones regulate secondary sexual features and reproductive organ development.
- The hypothalamus and kidneys control body temperature and blood pressure, not reproductive structures.
- Gametogenesis occurs in gonads—testes in males and ovaries in females.
A nurse is preparing a presentation on male reproductive physiology. Which of the following are functions of Sertoli cells within the seminiferous tubules? Select all that apply
Explanation
Sertoli cell function is central to spermatogenesis and testicular immune privilege. Located within seminiferous tubules, Sertoli cells regulate the development and protection of germ cells, form the blood-testis barrier, and secrete regulatory proteins. They produce inhibin, which inhibits follicle-stimulating hormone (FSH), and express androgen-binding protein to maintain high testosterone concentration locally. Serum FSH normal range is A.5–1B.4 mIU/mL in males, and inhibin B normally ranges between 80–400 pg/mL. Sertoli cells do not produce testosterone; Leydig cells do.
Rationale for correct answers
B. Sertoli cells form the blood-testis barrier using tight junctions. This barrier prevents autoimmune reactions by isolating developing sperm from systemic circulation and shields them from harmful substances.
D. Sertoli cells provide metabolic support, secrete nutrients, and phagocytose residual cytoplasm from developing spermatids. They also maintain a controlled environment for germ cell differentiation.
E. Sertoli cells secrete inhibin B in response to FSH stimulation. Inhibin provides negative feedback to the anterior pituitary to regulate FSH secretion and thus maintain spermatogenic homeostasis.
Rationale for incorrect answers
A. Testosterone is not secreted by Sertoli cells. It is synthesized by Leydig cells located in the interstitial tissue of the testes in response to luteinizing hormone (LH). Normal serum testosterone in males is 300–1,000 ng/dL.
C. Sertoli cells do not produce spermatozoa. They facilitate and support spermatogenesis, but spermatozoa are derived from spermatogonia through mitotic and meiotic divisions involving primary and secondary spermatocytes and spermatids.
Take home points
- Sertoli cells form the blood-testis barrier via tight junctions.
- They secrete inhibin, which negatively regulates FSH release.
- They nourish and support germ cell maturation but do not form sperm.
- Testosterone is produced by Leydig cells, not Sertoli cells.
A nurse is educating a client diagnosed with low testosterone. Which of the following physiological effects are attributed to testosterone in males? Select all that apply
Explanation
Testosterone physiology in males plays a vital role in reproductive, musculoskeletal, and behavioral functions. It is primarily synthesized by Leydig cells in the testes in response to luteinizing hormone (LH). Testosterone stimulates spermatogenesis, supports muscle and bone growth, and maintains sexual behavior. Normal serum testosterone levels range between 300–1,000 ng/dL. It exerts negative feedback on the hypothalamic-pituitary-gonadal axis by reducing gonadotropin-releasing hormone (GnRH) and luteinizing hormone, but inhibin, not testosterone, primarily suppresses follicle-stimulating hormone (FSH).
Rationale for correct answers
A. Testosterone stimulates spermatogenesis indirectly by acting on Sertoli cells, which express androgen receptors. It maintains the integrity of the seminiferous epithelium and supports germ cell development.
B. Testosterone promotes anabolic effects, increasing skeletal muscle mass and bone density by stimulating osteoblast activity and muscle protein synthesis. These effects are critical during puberty and for adult male maintenance.
D. Testosterone plays a central role in regulating libido and sexual arousal in males. Low testosterone is associated with decreased sexual desire and erectile dysfunction.
Rationale for incorrect answers
C. Testosterone exerts negative feedback on the hypothalamus, suppressing GnRH secretion. Elevated testosterone levels reduce GnRH, LH, and FSH to maintain homeostasis within the hypothalamic-pituitary-gonadal axis.
E. Testosterone does not directly inhibit FSH. FSH is primarily inhibited by inhibin B, which is secreted by Sertoli cells. Testosterone mainly inhibits LH release by acting on the anterior pituitary and GnRH neurons.
Take home points
- Testosterone supports spermatogenesis through Sertoli cell stimulation.
- It promotes muscle mass and bone growth via anabolic effects.
- It is essential for maintaining male libido and sexual behavior.
- Testosterone inhibits GnRH and LH, not FSH, which is suppressed by inhibin.
A nurse is providing pre-operative education to a client considering a vasectomy. Which of the following instructions should the nurse include? Select all that apply
Explanation
Vasectomy is a surgical male contraception technique that involves ligation or occlusion of the vas deferens to prevent sperm transport from the testes to the urethra. Sperm production by seminiferous tubules continues normally, but sperm are reabsorbed in the epididymis. Post-procedure, azoospermia (absence of sperm in semen) is confirmed by semen analysis after 15 to 20 ejaculations or approximately 3 months. Normal sperm count ranges from 15 million to over 200 million/mL.
Rationale for correct answers
B. After vasectomy, sperm may remain in the distal reproductive tract. Alternative contraception is necessary until a semen analysis confirms azoospermia, typically after 12 weeks or 15–20 ejaculations.
D. Vasectomy is a permanent form of male sterilization. Though reversal is technically possible, it is not guaranteed and is considered elective microsurgery with variable success rates.
E. By cutting or sealing the vas deferens, sperm are prevented from reaching the urethra, though seminal fluid from accessory glands is still ejaculated, making semen appear normal.
Rationale for incorrect answers
A. Sterility is not immediate after vasectomy because viable sperm remain in the vas deferens distal to the ligation site. Sperm clearance requires multiple ejaculations and must be confirmed by semen analysis.
C. The epididymis is not cut in a vasectomy. The procedure specifically targets the vas deferens, the duct that transports sperm from the epididymis to the ejaculatory ducts.
Take home points
- Vasectomy does not result in immediate sterility; contraception is still needed short-term.
- The vas deferens, not the epididymis, is the surgical target.
- Azoospermia confirmation is necessary post-vasectomy.
- Sperm continue to be produced but do not reach the ejaculate.
A nurse is assessing an older male client for symptoms indicative of benign prostatic hyperplasia (BPH). Which of the following symptoms are commonly associated with BPH? Select all that apply
Explanation
Benign prostatic hyperplasia (BPH) is a nonmalignant enlargement of the prostate gland that typically occurs in aging males due to increased dihydrotestosterone (DHT) stimulation of prostatic tissue. It leads to urethral compression and bladder outlet obstruction. Common symptoms include urinary frequency, nocturia, and hesitancy. A normal prostate volume is 20–30 mL in younger men and may increase to >40 mL with BPH. Normal post-void residual urine is <50 mL in younger men and <100 mL in men >65 years.
Rationale for correct answers
B. Urinary hesitancy is a classic obstructive symptom of BPH, resulting from increased resistance to urine flow due to compression of the prostatic urethra.
C. Increased urinary frequency, especially during the day, is a common irritative symptom due to incomplete bladder emptying and detrusor overactivity secondary to obstruction.
D. Nocturia, or waking multiple times at night to urinate, is a frequent symptom of BPH caused by reduced bladder capacity and residual urine volume.
Rationale for incorrect answers
A. Painful ejaculation is not a typical symptom of BPH. It is more commonly associated with prostatitis or other inflammatory or infectious conditions of the prostate or seminal vesicles.
E. Sudden, severe scrotal pain is characteristic of testicular torsion or epididymitis, not BPH. BPH does not cause acute scrotal symptoms.
Take home points
- BPH typically presents with lower urinary tract symptoms, both obstructive and irritative.
- BPH does not cause acute pain or symptoms related to ejaculation.
- Normal prostate volume increases with age but should not impair quality of life.
- Distinguishing BPH from prostatitis and malignancy requires careful symptom evaluation.
Exams on The Male Reproductive System
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
Upon completion of these notes, the student nurse will be able to:
• Identify and describe the major anatomical structures of the male reproductive system.
• Explain the primary physiological functions of each male reproductive organ.
• Discuss the process of spermatogenesis and its hormonal regulation.
• Recognize common health issues related to the male reproductive system.
• Apply nursing insights to patient education, assessment, and care concerning male reproductive health.
Introduction
The male reproductive system is a specialized biological network that functions primarily for the propagation of the human species. Unlike systems dedicated to sustaining individual survival, its primary goal is reproduction. This requires the coordinated function of anatomical structures, physiological processes, and endocrine regulation. For nurses, a deep understanding of this system is critical in both direct patient care and health education. Male reproductive health directly influences fertility outcomes and broader family well-being.
The Reproductive System
Overview and Functions
The reproductive system consists of internal and external organs specialized for the creation and delivery of gametes and the secretion of sex hormones.
Key Functions:
• Production of Gametes:
- Males produce spermatozoa in the testes.
- Females produce ova in the ovaries.
• Production of Hormones:
- Testes secrete testosterone.
- Ovaries secrete estrogen and progesterone.
• Transportation and Storage of Gametes:
- Sperm travels via ducts and is stored in the epididymis before ejaculation.
• Copulation: Facilitates sperm delivery into the female reproductive tract.
• Nurturing Offspring (female-specific).
Nursing Insight:
Understanding reproductive function helps nurses provide accurate education on fertility, contraception, and sexually transmitted infections (STIs), and to recognize deviations from normal physiology that may indicate pathology.
Male Reproductive Structures
1.0. External Genitalia
1.1. Penis
• Organ of copulation and urination.
• Composed of two corpora cavernosa and one corpus spongiosum.
• Anatomical Parts: root, shaft, glans penis, prepuce, and urethra.
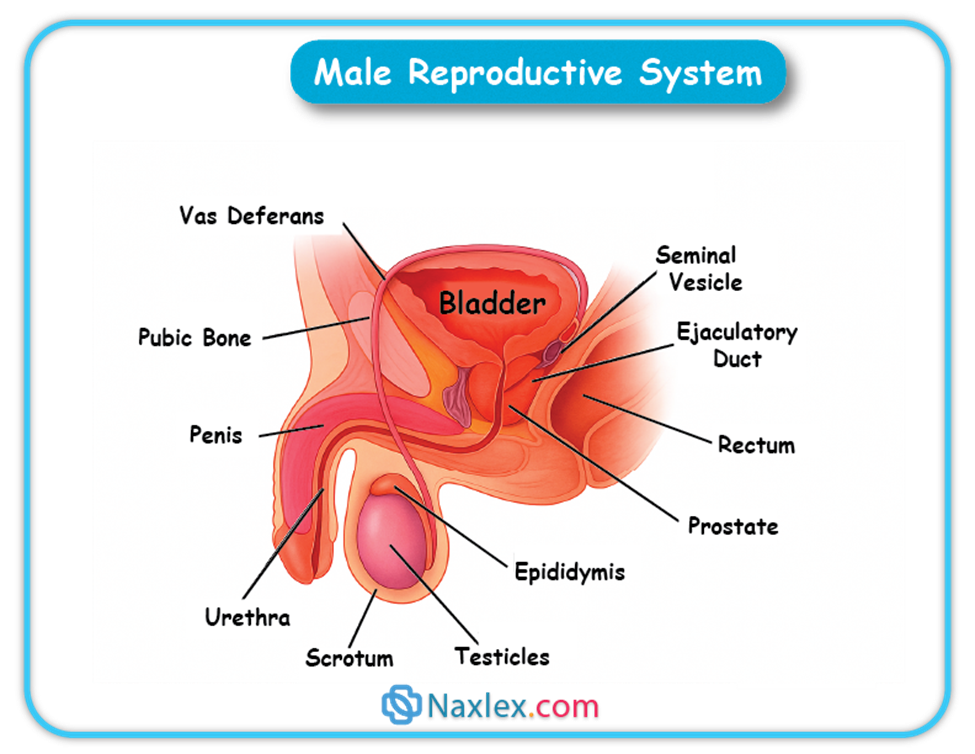
Physiology:
• Erection: Parasympathetic-induced vasodilation fills erectile tissues with blood.
• Ejaculation: Sympathetic reflex with emission and expulsion phases.
Nursing Insight:
• Educate on hygiene and foreskin care.
• Assess for lesions, discharge, or swelling as indicators of possible infection or systemic disease.
1.2 Scrotum
• Pouch of skin housing the testes.
• Contains dartos and cremaster muscles for temperature regulation.
Physiology:
• Maintains testes 2–3°C below core temperature to preserve spermatogenesis.
Nursing Insight:
• Teach testicular self-examination (TSE) for early detection of cancer.
• Advise on avoiding prolonged heat exposure to scrotum.
2.0. Internal Genitalia (Gonads and Ducts)
2.1 Testes
• Primary gonads producing sperm and testosterone.
• Contain seminiferous tubules for spermatogenesis.
• Leydig cells produce testosterone; Sertoli cells support sperm development.
Nursing Insight:
• Recognize urgent signs of testicular torsion.
• Educate on infertility risks with cryptorchidism.
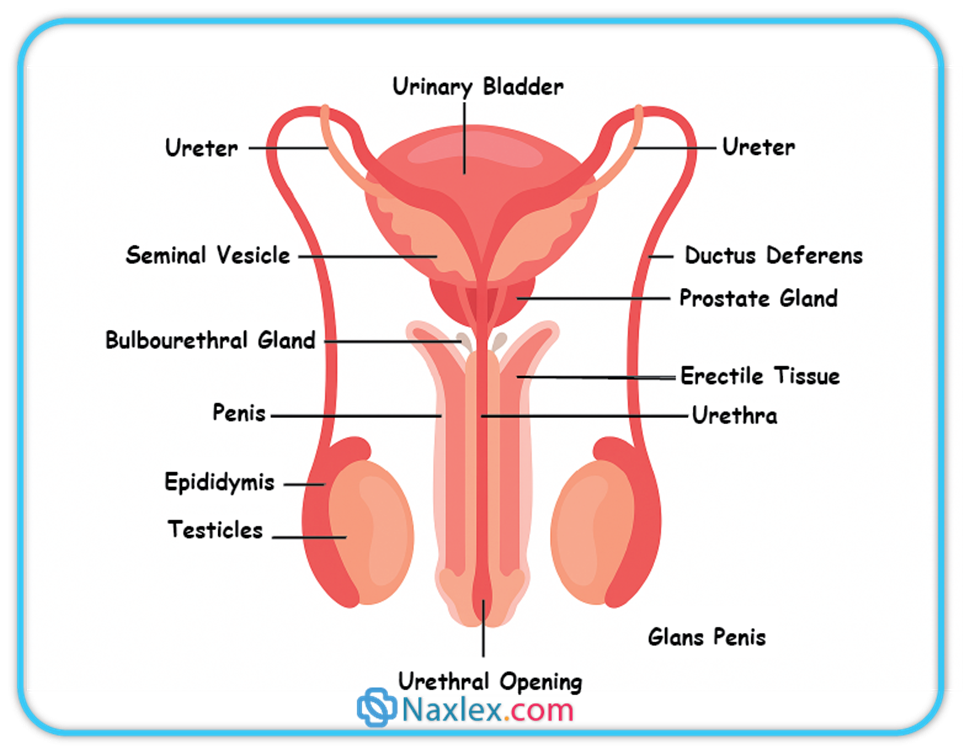
2.2 Epididymis
• Coiled duct posterior to testes.
• Stores and matures sperm over ~14 days.
2.3 Vas Deferens
• Muscular duct transporting sperm from epididymis to ejaculatory ducts.
2.4 Ejaculatory Ducts
• Formed by union of vas deferens and seminal vesicle ducts; empty into prostatic urethra.
3.0 Accessory Glands
3.1 Seminal Vesicles
• Produce alkaline, fructose-rich fluid (60% semen volume).
3.2 Prostate Gland
• Produces slightly acidic fluid with PSA and antimicrobial proteins.
3.3 Bulbourethral Glands
• Secrete alkaline mucus before ejaculation to neutralize urine and lubricate urethra.
4.0 Urethra (Male)
• Dual-function duct for urine and semen.
• Divided into prostatic, membranous, and spongy urethra.
Nursing Insight:
• UTIs in men often indicate underlying pathology such as BPH or strictures.
Spermatogenesis And Hormonal Regulation
- Spermatogenesis:
1. Mitosis of spermatogonia → primary spermatocytes
2. Meiosis I → secondary spermatocytes
3. Meiosis II → spermatids
4. Spermiogenesis → mature spermatozoa
- Hormonal Axis (HPG):
- GnRH (hypothalamus) → stimulates FSH & LH from anterior pituitary.
- FSH → acts on Sertoli cells for spermatogenesis.
- LH → stimulates Leydig cells to produce testosterone.
- Testosterone → promotes sperm production and secondary sexual characteristics.
- Inhibin (Sertoli cells) → inhibits FSH to regulate sperm production.
Nursing Insight:
• Low testosterone may cause infertility, erectile dysfunction, and reduced muscle mass.
• Educate on medication effects on fertility.
Summary Of Concepts
The male reproductive system includes external genitalia (penis, scrotum) and internal organs (testes, epididymis, vas deferens, accessory glands, urethra). The process of spermatogenesis, regulated by the HPG axis, produces sperm for reproduction. Nursing care focuses on assessment, education, and prevention of reproductive health issues.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on The Male Reproductive System
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


