Please set your exam date
Drugs Used for Depressive and Bipolar Disorders
Study Questions
Practice Exercise 1
A nurse is caring for a client who has a new prescription for phenelzine (Nardil) for the treatmentof depression. Which of the following indicates that the client has developed an adverse effect ofthis medication?
Explanation
Monoamine oxidase inhibitors (MAOIs) such as phenelzine (Nardil) are used in the treatment of depression,. While effective, they carry significant risks of side effects and drug/food interactions. One of the most notable and frequent adverse effects is orthostatic hypotension, caused by the drug’s inhibition of norepinephrine metabolism and effects on vascular tone.
Rationale for correct answer:
A. Orthostatic hypotension — This is a well-recognized and common adverse effect of phenelzine. By interfering with norepinephrine metabolism, MAOIs reduce vascular tone, leading to sudden drops in blood pressure upon standing. Monitoring and safety education (e.g., rising slowly, using support) are essential.
Rationale for incorrect answers:
B. Hearing loss — Phenelzine does not damage auditory function or cause ototoxicity. Hearing loss is unrelated to MAOI therapy and would prompt investigation for another cause.
C. Gastrointestinal bleeding — Not associated with phenelzine use. GI bleeding is a risk more relevant to NSAIDs, anticoagulants, or SSRIs due to platelet inhibition, but not to MAOIs.
D. Weight loss — Some antidepressants may affect weight, but phenelzine is more commonly associated with weight gain rather than weight loss. Thus, weight loss would not be expected as an adverse effect here.
Take-home points:
- Orthostatic hypotension is the most common cardiovascular side effect of MAOIs.
- Nurses should monitor blood pressure changes with position and educate clients on safety precautions.
- Phenelzine also carries risks of hypertensive crisis with tyramine-rich foods, requiring strict dietary teaching.
A nurse is providing teaching to a client who has a new prescription for amitriptyline (Elavil) for treatment of depression. Which of the following should the nurse include in the teaching? Select all that apply
Explanation
Amitriptyline (Elavil) is a tricyclic antidepressant (TCA) used for major depression and sometimes for neuropathic pain. TCAs are effective but have significant side effects due to their anticholinergic properties (dry mouth, constipation, blurred vision, urinary retention) and alpha-adrenergic blockade (orthostatic hypotension).
Rationale for correct answer:
C. Change positions slowly to minimize dizziness — TCAs cause orthostatic hypotension due to alpha-1 blockade. Rising slowly helps prevent dizziness, syncope, and falls.
E. Chew sugarless gum to prevent dry mouth — Dry mouth is a common anticholinergic side effect of TCAs. Chewing sugarless gum or sucking on hard candy helps relieve this discomfort.
Rationale for incorrect answers:
A. Expect therapeutic effects in 24 to 48 hr — TCAs do not work this quickly. The onset of therapeutic effects usually takes 2–4 weeks, sometimes up to 6 weeks, so this teaching would mislead the client.
B. Discontinue the medication after a week of improved mood — Abrupt discontinuation is unsafe and increases risk for withdrawal symptoms and relapse. Clients should never stop TCAs without provider guidance.
D. Decrease dietary fiber intake to control diarrhea — TCAs cause constipation, not diarrhea, because of anticholinergic effects. Clients should actually increase fiber and fluids to manage constipation.
Take-home points:
- TCAs take several weeks to show full therapeutic benefit; patience and adherence are crucial.
- Orthostatic hypotension and anticholinergic effects (dry mouth, constipation, urinary retention) are common teaching priorities.
- Nurses should reinforce safety (fall precautions) and comfort strategies (gum, fluids, fiber) in patient education.
A nurse is providing follow-up dietary teaching for a client who recently was prescribed phenelzine (Nardil). When reviewing the client’s dietary log, which of the following foods requires a need for further teaching?
Explanation
Monoamine oxidase inhibitors (MAOIs) such as phenelzine (Nardil) require strict dietary restrictions to avoid hypertensive crisis. Foods high in tyramine can trigger dangerously high blood pressure when combined with MAOIs. Common offenders include aged cheeses, smoked meats, red wine, and certain baked goods containing bananas or yeast extracts.
Rationale for correct answer:
B. Banana bread – Many banana breads contain ripe bananas and sometimes nuts or yeast extracts, which can contribute to elevated tyramine content. This poses a risk of hypertensive crisis in patients on MAOIs, making it unsafe.
Rationale for incorrect answers:
A. Cottage cheese – This dairy product is low in tyramine and considered safe in moderate amounts, unlike aged or fermented cheeses such as cheddar or blue cheese.
C. Apple pie – Apples are naturally low in tyramine, and apple pie does not typically contain problematic ingredients for patients on MAOIs.
D. Grilled steak – Freshly prepared meats are acceptable. The concern arises with aged, cured, or smoked meats, not freshly cooked options like grilled steak.
Take-home points:
- MAOIs like phenelzine require patients to avoid tyramine-rich foods to prevent hypertensive crisis.
- Fresh foods are generally safer, while aged, fermented, or overripe items are risky.
- Nurses must provide clear dietary teaching and assess food logs to reinforce safe eating habits.
A nurse is providing discharge teaching to a client who is to begin taking fluoxetine (Prozac) for posttraumatic stress disorder. Which of the following statements is appropriate for the nurse to include in the teaching?
Explanation
Fluoxetine (Prozac) is a selective serotonin reuptake inhibitor (SSRI) commonly prescribed for posttraumatic stress disorder (PTSD). While effective in improving mood, reducing anxiety, and decreasing intrusive thoughts, SSRIs are known to cause sexual dysfunction, which includes decreased libido, difficulty achieving orgasm, or erectile difficulties
A. “You may have a decreased desire for intimacy while taking this medication.”
Sexual dysfunction is one of the most common and distressing side effects of SSRIs like fluoxetine. Decreased libido can affect treatment adherence, so clients should be prepared for this possibility and encouraged to discuss concerns with the provider.
B. “You should take this medication at bedtime to help promote sleep.”
Fluoxetine can cause insomnia in patients. It is better taken in the morning to minimize sleep disturbance.
C. “You will have fewer urinary adverse effects if you urinate just before taking this medication.”
SSRIs are not associated with urinary retention or frequency issues, so this teaching is unnecessary and misleading.
D. “You’ll need to wear sunglasses when outdoors due to the light sensitivity caused by this medication.”
Photosensitivity is not a recognized adverse effect of fluoxetine; this advice applies more to medications such as tetracyclines or some antipsychotics, not SSRIs.
Take-home points:
- SSRIs like fluoxetine are first-line agents for PTSD but may cause sexual side effects, including reduced libido.
- Fluoxetine should generally be taken in the morning to avoid insomnia.
- Clients should be counseled on realistic side effects and encouraged to report bothersome symptoms to their provider.
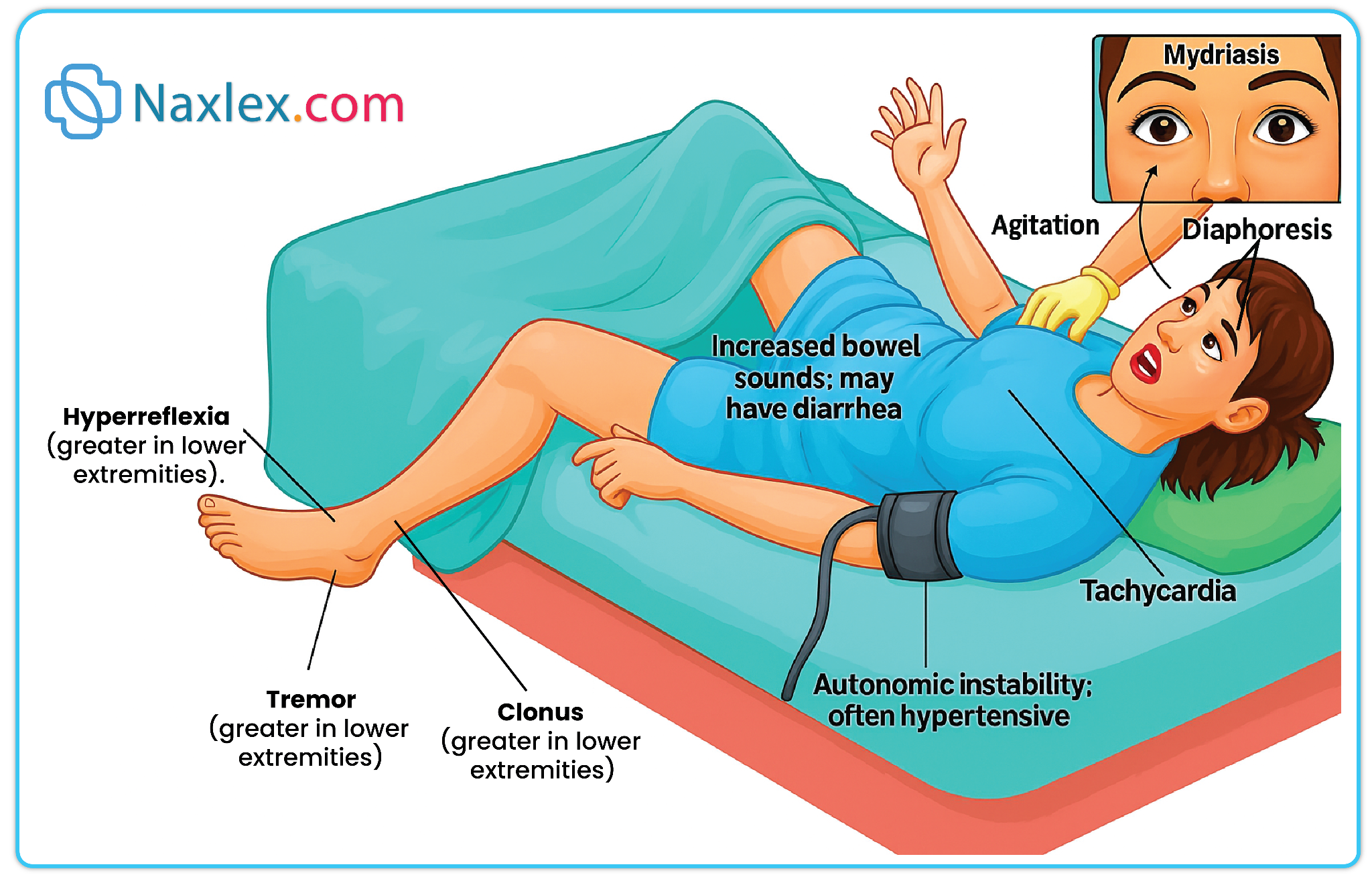
A nurse is caring for a client who has been taking sertraline (Zoloft) for the past 2 days. Which of the following assessment findings should alert the nurse to the possibility that the client is developing serotonin syndrome?
Explanation
Sertraline (Zoloft) is a selective serotonin reuptake inhibitor (SSRI) used to treat depression, PTSD, and anxiety disorders. A rare but potentially life-threatening complication of SSRIs is serotonin syndrome, which occurs when serotonin levels in the CNS become excessively high. Early recognition is essential, as symptoms can escalate quickly.
B. Fever
Hyperthermia is a hallmark of serotonin syndrome, often accompanied by autonomic instability (sweating, hypertension, tachycardia), neuromuscular changes (tremor, hyperreflexia, clonus), and altered mental status. This finding should immediately raise concern.
A. Bruising
While SSRIs can increase bleeding risk due to platelet dysfunction, bruising is not an indicator of serotonin syndrome.
C. Abdominal pain
GI upset such as nausea or diarrhea is common with SSRIs, but abdominal pain is not a defining feature of serotonin syndrome.
D. Rash
Rash is not typically associated with serotonin syndrome. It may occur with other drug reactions but is not a warning sign for serotonin toxicity.
Take-home points:
- Serotonin syndrome is a medical emergency characterized by fever, neuromuscular hyperactivity, and autonomic instability.
- Early detection is critical, especially in the first days or when combined with other serotonergic agents.
- Nurses should monitor closely and report symptoms such as hyperthermia, tremors, or confusion promptly.
Practice Exercise 2
A nurse is reviewing laboratory findings and notes that a client’s plasma lithium level is B.1 mEq/L, one hour after the previous lithium dose. Which of the following is an appropriate action by the nurse?
Explanation
Lithium is a mood stabilizer used in the treatment of bipolar disorder. The therapeutic plasma level is generally 0.6–A.2 mEq/L, with toxic effects beginning around A.5 mEq/L. A level of B.1 mEq/L indicates moderate toxicity, requiring urgent intervention to prevent life-threatening complications such as seizures, coma, and cardiovascular collapse.
A. Perform immediate gastric lavage
This is the most appropriate action for lithium toxicity at this level, as it can help remove unabsorbed lithium from the GI tract and prevent further absorption. Supportive care and monitoring should follow.
B. Prepare the client for hemodialysis
Hemodialysis is typically reserved for severe lithium toxicity (generally >B.5 mEq/L, or in patients with renal impairment or severe symptoms). At B.1 mEq/L, gastric lavage is the first intervention.
C. Administer an additional oral dose of lithium
This would worsen the toxicity and put the client at greater risk of severe complications. It is contraindicated.
D. Request a stat repeat of the laboratory test
While confirming lab results may be useful, immediate treatment should not be delayed, as the lithium level is already above therapeutic range with clear evidence of toxicity.
Take-home points:
- Lithium toxicity can occur at plasma levels greater than A.5 mEq/L; symptoms worsen with higher levels.
- Immediate gastric lavage is the first-line intervention for moderate lithium toxicity to limit absorption.
- Hemodialysis is reserved for severe toxicity (>B.5 mEq/L) or if symptoms are life-threatening.
A nurse is caring for a client who has a new prescription for lithium carbonate (Lithobid). When teaching the client about ways to prevent lithium toxicity, the nurse should advise the client to do which of the following?
Explanation
Lithium carbonate is a mood stabilizer commonly prescribed for bipolar disorder. Because it is excreted by the kidneys and competes with sodium for reabsorption, changes in fluid balance, sodium levels, and excessive sweating can increase the risk of lithium toxicity. Teaching should focus on maintaining hydration and preventing sodium depletion.
D. Limit aerobic activity in hot weather
Excessive sweating from exercise in hot weather can lead to fluid and sodium loss, increasing lithium reabsorption and risk for toxicity. Limiting intense activity in hot environments helps maintain balance.
A. Avoid the use of acetaminophen for headaches
Acetaminophen does not interact significantly with lithium and is generally safe for headache management. The risk is more with NSAIDs (e.g., ibuprofen, naproxen), which can raise lithium levels.
B. Restrict intake of foods rich in sodium
Sodium restriction can actually increase lithium reabsorption in the kidneys, raising the risk of toxicity. Clients should maintain a consistent, normal sodium intake.
C. Decrease fluid intake to less than 1,500 mL daily
Dehydration decreases renal clearance of lithium, raising serum levels and toxicity risk. Adequate hydration is essential, not restriction.
Take-home points:
- Lithium toxicity risk increases with dehydration, low sodium intake, or excessive sweating.
- Clients should maintain consistent fluid and sodium intake while on lithium.
- NSAIDs, not acetaminophen, are the main analgesics that interact with lithium.
A nurse in a primary care clinic is assessing a client who takes lithium carbonate (Lithotabs) for the treatment of bipolar disorder. The nurse should recognize which of the following findings as a possible indication of toxicity to this medication?
Explanation
Introduction:
Lithium carbonate is a mood stabilizer with a narrow therapeutic index (0.6–A.2 mEq/L). Toxicity can occur when serum levels rise above the therapeutic range. Early signs include gastrointestinal upset and fine tremors, while advanced toxicity presents with neurological changes such as coarse tremors, confusion, and seizures. Nurses must be alert for these warning signs to prevent severe complications.
B. Coarse tremors
Coarse tremors are a hallmark neurological finding of lithium toxicity, differentiating it from the mild fine tremors that may occur at therapeutic levels. This indicates that the client’s serum lithium levels are dangerously high.
A. Severe hypertension
Lithium toxicity does not typically cause hypertension. Cardiovascular effects may include dysrhythmias, but blood pressure elevations are not a common manifestation.
C. Constipation
Constipation is not a recognized symptom of lithium toxicity. Gastrointestinal signs usually include diarrhea, nausea, and vomiting instead.
D. Urinary retention
Lithium toxicity does not cause urinary retention. Polyuria and polydipsia are more common because lithium affects renal concentrating ability.
Take-home points:
- Coarse tremors signal lithium toxicity and require urgent evaluation.
- Early toxicity signs include GI upset and fine tremors, while severe toxicity leads to confusion, seizures, and coma.
- Lithium has a narrow therapeutic index; consistent monitoring and patient education on hydration and sodium intake are critical.
A nurse is caring for a client who has a new prescription for valproic acid (Depakote). The nurse should instruct the client that while taking this medication he will need to have which of the following laboratory tests completed periodically? Select all that apply
Explanation
Valproic acid (Depakote) is an anticonvulsant and mood stabilizer used in the management of seizure disorders, bipolar disorder, and migraine prophylaxis. While effective, it carries risks of significant adverse effects, including hepatotoxicity, pancreatitis, and thrombocytopenia. Regular laboratory monitoring is necessary to detect complications early and maintain client safety.
A. Thrombocyte count
Valproic acid can cause thrombocytopenia, which increases the risk of bleeding. Monitoring platelet counts helps ensure early detection of bone marrow suppression.
C. Amylase
Elevated amylase may indicate pancreatitis, a potentially life-threatening adverse effect of valproic acid. Monitoring amylase levels helps detect this complication early.
D. Liver function tests
Hepatotoxicity is a serious risk with valproic acid, especially in the first 6 months of therapy. Periodic liver function testing is essential to detect hepatic damage.
B. Hematocrit
Hematocrit monitoring is not routinely required for valproic acid therapy. It is more relevant for conditions involving anemia or blood loss.
E. Potassium
Valproic acid does not typically affect potassium levels, so monitoring serum potassium is not indicated.
Take-home points:
- Valproic acid requires monitoring of platelets, liver function, and amylase to prevent severe complications.
- The most serious risks are hepatotoxicity, pancreatitis, and thrombocytopenia.
- Routine labs like hematocrit and potassium are not necessary unless other conditions warrant.
A nurse is teaching a female client who has bipolar disorder about her new prescription for lithium carbonate (Lithobid). Which of the following is appropriate for the nurse to include in the teaching? Select all that apply
Explanation
Lithium carbonate (Lithobid) is a mood stabilizer commonly prescribed for bipolar disorder. While highly effective in reducing manic and depressive episodes, it has a narrow therapeutic index and several potential adverse effects. Safe administration requires client education about precautions, monitoring, and lifestyle considerations.
C. Take this medication with food or a glass of milk.
Taking lithium with food or milk reduces gastrointestinal upset, which is one of the most common early side effects of therapy.
D. Avoid pregnancy while taking this medication.
Lithium is teratogenic and associated with congenital heart defects, particularly Ebstein’s anomaly. Women of childbearing age should use effective contraception.
E. Thyroid function is assessed prior to lithium therapy.
Lithium can cause hypothyroidism and goiter. Baseline thyroid function testing is recommended before starting treatment and should be monitored periodically.
A. An adverse effect of this medication is amenorrhea.
Amenorrhea is not a typical adverse effect of lithium. Menstrual irregularities are more common with antipsychotics, not mood stabilizers like lithium.
B. An antidepressant is combined with lithium therapy during phases of mania.
Antidepressants are not used during mania because they can worsen manic symptoms. Lithium alone or in combination with antipsychotics is preferred in mania.
Take-home points:
- Lithium should be taken with food or milk to minimize GI distress.
- It is contraindicated in pregnancy due to teratogenic effects.
- Thyroid function testing is required before and during therapy.
Practice Exercise 3
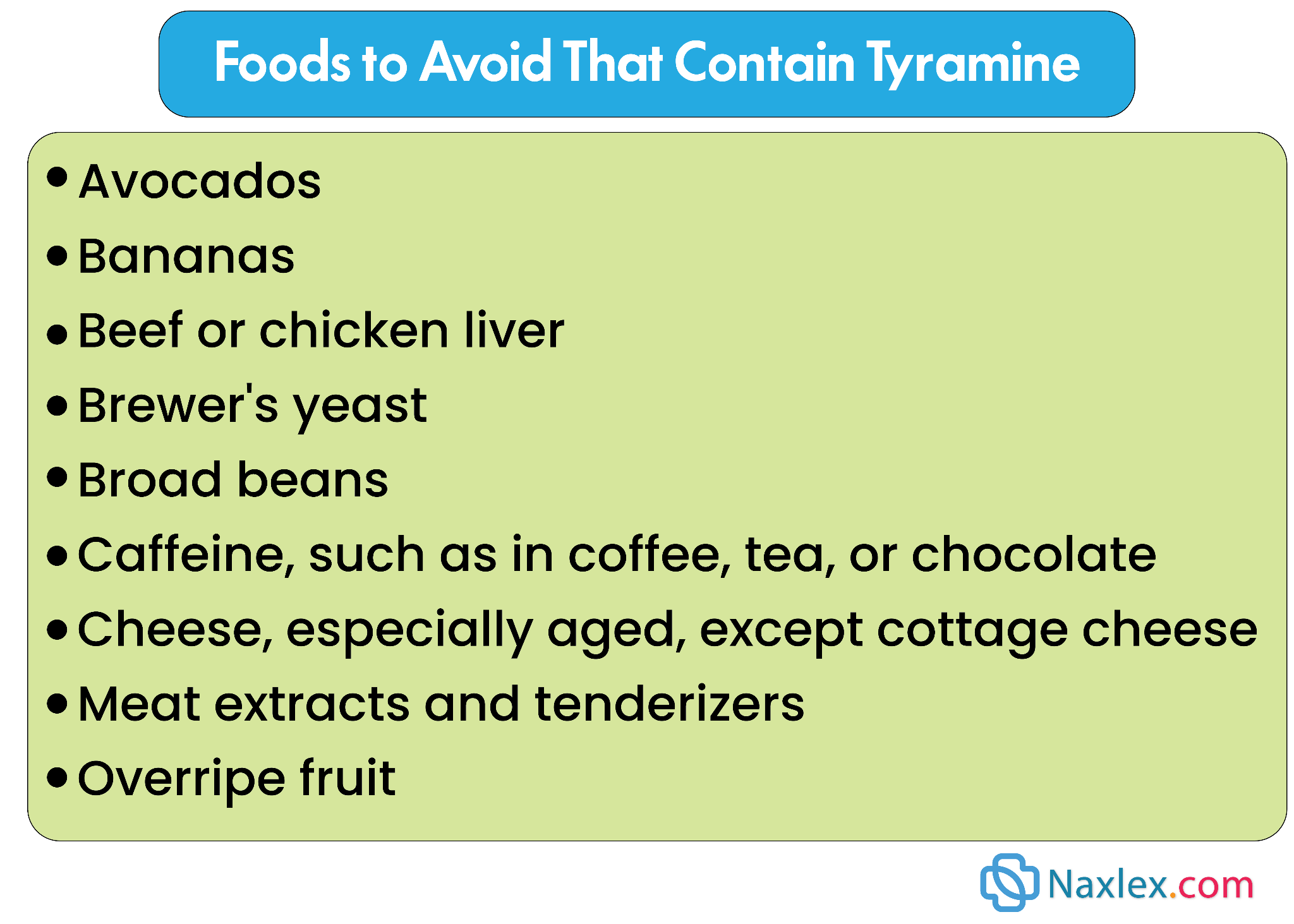
Patient teaching for a patient receiving an MAOI would include instructions to avoid which food products? Select all that apply
Explanation
Monoamine oxidase inhibitors (MAOIs), such as phenelzine (Nardil), are used to treat depression, particularly when other antidepressants have been ineffective. Because MAOIs inhibit the breakdown of tyramine, patients are at risk for hypertensive crises if they consume tyramine-rich foods. Nursing education must emphasize dietary restrictions to prevent serious cardiovascular complications.
B. Swiss cheese — Aged cheeses are high in tyramine, which can interact with MAOIs to cause a hypertensive crisis. Clients must avoid all aged, fermented, or cured cheeses.
E. Pepperoni pizza — Processed and cured meats are also high in tyramine and pose the same risk for dangerous blood pressure elevation. These foods should be avoided.
A. Orange juice — Fresh fruits and juices, including orange juice, are low in tyramine and safe to consume with MAOIs.
C. Shrimp — Fresh seafood is low in tyramine and does not interact adversely with MAOIs.
D. Milk — Fresh milk and most dairy products that are not aged or fermented are safe for clients on MAOIs.
Take-Home Points:
- Educate patients to avoid all tyramine-rich foods, including aged cheeses, cured meats, and fermented products.
- Monitor for signs of hypertensive crisis, such as severe headache, palpitations, or elevated blood pressure.
- Reinforce reading labels and checking ingredients on processed or packaged foods to avoid accidental intake of high-tyramine items.
After a patient has been treated for depression for 4 weeks, the nurse calls the patient to schedule a follow-up visit. What concern will the nurse assess for during the conversation with the patient?
Explanation
Follow-up after starting antidepressant therapy is essential to evaluate treatment effectiveness and patient safety. One critical concern during early treatment is the risk of suicidal ideation, as some patients may experience increased energy before mood improves, which can heighten the risk of acting on suicidal thoughts. Nurses must assess for any signs of self-harm during follow-up contacts.
C. Suicidal ideation — Antidepressants can increase energy and motivation before mood improves, which may place patients at higher risk for acting on pre-existing suicidal thoughts. Assessing for suicidal ideation is a priority during follow-up.
A. Weakness — While some patients may experience mild fatigue as a side effect, it is not the primary concern in early antidepressant follow-up.
B. Hallucinations — Hallucinations are not a typical adverse effect of standard antidepressant therapy and are not expected in routine follow-up.
D. Difficulty with urination — Urinary retention is uncommon with most antidepressants and is not a primary concern for early treatment monitoring.
Take-Home Points:
- Assess for suicidal thoughts or behaviors, especially within the first few weeks of therapy.
- Educate patients and families to report any sudden mood changes, agitation, or self-harm thoughts immediately.
- Schedule timely follow-ups to monitor treatment effectiveness and safety.
The nurse is teaching a patient about treatment with an SSRI antidepressant. Which teaching considerations are appropriate? Select all that apply.
Explanation
Selective serotonin reuptake inhibitors (SSRIs) are commonly prescribed for depression and anxiety. While generally safe, SSRIs can interact with other medications and herbal supplements, cause mild adverse effects, and require careful monitoring during initiation or discontinuation. Nurses play a key role in educating patients on safe use, potential interactions, and proper adherence to therapy.
B. Use caution when standing up from a sitting position — SSRIs can cause orthostatic hypotension, especially in older adults or those taking other medications affecting blood pressure. Patients should rise slowly to prevent dizziness or falls.
C. Do not take products containing St. John’s wort — Combining SSRIs with St. John’s wort can increase serotonin levels, raising the risk for serotonin syndrome, a potentially life-threatening condition.
D. Do not stop abruptly — Abrupt discontinuation of SSRIs can lead to withdrawal symptoms, such as dizziness, irritability, nausea, and flu-like symptoms. Gradual tapering under prescriber guidance is essential.
F. Check with the prescriber before taking over-the-counter medications — Many over-the-counter drugs, including decongestants and cold remedies, can interact with SSRIs or exacerbate side effects. Patient education ensures safe concurrent use.
Rationale for incorrect answer:
A. Tyramine-containing foods and 5: dehydration — These are not relevant for SSRIs; tyramine restrictions apply to MAOIs, and dehydration-related toxicity is more relevant for lithium.
Take-Home Points:
- Educate patients about orthostatic precautions and fall prevention.
- Avoid herbal supplements like St. John’s wort to reduce serotonin syndrome risk.
- Emphasize the importance of gradual discontinuation and consulting the prescriber before adding any new medications.
A patient with a feeding tube will be receiving risperidone (Risperdal) 8 mg in two divided doses via the feeding tube. The medication is available in a 1 mg/mL solution. How many milliliters will the nurse administer for each dose?
Explanation
To find the amount to administer for each dose, the nurse must first determine the amount of medication per dose, then calculate the corresponding volume.
Step 1: Calculate the dose for each administration
The patient is to receive a total of 8 mg per day, divided into two equal doses.
- Total daily dose ÷ Number of doses per day = Dose per administration
- 8mg÷2doses=4mgperdose
Step 2: Calculate the volume for each dose
The medication is available as a solution with a concentration of 1 mg per 1 mL. Use the following formula to find the volume needed for the 4 mg dose.
- Dose per administration ÷ Concentration of solution = Volume to administer
- 4mg÷1mg/mL=4mL
The nurse will administer 4 mL for each dose.
Take-home points:
- Always divide the total daily dose by the number of scheduled doses to determine the amount per administration.
- Use the formula: Dose ordered ÷ Drug concentration = Volume to administer when converting mg to mL.
Which statement is true concerning lithium?
Explanation
Lithium is a mood stabilizer used in the management of bipolar disorder, but it has a narrow therapeutic index, meaning toxicity can occur easily. Drug interactions are an important consideration in lithium therapy, particularly with NSAIDs, which can impair renal clearance of lithium and lead to elevated serum levels.
D. Concurrent NSAIDs may increase lithium levels.
NSAIDs reduce renal clearance of lithium, potentially causing toxic accumulation. This interaction requires close monitoring or avoidance of NSAIDs.
A. The maximum dose is C.4 g/d.
Lithium dosing varies based on therapeutic levels and individual response; it is titrated according to serum concentrations, not by a fixed maximum dose.
B. The therapeutic drug range is B.5 to C.5 mEq/L.
This range is toxic, not therapeutic. The therapeutic range is 0.6–A.2 mEq/L for maintenance, with levels above A.5 mEq/L considered toxic.
C. Lithium increases receptor sensitivity to GABA.
Lithium’s exact mechanism is not fully understood, but it is thought to alter sodium transport and influence neurotransmitter activity, not directly increase GABA receptor sensitivity.
Take-Home Points:
- Lithium has a narrow therapeutic index and requires regular serum monitoring.
- NSAIDs and diuretics can raise lithium levels, increasing risk of toxicity.
- Nurses must educate patients on early signs of toxicity such as tremors, confusion, and GI upset.
Comprehensive questions
A 16-year-old client has taken an overdosage of citalopram (Celexa) and is brought to the emergency department. What symptoms would the nurse expect to be present?
Explanation
Citalopram (Celexa) is a selective serotonin reuptake inhibitor (SSRI) used for depression. Overdose of SSRIs can lead to serotonin toxicity, which manifests with neurologic, autonomic, and psychiatric disturbances. The nurse must quickly recognize these symptoms to prevent complications such as seizures and cardiovascular instability.
A. Seizures, hypertension, tachycardia, extreme anxiety. SSRI overdose increases serotonin levels, leading to CNS overstimulation, autonomic instability, and neuromuscular hyperactivity. Seizures, agitation, tachycardia, and hypertension are common.
B. Hypotension, bradycardia, hypothermia, sedation.
This cluster is more consistent with CNS depressants (e.g., benzodiazepines, barbiturates, opioids), not SSRIs.
C. Miosis, respiratory depression, absent bowel sounds, hypoactive reflexes.
These are classic signs of opioid toxicity, not SSRI overdose.
D. Manic behavior, paranoia, delusions, tremors.
These findings are more associated with stimulant toxicity (e.g., amphetamines, cocaine) or untreated mania, not SSRI overdose.
Take-home points:
- SSRI overdose can lead to serotonin syndrome: seizures, hyperthermia, agitation, hypertension, and tachycardia.
- It must be differentiated from opioid and CNS depressant overdose presentations.
- Early recognition is critical because untreated serotonin toxicity can progress to life-threatening complications.
A 77-year-old female client is diagnosed with depression with anxiety and is started on imipramine. Because of this client’s age, the nurse will take precautions for care related to which adverse effects?
Explanation
Tricyclic antidepressants (TCAs) such as imipramine strongly block histamine and muscarinic receptors, leading to pronounced anticholinergic and sedative effects. In older adults, these adverse effects are magnified due to decreased drug clearance and sensitivity of the central nervous system, making fall precautions and safety interventions critical.
C. Drowsiness and sedation – TCAs have strong sedative properties from histamine receptor blockade. In elderly clients, this greatly increases fall risk, confusion, and potential injuries, making it the most important nursing precaution.
A. Dry mouth and photosensitivity – These can occur with TCAs but are not the most dangerous in older adults compared to sedation and fall risk.
B. Anxiety, headaches, insomnia – These are more common with SSRIs and SNRIs, not typically emphasized with TCAs like imipramine.
D. Urinary frequency – TCAs more often cause urinary retention due to anticholinergic effects, not increased frequency.
Take-Home Points:
- TCAs such as imipramine can cause strong sedation, especially problematic in older adults.
- Fall risk and confusion are major nursing concerns with TCAs in the elderly.
- Anticholinergic side effects are common, but sedation and safety issues take priority in this age group.
Which of the following would be a priority component of the teaching plan for a client prescribed phenelzine (Nardil) for treatment of depression?
Explanation
Phenelzine (Nardil) is a monoamine oxidase inhibitor (MAOI) used for treatment-resistant depression. The most important safety concern with MAOIs is the risk of a hypertensive crisis when foods or medications containing tyramine or sympathomimetic agents are ingested. Teaching should emphasize dietary and drug restrictions.
C. Read labels of food and over-the-counter drugs to avoid those with substances that should be avoided as directed. – This is the priority teaching point. Tyramine-containing foods (aged cheese, cured meats, wine) and many OTC medications (cold remedies, stimulants) can trigger hypertensive crisis when combined with phenelzine.
A. Headaches may occur. OTC medications will usually be effective. – OTC drugs such as decongestants can dangerously interact with MAOIs and precipitate a hypertensive crisis; this statement is unsafe.
B. Hyperglycemia may occur and any unusual thirst, hunger, or urination should be reported. – Blood sugar changes are not a major risk with phenelzine, so this teaching is not a priority.
D. Monitor blood pressure for hypotension and report any BP below 90/60. – Orthostatic hypotension may occur, but it is not as life-threatening as a hypertensive crisis, making this less critical than dietary and drug restrictions.
Take-Home Points:
- The most important teaching for clients on MAOIs is to avoid tyramine-rich foods and contraindicated OTC drugs.
- Failure to follow these precautions can lead to hypertensive crisis, a life-threatening emergency.
- Nurses should provide clients with a clear list of restricted foods and medications before discharge.
The nurse determines that the teaching plan for a client prescribed sertraline (Zoloft) has been effective when the client makes which statement?
Explanation
Sertraline (Zoloft) is a selective serotonin reuptake inhibitor (SSRI) used to treat depression, anxiety, and related disorders. A major part of teaching is helping clients understand the expected onset of action, risks with drug interactions, and the need for ongoing adherence even when results are not immediate.
C. “It may take up to a month for the drug to reach full therapeutic effects and I’m feeling better.”
– SSRIs typically require 2–4 weeks to achieve noticeable improvement in mood or anxiety symptoms, unlike benzodiazepines that act rapidly. Clients must be encouraged to continue adherence during this initial period, even if they do not feel immediate relief. Recognizing this timeline helps promote realistic expectations, better compliance, and reduced risk of early discontinuation.
A. “I should not decrease my sodium or water intake.”
– Sertraline does not require fluid or sodium restrictions. This instruction is more relevant for conditions such as hyponatremia risk or diuretic therapy, not SSRI use.
B. “The drug can be taken concurrently with the phenelzine (Nardil) that I’m taking.”
– Combining SSRIs with MAOIs is extremely dangerous because it may trigger serotonin syndrome, characterized by agitation, hyperthermia, and neuromuscular changes. At least 14 days must separate MAOI and SSRI use.
D. “There are no other drugs I need to worry about; Zoloft doesn’t react with them.”
– This is unsafe because sertraline interacts with multiple medications and supplements, including anticoagulants, other serotonergic agents, and St. John’s wort. These interactions may increase bleeding risk or precipitate serotonin syndrome.
Take-Home Points:
- SSRIs like sertraline require several weeks before full therapeutic effect is achieved.
- Concurrent use with MAOIs is contraindicated due to serotonin syndrome risk.
- Clients must be taught about drug-drug and herbal interactions to prevent serious complications.
The nurse realizes that some herbs interact with selective serotonin reuptake inhibitors. Which herb interaction may cause serotonin syndrome?
Explanation
Certain herbal supplements can dangerously interact with prescription medications. When combined with selective serotonin reuptake inhibitors (SSRIs), some herbs may increase serotonin levels, putting the patient at risk for serotonin syndrome, a potentially life-threatening condition.
C. St. John’s wort
– St. John’s wort is a popular herbal antidepressant that increases serotonin by inhibiting reuptake. When combined with an SSRI, serotonin levels can rise excessively, leading to serotonin syndrome. Symptoms include agitation, confusion, tremor, diaphoresis, hyperreflexia, and hyperthermia. This makes it the most concerning herb to avoid with SSRIs.
A. feverfew
– Feverfew is mainly used for migraine prevention. It does not increase serotonin levels significantly and is not strongly associated with serotonin syndrome when combined with SSRIs.
B. ma-huang (ephedra)
– Ephedra is a stimulant herb linked to hypertension, tachycardia, and cardiac complications. Its risk is primarily cardiovascular rather than serotonergic.
D. gingko biloba
– Ginkgo is used to improve memory and circulation. While it increases bleeding risk (especially with anticoagulants), it does not significantly elevate serotonin or interact with SSRIs to cause serotonin syndrome.
Take-Home Points:
- St. John’s wort + SSRI → serotonin syndrome risk.
- Patients should always disclose herbal supplement use to prevent drug interactions.
- Serotonin syndrome is a medical emergency requiring immediate discontinuation of serotonergic agents and supportive care.
A selective serotonin reuptake inhibitor (SSRI) is prescribed for a client. The nurse knows that which drug is an SSRI?
Explanation
Selective serotonin reuptake inhibitors (SSRIs) are a first-line treatment for depression and anxiety disorders. They act by inhibiting the reuptake of serotonin, thereby increasing its availability in the synaptic cleft and enhancing mood regulation. Knowing which drugs belong to this class is essential for safe nursing practice.
A. paroxetine (Paxil)
– Paroxetine is an SSRI, along with fluoxetine, sertraline, citalopram, and escitalopram. These drugs are widely prescribed because they are effective, well tolerated, and have fewer cardiovascular and anticholinergic effects compared to older antidepressants. Patients should be counseled that benefits may take several weeks to appear and to watch for adverse effects such as sexual dysfunction and insomnia.
B. amitriptyline (Elavil)
– Amitriptyline is a tricyclic antidepressant (TCA). TCAs work by blocking the reuptake of both serotonin and norepinephrine but are less selective than SSRIs. They carry risks of sedation, orthostatic hypotension, and anticholinergic effects (dry mouth, urinary retention, constipation).
C. divalproex sodium (Depakote)
– Divalproex is a mood stabilizer and anticonvulsant, commonly prescribed for bipolar disorder and seizure disorders. It does not act on serotonin reuptake and therefore is not classified as an SSRI.
D. bupropion HCl (Wellbutrin)
– Bupropion is an atypical antidepressant that inhibits the reuptake of dopamine and norepinephrine. It is useful in depression and smoking cessation but is not serotonergic and carries a risk of seizures at higher doses.
Take-Home Points:
- SSRIs: fluoxetine, paroxetine, sertraline, citalopram, escitalopram.
- SSRIs are first-line for depression/anxiety due to better tolerability.
- Always assess for serotonin syndrome and suicidal ideation when initiating therapy.
A patient is taking tranylcypromine sulfate (Parnate) for depression. What advice should the nurse include in the teaching plan for this medication?
Explanation
Monoamine oxidase inhibitors (MAOIs) such as tranylcypromine (Parnate) are prescribed for patients with depression who do not respond well to other antidepressants. While effective, they require careful monitoring because of their high potential for dangerous food and drug interactions. MAOIs such as tranylcypromine (Parnate) can cause hypertensive crisis when taken with foods high in tyramine. Patient education must emphasize strict dietary restrictions to prevent life-threatening complications.
B. Instruct the patient to avoid beer and cheddar cheese.
Beer, cheddar cheese, and other tyramine-rich foods can precipitate a sudden and dangerous rise in blood pressure. Patients must avoid these foods completely while on MAOIs.
A. Warn the patient about severe hypotension.
MAOIs are more likely to cause orthostatic hypotension rather than severe hypotension, but the greater safety concern is hypertensive crisis due to food-drug interactions.
C. Encourage the patient to take ginseng and ephedra.
Both ginseng and ephedra can dangerously increase blood pressure when combined with MAOIs and should be avoided.
D. Encourage the patient to eat fruit such as bananas.
Bananas contain tyramine (especially overripe ones) and should be avoided to prevent a hypertensive crisis.
Take-Home Points:
- MAOIs require strict dietary restrictions to prevent hypertensive crisis.
- Tyramine-rich foods such as aged cheese, beer, and cured meats must be avoided.
- Nurses must educate patients on drug–food and drug–herb interactions with MAOIs.
When a patient is taking an antidepressant, what should the nurse do? Select all that apply
Explanation
When caring for a patient prescribed an antidepressant, the nurse plays a crucial role in ensuring both safety and therapeutic effectiveness. Monitoring for side effects, providing education, and recognizing risks such as suicidal ideation are essential components of nursing care.
A. Monitor the patient for suicidal tendencies.
Antidepressants can initially increase energy before mood improves, which may heighten suicide risk, especially in the first weeks of therapy.
B. Observe the patient for orthostatic hypotension.
Some antidepressants, particularly tricyclics and MAOIs, can cause significant drops in blood pressure when standing.
C. Teach the patient to take the drug with food if GI distress occurs.
Nausea and GI upset are common side effects; taking the drug with food can reduce discomfort.
D. Tell the patient that the drug may not have full effectiveness for 1 to 2 weeks.
Most antidepressants require time before noticeable improvement occurs, which patients must understand to avoid premature discontinuation.
E. Advise the patient to maintain adequate fluid intake of 2 L/d.
This advice is not a standard precaution for antidepressants; it is more relevant for medications like lithium.
Take-Home Points:
- Nurses should closely monitor for suicidal thoughts during early therapy.
- Education on delayed onset of action helps improve adherence.
- Managing side effects like GI upset and orthostatic hypotension enhances patient safety and comfort.
Patient scenario:
A patient with known bipolar disorder was admitted to the mental health unit for medication adjustment.
The nurse was assessing the patient in the scenario who came in with increasing episodes of depression. Which components are part of the baseline assessment? Select all that apply
Explanation
Baseline assessment for a patient with bipolar disorder focuses on establishing a comprehensive understanding of the patient’s mental, emotional, and physical status to guide safe and effective medication management. Nurses gather information on previous episodes, current symptoms, and functional patterns to identify changes and risks.
A. Dietary history — Important to assess nutrition status and any potential impact on medication absorption or side effects (e.g., lithium requires consistent sodium and fluid intake).
B. History of previous depression episodes and treatments — Provides context for treatment response, medication efficacy, and risk of relapse, guiding future therapeutic decisions.
C. Sleep pattern — Sleep disturbances are common in bipolar disorder and can signal worsening depression or risk for mania; assessment helps guide interventions.
D. Suicidal ideation — Essential for safety assessment, particularly during depressive episodes, and informs risk management and monitoring plans.
G. Clarity of thought — Evaluates cognitive function, orientation, and thought processes, which are key for identifying changes in mental status or medication effects.
E. Tattoos present — Not relevant to mental health assessment or medication planning.
F. Oral hygiene and number of dental cavities — Important for general health but not critical to baseline psychiatric assessment or medication adjustment in bipolar disorder.
Take-Home Points:
- Baseline assessment should cover mental status, mood patterns, and functional behaviors relevant to bipolar disorder.
- Safety-focused assessments, including suicidal ideation, are critical during depressive episodes.
- Physical health components relevant to medication interactions or effects (e.g., nutrition, hydration) should be included.
A patient with known bipolar disorder was admitted to the mental health unit for medication adjustment.
The patient in the scenario was being treated for depression and the nurse will monitor for thoughts of suicide. Indicate with an X which behavior may indicate suicidal ideation and which is unrelated.
Explanation
Patient remarking that the patient had a plan and was intent on carrying it out → Significant Finding
Expressing a specific plan and intent is a major suicide risk indicator, requiring immediate safety interventions.
Poor hygiene → Unrelated Finding
Poor hygiene can reflect depression, but it is a nonspecific finding and does not directly indicate imminent suicidal intent.
Comments from the patient such as, “Things will get better after I’m gone.” → Significant Finding
Statements implying hopelessness or anticipating absence strongly suggest suicidal ideation and need urgent assessment.
Pacing in the room → Unrelated Finding
Pacing may indicate anxiety, restlessness, or agitation, but it is not a direct marker of suicidal ideation.
Excessive appetite → Unrelated Finding
Appetite changes occur with mood disorders, but alone they do not indicate suicidal intent.
Sleeping throughout the day → Unrelated Finding
Hypersomnia is common in depression, but by itself, it is not a red-flag suicidal behavior.
Patient’s relative indicated that the patient has recently given away a collection of expensive dishes → Significant Finding
Giving away prized possessions is a common pre-suicide behavior, showing preparation and finality.
Take-home Points:
- Direct verbal cues and a plan are the strongest indicators of suicide risk.
- Behavioral clues like giving away possessions signal possible preparation for suicide.
- Depressive symptoms (sleep, appetite, hygiene) raise concern but are not definitive for suicidal ideation.
The nurse is monitoring the client for early signs of lithium (Eskalith) toxicity. Which symptoms, if present, may indicate that toxicity is developing? Select all that apply
Explanation
- GI upset, confusion, and polyuria are early warning signs of lithium toxicity.
- Severe symptoms such as ataxia and seizures occur in advanced toxicity.
- Continuous monitoring of serum lithium levels and client symptoms is essential to maintain safety.
A patient is admitted with bipolar affective disorder. The nurse acknowledges that which medication is used to treat this disorder for some patients in place of lithium?
Explanation
Bipolar affective disorder is commonly managed with mood stabilizers. While lithium remains a first-line therapy, not all patients tolerate it due to side effects, drug interactions, or contraindications. In such cases, anticonvulsants such as divalproex (Depakote) are used as alternatives or adjuncts for mood stabilization.
D. divalproex (Depakote)
– Divalproex is an anticonvulsant that is also FDA-approved for bipolar disorder. It is especially effective in managing acute mania, mixed episodes, and rapid cycling. It is considered a reliable alternative for patients who cannot tolerate lithium due to renal impairment, toxicity risk, or lack of response.
A. thiopental
– Thiopental is a barbiturate used for induction of anesthesia and rapid sedation. It does not have a role in mood stabilization or long-term psychiatric management.
B. gingko biloba
– Ginkgo is an herbal supplement sometimes used to improve memory and circulation. It is not approved or effective for treating bipolar disorder and could potentially interact with psychiatric medications.
C. fluvoxamine (Luvox)
– Fluvoxamine is a selective serotonin reuptake inhibitor (SSRI) used for depression and obsessive-compulsive disorder. While it can treat depressive symptoms, SSRIs alone can trigger manic episodes in bipolar patients, making them inappropriate as primary treatment.
Take-Home Points:
- Lithium is first-line for bipolar disorder, but divalproex is a widely used alternative.
- Anticonvulsants such as valproate and carbamazepine can stabilize mood in patients who cannot take lithium.
- SSRIs and herbal supplements are not used as primary therapy for bipolar affective disorder.
A client is taking lithium. The nurse should be aware of the importance of which nursing intervention(s)? Select all that apply
Explanation
Lithium is a mood stabilizer widely used in the management of bipolar disorder, particularly for preventing manic and depressive episodes. Because it has a narrow therapeutic range, patients are at risk for toxicity if blood levels fluctuate due to dehydration, drug interactions, or dietary changes. Nurses must closely monitor clients and provide teaching to ensure safety, adherence, and therapeutic effectiveness.
A. Observe the patient for motor tremors — Tremors are one of the earliest and most common signs of lithium toxicity, often appearing before severe symptoms like ataxia, confusion, or seizures. Tremors can indicate even mild elevations in lithium levels and may be exacerbated by stress, fatigue, or changes in hydration. Regular neurological assessments allow the nurse to intervene promptly, adjust therapy if needed, and prevent progression to life-threatening toxicity.
B. Monitor the patient for orthostatic hypotension — Lithium can cause fluid shifts and mild hypotension, especially in older adults or clients on diuretics. Monitoring blood pressure in different positions helps prevent falls, dizziness, and injuries, which are critical considerations in safe patient care.
E. Advise the patient to avoid caffeinated foods and beverages — Caffeine can increase renal excretion of lithium, potentially lowering blood levels and decreasing effectiveness. Clients should be educated on maintaining consistent caffeine intake to avoid fluctuations.
F. Teach the patient to take lithium with meals to decrease gastric irritation — Lithium can cause nausea, vomiting, and diarrhea if taken on an empty stomach. Taking it with food reduces gastrointestinal discomfort and improves medication adherence.
C. Draw lithium blood levels immediately after a dose — Accurate lithium monitoring requires blood to be drawn 12 hours after the last dose. Drawing levels immediately post-dose can give falsely elevated results, leading to unnecessary dose adjustments or alarm.
D. Advise the patient to drink 750 mL/d of fluid in hot weather — Lithium therapy requires maintaining adequate hydration (A.5–3 L/day) to prevent concentration changes and toxicity. 750 mL is insufficient, especially in hot weather or with increased activity.
Take-Home Points:
- Monitor closely for early signs of lithium toxicity, such as tremors, GI upset, and cognitive changes.
- Ensure adequate hydration and dietary consistency to maintain therapeutic lithium levels.
- Provide patient education on timing, meal administration, and avoiding substances that alter lithium excretion.
The nurse is giving medications to a client. Which drug or drug class, when administered with lithium, increases the risk for lithium toxicity?
Explanation
Lithium is a mood stabilizer with a narrow therapeutic range, making patients susceptible to toxicity if drug interactions alter its excretion. Certain medications, particularly thiazide diuretics, can reduce renal clearance of lithium, increasing serum levels and the risk of toxicity. Nurses must be vigilant when patients are taking interacting drugs and monitor for early signs of toxicity.
A. Thiazides — Thiazide diuretics reduce renal excretion of lithium, leading to increased serum concentrations and a higher risk of lithium toxicity. Monitoring lithium levels and adjusting dosages are essential when these drugs are combined.
B. Levofloxacin — This antibiotic does not significantly affect lithium excretion or toxicity risk. Routine monitoring is standard but not heightened solely due to levofloxacin use.
C. Calcium citrate — Calcium supplements do not impact lithium metabolism or excretion and do not increase toxicity risk.
D. Beta blockers — Beta blockers may affect blood pressure and heart rate but do not significantly alter lithium levels or increase toxicity risk.
Take-Home Points:
- Monitor lithium levels closely when patients are taking thiazide diuretics.
- Educate patients to report symptoms of toxicity, including tremors, confusion, nausea, and ataxia.
- Adjust lithium dosage as needed when new medications affecting renal function are prescribed.
A client who has been taking lithium for 6 months has had severe vomiting and diarrhea from a gastrointestinal flu. The nurse will assess for which potential problem at this time?
Explanation
Lithium is a mood stabilizer with a narrow therapeutic range. Because lithium is primarily excreted by the kidneys, conditions that alter fluid and electrolyte balance, such as vomiting and diarrhea, can rapidly increase the risk for lithium toxicity. Nurses must assess hydration status and monitor for signs of toxicity in patients experiencing fluid loss.
D. Dehydration — Severe vomiting and diarrhea can lead to fluid depletion, which reduces renal clearance of lithium, increasing the risk of elevated lithium levels and toxicity. Assessment should include monitoring vital signs, intake and output, and signs of hypotension or dizziness.
A. Anxiety — While lithium can affect mood, acute gastrointestinal illness does not directly cause anxiety related to lithium therapy and is less urgent than fluid status.
B. Chest pain — Not a common complication of lithium therapy or fluid loss from GI illness. Any chest pain would warrant separate cardiac evaluation.
C. Agitation — Although agitation can be a symptom of lithium toxicity, in this scenario the primary concern is dehydration that may precipitate toxicity; agitation would be secondary if toxicity develops.
Take-Home Points:
- Monitor for dehydration and electrolyte imbalance in patients on lithium during illness.
- Understand that fluid loss can precipitate lithium toxicity.
- Prompt assessment and intervention can prevent life-threatening complications.
Exams on Drugs Used for Depressive and Bipolar Disorders
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Depression
- Antidepressants
- Selective serotonin reuptake inhibitors (SSRIs)
- Atypical ANTIDEPRESSANTS
- Tricyclic antidepressants
- Monoamine oxidase inhibitors (MAOIs)
- Practice Exercise 1
- Bipolar disorder
- Drugs used for bipolar disorders
- Mood stabilizers
- Mood Stabilizing antiepileptic drugs (aEDS)
- Atypical antipsychotics
- Practice Exercise 2
- Summary
- Practice Exercise 3
- Comprehensive questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
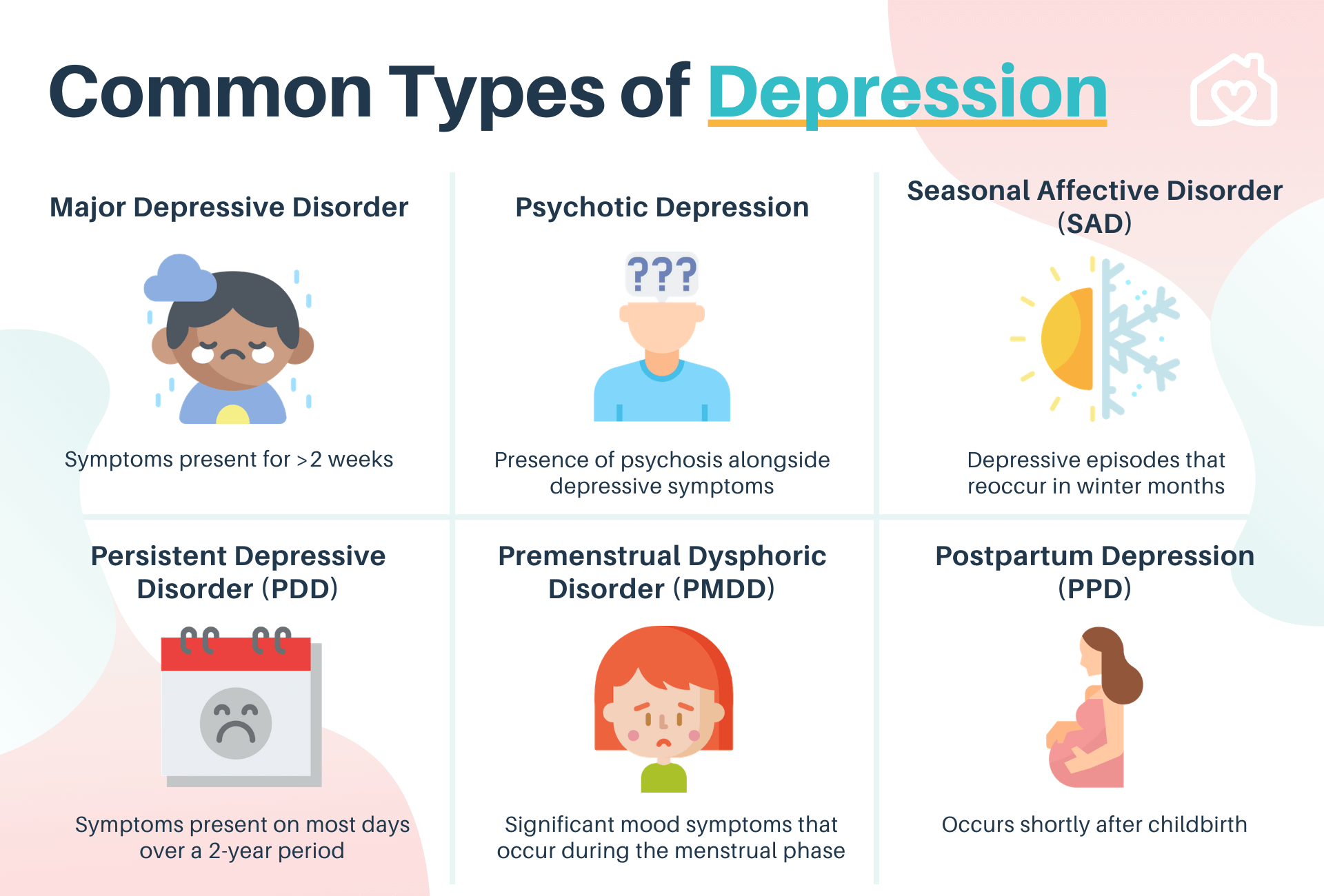
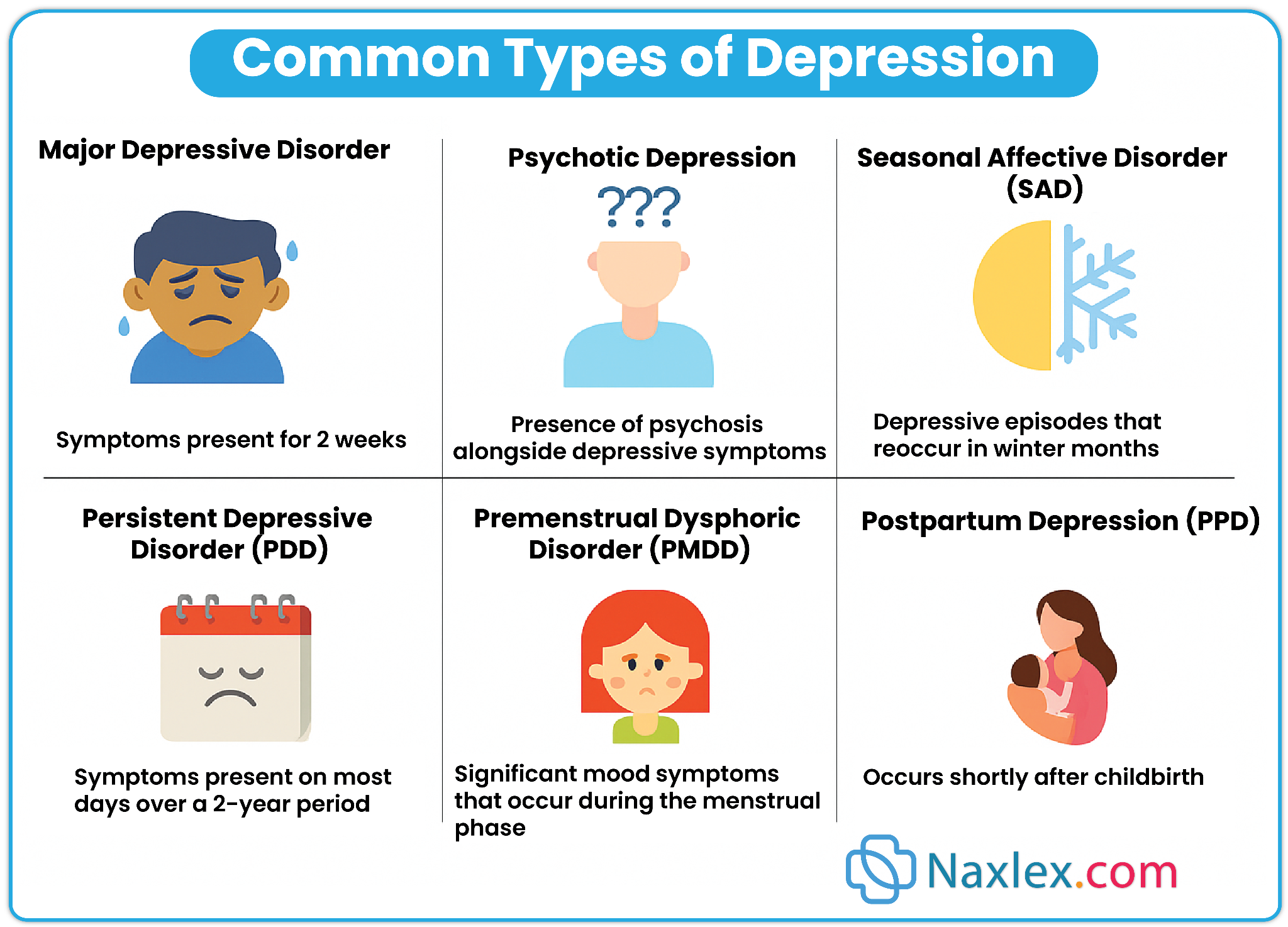
- Define depression and list its main types (MDD, dysthymia, situational, perinatal, seasonal, psychotic).
- Describe assessment of depression, including suicidal risk and psychosocial evaluation.
- Explain antidepressant classes (SSRIs, atypical, TCAs, MAOIs) regarding action, use, side effects, and nursing care.
- Identify nursing interventions for antidepressant therapy, including monitoring, adherence, and patient support.
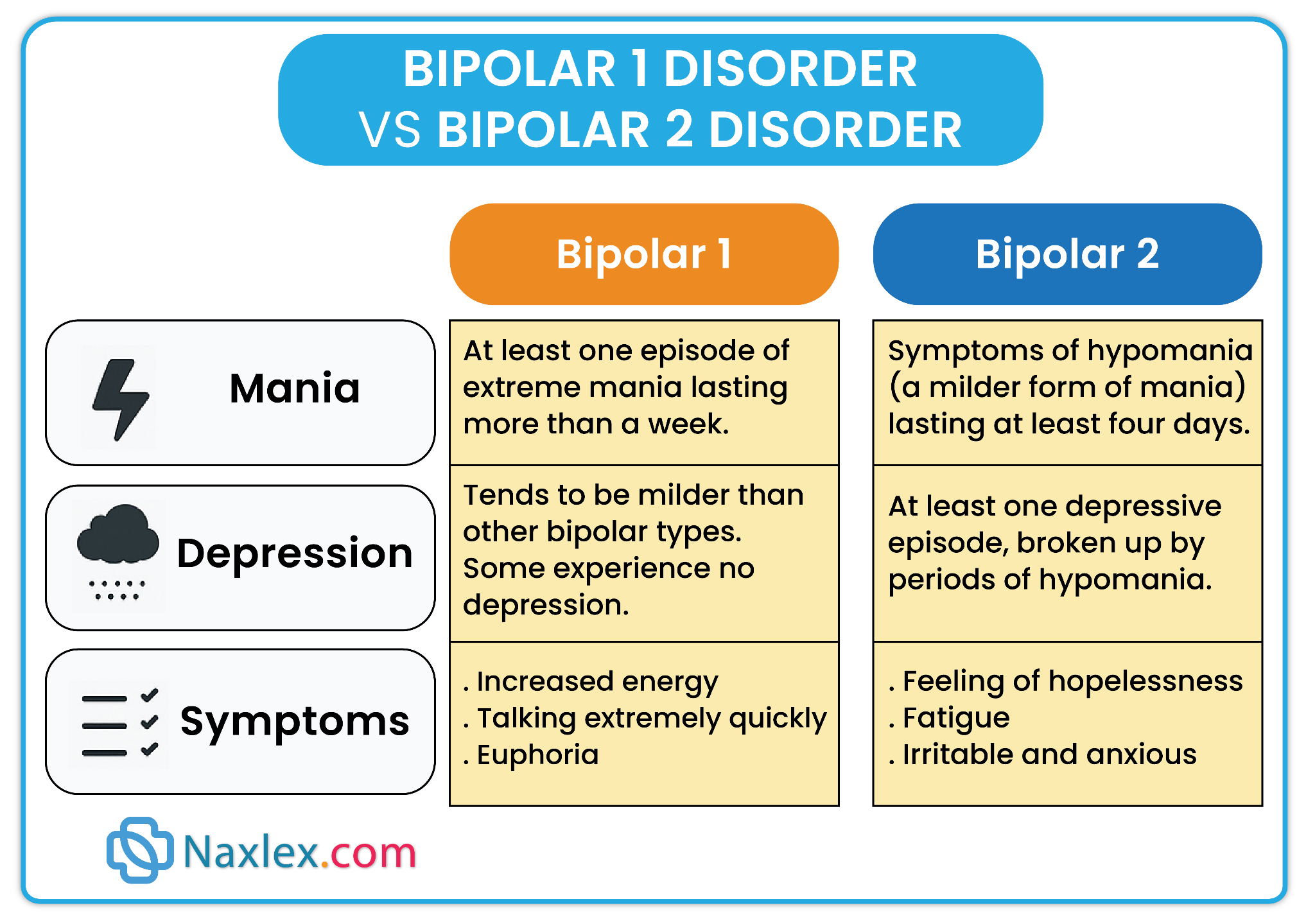
- Describe bipolar disorder, its types (Bipolar I, II, cyclothymic), and clinical features of mania, hypomania, and depression.
- Outline pharmacologic management of bipolar disorder with mood stabilizers, AEDs, antipsychotics, and adjuncts.
- List actions, uses, side effects, monitoring, and nursing considerations for lithium, carbamazepine, valproic acid, and lamotrigine.
- Describe atypical antipsychotics in bipolar disorder (olanzapine, risperidone, quetiapine, lurasidone, aripiprazole) and their risks/benefits.
- Outline nursing care for bipolar patients: safety, adherence, lifestyle, family education, and relapse prevention.
- Evaluate treatment effectiveness: mood stability, ADLs, social functioning, and absence of major side effects or toxicity.
Depression
Definition and Overview
-
Depression is a mood disorder characterized by a persistent sad, hopeless, or despondent affect accompanied by disturbances in energy, sleep, appetite, cognition, and social functioning.
-
It is the most common mental health disorder among older adults, but occurs across all age groups.
-
Key features: loss of interest/pleasure (anhedonia), impaired daily functioning, and potential suicidal ideation.

Forms and Characteristics of Depression
1. Major Depressive Disorder (MDD / Clinical Depression)
-
Affects ~5–10% of adults in the U.S.
-
DSM diagnostic criteria: Depressed affect + ≥ 5 symptoms for ≥ 2 weeks:
-
Sleep disturbance (insomnia/hypersomnia)
-
Fatigue/loss of energy
-
Appetite changes (↑ or ↓)
-
Physical complaints (e.g., GI pain, headaches, joint pain)
-
Poor concentration/indecisiveness
-
Feelings of guilt, worthlessness, despair
-
Suicidal ideation or preoccupation with death
-
Social withdrawal/loss of interest in appearance or sex
-
Delusions or hallucinations (in severe cases)
-
Clinical pearl: Most depressed patients are encountered in community or primary care settings rather than psychiatric hospitals.
-
Triggered by a major life event (e.g., divorce, job loss, bereavement).
-
Often short-term but may progress to clinical depression if prolonged.
3. Dysthymic Disorder (Persistent Depressive Disorder)
-
Chronic, less severe symptoms that last ≥ 2 years.
-
Patients may not feel well or function optimally but are not acutely incapacitated.
-
Hormonal and situational triggers: menstrual cycle, pregnancy, postpartum period, and menopause.
-
Postpartum depression:
-
Affects up to 80% with mild symptoms (“baby blues”).
-
~10% develop major depression within 6 months postpartum.
-
-
Risks: hormonal shifts + life stressors (e.g., caregiving, single parenthood).
-
Premenstrual Dysphoric Disorder (PMDD): Severe premenstrual mood disturbance requiring treatment.ig
Clinical note: Some states mandate screening/education for postpartum depression before discharge.
5. Seasonal Affective Disorder (SAD)
-
Associated with increased melatonin during low-light months (winter).
-
Symptoms improve with light therapy.
-
Severe depression with hallucinations, delusions, and disorganized speech/behavior.
-
Requires antipsychotic therapy + antidepressant management.
-
Rule out medical or drug-induced causes (e.g., corticosteroids, levodopa, OCPs, thyroid disorders, B-vitamin deficiencies, early Alzheimer’s).
-
Conduct thorough physical + psychological exam.
-
Assess alcohol/drug use and suicidal ideation.
-
Collect family psychiatric history (response to therapies is often hereditary).
-
Safety first: always assess for suicidal thoughts or intent.
-
Recognize psychosocial effects on caregivers — they may need support or counseling.
-
Assessment:
-
Screen for suicidal ideation and substance abuse.
-
Monitor for physical conditions mimicking depression.
-
-
Patient education:
-
Emphasize adherence to medications (effects may take 2–6 weeks).
-
Inform about side effects and potential drug interactions.
-
-
Support system:
-
Engage family/caregivers; provide education and counseling resources.
-
Address caregiver fatigue and guilt.
-
-
Monitoring:
-
Watch for worsening symptoms during early therapy (risk of suicide ↑ when energy returns before mood improves).
-
Antidepressants
Introduction
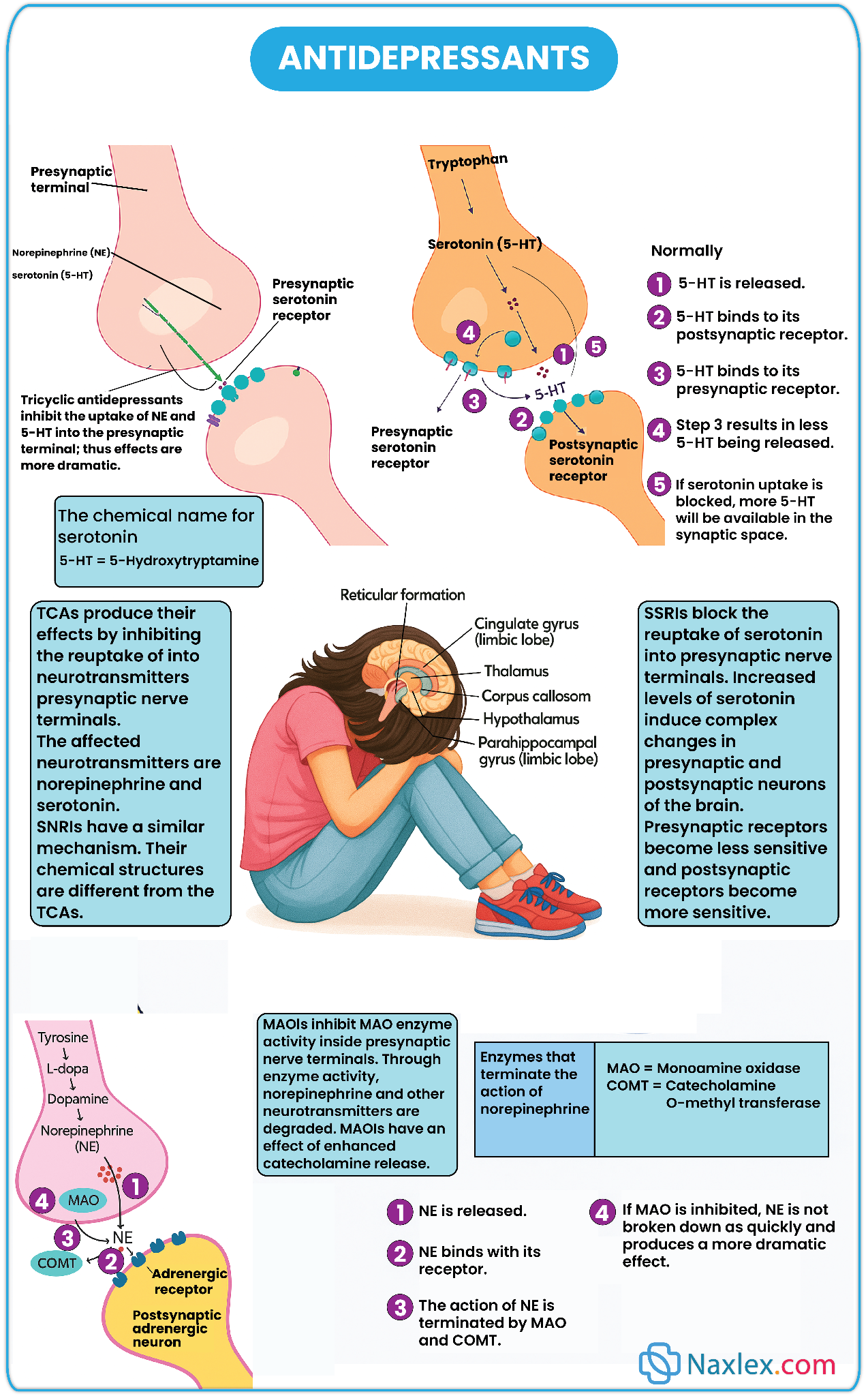
Antidepressants are medications prescribed to treat depressive disorders and other related psychiatric conditions. These drugs enhance neurotransmission of monoamines—primarily serotonin, norepinephrine, and dopamine—thereby improving mood, cognition, and overall functioning.
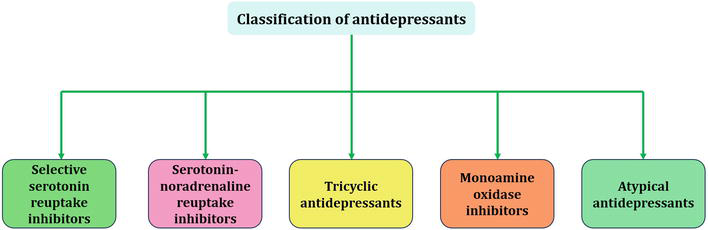
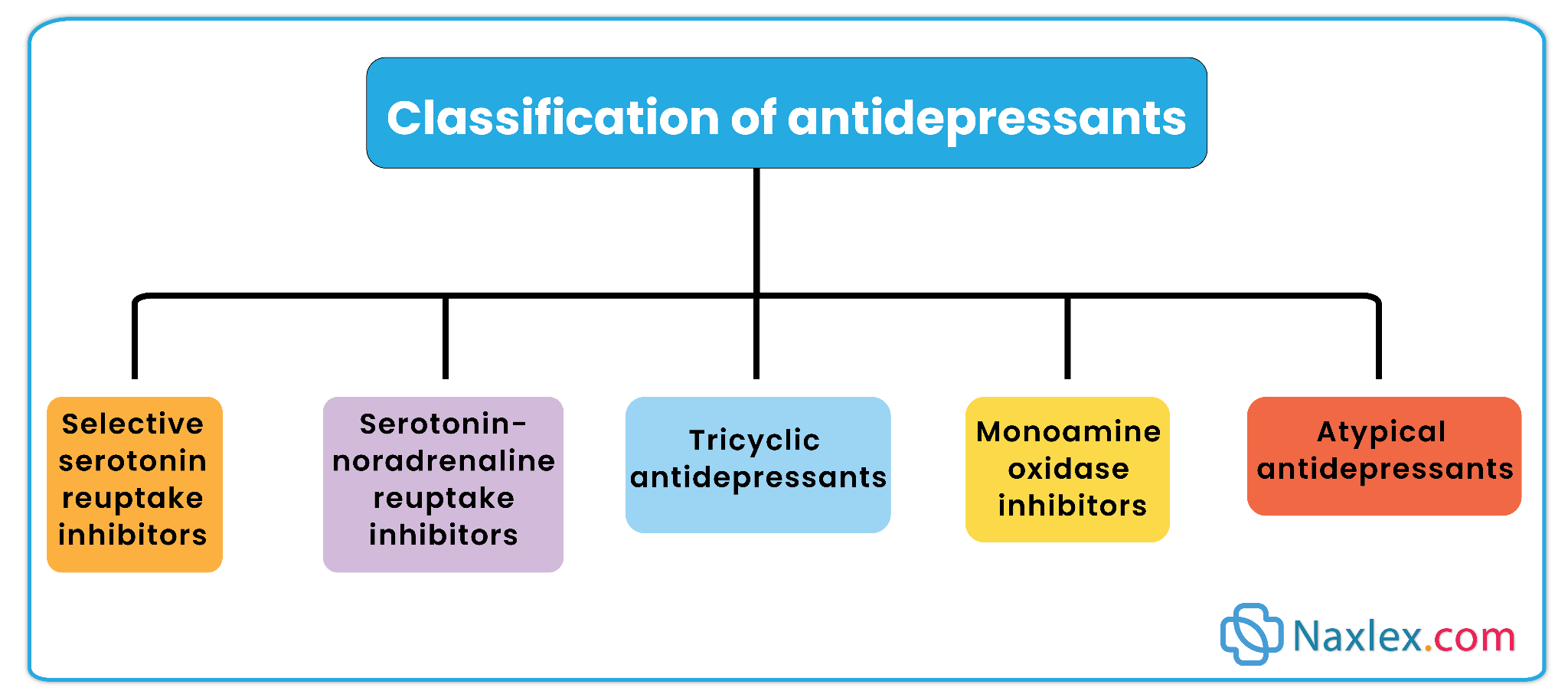
Classification:
They are classified into :
- Selective Serotonin Reuptake Inhibitors (SSRIs)
- Serotonin noradrenaline reuptake inhibitors (SNRIs)
- Atypical Antidepressants
- Tricyclic Antidepressants (TCAs)
- Monoamine Oxidase Inhibitors (MAOIs)
While these medications are effective in relieving depressive symptoms, their selection depends on patient-specific factors including comorbidities, adverse effect profiles, drug interactions, and individual response.
Selective serotonin reuptake inhibitors (SSRIs)
Fluoxetine (Prozac)
Other Medications: Citalopram (Celexa), Escitalopram (Lexapro), Paroxetine (Paxil), Sertraline (Zoloft), Vilazodone (Viibryd)
Mechanism of Action
-
Selectively inhibit reuptake of serotonin in the synaptic cleft.
-
Increases serotonin availability and neurotransmission, improving mood and anxiety symptoms.
Therapeutic Uses
-
Major depressive disorder
-
Obsessive-compulsive disorder (OCD)
-
Bulimia nervosa
-
Premenstrual dysphoric disorder
-
Panic disorder
-
Posttraumatic stress disorder (PTSD)
Adverse Effects
-
Sexual dysfunction: Impotence, decreased libido, anorgasmia
-
CNS stimulation: Insomnia, agitation, anxiety
-
Weight changes: Initial weight loss, possible long-term gain
-
Serotonin syndrome: Mental confusion, hyperreflexia, diaphoresis, tremors; may be lethal
-
Withdrawal syndrome: Headache, nausea, dizziness, anxiety
-
Hyponatremia: Particularly in older adults taking diuretics
-
GI bleeding and bruxism
Nursing Insights:
-
Educate patients about onset (weeks) and need for adherence.
-
Monitor weight, sodium levels, and signs of serotonin syndrome.
-
Avoid concurrent use with MAOIs or TCAs.
-
Advise taking the medication in the morning to reduce insomnia.
-
Encourage reporting of sexual side effects; consider switching to bupropion if intolerable.
Contraindications/Precautions
-
Pregnancy Risk Category C; paroxetine and fluoxetine have higher teratogenic risk.
-
Caution in liver/renal impairment, cardiac disease, seizure disorders, diabetes, and history of GI bleeding.
Interactions
-
Increased serotonin syndrome risk with MAOIs, TCAs, and St. John’s wort.
-
Fluoxetine may increase levels of warfarin, TCAs, and lithium.
-
Concomitant NSAIDs increase risk of bleeding.
Atypical ANTIDEPRESSANTS
Bupropion HCl (Wellbutrin)
Other Examples: Venlafaxine (Effexor), Duloxetine (Cymbalta), Mirtazapine (Remeron), Reboxetine (Edronax), Trazodone (Desyrel)
Mechanism of Action
-
Varies by agent:
-
Bupropion inhibits dopamine uptake.
-
Venlafaxine and duloxetine inhibit serotonin and norepinephrine reuptake.
-
Mirtazapine increases serotonin and norepinephrine release.
-
Reboxetine selectively inhibits norepinephrine reuptake.
-
Trazodone blocks serotonin receptors moderately.
-
Therapeutic Uses
-
Depression
-
Alternative to SSRIs for sexual dysfunction
-
Smoking cessation aid (bupropion)
-
Seasonal affective disorder prevention
-
Insomnia (trazodone adjunct)
Adverse Effects
-
Headache, dry mouth, GI distress, insomnia, restlessness
-
Appetite suppression (bupropion) → weight loss
-
Seizures (bupropion)
-
Hyponatremia, increased blood pressure (SNRIs)
-
Sedation (mirtazapine, trazodone)
-
Rare priapism with trazodone
Nursing Insights
-
Monitor for seizure activity with bupropion.
-
Advise gradual tapering to prevent withdrawal.
-
Educate about potential sedation and avoid CNS depressants.
-
Monitor blood pressure, weight, and electrolyte balance with SNRIs.
-
Avoid concurrent use with MAOIs.
Contraindications/Precautions
-
Bupropion contraindicated in seizure disorders or MAOI therapy.
-
Use SNRIs cautiously in hypertension and hyponatremia risk.
TRICYCLIC ANTIDEPRESSANTS (TCAS)
Other Medications: Imipramine (Tofranil), Doxepin (Sinequan), Nortriptyline (Aventyl), Amoxapine (Asendin), Trimipramine (Surmontil)
Mechanism of Action
-
Inhibit reuptake of norepinephrine and serotonin at synapses.
-
Intensify neurotransmission to alleviate depression.
Therapeutic Uses
-
Depression
-
Depressive episodes of bipolar disorder
-
Neuropathic pain, fibromyalgia, anxiety disorders, insomnia
Adverse Effects
-
Orthostatic hypotension
-
Anticholinergic effects: dry mouth, blurred vision, constipation, urinary retention, tachycardia
-
Sedation
-
Cardiac toxicity (dysrhythmias, seizures, coma in overdose)
-
Decreased seizure threshold
Nursing Insights
-
Administer at bedtime to reduce daytime sedation.
-
Monitor vital signs, orthostatic hypotension, and cardiac rhythm.
-
Educate patients on anticholinergic effects and ways to minimize them.
-
Limit supply for high-risk suicide clients due to overdose potential.
Contraindications/Precautions
-
Pregnancy Risk Category C
-
Caution in seizure disorders, coronary artery disease, liver/renal impairment, BPH, glaucoma.
Interactions
-
Avoid combination with MAOIs, St. John’s wort, other anticholinergic agents, and CNS depressants.
Monoamine oxidase inhibitors (MAOIs)
Phenelzine (Nardil)
Other Medications: Isocarboxazid (Marplan), Tranylcypromine (Parnate), Selegiline transdermal (Emsam)
Mechanism of Action
-
Inhibit monoamine oxidase enzyme, increasing availability of norepinephrine, serotonin, and dopamine.
-
Enhances neurotransmission, alleviating depressive symptoms.
Therapeutic Uses
-
Depression
-
Bulimia nervosa
Adverse Effects
-
CNS stimulation: anxiety, agitation, mania/hypomania
-
Orthostatic hypotension
-
Hypertensive crisis from dietary tyramine: headache, nausea, elevated BP/HR
-
Local rash with transdermal application
Nursing Insights
-
Educate clients to avoid tyramine-rich foods: aged cheese, smoked meats, soy products, some beers, red wine.
-
Monitor blood pressure and heart rate; treat hypertensive crisis with IV phentolamine or SL nifedipine.
-
Emphasize adherence and gradual dose titration.
-
Avoid concurrent use with SSRIs, TCAs, and sympathomimetics.
Contraindications/Precautions
-
Pregnancy Risk Category C
-
Contraindicated in cardiovascular disease, cerebrovascular disease, pheochromocytoma, severe renal insufficiency
-
Use caution with diabetes, seizure disorders, or concomitant TCA therapy
Nursing Administration for All Antidepressants
-
Initiate therapy daily at the prescribed dose.
-
Therapeutic effects may begin within 1–3 weeks; full effect in 2–3 months.
-
Continue therapy for at least 6 months after symptom resolution; may extend longer.
-
Monitor for suicidal ideation, especially in patients <25 years during early treatment.
-
Tailor administration:
-
SSRIs in the morning
-
TCAs at bedtime
-
Avoid MAOI dietary and drug interactions
-
Evaluation of Effectiveness
-
Verbalized mood improvement
-
Improved performance in activities of daily living (ADLs)
-
Normalized sleep and appetite
-
Increased social interaction
Bipolar disorder
I. Introduction to Bipolar Disorder
Bipolar disorder, historically known as manic-depressive illness, is a chronic psychiatric condition characterized by recurrent episodes of depression and mania (or hypomania). It is a severe mood disorder with high rates of morbidity, disability, and suicide if untreated.
-
Etiology: Largely multifactorial, involving genetic predisposition, neurobiological imbalances, and environmental triggers.
-
Neurobiology: Dysfunction in neurotransmitters (dopamine, serotonin, norepinephrine, glutamate, GABA) and abnormal receptor regulation contribute to mood instability.
-
Clinical Significance: Differentiation is important from other conditions such as substance-induced mania or schizophrenia, as management strategies differ significantly.

II. Clinical Characteristics of Bipolar Disorder
Bipolar disorder is defined by alternating depressive episodes (similar to major depression) and manic/hypomanic episodes.
-
Symptoms mirror major depressive disorder (MDD):
-
Depressed mood most of the day
-
Loss of interest/pleasure (anhedonia)
-
Fatigue and psychomotor retardation
-
Sleep disturbances (insomnia/hypersomnia)
-
Changes in appetite/weight
-
Feelings of guilt or worthlessness
-
Poor concentration or indecisiveness
-
Suicidal thoughts or behavior
-
Defined as abnormally elevated, expansive, or irritable mood with increased goal-directed activity or energy for ≥1 week. Must cause marked impairment in functioning or require hospitalization.
Key Symptoms of Mania:
-
Inflated self-esteem or grandiosity
-
Decreased need for sleep (e.g., feels rested after only 3 hrs)
-
Increased talkativeness or pressured speech
-
Racing thoughts or flight of ideas
-
Distractibility
-
Increased goal-directed activity or psychomotor agitation
-
Impulsive, high-risk behaviors (e.g., excessive spending, hypersexuality, reckless business decisions)
-
Shares the same symptom profile as mania but is less severe.
-
Duration: ≥4 days.
-
Does not cause marked impairment, hospitalization, or psychotic features.
III. Classification of Bipolar Disorders
-
-
At least 1 manic episode (often alternating with depression).
-
Severe, often requires hospitalization.
-
-
-
At least 1 hypomanic episode + 1 major depressive episode.
-
No full manic episode.
-
Higher risk of misdiagnosis as recurrent depression.
-
-
-
Numerous periods of hypomanic symptoms and depressive symptoms for at least 2 years (1 year in children/adolescents).
-
Does not meet criteria for full mania or major depression.
-
-
Suicidal Ideation: Especially during depressive or mixed episodes.
-
Safety Concerns: During mania, impulsivity and risk-taking behaviors may endanger self/others.
-
Adherence Issues: Patients may discontinue medications due to side effects or belief they no longer need treatment during mood improvement.
-
Comorbidities: Anxiety disorders, substance abuse, cardiovascular disease, and metabolic syndrome.
-
Promote Safety
-
During mania: Reduce stimuli, set firm boundaries, supervise risky activities.
-
During depression: Suicide precautions, frequent assessments.
-
-
Medication Adherence
-
Stress the importance of lifelong therapy even when symptoms improve.
-
Teach to report early toxicity symptoms (esp. with lithium).
-
-
Lifestyle & Self-Care
-
Adequate sleep and structured routines reduce relapse risk.
-
Hydration and consistent sodium intake are crucial with lithium.
-
Avoid alcohol and stimulant use.
-
-
Family Education
-
Teach families to recognize early warning signs of mania/depression.
-
Encourage involvement in psychotherapy and support groups.
-
-
Lithium = Gold standard, narrow therapeutic index, monitor closely.
-
Valproic acid & carbamazepine = Effective for rapid cycling; monitor liver and blood counts.
-
Lamotrigine = Best for bipolar depression; watch for rash/Stevens-Johnson syndrome.
-
Antidepressants alone can precipitate mania; always pair with a mood stabilizer.
-
Bipolar I = At least one manic episode. Bipolar II = Hypomania + depression, no mania.
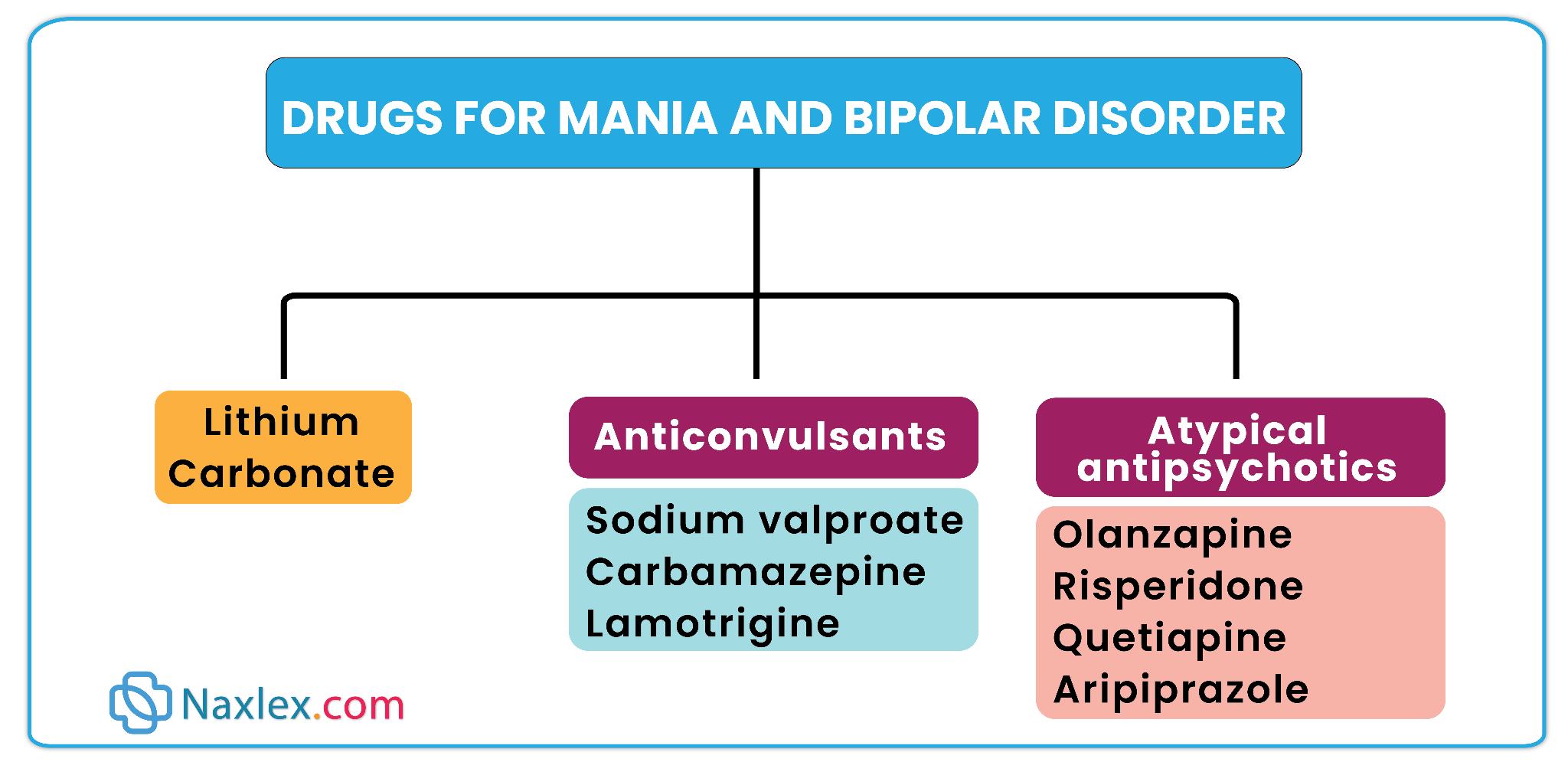
Drugs used for bipolar disorders
Classification:
Bipolar disorders are primarily managed with:
-
Mood-stabilizing medications such as lithium carbonate (Lithane, Eskalith, Lithotabs).
-
Antiepileptic medications
-
Valproic acid (Depakote)
-
Carbamazepine (Tegretol, Equetro)
-
Lamotrigine (Lamictal)
-
-
Atypical antipsychotics – Useful in early treatment to promote sleep, reduce anxiety and agitation, and demonstrate mood-stabilizing properties.
-
Anxiolytics – Clonazepam (Klonopin) and lorazepam (Ativan) are used to treat acute mania and psychomotor agitation.
-
Antidepressants – Bupropion (Wellbutrin) and sertraline (Zoloft) can treat depressive episodes, typically combined with a mood stabilizer to prevent rebound mania.
Mood stabilizers
1. Lithium Carbonate (Lithane, Eskalith, Lithotabs)
Mechanism of Action
-
Alters sodium transport in nerve cells, modulating neuronal excitability.
-
Affects neurotransmitter release, including serotonin and norepinephrine.
-
May decrease neuronal atrophy and enhance neuronal growth.
Therapeutic Uses
-
Acute mania and manic episodes.
-
Maintenance therapy to prevent relapse of mania or depression.
-
Reduces suicide risk in bipolar disorder.
Monitoring
-
Narrow therapeutic range: 0.6–1.2 mEq/L (maintenance), 0.8–1.4 mEq/L (acute mania).
-
Plasma lithium levels: initially every 2–3 days, then every 1–3 months.
-
Baseline and periodic kidney function tests (BUN, creatinine).
-
Baseline and annual thyroid function tests (T3, T4, TSH).
Adverse Effects
-
GI distress: nausea, vomiting, diarrhea, abdominal discomfort.
-
Fine hand tremors, polyuria, mild thirst, weight gain.
-
Long-term: hypothyroidism, goiter, renal toxicity, bradydysrhythmias.
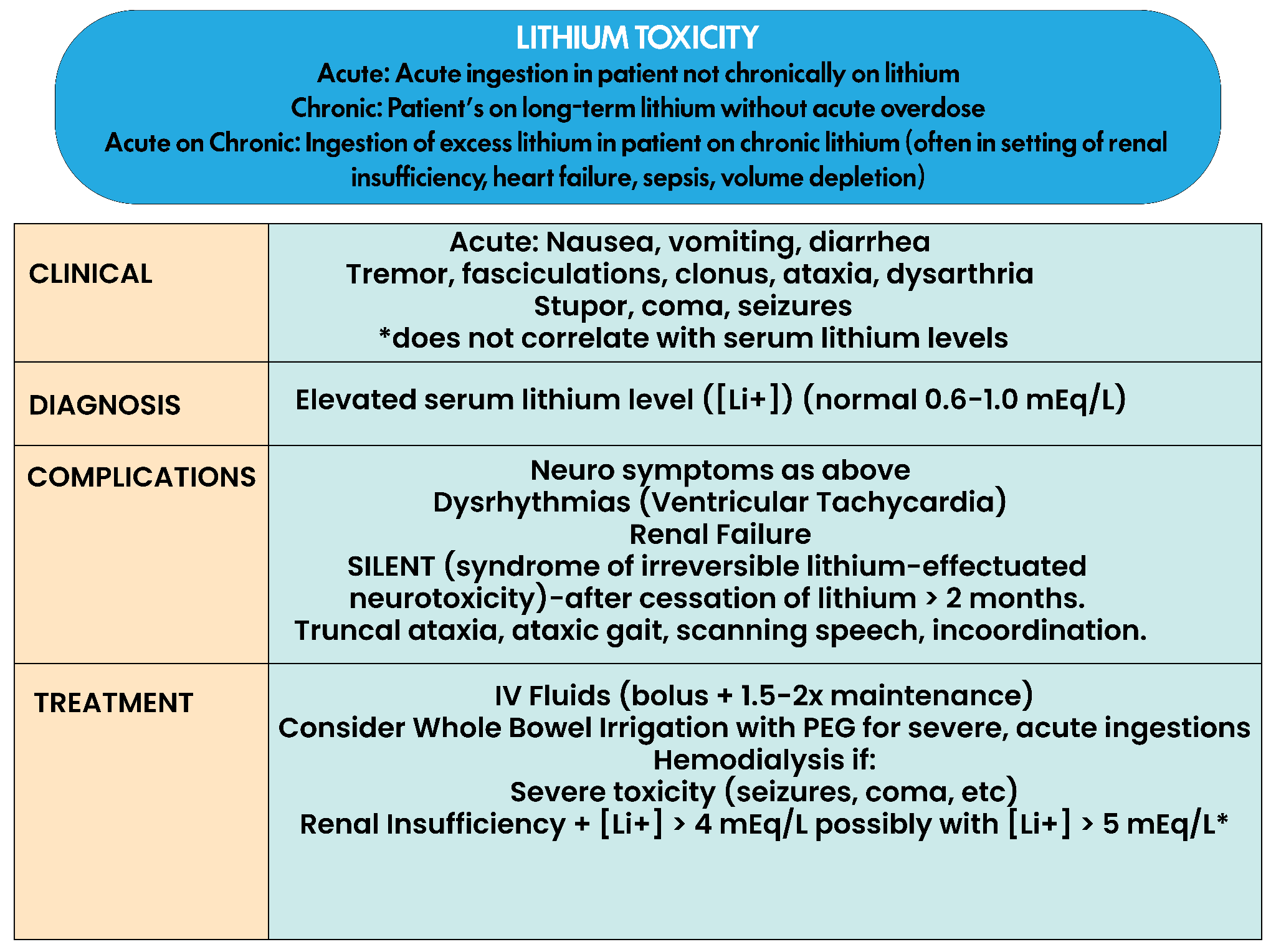
-
Early ( <1.5 mEq/L ): Tremors, nausea, vomiting, diarrhea, thirst, polyuria, mild confusion.
-
Advanced (1.5–2.0 mEq/L): Coarse tremors, mental confusion, poor coordination, persistent GI upset.
-
Severe (2.0–2.5 mEq/L): Ataxia, blurred vision, tinnitus, extreme polyuria, seizures, hypotension, coma.
-
Life-threatening (>2.5 mEq/L): Rapid progression to coma and death; hemodialysis indicated.
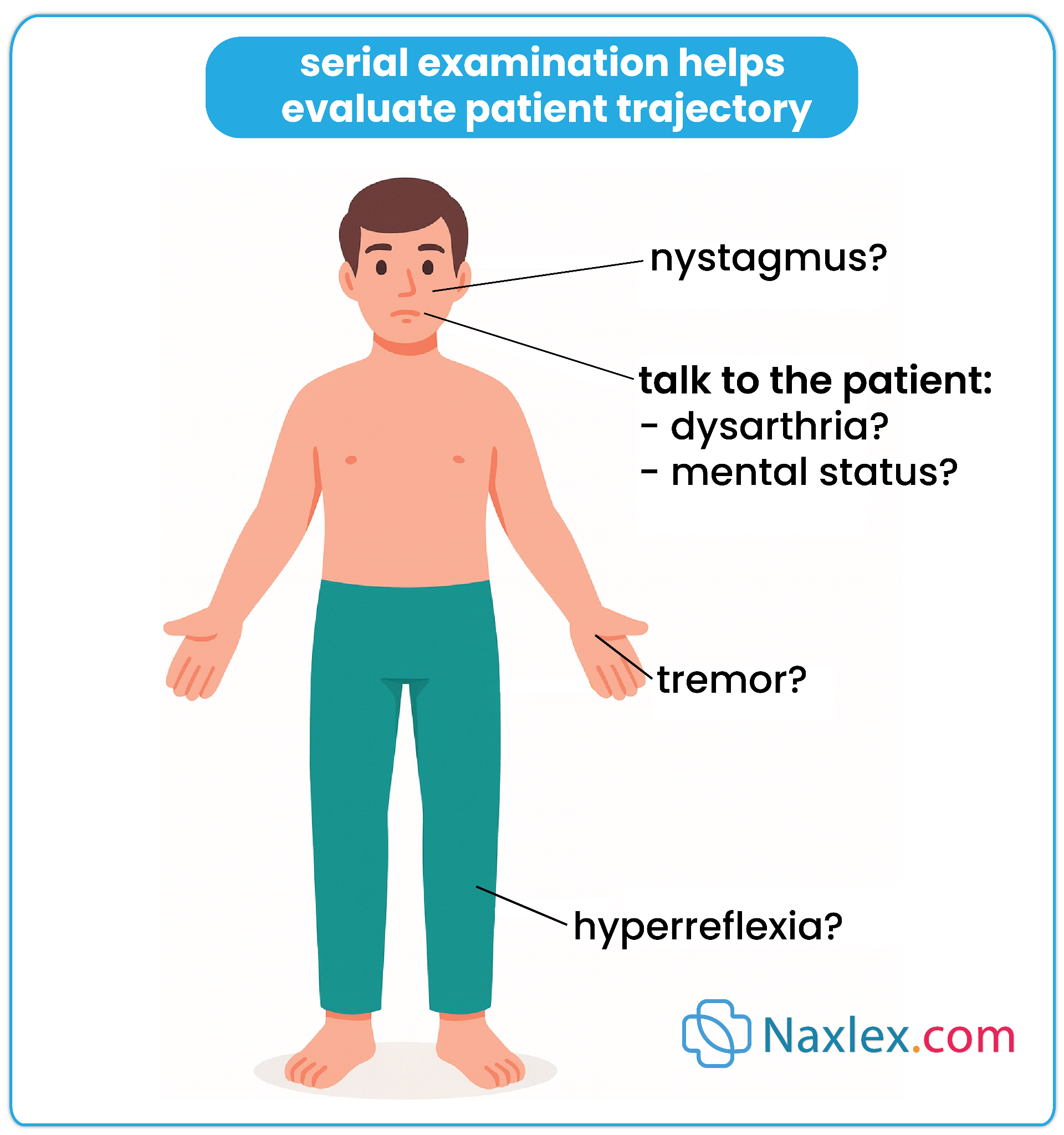
Nursing Insights
-
Maintain consistent fluid intake (2–3 L/day) and sodium intake.
-
Avoid dehydration, excessive sweating, and diuretics.
-
Administer with food to minimize GI upset.
-
Educate about signs of toxicity and when to contact the provider.
-
Monitor for drug interactions: NSAIDs, ACE inhibitors, and diuretics may increase lithium levels.
Mood Stabilizing antiepileptic drugs (aEDS)
1. Carbamazepine (Tegretol, Equetro)
Mechanism of Action
-
Anticonvulsant that reduces neuronal excitability by slowing sodium channel recovery.
-
Enhances inhibitory neurotransmission indirectly.
Therapeutic Uses
-
Acute mania, mixed episodes.
-
Prevention of relapse in bipolar disorder, especially rapid cycling.
Adverse Effects
-
CNS: dizziness, drowsiness, nystagmus, double vision, headache.
-
Hematologic: leukopenia, anemia, thrombocytopenia.
-
Liver toxicity, hyponatremia, teratogenicity.
-
Dermatologic: rash, Stevens–Johnson syndrome.
Monitoring
-
CBC and platelets.
-
Liver function tests (LFTs).
-
Serum sodium.
Nursing Insights
-
Start low, titrate slowly; administer at bedtime.
-
Advise clients to report bruising, infections, or severe rash.
-
Avoid in pregnancy or clients with bone marrow suppression.
-
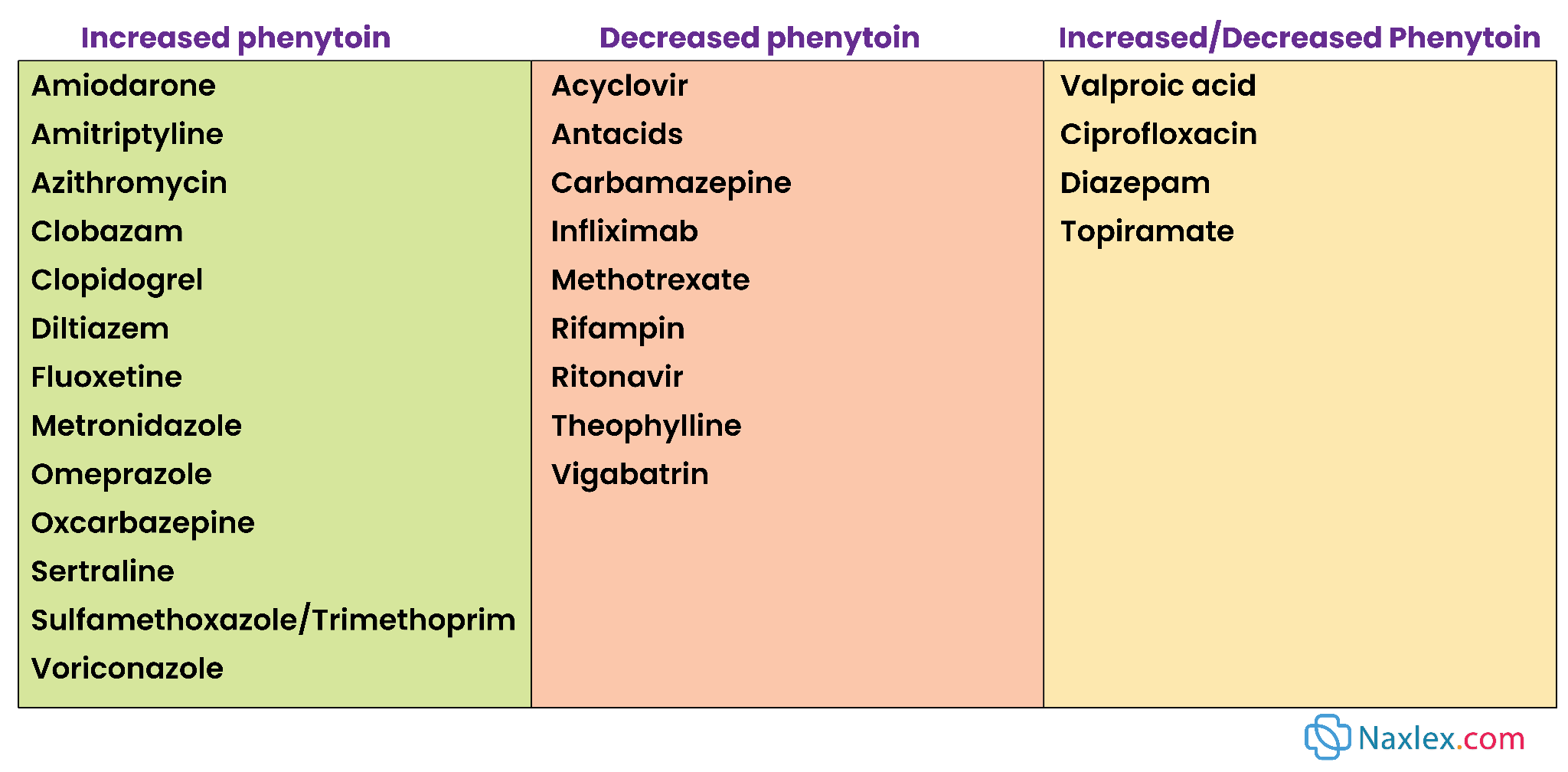
Interactions: decreases effectiveness of oral contraceptives and warfarin; avoid grapefruit juice; monitor phenytoin and phenobarbital levels.

2. Valproic Acid (Divalproex, Depakote)
Mechanism of Action
-
Increases GABA levels, stabilizing neuronal firing and reducing CNS excitability.
Therapeutic Uses
-
Acute mania, rapid cycling bipolar disorder.
-
Effective in mixed episodes.
Adverse Effects
-
Hepatotoxicity: nausea, vomiting, fatigue, jaundice.
-
Pancreatitis: abdominal pain, nausea, vomiting.
-
Weight gain, GI upset, thrombocytopenia.
-
Teratogenicity (avoid in pregnancy).
Monitoring
-
LFTs, CBC, serum drug levels.
-
Amylase levels if pancreatitis suspected.
Nursing Insights
-
Administer with food or use enteric-coated tablets to minimize GI effects.
-
Advise clients to report abdominal pain, jaundice, or bruising.
-
Avoid in children <2 years old and in liver disease.
-
Monitor concurrent medications (phenytoin, phenobarbital) as levels may increase.
Mechanism of Action
-
Stabilizes neuronal membranes by inhibiting sodium and calcium channels.
-
Reduces release of excitatory neurotransmitters such as glutamate.
Therapeutic Uses
-
Best for bipolar depression and maintenance therapy.
-
Prevention of depressive episodes in bipolar disorder.
Adverse Effects
-
CNS: dizziness, headache, blurred or double vision, nausea, vomiting.
-
Severe dermatologic: Stevens–Johnson syndrome (rash must be reported immediately).
Monitoring
-
Monitor for rash, CNS side effects, and liver function if indicated.
-
Adjust dosage if used with carbamazepine, phenytoin, phenobarbital, or valproic acid.
Nursing Insights
-
Educate clients to report any rash immediately.
-
Start low, titrate slowly to reduce risk of severe skin reactions.
-
Caution in combination with enzyme-inducing or inhibiting drugs.
Atypical antipsychotics
Used for: Acute mania, bipolar depression, and maintenance therapy.
Advantages: Rapid symptom control, mood stabilization, effective in psychosis.
Risks: Metabolic syndrome, weight gain, extrapyramidal symptoms (EPS), sedation.
Mechanism of Action
- Dopamine and serotonin receptor antagonist.
Therapeutic Uses
- Acute mania, mixed episodes, maintenance therapy.
Adverse Effects
- Weight gain, hyperglycemia, dyslipidemia, sedation, anticholinergic effects.
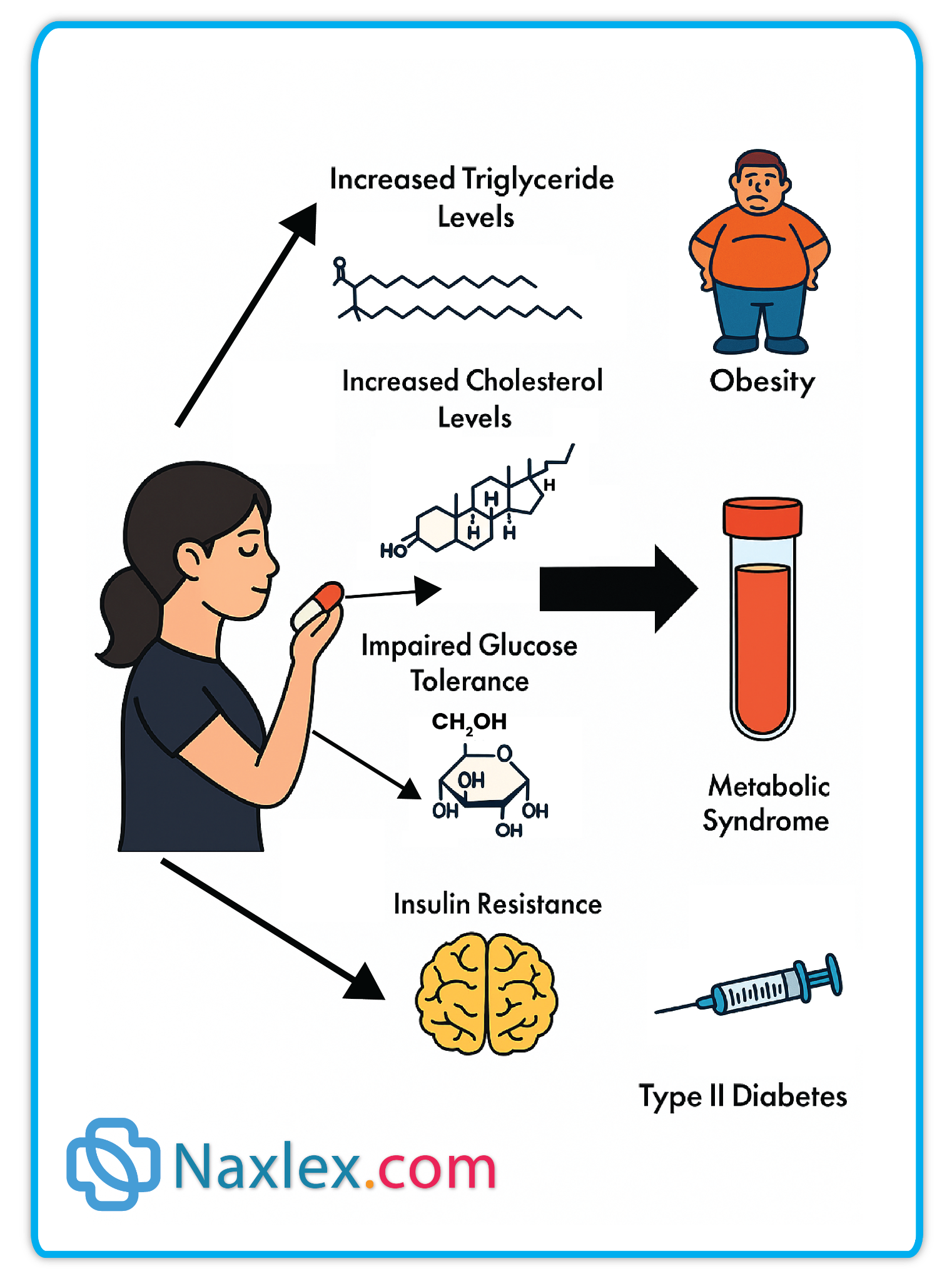
Nursing Insights
- Monitor metabolic parameters (weight, blood glucose, lipids).
- Assess for EPS and orthostatic hypotension.
2. Risperidone (Risperdal)
Mechanism of Action
- Serotonin-dopamine antagonist.
Therapeutic Uses
- Acute mania, bipolar maintenance, adjunct for depressive episodes.
Adverse Effects
- EPS, hyperprolactinemia, weight gain, sedation.
Nursing Insights
- Monitor for EPS and prolactin-related changes (galactorrhea, menstrual irregularities).
- Assess metabolic profile regularly.
Mechanism of Action
- Serotonin-dopamine antagonist; sedating properties due to histamine antagonism.
Therapeutic Uses
- Acute mania, bipolar depression, maintenance therapy.
Adverse Effects
- Sedation, weight gain, orthostatic hypotension, metabolic syndrome.
Nursing Insights
- Advise bedtime administration to minimize daytime sedation.
- Monitor weight, blood pressure, and blood glucose.
Mechanism of Action
- Dopamine and serotonin receptor antagonist.
Therapeutic Uses
- Bipolar depression, adjunct therapy for bipolar maintenance.
Adverse Effects
- Nausea, akathisia, somnolence, minimal metabolic effects compared to other antipsychotics.
Nursing Insights
- Take with food to enhance absorption.
- Monitor for EPS and akathisia.
- Assess adherence and depressive symptom improvement.
Mechanism of Action
- Partial dopamine agonist and serotonin antagonist.
Therapeutic Uses
- Acute mania, mixed episodes, adjunct for bipolar depression, maintenance therapy.
Adverse Effects
- Akathisia, insomnia, nausea, minimal metabolic risk.
Nursing Insights
- Monitor for restlessness or agitation (akathisia).
- Assess sleep patterns and adherence.
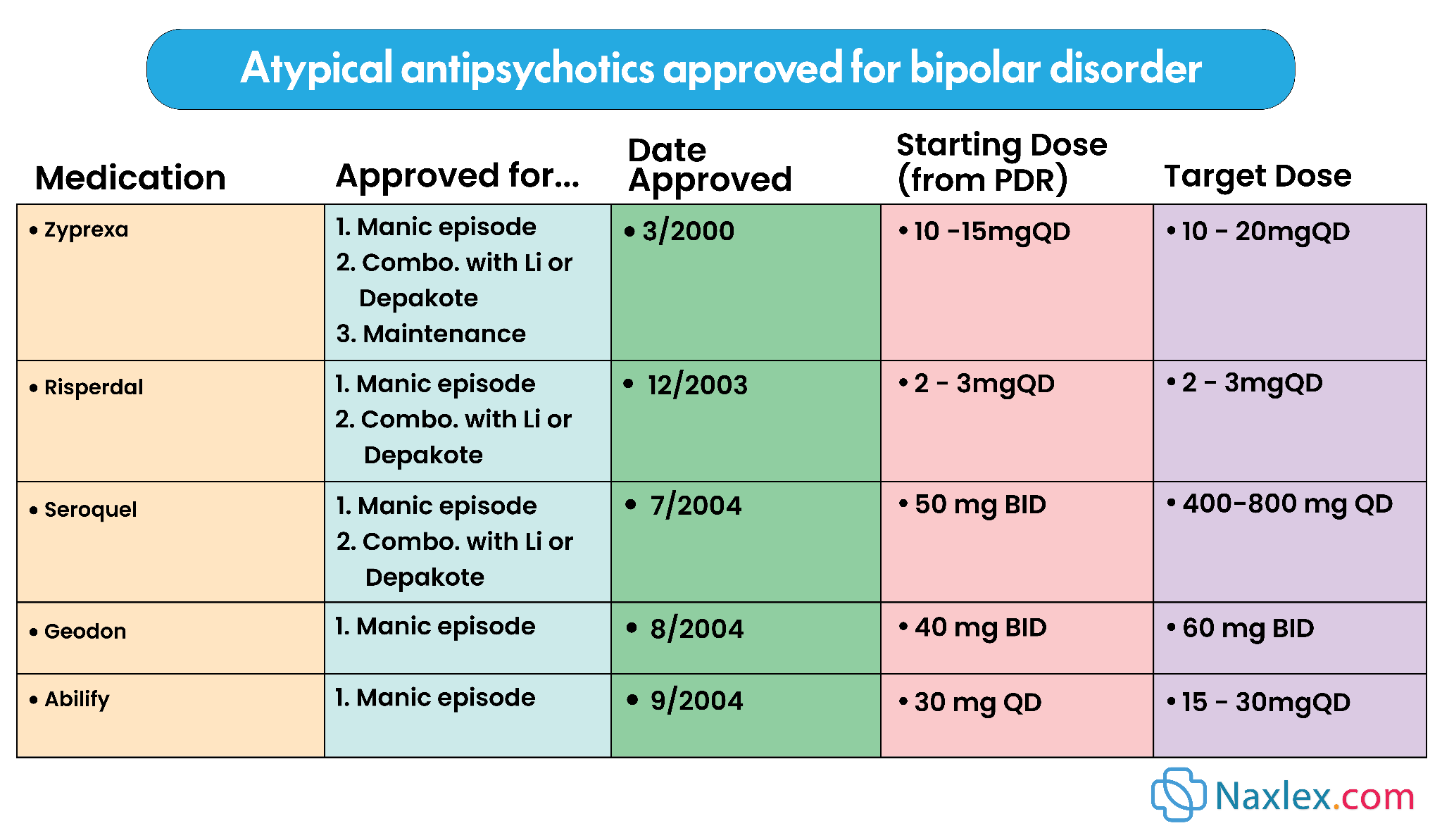
Nursing Evaluation of Effectiveness (Mood Stabilizers & Antipsychotics)
- Stabilization of mood: reduction in manic or depressive symptoms.
- Ability to perform ADLs, maintain sleep and appetite.
- Improved social and occupational functioning.
- Absence of severe side effects or toxicity.
Summary
Depression
- Persistent mood disorder causing sadness, hopelessness, anhedonia, and impaired functioning.
- Types: MDD, dysthymia, situational, perinatal, seasonal, psychotic.
- Assessment: Rule out medical/drug causes, suicidal ideation, substance use, psychosocial factors.
- Treatment: Pharmacologic (SSRIs, atypical antidepressants, TCAs, MAOIs), psychotherapy, somatic therapies (ECT, rTMS).
- Nursing: Monitor for suicidal risk, adherence, side effects, serotonin syndrome, family/caregiver support.
Antidepressants
- SSRIs: Inhibit serotonin reuptake; adverse effects include sexual dysfunction, insomnia, hyponatremia, serotonin syndrome.
- Atypical antidepressants: Variable mechanisms; examples include bupropion, venlafaxine, duloxetine, mirtazapine, trazodone. Monitor seizure risk, sedation, BP, weight.
- TCAs: Inhibit norepinephrine/serotonin reuptake; monitor cardiac function, anticholinergic effects, sedation.
- MAOIs: Inhibit monoamine oxidase; risk of hypertensive crisis with tyramine-rich foods; avoid SSRIs/TCAs.
Bipolar Disorder
- Chronic mood disorder with alternating depressive and manic/hypomanic episodes.
- Bipolar I: ≥1 manic episode; Bipolar II: hypomania + depression; Cyclothymic: mild mood fluctuations ≥2 years.
- Assessment: Suicidal ideation, safety, adherence, comorbidities (substance abuse, metabolic syndrome).
Drugs for Bipolar Disorder
Mood Stabilizers
- Lithium: Alters sodium transport; narrow therapeutic index; monitor levels, renal/thyroid function; educate on hydration/sodium intake.
- Valproic Acid: Increases GABA; monitor LFTs, CBC; risk of hepatotoxicity, pancreatitis, weight gain.
- Carbamazepine: Sodium channel blocker; monitor CBC, LFTs, sodium; risk of hematologic toxicity, Stevens–Johnson syndrome.
- Lamotrigine: Prevents bipolar depression; monitor for rash/Stevens–Johnson syndrome.
Atypical Antipsychotics
- Olanzapine: Metabolic monitoring; sedation, weight gain.
- Risperidone: EPS, hyperprolactinemia, weight gain.
- Quetiapine: Sedation, metabolic risk; bedtime dosing.
- Lurasidone: Take with food; monitor EPS/akathisia.
- Aripiprazole: Minimal metabolic risk; monitor for akathisia/insomnia.
Nursing Insights
- Ensure safety during manic/depressive episodes.
- Educate on medication adherence, side effects, and toxicity.
- Encourage structured routines, adequate sleep, hydration, avoidance of alcohol/stimulants.
- Engage family/caregivers in recognizing early warning signs.
- Evaluate effectiveness: mood stabilization, ADL performance, social functioning, minimal side effects.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Drugs Used for Depressive and Bipolar Disorders
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


