Please set your exam date
Multiple Sclerosis, ALS, and Myasthenia Gravis
Study Questions
Practice Exercise 1
A nurse is conducting a health history for a client suspected of having multiple sclerosis (MS). Which of the following symptoms, if reported by the client, would the nurse identify as an early, common manifestation of MS?
Explanation
Sudden, unilateral vision loss or blurring often caused by optic neuritis is one of the most common early manifestations of multiple sclerosis. This results from inflammation and demyelination of the optic nerve, which disrupts visual signal transmission. Early MS symptoms are often sensory and visual disturbances, which may resolve partially or completely before recurring. Recognizing these initial signs is critical for early diagnosis and management, as MS often presents in relapsing-remitting patterns.
Rationale for correct answer:
2. Sudden, unilateral vision loss or blurring: Optic neuritis is a hallmark early symptom of MS. It is characterized by pain with eye movement and visual changes in one eye, often preceding or accompanying other neurological symptoms. This occurs due to immune-mediated demyelination in the central nervous system.
Rationale for incorrect answers:
1. Severe, stabbing pain in the face: This describes trigeminal neuralgia, which can occur in MS but is more typical in later stages, not as a primary early manifestation.
3. Progressive muscle weakness in the hands and feet: Weakness can occur in MS but usually develops later or in combination with other neurological signs, rather than being the most common early symptom.
4. Auditory hallucinations and cognitive decline: Cognitive changes can occur in advanced MS, but hallucinations are not a typical manifestation and should prompt evaluation for other conditions.
Take-home points:
- Early MS often presents with visual disturbances, particularly optic neuritis.
- Symptoms can be transient and may improve between relapses.
- Prompt recognition of early neurological signs can help initiate treatment to slow disease progression.
- MS involves immune-mediated demyelination of the CNS, affecting vision, sensation, and movement over time.
A nurse is providing education to a client with a new diagnosis of multiple sclerosis. The nurse should include which of the following instructions to help the client manage their symptoms and prevent exacerbations? Select all that apply
Explanation
Clients with multiple sclerosis benefit from measures that reduce fatigue, prevent overheating, and avoid symptom triggers. Strenuous activity can lead to increased body temperature, worsening neurological symptoms (Uhthoff’s phenomenon). Lukewarm baths prevent heat-induced symptom flare-ups. Balancing activity with rest periods helps manage fatigue one of the most common MS complaints.
Rationale for correct answers:
1. Avoid strenuous exercise and overexertion: Overheating from intense activity can temporarily worsen neurological deficits in MS. Light to moderate exercise is beneficial, but overexertion should be avoided.
2. Take lukewarm baths rather than hot baths: Heat can exacerbate MS symptoms by slowing nerve conduction in demyelinated fibers. Lukewarm baths help avoid heat-related flare-ups.
4. Consider a balance of rest and activity to combat fatigue: Scheduled rest periods prevent exhaustion and help maintain daily function.
Rationale for incorrect answers:
3. Increase your intake of high-fat dairy products: There is no evidence that high-fat dairy helps MS; a balanced, healthy diet is recommended to support overall health.
5. Limit fluid intake to prevent bladder urgency: Restricting fluids can lead to dehydration and urinary tract infections, which may trigger MS exacerbations. Bladder training is preferred over fluid restriction.
Take-home points:
- MS symptoms often worsen with heat and fatigue; prevention strategies are key.
- Moderate exercise, cooling measures, and adequate rest improve daily functioning.
- Fluid restriction is not recommended; hydration supports overall health and bladder function.
- Early lifestyle adjustments can help maintain independence and reduce relapses.
A client with relapsing-remitting multiple sclerosis is prescribed interferon beta-1α. The nurse should instruct the client to monitor for which of the following common side effects?
Explanation
Flulike symptoms such as fever, chills, muscle aches, and fatigue are common side effects of interferon beta-1α therapy. These symptoms usually occur within hours of injection and tend to lessen over time. Premedicating with acetaminophen or ibuprofen and administering the injection in the evening can help reduce discomfort. Monitoring and managing these effects is important to promote adherence to treatment.
Rationale for correct answer:
2. Flulike symptoms: Interferon beta-1α triggers an immune response that can mimic viral infection symptoms. This side effect is most noticeable at the start of therapy and generally improves with continued use.
Rationale for incorrect answers:
1. Increased blood pressure: Interferon beta-1α is not typically associated with hypertension; cardiovascular monitoring is not a primary concern with this medication.
3. Weight gain: This is not a known side effect of interferon therapy; lifestyle factors are more likely to influence weight in MS patients.
4. Constipation: While constipation can occur in MS due to neurological effects, it is not a common adverse effect of interferon beta-1α.
Take-home points:
- Interferon beta-1a commonly causes transient flulike symptoms after injection.
- Premedication and evening dosing can improve tolerability.
- Side effects often decrease with continued therapy, supporting adherence.
- Patient education on symptom management promotes long-term treatment success in MS.
A nurse is assessing a client with multiple sclerosis who is experiencing cerebellar symptoms. The nurse should anticipate which of the following findings? Select all that apply
Explanation
Cerebellar symptoms in multiple sclerosis arise from demyelination affecting the cerebellum and its pathways, which coordinate voluntary movement, balance, and speech. Ataxia, intention tremors, and dysarthria are hallmark cerebellar signs.
Rationale for correct answers:
1. Ataxia: Indicates impaired balance and coordination, a classic cerebellar manifestation in MS.
3. Intention tremors: Occur during purposeful movement and are strongly linked to cerebellar dysfunction.
4. Dysarthria: Speech changes result from impaired coordination of the muscles used for speaking.
Rationale for incorrect answers:
2. Diplopia: Double vision is related to brainstem or cranial nerve involvement, not primarily cerebellar function.
5. Numbness and tingling: These are sensory symptoms caused by lesions in sensory pathways, not the cerebellum.
Take-home points:
- Cerebellar involvement in MS affects coordination, voluntary movement control, and speech.
- Ataxia, intention tremors, and dysarthria are hallmark cerebellar signs.
- Sensory disturbances and visual changes arise from other CNS lesion sites, not the cerebellum.
- Symptom location in MS reflects the specific neural pathways affected by demyelination.
A nurse is discussing the pathophysiology of multiple sclerosis with a client. The nurse accurately explains that the disease is characterized by:
Explanation
Multiple sclerosis is an autoimmune disorder in which the body’s immune system attacks the myelin sheath the protective covering surrounding nerve fibers in the central nervous system (CNS). This demyelination disrupts the efficient transmission of electrical impulses along neurons, leading to a wide range of neurological symptoms. Over time, nerve fibers themselves may become damaged, resulting in permanent disability.
Rationale for correct answer:
3. An autoimmune attack on the myelin sheath of the central nervous system: MS involves inflammation and immune-mediated destruction of CNS myelin, causing slowed or blocked nerve conduction and contributing to relapsing-remitting or progressive neurological deficits.
Rationale for incorrect answers:
1. The degeneration of motor neurons in the brain and spinal cord: This describes amyotrophic lateral sclerosis (ALS), not MS.
2. A defect in nerve impulse transmission at the neuromuscular junction: This is characteristic of myasthenia gravis, not MS.
4. A decrease in dopamine production in the basal ganglia: This occurs in Parkinson’s disease, not MS.
Take-home points:
- MS is caused by immune-mediated demyelination of CNS nerve fibers.
- Damaged myelin impairs nerve conduction, producing diverse neurological symptoms.
- Over time, axonal loss can lead to permanent disability.
- MS differs from other neurological disorders such as ALS, myasthenia gravis, and Parkinson’s disease in both cause and pathology.
Practice Exercise 2
A nurse is caring for a client with Amyotrophic Lateral Sclerosis (ALS) who has developed dysphagia. Which of the following nursing interventions is most appropriate to ensure the client's safety and nutritional intake?
Explanation
Consult with a speech-language pathologist to develop a swallowing plan and recommend thickened liquids is the most appropriate intervention. In ALS, dysphagia results from progressive weakness of the bulbar muscles, increasing the risk of aspiration and malnutrition. A speech-language pathologist (SLP) can assess swallowing function, recommend safe food and liquid textures, and teach compensatory strategies to reduce aspiration risk.
Rationale for correct answer:
3. Consult with a speech-language pathologist: The SLP provides individualized assessment and interventions, including recommending thickened liquids, altering food textures, and teaching posture or swallowing techniques to improve safety during eating.
Rationale for incorrect answers:
1. Encourage a solid, high-fiber diet: Solid foods may be difficult to swallow and increase aspiration risk; diet should be modified to match the client’s swallowing ability.
2. Position with head tilted back: Tilting the head back actually increases the risk of aspiration; safer positions may include chin-tuck, as recommended by an SLP.
4. Provide a straw with all beverages: Using a straw can worsen aspiration risk in dysphagic patients unless specifically approved by the SLP.
Take home points:
- ALS-related dysphagia requires specialized swallowing assessment and diet modification.
- Safety during meals focuses on preventing aspiration while maintaining adequate nutrition.
- A speech-language pathologist is an essential part of the care team for patients with swallowing difficulties.
A patient with advanced ALS is having difficulty swallowing and frequently chokes while eating. The nurse should anticipate which of the following interventions?
Explanation
In advanced ALS, dysphagia increases the risk of aspiration, malnutrition, and dehydration. A percutaneous endoscopic gastrostomy (PEG) tube provides a long-term, safe method for delivering nutrition, hydration, and medications when oral intake is unsafe or inadequate. Early referral for PEG placement before respiratory function declines severely is recommended to optimize outcomes.
Rationale for correct answer:
3. Referring the patient for a percutaneous endoscopic gastrostomy (PEG) tube placement: PEG placement ensures nutritional support while minimizing aspiration risk. It is preferred for long-term feeding in ALS patients with progressive dysphagia.
Rationale for incorrect answers:
1. Initiating a pureed diet: While a texture-modified diet may be used in early dysphagia, frequent choking indicates a higher aspiration risk requiring more definitive intervention.
2. Inserting a nasogastric tube for feeding: NG tubes are typically for short-term use and can be uncomfortable, with higher risk of dislodgement; they are not ideal for long-term ALS management.
4. Encouraging the patient to continue eating as long as possible to maintain muscle strength: This approach ignores the significant aspiration risk and could lead to pneumonia or respiratory distress.
Take-home points:
- Dysphagia in ALS increases the risk of aspiration and malnutrition.
- PEG tubes provide a safer, long-term feeding option when oral intake is no longer safe.
- Early planning for PEG placement before advanced respiratory decline improves outcomes.
- Diet modification is helpful in early stages, but advanced disease requires more definitive feeding interventions.
The nurse is assessing a patient with a suspected diagnosis of ALS. Which of the following findings would be consistent with the disease? Select all that apply
Explanation
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disorder affecting both upper and lower motor neurons. Upper motor neuron involvement produces increased deep tendon reflexes and spasticity. While muscle weakness is common, it typically begins asymmetrically and progresses rather than starting equally in all limbs. ALS generally spares ocular movements and bladder function until very late in the disease.
Rationale for correct answers:
1. Increased deep tendon reflexes: Indicates upper motor neuron involvement, a hallmark feature of ALS.
2. Presence of spasticity: Another sign of upper motor neuron damage, leading to stiffness and resistance to movement.
5. Preserved eye movement and bladder function: ALS usually spares extraocular muscles and bladder control, differentiating it from other neurological disorders.
Rationale for incorrect answers:
3. Symmetric muscle weakness in all four limbs: Weakness in ALS often starts in one limb or region and then spreads; early symmetry is uncommon.
4. Intention tremor: This is associated with cerebellar disorders such as multiple sclerosis, not ALS.
Take-home points:
- ALS involves both upper and lower motor neuron degeneration.
- Early signs include increased reflexes, spasticity, and asymmetric muscle weakness.
- Eye movements and bladder function are typically preserved until late stages.
- Symptom distribution and preservation of certain functions help distinguish ALS from other neurodegenerative diseases.
Which of the following statements about Amyotrophic Lateral Sclerosis (ALS) are correct? Select all that apply
Explanation
ALS is a progressive neurodegenerative disease involving both upper and lower motor neurons, leading to mixed signs such as spasticity and muscle atrophy. Early symptoms often include muscle cramps, twitching, and weakness. Sensory neurons are generally spared, and most patients retain normal sensation. Cognitive function is usually preserved, though mild cognitive or behavioral changes can occur in some cases. Respiratory muscle weakness ultimately leads to respiratory failure, the most common cause of death in ALS.
Rationale for correct answers:
2. The disease is characterized by the degeneration of both upper and lower motor neurons: This explains the combination of hyperreflexia, spasticity, and muscle wasting seen in ALS.
3. Early symptoms often include muscle cramps and fasciculations: These result from irritation of damaged motor neurons and are often among the first signs.
5. The most common cause of death in ALS patients is respiratory failure: Progressive weakness of the diaphragm and intercostal muscles leads to inadequate ventilation.
Rationale for incorrect answers:
1. ALS primarily affects the sensory neurons, leading to a loss of sensation: Sensory function is typically intact in ALS, as the disease targets motor neurons.
4. Patients with ALS typically experience a rapid loss of cognitive function: Cognitive decline is not a defining feature of ALS; most patients remain mentally alert.
Take-home points:
- ALS affects both upper and lower motor neurons, producing mixed neurological signs.
- Sensory pathways are usually preserved, helping distinguish ALS from other conditions.
- Fasciculations, cramps, and progressive weakness are common early symptoms.
- Respiratory failure is the leading cause of death in ALS, making respiratory monitoring essential.
When planning care for a patient with ALS, what is the most important long-term goal for the nurse to focus on?
Explanation
Because ALS is a progressive and incurable disease, the primary long-term nursing goal is to maximize the patient’s functional abilities and quality of life for as long as possible. This involves early interventions to maintain mobility, communication, nutrition, and respiratory function, as well as emotional and psychosocial support. While preventing complications, controlling pain, and promoting emotional well-being are all important, they are part of the broader overarching goal of optimizing quality of life and independence.
Rationale for correct answer:
2. Maximizing the patient's functional abilities and quality of life for as long as possible: This holistic goal guides all aspects of ALS care, from physical therapy to respiratory management and psychosocial support.
Rationale for incorrect answers:
1. Helping the patient maintain a positive attitude toward their diagnosis: Emotional support is important, but it is one component of the larger aim to preserve quality of life.
3. Preventing the patient from developing aspiration pneumonia: This is a critical short-term objective, but it is a specific complication-prevention goal, not the overarching long-term focus.
4. Ensuring the patient remains pain-free throughout the disease process: Pain management is essential for comfort but does not address the full scope of the disease’s impact.
Take-home points:
- ALS care centers on preserving function, independence, and quality of life for as long as possible.
- Goals should address physical, emotional, and social needs through a multidisciplinary approach.
- Preventing complications like aspiration, respiratory failure, and immobility is part of achieving the larger goal.
- Early proactive care planning improves patient outcomes and supports dignity in progressive illness.
Practice Exercise 3
A nurse is conducting an initial assessment on a client presenting with signs of myasthenia gravis. The nurse should anticipate which of the following clinical manifestations? Select all that apply
Explanation
Myasthenia gravis (MG) is a chronic autoimmune disorder affecting the neuromuscular junction, leading to fluctuating skeletal muscle weakness that worsens with activity and improves with rest. Weakness commonly affects ocular muscles, causing diplopia and ptosis. Fine motor tasks, such as writing, become difficult due to fatigable weakness. Cognitive function is typically preserved, and MG does not cause mask-like facies, which is more typical of Parkinson’s disease.
Rationale for correct answers:
2. Muscle weakness that improves with rest: Hallmark sign of MG due to impaired acetylcholine receptor function.
4. Difficulty with fine motor skills, such as writing: Weakness in small muscle groups is common, especially with repeated use.
5. Diplopia and ptosis: Early and common signs due to ocular muscle involvement.
Rationale for incorrect answers:
1. Progressive, symmetrical weakness of the limbs: MG weakness is not typically symmetrical or steadily progressive; it fluctuates throughout the day.
3. A mask-like facial expression: Seen in Parkinson’s disease, not MG.
6. Cognitive decline and memory loss: MG does not affect cognitive function; symptoms are purely motor.
Take-home points:
- MG causes fluctuating skeletal muscle weakness that improves with rest.
- Ocular muscles are often affected first, leading to diplopia and ptosis.
- Fine motor skill difficulties arise from fatigable weakness in small muscle groups.
- Cognitive function remains intact, helping differentiate MG from other neurological disorders.
A client with myasthenia gravis is prescribed pyridostigmine (Mestinon). The nurse should instruct the client to take this medication at which of the following times?
Explanation
Pyridostigmine is an anticholinesterase medication that increases the availability of acetylcholine at the neuromuscular junction, improving muscle strength. Taking it 30 to 60 minutes before meals ensures peak muscle strength during eating, reducing the risk of aspiration and making chewing and swallowing easier.
Rationale for correct answer:
3. 30 to 60 minutes before a meal to improve swallowing: Timing the medication before meals aligns peak drug action with the period when strong bulbar muscle function is needed for safe eating.
Rationale for incorrect answers:
1. Immediately upon waking up to prevent morning weakness: While some patients may need an early dose for morning activity, the critical priority is to time doses around meals to ensure safe swallowing.
2. 45 to 60 minutes after a meal to aid in digestion: Post-meal dosing misses the opportunity to improve chewing and swallowing function during the meal.
4. At bedtime to ensure adequate rest: MG symptoms are less problematic during sleep, so dosing at bedtime offers little benefit.
Take-home points:
- Pyridostigmine improves muscle strength by enhancing neuromuscular transmission.
- Dosing should be timed to match activities requiring maximum muscle function, such as eating.
- Taking the medication before meals helps prevent aspiration in patients with bulbar muscle weakness.
- Consistent dosing and symptom tracking are key to optimizing MG management.
A client with myasthenia gravis is experiencing a myasthenic crisis. The nurse should prepare to implement which of the following interventions? Select all that apply
Explanation
A myasthenic crisis is a life-threatening exacerbation of myasthenia gravis characterized by severe muscle weakness, including the respiratory muscles, often triggered by infection, stress, or inadequate medication. Immediate priorities include airway and breathing support, rapid immunomodulatory therapy, and diagnostic confirmation if the cause of weakness is unclear. The edrophonium (Tensilon) test can help differentiate a myasthenic crisis from a cholinergic crisis.
Rationale for correct answers:
2. Preparing for mechanical ventilation due to respiratory muscle failure: Respiratory compromise is the leading cause of mortality in myasthenic crisis, requiring readiness for intubation and ventilation.
4. Administering IV immunoglobulin (IVIG) as a rapid immunosuppressant therapy: IVIG provides fast immune suppression, improving symptoms within days.
6. Administering a dose of edrophonium (Tensilon) to confirm the diagnosis: If diagnosis is uncertain, edrophonium can distinguish between myasthenic and cholinergic crisis—symptoms improve temporarily in a myasthenic crisis.
Rationale for incorrect answers:
1. Administering a dose of atropine to counteract muscle weakness: Atropine is not used to treat muscle weakness; it is used to counteract cholinergic side effects, not myasthenic crisis.
3. Withholding all doses of anticholinesterase medications: These medications are usually continued unless contraindicated; withholding can worsen weakness.
5. Educating the client on energy-conservation techniques: This is an important long-term management strategy, but it is not a priority during a crisis.
Take-home points:
- Myasthenic crisis is a medical emergency due to the risk of respiratory failure.
- Airway support and rapid immunomodulatory treatment are top priorities.
- The edrophonium test helps differentiate between myasthenic and cholinergic crisis.
- Prompt intervention greatly improves survival and recovery.
A nurse is providing discharge teaching to a client with myasthenia gravis. The nurse should advise the client to avoid which of the following activities or situations that can exacerbate their symptoms?
Explanation
Avoiding exposure to extreme cold or heat is important for clients with myasthenia gravis because temperature extremes can worsen muscle weakness and fatigue. Heat can increase metabolic demands, impair neuromuscular transmission, and precipitate a myasthenic crisis. Cold can also impair muscle function and exacerbate weakness. Maintaining a stable, comfortable temperature helps minimize symptom flare-ups and supports optimal daily functioning.
Rationale for correct answer:
4. Avoiding exposure to extreme cold or heat: Myasthenia gravis symptoms are highly sensitive to changes in body temperature. Extreme heat can worsen neuromuscular transmission, while cold can impair muscle contractility, both leading to increased weakness.
Rationale for incorrect answers:
1. Taking a lukewarm shower: This is safe and may even help with comfort, as it avoids extreme temperatures.
2. Engaging in moderate-intensity exercise: Gentle, balanced exercise is beneficial as long as the client avoids overexertion and rests when fatigued.
3. Receiving the flu vaccination: Vaccination is generally recommended to prevent respiratory infections, which can trigger symptom exacerbation.
Take home points
- Myasthenia gravis symptoms can be worsened by extreme environmental temperatures.
- Heat increases metabolic stress and can precipitate a crisis; cold can impair muscle function.
- Stable, moderate environmental conditions and pacing of activities are key in symptom management.
The primary pathophysiology of myasthenia gravis involves an autoimmune response that results in the destruction of what?
Explanation
Myasthenia gravis is caused by an autoimmune attack in which antibodies target and destroy acetylcholine receptors (AChRs) at the neuromuscular junction. This prevents effective transmission of nerve impulses to skeletal muscles, leading to weakness that worsens with activity and improves with rest.
Rationale for correct answer:
3. Acetylcholine (ACh) receptors at the neuromuscular junction: The destruction or blockade of AChRs reduces the number of available receptors for acetylcholine, impairing synaptic transmission and causing muscle weakness.
Rationale for incorrect answers:
1. Dopamine-producing cells in the basal ganglia: This occurs in Parkinson’s disease, not myasthenia gravis.
2. The myelin sheath in the central nervous system: Demyelination of CNS neurons occurs in multiple sclerosis.
4. Lower motor neurons in the spinal cord: Damage here is seen in conditions like amyotrophic lateral sclerosis (ALS), not myasthenia gravis.
Take home points
- Myasthenia gravis is an autoimmune disease targeting acetylcholine receptors at the neuromuscular junction.
- Impaired receptor function leads to fluctuating muscle weakness.
- The disease is distinct from disorders affecting dopamine, myelin, or lower motor neurons.
Comprehensive Questions
A nurse is caring for a client who was diagnosed with Amyotrophic Lateral Sclerosis (ALS) approximately 1 year ago. Which of the following client findings should the nurse anticipate? Select all that apply
Explanation
Clients with ALS typically develop progressive muscle weakness due to the degeneration of upper and lower motor neurons, while sensory and cognitive functions are usually preserved. Weakness in respiratory muscles leads to an ineffective cough, increasing the risk for pneumonia and other respiratory complications.
Rationale for correct answer:
3. Incontinence: Incontinence due to muscle weakness is a finding in a client who has ALS.
4. Ineffective cough: ALS causes weakness of respiratory muscles, making it difficult for the client to clear secretions effectively, which can lead to respiratory infections and compromised oxygenation.
Rationale for incorrect answers:
1. Loss of sensation: Sensory pathways remain intact in ALS; sensation is usually unaffected.
2. Fluctuations in blood pressure: Autonomic nervous system involvement is rare in ALS, so blood pressure regulation remains largely normal.
5. Loss of cognitive function: Cognition is generally preserved, though a small subset of clients may develop frontotemporal dementia, this is not the norm.
Take home points
- ALS affects motor neurons, leading to muscle weakness and atrophy, but typically spares sensory and cognitive function.
- Respiratory muscle weakness and ineffective cough are key complications.
- Early interventions to support airway clearance can improve quality of life and reduce complications.
A nurse is caring for a client who has myasthenia gravis (MG) and has developed drooping eyelids. Which of the following actions should the nurse take? Select all that apply
Explanation
Drooping eyelids in myasthenia gravis can result in incomplete eyelid closure, which exposes the eyes to dryness, irritation, and injury. Preventive measures such as lubrication, protection from environmental elements, and nighttime taping can help preserve vision and comfort. In addition, rest periods reduce muscle fatigue and allow for better symptom control, as weakness in MG worsens with sustained activity.
Rationale for correct answers:
1. Apply lubricating eye drops: This prevents corneal dryness and irritation by keeping the eyes moist despite incomplete eyelid closure. Without adequate lubrication, the cornea can become damaged, leading to discomfort and vision problems.
4. Tape eyes closed at night: Taping helps ensure the eyes remain fully closed during sleep, preventing drying and potential corneal injury. This is especially important because many individuals with MG are unable to maintain eyelid closure overnight due to muscle weakness.
Rationale for incorrect answer:
2. Encourage use of sunglasses: Wearing sunglasses does not prevent corneal dryness and irritation.
3. Support the head with pillows: While this may help a client with neck weakness, it does not address the risks or complications associated with drooping eyelids in MG. Ptosis requires targeted interventions to protect the eyes rather than general head support.
5. Provide for periods of rest during the day: Promoting rest does not reduce eyelid drooping in the client who has MG.
Take home points
- Ptosis in MG can cause corneal dryness and injury due to incomplete eyelid closure.
- Eye lubrication, physical protection, and nighttime measures are essential to maintain vision.
- Rest periods are critical in MG to manage fatigue and preserve muscle function.
A nurse instructs a client who has MG about home care and the risk factors that can exacerbate the disease. Which of the following client statements indicates a need for further teaching?
Explanation
Clients with myasthenia gravis should avoid hot environments and heat exposure because elevated body temperature can worsen muscle weakness and trigger a myasthenic crisis. A daily warm bath may seem relaxing, but it can raise core body temperature and exacerbate symptoms, making it unsafe for MG management.
Rationale for correct answer:
3. “I will soak in a warm bath every day.” Warm baths can increase body temperature, which impairs neuromuscular transmission and can worsen muscle weakness in MG. Overheating is a known trigger for exacerbations and should be avoided to prevent symptom flares or a potential crisis.
Rationale for incorrect answers:
1. “I should take my medication 45 min before meals.” This is correct because taking anticholinesterase medication before meals ensures optimal muscle strength for chewing and swallowing. Proper timing reduces the risk of aspiration and improves nutritional intake.
2. “I have suction equipment at home in case I start to choke.” This is appropriate as MG can cause bulbar muscle weakness, increasing the risk of choking and aspiration. Having suction available allows for prompt airway clearance and helps prevent complications such as pneumonia.
4. “I ordered a medical identification bracelet to wear.” This is a correct action because it alerts healthcare professionals to the client’s diagnosis in an emergency. Rapid recognition of MG is essential for safe and effective treatment, especially during a crisis.
Take home points
- Heat exposure, including warm baths, can worsen MG symptoms and should be avoided.
- Proper medication timing supports safe swallowing and eating.
- Safety measures like suction equipment and medical alert identification improve emergency preparedness in MG.
A nurse is beginning a physical assessment of a client who was recently diagnosed with multiple sclerosis (MS). Which of the following findings should the nurse expect? Select all that apply
Explanation
Multiple sclerosis is a demyelinating disease of the central nervous system that disrupts nerve impulse transmission. Clients often present with sensory changes such as paresthesia, visual disturbances like involuntary eye movements, and impaired coordination such as ataxia. These symptoms occur due to lesions in various areas of the brain and spinal cord.
Rationale for correct answers:
1. Areas of paresthesia: MS frequently causes numbness, tingling, or “pins and needles” sensations due to demyelination of sensory pathways. These altered sensations may occur in isolated patches and can change location over time.
2. Involuntary eye movements: Nystagmus in MS results from lesions in the brainstem or cerebellum that affect eye movement control. This can cause dizziness, visual disturbance, and difficulty focusing.
5. Ataxia: Poor muscle coordination in MS is related to cerebellar involvement. Clients may present with unsteady gait, difficulty with balance, and clumsy movements.
Rationale for incorrect answers:
3. Alopecia: Hair loss is not a typical symptom of MS and is not caused by demyelination. If alopecia occurs, it is more likely related to medication side effects or another unrelated condition.
4. Increased salivation: MS is more often associated with difficulty swallowing and sometimes dry mouth due to muscle weakness, not excessive saliva production.
Take home points
- MS causes sensory, visual, and motor deficits due to CNS demyelination.
- Paresthesia, nystagmus, and ataxia are hallmark findings in early disease.
- Alopecia and increased salivation are not expected MS manifestations.
The nurse is reinforcing teaching with a newly diagnosed patient with amyotrophic lateral sclerosis. Which statement would be appropriate to include in the teaching?
Explanation
Amyotrophic lateral sclerosis (ALS) is a progressive neurodegenerative disease affecting motor neurons in the brain and spinal cord, leading to muscle weakness, atrophy, and eventual paralysis. However, unlike many other neurological disorders, ALS typically does not impair cognitive function, meaning patients remain mentally alert and aware as the disease progresses. This understanding is important for patient education, emotional preparation, and care planning.
Rationale for correct answer:
4. This is a progressing disease that eventually results in permanent paralysis, though you will not lose any cognitive function: This accurately reflects the nature of ALS, helping the patient understand disease progression and prepare for future needs.
Rationale for incorrect answers:
1. ALS results from an excess chemical in the brain, and the symptoms can be controlled with medication: There is no single excess chemical causing ALS; while medications like riluzole can modestly slow progression, there is no cure.
2. Even though the symptoms you are experiencing are severe, most people recover with treatment: ALS is not reversible; progression continues despite therapy.
3. You need to consider advance directives now, since you will lose cognitive function as the disease progresses: Cognitive decline is not a typical feature of ALS; advance directives are important for other reasons, such as anticipated physical decline, but not due to cognitive loss.
Take-home points:
- ALS is a progressive motor neuron disease causing muscle weakness, paralysis, and respiratory failure.
- Cognitive function is typically preserved, allowing patients to remain mentally engaged.
- There is no cure, but certain medications and supportive care can improve quality of life.
- Early care planning is essential to address future mobility, communication, and respiratory needs.
A 38-year-old woman has newly diagnosed multiple sclerosis (MS) and asks the nurse what is going to happen to her. What is the best response by the nurse?
Explanation
Multiple sclerosis has several patterns, but the most common is the relapsing-remitting form, characterized by episodes of new or worsening neurological symptoms followed by periods of partial or complete recovery. Some individuals may later develop a progressive form of the disease, where symptoms gradually worsen over time. Providing this information helps set realistic expectations while acknowledging variability in disease progression.
Rationale for correct answer:
1. “You will have either periods of attacks and remissions or progression of nerve damage over time.” This statement accurately reflects the typical course of MS, which may begin with relapsing-remitting episodes and, in some cases, transition into a secondary progressive form. It provides truthful, balanced information without being unnecessarily discouraging or overly optimistic.
Rationale for incorrect answers:
2. “You need to plan for a continuous loss of movement, sensory functions, and mental capabilities.” This overgeneralizes and implies a worst-case scenario. MS progression varies greatly among individuals, and not all experience severe continuous decline or significant cognitive impairment.
3. “You will most likely have a steady course of chronic progressive nerve damage that will change your personality.” This is inaccurate because only a minority of patients are diagnosed with primary progressive MS at onset. Personality change is not a hallmark symptom of MS.
4. “It is common for people with MS to have an acute attack of weakness and then not to have any other symptoms for years.” While some may experience long remission periods, it is not typical for symptoms to disappear for years without recurrence, especially without disease-modifying treatment.
Take home points
- MS most often follows a relapsing-remitting course at onset.
- Some individuals may later develop progressive disease with gradual worsening.
- Education should be accurate, realistic, and supportive to help clients prepare for variability in disease progression.
During assessment of a patient admitted to the hospital with an acute exacerbation of MS, what should the nurse expect to find?
Explanation
Multiple sclerosis exacerbations are caused by inflammation and demyelination in the central nervous system, which disrupt nerve signal transmission. The most common acute findings include muscle weakness or spasticity, optic neuritis or other vision problems, and altered sensations like numbness or tingling. These symptoms may appear suddenly or worsen over hours to days during a relapse.
Rationale for correct answer:
3. Motor impairment, visual disturbances, and paresthesias: Demyelination in motor pathways leads to weakness and coordination problems, while damage to the optic nerve or visual pathways causes blurred vision, double vision, or vision loss. Sensory pathway involvement produces tingling, numbness, or burning sensations, which are hallmark MS symptoms.
Rationale for incorrect answers:
1. Tremors, dysphasia, and ptosis: While tremors can occur in MS, dysphasia (language disorder) and ptosis (drooping eyelid) are not typical acute findings; ptosis is more associated with myasthenia gravis.
2. Bowel and bladder incontinence and loss of memory: Bowel/bladder issues can develop in MS but are usually chronic rather than acute. Significant memory loss is not a primary early symptom in an exacerbation.
4. Excessive involuntary movements, hearing loss, and ataxia: Involuntary choreiform movements are more characteristic of Huntington’s disease, and hearing loss is not common in MS. Ataxia can occur but is not typically accompanied by the other two symptoms in MS relapses.
Take home points
- MS exacerbations commonly present with new or worsening motor, sensory, and visual symptoms.
- Optic neuritis, muscle weakness, and paresthesias are hallmark acute findings.
- Symptom patterns reflect the location of CNS lesions and can vary greatly between relapses.
The nurse explains to a patient newly diagnosed with MS that the diagnosis is made primarily by:
Explanation
The diagnosis of multiple sclerosis is primarily based on the patient’s history and clinical manifestations, supported by diagnostic tests such as MRI and cerebrospinal fluid analysis. MS is identified by evidence of lesions in the central nervous system that occur in different locations and at different points in time, consistent with the pattern of demyelination. A thorough history and neurological examination are essential in recognizing these patterns.
Rationale for correct answer:
4. History and clinical manifestations: The hallmark of MS diagnosis is demonstrating dissemination of neurological lesions in both time and space, which is determined by a patient’s symptom history and physical findings. MRI and lab tests are used to support the diagnosis, but the pattern of clinical presentation remains the cornerstone.
Rationale for incorrect answers:
1. Spinal x-ray findings: X-rays do not detect demyelinating lesions and have no role in confirming MS. They are used primarily to evaluate bony structures, not central nervous system pathology.
2. T-cell analysis of the blood: While MS is immune-mediated and involves T-cell activity, blood tests for T-cells are not diagnostic. No single blood test can confirm MS.
3. Analysis of cerebrospinal fluid: CSF analysis may show oligoclonal bands or elevated IgG, which support the diagnosis, but these findings are not specific to MS and must be interpreted in the context of the patient’s history and clinical picture.
Take home points
- MS diagnosis relies on evidence of CNS lesions separated in time and space.
- History and neurological examination are essential, with MRI and CSF tests serving as supportive tools.
- No single lab or imaging test can independently confirm MS.
Mitoxantrone (Novantrone) is being considered as treatment for a patient with progressive-relapsing MS. The nurse explains that a disadvantage of this drug compared with other drugs used for MS is what?
Explanation
Mitoxantrone is a potent immunosuppressant used in certain aggressive forms of MS, including progressive-relapsing MS. Its major disadvantage is that it can cause irreversible cardiac damage, so there is a strict lifetime cumulative dose limit to minimize the risk of cardiotoxicity. Regular cardiac monitoring is required before each infusion.
Rationale for correct answer:
2. It has a lifetime dose limit because of cardiac toxicity: Mitoxantrone can lead to cardiomyopathy and heart failure, especially when the total cumulative dose exceeds recommended limits. This risk makes it unsuitable for long-term continuous use and requires careful tracking of total doses administered.
Rationale for incorrect answers:
1. It must be given subcutaneously every day: This is incorrect because mitoxantrone is given intravenously, typically once every 3 months, not daily.
3. It is an anticholinergic agent that causes urinary incontinence: Mitoxantrone is not an anticholinergic drug; urinary issues in MS are related to the disease process, not this medication’s mechanism.
4. It is an immunosuppressant agent that increases the risk for infection: While it is true that mitoxantrone increases infection risk, this is a general effect of many MS drugs. The unique disadvantage that sets it apart is the lifetime dose limit due to cardiac toxicity.
Take home points
- Mitoxantrone is reserved for aggressive MS forms due to its potency and risks.
- Cardiotoxicity limits the total lifetime dose and requires ongoing cardiac monitoring.
- Administration is IV every 3 months, not daily, making dosing convenient but long-term use restricted.
A patient with MS has a nursing diagnosis of self-care deficit related to muscle spasticity and neuromuscular deficits. In providing care for the patient, what is most important for the nurse to do?
Explanation
Promoting the use of assistive devices enables the patient to perform self-care activities independently despite muscle spasticity and neuromuscular deficits. This fosters autonomy, enhances self-esteem, and maintains functional ability for as long as possible. In chronic illnesses like MS, independence in daily living is a key rehabilitation goal.
Rationale for correct answer:
3. Promote the use of assistive devices so the patient can participate in self-care activities: Using tools such as grab bars, dressing sticks, or modified utensils helps the patient adapt to physical limitations and maintain independence. This approach maximizes function and supports psychological well-being by preventing learned helplessness.
Rationale for incorrect answers:
1. Teach the family members how to care adequately for the patient’s needs: While caregiver education is important, it should not replace promoting the patient’s own ability to perform tasks whenever possible.
2. Encourage the patient to maintain social interactions to prevent social isolation: Social interaction is beneficial, but it does not directly address the self-care deficit caused by muscle spasticity.
4. Perform all activities of daily living (ADLs) for the patient to conserve the patient’s energy: This may be appropriate during acute exacerbations, but routinely doing everything for the patient can accelerate functional decline and reduce independence.
Take home points
- Independence in ADLs is a central goal in MS care.
- Assistive devices bridge the gap between physical limitations and functional needs.
- Over-assistance can hinder skill retention and autonomy.
A patient with newly diagnosed MS has been hospitalized for evaluation and initial treatment of the disease. Following discharge teaching, the nurse realizes that additional instruction is needed when the patient says what?
Explanation
Stopping prednisone suddenly is unsafe and can cause adrenal insufficiency and rebound symptoms. In MS management, corticosteroids like prednisone are often prescribed for acute exacerbations, and discontinuing them abruptly without medical guidance can worsen inflammation, trigger relapse, and cause systemic complications. The patient must be educated to follow the prescriber’s tapering schedule.
Rationale for correct answer:
2. “When I begin to feel better, I should stop taking the prednisone to prevent side effects.” Corticosteroids must be tapered under provider supervision to allow the adrenal glands to resume normal cortisol production and to avoid sudden MS symptom flare-ups. Stopping abruptly can lead to severe fatigue, hypotension, and potentially life-threatening adrenal crisis.
Rationale for incorrect answers:
1. Avoiding contact with people who have respiratory infections is appropriate because infections can trigger MS relapses and worsen neurological function.
3. A high-protein diet and vitamin supplementation can support immune health, muscle strength, and overall energy in patients with MS.
4. Planning with family for possible disease progression is proactive and helps ensure coordinated care and emotional support.
Take home points
- Never stop corticosteroids abruptly; tapering is essential to prevent adrenal insufficiency.
- Infection prevention is critical for minimizing MS flare-ups.
- Nutrition and supplementation can help maintain physical strength and energy.
- Early care planning supports both patient independence and family preparedness.
When providing care for a patient with ALS, the nurse recognizes what as one of the most distressing problems experienced by the patient?
Explanation
In amyotrophic lateral sclerosis (ALS), motor neurons progressively degenerate, leading to muscle weakness, paralysis, and loss of voluntary movement. However, cognitive function is typically preserved, leaving patients fully aware of their progressive physical decline. This combination of complete physical dependence with intact mental awareness is often one of the most psychologically and emotionally distressing aspects of the disease.
Rationale for correct answer:
2. Retention of cognitive function with total degeneration of motor function: ALS spares most cognitive abilities, meaning patients remain mentally alert while losing the ability to move, speak, swallow, and eventually breathe independently. This awareness can lead to profound frustration, depression, and emotional distress.
Rationale for incorrect answers:
1. Painful spasticity of the face and extremities: While spasticity and muscle cramps can occur, they are not usually the most distressing symptom compared to the psychological impact of losing all motor function while staying cognitively intact.
3. Uncontrollable writhing and twisting movements: This describes chorea, which is seen in Huntington’s disease, not ALS.
4. Knowledge that there is a 50% chance the disease has been passed to offspring: This is true for Huntington’s disease, which is autosomal dominant, but most ALS cases are sporadic and not inherited; only about 5–10% are familial.
Take home points
- ALS causes progressive motor neuron loss with preserved cognitive function in most patients.
- The emotional burden stems from full awareness of one’s physical decline.
- Supportive care must address psychological as well as physical needs.
- Clear patient and family communication is essential for advance care planning.
In providing care for patients with chronic, progressive neurologic disease, what is the major goal of treatment that the nurse works toward?
Explanation
For chronic, progressive neurologic diseases such as multiple sclerosis, Parkinson’s disease, or ALS, complete restoration of neurologic function is generally not possible. The primary treatment goal is to preserve the patient’s independence and quality of life by maintaining optimal neurologic function for as long as possible through symptom management, rehabilitation, and supportive interventions.
Rationale for correct answer:
3. Maximize neurologic functioning for as long as possible: This goal focuses on slowing functional decline, improving mobility, enhancing self-care ability, and supporting emotional well-being, thereby prolonging independence and quality of life.
Rationale for incorrect answers:
1. Meet the patient’s personal care needs: While important, this is a short-term objective. The broader aim is to maintain the patient’s ability to meet their own needs for as long as possible.
2. Return the patient to normal neurologic function: This is not realistic in chronic, progressive neurologic diseases because nerve damage is often irreversible.
4. Prevent the development of additional chronic diseases: Although managing comorbidities is important, it is not the central goal in managing the neurologic condition itself.
Take home points
- In chronic, progressive neurologic disease, cure is typically not possible.
- The main focus is on slowing progression and preserving function.
- Multidisciplinary care, rehabilitation, and patient education are key to maintaining independence.
- Emotional and psychosocial support are essential alongside physical management.
A patient with myasthenia gravis is admitted to the hospital with respiratory insufficiency and severe weakness. When is a diagnosis of cholinergic crisis made?
Explanation
Cholinergic crisis in myasthenia gravis occurs due to excessive anticholinesterase medication, leading to overstimulation of acetylcholine receptors. This paradoxically worsens muscle weakness, including respiratory muscles. The Tensilon (edrophonium) test helps distinguish cholinergic crisis from myasthenic crisis: in cholinergic crisis, giving edrophonium makes symptoms worse because it further increases acetylcholine levels.
Rationale for correct answer:
2. Administration of edrophonium (Tensilon) increases muscle weakness: This confirms cholinergic crisis, as excessive acetylcholine overstimulates receptors, leading to depolarization block and worsening weakness.
Rationale for incorrect answers:
1. The patient’s respiration is impaired because of muscle weakness: This occurs in both myasthenic and cholinergic crises, so it is not diagnostic by itself.
3. Administration of edrophonium (Tensilon) results in improved muscle contractility: This finding indicates myasthenic crisis, not cholinergic crisis.
4. EMG reveals a decreased response to repeated stimulation of muscles: This is a general diagnostic finding in myasthenia gravis but does not differentiate between crisis types.
Take home points
- Cholinergic crisis is due to overmedication with anticholinesterase drugs.
- Tensilon test worsens weakness in cholinergic crisis, improves it in myasthenic crisis.
- Respiratory failure can occur in both crises, so careful assessment is essential.
- Management involves withholding anticholinesterase drugs and providing respiratory support.
During care of a patient in myasthenic crisis, maintenance of what is the nurse’s first priority for the patient?
Explanation
Respiratory function is the nurse’s first priority during a myasthenic crisis. The severe muscle weakness associated with the crisis can impair respiratory muscles, leading to inadequate ventilation and potentially life-threatening respiratory failure. Early recognition and intervention such as airway management, supplemental oxygen, and possibly mechanical ventilation are critical to patient survival.
Rationale for correct answer:
3. Respiratory function: In a myasthenic crisis, weakness of the diaphragm and intercostal muscles compromises breathing. Maintaining airway patency and adequate oxygenation is the most urgent nursing priority, consistent with the ABCs (Airway, Breathing, Circulation).
Rationale for incorrect answers:
1. Mobility: Important for long-term management but not the immediate life-saving priority in an acute crisis.
2. Nutrition: Dysphagia may occur, but feeding is secondary to stabilizing breathing.
4. Verbal communication: While communication is important for patient comfort, it is not as urgent as maintaining life-sustaining respiratory function.
Take home points:
- Myasthenic crisis is a medical emergency that can cause acute respiratory failure.
- ABCs guide nursing priorities—airway and breathing come first.
- Rapid assessment and intervention prevent hypoxia and death.
- Respiratory support may require intubation and mechanical ventilation until muscle strength improves.
Exams on Multiple Sclerosis, ALS, and Myasthenia Gravis
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Define Multiple Sclerosis (MS), Amyotrophic Lateral Sclerosis (ALS), and Myasthenia Gravis (MG), including their respective etiologies and pathophysiologies.
- Identify the key clinical manifestations and diagnostic findings for MS, ALS, and MG.
- Differentiate between the three disorders based on their unique pathological processes, affected body systems, and common symptoms.
- Describe the primary nursing interventions and management strategies for clients with MS, ALS, and MG, including pharmacological and non-pharmacological approaches.
- Explain the critical differences between a myasthenic crisis, a cholinergic crisis, and a mixed crisis in Myasthenia Gravis, and outline the appropriate nursing responses for each.
- Prioritize nursing interventions based on a client's specific needs and stage of disease progression for each of the three conditions.
- Recognize common risk factors and triggers that can exacerbate symptoms in clients with MS and MG.
Multiple Sclerosis
MS is a chronic, progressive, degenerative disorder of the central nervous system (CNS) characterized by disseminated demyelination of nerve fibers of the brain and spinal cord. The disease process involves an autoimmune attack on the myelin sheath, which is the fatty protective covering around nerve fibers. The resulting damage to the myelin sheath impairs nerve impulse transmission, leading to a variety of neurological symptoms.
Etiology and Pathophysiology
The exact cause of MS is unknown, but it is believed to be an autoimmune disease triggered by environmental factors in genetically susceptible individuals. The disease process involves:
- Initial attack: An inflammatory response damages the myelin sheath, leading to demyelination.
- Plaque formation: Scar tissue (sclerosis) forms in the damaged areas, creating plaques. These plaques can be found throughout the CNS.
- Nerve damage: The underlying nerve axons are eventually damaged, leading to permanent neurological deficits.
Clinical Manifestations
Symptoms of MS are highly variable and depend on the location and extent of the demyelination. Common symptoms include:
- Motor symptoms: Weakness or paralysis of the limbs, trunk, or head; diplopia (double vision); spasticity of muscles.
- Sensory symptoms: Numbness, tingling, or "pins and needles" sensations; pain; paresthesias.
- Cerebellar symptoms: Ataxia (lack of coordination); dysarthria (slurred speech); intention tremor (tremor that worsens with purposeful movement).
- Emotional symptoms: Mood swings, depression, or euphoria.
- Other symptoms: Fatigue, bowel and bladder dysfunction (urinary frequency, urgency, incontinence), sexual dysfunction, cognitive changes (memory loss, difficulty with concentration).
Diagnostic Studies
Diagnosis of MS can be challenging, as there is no single definitive test. The diagnosis is based on a combination of clinical manifestations, medical history, and diagnostic tests, which may include:
- Magnetic Resonance Imaging (MRI): The gold standard for diagnosis. MRI scans can detect the presence of plaques in the brain and spinal cord.
- Cerebrospinal Fluid (CSF) analysis: Examination of CSF obtained via lumbar puncture may reveal an increase in T cells and IgG antibodies.
- Evoked Potential Studies: These tests measure the speed of nerve impulses in response to visual, auditory, or somatosensory stimuli.
Management
There is no cure for MS, but treatment is aimed at managing symptoms, reducing the frequency and severity of relapses, and slowing disease progression.
- Immunomodulatory therapy: Medications such as interferon beta and glatiramer acetate are used to modify the disease course and reduce the frequency of relapses.
- Symptom management: Medications can be used to treat specific symptoms, such as muscle relaxants for spasticity, anticholinergics for bladder dysfunction, and antidepressants for depression.
- Physical and occupational therapy: These therapies can help patients maintain mobility, strength, and independence.
Nursing Insight
Holistic and individualized care is crucial for clients with MS, as symptoms are highly variable and can fluctuate over time. A primary nursing focus is on energy conservation, teaching clients to manage fatigue by planning activities and incorporating rest periods, as this is one of the most disabling symptoms. Nurses also play a vital role in patient education, empowering clients to adhere to their medication regimens and avoid exacerbating triggers like extreme temperatures and infections. Safety is paramount, requiring ongoing assessment of mobility and fall risk, while psychosocial support is essential to address the emotional challenges and unpredictability of the disease, helping clients manage anxiety, depression, and social isolation.
Amyotrophic Lateral Sclerosis
ALS, also known as Lou Gehrig's disease, is a rare, progressive neurological disorder that affects nerve cells (neurons) in the brain and spinal cord that control voluntary muscle movement. The disease leads to muscle weakness, atrophy, and eventually paralysis.
 Etiology and Pathophysiology
Etiology and Pathophysiology
The exact cause of ALS is unknown, but it is believed to be a combination of genetic and environmental factors. The disease process involves the degeneration of both upper and lower motor neurons.
- Upper motor neurons: Located in the brain, these neurons send signals to the lower motor neurons. Degeneration of upper motor neurons leads to spasticity and hyperreflexia.
- Lower motor neurons: Located in the spinal cord and brainstem, these neurons send signals to the muscles. Degeneration of lower motor neurons leads to muscle weakness, atrophy, and fasciculations (muscle twitching).
Clinical Manifestations
Symptoms of ALS typically begin in the hands, feet, or limbs and progress to other parts of the body. Common symptoms include:
- Early symptoms: Muscle weakness or stiffness, especially in the hands and feet; muscle cramps and fasciculations.
- Progressive symptoms: Difficulty walking, speaking (dysarthria), swallowing (dysphagia), and breathing.
- Cognitive changes: In some cases, patients may experience mild cognitive impairment or frontotemporal dementia.
Diagnostic Studies
There is no single test to diagnose ALS. Diagnosis is based on a thorough neurological examination, a review of the patient's medical history, and a combination of tests to rule out other conditions.
- Electromyography (EMG) and Nerve Conduction Study (NCS): These tests can measure the electrical activity of muscles and nerves and help to confirm the presence of motor neuron damage.
- MRI: An MRI scan can be used to rule out other conditions that may mimic ALS, such as a spinal cord tumor or a herniated disc.
Management
There is no cure for ALS, and treatment is focused on managing symptoms, providing supportive care, and improving the patient's quality of life.
- Medications: Riluzole is the only FDA-approved drug for ALS, and it has been shown to slow the progression of the disease. Other medications may be used to treat specific symptoms, such as muscle cramps, spasticity, and excessive salivation.
- Supportive care: Physical, occupational, and speech therapy can help patients maintain function and independence. Respiratory support, such as non-invasive ventilation, may be needed as the disease progresses.
Nursing Insight
For clients with ALS, the priority nursing insight is the critical need for respiratory management, as progressive respiratory muscle weakness is the leading cause of death. Nurses must continuously monitor respiratory status and be prepared for interventions ranging from non-invasive ventilation to mechanical ventilation, while also facilitating early discussions about end-of-life care. Another key focus is communication, as clients will inevitably lose their ability to speak; nurses should work with a speech-language pathologist to introduce alternative communication methods early on to preserve the client's autonomy and dignity. Addressing dysphagia is also crucial to ensure nutritional and hydration needs are met safely, which requires collaborative care with dietitians and speech therapists to prevent aspiration and plan for long-term feeding solutions.
Myasthenia Gravis
Myasthenia Gravis is a chronic, autoimmune neuromuscular disease characterized by fluctuating weakness of voluntary muscles. It is caused by a defect in the transmission of nerve impulses to muscles at the neuromuscular junction.
Etiology and Pathophysiology
MG is an autoimmune disease in which the body produces antibodies that block or destroy the acetylcholine (ACh) receptors at the neuromuscular junction. Acetylcholine is a neurotransmitter that is essential for muscle contraction.
- Normal function: When a nerve impulse arrives at the neuromuscular junction, ACh is released and binds to receptors on the muscle fiber, causing the muscle to contract.
- MG function: In MG, the antibodies block the ACh receptors, preventing ACh from binding and causing a weakened or absent muscle contraction.
Clinical Manifestations
The hallmark of MG is fluctuating muscle weakness that worsens with activity and improves with rest. The muscles most commonly affected are those of the eyes, face, and throat.
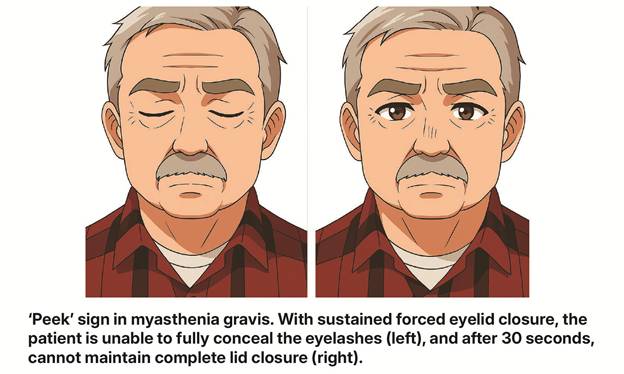
- Ocular symptoms: Ptosis (drooping of the eyelids) and diplopia (double vision) are often the first signs of the disease.
- Facial and bulbar symptoms: Mask-like facial expression, difficulty chewing and swallowing (dysphagia), and slurred speech (dysarthria).
- Generalized symptoms: Weakness of the limbs, trunk, and respiratory muscles. This can lead to a myasthenic crisis, a medical emergency characterized by respiratory failure.
Diagnostic Studies
Diagnosis of MG is based on a combination of clinical manifestations, medical history, and diagnostic tests.
- Tensilon Test: A small dose of edrophonium (Tensilon), an acetylcholinesterase inhibitor, is injected intravenously. A rapid improvement in muscle strength (e.g., improved ptosis) is a positive sign for MG.
- Acetylcholine Receptor (AChR) Antibody Test: This blood test detects the presence of antibodies that block the ACh receptors.
- Electromyography (EMG): An EMG can be used to detect the characteristic "decremental response" of muscle fibers to repeated nerve stimulation.
Management
There is no cure for MG, but treatment is aimed at improving muscle strength, controlling symptoms, and preventing complications.
- Anticholinesterase drugs: Medications such as pyridostigmine (Mestinon) are the first-line treatment for MG. They work by inhibiting the enzyme that breaks down ACh, thereby increasing the amount of ACh available at the neuromuscular junction.
- Corticosteroids and immunosuppressants: These medications may be used to suppress the immune system and reduce the production of antibodies.
- Thymectomy: Surgical removal of the thymus gland may be performed, as the thymus is believed to play a role in the autoimmune response.
- Plasmapheresis and IVIG: These treatments may be used in severe cases or during a myasthenic crisis to remove antibodies from the blood.
Myasthenic Vs Cholinergic Crises
|
Type of Crisis |
Underlying Cause |
Key Clinical Manifestations |
Diagnostic Test and Nursing Actions |
|
Myasthenic Crisis |
Undermedication or a precipitating factor (e.g., infection, surgery, or emotional stress) leading to severe muscle weakness. |
Respiratory muscle weakness: Severe dyspnea, leading to respiratory failure and the need for mechanical ventilation. |
Tensilon Test: Symptoms temporarily improve with the administration of edrophonium (Tensilon). |
|
|
|
General myasthenic findings: Exacerbation of weakness, fatigue, ptosis, and dysphagia. |
Nursing Actions: Administer prescribed anticholinesterase medications (e.g., pyridostigmine). Prepare for and manage mechanical ventilation. Provide respiratory support. |
|
|
|
Other signs: Hypertension, urinary and fecal incontinence. |
|
|
Cholinergic Crisis |
Overmedication with anticholinesterase drugs, leading to an excess of acetylcholine (ACh) at the neuromuscular junction. |
Muscle twitching and weakness: Muscle fasciculations progressing to profound weakness, including respiratory muscles, requiring mechanical ventilation. |
Tensilon Test: Symptoms worsen or show no improvement with the administration of edrophonium (Tensilon). |
|
|
|
Cholinergic manifestations: Hypersecretions (nausea, vomiting, diarrhea, increased respiratory secretions), abdominal cramps (hypermotility). |
Nursing Actions: Immediately withhold all anticholinesterase medications. Administer atropine as prescribed to counteract the effects of excess ACh. Prepare for and manage mechanical ventilation. |
|
|
|
Other signs: Hypotension, constricted pupils (miosis). |
|
|
Mixed Crisis |
Overtreatment of a myasthenic crisis with anticholinesterase drugs, leading to a combination of myasthenic and cholinergic symptoms. |
Combined symptoms: Dyspnea, dysphagia, and dysarthria. |
The client may present with an ambiguous clinical picture, making diagnosis challenging. |
|
|
|
Additional signs: Restlessness, apprehension, increased salivation, and lacrimation. |
Nursing Actions: Requires careful clinical assessment to differentiate from a pure myasthenic or cholinergic crisis. Treatment will involve a balance of managing both types of symptoms, often starting with withholding anticholinesterase medications and providing respiratory support. |
Differentiation of the Three Disorders
|
Feature |
Multiple Sclerosis (MS) |
Amyotrophic Lateral Sclerosis (ALS) |
Myasthenia Gravis (MG) |
|
Pathophysiology |
Autoimmune demyelination of CNS |
Degeneration of motor neurons |
Autoimmune destruction of ACh receptors |
|
Affected System |
Central Nervous System (CNS) |
Central and Peripheral Nervous System |
Neuromuscular Junction |
|
Muscle Weakness |
Spasticity, weakness, and loss of coordination |
Progressive muscle weakness and atrophy |
Fluctuating weakness that worsens with activity |
|
Cognition |
Cognitive changes are common |
Cognitive changes may occur |
Cognition is generally unaffected |
|
Prognosis |
Variable; often with periods of remission and relapse |
Progressive and fatal, typically within 2-5 years |
Chronic but manageable; normal life expectancy with treatment |
Nursing Insight
A central nursing insight for Myasthenia Gravis is the absolute importance of medication adherence, as the precise timing of anticholinesterase drugs is critical for symptom management and preventing a crisis. Nurses must be vigilant in educating clients on taking medication at the right time, typically 30-60 minutes before meals, to improve swallowing and function. Furthermore, nurses must understand the distinct differences between a myasthenic crisis (undermedication) and a cholinergic crisis (overmedication), using diagnostic tools like the Tensilon test to guide emergency interventions. Encouraging rest periods and helping clients identify and avoid common triggers—such as stress, infection, and certain medications—are also fundamental to managing fluctuating muscle weakness and preserving the client's overall quality of life.
Summary
- Multiple Sclerosis (MS): An autoimmune disorder causing demyelination of the central nervous system. Key features include highly variable symptoms like fatigue, muscle spasticity, and visual disturbances, with a disease course that can involve attacks and remissions.
- MS Management: Treatment focuses on modifying the disease course with immunomodulatory therapy and managing specific symptoms. Nursing care prioritizes energy conservation, fall prevention, patient education on triggers, and psychosocial support.
- Amyotrophic Lateral Sclerosis (ALS): A progressive and fatal neurodegenerative disease that destroys both upper and lower motor neurons, leading to muscle weakness, atrophy, and eventual paralysis. Cognitive function is typically retained.
- ALS Management: Care is palliative and supportive, as there is no cure. The primary nursing focus is on respiratory management, as respiratory failure is the leading cause of death. Other priorities include ensuring nutritional intake, facilitating communication, and providing sensitive end-of-life care.
- Myasthenia Gravis (MG): A chronic autoimmune disease affecting the neuromuscular junction. It is characterized by fluctuating muscle weakness that worsens with activity and improves with rest, commonly affecting muscles of the eyes, face, and throat.
- MG Management: Treatment involves anticholinesterase drugs to improve muscle strength, as well as immunosuppressants. Nursing care emphasizes strict medication adherence, promoting rest, and educating clients on avoiding triggers that can exacerbate symptoms.
- Crises in MG: It is crucial to differentiate between a myasthenic crisis and a cholinergic crisis. The Tensilon test is a key diagnostic tool to distinguish between them.
- For all three conditions, the major goal of nursing care is to maximize neurologic functioning for as long as possible, manage debilitating symptoms, enhance safety, and maintain the client's quality of life and dignity.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Multiple Sclerosis, ALS, and Myasthenia Gravis
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


