Please set your exam date
Delirium
Study Questions
Practice Exercise 1
A client is experiencing acute confusion due to poisoning from an accidental exposure to toxic chemicals in the workplace. What type of behavior should the nurse expect this client to demonstrate upon admission to the nursing unit?
Explanation
Acute confusioncaused by toxic chemical exposure is a form of delirium, characterized by sudden onset of impaired attention, orientation, and communication. Neurotoxicity disrupts neurotransmitter balance and cerebral function, leading to difficulty organizing thoughts, expressing needs, and maintaining coherent speech.
Rationale for correct answer:
3.Toxic poisoning alters cognitive processingand language function, resulting in difficulty expressing ideas and needs. This is consistent with acute delirium, where impaired attention and disorganized thinking are hallmark features. The nurse should expect communication deficits upon admission.
Rationale for incorrect answers:
1.Nausea may occur with chemical exposure but is a gastrointestinal symptom, not the defining feature of acute confusion. The stem emphasizes cognitive impairment, making this option less appropriate.
2.Ambivalent feelings reflect emotional conflict but are not typical of acute delirium. The primary issue is disorganized thoughtand impaired communication, not frequent verbalization of mixed emotions.
4.Despondency in the presence of family suggests depressionor withdrawal. Acute confusion from poisoning presents with fluctuating cognition and communication deficits, not sustained despondency.
Test-taking strategy
- Identify the condition: acute confusion from toxic exposure = delirium.
- Apply Maslow: prioritize neurological and communication deficits over GI or emotional symptoms.
- Eliminate options that describe depression or emotional states.
- Select the option that reflects impaired communication and thought organization.
Take Home Points
- Acute confusion from toxic poisoning is a form of delirium with sudden cognitive impairment.
- Difficulty expressing ideas and needs is a hallmark of delirium due to disorganized thinking.
- Nausea or emotional symptoms may occur but are not primary indicators of acute confusion.
- Differentiating delirium from depression or anxiety ensures accurate nursing assessment and intervention.
A nursing student is studying delirium. Which of the following student statements indicates that learning has occurred? Select all that apply.
Explanation
Deliriumis an acute neurocognitive disturbancemarked by altered consciousness, attention deficits, and rapid onset. It typically results from an underlying medical condition or insultand is usually reversiblewith treatment and resolution of the cause. The condition fluctuates over hours to days and is not a primary degenerative cognitive disorder.
Rationale for correct answers:
1.Delirium symptoms develop rapidlyover a short period (hours to days), contrasting with chronic cognitive disorders. This rapid onset is a hallmark distinguishing delirium from dementia and other slow-progressing cognitive impairments.
4.Delirium fundamentally involves a disturbance of consciousness, with reduced clarity of awareness and impaired focus, shifting attention and responsiveness. This altered state is central to its diagnostic criteria and differentiates it from other neurocognitive conditions.
5.Delirium is secondary to another condition, such as infection, metabolic imbalance, or substance withdrawal. It rarely presents as a primary disorder; instead, it reflects an acute physiological or toxic trigger affecting brain function.
Rationale for incorrect answers:
2.Delirium does not permanently impair new learningin the way chronic dementias do; it is typically reversibleonce the underlying cause is treated, and cognitive function often returns toward baseline.
3.Aphasia, apraxia, and agnosia are more characteristic of dementia and focal neurological deficits, not core features of delirium, which primarily involves fluctuating attention and consciousness rather than specific language or motor planning losses.
Test-taking strategy
- Step 1: Identify acute vs chroniconset — select options indicating rapid development.
- Step 2: Look for core diagnostic features — disturbed consciousness and attention.
- Step 3: Exclude statements implying permanent cognitive lossor features of other disorders.
- Step 4: Choose options reflecting delirium’s secondary natureand clinical presentation.
Take Home Points
- Delirium presents with acute onsetand fluctuating attention.
- It involves a disturbance of consciousness, not just memory.
- Delirium is generally secondary to underlying physical causes.
- Aphasia, apraxia, and agnosia are not primary featuresof delirium.
A nurse is caring for an 80-year-old postoperative patient who suddenly becomes confused, disoriented to time and place, and shows fluctuating attention. Which features indicate that the patient is experiencing delirium rather than chronic cognitive impairment? Select all that apply.
Explanation
Deliriumis a transient neuropsychiatric syndromecharacterized by an acute, fluctuating impairment in attention and cognitive function. It is considered a medical emergencythat often signals an underlying systemic illness, such as sepsis or metabolic imbalance, requiring frequent surveillanceto distinguish it from static conditions like dementia.
Rationale for correct answer:
1.Because the hallmark of delirium is a waxing and waningcourse, the nurse must perform continuous, serial assessments of the patient's mental status. Subtle changes in the ability to sustain attentionor follow simple commands are often the earliest clinical indicators of an acute physiological decline, even before overt agitation or vital sign changes occur.
Rationale for incorrect answers:
2.The immediate administration of antipsychotic medicationsbefore a thorough diagnostic assessment is contraindicated as these drugs can mask clinical symptomsand hinder the identification of the underlying cause. Pharmacological interventions are reserved for patients in severe distress or those posing an immediate safety riskafter non-pharmacological strategies have failed.
3.Relying exclusively on neuroimaging resultsis inappropriate because delirium is a functional, rather than a primarily structural, brain disturbance. While CT or MRI scans may be used to rule out a stroke or intracranial hemorrhage, the diagnosis of delirium is fundamentally a clinical onebased on history, bedside assessment, and the identification of precipitating medical factors.
4.Delaying clinical documentationuntil a formal diagnosis is confirmed is a violation of nursing standards and jeopardizes patient safety. Accurate, real-time charting of behavioral fluctuationsand cognitive deficits is essential for the interdisciplinary team to recognize the fluctuating patternthat is diagnostic of delirium and to track the effectiveness of interventions.
Test-taking strategy
- Identify the "hallmark" characteristic of the condition (fluctuation) and match it to the nursing action (continuous monitoring).
- Eliminate "all-or-nothing" words like "solely" or "immediately" which often indicate incorrect, narrow nursing actions.
- Prioritize assessment (nursing process) over immediate pharmacological intervention in a diagnostic scenario.
Take Home Points
- The Confusion Assessment Method (CAM) is the gold standard bedside tool used by nurses to detect delirium by focusing on acute onset and inattention.
- Hypoactive delirium is the most frequently missed subtype because patients appear lethargic or depressed rather than agitated.
- Nurses are in a strategic position to prevent delirium by implementing non-pharmacological protocols like early mobilization and sleep hygiene.
- A collateral history from family members is vital during evaluation to establish the patient's baseline cognitive and functional status.
A client in the ICU exhibits visual hallucinations, restlessness, and sleep-wake reversal. Which nursing interventions are appropriate to manage the client’s delirium? Select all that apply.
Explanation
Deliriumis a transient, acute neuropsychiatric syndrome characterized by fluctuating levelsof consciousness, reduced environmental awareness, and cognitive deficits. It results from underlying physiological stressors, such as infection, organ failure, or medication toxicity, which disrupt global cerebral neurotransmission. In the intensive care unit, this condition is often exacerbated by sensory overloador deprivation, leading to sleep-wake reversal and distressing visual hallucinations.
Rationale for correct answers:
1.Providing frequent reorientationis essential because delirium disrupts the client’s ability to process and retain information. Repetitive verbal cues regarding the current date, location, and identity help stabilize the client’s cognitive framework and reduce the anxiety associated with acute confusion.
2.Maintaining a well-lit environmentduring the day and a quiet atmosphere at night promotes circadian rhythm alignment. Reducing excessive noiseand providing familiar items helps minimize sensory perceptual distortions and prevents the worsening of restlessness and agitation.
4.Ensuring client safetyis a priority since restless and hallucinating clients are at high risk for falls or self-injury. Removing hazardous objectsand providing continuous supervision prevents accidental trauma or the dislodgement of critical medical equipment like intravenous lines.
5.Encouraging the use of sensory aidsreduces misinterpretation of environmental stimuli, which often triggers hallucinations. Correcting sensory deficitswith glasses and hearing aids allows the client to perceive their surroundings accurately, thereby decreasing cognitive load and paranoia.
Rationale for incorrect answer:
3.Routine administration of high-dose sedativesis contraindicated as it can worsen the underlying encephalopathy and prolong the duration of delirium. Benzodiazepines, in particular, often trigger paradoxical agitationand increase the risk of respiratory depression and further cognitive clouding in critically ill patients.
Test-taking strategy:
- Identify the clinical problem: The client has hyperactive delirium with sensory-perceptual alterations.
- Prioritize non-pharmacological interventions: Choices 1, 2, and 5 focus on environmental and cognitive stabilization.
- Apply safety principles: Choice 4 addresses the immediate physical risk associated with hallucinations and restlessness.
- Eliminate harmful actions: Choice 3 is incorrect because heavy sedation often masks the cause and exacerbates cognitive decline.
Take Home Points
- Delirium is an acute, fluctuating change in mental status that requires the identification and treatment of the underlying physiological cause.
- Non-pharmacological management, including the ABCDEF bundle, is the gold standard for reducing the duration and severity of ICU-related cognitive impairment.
- Safety interventions should focus on environmental modification and the use of sensory aids rather than physical or chemical restraints.
- Clinical differentiation from dementia is based on the acute onset and fluctuating course of delirium, whereas dementia involves a progressive, irreversible decline.
Practice Excercise 2
A client diagnosed with delirium is restrained in order to prevent the removal of a Foley catheter and an intravenous fluid line. Which response should the nurse expect after the client is restrained?
Explanation
Deliriumis an acute disturbance in attention, awareness, and cognitionoften triggered by medical illness, surgery, or medications. Clients with delirium are highly sensitive to environmental changes and restrictions. Physical restraints typically worsen agitation, increase confusion, and heighten risk of injury rather than calming the client.
Rationale for correct answer:
2.Restraints increase agitationbecause the client perceives them as threatening. In delirium, impaired judgmentand orientationmake restraints confusing and frightening, leading to restlessness, combativeness, and potential injury. This response is expected after restraint use.
Rationale for incorrect answers:
1.Restraints do not promote rest. Instead, they disrupt sleep-wake cyclesand increase agitation. Clients with delirium often experience worsened confusion at night, known as sundowning, which restraints exacerbate.
3.Pain medication needs are not reduced by restraints. In fact, restraints may cause discomfort, skin breakdown, or musculoskeletal pain, potentially increasing the need for analgesics rather than decreasing it.
4.Blood pressure changes are not a direct or consistent effect of restraints. While agitation may elevate blood pressure, restraints do not physiologically lower it. The primary effect is behavioral agitation, not hemodynamic stabilization.
Test-taking strategy
- Identify the condition: delirium involves acute confusion and agitation.
- Apply Maslow: prioritize safety and psychological comfort.
- Recognize that restraints worsen agitation rather than calm clients.
- Eliminate options suggesting rest, reduced pain, or blood pressure changes.
Take Home Points
- Delirium is an acute, reversible disturbance in cognition and attention.
- Restraints worsen agitation and confusion rather than calming the client.
- Alternative safety measures include close observation, environmental modification, and family presence.
- Nurses should avoid restraints whenever possible and prioritize non-restrictive interventions.
An elderly male client develops symptoms of delirium after a surgical procedure. To effectively minimize the client’s agitation, which action should the nurse take?
Explanation
Deliriumis an acute disturbance in attention, awareness, and cognitionoften triggered by medical illness, surgery, or medications. It is characterized by fluctuating consciousness, disorganized thinking, and agitation. Continuous staff-client contact provides reassurance, reduces confusion, and minimizes unsafe behaviors.
Rationale for correct answer:
2.Maintaining continuous staff-client contactensures close observation, immediate intervention for unsafe behaviors, and therapeutic reassurance. Familiar presence reduces agitation, stabilizes orientation, and promotes safety, which is the priority in postoperative delirium.
Rationale for incorrect answers:
1.Discussing behavior change with the client is ineffective because delirium impairs insightand judgment. The client cannot process abstract explanations, and this may increase frustration rather than reduce agitation.
3.Introducing sensory stimulation can worsen confusionand agitation. Clients with delirium benefit from calm, low-stimulation environments rather than additional stimuli that overwhelm impaired cognition.
4.Limiting unnecessary interactions may reduce overstimulation but does not provide the supervisionand reassurance needed. Isolation can increase fearand worsen agitation, making this option less effective.
Test-taking strategy
- Identify the condition: delirium after surgery = acute confusion with agitation.
- Apply Maslow: prioritize safetyand stabilization.
- Eliminate options that increase confusion or fail to provide supervision.
- Select the option that ensures continuous observation and reassurance.
Take Home Points
- Delirium is an acute, reversible disturbance in cognition often triggered by surgery or illness.
- Continuous staff presence reduces agitation and ensures safety.
- Excessive stimulation worsens confusion; calm reassurance is therapeutic.
Explaining behavior changes or isolating the client is ineffective in managing delirium.
A nurse is assessing a 78-year-old postoperative client who is exhibiting signs of delirium. The nurse observes that the client is convinced that it is 1954 and is complaining about “the bugs in this hotel.” The nurse’s priority intervention should be to:
Explanation
Deliriumis an acute disturbance in attention, orientation, and perceptionoften triggered by medical illness, surgery, or medications. Clients may experience hallucinations, disorientation, and agitation, which place them at high risk for injury. The priority nursing intervention is to ensure close observation and immediate access to staff for safety.
Rationale for correct answer:
2.Transferring the client to a room near the nursing stationensures continuous monitoring, rapid intervention if agitation escalates, and immediate response to unsafe behaviors. This placement reduces risk of falls, wandering, and injury, making it the priority intervention for postoperative delirium.
Rationale for incorrect answers:
1.Obtaining a PRN order for haloperidolmay be appropriate for severe agitation, but medication is not the first-line intervention. Safety and monitoring must be established before pharmacologic measures are considered.
3.Calling family to stay with the client may provide reassurance but does not guarantee continuous clinical supervision. Family members are not trained to manage delirium-related behaviors and cannot replace nursing staff observation.
4.Arranging for an unlicensed sitter provides supervision but is less reliable than placing the client near the nursing station, where trained staff can intervene immediately. Sitters may assist but do not replace the need for direct nursing oversight.
Test-taking strategy
- Identify the condition: delirium = acute confusion with hallucinations and disorientation.
- Apply Maslow: prioritize safetyand injury prevention.
- Eliminate options that rely on family or unlicensed staff.
- Select the intervention that ensures continuous monitoring by trained personnel (room near nursing station).
Take Home Points
- Delirium is an acute, reversible disturbance in cognition often triggered by surgery or illness.
- Safety is the priority due to risk of falls, wandering, and hallucination-driven behaviors.
- Placement near the nursing station ensures rapid intervention and continuous monitoring.
Medications and family support may help but are secondary to immediate safety measures.
A client who is delirious yells out to the nurse, “You are an idiot, get me your supervisor.” Which is the best nursing response in this situation?
Explanation
Delirium interpersonal carerequires therapeutic presenceand reassurance when clients display disorientationand agitation. Individuals with fluctuating cognition and impaired attention may misinterpret reality; offering calm support and presence reduces anxiety and reinforces safety.
Rationale for correct answer:
3.Staying with the client and acknowledging that they’re experiencing a difficult timeprovides safety, reduces distress, and uses therapeutic presence. In delirium, reality orientation and consistent support help decrease agitation and foster trust when thought processes are impaired.
Rationale for incorrect answers:
1.Telling the client to calm downand listen dismisses their feelings and can escalate agitation; clients with delirium have impaired attention and cannot simply refocus on instruction without support.
2.Offering to call the supervisor may unintentionally reinforce the delusion and shift focus away from current safety and reassurance; therapeutic presence takes priority over deferring to authority.
4.Asking why they feel calling a supervisor will solve things invites abstract reasoning, which is difficult for someone in a delirious state and may increase confusion rather than provide comfort.
Test-taking strategy
- Identify option that provides therapeutic supportand minimizes escalation.
- Eliminate choices that require abstract reasoningor reinforce delusional beliefs.
- Prioritize safety and reassurancefor an acutely confused client.
Take Home Points
- Delirious clients benefit from therapeutic presence and reassurance.
- Avoid arguing or reinforcing delusional interpretations.
- Use simple, direct, supportive communication.
- Redirect focus to safety and comfort, not abstract explanations.
A delirious client sees a design on the wallpaper and perceives it as an animal. How should a nurse communicate what the client perceived at the change-of-shift report?
Explanation
Deliriuminvolves a global disruption of sensory processingwithin the cerebral cortex. This physiological state leads to an inability to accurately interpret environmental stimuli, resulting in a specific type of perceptual distortion where a real object is transformed into a false mental image.
Rationale for correct answer:
2.This term describes a misinterpretation of realitywhere an actual external stimulus is present but is perceived incorrectly. Unlike a hallucination, which occurs without an object, this phenomenon involves the distortion of physicallight or patterns, such as seeing an animal in a wallpaper design.
Rationale for incorrect answers:
1.A firm, false beliefthat is resistant to logical reasoning is categorized as a thought content disorder. While the client may believe the animal is real, the specific act of misperceiving a visualpattern is a sensory-perceptual error rather than a primary disturbance in the belief system.
3.A sensory experience that occurs in the absence of stimuliis defined as a hallucination. In this scenario, the presence of the wallpaper design provides a physical basis for the perception, which means the experience is an error of interpretationrather than an internally generated sensation.
4.This cognitive distortion occurs when an individual believes that neutral eventsor coincidences have a direct, personal significance. It involves a misinterpretation of the meaning of eventsrather than a literal visual misperception of a physical object or pattern in the room.
Test-taking strategy
- Identify if an external stimulus is present in the question stem.
- Differentiate between sensory-perceptual errors and thought content errors.
- Use the presence of the "wallpaper" as the defining factor for the answer.
- Apply the definition that specifically links an object to a false perception.
Take Home Points
- Illusions are common in delirious states because the brain's ability to integrate and process sensory input is significantly compromised.
- Hallucinations are distinguished by the total lack of an external stimulus, whereas illusions always have a physical trigger.
- Providing adequate lighting and removing patterned rugs or wallpaper can reduce the occurrence of illusions in confused patients.
- Accurate documentation of perceptual disturbances is essential for tracking the severity of a client's neurocognitive dysfunction and response to treatment.
Practice Exercise 3
A nurse is assessing an older adult with the diagnosis of dementia. Which manifestations are expected in this client? Select all that apply.
Explanation
Dementiarepresents a chronic, irreversible loss of neuronal connectivitywithin the cerebral cortex. This progressive decline involves the accumulation of protein aggregatesthat disrupt synaptic transmission, leading to a permanent impairment in memory, language, and the ability to process sensory informationaccurately.
Rationale for correct answer:
2.The clinical term for this manifestation is agnosia, a hallmark of progressive neurodegeneration. It occurs when the sensory associationareas of the brain can no longer link a perceived object to its stored meaning, causing the client to fail at identifying common everyday itemsor faces.
Rationale for incorrect answers:
1.A rigid adherence to routine is a compensatory mechanismused by those with cognitive deficits to maintain a sense of order. While common, it is a behavioral adaptationto loss rather than a primary diagnostic manifestation of the physiological brain damage itself, and thus not the single most representative expected finding.
3.Individuals with advancing cognitive decline typically exhibit a decline in groomingand hygiene due to executive dysfunction. They lose the ability to sequence tasksor maintain the social awareness required for vanity, making a preoccupation with appearance the opposite of what is clinically expected.
4.This symptom refers to distractibility or inattention, which is actually the defining feature of acute delirium. In the stable stages of dementia, the client may be able to focus for short periods, but their primary deficit is the inability to encodeor store the new information they are focusing on.
5.Focusing on early life events is a result of retrograde memorypreservation where long-term memories remain intact while recent ones fade. While frequent in the elderly, it is a feature of agingand mild impairment rather than a specific, defining diagnostic manifestation of the dementia syndrome itself.
Test-taking strategy
- Identify the classic "4 A's" of Alzheimer's (Amnesia, Aphasia, Apraxia, Agnosia).
- Eliminate symptoms that are hallmark indicators of delirium (inattention).
- Recognize that hygiene usually declines rather than improves in dementia.
- Select the option that describes a core neurological deficit of the condition.
Take Home Points
- Agnosia is the physiological inability to recognize objects or people despite intact sensory organs, signifying advanced cortical damage.
- Dementia is characterized by a stable level of consciousness, which differentiates it from the fluctuating awareness seen in delirium.
- Executive dysfunction leads to the loss of complex task sequencing, resulting in the characteristic neglect of personal hygiene and grooming.
- In the clinical setting, nurses must provide frequent reorientation and use simple, direct communication to support the client's impaired sensory processing.
A nurse’s best approach when caring for a confused, older client is to provide an environment with:
Explanation
Confusional statesin the elderly often involve a disruption of cholinergic neurotransmissionand increased sensitivity to environmental stressors. This physiological vulnerability leads to sensory overloadand increased cortisol secretion, which further impairs the client's ability to process information and maintain a sense of environmental security.
Rationale for correct answer:
3.Establishing a consistent therapeutic bondis the most effective way to lower the client's anxiety and provide a sense of stability. A reliable caregiver acts as an external cognitive anchor, helping to orient the patient and reduce the behavioral agitationthat frequently results from the fear and disorientation of cognitive loss.
Rationale for incorrect answers:
1.Providing excessive seclusion often leads to sensory deprivation, which can paradoxically worsen disorientation and trigger visual or auditory hallucinations. For a confused client, isolation removes the external orienting cuesnecessary to maintain a connection to reality, leading to a state of increased psychological withdrawal.
2.High-stimulus social settings can be overwhelming for a brain with impaired executive function, leading to a "catastrophic reaction" or acute distress. While social interaction is important, unstructured group involvementoften provides too many simultaneous stimuli for the client to process, causing cognitive exhaustionand frustration.
4.Introducing frequent changes in routine or a wide range of tasks causes neurological fatigueand increases confusion. Patients with neurocognitive disorders thrive on predictable repetitionand environmental consistency; therefore, a varied schedule creates unnecessary cognitive demandthat the client cannot meet, potentially escalating agitation.
Test-taking strategy
- Identify the client's primary need as safety and security within Maslow's hierarchy.
- Select the option that minimizes stress and maximizes environmental stability.
- Eliminate choices that increase sensory input or cognitive complexity.
- Focus on the psychosocial foundation of the nurse-client relationship.
Take Home Points
- The primary goal of environmental management for a confused client is to minimize anxiety by providing a predictable and supportive atmosphere.
- Consistent caregivers and daily routines help compensate for memory deficits by utilizing environmental cues and habitual patterns.
- Overstimulation is a major trigger for behavioral symptoms in dementia; therefore, interventions should focus on simplicity and calm interaction.
- A trusting relationship allows the nurse to become a familiar point of reference, which is essential for effective reorientation and emotional regulation.
A nurse is planning care for a client with substance abuse delirium. When the nurse implements care that addresses the client’s hygiene needs, which action should be taken?
Explanation
Substance abuse deliriumis an acute disturbance in attention, awareness, and cognitioncaused by intoxication or withdrawal. Clients often exhibit confusion, impaired judgment, and unpredictable behavior, which increases risk for injury during routine care. Safety precautions are essential when addressing hygiene needs.
Rationale for correct answer:
1.Providing an electric shaverinstead of a razor minimizes risk of self-injuryor accidental harm to staff. Clients with delirium may have impaired coordination or sudden agitation, making sharp objects unsafe. This intervention ensures hygiene while prioritizing safety.
Rationale for incorrect answers:
2.Administering medication before hygiene care is inappropriate unless specifically ordered for agitation or withdrawal symptoms. Routine hygiene does not require pre-medication, and unnecessary drug use may worsen delirium.
3.Setting limits for staff involvement does not address the client’s safetyor hygiene needs. Limiting staff could reduce supervision and increase risk of injury during care. Collaboration is necessary, not restriction.
4.Allowing family to dress the client after bathing does not ensure safety or proper hygiene. Family members may lack training to manage delirium-related behaviors, and staff must maintain responsibility for care delivery.
Test-taking strategy
- Identify the condition: delirium from substance abuse involves confusion and unsafe behaviors.
- Apply Maslow: prioritize safetyduring hygiene care.
- Eliminate options that do not directly reduce risk of injury.
- Select the intervention that ensures hygiene while preventing harm (electric shaver).
Take Home Points
- Substance abuse delirium causes acute confusion and impaired judgment, requiring safety-focused care.
- Sharp objects like razors pose risk; electric shavers are safer alternatives.
- Medication is not routinely required before hygiene unless ordered for agitation.
- Staff must maintain responsibility for hygiene care, with family support as appropriate.
A patient presents with sudden confusion, agitation, and hallucinations. The nurse orders laboratory and imaging investigations. Which findings are commonly associated with delirium? Select all that apply.
Explanation
Deliriumis a transient, usually reversible neuropsychiatric disordercharacterized by an acute decline in attention and cognitive function. It is frequently triggered by systemic illness, toxicity, or metabolic derangements that disrupt neurotransmitter balance, particularly involving cholinergic and dopaminergic pathways within the brain.
Rationale for correct answers:
1.Significant shifts in serum sodiumor calcium levels directly impair neuronal excitability and signal transduction. These metabolic disturbancesare classic triggers for encephalopathy, manifesting as the acute cognitive fluctuations and altered consciousnessobserved in the delirious patient.
2.Adequate cerebral oxygenation is vital for maintaining cognitive clarity and synaptic function. Low oxygen levels detected via arterial blood gasresult in global cerebral dysfunction, which is a frequent and life-threatening cause of acute confusionin clinical settings.
4.The presence of a urinary tract infection, especially in the elderly, releases inflammatory cytokines that can cross the blood-brain barrier. This systemic inflammatory response often presents solely as acute behavioral changesand agitation rather than typical focal symptoms.
5.While not specific for the cause, an electroencephalogramtypically reveals a diffuse reduction in the frequency of background activity. This generalized slowingis a hallmark physiological finding that helps clinicians differentiate delirium from certain primary psychiatric disorders.
Rationale for incorrect answer:
3.Evidence of cortical atrophyon neuroimaging is a structural finding typically associated with chronic, progressive conditions like Alzheimer’s disease. While patients with atrophy are at higher risk for delirium, the atrophy itself represents permanent tissue lossrather than the acute, reversible process.
Test-taking strategy
- Distinguish between "acute" vs. "chronic" indicators; delirium is characterized by sudden physiological changes.
- Identify which choices represent systemic "triggers" versus structural "changes."
- Evaluate each option against the clinical presentation of sudden onset and fluctuating course.
Take Home Points
- Delirium is defined by an acute onset and a fluctuating course of symptoms, unlike the slow, steady decline seen in dementia.
- Laboratory investigations should focus on reversible causes such as occult infection, medication toxicity, and metabolic imbalances.
- Management primarily involves treating the underlying medical condition while ensuring the patient's physical safety and psychological comfort.
- Sensory impairments, such as hearing or vision loss, can exacerbate the symptoms of delirium and should be corrected to aid reorientation.
A nurse is assisting with the diagnostic evaluation of a patient who has developed acute confusion and fluctuating attention. Which nursing action is essential during the diagnostic evaluation of delirium?
Explanation
Deliriumis a transient neuropsychiatric syndromecharacterized by an acute, fluctuating impairment in attention and cognitive function. It is considered a medical emergencythat often signals an underlying systemic illness, such as sepsis or metabolic imbalance, requiring frequent surveillanceto distinguish it from static conditions like dementia.
Rationale for correct answer:
1.Because the hallmark of delirium is a waxing and waningcourse, the nurse must perform continuous, serial assessments of the patient's mental status. Subtle changes in the ability to sustain attentionor follow simple commands are often the earliest clinical indicators of an acute physiological decline, even before overt agitation or vital sign changes occur.
Rationale for incorrect answers:
2.The immediate administration of antipsychotic medicationsbefore a thorough diagnostic assessment is contraindicated as these drugs can mask clinical symptomsand hinder the identification of the underlying cause. Pharmacological interventions are reserved for patients in severe distress or those posing an immediate safety riskafter non-pharmacological strategies have failed.
3.Relying exclusively on neuroimaging resultsis inappropriate because delirium is a functional, rather than a primarily structural, brain disturbance. While CT or MRI scans may be used to rule out a stroke or intracranial hemorrhage, the diagnosis of delirium is fundamentally a clinical onebased on history, bedside assessment, and the identification of precipitating medical factors.
4.Delaying clinical documentationuntil a formal diagnosis is confirmed is a violation of nursing standards and jeopardizes patient safety. Accurate, real-time charting of behavioral fluctuationsand cognitive deficits is essential for the interdisciplinary team to recognize the fluctuating patternthat is diagnostic of delirium and to track the effectiveness of interventions.
Test-taking strategy
- Identify the "hallmark" characteristic of the condition (fluctuation) and match it to the nursing action (continuous monitoring).
- Eliminate "all-or-nothing" words like "solely" or "immediately" which often indicate incorrect, narrow nursing actions.
- Prioritize assessment (nursing process) over immediate pharmacological intervention in a diagnostic scenario.
Take Home Points
- The Confusion Assessment Method (CAM) is the gold standard bedside tool used by nurses to detect delirium by focusing on acute onset and inattention.
- Hypoactive delirium is the most frequently missed subtype because patients appear lethargic or depressed rather than agitated.
- Nurses are in a strategic position to prevent delirium by implementing non-pharmacological protocols like early mobilization and sleep hygiene.
- A collateral history from family members is vital during evaluation to establish the patient's baseline cognitive and functional status.
Practice Exercise 4
A nurse is assessing a 72-year-old client with sudden confusion and fluctuating attention. To differentiate delirium from dementia, which features should the nurse consider? Select all that apply.
Explanation
The primary challenge in geriatric nursing is distinguishing between Delirium(a medical emergency) and Dementia(a chronic condition). Delirium is essentially "acute brain failure" triggered by a systemic issue, whereas dementia is a structural, neurodegenerative process.
Rationale for correct answers:
1.The temporal onsetis a definitive diagnostic feature. Delirium occurs acutely(hours to days), often triggered by a specific event like an infection or medication change. Dementia is a "slow-motion" decline that is often only noticed in retrospect over months or years.
2.The fluctuating courseis a hallmark of delirium. Symptoms "wax and wane," meaning a patient may seem perfectly lucid during morning rounds but become profoundly disoriented and agitated in the evening ("sundowning"). Dementia symptoms are generally stable day-to-day.
4.Inattentionis the diagnostic "anchor" for delirium. A delirious patient cannot maintain a conversation or follow simple commands because their brain cannot filter stimuli. In the early to middle stages of dementia, a patient is usually still able to pay attention, even if their memory is failing.
Rationale for incorrect answers:
3.This describes Dementia. A gradual decline is the expected path of neurodegenerative diseases like Alzheimer’s. If the decline is sudden, it is delirium until proven otherwise.
5.This is a feature of Dementia. In dementia, the patient is usually "awake and alert" (clear consciousness) despite their memory deficits. In delirium, the level of consciousnessis almost always altered—ranging from hyper-alert and agitated to drowsy and lethargic.
Test-taking strategy
- Use the "3 A's" of Delirium: Acute, Attention (impaired), and Altered consciousness.
- Remember that Delirium is reversibleand Dementia is progressive.
- Look for "fluctuation"—if the patient's status changes within a single shift, it points to delirium.
Take Home Points
- When an elderly patient with existing dementia suddenly becomes "much worse," this is called delirium superimposed on dementiaand requires an immediate medical workup (usually for a UTI or pneumonia).
- The Confusion Assessment Method (CAM)is the best tool to identify these differentiating features at the bedside.
- Delirium is a physiological "warning light" for the body; treating the underlying cause (dehydration, infection, or pain) is the only way to resolve the confusion.
A nurse is evaluating a patient who appears withdrawn and has difficulty concentrating. Which feature best distinguishes delirium from depression?
Explanation
Deliriumand depressioncan often look similar in older adults, particularly in the hypoactivesubtype where the patient is withdrawn and lethargic. However, the physiological basis of delirium (acute metabolic/chemical insult) allows for a recovery profile that is distinct from the neurotransmitter changes and psychological patterns seen in clinical depression.
Rationale for correct answer:
1.The most significant differentiator is the reversibilityof symptoms. Delirium is a secondary symptom of a primary medical problem (like a UTI, hypoxia, or electrolyte imbalance). Once that "trigger" is identified and corrected, the cognitive symptoms—the confusion and inattention—resolve rapidly. Depression requires long-term pharmacological or psychotherapeutic intervention over weeks or months to show significant improvement.
Rationale for incorrect answers:
2.While low mood and hopelessnessare hallmarks of depression, they are psychological states rather than physiological markers. A delirious patient may appear "sad" or "flat," but this is due to a depressed level of consciousness or global brain failure rather than the primary mood disorder seen in depression.
3.This is a common feature of depression(specifically melancholic depression). In contrast, delirium typically exhibits sundowning, where symptoms significantly worsen in the late afternoon and eveningdue to fatigue and the loss of orienting light cues.
4.An insidious onsetis characteristic of dementiaor major depressive disorder, which develop over weeks or years. Delirium is defined by its acute onset, appearing suddenly over hours or days.
Test-taking strategy
- Focus on the cause-and-effectrelationship: Delirium has a medical "cause" and a rapid "effect" (resolution) once treated.
- Remember that Delirium is a "physiological"problem, while Depression is a "psychiatric/mood"problem.
- In the elderly, always look for the word "Acute"for delirium and "Chronic/Long-term"for depression or dementia.
Take Home Points
- Inattentionis the diagnostic key: A depressed patient can usually focus on a conversation if prompted, whereas a delirious patient physically cannot maintain attention due to neurochemical imbalance.
- Delirium is often the first sign of physical illness in the elderly; never assume a withdrawn older adult is "just depressed" until medical causes are ruled out.
- The Geriatric Depression Scale (GDS)can be used once the patient's delirium has cleared to determine if an underlying mood disorder exists.
- Nursing care for both involves safety, but the priority for delirium is medical stabilization, while for depression it is psychosocial support and safety(suicide precautions).
A client presents with acute confusion, visual hallucinations, and disorientation. Which assessment findings help differentiate delirium from schizophrenia? Select all that apply.
Explanation
While both deliriumand schizophreniainvolve a detachment from reality, they originate from entirely different pathophysiological roots. Delirium is an acute medical syndromecaused by systemic physiological stress, whereas schizophrenia is a chronic psychiatric disorderinvolving complex dopamine dysregulation in specific brain pathways.
Rationale for correct answers:
1.Attention and consciousnessare the primary physiological markers that separate the two. In delirium, the patient’s level of consciousness fluctuates(waxing and waning), and they have a profound inability to focus. In schizophrenia, unless the patient is heavily medicated, they are typically alert and have stable consciousness, even if they are actively hallucinating.
2.Disorientationis common in delirium. A delirious patient often forgets where they are or what year it is because their brain cannot process environmental cues. Patients with schizophrenia are usually oriented to person, place, and time, although their interpretation of that reality may be delusional.
5.Delirium is a secondary symptomof an underlying medical condition (e.g., toxicity, infection, or metabolic failure). Once that medical trigger is treated, the confusion and hallucinations are reversible. Schizophrenia is a lifelong, chronic condition that requires ongoing management rather than a "cure" for an underlying acute illness.
Rationale for incorrect answers:
3.Hallucination types are a key clue. Delirium is strongly associated with visual hallucinations(seeing things that aren't there), whereas schizophrenia is most often characterized by auditory hallucinations(hearing voices). The client in the stem has visual hallucinations, which points more toward delirium.
4.Delirium is acute and fluctuating, not chronic or stable. A "chronic, stable course" describes the residual phase of schizophrenia or certain types of dementia, but it is the polar opposite of the rapid, unstable nature of delirium.
Test-taking strategy
- Use the "Medical vs. Psychiatric"filter: If the symptoms fluctuate and attention is gone, think Medical (Delirium).
- Remember the "Eyes vs. Ears"rule: Visual hallucinations are usually medical/organic (Delirium); Auditory hallucinations are usually psychiatric (Schizophrenia).
- Any mention of "reversibility" or "underlying cause" should immediately lead you to Delirium.
Take Home Points
- When an older adult suddenly starts seeing "bugs on the wall" or "shadows," the nurse should look for a physical trigger(like a new medication or dehydration) before considering a psychiatric diagnosis.
- Vital signsare often unstable in delirium (tachycardia, fever, hypertension) but typically remain normal in schizophrenia.
- A patient in a schizophrenic crisis may be "disorganized" in their thoughts, but their circadian rhythmand basic arousal are usually not as fragmented as those of a patient in delirium.
A nurse is planning non-pharmacological management for a client with delirium. Which interventions should be included? Select all that apply.
Explanation
Delirium managementprioritizes non-pharmacological interventions because they address the root cause of cognitive fragmentation without introducing the side effects of sedative-hypnotic drugs. These strategies focus on "stabilizing the sensorium"—helping the brain correctly interpret the environment and maintain its natural circadian rhythm.
Rationale for correct answers:
1.A well-lit environmentduring the day and a quiet one at night help regulate the client’s internal clock and reduce sensory misperceptions. Familiar objects (like a family photo or personal clock) provide "visual anchors" that decrease the likelihood of hallucinations or illusions.
2.Since delirium involves an inability to maintain attention, the nurse must provide frequent reorientation. Repeatedly stating the date, time, and location helps the client bridge memory gaps and reduces the fear that often leads to agitation.
3.Early mobilizationis a key component of the Hospital Elder Life Program (HELP). Physical activity improves cerebral oxygenation, reduces the risk of inflammation, and helps reset the sleep-wake cycle, all of which facilitate a faster return to a normal mental state.
5.Family engagementis one of the most effective tools in delirium care. Familiar voices and faces provide a level of security and "reality testing" that staff members cannot replicate, effectively reducing the need for chemical or physical restraints.
Rationale for incorrect answer:
4.Benzodiazepinesare generally avoidedin the management of delirium because they frequently cause a "paradoxical reaction," making the client more confused and agitated. They also increase the risk of falls and respiratory depression. They are typically reserved only for delirium associated with alcohol or sedative withdrawal.
Test-taking strategy
- Look for "Natural" vs. "Artificial": Choose interventions that mimic normal life (light, family, moving).
- Recognize Benzodiazepinesas a "red flag" drug for the elderly and those with delirium.
- Think of the "Environmental Stability"rule: Anything that makes the environment more predictable is usually a correct answer.
Take Home Points
- Non-pharmacological interventions are the first-line therapyfor all types of delirium.
- Sleep hygiene(clustering care to avoid waking the patient at night) is just as important as daytime orientation.
- Ensuring the patient has their glasses and hearing aidsis a critical non-pharmacological step to prevent sensory deprivation.
- If a patient becomes agitated, the nurse should first look for a physical source of discomfort(like a full bladder or pain) before considering medication.
A nurse is caring for a patient who has developed acute delirium during hospitalization. Which nursing action is most important in preventing complications in a patient with delirium?
Explanation
Deliriumis an acute neurocognitive syndromecharacterized by a fluctuating disturbance in attention and awareness. It often results from underlying physiological triggers like metabolic imbalancesor infections, requiring immediate identification of the precipitating causeto prevent permanent cognitive decline or mortality.
Rationale for correct answer:
1.Prioritizing safety and physiological stabilityaddresses the immediate risk of injury and functional decline. Constant monitoring of vital signs and hydrationprevents secondary complications like acute kidney injury or falls, while early detectionof behavioral shifts allows for non-pharmacological stabilization.
Rationale for incorrect answers:
2.Relying solely on pharmacological managementis dangerous because sedatives like benzodiazepines or antipsychotics can often exacerbate cognitive cloudingor cause paradoxical agitation. Nursing care must focus on the underlying etiologyrather than just suppressing behavioral symptoms with medication.
3.Restricting family visits is counterproductive as familiar facesprovide essential reorientation and emotional support. Family presence helps reduce the anxiety and fearassociated with a strange hospital environment, which is a primary non-pharmacological intervention for decreasing agitation.
4.Limiting orientation to once daily is insufficient because delirium fluctuates throughout the day. Patients require frequent reorientationusing clocks, calendars, and verbal cues to maintain a connection to reality and reduce the profound sensory perceptual distortionscommon in this state.
Test-taking strategy
- Apply Maslow's Hierarchy of Needs; safety and physiological integrity (hydration) take precedence over other interventions.
- Use the "Acute vs. Chronic" rule; delirium is an emergency requiring constant assessment rather than infrequent or limited interventions.
- Identify the most comprehensive option that addresses multiple patient needs simultaneously.
Take Home Points
- Delirium is a medical emergency that is often reversible if the underlying physiological or pharmacological trigger is identified and treated promptly.
- Nursing interventions must prioritize a calm, well-lit environment and consistent reorientation to prevent sensory overload and injury.
- The Confusion Assessment Method (CAM) is a standardized tool used by clinicians to distinguish delirium from dementia based on its acute onset and fluctuating course.
- Physical restraints should be avoided as they often increase agitation and the risk of complications like skin breakdown or strangulation in a delirious patient.
Practice Exercise 5
A nurse is caring for clients who have extended stays in the critical care unit, where they often experience delirium. The known predisposing contributors to the development of delirium are: Select all that apply.
Explanation
Deliriumis a complex syndrome resulting from the acute disruption of neurotransmitter homeostasis, specifically involving acetylcholine and dopamine. This neurobiological instability is frequently triggered by systemic inflammationor metabolic insults that affect the brain's ability to maintain a stable and coherent level of conscious awareness.
Rationale for correct answers:
2.Underlying structural injuries significantly lower the cerebral reserveavailable to handle physiological stress. Any previous neurological insultmakes the blood-brain barrier more permeable and the neurons more susceptible to the neurotoxic effectsof systemic illness, dramatically increasing the risk of acute confusion.
3.Existing neurodegenerative conditions, such as dementia, are the most significant predisposing factorsfor acute cognitive failure. The brain's baseline synaptic dysfunctionmeans that even minor metabolic changes can trigger a profound and rapid decline in the level of consciousnessand attention.
Rationale for incorrect answers:
1.Clinical evidence shows that advanced age, specifically being over 65 years, is a primary risk factor for cognitive instability. Younger patients generally have a higher physiological resilienceand a more robust neurovascular system, making them less likely to develop delirium compared to the vulnerable geriatric population.
4.The presence of familiar individuals is actually a protective factorrather than a contributor to the syndrome. Family members provide essential orienting cuesand emotional support, which can help mitigate the sensory overload of the critical care environment and reduce the severity of confusion.
Test-taking strategy
- Distinguish between predisposing (baseline) and precipitating (triggering) factors.
- Recognize that "presence of family" is a therapeutic intervention, not a risk.
- Identify that structural or chronic brain changes reduce neurobiological resilience.
- Apply the age-related principle that risk increases with advancing years.
Take Home Points
- Delirium is often the result of a "double hit": a vulnerable brain (predisposing factor) meeting an acute medical stressor (precipitating factor).
- Chronic cognitive impairment is the leading risk factor for developing delirium, as these patients have significantly reduced neurotransmitter stores.
- Environmental interventions, such as ensuring the presence of family and maintaining a day-night cycle, are key to preventing cognitive rot in critical care.
- Early identification of high-risk patients allows for proactive monitoring and the minimization of deliriogenic medications like benzodiazepines.
A nurse is reviewing examples of treatable (reversible) forms of neurocognitive disorder (NCD). Which of the following causes are treatable? Select all that apply.
Explanation
Treatable (reversible) neurocognitive disordersresult from acute, correctable medical, metabolic, or nutritional conditionsthat cause cognitive impairment. Identifying and addressing these causes early can restore cognitive function, differentiating them from progressive, irreversible dementiaslike Alzheimer’s disease.
Rationale for correct answers:
3.Electrolyte imbalances(e.g., sodium, calcium, or potassium disturbances) can disrupt neuronal function, causing confusion or cognitive deficits. Correcting the imbalance often reverses cognitive impairmentquickly.
4.HIV-related cognitive impairmentcan be improved with antiretroviral therapy, especially in early stages, making it a reversible cause of NCDif treated appropriately.
5.Folate deficiencyimpairs DNA synthesis and neurotransmitter function, leading to cognitive decline. Supplementation with folic acidcan restore cognitive function if caught early.
Rationale for incorrect answers:
1.Multiple sclerosiscauses chronic, progressive demyelination; cognitive deficits are part of a non-reversible neurodegenerative process, so it is not fully treatable.
2.Multiple small brain infarcts(vascular dementia) lead to irreversible neuronal loss. While risk factors can be managed, existing cognitive deficits are generally not reversible.
Test-taking strategy
- Identify causes that are acute, correctable, or metabolic/nutritional.
- Differentiate progressive neurodegenerative disordersfrom reversible conditions.
- Focus on interventions that restore cognitive function.
Take Home Points
- Treatable NCDs often result from metabolic, infectious, or nutritional causes.
- Reversal is possible with early identification and treatment.
- Progressive disorders like MS or vascular dementiaare not reversible.
- Electrolyte, HIV, and folate deficiencies are key reversible contributors to cognitive impairment.
A 68-year-old client in the ICU develops sudden confusion, fluctuating attention, and hallucinations. Which pathophysiological mechanisms are most likely contributing to delirium? Select all that apply.
Explanation
Deliriumis a complex neuropsychiatric syndrome resulting from a breakdown in neuronal communication. It occurs when a systemic physiological stressor (like ICU-related sepsis or hypoxia) disrupts the delicate balance of neurotransmitters and impairs the metabolic efficiency of the cerebral cortex.
Rationale for correct answers:
1.Acetylcholine is the primary neurotransmitter responsible for attention, learning, and memory. A sudden cholinergic deficitis the most common pathway to delirium; when these levels drop, the brain loses its "executive filter," leading to the hallmark symptoms of inattention and disorganized thinking.
2.While acetylcholine is too low, dopamine is often too highin acute confusional states. This catecholamine excess—frequently seen in the hyperactive subtype—is directly linked to psychomotor agitationand the vivid visual hallucinations the client is experiencing.
3.The brain requires a constant, high-volume supply of glucose and oxygen. In the ICU, conditions like hypotension, anemia, or respiratory failure lead to global cerebral hypometabolism. When the brain is "starved" of these resources, neurons cannot maintain their membrane potential, leading to acute cognitive failure.
Rationale for incorrect answers:
4.While acute electrolyte shifts can trigger delirium, chronicconditions like hypocalcemia generally do not cause sudden-onset confusion. The brain has typically adapted to chronic imbalances over time. It is acute changes(e.g., sudden hypomagnesemia or hyponatremia) that precipitate a delirious state.
5.High levels of serotonin are associated with Serotonin Syndrome, which is a specific drug-induced toxidrome (causing tremors, hyperreflexia, and fever). Delirium itself is more commonly associated with a relative deficiencyof serotonin or imbalances in the tryptophan pathway, rather than a general state of "excessive release."
Test-taking strategy
- Connect "Inattention" to Acetylcholine(the attention chemical).
- Connect "Hallucinations/Agitation" to Dopamine(the arousal chemical).
- Recognize that "Sudden" symptoms require "Acute" causes—eliminate "Chronic" options.
- Always prioritize Cerebral Perfusionas the brain's baseline requirement for any function.
Take Home Points
- Delirium is often called "acute brain failure," emphasizing that it is a physiological emergency just like heart or kidney failure.
- The balance between acetylcholine (inhibitory/attentional)and dopamine (excitatory)is the key neurochemical axis in delirium management.
- ICU delirium is frequently driven by neuroinflammation, where systemic cytokines cross the blood-brain barrier and disrupt synaptic transmission.
- Addressing the underlying cause (e.g., fixing blood pressure to improve perfusion) is the only way to restore normal neurochemical balance.
A client with hyperactive delirium is pulling at IV lines and wandering the unit. Which intervention is priority for the nurse?
Explanation
Hyperactive deliriumpresents an immediate challenge to patient safety due to the combination of psychomotor agitationand impaired judgment. The priority is to implement a "safety-first" approach that utilizes the least restrictive measures to prevent the displacement of essential medical devices and falls.
Rationale for correct answer:
2.The priority nursing actionis to ensure the client's physical safety through non-pharmacological means first. Providing close observation(such as a 1:1 sitter or moving the patient closer to the nurse's station) allows for immediate intervention if the client attempts to pull at lines. Simultaneously, frequent reorientationhelps calm the patient's fear and "ground" them in reality, which can reduce the drive to wander or interfere with care.
Rationale for incorrect answers:
1.Physical restraints are a last resortand should only be used after all other safety measures have failed. Restraints often increase agitationand can lead to serious injury or psychological trauma in a delirious patient. They also require a specific physician's order and cannot be applied "immediately" unless there is an imminent life-threatening risk.
3.Administering a potent antipsychotic like haloperidol requires a thorough clinical reassessmentof the patient's status and vital signs. While it can be used for severe agitation, it is not the first-line action. Furthermore, haloperidol carries risks such as QTc prolongationand extrapyramidal side effects, making careful monitoring essential.
4.Restricting nutrition and hydration is counterproductiveand dangerous. Dehydration and metabolic imbalances are frequent causes of delirium; reducing intake will likely worsen the client's physiological instability and increase their confusion and agitation.
Test-taking strategy
- Always prioritize least invasiveand non-pharmacologicalinterventions first.
- In safety questions, look for "Observation" or "Reorientation" before "Restraint" or "Medication."
- Eliminate options that suggest withholding basic needs (food/water) or skipping assessment steps.
Take Home Points
- The use of "sleeves" or wrapsover IV sites can often prevent a confused patient from pulling at lines without the need for full physical restraints.
- Wanderingis a sign of disorientation; creating a safe path for the patient to walk or providing a "low bed" with floor mats can mitigate fall risks.
- Delirium is often multifactorial; while maintaining safety, the nurse must continue to investigate the "why" behind the behavior (e.g., Is the patient in pain? Is their bladder full?).
- Continuous observation provides the most accurate data on the fluctuating natureof the delirium, allowing for timely adjustments to the care plan.
A nurse is caring for a client with delirium caused by urinary tract infection. Which clinical manifestations differentiate delirium from dementia? Select all that apply.
Explanation
Deliriumis a medical emergency that represents an acute physiological disruption, whereas dementiais a chronic, neurodegenerative process. Differentiating between the two is critical because the management of a delirium trigger, such as a urinary tract infection (UTI), must be immediate to prevent permanent brain injury or death.
Rationale for correct answers:
1.Delirium is characterized by an acute onset, often occurring over hours or days. In this scenario, the UTI serves as the physiological stressor that causes the client's mental status to "crash" suddenly. In contrast, dementia symptoms are stable day-to-day for long periods.
2.The "hallmark" of delirium is a fluctuating level of consciousness. A client may be alert and oriented at 09:00 but somnolent or highly agitated by 11:00. This "waxing and waning" of attention and arousal does not occur in the early or middle stages of dementia, where alertness remains relatively stable.
5.Unlike dementia, which is currently incurable and progressive, delirium is potentially reversible. Once the underlying cause (the UTI) is treated with appropriate antibiotics and hydration, the client's cognitive function typically returns to its previous baseline.
Rationale for incorrect answers:
3.This is a characteristic of dementia. In delirium, short-term memory and immediate attention are impaired, but long-term memories usually remain intact until the delirium becomes very severe. In dementia, particularly Alzheimer's, the loss of long-term memories occurs as the disease progresses over years.
4.This describes the pathological trajectory of dementia. Dementia is a "slow burn" where the brain gradually loses its ability to function. Delirium is an "acute fire" that requires urgent intervention to extinguish the underlying cause.
Test-taking strategy
- Think of Deliriumas a "Storm" (Sudden, violent, and passes once the weather clears).
- Think of Dementiaas "Erosion" (Slow, permanent, and progressive).
- Associate "Fluctuation" and "Acute" exclusively with Delirium in multiple-choice questions.
Take Home Points
- In older adults, a UTImay not present with classic symptoms like fever or dysuria; instead, acute confusionis often the first and only sign.
- When a patient with known dementia suddenly gets "worse," the nurse should suspect superimposed deliriumand look for an infection or medication change.
- Assessing for inattention(e.g., asking the patient to name the months of the year backward) is the most sensitive way to detect the "sudden" change in delirium.
- The recovery from delirium can take days or weeks after the infection is cleared, especially in the elderly with low cognitive reserve.
Comprehensive questions
A 75-year-old client is admitted with sudden confusion, restlessness, and agitation. Which predisposing factors are likely contributing to the development of delirium? Select all that apply.
Explanation
Deliriumis an acute neurocognitive failure characterized by a global disruptionof cerebral metabolism. This syndrome occurs when the neurobiological resilienceof a patient is overwhelmed by a combination of baseline vulnerabilities and acute physiological insults, leading to synaptic dysfunction.
Rationale for correct answers:
1.Biological senescence leads to a reduction in neurotransmitterreserves, particularly acetylcholine, which is essential for maintaining attention. This decreased physiological reservemakes the older brain significantly more vulnerable to metabolic stress compared to younger individuals, serving as a primary risk factor.
2.Prolonged ethanol exposure causes permanent neurostructural changesand chronic depletion of thiamine and other essential nutrients. This history creates a state of neuronal hypersensitivityand impaired neurovascular regulation, which dramatically increases the probability of an acute confusional episode during illness.
5.The physiological stress of a major procedure triggers a systemic inflammatory responsethat can cross the blood-brain barrier. Combined with the neurotoxic effectsof anesthetic agents and postoperative pain, surgical intervention is one of the most common precipitating factors for cognitive failure.
Rationale for incorrect answers:
3.This is classified as a precipitating factorrather than a predisposing factor. While it is the immediate trigger for the confusion, it is an acute physiological insultthat acts upon the patient's existing vulnerabilities, rather than being a baseline characteristic of the patient themselves.
4.Chronic management of blood pressure is generally considered a protective factorfor brain health as it prevents vascular damage. Unless the medication causes acute electrolyte imbalancesor profound hypotension, its long-term use does not typically predispose a patient to the development of delirium.
Test-taking strategy
- Distinguish between predisposing (baseline) and precipitating (triggering) factors.
- Focus on the patient's history and age as baseline vulnerabilities.
- Recognize that acute medical events like infections are triggers, not predispositions.
- Apply knowledge of how chronic substance use lowers the threshold for confusion.
Take Home Points
- Predisposing factors are baseline vulnerabilities like advanced age, sensory impairment, or pre-existing brain damage that lower the delirium threshold.
- Precipitating factors are the immediate triggers, such as infections, medications, or metabolic disturbances, that push a vulnerable brain into delirium.
- Identifying high-risk patients early allows for non-pharmacological interventions, such as early mobilization and reorientation, to prevent cognitive decline.
- Delirium is often multifactorial, occurring when a highly vulnerable patient experiences even a minor physiological stressor.
A client with postoperative confusion is hyperactive, restless, and hallucinating. Which type of delirium is this client exhibiting?
Explanation
Hyperactive deliriumis a neurobehavioral state driven by autonomic nervous systemoveractivity and increased dopaminergic signaling. It involves a rapid fluctuation in cortical excitability, manifesting as psychomotor agitation and heightened arousal levels that can compromise patient safety.
Rationale for correct answer:
1.This subtype is characterized by increased psychomotor activity, agitation, and vivid sensory-perceptual distortions. The client's specific presentation of excessive restlessnessand the presence of hallucinations are the hallmark diagnostic indicators of the hyperactive variant of this acute syndrome.
Rationale for incorrect answers:
2.This clinical variant presents with lethargy and sedation, often being misidentified as depression or simple fatigue. Clients in this state exhibit reduced motor activityand a withdrawal from the environment, which is the exact opposite of the restlessness and hyperactivity described in the question.
3.This classification is reserved for patients whose symptoms oscillate between statesof agitation and extreme somnolence. While common in the clinical setting, the scenario specifically describes a sustained hyper-aroused staterather than a transition between hyperactivity and the lethargic behaviors of the hypoactive type.
4.This term is a clinical misnomer because the syndrome is defined by its acute and reversiblenature. Cognitive impairment that persists long-term is categorized as a neurodegenerative disorderor dementia, whereas this condition must involve a sudden onset related to a physiological stressor.
Test-taking strategy
- Match the clinical descriptors (restless, hyperactive) directly to the subtype name.
- Differentiate between "active" behaviors and "passive" withdrawal.
- Recognize that delirium is by definition an acute, not chronic, condition.
- Eliminate "mixed" unless the stem describes a transition between arousal levels.
Take Home Points
- Hyperactive delirium is the most easily recognized form due to overt behaviors like agitation, climbing out of bed, and hallucinations.
- Hypoactive delirium is more common in the elderly but frequently goes undiagnosed because the patient appears quiet or pleasantly confused.
- Mixed delirium involves a fluctuating course where the patient may be agitated at night (sundowning) and somnolent during the day.
- Management of hyperactive delirium focuses on identifying the underlying physiological trigger while ensuring the patient's immediate physical safety.
A nurse is caring for a client with hypoactive delirium. Which clinical manifestations should the nurse expect? Select all that apply.
Explanation
Hypoactive deliriumis a neurocognitive state characterized by a profound reduction in metabolic cerebral activity. It involves a disruption of the ascending reticularactivating system, leading to a state of pathological withdrawal and decreased responsiveness to the immediate environment.
Rationale for correct answers:
1.A significant reduction in psychomotoroutput is the defining clinical feature of this subtype. The client exhibits a lack of spontaneous movement and physical unresponsiveness, which results from a global depression of the motor cortex and executive planning areas of the brain.
2.The neurocognitive slowing associated with this condition results in delayed verbal processingand execution. This manifestation reflects the reduced synaptic efficiencyand slowed conduction velocity within the language and speech centers, leading to significant pauses and diminished vocal output.
5.A restricted range of emotional expression is common as the client becomes internally preoccupiedand disconnected. This diminished responsiveness to social stimuli is a physiological consequence of decreased dopaminergic activity, causing the client to appear apathetically detached from their surroundings or family members.
Rationale for incorrect answers:
3.Sensory-perceptual distortions are predominantly associated with the hyperactive variantof this syndrome. While they can occasionally occur in mixed states, the hypoactive profile is characterized by sensory withdrawaland a lack of active engagement with false perceptions or environmental stimuli.
4.Heightened psychomotor arousal and irritability are the clinical opposites of the lethargic statedescribed. These behaviors indicate a state of sympathetic nervous systemoveractivity, which is the hallmark of the hyperactive subtype rather than the passive, withdrawn presentation of the hypoactive type.
Test-taking strategy
- Identify the prefix "hypo-" as meaning low or decreased.
- Group symptoms that reflect a "slowed" or "withdrawn" physiological state.
- Eliminate "active" symptoms like agitation or vivid sensory distortions.
- Recognize that hypoactive delirium is often misdiagnosed as depression due to the flattened affect.
Take Home Points
- Hypoactive delirium is the most common form of the syndrome in the elderly but is frequently overlooked because the patient is quiet and non-disruptive.
- The primary clinical markers include lethargy, somnolence, and a significant slowing of both physical movements and speech patterns.
- This subtype carries a poorer prognosis than the hyperactive form, often because the underlying medical cause remains undetected for a longer period.
- Nursing care for hypoactive delirium must focus on frequent skin assessments and mobilization to prevent the complications of prolonged immobility.
A client recovering from hip surgery becomes disoriented, restless, and asks repeatedly where the bathroom is. What is the nurse’s priority intervention?
Explanation
Postoperative disorientationin the elderly often results from neurochemical instabilitycaused by anesthetic agents and the physiological stress of surgery. This state leads to a loss of situational awareness, where the brain's ability to process and store new environmental information is temporarily impaired by metabolic and inflammatory insults.
Rationale for correct answer:
2.The initial nursing action must focus on providing cognitive anchorsthrough therapeutic communication. Verbal reorientation and calm reassurance help stabilize the patient’s sensory-perceptual processing, reducing the anxiety that drives restless behavior and preventing the escalation of an acute confusional state into a safety crisis.
Rationale for incorrect answers:
1.Assigning a dedicated observer is a valid safety intervention, but it is not the primary therapeutic action for addressing the disorientation itself. While it provides for constant monitoring, it does not directly intervene to correct the underlying cognitive deficit or soothe the client's immediate psychological distress.
3.Pharmacological sedation should only be utilized as a last resortwhen the patient’s behavior poses an imminent threat to physical safety. Administering antipsychotics before attempting non-pharmacological de-escalation can worsen the clinical pictureby masking symptoms or causing adverse extrapyramidal side effects in a vulnerable brain.
4.Complete social isolation often exacerbates confusion by removing meaningful stimuliand orienting cues. While high-intensity environments should be managed, the presence of supportive family membersor familiar faces is actually a protective factor that can help the client regain their sense of place and identity.
Test-taking strategy
- Prioritize the least invasive and most therapeutic intervention first.
- Follow the nursing process by attempting to reorient before using physical or chemical restraints.
- Apply Maslow's hierarchy by addressing the psychological safety of the client through communication.
- Eliminate options that move directly to medication or isolation without first attempting verbal intervention.
Take Home Points
- Reorientation should be the first step in managing acute confusion, utilizing clocks, calendars, and frequent verbal cues to ground the patient.
- Postoperative delirium is often transient, and non-pharmacological strategies can effectively manage restlessness without the side effects of psychotropic drugs.
- Nursing interventions for a disoriented patient must balance the need for a quiet environment with the need for meaningful, orienting social contact.
- Promptly addressing the client's immediate needs, such as the frequent questions about the bathroom, can prevent the escalation of agitation and reduce the risk of falls.
A nurse is assessing a 78-year-old postoperative client who is confused, agitated, and reports seeing “bugs crawling on the walls.” Which manifestations support a diagnosis of delirium? Select all that apply.
Explanation
Deliriumrepresents an acute failure of cerebral neurotransmission, often involving a deficit in cholinergic activity and an excess of dopaminergic signaling. This neurochemical imbalance leads to a disrupted consciousnesswhere the brain cannot accurately filter or interpret sensory input, resulting in the rapid development of neuropsychiatric symptoms.
Rationale for correct answers:
1.A sudden shift in mental status occurring over hours or daysis a primary diagnostic requirement. This rapid change indicates an acute physiological insult, such as surgical stress or metabolic derangement, which overwhelms the brain’s homeostatic mechanisms more quickly than the years-long progression seen in neurodegenerative diseases.
2.The waxing and waningof arousal levels is the most specific clinical indicator of this condition. Unlike the stable alertness of a dementia patient, the delirious individual may shift from being lethargic to hyper-alertwithin a single shift, reflecting the unstable metabolic state of the cortical neurons.
5.Sensory-perceptual distortions are hallmark signs of acute cortical irritationand toxic encephalopathy. Seeing "bugs" where there are none indicates that the visual processing centersare misfiring or failing to inhibit internal stimuli, a phenomenon frequently associated with the heightened autonomic arousal of the hyperactive subtype.
Rationale for incorrect answers:
3.Difficulty with recent recall is a non-specific findingthat characterizes nearly all forms of cognitive impairment, including both acute confusion and chronic dementia. Because it does not help distinguish between the twoconditions, it is not considered a unique or defining manifestation specifically supporting an acute diagnosis.
4.Persistent and slow intellectual deterioration over several months or years is the defining temporal pattern of chronic dementia. This finding actually contradicts a diagnosisof delirium, which is fundamentally defined by its acute, time-limited, and potentially reversible nature following the resolution of the underlying medical trigger.
Test-taking strategy
- Focus on the elements of the Confusion Assessment Method (CAM).
- Prioritize symptoms that reflect "acuity" and "instability."
- Differentiate between sensory distortions (acute) and long-term decline (chronic).
- Recognize that hallucinations in the elderly often point toward an acute toxic or metabolic cause.
Take Home Points
- Delirium is characterized by an acute onset and a fluctuating clinical course, making serial nursing assessments throughout the day essential.
- Visual and tactile hallucinations in the postoperative period are significant indicators of acute neurotoxicity or withdrawal rather than primary psychiatric illness.
- Cognitive deficits in delirium are primarily driven by an inability to focus attention, whereas dementia is driven by the loss of stored memory.
- The presence of a fluctuating level of consciousness is the most reliable factor in differentiating acute delirium from the stable impairment of dementia.
A nurse is caring for an older adult who suddenly develops acute confusion and fluctuating levels of consciousness. Which neurotransmitter imbalance is most commonly associated with delirium?
Explanation
Deliriumis fundamentally understood through the neurotransmitter hypothesis, which identifies specific chemical imbalances that disrupt cortical integration. The syndrome involves a complex interplay of neuroinflammationand oxidative stress that leads to a global reduction in the brain's ability to maintain synaptic homeostasis, particularly in the ascending reticular activating system.
Rationale for correct answer:
2.A profound deficiency in cholinergic transmissionis the most widely recognized physiological pathway for acute confusion. Acetylcholine is the primary mediator for attention and arousal; therefore, when levels drop due to metabolic stress or anticholinergic drugs, the brain loses its ability to filter stimuli and maintain a stable level of consciousness.1
Rationale for incorrect answers:
1.While an elevation in this specific catecholamine is often observed during the hyperactive variantof the syndrome, it is not the primary universal cause. High levels of this neurotransmitter contribute to psychomotor agitationand hallucinations, but the underlying cognitive failure and inattention are more directly tied to the failure of the parasympathetic signalingsystem.
3.Excess levels of this chemical are typically associated with serotonin syndrome, a specific toxic state characterized by hyperreflexia and autonomic instability.2While this can cause confusion, it is a specific drug-inducedcondition rather than the primary neurochemical mechanism found in the general development of geriatric deliriumduring systemic illness.
4.This neurotransmitter is usually involved in the stress responseand alertness; a decrease is more characteristic of certain types of depression or chronic autonomic failure.3In the acute confusional state, the sympathetic nervous systemis often over-active, leading to an increase rather than a decrease in this chemical, especially during periods of restlessness and tachycardia.
Test-taking strategy
- Identify acetylcholine as the "attention" neurotransmitter.4
- Link anticholinergic side effects directly to the symptoms of confusion.
- Recognize that delirium is most often a deficit of "activation" chemicals.
- Select the option that represents the core neurochemical pillar of the disorder.
Take Home Points
- Acetylcholine deficiency is the primary neurochemical driver of the inattention and cognitive fragmentation seen in delirious patients.
- Many medications commonly prescribed to the elderly possess anticholinergic properties, significantly increasing the risk of acute cognitive failure.5
- Dopamine excess often works in tandem with acetylcholine deficiency to produce the vivid hallucinations and agitation seen in hyperactive states.
- Managing delirium involves not only treating the underlying cause but also minimizing the use of drugs that further deplete the brain's cholinergic reserves.
A client in the ICU has hypoactive delirium. Which behavior would the nurse most likely observe?
Explanation
Hypoactive deliriumis characterized by a global depression of the central nervous system, often resulting from metabolic disturbances or the accumulation of sedating medications. Unlike the more obvious hyperactive form, this subtype involves a decrease in synaptic signalingwithin the brain's arousal centers, leading to a state of pathological passivity.
Rationale for correct answer:
2.The hallmark of the hypoactive subtype is reduced psychomotor activity. The nurse will observe a client who appears "pleasantly confused," stays in bed without movement, and exhibits increased somnolence. Because these patients do not disrupt care, this form of delirium is frequently under-recognized or mistaken for fatigue or depression.
Rationale for incorrect answers:
1.These are the defining features of hyperactive delirium. Agitation is driven by an excess of dopamine and a lack of inhibitory neurotransmitters, which is the physiological opposite of the withdrawn state seen in the hypoactive variant.
3.Rapid, pressured speech and irritability indicate heightened arousaland sympathetic nervous system activation. These symptoms are typical of the hyperactive subtype or a manic episode, rather than the slowed, lethargic processing characteristic of hypoactive states.
4.While fluctuationis a core component of all delirium types, this specific description of "confusion alternating with alert periods" describes the fluctuating courserather than the specific behavior (hypoactivity) the question is asking to identify.
Test-taking strategy
- Associate "Hypo" with "Low" (Low activity, low speech, low energy).
- Remember that hypoactive delirium is the "quiet" type.
- Eliminate any options that describe "active" or "energetic" behaviors (agitation, rapid speech).
Take Home Points
- Hypoactive deliriumhas the highest mortality rate of all delirium subtypes, primarily because it is frequently missed by clinical staff.
- Patients with this condition are at high risk for complications of immobility, such as pressure ulcers and pneumonia.
- Assessment should focus on the level of engagement; a patient who is unusually quiet or difficult to arouse should be screened for delirium using the CAM-ICU tool.
- Nursing care must prioritize frequent stimulation, early mobilization, and checking for underlying causes like hypoxia or metabolic imbalances.
A nurse is reviewing risk factors for delirium in hospitalized older adults. Which factors increase the likelihood of developing delirium? Select all that apply.
Explanation
Deliriumis a multifactorial syndrome that occurs when a patient's cognitive reserveis overwhelmed by physiological stressors. Hospitalized older adults are particularly vulnerable because the acute illness that caused the hospitalization acts as a precipitating factoron top of existing predisposing vulnerabilities.
Rationale for correct answers:
1.Deficits in hearing or vision lead to sensory misperceptionsand a lack of orienting cues. When the brain cannot accurately process environmental data, it is more likely to develop illusions or hallucinations, significantly lowering the threshold for acute confusion.
2.The disruption of the circadian rhythmin a hospital setting leads to profound neurochemical instability. Lack of sleep impairs the brain's ability to clear metabolic waste(via the glymphatic system) and disrupts the balance of neurotransmitters needed for attention and awareness.
3.Polypharmacy increases the risk of drug-drug interactionsand toxicity. Many common hospital medications (such as benzodiazepines, antihistamines, and opioids) have anticholinergic effectsor central nervous system depressant qualities that directly interfere with cholinergic signaling in the brain.
5.A lack of familiar faces and meaningful social interaction causes environmental disengagement. Without "social anchors" to provide reality testing and emotional security, a vulnerable older adult is more likely to experience the psychological withdrawalor agitation characteristic of delirium.
Rationale for incorrect answer:
4.Consistent and normal physiological parameters generally indicate hemodynamic stabilityand adequate cerebral perfusion. While a patient with stable vitals can still develop delirium, this factor is considered a protective signrather than a risk factor, as delirium is more often associated with instability (e.g., hypoxia, hypotension, or fever).
Test-taking strategy
- Think of delirium as a "brain failure" caused by too much stress and too few orienting cues.
- Group "sensory," "sleep," "drugs," and "social" as the "Big Four" environmental risk factors.
- Recognize that anything that interrupts the brain's normal input or chemistry increases the risk.
Take Home Points
- Sensory enhancement(ensuring the patient has their glasses and hearing aids) is one of the most effective non-pharmacological interventions to prevent delirium.
- Sleep hygieneprotocols, such as "quiet at night" and avoiding cluster care during sleep hours, are critical in the acute care setting.
- Medication reconciliationis essential to identify and discontinue "high-risk" medications listed on the Beers Criteria for older adults.
- Family involvement should be encouraged to provide a familiar social environment, which acts as a powerful orienting tool.
A nurse is caring for a hospitalized adult who suddenly becomes acutely confused and disoriented. Which assessment tool is commonly used to detect delirium in hospitalized adults?
Explanation
Deliriumis a medical emergency that requires a rapid and specific screening tool. While many assessments measure general cognitive function, the detection of an acute confusional staterequires an instrument that focuses specifically on attentionand the temporal courseof the symptoms.
Rationale for correct answer:
2.The Confusion Assessment Method (CAM)is the gold standard for bedside delirium screening. It is uniquely designed to identify the syndrome based on four key criteria: (1) Acute onset and fluctuating course, (2) Inattention, (3) Disorganized thinking, and (4) Altered level of consciousness. A diagnosis of delirium requires the presence of both 1 and 2, plus either 3 or 4.
Rationale for incorrect answers:
1.The Mini-Mental State Examination (MMSE)is a general tool used to measure cognitive impairmentand the progression of dementia. While it tracks memory and orientation, it does not specifically assess for the fluctuationor inattentionthat distinguishes delirium from other conditions.
3.This inventory is a self-report scale used to measure the severity of depression. It assesses mood, pessimism, and physical symptoms like fatigue, but it has no diagnostic utility in evaluating acute neurological changesor cognitive disorientation.
4.The Montreal Cognitive Assessment (MoCA)is a screening tool for Mild Cognitive Impairment (MCI)and early-stage dementia. Although more sensitive than the MMSE, it is a static test that does not account for the rapidly changing mental statusfound in a delirious patient.
Test-taking strategy
- Look for the tool that matches the speed of onset(Acute = CAM).
- Remember: Dementia= MMSE/MoCA; Delirium= CAM; Depression= Beck/GDS.
- Identify that "Confusion" is in the name of the correct tool, making it the most specific choice for a "confused" patient.
Take Home Points
- The CAMis highly sensitive and specific, allowing nurses to differentiate delirium from dementia in less than five minutes at the bedside.
- Inattentionis the most critical component of the CAM; if a patient cannot follow a simple command or stay focused on a conversation, they meet a primary criterion for delirium.
- For patients in the ICU who are non-verbal (intubated), nurses use the CAM-ICU, a modified version that uses non-verbal tasks to assess for the same four criteria.
- Positive CAM results should immediately trigger a search for underlying causes, such as urinary tract infections (UTIs), electrolyte imbalances, or medication toxicity.
A nurse is planning non-pharmacological interventions for a client with delirium. Which actions should the nurse include? Select all that apply.
Explanation
Delirium managementprioritizes non-pharmacological interventionsaimed at reducing physiological stress and restoring sensory clarity. Because delirium is a state of cortical fragmentation, nursing care focuses on stabilizing the environment to help the brain re-integrate sensory data and maintain a consistent circadian rhythm.
Rationale for correct answers:
1.Establishing a predictable routinehelps regulate the client's internal clock. By keeping blinds open during the day and dimming lights at night, the nurse supports the natural melatonin-cortisol cycle, which is frequently disrupted in hospitalized older adults, leading to "sundowning" or nighttime agitation.
2.A delirious brain lacks the inhibitory controlto filter out background noise. Excessive stimuli—such as beeping monitors or loud conversations—can be perceived as threatening or overwhelming, triggering catastrophic reactionsor worsening hallucinations. Minimizing noise creates a "low-stimulus" environment that promotes neurological rest.
4.Delirium is often exacerbated by sensory deprivation. If a client cannot see or hear clearly, they are more likely to experience illusions(misinterpreting actual stimuli). Ensuring the use of glasses and hearing aids provides the brain with the accurate data it needs to interpret the environment correctly.
5.Frequent, gentle reorientationacts as a cognitive anchor. Since the client’s short-term memory and attention are impaired, providing consistent cues about their location and the time helps bridge the gaps in their situational awarenessand reduces the fear associated with being in an unfamiliar place.
Rationale for incorrect answer:
3.This is a pharmacological interventionand is not considered a first-line action. Furthermore, administering any potent antipsychotic "without reassessment" is unsafe nursing practice. Haloperidol should only be used when non-pharmacological methods fail and the client poses an imminent safety riskto themselves or others.
Test-taking strategy
- Focus on the phrase "non-pharmacological"—immediately eliminate any mention of medications.
- Choose interventions that "add clarity" (glasses, orientation) and "remove chaos" (noise reduction).
- Remember the "HELP" (Hospital Elder Life Program) protocols, which emphasize sleep, vision, hearing, and orientation.
Take Home Points
- Non-pharmacological interventions are the gold standardfor delirium because they address the root environmental causes without adding the risk of drug side effects.
- Family presenceis a highly effective orienting tool; having a familiar face can often de-escalate agitation more effectively than medication.
- Early mobilization and adequate hydrationare also key non-pharmacological strategies to prevent the worsening of cognitive failure.
- The goal of these interventions is to maximize autonomyand safety while the underlying medical cause of the delirium is being treated.
A client with delirium has been restrained due to risk of injury. Which is the most appropriate nursing action?
Explanation
Restraint usein a delirious client is a high-risk intervention that should only be employed as a last resortwhen all non-pharmacological de-escalation strategies have failed. Because restraints can paradoxically increase agitation, fear, and the risk of injury (such as strangulation or skin breakdown), they must be managed with strict adherence to safety protocols and ethical standards.
Rationale for correct answer:
1.The primary goal is to maintain the least restrictive environmentpossible. Restraints are temporary safety measures, not treatments. As soon as the client's behavior stabilizes, the underlying cause of delirium is addressed, or a sitter/family membercan provide supervision, the restraints must be discontinued to prevent the physical and psychological complications associated with immobilization.
Rationale for incorrect answers:
2.Keeping restraints in place for an entire stay is a violation of Patient Rightsand regulatory standards. Restraint orders must be time-limited and require frequent re-evaluation(often every 4 to 24 hours depending on the facility and age of the patient) to determine if the need still exists.
3.Routine sedation to manage the removal of restraints is inappropriate and can be dangerous. Many sedatives, particularly benzodiazepines, can actually worsen delirium (a "paradoxical reaction") or lead to respiratory depression. The nurse should use reorientationand environmental modification to transition the client away from restraints.
4.All restraint applications require meticulous documentation. This includes the specific behavior that necessitated the restraint, the less-restrictive measuresattempted first, the type of restraint used, the client's response, and the ongoing assessments of circulation, skin integrity, and the continued need for the device.
Test-taking strategy
- Choose the option that emphasizes patient autonomyand the "least restrictive" principle.
- Eliminate any answer that suggests "permanent" or "undocumented" use of restraints.
- Remember that in nursing, "assessment" and "safety" drive the discontinuation of restrictive interventions.
Take Home Points
- Restraints often worsen deliriumbecause they increase the client's sense of being trapped and threatened, leading to higher levels of cortisol and agitation.
- While a client is restrained, the nurse must perform assessments at least every 2 hours(or more frequently per policy), checking for neurovascular status, offering fluids, and providing toileting.
- Alternative strategies, such as bed alarms, low beds with floor mats, or "distraction boxes" (folders to sort, towels to fold), should be prioritized over physical restraints.
- The ultimate "treatment" for delirium is identifying and correcting the underlying medical cause(e.g., hypoxia, infection, or drug toxicity), which naturally leads to the safe removal of restraints.
A nurse is caring for a patient who develops sudden confusion and fluctuating attention during hospitalization. Which laboratory or imaging finding may help identify underlying causes of delirium?
Explanation
Deliriumis frequently the clinical manifestation of a systemic physiological crisis. Unlike dementia, which is characterized by structural changes in the brain, delirium is driven by metabolic and chemical disturbancesthat disrupt the delicate balance of neurotransmitters, particularly in the frontal and parietal lobes.
Rationale for correct answer:
1.Abnormalities in serum levels of sodium, potassium, calcium, or magnesiumare major triggers for acute cognitive failure. For example, hyponatremiacauses cerebral edema, while hypercalcemiainterferes with neuronal membrane stability. These imbalances disrupt electrical conduction and chemical signaling between neurons, leading to the sudden onset of confusion and altered consciousness.
Rationale for incorrect answers:
2.This finding is a hallmark of Alzheimer's diseaseor other forms of chronic dementia. While it indicates a loss of cerebral reserve, it represents a permanent structural change rather than an acute, reversible cause of the sudden mental status changes seen in delirium.
3.Hemoglobin that remains within normal limits indicates adequate oxygen-carrying capacityand a lack of acute hemorrhage. This represents a stable physiological state and would not be a "finding" that explains why a patient has suddenly become delirious; conversely, a lowhemoglobin level (anemia) could be a contributing factor.
4.A normal urine study rules out a urinary tract infection (UTI), which is one of the most common causes of delirium in the elderly. Since the urinalysis is normal, it provides no evidence of a trigger, whereas an abnormalurinalysis (showing nitrites, leukocytes, or bacteria) would help identify the cause.
Test-taking strategy
- Look for an "abnormal" finding that suggests a temporary physiological stressor.
- Distinguish between "acute/metabolic" (Delirium) and "chronic/structural" (Dementia).
- Eliminate "normal" or "stable" findings, as they do not explain a sudden change in patient status.
Take Home Points
- The "workup" for delirium typically includes a Complete Metabolic Panel (CMP), Complete Blood Count (CBC), and Urinalysis (UA) to screen for infection and chemical imbalances.
- Hyponatremiais particularly dangerous in the elderly and can cause a rapid decline in mental status and seizure activity.
- Lab results should be compared to the patient's baselineto determine if the imbalance is new and likely responsible for the acute confusion.
- Nursing assessment must include monitoring for physical signs of electrolyte disturbances, such as muscle weakness, cardiac arrhythmias, or changes in skin turgor.
A nurse is evaluating a client’s delirium management plan. Which interventions are appropriate? Select all that apply.
Explanation
Delirium managementinvolves a holistic, multi-modal approach designed to support the brain's recovery while treating the underlying systemic cause. The goal is to stabilize the neurochemical environmentand provide the client with enough external structure to compensate for their temporary loss of internal cognitive processing.
Rationale for correct answers:
1.Frequent reorientationprovides essential "cognitive anchors." Since delirium involves impaired attention and short-term memory, the nurse must repeatedly ground the client in reality by stating the date, time, and location to reduce the fear and anxiety associated with disorientation.
2.The presence of familiar facesacts as a powerful non-pharmacological stabilizer. Family members provide a sense of security and can help with reality testing, often de-escalating agitation more effectively than clinical staff or chemical sedatives.
4.Many medications prescribed for acute illness (such as opioids or anti-emetics) can exacerbate anticholinergic deficiencyor cause sedation, worsening the delirium. Constant monitoring allows the nurse to identify and advocate for the removal of "deliriogenic" drugs from the client's regimen.
5.Adequate hydration and nutritionare vital for maintaining cellular homeostasis. Dehydration leads to electrolyte shifts and decreased cerebral perfusion, both of which are major triggers for acute confusional states in the vulnerable older adult.
Rationale for incorrect answer:
3.Total immobility is a significant risk factorfor worsening delirium. Unless physically contraindicated (e.g., immediate post-op restrictions), early mobilization is encouraged. Physical activity promotes circulation, improves sleep quality, and prevents complications like pneumonia or pressure ulcers, which could further stress the patient's physiology.
Test-taking strategy
- Choose interventions that promote homeostasis(hydration, meds) and safety(orientation, family).
- Eliminate any options that suggest "complete restriction" or "immobility" unless a specific injury is mentioned.
- Think of the "HELP" (Hospital Elder Life Program) model: Orientation, Early Mobility, Sleep Hygiene, and Sensory Support.
Take Home Points
- The "gold standard" for delirium care is non-pharmacological; drugs like haloperidol are reserved only for cases where the patient's behavior prevents life-saving treatment.
- Early mobilizationshould be a priority; even sitting on the edge of the bed or performing simple range-of-motion exercises can help "clear" the sensorium.
- Nursing documentation should reflect the fluctuating natureof the condition, noting when the patient is most clear and when they are most confused.
- Ensuring the client has their sensory aids(glasses and hearing aids) is one of the most effective ways to promote orientation and prevent hallucinations.
A nurse is assessing a patient who alternates between periods of agitation and restlessness, and times of lethargy and reduced responsiveness. Which type of delirium presents with both hyperactive and hypoactive symptoms?
Explanation
Mixed deliriumis the most common clinical subtype, occurring when a patient’s neurobehavioral state fluctuates between extremes of arousal. This condition reflects an unstable balance of neurotransmitters, where the brain oscillates between a state of dopaminergic excess(agitation) and cholinergic deficiencyor global metabolic depression (lethargy).
Rationale for correct answer:
1.This subtype is specifically defined by a fluctuating presentationwhere the client exhibits both hyperactive behaviors (restlessness, pulling at tubes, hallucinations) and hypoactive behaviors (sluggishness, withdrawal, somnolence). It is common for these patients to be drowsy during the day and become highly agitated at night, a phenomenon often referred to as "sundowning."
Rationale for incorrect answers:
2.This variant is characterized by persistent psychomotor agitation, irritability, and a hyper-alert state. While the client in the scenario has these symptoms, they also experience periods of lethargy, which excludes a "pure" hyperactive diagnosis.
3.This presentation is marked by consistent sedation, slowed speech, and apathy. It lacks the periods of agitation and restlessness described in the assessment, making it an incomplete diagnosis for this specific client.
4.As established in previous assessments, delirium is by definition an acute and reversiblesyndrome. There is no such clinical diagnosis as "chronic delirium"; persistent cognitive impairment over months or years is classified as dementiaor a major neurocognitive disorder.
Test-taking strategy
- Identify the key word "alternates"in the stem, which points directly to a "mixed" or fluctuating state.
- Recognize that "Mixed" is the combination of "Hyper" (high energy) and "Hypo" (low energy).
- Eliminate "Chronic" immediately, as delirium is always an acute condition.
Take Home Points
- Mixed deliriumis particularly challenging to manage because the nursing care must adapt to the patient's rapidly changing needs throughout a single shift.
- Patients with the mixed subtype are at high risk for fallsduring hyperactive phases and pressure ulcersor aspiration during hypoactive phases.
- The presence of a "lucid interval"—where the patient seems temporarily clear—is a common feature of mixed delirium but does not mean the episode has resolved.
- Monitoring should include the use of a standardized scale like the Richmond Agitation-Sedation Scale (RASS)to track the severity of these fluctuations.
A 70-year-old client in the ICU demonstrates confusion, restlessness, and fluctuating alertness. Which complications are associated with untreated delirium? Select all that apply.
Explanation
Deliriumis not merely a temporary state of confusion; it is a form of acute brain failure. When left untreated or unrecognized, the prolonged metabolic stress and neuroinflammation can lead to permanent neuronal damage. This "toxic" environment in the brain significantly increases the risk of secondary physical and psychological injuries.
Rationale for correct answers:
1.Psychomotor agitation, coupled with a lack of situational awareness, creates a high-risk environment for accidents. A delirious client may attempt to climb over bed rails or forget their physical limitations (such as post-surgical weight-bearing restrictions), making fallsand subsequent fractures a frequent and severe complication.
2.Delirium is a major predictor of hospital length of stay. The cognitive impairment often interferes with the patient's ability to participate in physical therapy, follow post-operative instructions, or manage self-care. Furthermore, the complications arising from delirium (like infections or pressure ulcers) necessitate extended medical management.
4.Evidence suggests that an episode of delirium can accelerate the trajectory of permanent cognitive impairment. The neurochemical storm and oxidative stress experienced during delirium can lead to the loss of synaptic connections, potentially unmasking or worsening pre-existing dementia.
Rationale for incorrect answers:
3.Delirium is associated with delayed recoveryand increased morbidity. Because it indicates a systemic failure of the body's homeostatic mechanisms, it serves as a marker for a more complex and difficult clinical course, rather than a fast one.
5.Delirium characteristically involves a profound disruption of the sleep-wake cycle. Rather than improved sleep, patients typically experience "circadian fragmentation," where they may be somnolent during the day and highly agitated or wakeful at night.
Test-taking strategy
- Focus on the word "untreated"—think of the negative "domino effect" on a patient's health.
- Recognize that delirium is a systemic stressor; stressors rarely lead to "improved" or "rapid" positive outcomes.
- Link "confusion" to "safety risks" (falls) and "inflammation" to "brain damage" (cognitive decline).
Take Home Points
- Delirium is an independent predictor of increased mortality; patients who develop delirium in the ICU have significantly higher death rates than those who do not.
- The presence of delirium often marks the beginning of a decline in functional status, leading to a loss of independence and a higher likelihood of discharge to a long-term care facility.
- Early detectionusing tools like the CAM-ICU is the most effective way to prevent these long-term complications.
- Post-hospitalization, many survivors of delirium experience "Post-Intensive Care Syndrome" (PICS), which includes long-term cognitive and psychological deficits.
Exams on Delirium
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
- Objectives
- Introduction
- Definition And Concept Of Delirium
- Clinical Manifestations Of Delirium
- Practice Exercise 1
- Types Of Delirium
- Practice Excercise 2
- Diagnosis Of Delirium
- Practice Exercise 3
- Differential Diagnosis Of Delirium
- Management Of Delirium
- Nursing Management Of Delirium
- Practice Exercise 4
- Complications Of Delirium
- Delirium In Special Populations
- Practice Exercise 5
- Summary
- Comprehensive questions
Notes Highlighting is available once you sign in. Login Here.
Objectives
By the end of this topic, the nursing student should be able to:
- Define delirium and describe its underlying neuropsychiatric mechanisms.
- Discuss the epidemiology and prevalence trends of delirium across different age groups and healthcare settings.
- Identify and analyze the etiological factors, both predisposing and precipitating, that contribute to delirium.
- Explain the neurobiological and pathophysiological processes implicated in the onset and progression of delirium.
- Recognize and describe the key clinical manifestations and subtypes of delirium.
- Differentiate delirium from other psychiatric and neurological disorders.
- Outline diagnostic criteria and assessment tools used to identify delirium.
- Discuss evidence-based management, including both pharmacological and non-pharmacological approaches.
- Formulate comprehensive nursing care plans tailored to patients with delirium.
- Emphasize preventive strategies and patient/family education for delirium management.
Introduction
- Delirium is an acute, fluctuating disturbance in attention, awareness, and cognition, often resulting from an underlying medical condition or substance-induced cause.
- It represents a neuropsychiatric emergency that requires prompt identification and intervention to prevent morbidity and mortality.
- The disorder is transient and reversible, unlike dementia, but can have significant long-term consequences if untreated.
- Delirium commonly occurs in hospitalized and critically ill patients, particularly the elderly, postoperative patients, and those with preexisting brain disorders.
- It affects various cognitive domains including attention, orientation, memory, perception, and psychomotor behavior.
- The hallmark feature is fluctuation in mental status, typically worsening at night (known as “sundowning”).
- Pathophysiologically, delirium involves neurotransmitter imbalances (especially acetylcholine deficiency and dopamine excess), neuroinflammation, and disturbed cerebral metabolism.
- Delirium is often underdiagnosed because symptoms mimic dementia or depression.
- Nurses play a crucial role in early recognition, as they are in continuous contact with patients.
- Early detection prevents complications such as injury, prolonged hospital stay, and poor prognosis.
- Continuous mental status assessments (e.g., using CAM – Confusion Assessment Method) should be part of daily nursing practice.
Definition And Concept Of Delirium
- Delirium is defined as an acute confusional state characterized by disturbances in consciousness, attention, cognition, and perception that develop over a short period (hours to days) and fluctuate during the course of the day.
- It is classified as a neurocognitive disorder according to the DSM-5.
- It reflects transient brain dysfunction caused by reversible physiological disturbances rather than structural brain damage.
- The core feature is inattention, typically accompanied by disorientation, perceptual disturbances (hallucinations or illusions), and memory deficits.
- The condition may present with psychomotor agitation or retardation, depending on the subtype.
- Nurses should understand that delirium is not a psychiatric illness but a manifestation of a medical emergency.
- Rapid onset and fluctuation are diagnostic clues that distinguish delirium from chronic mental disorders.
- Any sudden confusion in a patient should be treated as delirium until proven otherwise.
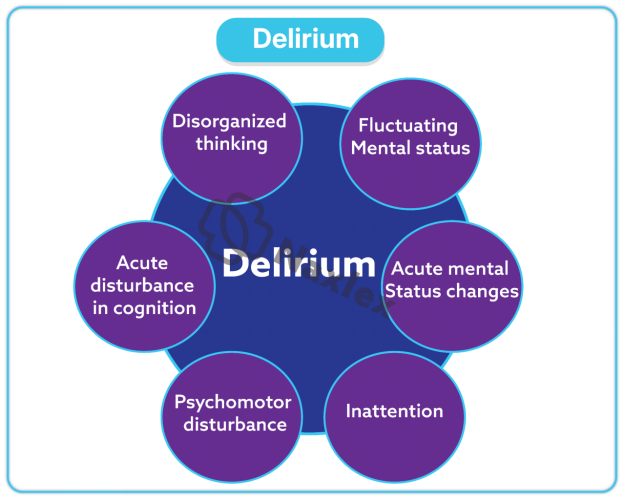
1.1 Overview Of Delirium
- Delirium is a multifactorial syndrome with diverse causes including metabolic derangements, infections, organ failure, drugs, and environmental factors.
- It can occur in medical, surgical, and psychiatric settings.
- The incidence is highest among:
- Elderly (>65 years)
- Postoperative patients (especially after orthopedic or cardiac surgeries)
- ICU patients (mechanically ventilated individuals)
- Patients with dementia, stroke, or chronic illnesses -
Nursing Insights
- Nurses must identify high-risk groups early to implement preventive measures such as orientation protocols, minimizing restraints, and optimizing sensory input (glasses, hearing aids).
1.2 Epidemiology
- The prevalence of delirium in hospitalized elderly patients ranges between 10–30%, increasing to up to 80% in ICU settings.
- In postoperative patients, incidence ranges between 15–50%, depending on surgery type and age.
- Mortality rate for patients with delirium is significantly higher, reaching up to 25–33% within 6 months post-diagnosis.
- Delirium is associated with prolonged hospital stays, functional decline, and increased healthcare costs.
- Recognize that delirium is a predictor of poor outcomes, including institutionalization and mortality.
- Early nursing interventions can reduce duration and severity of delirium.
1.3 Etiology And Risk Factors
Delirium results from the interaction between predisposing and precipitating factors, leading to acute brain dysfunction.
Etiological Factors Include:
- Infections: e.g., urinary tract infections, pneumonia, sepsis.
- Metabolic disorders: e.g., hypoglycemia, hyponatremia, hypoxia.
- Drug-induced: e.g., sedatives, anticholinergics, opioids, corticosteroids, alcohol or substance withdrawal.
- Neurological disorders: e.g., stroke, epilepsy, head injury.
- Organ failure: e.g., hepatic encephalopathy, renal failure.
- Environmental causes: sensory deprivation, ICU environment, sleep deprivation.
- Pain and dehydration: often overlooked triggers.
- Always review medications in patients presenting with confusion. Polypharmacy is a major contributor.
- Nurses should ensure adequate hydration, pain control, and sensory support to reduce risk.
1.4 Pathophysiology Of Delirium
Delirium is caused by disturbances in neurotransmission, cerebral metabolism, and inflammation.
Key Mechanisms Include:
- Neurotransmitter Imbalance:
- ↓ Acetylcholine (primary deficit) → cognitive impairment and attention deficits.
- ↑ Dopamine → agitation, hallucinations.
- Altered serotonin, GABA, and norepinephrine levels. - Neuroinflammation:
- Release of cytokines (IL-1, IL-6, TNF-α) → neuronal dysfunction.
- Blood-brain barrier permeability increases → altered neuronal signaling. - Cerebral Hypoperfusion:
- Reduced cerebral blood flow causes metabolic insufficiency and neuronal stress. - Oxidative Stress:
- Reactive oxygen species damage neuronal structures. -
Nursing Insights
- Nurses must understand the biological underpinnings to appreciate why correcting metabolic and infectious causes reverses delirium.
- Regular monitoring of vital signs, oxygenation, and lab results helps detect reversible causes early.
1.5 Predisposing And Precipitating Factors
1.5.1 Predisposing Factors
- Advanced age (>65 years)
- Pre-existing dementia or cognitive impairment
- Multiple comorbidities (e.g., diabetes, heart failure)
- Sensory impairments (visual, hearing loss)
- Alcoholism or substance dependence
- Previous episodes of delirium
- Malnutrition or dehydration
1.5.2 Precipitating Factors
- Acute medical illness (e.g., infection, sepsis)
- Medications (sedatives, narcotics, anticholinergics)
- Surgery and anesthesia
- Sleep deprivation
- Pain, emotional stress
- Environmental changes or sensory overload
- Hypoxia, electrolyte imbalances, hypoglycemia
Nursing Insights
- Delirium often develops due to synergistic effects of multiple risk factors.
- A nurse’s vigilance in detecting early behavioral or cognitive changes can prevent full-blown episodes.
- Implementing multicomponent prevention protocols (reorientation, hydration, pain control, early mobilization) is essential in at-risk patients.
Clinical Manifestations Of Delirium
Delirium is characterized by a sudden onset of fluctuating disturbances in attention, cognition, and perception. Symptoms typically develop within hours to days and tend to fluctuate throughout the day, often worsening at night (a phenomenon known as “sundowning”).
- The clinical presentation varies depending on the underlying cause, patient’s age, and the type of delirium. The features can be grouped into cognitive, perceptual, psychomotor, and sleep-wake cycle disturbances.
1.1 Cognitive Disturbances
- Disturbance in Attention and Concentration
- The patient is unable to focus, sustain, or shift attention appropriately.
- They are easily distractible, unable to follow conversations or instructions.
- May appear confused and repeatedly ask questions already answered. - Disorientation
- Primarily to time and place, and later to person in severe cases.
- Patients often confuse day and night, or their current environment. - Memory Impairment
- Immediate and short-term memory are affected more than long-term memory.
- Patients may not recall recent events, meals, or medical procedures. - Language Disturbances (Aphasia-like symptoms)
- Speech may be incoherent, illogical, or irrelevant.
- Word-finding difficulty and rambling conversation are common. - Impaired Executive Function
- Difficulty in organizing, planning, or abstract thinking.
- Judgement becomes poor, and decision-making ability declines.
Nursing Insights
- Cognitive impairment is the core feature of delirium and must be continuously monitored.
- Use brief cognitive screening tools such as Mini-Mental State Examination (MMSE) or Confusion Assessment Method (CAM) to assess changes.
- Nurses should communicate clearly, calmly, and repeatedly reorient the patient to place, person, and time.
- Family involvement helps to maintain familiarity and minimize anxiety.
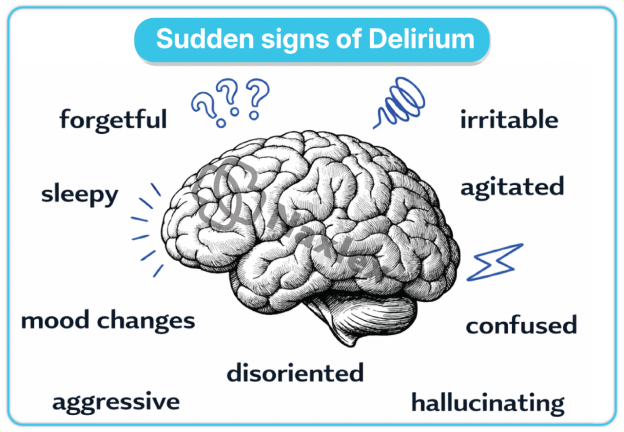
1.2 Perceptual Disturbances
- Illusions
- Misinterpretation of real external stimuli (e.g., mistaking a coat for a person).
- Common during low lighting or at night. - Hallucinations
- False sensory perceptions, most often visual or tactile.
- Patients may see animals, insects, or people who are not present.
- Auditory hallucinations can occur but are less frequent than visual ones. - Delusions
- Fixed false beliefs, usually paranoid or persecutory (e.g., believing staff are plotting harm).
- These beliefs may contribute to agitation and non-cooperation. - Disorganized Thinking
- Tangential, irrelevant, or incoherent thought processes.
- Speech may be rambling, with frequent topic changes. -
Nursing Insights
- Perceptual disturbances increase risk of self-injury or aggression; environmental safety is crucial.
- Ensure adequate lighting and minimize sensory overload.
- Avoid arguing with patients; instead, acknowledge their feelings and redirect attention gently.
1.3 Psychomotor Changes
Delirium may present with increased or decreased psychomotor activity, or a mixture of both.
- Hyperactivity
- Restlessness, agitation, pacing, pulling at IV lines or catheters.
- Increased talkativeness and combativeness. - Hypoactivity
- Lethargy, reduced responsiveness, sluggishness, or apathy.
- The patient may appear quiet but confused or disoriented. - Fluctuating Activity
- Periods of hyperactivity alternating with hypoactivity. - Emotional Disturbances
- Anxiety, fear, irritability, or emotional lability (crying, laughing inappropriately).
- Sudden mood changes without apparent cause.
Nursing Insights
- Psychomotor changes determine type of delirium (hyperactive, hypoactive, or mixed).
- In hypoactive delirium, symptoms are often missed—nurses should actively observe for subtle signs of withdrawal or inattention.
- Ensure patient safety by removing hazardous objects and maintaining calm surroundings.
1.4 Sleep-Wake Cycle Disturbances
- Reversal of Sleep Pattern
- Patients sleep during the day and stay awake or restless at night. - Fragmented Sleep
- Frequent awakenings, difficulty maintaining sleep. - Nocturnal Agitation (“Sundowning”)
- Confusion and agitation intensify at night or in dimly lit settings. - Daytime Drowsiness
- Excessive daytime sleepiness with decreased night-time rest.
Nursing Insights
- Maintain consistent day-night cues (open blinds during the day, dim lights at night).
- Encourage non-pharmacological sleep promotion: relaxation, quiet environment, and minimal interruptions.
- Avoid unnecessary sedatives; they may worsen confusion.
Types Of Delirium
- Delirium can be classified based on psychomotor activity and arousal level into three primary types: hyperactive, hypoactive, and mixed. Each presents distinct clinical and behavioral patterns that influence nursing care and medical management.
1.1 Hyperactive Delirium
- Characterized by increased psychomotor activity and agitation.
- Patients are restless, talkative, aggressive, and easily distracted.
- They may experience hallucinations, delusions, or intense fear.
- Commonly seen in alcohol withdrawal (delirium tremens) and certain drug reactions.
- Associated with higher risk of injury and restraint use.
- Maintain low-stimulus environment and reduce triggers (noise, bright lights).
- Use therapeutic communication; avoid confrontation.
- Provide close supervision and consider sitter support for safety.
- Ensure IV lines, catheters, and tubes are well secured.
1.2 Hypoactive Delirium
- Presents with reduced psychomotor activity, lethargy, and decreased responsiveness.
- Patient may appear quiet, withdrawn, and apathetic, often misdiagnosed as depression.
- Attention and orientation remain impaired, though physical activity is low.
- Common in elderly and critically ill patients.
- Frequently underdiagnosed and associated with poor prognosis.
- Nurses must actively assess mental status in patients who appear unusually quiet.
- Promote stimulation and engagement (e.g., conversation, reorientation, mobilization).
- Monitor for complications such as pressure ulcers, aspiration, or infection due to inactivity.
1.3 Mixed Delirium
- Patients alternate between hyperactive and hypoactive states during the same day.
- Represents the most common and fluctuating type seen clinically.
- Challenging to manage as the patient’s behavior is unpredictable.
- Requires dynamic nursing interventions that adapt to the patient’s current state.
- Continuous assessment and documentation of behavior changes are vital.
- Collaborate with interdisciplinary teams for flexible care plans.
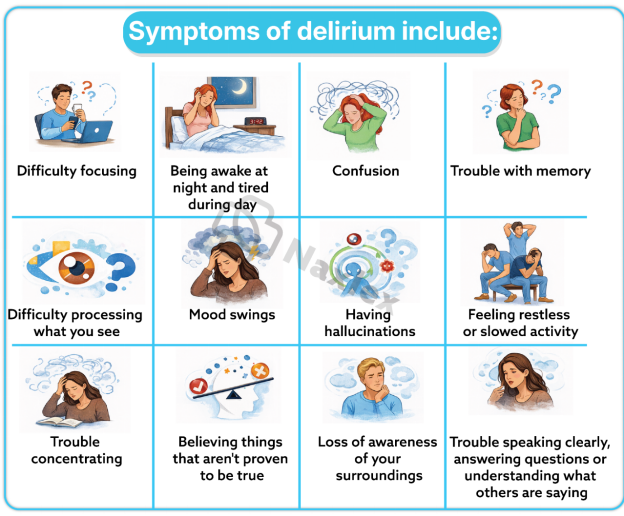
Diagnosis Of Delirium
- The diagnosis of delirium requires a comprehensive clinical assessment that integrates patient history, mental status examination, and supporting laboratory or imaging data. The diagnosis is primarily clinical, based on DSM-5 criteria, supported by validated assessment tools such as the Confusion Assessment Method (CAM).
- Early and accurate identification is essential to initiate prompt treatment and prevent complications.
1.1 Diagnostic Criteria (DSM-5)
According to the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), the diagnostic criteria for delirium are as follows:
A. Disturbance in attention and awareness:
- Reduced ability to direct, focus, sustain, or shift attention.
- Decreased orientation to the environment.
B. Disturbance develops over a short period (usually hours to days) and represents a change from baseline attention and awareness, with symptoms fluctuating during the course of the day.
C. An additional disturbance in cognition (e.g., memory deficit, disorientation, language, visuospatial ability, or perception).
D. The disturbances in criteria A and C are not better explained by another preexisting, established, or evolving neurocognitive disorder (such as dementia) and do not occur in the context of a severely reduced level of arousal (e.g., coma).
**E. There is evidence from the history, physical examination, or laboratory findings that the disturbance is a direct physiological consequence of another medical condition, substance intoxication or withdrawal, exposure to a toxin, or multiple etiologies.
Nursing Insights
- Nurses must recognize that fluctuating attention and acute onset are the hallmark features distinguishing delirium from chronic cognitive disorders.
- Early recognition and reporting are critical, as delirium may be the first sign of an underlying life-threatening medical condition (e.g., sepsis, hypoxia).
- The DSM-5 framework provides a standardized approach that guides both medical and nursing diagnosis in clinical settings.
1.2 Assessment Tools
Assessment tools are designed to standardize detection and monitoring of delirium severity. They complement but do not replace clinical judgment.
1. Confusion Assessment Method (CAM)
- The most widely used bedside tool for delirium assessment.
- Based on four key features:
1. Acute onset and fluctuating course
2. Inattention
3. Disorganized thinking
4. Altered level of consciousness - Diagnosis: Delirium is present when features 1 and 2 are present plus either 3 or 4.
- Simple, quick (takes 5–10 minutes), and can be administered by trained nurses.
2. CAM-ICU (Confusion Assessment Method for Intensive Care Units)
- Adapted for non-verbal or mechanically ventilated ICU patients.
- Assesses acute onset, inattention, altered consciousness, and disorganized thinking.
- Allows delirium monitoring even in sedated or intubated patients.
3. Delirium Rating Scale – Revised-98 (DRS-R-98)
- Rates severity and tracks progression over time.
- Useful in research and detailed clinical evaluation.
4. Nursing Delirium Screening Scale (Nu-DESC)
- A 5-item scale assessing disorientation, inappropriate behavior, inappropriate communication, illusions/hallucinations, and psychomotor retardation.
- Takes <2 minutes to complete.
5. Mini-Mental State Examination (MMSE)
- Evaluates general cognitive function, but less sensitive to delirium detection; best for baseline comparison.
Nursing Insights
- Routine use of CAM or Nu-DESC during every shift allows early detection and documentation.
- The nurse’s role is critical in noticing subtle fluctuations and reporting to the medical team.
- Training in tool application ensures accuracy and reliability in delirium screening programs.
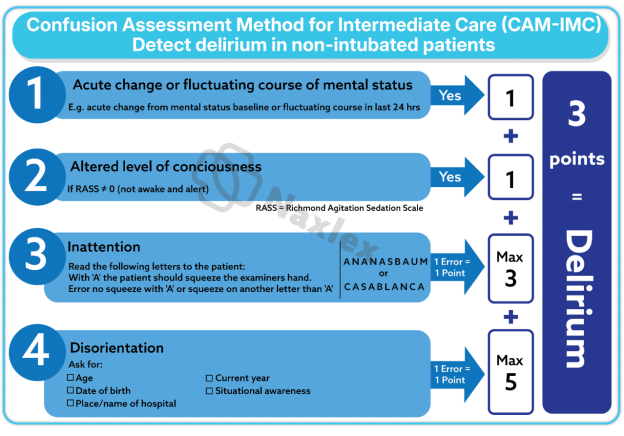
1.3 Laboratory And Imaging Investigations
Investigations aim to identify the underlying cause of delirium. Since delirium is a secondary syndrome, diagnostic workup should be thorough and guided by history and clinical findings.
1. Laboratory Investigations
- Complete Blood Count (CBC): Detects infection, anemia.
- Electrolytes (Na⁺, K⁺, Ca²⁺, Cl⁻): Identify metabolic imbalances.
- Renal and Liver Function Tests: Assess for hepatic encephalopathy or uremia.
- Blood Glucose: Detect hypoglycemia or hyperglycemia.
- Arterial Blood Gas (ABG): Evaluates hypoxia and acid-base imbalances.
- Thyroid Function Tests: Rule out thyroid dysfunction.
- Toxicology Screen: Identifies drug toxicity or withdrawal.
- Urinalysis and Urine Culture: Screens for urinary tract infection.
- Vitamin B₁₂ and Folate Levels: Detect deficiencies causing neuropsychiatric symptoms.
2. Imaging Studies
- CT Scan or MRI Brain: Rule out structural lesions (stroke, tumor, hemorrhage).
- Chest X-ray: Identify pneumonia or pulmonary infections causing hypoxia.
- EEG (Electroencephalogram): Shows generalized slowing in delirium, differentiating it from seizure activity.
3. Other Diagnostic Measures
- Lumbar Puncture: If central nervous system infection (meningitis, encephalitis) is suspected.
- ECG and Echocardiography: Assess cardiovascular causes affecting cerebral perfusion.
-
Nursing Insights
- Nurses assist in specimen collection, monitoring for adverse reactions, and ensuring accurate documentation of results.
- Observation of clinical improvement after correction of abnormalities (e.g., electrolyte replacement, infection treatment) supports the diagnosis of delirium.
- Continuous monitoring of vital signs and neurological status is crucial throughout diagnostic evaluation.
Differential Diagnosis Of Delirium
- Because delirium presents with cognitive and behavioral disturbances, it may mimic other neuropsychiatric disorders. Differentiating it from dementia, depression, and schizophrenia is essential for appropriate management.
1.1 Delirium Vs Dementia
|
Feature |
Delirium |
Dementia |
|
Onset |
Acute (hours to days) |
Gradual (months to years) |
|
Course |
Fluctuating, worse at night |
Progressive, steady decline |
|
Attention |
Markedly impaired |
Generally intact until late stages |
|
Consciousness |
Altered |
Usually clear until late stages |
|
Reversibility |
Often reversible if cause treated |
Irreversible, except some secondary dementias |
|
Perceptual Disturbances |
Common (hallucinations, illusions) |
Rare until advanced stages |
|
Speech |
Incoherent, rambling |
Word-finding difficulty, aphasia |
|
EEG Findings |
Diffuse slowing |
Normal or mild slowing |
|
Associated Medical Conditions |
Common |
May coexist with other chronic diseases |
Nursing Insights
- Any acute cognitive deterioration in a demented patient should be considered superimposed delirium until proven otherwise.
- Nurses should assess for new-onset confusion or attention deficits even in patients with preexisting dementia.
1.2 Delirium Vs Depression
|
Feature |
Delirium |
Depression |
|
Onset |
Acute, fluctuating |
Gradual, over weeks or months |
|
Mood |
Labile, may be irritable or fearful |
Persistently low, hopeless |
|
Cognition |
Disorganized thinking, fluctuating attention |
Pseudodementia (consistent cognitive slowing) |
|
Diurnal Variation |
Worse at night (“sundowning”) |
Worse in the morning |
|
Hallucinations |
Common (especially visual) |
Rare, usually auditory if present |
|
Sleep Pattern |
Fragmented, reversal of sleep cycle |
Early morning awakening |
|
Reversibility |
Rapid improvement after treating cause |
Improves with antidepressants/psychotherapy |
Nursing Insights
- Distinguish between emotional withdrawal in depression and reduced awareness in delirium.
- Screening with both CAM and depression inventories helps differentiate overlapping presentations.
1.3 Delirium Vs Schizophrenia
|
Feature |
Delirium |
Schizophrenia |
|
Onset |
Acute, short duration |
Chronic, insidious |
|
Attention |
Impaired |
Usually intact |
|
Hallucinations |
Predominantly visual or tactile |
Primarily auditory |
|
Orientation |
Disoriented to time/place |
Generally oriented |
|
Memory |
Impaired short-term recall |
Relatively preserved |
|
Course |
Fluctuating |
Chronic and stable |
|
Reversibility |
Reversible with treatment |
Usually persistent, requires long-term therapy |
|
EEG Findings |
Diffuse slowing |
Typically normal |
Nursing Insights
- In delirium, fluctuating consciousness and disorientation are key differentiators.
- Schizophrenia patients maintain attention and awareness despite psychosis.
Nurses should always rule out organic causes before labeling a psychotic episode as schizophrenia.
Management Of Delirium
- The management of delirium is a medical and nursing emergency that requires prompt identification and correction of the underlying cause, supportive care, and environmental modifications.
- Effective management focuses on multidisciplinary collaboration, involving physicians, nurses, pharmacists, and family members. The goals are to:
- Reverse the underlying cause.
- Maintain patient safety and comfort.
- Prevent complications such as injury, aspiration, or chronic cognitive decline.
1.1 General Principles Of Management
The following are the core principles guiding delirium management:
- Identify and Treat Underlying Cause:
- Correct infections, metabolic disturbances, hypoxia, or drug toxicity.
- Discontinue or substitute offending medications (e.g., benzodiazepines, anticholinergics). - Ensure Patient Safety:
- Maintain close supervision to prevent falls, pulling of IV lines, or self-harm.
- Use restraints only as a last resort and with proper documentation. - Optimize Environment:
- Provide adequate lighting and reduce environmental noise.
- Ensure clocks, calendars, and familiar objects are visible to promote orientation. - Provide Supportive Care:
- Maintain hydration, nutrition, and electrolyte balance.
- Manage pain effectively using appropriate analgesia.
- Promote early mobilization and physical activity. - Enhance Communication:
- Speak slowly, calmly, and clearly.
- Use simple, short sentences and repeat information when necessary.
Nursing Insights
- Nurses play a vital role in constant observation and reporting of symptom fluctuations.
- Early recognition of triggers such as pain, hypoxia, or medication side effects can prevent worsening of delirium.
- Encourage family presence to provide reassurance and familiarity.
1.2 Non-Pharmacological Interventions
These are first-line strategies in managing and preventing delirium, focusing on environmental control, patient orientation, and supportive care.
Environmental and Behavioral Measures:
- Maintain a quiet, well-lit, familiar environment.
- Reduce stimuli (e.g., avoid loud alarms, frequent staff changes).
- Provide consistent caregivers to build trust and reduce confusion.
- Place clocks, calendars, and personal belongings within view to maintain orientation.
- Ensure glasses and hearing aids are available and functional.
Orientation and Cognitive Stimulation:
- Reorient the patient regularly to time, place, and person.
- Encourage conversation about familiar people and events.
- Involve family in cognitive engagement (e.g., reminiscence therapy).
Physiological Support:
- Maintain adequate oxygenation, hydration, and nutrition.
- Control pain using non-sedating analgesics.
- Encourage early mobilization and ambulation when safe.
- Promote normal sleep-wake cycle by reducing nighttime disturbances.
Communication and Interaction:
- Approach the patient calmly and respectfully.
- Use reassuring touch and eye contact.
- Avoid confrontation or argument over false beliefs; instead, gently redirect attention.
Safety Measures:
- Keep the bed in low position, with side rails padded.
- Remove unnecessary equipment or wires that may cause injury.
- Provide constant observation (one-on-one nursing care if needed).
Nursing Insights
- Non-pharmacological interventions should be the foundation of delirium care.
- Nurses must prioritize orientation, hydration, and mobility to promote recovery.
- Environmental stability reduces the need for sedative medications and minimizes complications.
1.3 Pharmacological Management
Pharmacotherapy should be used only when non-pharmacological methods fail, or when the patient poses a risk to themselves or others due to agitation or psychosis. The choice of drug depends on the underlying cause, symptom severity, and comorbid conditions.
1. Antipsychotics (First-line for agitation or severe confusion):
- Haloperidol:
- Dose: 0.5–2 mg PO/IM every 4–6 hours as needed.
- Advantages: Minimal anticholinergic and sedative effects.
- Monitor for extrapyramidal symptoms (EPS), QT prolongation, and sedation. - Atypical Antipsychotics: (Used when haloperidol is contraindicated)
- Risperidone (0.5–1 mg PO daily)
- Olanzapine (2.5–5 mg PO daily)
- Quetiapine (25–50 mg PO at night)
- Lower risk of EPS; preferred in elderly patients.
2. Benzodiazepines:
- Indicated only for delirium due to alcohol or sedative withdrawal.
- Lorazepam: 0.5–1 mg PO/IM/IV every 4 hours as needed.
- Avoid in elderly or hepatic impairment due to risk of oversedation and worsening confusion.
3. Other Medications:
- Melatonin or Ramelteon: For regulating sleep-wake cycle.
- Cholinesterase inhibitors (experimental use): Not routinely recommended.
Nursing Insights
- Always evaluate the risk-benefit ratio before administering psychotropics.
- Continuous monitoring for side effects such as hypotension, sedation, or EPS is critical.
- Nurses should document behavioral responses after medication administration to assess effectiveness.
- Pharmacologic restraint must be guided by physician orders and institutional protocols.
1.4 Prevention Of Delirium
Prevention remains the most effective management strategy, especially in high-risk patients (elderly, postoperative, ICU).
Preventive Strategies:
- Early Identification of High-Risk Patients: Screen for cognitive impairment, dehydration, or sensory deficits.
- Medication Review: Avoid polypharmacy and high-risk drugs (e.g., benzodiazepines, anticholinergics).
- Optimize Physiological Stability: Maintain oxygenation, hydration, and electrolyte balance.
- Promote Sleep Hygiene: Encourage uninterrupted nighttime sleep and limit daytime naps.
- Pain and Stress Control: Use appropriate analgesics and relaxation measures.
- Encourage Mobility: Implement early mobilization and physiotherapy programs.
- Provide Environmental Orientation: Clocks, calendars, and consistent caregiver presence.
- Family Involvement: Family members can help reorient and comfort the patient.
Nursing Insights
- Nurses are in a unique position to apply daily preventive interventions.
- Implementing a multicomponent nursing protocol has been proven to reduce incidence and severity of delirium.
- Vigilant monitoring for early warning signs (restlessness, inattention, altered sleep) allows for immediate intervention.
1.5 Prognosis And Complications
Prognosis:
- With early detection and treatment, delirium is reversible in most cases.
- Duration varies from hours to weeks, depending on the underlying cause and patient’s baseline health.
- Persistent delirium is associated with higher mortality and cognitive decline.
Complications:
- Increased Mortality: Especially in elderly and critically ill patients.
- Functional Decline: Loss of independence in activities of daily living (ADLs).
- Prolonged Hospital Stay: Leads to increased healthcare costs.
- Falls and Injuries: Due to disorientation and agitation.
- Pressure Ulcers and Infections: Particularly in hypoactive delirium due to immobility.
- Chronic Cognitive Impairment: Some patients develop long-term deficits similar to dementia.
Nursing Insights
- Nurses must focus on early rehabilitation and prevention of immobility-related complications.
- Continuous follow-up and communication with families regarding prognosis help prepare them for potential outcomes.
Nursing Management Of Delirium
- Nursing management focuses on comprehensive assessment, individualized care planning, and close monitoring to ensure safety and facilitate recovery. It involves physiological, psychological, and environmental care aimed at restoring normal cognition and preventing complications.
1.1 Nursing Assessment
Data Collection:
- History: Onset, duration, fluctuations, medication use, substance abuse, past mental health history.
- Physical Examination: Vital signs, neurological status, hydration, infection signs.
- Mental Status Examination: Orientation, attention span, memory, thought content, perception, mood.
- Environmental Factors: Sensory deprivation, lighting, or noise.
Assessment Tools:
- Use CAM or Nu-DESC for early detection.
- Evaluate risk factors such as age, comorbidities, and drug exposure.
Nursing Insights
- Conduct baseline cognitive assessment on admission for comparison during hospitalization.
- Document changes meticulously to assist in medical decision-making.
1.2 Nursing Diagnoses
Common nursing diagnoses for patients with delirium include:
- Acute confusion related to metabolic imbalance or infection.
- Risk for injury related to disorientation or impaired judgment.
- Disturbed sensory perception (visual/auditory) related to altered mental state.
- Sleep pattern disturbance related to altered circadian rhythm.
- Anxiety related to misinterpretation of environmental stimuli.
- Impaired verbal communication related to disorganized thinking.
1.3 Nursing Interventions And Rationales
|
Nursing Intervention |
Rationale |
|
Maintain safe environment (remove hazards, low bed position) |
Prevents falls and injuries. |
|
Provide frequent reorientation (time, place, person) |
Reinforces reality and reduces confusion. |
|
Maintain consistent caregivers and routines |
Decreases anxiety and enhances familiarity. |
|
Ensure adequate hydration and nutrition |
Corrects physiological imbalances contributing to delirium. |
|
Encourage family participation |
Provides comfort and reassurance. |
|
Promote normal sleep patterns |
Reduces confusion and fatigue. |
|
Monitor vital signs and neurological status |
Detects physiological deterioration early. |
|
Administer medications as prescribed and monitor effects |
Ensures therapeutic response and prevents adverse reactions. |
|
Document behavioral observations |
Provides data for ongoing evaluation and team communication. |
Nursing Insights
- Never argue or challenge delusional statements; use reassurance instead.
- Reorient frequently using clocks, calendars, and familiar faces.
- Recognize subtle signs of hypoactive delirium, as these patients are often overlooked.
1.4 Patient And Family Education
- Educate the patient (when recovered) and family on:
- Causes and risk factors of delirium.
- Importance of medication adherence and hydration.
- Recognizing early warning signs of confusion.
- Need for regular follow-up, especially in elderly or cognitively impaired patients.
- Maintaining a safe, well-lit, calm home environment.
- Families play a key role in delirium prevention and monitoring after discharge.
- Teach caregivers about reorientation strategies, mobility promotion, and sleep hygiene.
1.5 Documentation And Evaluation
- Document:
- Onset, duration, and fluctuation of symptoms.
- Interventions performed and patient’s response.
- Communication with family and multidisciplinary team.
- Progress toward reorientation and cognitive improvement. - Evaluate:
- Resolution of confusion and return to baseline cognition.
- Patient’s ability to maintain safety and perform ADLs.
- Effectiveness of interventions and need for adjustments.
- Accurate documentation ensures continuity of care and legal protection.
Evaluation helps identify residual cognitive deficits needing rehabilitation.
Complications Of Delirium
Delirium is a serious acute neuropsychiatric syndrome with significant short-term and long-term complications that affect physical, cognitive, psychological, and social functioning. Complications can result from the pathophysiological effects of delirium itself, immobility, injuries, or secondary medical problems that occur during or after the episode.
1.1 Physical Complications
- Falls and Fractures:
- Disorientation and psychomotor agitation increase risk of falls.
- May lead to head injuries, hip fractures, or internal bleeding. - Aspiration Pneumonia:
- Altered consciousness and poor coordination of swallowing lead to aspiration during feeding or vomiting. - Pressure Ulcers:
- Immobility and hypoactive states predispose to skin breakdown and pressure sores, especially in elderly patients. - Dehydration and Malnutrition:
- Poor oral intake, confusion, or refusal to eat results in electrolyte imbalance and weight loss. - Incontinence:
- Disorientation leads to inability to recognize toileting needs, resulting in skin irritation and infection. - Nosocomial Infections:
- Due to prolonged hospitalization, use of invasive devices (catheters, IV lines), and decreased immunity.
Nursing Insights
- Nurses should assess mobility and toileting regularly to prevent skin and musculoskeletal complications.
- Maintain adequate hydration and nutritional intake to prevent electrolyte disturbances.
- Implement fall prevention protocols immediately when delirium is diagnosed.
1.2 Psychological Complications
- Post-Delirium Depression:
- Patients may develop reactive depression after regaining awareness of their confusion and hospital experiences. - Anxiety Disorders:
- Delusional or hallucinatory experiences during delirium may cause persistent anxiety, fear, or distrust of caregivers. - Post-Traumatic Stress Disorder (PTSD):
- Especially common in ICU survivors who experienced hallucinations, restraint, or mechanical ventilation during delirium.
- After recovery, assess patients for depressive or anxious symptoms and refer for mental health support.
- Reassure patients that hallucinations or delusions were temporary and due to a medical condition.
1.3 Cognitive Complications
- Persistent Cognitive Impairment:
- Some patients do not fully regain baseline cognition, leading to chronic confusion, attention deficits, or memory impairment. - Increased Risk of Dementia:
- Delirium may accelerate underlying neurodegenerative processes, especially in older adults.
- Nurses should educate families that cognitive recovery can take weeks to months.
- Encourage participation in cognitive rehabilitation activities post-hospitalization.
1.4 Social and Functional Complications
- Loss of Independence:
- Post-delirium weakness and cognitive decline can lead to dependency in activities of daily living (ADLs). - Family Distress:
- Sudden changes in behavior and cognition cause significant caregiver burden and emotional distress. - Institutionalization:
- Persistent deficits may necessitate long-term care placement.
- Engage social workers early to coordinate discharge planning and community support services.
- Provide emotional counseling to family caregivers to reduce burnout.
1.5 Mortality and Long-Term Outcomes
- Delirium is associated with 2–4× increased mortality in hospitalized patients.
- Post-delirium patients have higher 6-month and 1-year mortality rates.
- Contributing factors include comorbidities, infections, immobility, and malnutrition.
- Ongoing follow-up and patient monitoring after discharge are crucial.
- Educate families on early recognition of recurrent confusion or infection symptoms.
Delirium is a serious acute neuropsychiatric syndrome with significant short-term and long-term complications that affect physical, cognitive, psychological, and social functioning. Complications can result from the pathophysiological effects of delirium itself, immobility, injuries, or secondary medical problems that occur during or after the episode.
1.1 Physical Complications
- Falls and Fractures:
- Disorientation and psychomotor agitation increase risk of falls.
- May lead to head injuries, hip fractures, or internal bleeding. - Aspiration Pneumonia:
- Altered consciousness and poor coordination of swallowing lead to aspiration during feeding or vomiting. - Pressure Ulcers:
- Immobility and hypoactive states predispose to skin breakdown and pressure sores, especially in elderly patients. - Dehydration and Malnutrition:
- Poor oral intake, confusion, or refusal to eat results in electrolyte imbalance and weight loss. - Incontinence:
- Disorientation leads to inability to recognize toileting needs, resulting in skin irritation and infection. - Nosocomial Infections:
- Due to prolonged hospitalization, use of invasive devices (catheters, IV lines), and decreased immunity.
Nursing Insights
- Nurses should assess mobility and toileting regularly to prevent skin and musculoskeletal complications.
- Maintain adequate hydration and nutritional intake to prevent electrolyte disturbances.
- Implement fall prevention protocols immediately when delirium is diagnosed.
1.2 Psychological Complications
- Post-Delirium Depression:
- Patients may develop reactive depression after regaining awareness of their confusion and hospital experiences. - Anxiety Disorders:
- Delusional or hallucinatory experiences during delirium may cause persistent anxiety, fear, or distrust of caregivers. - Post-Traumatic Stress Disorder (PTSD):
- Especially common in ICU survivors who experienced hallucinations, restraint, or mechanical ventilation during delirium.
- After recovery, assess patients for depressive or anxious symptoms and refer for mental health support.
- Reassure patients that hallucinations or delusions were temporary and due to a medical condition.
1.3 Cognitive Complications
- Persistent Cognitive Impairment:
- Some patients do not fully regain baseline cognition, leading to chronic confusion, attention deficits, or memory impairment. - Increased Risk of Dementia:
- Delirium may accelerate underlying neurodegenerative processes, especially in older adults.
- Nurses should educate families that cognitive recovery can take weeks to months.
- Encourage participation in cognitive rehabilitation activities post-hospitalization.
1.4 Social and Functional Complications
- Loss of Independence:
- Post-delirium weakness and cognitive decline can lead to dependency in activities of daily living (ADLs). - Family Distress:
- Sudden changes in behavior and cognition cause significant caregiver burden and emotional distress. - Institutionalization:
- Persistent deficits may necessitate long-term care placement.
- Engage social workers early to coordinate discharge planning and community support services.
- Provide emotional counseling to family caregivers to reduce burnout.
1.5 Mortality and Long-Term Outcomes
- Delirium is associated with 2–4× increased mortality in hospitalized patients.
- Post-delirium patients have higher 6-month and 1-year mortality rates.
- Contributing factors include comorbidities, infections, immobility, and malnutrition.
- Ongoing follow-up and patient monitoring after discharge are crucial.
- Educate families on early recognition of recurrent confusion or infection symptoms.
Delirium In Special Populations
- Delirium manifests differently across populations depending on age, comorbidities, and physiological resilience. Understanding these variations aids in early recognition and tailored care strategies.
1.1 Delirium In The Elderly
Elderly individuals are the most susceptible group due to age-related physiological changes and comorbid conditions.
Characteristics:
- Often presents as hypoactive delirium (quiet confusion, lethargy, withdrawal).
- Fluctuating attention, memory impairment, and decreased psychomotor activity are common.
- Frequently mistaken for dementia or depression.
Risk Factors:
- Polypharmacy and use of psychoactive drugs.
- Sensory deficits (hearing or vision impairment).
- Dehydration, infections (especially urinary tract and respiratory).
- Malnutrition and immobility.
- Postoperative stress and anesthesia effects.
Consequences:
- Higher mortality and morbidity rates.
- Increased risk of institutionalization and functional decline.
- Nurses should screen all elderly patients using validated tools such as CAM or Nu-DESC.
- Avoid physical restraints; use reorientation, calm communication, and family presence.
- Monitor hydration, nutrition, and bowel/bladder function vigilantly.
1.2 Delirium In Intensive Care Units (ICU Delirium)
ICU delirium is a common and critical complication of intensive care, occurring in 30–80% of mechanically ventilated patients.
Pathophysiology and Contributing Factors:
- Sedation and mechanical ventilation disrupt sleep-wake cycles.
- Hypoxia, sepsis, and metabolic imbalances alter brain function.
- Use of sedative-hypnotic medications (e.g., midazolam, propofol).
- Sensory deprivation or overload from alarms, bright lights, and isolation.
Clinical Features:
- Agitation, hallucinations, restlessness, or quiet confusion.
- Day-night reversal and disorientation.
- Fluctuating course with lucid intervals.
Management Strategies:
- Implement the ABCDE bundle (Awakening, Breathing coordination, Choice of sedation, Delirium monitoring, Early mobilization).
- Daily sedation interruption and early mobilization.
- Use non-pharmacological methods to promote orientation and sleep hygiene.
- Minimal use of benzodiazepines; prefer dexmedetomidine if sedation is required.
Nursing Insights
- Regularly assess delirium using CAM-ICU or ICDSC.
- Maintain environmental cues (clock, family photos) even in ICU.
- Provide reassurance and explain all procedures to minimize anxiety.
1.3 Delirium In Children
Although less common, delirium in children is frequently underdiagnosed due to developmental differences in behavior and communication.
Etiology:
- Febrile illnesses, infections (meningitis, sepsis), dehydration.
- Drug toxicity or withdrawal (especially anticonvulsants, sedatives).
- Postoperative causes or ICU-related factors.
Clinical Features:
- Irritability, restlessness, and disorientation.
- Incoherent speech, crying, or inconsolability.
- Visual hallucinations (often of animals or monsters).
- Sleep-wake reversal and attention deficits.
Management:
- Identify and treat underlying cause.
- Provide a quiet, well-lit environment with parental presence.
- Use minimal pharmacologic interventions—prefer reassurance and comfort.
- Avoid physical restraint; ensure safety through gentle supervision.
Nursing Insights
- Parental involvement is therapeutic; parents can help reorient and comfort the child.
- Use age-appropriate language and familiar toys to reduce anxiety.
- Monitor vital signs closely to detect worsening systemic illness.
Summary
- Delirium is an acute, fluctuating disturbance in attention, awareness, and cognition, resulting from multiple physiological or environmental causes.
- It presents in hyperactive, hypoactive, or mixed forms, with rapid onset and fluctuating symptoms.
- Pathophysiology involves disturbances in neurotransmitters, inflammation, and cerebral metabolism.
- Clinical features include disorientation, hallucinations, altered psychomotor activity, and sleep disturbance.
- Diagnosis relies on clinical criteria (DSM-5) and tools like CAM, supported by laboratory and imaging investigations.
- Management requires identifying underlying causes, environmental modification, and symptom control.
- Non-pharmacological interventions are first-line, focusing on orientation, hydration, safety, and comfort.
- Pharmacologic management is reserved for agitation or danger to self/others.
- Prevention is key—through risk identification, medication review, and supportive care.
- Nursing management emphasizes assessment, reorientation, safety, family education, and documentation.
- Complications include physical injuries, prolonged hospitalization, cognitive decline, and increased mortality.
- Special populations—elderly, ICU patients, and children—require tailored approaches emphasizing early detection and environmental control.
- Early recognition and multidisciplinary care significantly reduce delirium-related mortality and morbidity.
- Nurses are central in prevention, monitoring, and rehabilitation post-delirium through patient-centered care and environmental stabilization.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Delirium
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


