Please set your exam date
Pediatric anatomy and physiology of the cardiac system, tests of cardiac function, and common cardiac treatments.
Study Questions
Practice Exercise 1
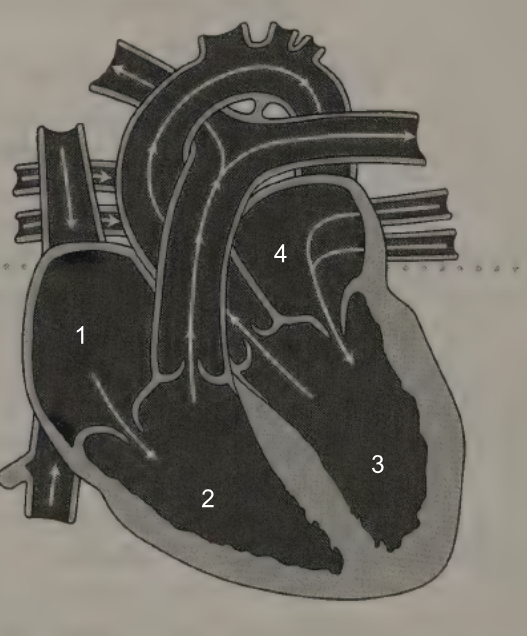
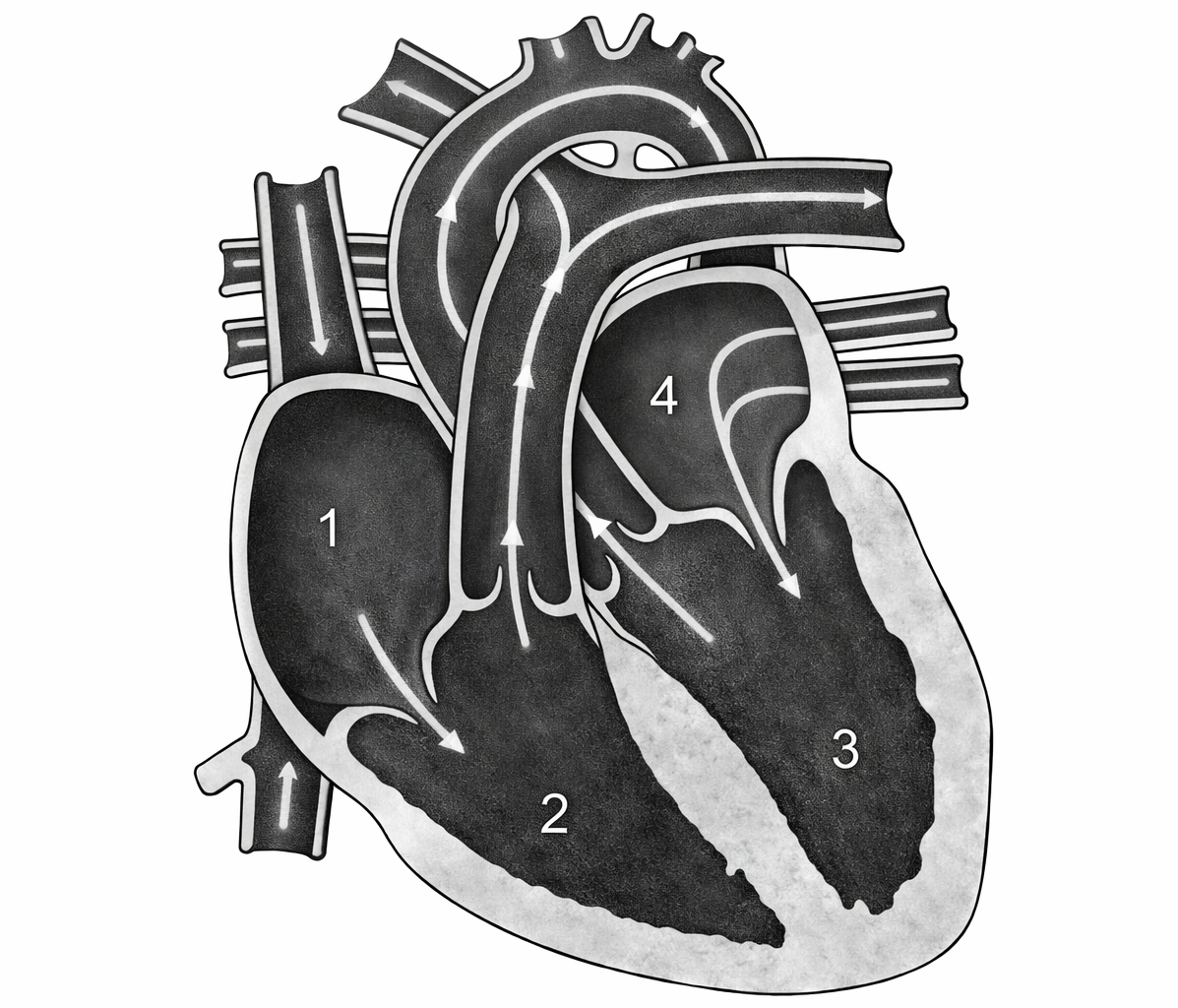
The outpatient cardiac nurse is teaching a class for parents of children with congenital cardiac defects. Before explaining how blood moves through septal defects, the nurse describes pressure gradients in the normal heart. Which chamber should the nurse indicate on this picture of the heart as having the highest pressure?
Explanation
Understanding normal pressure gradients in the heart is essential before explaining septal defects because blood always flows from an area of higher pressure to lower pressure. In a normal heart, pressure differences between chambers determine the direction of blood flow and explain why certain defects cause left-to-right shunting.
Rationale for correct answer:
C. The left ventricle must generate high pressure to pump blood through the systemic circulation. Systemic vascular resistance is much higher than pulmonary resistance, requiring the left ventricle to work harder. Because of this, the left ventricle has the highest pressure of all four chambers. This pressure difference explains why septal defects typically cause left-to-right shunting initially.
Rationale for incorrect answers
A. The right atrium receives blood returning from the body and functions as a low-pressure reservoir. It has the lowest pressure of all four chambers.
B. The right ventricle pumps blood to the lungs, which is a low-pressure system. Although its pressure is higher than the right atrium, it is much lower than the left ventricle.
D. The left atrium receives oxygenated blood from the lungs and has moderate pressure, but it does not generate the force needed for systemic circulation. Its pressure is lower than the left ventricle.
Test-taking strategy
- Ask: Which chamber pumps to the body? This is the left ventricle.
- Remember:
- Pulmonary circulation = low pressure
- Systemic circulation = high pressure
- The chamber responsible for systemic circulation will always have the highest pressure.
Take-home points
- The left ventricle has the highest pressure in the normal heart.
- Pressure gradients explain blood flow direction and shunting patterns in congenital heart defects.
- Septal defects usually cause left-to-right shunting initially because left-sided pressures are higher.
A graduate nurse has started working in a pediatric intensive care unit. The nurse is measuring the client’s cardiac output. To understand cardiac output, the nurse must know that stroke volume is the:
Explanation
Cardiac output (CO) is the total volume of blood the heart pumps per minute and is calculated as: CO=StrokeVolume(SV)×HeartRate(HR). Understanding stroke volume (SV) is essential because it represents the volume of blood ejected by the ventricles with each heartbeat, directly influencing cardiac output.
Rationale for correct answer:
D. Stroke volume is the volume of blood pumped by the left ventricle per beat. Typical pediatric SV depends on age, heart size, preload, afterload, and contractility. SV, along with heart rate, determines cardiac output, which is crucial for maintaining tissue perfusion.
Rationale for incorrect answers:
A. Volume of blood returning to the heart refers to venous return, which affects preload, not stroke volume. Preload is a determinant of SV, but it is not the definition of SV.
B. Ability of the cardiac muscle to act as an efficient pump describes contractility, which influences SV, but is not stroke volume itself.
C. Resistance the ventricles pump against when ejecting blood describes afterload, such as systemic vascular resistance, which affects SV, but is not stroke volume.
Test-taking strategy:
- Remember key cardiovascular definitions:
- Stroke volume is blood ejected per beat.
- Preload is volume of blood in ventricles before contraction.
- Afterload is resistance ventricles overcome to eject blood.
- Contractility is cardiac muscle’s pumping efficiency.
- Identify what is being measured vs what affects it.
Take home points
- Stroke volume is the volume of blood ejected by the ventricles with each contraction.
- Cardiac output = SV × HR, and both determine tissue perfusion.
- Preload, afterload, and contractility are factors influencing SV, not its definition.
- In pediatrics, understanding SV is crucial because children often maintain cardiac output by increasing HR rather than SV.
A nurse is educating a group of nurses on the anatomy of the cardiac system. Which of the following is the function of the Purkinje fibers?
Explanation
The Purkinje fibers are specialized conduction fibers located in the ventricular myocardium. Their main role is to deliver electrical impulses directly to the ventricular muscle cells, ensuring that the ventricles contract efficiently and in a coordinated manner.
Rationale for correct answer:
C. Purkinje fibers carry the action potential from the bundle branches directly into the ventricular myocardium. This allows ventricular muscle cells to depolarize almost simultaneously, producing coordinated, forceful contractions. Proper conduction through Purkinje fibers is essential for effective ejection of blood into the pulmonary artery and aorta.
Rationale for incorrect answers:
A. Delaying impulses to keep ventricles from contracting too quickly is the function of the atrioventricular (AV) node, which slows the conduction to allow ventricular filling.
B. Controlling the heart rate rhythm is primarily the sinoatrial (SA) node, the heart’s natural pacemaker.
D. While Purkinje fibers rapidly transmit impulses, the most precise description of their function is that they conduct impulses into the ventricular muscle, not just “resume rapid conduction.” The Purkinje fibers don’t “resume” conduction; they are the final rapid conduction pathway.
Test-taking strategy:
- Recall the cardiac conduction system sequence:
- SA nde is the pacemaker
- AV nde delays impulse
- Bundle f His conducts to ventricles
- Purkinje fibers cnduct directly into ventricular muscle
- Focus on the specific role of each structure rather than general statements about speed or rhythm.
Take home points
- Purkinje fibers conduct impulses directly into the ventricular myocardium, allowing synchronized contraction.
- AV node delays impulses, SA node sets the rhythm, and bundle branches transmit impulses to Purkinje fibers.
- Understanding conduction helps in interpreting ECG findings and arrhythmias.
A nurse is educating a group of nurses on the anatomy of the cardiac system. Which of the following is the purpose of the foramen ovale?
Explanation
The foramen ovale is a fetal cardiac structure that shunts blood directly from the right atrium to the left atrium, bypassing the nonfunctional fetal lungs. In utero, the lungs are not used for oxygenation since oxygenated blood comes from the placenta, so shunting allows efficient delivery of oxygenated blood to systemic circulation.
Rationale for correct answer:
B. In the fetus, the lungs are collapsed and have high resistance, so blood flow through them is limited. The foramen ovale directly connects the right and left atria, allowing most of the oxygenated blood from the inferior vena cava to flow into the left atrium and then into systemic circulation. This shunting is vital for fetal oxygenation before birth. After birth, when the lungs expand and pulmonary resistance decreases, the foramen ovale normally closes, becoming the fossa ovalis.
Rationale for incorrect answers:
A. Carrying oxygenated blood from placenta to fetus describes the umbilical vein, which brings oxygenated blood from the placenta to the fetus, not the foramen ovale.
C. Carrying deoxygenated blood from fetus to placenta describes the umbilical arteries, which return deoxygenated blood from the fetus to the placenta. The foramen ovale does not carry blood to the placenta.
D. Connecting pulmonary artery to the aorta describes the ductus arteriosus, another fetal shunt that bypasses the lungs by connecting the pulmonary artery to the aorta. The foramen ovale, in contrast, shunts blood atrial-to-atrial, not arterial-to-arterial.
Test-taking strategy:
- Identify fetal shunts:
- Foramen ovale is an atrial shunt
- Ductus arteriosus is an arterial shunt
- Umbilical vein shunts oxygenated blood to fetus
- Umbilical arteries shunt deoxygenated blood to placenta
- Link structure with function in fetal circulation.
Take home points
- The foramen ovale allows right-to-left atrial shunting, bypassing nonfunctional fetal lungs.
- This ensures oxygenated blood reaches systemic circulation efficiently.
- After birth, the foramen ovale closes as the lungs expand and pulmonary circulation becomes functional.
- Understanding fetal shunts is essential for recognizing congenital heart defects if shunts fail to close.
Practice Exercise 2
The nurse auscultates the first heart sound, interpreting this sound as occurring:
Explanation
Heart sounds are produced by valve closure and changes in blood flow within the heart. Correct interpretation of heart sounds requires understanding the cardiac cycle, specifically the relationship between atrial contraction, ventricular contraction, and valve movement.
Rationale for correct answer:
C. S1 is directly caused by AV valve closure. It signifies the beginning of ventricular systole. This sound is best heard at the apex of the heart, where the mitral valve is located. Clinically, S1 coincides with the carotid pulse, ventricular contraction, and rising ventricular pressure.
Rationale for incorrect answers:
A. Late diastole is characterized by atrial contraction and ventricular filling. The AV valves are still open at this time, so no S1 occurs yet.
B. Early diastole begins after ventricular relaxation, when the semilunar valves close (aortic and pulmonic valves), producing S2, not SA.
D. Closure of the aortic and pulmonic (semilunar) valves generates the second heart sound (S2), which marks the end of systole and beginning of diastole.
Test-taking strategy:
- Always match valve type to heart sound:
- AV valves closure (mitral, tricuspid) causes SA.
- Semilunar valves closure (aortic, pulmonic) causes SB.
- Use timing clues:
- Systole begins with S1
- Diastole begins with S2
Take home points
- S1 (“lub”) occurs with closure of the mitral and tricuspid valves and marks the beginning of ventricular systole.
- S1 is best heard at the apex and coincides with the carotid pulse.
- S2 (“dub”) results from semilunar valves closure and marks the start of diastole.
- Understanding heart sounds requires linking valve movement, pressure changes, and the cardiac cycle.
A nurse is performing a physical assessment of a pediatric client. While auscultating the heart, the nurse hears physiological splitting of S2 when the child takes a deep breath. Which action should be taken by the nurse?
Explanation
Physiological splitting of S2 occurs when the aortic (A2) and pulmonic (P2) components of the second heart sound are heard as two distinct sounds during inspiration. This is a normal finding in healthy children and adults, caused by increased venous return during inspiration, which delays closure of the pulmonic valve.
Rationale for correct answer:
D. Document the findings as a normal finding: Physiological splitting is most prominent during deep inspiration and is considered normal, especially in children, adolescents, and young adults. No intervention or provider notification is required unless other abnormal findings are present such as cyanosis, murmurs, or signs of heart failure. Accurate documentation ensures continuity of care and reflects the child’s normal cardiac physiology.
Rationale for incorrect answers:
A. Notify the provider of suspected atrial-septal defect (ASD): ASD can cause fixed splitting of S2, which is present in both inspiration and expiration. Physiological splitting is variable with respiration and does not indicate a septal defect.
B. Notify the provider of suspected pulmonary stenosis: Pulmonary stenosis may produce a loud systolic ejection murmur with fixed splitting, not normal physiological splitting. The described finding does not suggest pathology.
C. Follow institutional policy for initiating an emergency response: This is unnecessary because physiological splitting of S2 is a normal, nonemergent finding.
Test-taking strategy:
- Distinguish physiological vs. pathological splitting:
- Physiological splitting: occurs only with inspiration, varies with respiration, normal in children.
- Pathological splitting: fixed or paradoxical, may indicate ASD, bundle branch block, or pulmonary stenosis.
- If the split changes with breathing and no other abnormalities are present, it is normal.
Take home points
- Physiological splitting of S2 is a normal variation in children and adults during deep inspiration.
- Documenting normal findings is appropriate; no emergency or provider notification is required.
- Fixed or paradoxical splitting, loud murmurs, or other abnormal signs should prompt further evaluation.
- Understanding normal cardiac sounds prevents unnecessary interventions and anxiety.
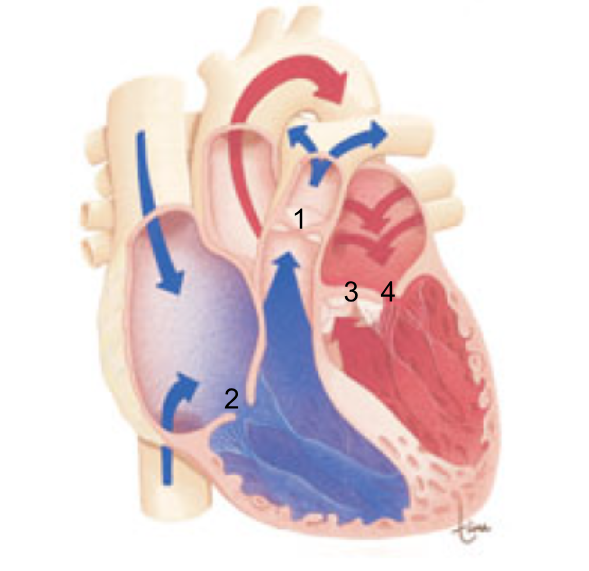
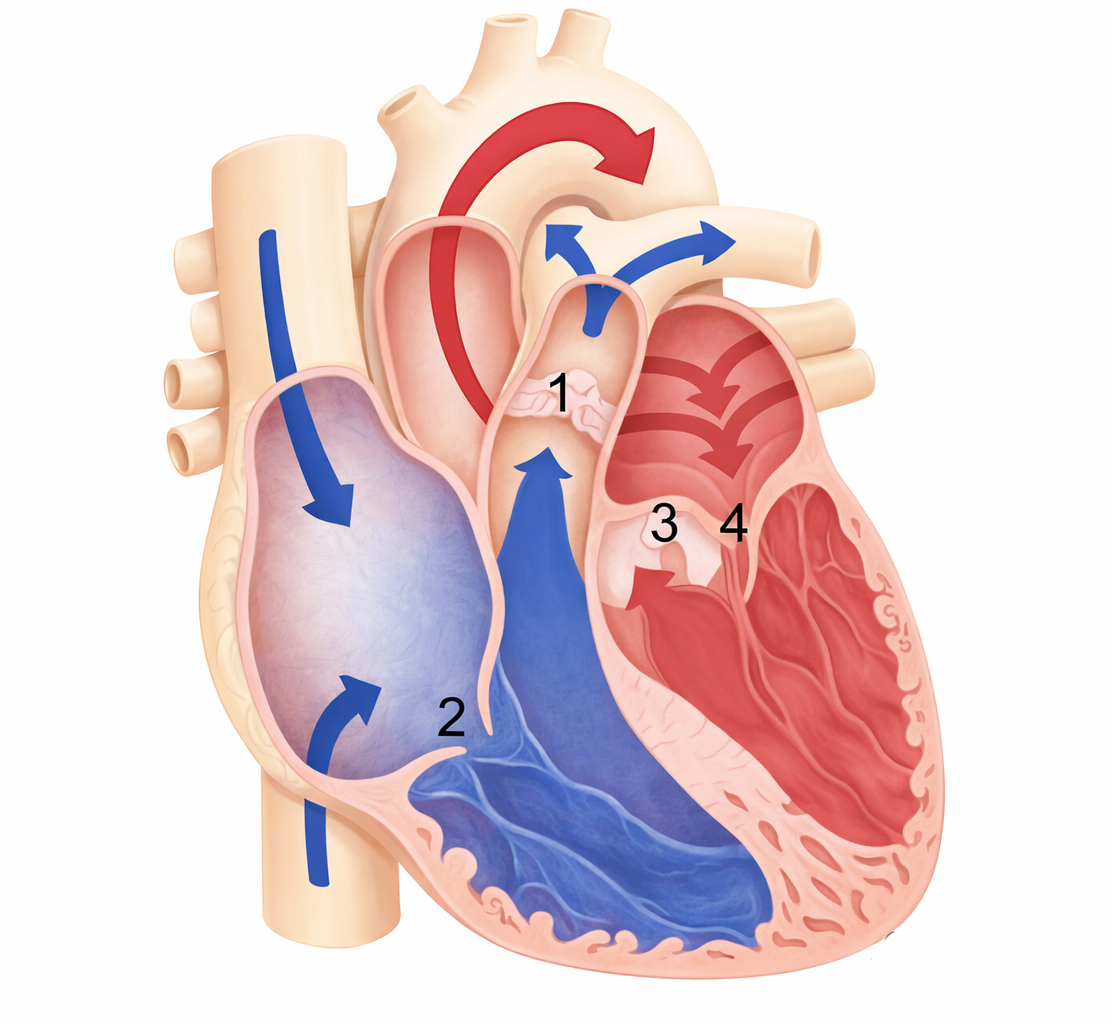
A nurse is using a picture to educate the parents of a child with a congenital murmur about the etiology
of the condition. Which of the following sites demonstrate the location of the tricuspid valve?
Explanation
Heart murmurs often originate from abnormal blood flow across heart valves. To understand murmurs, parents must first understand where each valve is located and what it does. The tricuspid valve is one of the atrioventricular (AV) valves, and its location is key in explaining right-sided heart conditions.
Rationale for correct answer
B. The tricuspid valve is located between the right atrium and the right ventricle. It allows blood to flow from the right atrium into the right ventricle and prevents backflow during ventricular contraction. Murmurs related to the tricuspid valve are typically heard along the left lower sternal border.
Rationale for incorrect answers
A. The pulmonic valve is located between the right ventricle and pulmonary artery. It is a semilunar valve, not an atrioventricular valve.
C. The aortic valve is located between the left ventricle and the aorta. It is also a semilunar valve, associated with systemic outflow.
D. The mitral valve is located between the left atrium and left ventricle. This is the left-sided AV valve, not the tricuspid valve.
Test-taking strategy
- First identify whether the valve is atrioventricular (AV) or semilunar.
- Remember:
- Right side AV valve = Tricuspid
- Left side AV valve = Mitral
- Outflow valves = Aortic and Pulmonic
Take-home points
- The tricuspid valve lies between the right atrium and right ventricle.
- AV valves (tricuspid and mitral) are common sources of murmurs due to regurgitation or stenosis.
- Understanding valve location helps parents grasp the cause and significance of congenital murmurs.
A nurse is performing a cardiac assessment on a child. Which characteristic would indicate a diagnosis of a grade 1 heart murmur?
Explanation
Heart murmurs are extra sounds, like whooshing or swishing, heard during a heartbeat, caused by turbulent blood flow through the heart or its valves. They can be harmless (“innocent”) or signal underlying heart problems such as valve defects or congenital heart disease. Heart murmurs are graded on a scale from 1 to 6 based on their loudness, audibility, and associated physical findings.
Rationale for correct answer:
B. A grade 1 murmur is very faint, requiring focused auscultation. It is softer than the normal S1 and S2 sounds. Often, these murmurs are innocent or functional and not indicative of significant heart disease.
Rationale for incorrect answers:
A. A murmur that is equal to the heart sounds describes a grade 3 murmur, not grade A. Grade 1 is softer, not equal in intensity.
C. This describes grade 6 murmurs which can be heard with the naked ear.
D. A precordial thrill indicates a grade 4 or higher murmur, which is louder and more significant than grade A.
Test-taking strategy:
- Recall the Levine scale for murmur grading:
- Grade 1: Barely audible; softer than the normal heart sounds; heard only with careful auscultation in a quiet room.
- Grade 2: Soft but easily heard immediately.
- Grade 3: Loud murmur, comparable to heart sounds.
- Grade 4: Loud murmur with a palpable thrill.
- Grade 5: Very loud, heard with stethoscope partially off the chest, with thrill.
- Grade 6: Extremely loud, heard with stethoscope off the chest, with thrill.
- Focus on descriptive words like “soft,” “faint,” or “palpable thrill” to differentiate grades.
Take home points
- Grade 1 murmur is very faint, softer than heart sounds, requires careful auscultation.
- Murmur grading helps determine clinical significance and guides further evaluation.
- Thrills and loud murmurs suggest more severe cardiac pathology, while grade 1 murmurs are often innocent in children.
A nurse is performing a cardiac assessment on a 2-year-old. The first heart sound (S1) can best be heard at which location?
Explanation
Cardiac assessment is a systematic evaluation of the heart and circulation that combines history-taking, physical examination, and diagnostic techniques to identify cardiovascular health, risks, or disease. It focuses on vital signs, inspection, palpation, auscultation, and sometimes point-of-care imaging to detect abnormalities in heart function and blood flow.
Rationale for correct answer:
D. Fifth intercostal space, left midclavicular line: The first heart sound (S1) is produced by the closure of the atrioventricular (AV) valves, the mitral and tricuspid valves, at the beginning of ventricular systole. S1 is loudest at the apical area. In clinical testing, the apex is classically identified as the 5th intercostal space at the left midclavicular line, which is considered the standard landmark for auscultating SA. The diaphragm of the stethoscope is preferred because S1 is a high-pitched sound.
Rationale for incorrect answers:
A. Third or fourth intercostal space: These locations are closer to the base of the heart, where S2, the closure of aortic and pulmonic valves is louder than SA.
B. The apex with the stethoscope bell: Using the bell is better for low-pitched sounds, like S3 or S4, not the high-pitched SA.
C. Second intercostal space, midclavicular line: The second intercostal space corresponds to the aortic and pulmonic areas, where S2 is best heard, not SA.
Test-taking strategy:
- For heart sounds, exams often prefer precise anatomical landmarks over general descriptions.
- Remember S1 is caused by AV valve closure (mitral/tricuspid) best heard at the apex of the heart.
- Remember S2 is caused by semilunar valve closure (aortic/pulmonic).
- Use the diaphragm for high-pitched sounds (S1, S2), and bell for low-pitched sounds (S3, S4, murmurs).
Take home points
- S1 results from mitral and tricuspid valve closure and is best at apex (5th ICS, left midclavicular line).
- S2 is caused by aortic and pulmonic valve closure and is best at base (2nd ICS, right and left).
- Correct auscultation location is essential for identifying murmurs, rhythm abnormalities, and cardiac function in children.
Practice Exercise 3
A child returns to his room after a cardiac catheterization. Which nursing intervention is most appropriate?
Explanation
Cardiac catheterization is a medical procedure where a thin, flexible catheter is inserted into a blood vessel, usually in the arm, groin, or neck, and guided to the heart to diagnose or treat cardiovascular conditions. After a cardiac catheterization, the primary nursing concern is preventing bleeding, hematoma, and vascular injury at the catheter insertion site, usually the femoral artery or vein.
Rationale for correct answer:
B. Catheterization punctures the vascular system and the arterial or venous puncture site is at risk for bleeding. Bed rest prevents movement that could dislodge the clot forming at the puncture site. Immobilizing the extremity maintains pressure at the site, reduces risk of hematoma, and allows for safe healing. Typically, bed rest is maintained for 4–8 hours, depending on the child’s age, size, and the type of catheterization.
Rationale for incorrect answers:
A. Maintain the child on bed rest with no further activity restrictions is inaccurate since the affected extremity must be immobilized. Allowing movement could disrupt hemostasis and cause bleeding.
C. Getting out of bed prematurely increases the risk of bleeding and hematoma formation, especially in younger children who may have poor understanding of activity restrictions.
D. Even with the extremity immobilized, sitting upright too soon increases pressure at the femoral site, raising the risk of bleeding. Strict bed rest is preferred in the immediate post-procedure period.
Test-taking strategy:
- Immediately after cardiac catheterization, think bleeding first.
- Remember post-catheterization precautions:
- Bed rest
- Affected extremity immobilized
- Continuous monitoring for bleeding, hematoma, or distal pulses
- Eliminate options that allow premature activity or movement of the affected extremity.
Take home points
- Post-catheterization care focuses on hemostasis and vascular protection.
- Bed rest with immobilization of the affected extremity is standard practice.
- Observe the insertion site for:
- Bleeding
- Bruising or hematoma
- Distal pulses and skin color
- Activity restrictions are gradually lifted based on the child’s age, procedure type, and physician orders.
A child is scheduled for echocardiography. The nurse is providing teaching to the child’s mother. Which statement by the mother about echocardiography indicates the need for further teaching?
Explanation
Echocardiography (also called an echo) is a noninvasive imaging test that uses ultrasound waves to visualize the heart’s structure, function, and blood flow. It is commonly performed in children to assess congenital heart defects, valve function, chamber size, and cardiac output. Understanding which aspects of the procedure require preparation helps the nurse provide accurate parent teaching.
Rationale for correct answer:
C. “How am I going to explain to my son that he can’t have anything to eat before the test?” This statement indicates a misconception about echocardiography. Standard echocardiography does not require fasting, as there is no sedation, anesthesia, or invasive catheterization involved. Fasting is only required for procedures that involve sedation or general anesthesia, like some transesophageal echocardiograms or cardiac catheterizations, not a routine transthoracic echo. If a parent believes fasting is necessary, they may unnecessarily restrict the child’s intake, causing distress or hypoglycemia in young children.
Rationale for incorrect answers:
A. “I’m glad my child won't have an IV catheter inserted for this procedure.” Echocardiography is noninvasive, performed externally with a transducer on the chest. No IV access is required for routine echo, so this reflects accurate understanding.
B. “I’m glad my child won’t need to have dye injected into him before the procedure.” Standard echocardiography uses ultrasound only. No contrast dye or radioactive agents are typically required, except for rare contrast echocardiography, which is specialized and not routine in pediatrics.
D. “I know my child may need to lie on his left side and breathe in and out slowly during the procedure.” Echocardiography often requires the child to assume the left lateral recumbent position, which optimizes visualization of the heart structures, especially the left chambers. The nurse may instruct the child to breathe slowly or hold a breath briefly to improve image quality.
Test-taking strategy:
- Look for misconceptions about preparation or invasiveness of the procedure.
- Key facts about standard transthoracic echocardiography in children:
- Noninvasive
- Usually no IV or contrast dye
- Fasting is not required
- Cooperation for positioning and breathing is necessary
- Statements that conflict with these facts indicate the need for further teaching.
Take home points
- Routine echocardiography is noninvasive and does not require fasting, IV access, or dye injection.
- Parental misconceptions about preparation can lead to unnecessary anxiety or unnecessary restrictions for the child.
- Teaching should emphasize proper positioning (left side), breathing instructions, duration of the procedure, the safe, and the noninvasive nature of the test.
- Correcting misunderstandings ensures parental confidence, child cooperation, and safe preparation.
The nurse has attended a staff education program on diagnostic tests for cardiac conditions. Which evaluation of cardiovascular status is noninvasive?
Explanation
Diagnostic cardiac tests are specialized procedures used to evaluate heart structure, blood flow, and electrical activity. Noninvasive cardiac tests are those that do not require puncturing the skin, inserting catheters, or exposing the patient to significant procedural risk.
Rationale for correct answer:
A. Transthoracic echocardiogram (TTE) is completely noninvasive and painless. A transducer is placed on the child’s chest to generate ultrasound images of the heart. No catheters, IVs, or sedation are needed for standard imaging. It provides real-time information on chamber size, valve function, ejection fraction and cardiac output, and the presence of congenital defects.
Rationale for incorrect answers:
B. Cardiac enzyme levels requires venipuncture to draw blood, making it minimally invasive rather than noninvasive. Enzyme levels (like troponin) provide biochemical evidence of myocardial injury but do not assess cardiac structure or function directly.
C. Cardiac catheterization is an invasive procedure requiring the insertion of a catheter into a vein or artery, usually femoral, to measure pressures, inject contrast dye, and perform angiography. It has a high risk for bleeding, infection, and arrhythmias. It provides detailed hemodynamic data but is not noninvasive.
D. Transesophageal pacing involves placing a pacing electrode into the esophagus to stimulate the heart. Technically minimally invasive because it enters the body and can cause discomfort or complications.
Test-taking strategy:
- Focus on the word “noninvasive” meaning the test cannot break the skin or enter the body internally.
- Ultrasound, external ECG, and imaging scans are usually noninvasive.
- Blood tests are minimally invasive, and catheter-based procedures are invasive.
- Eliminate options that involve catheters, IVs, or internal devices.
Take home points
- Transthoracic echocardiography is noninvasive, safe, and widely used in pediatric cardiology.
- Invasive tests (catheterization, transesophageal pacing) provide detailed data but carry procedural risks.
- Blood tests require puncture, so they are minimally invasive, not fully noninvasive.
- Understanding invasiveness helps prioritize teaching, preparation, and patient safety.
The nurse is teaching the parents of a child who is scheduled for a cardiac catheterization. Which statement by the nurse is the most accurate regarding cardiac catheterization?
Explanation
Cardiac catheterization is an invasive diagnostic and sometimes interventional procedure. It involves inserting a catheter into a vein or artery (commonly the femoral vessel) and advancing it to the heart. Radiopaque dye (contrast medium) is injected to allow visualization of cardiac chambers, valves, and great vessels under fluoroscopy.
Rationale for correct answer:
D. Cardiac catheterization allows assessment of blood flow, pressures, and oxygen saturations in the heart chambers, visualization of structural anomalies, such as septal defects or stenotic valves, and an opportunity for interventions such as balloon dilation and device closure during the same procedure The use of contrast dye is essential for imaging the heart and vessels under X-ray (fluoroscopy).
Rationale for incorrect answers:
A. Cardiac catheterization is invasive, requiring vascular access. There is a risk of bleeding, infection, arrhythmias, and vascular injury.
B. Some children may require sedation or anesthesia depending on age, cooperation, or procedural complexity, but it is not universally required. Older, cooperative children may undergo conscious sedation rather than general anesthesia.
C. The use of high-frequency sound waves to produce an image of the heart in motion describes echocardiography, not cardiac catheterization. Echo is noninvasive and uses ultrasound, whereas catheterization uses fluoroscopy with contrast dye.
Test-taking strategy:
- Identify the key feature of cardiac catheterization which is invasive with catheter insertion and contrast dye.
- Avoid confusion with echocardiography or other noninvasive imaging.
- Look for terms like “visualization with dye” or “vascular access”, which indicate cardiac catheterization.
Take home points
- Cardiac catheterization is invasive and provides detailed anatomical and hemodynamic information.
- Radiopaque dye is used for visualization under fluoroscopy.
- It may allow therapeutic interventions in addition to diagnostic evaluation.
- Parents must understand risks, purpose, and preparation, including possible sedation, fasting, and post-procedure care.
The nurse is preparing a staff education program about cardiac diagnostic tests. What can an electrocardiogram (ECG) detect? Select all that apply
Explanation
An electrocardiogram (ECG or EKG) is a noninvasive test that records the electrical activity of the heart. It provides information about heart rate, rhythm, conduction pathways, and myocardial electrical changes caused by ischemia, injury, or infarction. It does not directly measure hemodynamic parameters such as cardiac output or vascular resistance.
Rationale for correct answers:
A. ECG can detect myocardial ischemia, which shows as ST-segment depression or T-wave inversion. Ischemia represents reduced blood flow to the myocardium without permanent damage.
B. ECG detects myocardial injury, typically indicated by ST-segment elevation, signaling acute damage to cardiac tissue. Helps identify conditions like acute myocardial infarction.
D. ECG is the primary tool for identifying arrhythmias, including atrial fibrillation, ventricular tachycardia, and premature contractions. It provides information about rate, rhythm, and ectopic activity.
J. ECG can detect delays in impulse conduction, such as bundle branch blocks, AV blocks, and prolonged PR or QRS intervals. This reflects problems in the cardiac conduction system.
Rationale for incorrect answers:
C. ECG does not measure cardiac output, which is the volume of blood ejected per minute. Cardiac output is measured via echocardiography, cardiac catheterization, or hemodynamic monitoring.
E. Systemic vascular resistance (SVR) is a hemodynamic parameter related to arterial tone and afterload, not electrical activity. ECG cannot measure vascular resistance. SVR is calculated from mean arterial pressure (MAP), central venous pressure (CVP), and cardiac output (CO).
F. Occlusion pressure refers to blood pressure in vessels during catheterization or vascular testing. ECG cannot directly detect pressure or mechanical obstruction. Pulmonary capillary wedge pressure (PCWP) is measured via a pulmonary artery catheter, not ECG.
Test-taking strategy:
- Determine whether the parameter involves electrical activity or mechanical function.
- ECG detects electrical events, such as ischemia, injury, dysrhythmias, and conduction delays.
- Eliminate options that relate to hemodynamics, pressures, or resistance, which require other diagnostic tools.
Take home points
- ECG is a noninvasive electrical assessment of the heart.
- Detects:
- Ischemia (ST depression, T-wave inversion)
- Injury (ST elevation)
- Dysrhythmias (arrhythmias)
- Conduction delays (blocks, prolonged intervals)
- ECG does not measure cardiac output, systemic vascular resistance, or occlusion pressures—these require hemodynamic or imaging assessments.
A 1-year-old client is scheduled for a cardiac catherization procedure. Which of the following findings might delay the procedure for this client?
Explanation
Cardiac catheterization is an invasive diagnostic and sometimes interventional procedure. It involves inserting a catheter into a vein or artery (commonly the femoral vessel) and advancing it to the heart. Before a cardiac catheterization, the skin at the catheter insertion site (usually the femoral area) must be intact and free from infection or irritation to prevent infection and complications.
Rationale for correct answer:
B. Severe diaper rash: The femoral area is commonly used for catheter insertion, and broken or irritated skin increases infection risk. Cardiac catheterization is an invasive procedure, so any skin compromise at the access site is a contraindication until resolved. Delaying the procedure allows the rash to heal and reduces risk of local or systemic infection.
Rationale for incorrect answers:
A. 30th percentile for weight: Being in the 30th percentile for weight is not a contraindication. Low weight may affect catheter size or medication dosing, but it does not delay the procedure if within safe limits.
C. Allergy to soy: Most contrast agents or medications used in pediatric cardiac catheterization do not contain soy, so this allergy alone is not a reason to delay. Relevant allergies should always be checked, but soy allergy is usually not a procedural contraindication.
D. Oxygen saturation of 91% on room air: Mild hypoxemia is common in children with congenital heart defects, especially those with cyanotic heart disease. This finding does not automatically delay the procedure, though it may require pre-procedural optimization and monitoring.
Test-taking strategy:
- Focus on contraindications to invasive procedures:
- Infection or skin breakdown at the insertion site
- Active illness or unstable condition
- Other findings such as weight percentile, mild hypoxemia, and common allergies may require adjustments but do not usually delay catheterization.
Take home points
- Severe diaper rash or skin infection at the catheter site is a contraindication until resolved.
- Pre-procedural assessment must include skin integrity, infection signs, and allergy checks.
- Mild hypoxemia or low weight usually does not delay the procedure but may require careful monitoring and adjustments.
- Ensuring site sterility is critical to prevent post-procedure infection or sepsis.
A nurse is reviewing the waveforms of an electrocardiogram of an infant with a nursing student. The nurse will tell the student that which waveform indicates ventricular depolarization and contraction?
Explanation
An electrocardiogram (ECG) is a quick, painless test that records the electrical activity of the heart to check its rhythm, rate, and overall function. It helps detect heart problems such as arrhythmias, heart attacks, or structural abnormalities.
Rationale for the correct answer:
C. The QRS complex represents ventricular depolarization, which directly leads to ventricular contraction (systole). This is the most prominent waveform on the ECG because the ventricles have the largest muscle mass.
Rationale for incorrect answers:
A. P wave represents atrial depolarization, which leads to atrial contraction, not ventricular activity.
B. PR interval represents the time it takes for the impulse to travel from the atria through the AV node to the ventricles. It does not represent depolarization or contraction itself.
D. T wave represents ventricular repolarization, which occurs during ventricular relaxation, not contraction.
Test-taking strategy:
- Associate QRS with the ventricles.
- If the question asks about ventricular contraction, always look for QRS complex.
Take home points
- P wave = atrial depolarization
- QRS complex = ventricular depolarization and contraction
- T wave = ventricular repolarization
Practice Exercise 4
A 2-year-old child is being monitored after cardiac surgery. Which sign represents a decrease in cardiac output?
Explanation
Cardiac surgery is any surgical procedure performed on the heart or its major blood vessels to correct structural problems, restore blood flow, or improve heart function. It is often used to treat conditions like coronary artery disease, heart valve disorders, congenital heart defects, or advanced heart failure.
Rationale for the correct answer:
C. Weak peripheral pulses: Cardiac output depends on heart rate and stroke volume. When cardiac output decreases, less blood is ejected into the systemic circulation, resulting in diminished pulse strength, especially in the extremities. Weak pulses are an early and reliable bedside indicator of poor perfusion, particularly important in post–cardiac surgery pediatric patients.
Rationale for incorrect answers:
A. Hypertension: This is not typical of decreased cardiac output. Reduced cardiac output more commonly leads to hypotension, not elevated blood pressure.
B. Increased urine output: Adequate or increased urine output indicates good renal perfusion, which suggests adequate cardiac output, not decreased output.
D. Capillary refill less than 2 seconds: A refill time under 2 seconds indicates normal peripheral perfusion. Decreased cardiac output is associated with delayed capillary refill (>2–3 seconds).
Test-taking strategy:
- Think “poor pump = poor perfusion.”
- Signs of decreased cardiac output include weak pulses, delayed capillary refill, low urine output, hypotension, and altered mental status.
Take home points
- Weak peripheral pulses = decreased cardiac output.
- Good urine output and fast capillary refill indicate adequate perfusion.
- After cardiac surgery, pulse quality is a key priority assessment.
A 3-year-old child is experiencing distress after having cardiac surgery. Which sign indicates cardiac tamponade?
Explanation
Cardiac tamponade is a life-threatening postoperative complication caused by fluid accumulation in the pericardial sac, which compresses the heart and impairs ventricular filling, leading to reduced cardiac output.
Rationale for the correct answer:
B. Muffled heart sounds: In cardiac tamponade, fluid around the heart dampens the transmission of heart sounds, making them sound distant or muffled. This finding strongly suggests pericardial fluid compressing the heart, requiring immediate intervention.
Rationale for incorrect answers:
A. Hypertension: Cardiac tamponade leads to decreased cardiac output, which typically causes hypotension, not hypertension.
C. Widened pulse pressures: Tamponade causes a narrowed pulse pressure due to reduced stroke volume. Widened pulse pressure is more consistent with conditions like patent ductus arteriosus.
D. Increased chest tube drainage: Tamponade is more likely when chest tube drainage decreases or suddenly stops, allowing fluid to accumulate in the pericardial space. Increased drainage is generally a protective sign, indicating fluid is being removed.
Test-taking strategy:
- Think “pressure on the heart = quiet heart.”
- After cardiac surgery, muffled heart sounds + distress should immediately raise concern for cardiac tamponade.
- Remember the Beck’s triad:
- Muffled heart sounds
- Hypotension
- Jugular venous distention (harder to see in young children, but still relevant physiologically)
Take home points
- Muffled heart sounds are a hallmark sign of cardiac tamponade.
- Tamponade results in impaired filling with eventual decreased cardiac output.
- In post–cardiac surgery children, tamponade is a medical emergency requiring rapid recognition and intervention
A nurse is teaching wound care to parents after cardiac surgery. Which statement is most appropriate?
Explanation
Post–cardiac surgery discharge teaching focuses on normal wound healing expectations, infection prevention, and safe home care. Parents should be reassured about findings that are expected and non-dangerous, while being warned about findings that require medical attention.
Rationale for the correct answer:
C. Tingling, itching, and numbness are normal sensations at the wound site commonly occur as nerves heal and regenerate following surgery. Mild itching is also associated with normal tissue repair. Teaching this helps reduce parental anxiety and prevents unnecessary calls or clinic visits. Parents should still be instructed to report increasing pain, redness, swelling, drainage, or fever, which are not normal.
Rationale for incorrect answers:
A. Lotions and powders can trap moisture and bacteria, increasing the risk of infection. Incisions should be kept clean and dry unless otherwise prescribed.
B. Full immersion (baths, swimming) is usually restricted until the incision is well healed. Sponge baths are typically recommended initially to avoid soaking the incision.
D. Sterile adhesive strips (Steri-Strips®) are designed to fall off on their own as healing occurs. Parents should be taught not to pull them off, but falling off naturally does not require notifying the provider.
Test-taking strategy:
- Choose options that normalize expected postoperative findings rather than those that create unnecessary restrictions or anxiety.
- Look for answers that support healing physiology and safe home management.
Take home points
- Mild itching, tingling, and numbness are expected after cardiac surgery.
- Keep incisions clean, dry, and free of lotions or powders.
- Avoid full baths until cleared by the provider.
- Sterile adhesive strips falling off naturally is normal.
A nurse is providing discharge education to the parents of an 8-year-old client post cardiac surgery. Parents ask a nurse about son’s activity level after cardiac surgery. Which response would be best?
Explanation
Post–cardiac surgery care in children focuses on gradual recovery, energy conservation, and prevention of complications. Activity guidance must be realistic, flexible, and developmentally appropriate, rather than overly restrictive or unsafe.
Rationale for the correct answer:
C. Encourage a balance of rest and exercise: After cardiac surgery, children fatigue easily due to healing tissues, altered circulation, and reduced endurance. A balance of rest and activity allows the child to gradually rebuild strength and stamina without overexertion. This guidance supports safe recovery, promotes normal growth and development, and helps parents monitor tolerance (e.g., stopping activity if the child becomes tired, short of breath, or uncomfortable).
Rationale for incorrect answers:
A. There are no exercise limitations: This is unsafe and incorrect. Children typically have temporary activity restrictions following cardiac surgery to protect the sternum, incision, and heart. Overexertion can increase the risk of complications.
B. The child may resume school in 3 days: Return to school is not standardized and depends on the child’s recovery, endurance, and provider recommendations. Most children require more than a few days before resuming full school activities.
D. Climbing and contact sports are restricted for 1 week: Contact sports and climbing are usually restricted for several weeks, not just one. The sternum and surgical site require adequate healing to prevent injury or wound disruption.
Test-taking strategy:
- Avoid answers that are absolute or overly specific when recovery timelines vary.
- Choose responses that emphasize individualized care and gradual progression, which are commonly correct in pediatric postoperative questions.
Take home points
- Children recovering from cardiac surgery need gradual activity progression.
- Fatigue is expected; rest periods are essential.
- High-risk activities (contact sports, climbing) are restricted for weeks, not days.
- Balanced, flexible guidance is safer than rigid timelines.
A nurse is caring for an infant with congestive heart failure on digoxin therapy. Which assessment finding would lead the nurse to suspect a child has a digoxin level greater than 2 ng/ml?
Explanation
Digoxin is a prescription medication from the cardiac glycoside class that strengthens heart contractions and slows the heart rate. It is mainly used to treat heart failure and certain abnormal heart rhythms (arrhythmias), such as atrial fibrillation.
Rationale for the correct answer:
C. Gastrointestinal symptoms are among the earliest and most common signs of digoxin toxicity, even in pediatric clients. A digoxin level greater than 2 ng/mL is considered toxic. In infants, toxicity may present subtly, but poor feeding, nausea, and vomiting are classic early warning signs that require immediate attention and drug withholding until levels are verified.
Rationale for incorrect answers:
A. Weight gain is more consistent with fluid retention from worsening heart failure, not digoxin toxicity.
B. Digoxin toxicity more commonly causes bradycardia and dysrhythmias, not tachycardia.
D. Seizures can occur in severe or advanced toxicity, but they are not an early or typical finding and would indicate a life-threatening progression rather than initial suspicion.
Test-taking strategy:
- With digoxin questions, think “GI first” for early toxicity.
- Choose early, common signs over late, catastrophic ones unless the question specifically asks for severe toxicity.
Take home points
- Digoxin has a narrow therapeutic index.
- GI symptoms (nausea, vomiting, poor feeding) are early indicators of toxicity.
- Bradycardia and dysrhythmias are also concerning signs.
- Always assess apical pulse and clinical symptoms before administering digoxin.
A teenage client with heart failure is prescribed digoxin (Lanoxin) and asks the nurse, “What’s the drug supposed to do?” The nurse teaches the teenager based on the understanding that this drug belongs to which classification?
Explanation
Heart failure is a serious condition where the heart cannot pump blood effectively enough to meet the body’s needs. It does not mean the heart has stopped, but rather that it is weakened or stiff, leading to symptoms such as shortness of breath, fatigue, and swelling in the legs or abdomen.
Rationale for the correct answer:
B. Digoxin is classified as a cardiac glycoside. It works by increasing the force of myocardial contraction (positive inotrope) and slowing the heart rate by enhancing vagal tone. These effects improve cardiac output and circulation in clients with heart failure.
Rationale for incorrect answers:
A. Angiotensin-converting enzyme (ACE) inhibitor such as enalapril and captopril reduce afterload and preload by blocking the renin–angiotensin–aldosterone system. Digoxin does not act on this system.
C. Diuretic such as furosemide reduce fluid overload by increasing urine output. Digoxin does not promote diuresis.
D. Vasodilator decrease vascular resistance to improve forward blood flow. Digoxin’s primary action is increasing contractility, not dilating blood vessels.
Test-taking strategy:
- If the medication is digoxin/Lanoxin, think cardiac glycoside.
- Associate digoxin with increased contractility + slowed heart rate, not fluid removal or blood pressure control.
Take home points
- Digoxin is a cardiac glycoside.
- It improves cardiac output by strengthening contractions.
- It slows heart rate and improves filling time.
- Digoxin requires close monitoring due to a narrow therapeutic range.
Comprehensive Questions
The nurse is preparing a staff education program about echocardiography. Which statement about using an echocardiogram to evaluate cardiac function in a child is the most correct?
Explanation
An echocardiogram is a noninvasive diagnostic test that uses ultrasound (sound waves) to produce images of the heart. It provides information about chamber size, wall motion, valve function, and blood flow, making it an essential tool for assessing pediatric cardiac function.
Rationale for correct answer:
B. Echocardiography works by emitting high-frequency sound waves, which bounce off cardiac structures and return to a transducer to create images. This method is noninvasive, painless, and safe, even for infants and young children. It provides real-time information on chamber size and wall thickness, valve motion and regurgitation, blood flow patterns (with Doppler), and ejection fraction and cardiac output. It is the standard initial tool for evaluating congenital and acquired heart disease in children.
Rationale for incorrect answers:
A. Most echocardiograms do not require sedation. Sedation may only be necessary for very young, uncooperative children who cannot remain still. Saying sedation is always required is inaccurate.
C. Transthoracic echocardiography (TTE) is noninvasive, using only a transducer on the chest wall. Invasive procedures include transesophageal echocardiography or cardiac catheterization, not TTE.
D. While echocardiography is excellent for most evaluations, cardiac catheterization provides more precise hemodynamic data, making it the definitive method in certain complex cases. Therefore, stating echocardiography is the most definitive is overstating its role.
Test-taking strategy:
- Focus on basic principles of the procedure:
- Noninvasive
- Uses sound waves
- Provides structural and functional assessment
- Avoid statements that generalize sedation or invasiveness.
- Remember that “definitive” tests are usually invasive procedures.
Take home points
- Echocardiography is a noninvasive ultrasound technique for evaluating cardiac structures and function.
- Sedation is not routinely required, except in select pediatric patients.
- Transthoracic echocardiography is noninvasive, safe, and widely used in children.
- While excellent for assessment, it is not always the definitive test; invasive procedures may be required for detailed hemodynamic evaluation.
A toddler with a congenital heart defect is scheduled for a cardiac catheterization. Before the procedure, which intervention is most appropriate for a child and his parents?
Explanation
Cardiac catheterization is an invasive procedure that can be stressful for both the child and parents. Preprocedural preparation aims to reduce anxiety, increase cooperation, and improve understanding of what will happen. Providing a guided tour of the hospital and catheterization lab helps familiarize the child and parents with the environment, staff, and equipment.
Rationale for correct answer:
C. Offering a guided tour of the hospital and catheterization laboratory: Familiarization helps reduce fear and anxiety for toddlers and parents. The child can see equipment, hear sounds, and meet staff in a safe, nonthreatening setting, which improves cooperation during the procedure. Parents gain a better understanding of the procedure, which allows them to support and reassure the child effectively.
Rationale for incorrect answers:
A. Supplying a map of the hospital: A map is unlikely to reduce anxiety or help a toddler understand the procedure. It does not provide hands-on exposure or emotional preparation.
B. Limiting visitors to parents only: Restricting visitors may reduce overstimulation, but it does not prepare the child or parents for the procedure itself. Emotional preparation and understanding are more important than visitor restrictions at this stage.
D. Explaining that the child can’t eat or drink for 1 to 2 days postoperatively: This is incorrect and potentially frightening, as fasting for a cardiac catheterization is usually only 4–6 hours pre-procedure, not days. Misstating fasting instructions may cause confusion, unnecessary anxiety, or harm.
Test-taking strategy:
- Focus on preprocedural preparation that reduces anxiety and promotes cooperation.
- Identify interventions that are developmentally appropriate for toddlers:
- Guided tours, play therapy, or age-appropriate explanations
- Eliminate options that are:
- Logistically irrelevant such as a hospital map.
- Overly restrictive such as visitor limitation alone.
- Incorrect medically such as extended fasting.
Take home points
- Guided tours and preparation are essential to reduce stress for pediatric patients and parents before invasive procedures.
- Accurate pre-procedural instructions such as correct fasting time are critical to ensure safety.
- Developmentally appropriate interventions improve child cooperation, parent understanding, and procedural success and safety.
- Avoid overgeneralizing fasting instructions; always use age- and procedure-specific guidelines.
A nurse is caring for a 2-year-old client post cardiac catheterization. Which nursing intervention is most appropriate when caring for the client in the immediate post catheterization phase?
Explanation
Cardiac catheterization is an invasive diagnostic and sometimes interventional procedure. It involves inserting a catheter into a vein or artery (commonly the femoral vessel) and advancing it to the heart. After cardiac catheterization, the primary concern is preventing bleeding, hematoma, and vascular complications at the catheter insertion site, usually the femoral artery or vein.
Rationale for correct answer:
B. Keeping the child flat immediately after the procedure minimizes movement at the puncture site, which prevents dislodging the clot that forms to stop bleeding. Immobility of the affected leg is essential for the first 4–8 hours post-procedure (time may vary by physician order). This intervention directly protects circulation and prevents hemorrhage, the most urgent concern after catheterization.
Rationale for incorrect answers:
A. Elevate the head of the bed 45 degrees increases pressure on the femoral site, potentially promoting bleeding. The child should remain flat until the catheter site is stable.
C. Vital signs should be monitored frequently, often every 15 minutes initially, because early detection of bleeding or shock is critical. Assessing only every 2–4 hours is insufficient for immediate post-procedure care.
D. A bloody dressing is an emergency sign. Replacing it without first assessing and applying direct pressure can worsen bleeding. The correct response is to apply firm pressure and notify the physician, not routine dressing replacement.
Test-taking strategy:
- Immediately post-catheterization, think hemostasis and immobility first.
- Interventions that prevent bleeding and hematoma formation take priority over comfort, routine assessments, or dressing changes.
- ABCs: Circulation (C) is the critical focus in the immediate phase.
Take home points
- After cardiac catheterization, immobilize the affected extremity and keep the child flat to prevent bleeding.
- Monitor vital signs frequently, watching for hypotension, tachycardia, or pallor.
- Do not elevate the head or allow early ambulation until cleared by the physician.
- A bloody dressing is a warning sign; apply direct pressure and intervene immediately rather than simply changing the dressing.
A nurse is providing discharge education to the caregivers of a toddler post-cardiac catheterization. Which home care instruction is included in the teaching?
Explanation
Cardiac catheterization is an invasive diagnostic and sometimes interventional procedure. It involves inserting a catheter into a vein or artery (commonly the femoral vessel) and advancing it to the heart. After a cardiac catheterization, home care focuses on hydration, monitoring the catheter insertion site, preventing complications, and promoting healing.
Rationale for correct answer:
A. Encouraging fluids helps flush contrast dye used during the procedure and prevents dehydration. Returning to a normal diet supports energy needs and healing. This instruction is safe and appropriate for toddlers once awake, alert, and able to tolerate oral intake. It is a standard post-discharge instruction and does not interfere with the catheter site.
Rationale for incorrect answers:
B. Strenuous activity and rough play are restricted for several days (usually 2–5 days) to prevent bleeding or hematoma at the catheter site.
C. Baths or swimming may wet the catheter site too soon, increasing the risk of infection or dislodging the clot. Sponge baths are usually recommended until site healing is confirmed.
D. Activity restrictions and recovery needs usually prevent a full return to school immediately. Children may need 1–2 days at home depending on the provider’s instructions and activity restrictions.
Test-taking strategy:
- Focus on safety and gradual return to normal activities.
- Identify instructions that:
- Promote healing and hydration
- Do not stress the catheter site
- Eliminate options that involve early strenuous activity, bathing, or school attendance, which pose risk for complications.
Take home points
- Hydration and normal diet are safe and encouraged after cardiac catheterization.
- Activity restrictions should be followed to prevent bleeding or hematoma.
- Sponge baths are recommended until the site is fully healed.
- Gradual return to school and play depends on physician instructions and the child’s recovery status.
A pediatric client has had a cardiac catheterization, which intervention would the nurse consider to be of
highest priority during the immediate post-procedure period?
Explanation
Immediately after a cardiac catheterization, the greatest risk is bleeding or hematoma formation at the catheter insertion site, usually the femoral artery or vein. The priority intervention is to maintain hemostasis by applying direct pressure, which prevents blood loss and life-threatening complications.
Rationale for correct answer:
D. Direct pressure promotes clot formation and prevents bleeding. This is especially important for arterial catheterization, where bleeding can be rapid and significant. It is the first action before monitoring, fluid intake, or parent education. It ensures stability of the puncture site during the critical immediate post-procedure period.
Rationale for incorrect answers:
A. Encouraging the intake of small amounts of fluid is important for hydration and flushing contrast dye, but this is not immediately life-saving. Fluid intake can be addressed after hemostasis is ensured.
B. Teaching the parents signs of congestive heart failure is essential, but it is not urgent in the immediate post-procedure period. Teaching can occur once the child is stable.
C. Monitor the site for signs of infection is important but is a long-term concern; it does not address immediate bleeding risk, which is more critical right after catheter removal.
Test-taking strategy:
- Identify immediate, life-threatening risks first.
- After cardiac catheterization, bleeding and vascular compromise are priority over hydration, education, or infection monitoring.
- Apply the ABC principle:
- C (Circulation): Bleeding is a circulation threat requiring first priority.
Take home points
- Direct pressure to the catheter insertion site is the highest priority immediately after cardiac catheterization.
- Ensure hemostasis before allowing movement, fluids, or other interventions.
- Once stable, the nurse can address fluid intake, parent education, and infection monitoring.
- Always prioritize immediate threats to circulation in post-procedure care.
The nurse is caring for a child who has undergone a cardiac catheterization. During recovery, the nurse notices the dressing is saturated with bright red blood. The nurse’s first action is to:
Explanation
Cardiac catheterization is an invasive diagnostic and sometimes interventional procedure. It involves inserting a catheter into a vein or artery (commonly the femoral vessel) and advancing it to the heart. Post-cardiac catheterization, bleeding from the insertion site, usually femoral artery or vein, is a potentially life-threatening emergency.
Rationale for correct answer:
D. Applying direct manual pressure over or just above the insertion site compresses the vessel, stopping blood flow. Bright red blood indicates arterial bleeding, which can lead to rapid blood loss if not controlled immediately. Applying pressure is the first, life-saving intervention, and other actions such as calling the cardiologist and sending the child back to the lab follow after bleeding is controlled.
Rationale for incorrect answers:
A. Calling the interventional cardiologist is important, but delaying direct pressure can worsen bleeding and put the child at risk. Life-saving action must come before notifying the physician.
B. Sending the child back without controlling bleeding is dangerous. This does not address the immediate threat of hemorrhage.
C. Apply a bulky pressure dressing over the present dressing does not provide adequate hemostasis. Manual direct pressure is required first to control active arterial bleeding.
Test-taking strategy:
- Recognize bright red blood post-catheterization as a sign of arterial bleeding and the immediate action is manual pressure.
- Use the ABC principle: Circulation is threatened.
- Life-saving interventions always come before communication or documentation.
Take home points
- Bright red bleeding at catheter site signify arterial hemorrhage and direct pressure should be applied immediately.
- Manual pressure is the priority; only after bleeding is controlled do you:
- Call the cardiologist
- Prepare for potential transfer back to the lab
- Avoid relying solely on dressing reinforcement—it does not stop active bleeding.
- Monitor vital signs, distal pulses, and perfusion continuously during and after hemostasis.
A 10-year-old has undergone a cardiac catheterization. At the end of the procedure, the nurse should first assess:
Explanation
Cardiac catheterization is an invasive diagnostic and sometimes interventional procedure. It involves inserting a catheter into a vein or artery (commonly the femoral vessel) and advancing it to the heart. Immediately after a cardiac catheterization, the most critical assessment focuses on circulation to the extremity used for catheter insertion, usually the femoral artery. Complications such as arterial occlusion, thrombosis, or hematoma can impair distal blood flow.
Rationale for correct answer:
B. Post-procedure, the nurse must assess distal pulses (pedal, posterior tibial, dorsalis pedis) in the affected extremity. A decreased or absent pulse may indicate arterial obstruction, thrombosis, or severe bleeding, which requires immediate intervention. Ensuring adequate perfusion is a priority before other assessments such as pain or labs.
Rationale for incorrect answers:
A. Pain assessment is important but not the first priority. Pain is typically secondary to local trauma or discomfort, and circulatory compromise is more urgent.
C. Monitoring for blood loss is important, but lab tests such as hemoglobin and hematocrit levels
take time to process and do not provide immediate information about vascular compromise.
Assessing distal pulses is faster and directly indicates acute circulation status.
D. Reviewing the catheterization report is useful for planning care but does not address the immediate safety of the patient. Immediate physical assessment of circulation is priority.
Test-taking strategy:
- After invasive procedures, always consider life-threatening complications first:
- Circulation (pulses, bleeding)
- Airway
- Breathing
- Use the ABC principle in conjunction with procedure-specific risks.
- Remember arterial catheterization can compromise distal perfusion, especially in children.
Take home points
- Assess distal pulses immediately after cardiac catheterization to detect vascular compromise.
- Pain, labs, and procedural details are important but secondary.
- Early detection of absent or weak pulses allows for rapid intervention, preventing long-term complications such as limb ischemia.
- Continuous monitoring of the insertion site and extremity perfusion is crucial during the immediate recovery phase.
At 0730 hours, a nurse receives a verbal order for a cardiac catheterization to be completed on a client at
Explanation
Cardiac catheterization is an invasive diagnostic and sometimes interventional procedure. It involves inserting a catheter into a vein or artery (commonly the femoral vessel) and advancing it to the heart. It may require sedation or general anesthesia.
Rationale for correct answer:
A. Clients undergoing cardiac catheterization must fast prior to sedation or anesthesia, typically 4–6 hours for solids, 2 hours for clear liquids. Initiating NPO early ensures safety during the procedure and prevents aspiration. Other tasks, such as teaching or obtaining consent, can occur after NPO status is established.
Rationale for incorrect answers:
B. Patient teaching is important, but teaching after initiating NPO ensures the client’s safety is addressed first. Teaching can be provided later in the pre-procedure period, as long as the client is cognitively able to understand and comply.
C. Starting an intravenous (IV) infusion of 0.9% NaCl may be needed, but it is not the first action. Ensuring the client is NPO before anesthesia or sedation takes priority for airway safety.
D. Obtaining informed consent is mandatory, but this can occur after initiating NPO and before the procedure itself. Safety from aspiration is more urgent than documentation at this point.
Test-taking strategy:
- Consider time-sensitive safety priorities first. Anything that prevents life-threatening complications (aspiration, bleeding, arrhythmia) comes before teaching or documentation.
- Use the ABC principle in conjunction with procedural preparation: airway safety is prioritized.
Take home points
- NPO status is initiated immediately after the order for a cardiac catheterization to prevent aspiration during sedation or anesthesia.
- Teaching, IV access, and consent are important but secondary to safety measures.
- Always verify procedure-specific fasting guidelines based on the client’s age and clinical status.
Question 9 Davis’s Q&A by Kathleen
A new nurse is managing the care of a pediatric client preparing for a cardiac catheterization under
the supervision of an experienced nurse. Which factor identified by the new nurse demonstrates an understanding of the information that can be collected during cardiac catheterization? Select all that apply
Explanation
Cardiac catheterization is an invasive procedure that provides direct access to the heart chambers and great vessels, allowing for measurement of hemodynamic parameters, evaluation of cardiac function, and visualization of structural abnormalities. Some advanced catheterization techniques also allow for estimation of ejection fraction (EF) by measuring ventricular volumes during the procedure.
Rationale for correct answers:
A. Catheterization allows direct sampling of blood from atria, ventricles, and vessels to measure oxygen saturation. It is useful for detecting shunts, cyanotic defects, or oxygen delivery abnormalities.
B. Direct measurement of intracardiac pressures helps diagnose stenosis, regurgitation, or heart failure.
C. Cardiac output (CO) can be calculated using measurements obtained during catheterization, such as the Fick principle or thermodilution.
D. Contrast dye and fluoroscopy allow visualization of structural defects such as septal defects, valve stenosis, or abnormal vessel connections.
F. Ejection fraction (EF) can be estimated during cardiac catheterization by measuring ventricular end-diastolic and end-systolic volumes using contrast ventriculography. This provides information about ventricular systolic function, complementing noninvasive measurements.
Rationale for incorrect answers:
E. Ankle brachial index (ABI) is a noninvasive test comparing blood pressure in the ankle and arm to assess peripheral arterial perfusion. It is not obtained during cardiac catheterization.
Test-taking strategy:
- Identify information that can be obtained invasively from the heart itself.
- Recognize that hemodynamic parameters, structural visualization, and ventricular function estimates can all be measured during catheterization.
- Eliminate peripheral or purely noninvasive measures, such as ABI.
Take home points
- Cardiac catheterization provides direct measurement of oxygen saturation, pressures, cardiac output, anatomic structures, and sometimes ejection fraction.
- Peripheral assessments, like ABI, are not part of the procedure.
- Understanding what can be measured helps in preparing the patient, guiding interventions, and interpreting results.
A nurse is preparing to perform an electrocardiogram (ECG) on several pediatric clients. Which
Explanation
An ECG is a diagnostic tool used to assess electrical activity, heart rate, rhythm, and conduction abnormalities. Children with tachycardia, bradycardia, or an irregular pulse may have underlying arrhythmias or conduction defects, making an ECG helpful.
Rationale for correct answer:
D. An infant with a splitting of the S2 heart sound only when the infant takes a deep breath: Physiological splitting of S2 during inspiration is normal and reflects delayed closure of the pulmonic valve. No arrhythmia or conduction abnormality is suggested; therefore, an ECG would not provide additional clinically useful information. Monitoring and documentation of normal findings are sufficient.
Rationale for incorrect answers:
A. A 4-year-old with tachycardia: Tachycardia can indicate arrhythmia, fever, dehydration, or cardiac pathology. ECG is useful to determine if the tachycardia is sinus or pathologic.
B. A 3-year-old with bradycardia: Bradycardia can indicate heart block or conduction defects. ECG is necessary to evaluate rhythm and conduction intervals.
C. A 10-year-old with an irregular pulse: An irregular pulse suggests arrhythmia or ectopic beats. ECG is essential to identify the type and origin of irregularity.
Test-taking strategy:
- Determine which finding is normal vs. abnormal:
- Normal physiological findings (e.g., S2 splitting on inspiration) do not require ECG.
- Signs of arrhythmia or abnormal heart rate are indications for ECG.
- Ask: “Is there a possible electrical or rhythm problem?” If yes ECG indicated; if no ECG not needed.
Take home points
- ECG is indicated for abnormal heart rates, irregular rhythms, or suspected conduction problems.
- Physiological S2 splitting in children is normal and does not require ECG.
- Accurate assessment prevents unnecessary procedures and anxiety for patients and caregivers.
The nurse is caring for a child after a cardiac catheterization. What is the nursing priority?
Explanation
Cardiac catheterization is an invasive diagnostic and sometimes interventional procedure. It involves inserting a catheter into a vein or artery (commonly the femoral vessel) and advancing it to the heart. After a cardiac catheterization, the greatest risk is vascular compromise due to bleeding, hematoma, or arterial obstruction at the catheter insertion site (usually femoral artery).
Rationale for correct answer:
C. Monitoring distal circulation ensures that the catheter has not caused arterial occlusion or thrombosis. Cool, pale, or cyanotic extremities may indicate compromised blood flow, which is a medical emergency. Early detection allows prompt intervention, preventing permanent tissue damage.
Rationale for incorrect answers:
A. Early ambulation is contraindicated immediately after cardiac catheterization. The affected extremity must remain immobilized for several hours to prevent bleeding or hematoma formation.
B. Pulses above the site are not as clinically relevant as distal pulses. The primary concern is perfusion distal to the puncture site, where ischemia would manifest.
D. Dressing changes are not performed immediately. Manipulating the site could dislodge a clot or introduce infection. Initial assessment is inspection and observation, not dressing removal.
Test-taking strategy:
- Identify post-procedure complications:
- Circulatory compromise is priority hence assessing distal perfusion first.
- Apply the ABC principle with circulation focus:
- Airway/Breathing are stable post-procedure hence circulation takes precedence at the catheter site.
Take home points
- Distal extremity assessment such as temperature, color, and capillary refill is the highest priority nursing action after cardiac catheterization.
- Keep the extremity immobilized and avoid early ambulation or dressing changes initially.
- Early recognition of ischemia or impaired perfusion prevents serious complications such as limb loss or permanent damage.
A nurse is working with a new graduate on the pediatric unit and a patient is returning from the cardiac catheterization laboratory. The nurse feels the graduate understands the important nursing interventions when they say which of the following? Select all that apply
Explanation
Cardiac catheterization is an invasive diagnostic and sometimes interventional procedure. It involves inserting a catheter into a vein or artery (commonly the femoral vessel) and advancing it to the heart. After cardiac catheterization, the primary nursing priority is maintaining hemostasis and monitoring circulation in the extremity used for catheter insertion.
Rationale for correct answers:
A. “Check pulses, especially below the catheterization site, for equality and symmetry.” Distal pulses assess blood flow to the extremity and identify arterial occlusion, thrombosis, or compromised circulation. Immediate recognition allows prompt intervention, preventing tissue ischemia.
D. “Check the dressing for evidence of bleeding or hematoma formation in the femoral or antecubital area.” The insertion site is high-risk for bleeding after the procedure. Observing for hematoma, swelling, or active bleeding ensures early management and prevents further complications.
Rationale for incorrect answers:
B. “Check vital signs, which may be taken as frequently as every 30 to 45 minutes, with special emphasis on the heart rate, which is counted for 1 full minute for evidence of dysrhythmias or bradycardia.” While the parameters to watch that is the HR and rhythm are correct, the frequency is wrong. Post-procedure vitals are typically taken much more frequently, usually every 15 minutes for the first hour, to catch acute changes or bleeding immediately.
C. “Special attention needs to be given to the BP, especially for hypertension, which may indicate hemorrhage or bleeding from the catheterization site.” Hemorrhage or bleeding would cause hypotension (low blood pressure) and tachycardia, not hypertension.
E. “Allow the child to ambulate because this will prevent skin breakdown from lying so long in one place.” Ambulation is contraindicated immediately post-catheterization, as movement of the affected extremity increases risk of bleeding or hematoma. Children must remain on strict bed rest with the affected extremity kept straight for 4 to 8 hours to allow the arterial puncture site to heal and prevent a massive bleed.
Test-taking strategy:
- Focus on immediate, life- or limb-threatening complications:
- Circulatory compromise
- Active bleeding
- Interventions like vital signs, BP monitoring, and ambulation are secondary or may be contraindicated immediately after the procedure.
Take home points
- Checking distal pulses and the dressing site for bleeding are the most critical nursing interventions post-cardiac catheterization.
- Ambulation and routine vital signs are secondary and may be postponed until the extremity is stable.
- Early recognition of vascular compromise or bleeding prevents serious complications such as hematoma expansion, ischemia, or hemorrhagic shock.
A 4-year-old child has just returned to the pediatric floor following a cardiac catheterization. Which of
the following actions should the nurse perform at this time?
Explanation
After a cardiac catheterization, the femoral or antecubital extremity used for catheter insertion is at risk for bleeding, hematoma, and vascular compromise. Keeping the extremity immobilized and straight helps maintain hemostasis at the puncture site and prevents complications during the immediate post-procedure period.
Rationale for correct answer:
C. Keep the child’s affected extremity straight for the next 4 to 6 hours: Immobilization prevents dislodgment of the clot at the insertion site. This reduces the risk of bleeding, hematoma, or arterial injury. The child’s extremity should be monitored while remaining supine and straight, with careful observation for color, temperature, and pulse changes.
Rationale for incorrect answers:
A. Administer oxygen via facemask at 8 to 10 liters per minute: Supplemental oxygen is not routinely required unless the child is hypoxemic. Routine oxygen administration without indication is unnecessary and does not address post-catheterization priorities.
B. Assess the child’s upper extremities for color change every 5 to 10 minutes: The insertion site is usually in the femoral artery or vein, so assessment should focus on the affected lower extremity, not the upper extremities, unless the catheter was inserted in the arm.
D. Continue the infusion of whole blood for another 1 to 2 hours: Blood transfusion is not routinely part of post-catheterization care unless ordered for a separate indication such as anemia or blood loss. Unnecessary transfusions can cause complications.
Test-taking strategy:
- Identify the most immediate post-procedure nursing priority that is immobilization of the affected extremity to prevent bleeding.
- Differentiate between routine monitoring or interventions and critical post-catheterization care.
Take home points
- Post-cardiac catheterization care focuses on maintaining hemostasis:
- Keep the affected extremity straight and immobilized for 4–6 hours.
- Monitor for bleeding, hematoma, distal pulses, color, and temperature.
- Oxygen and transfusions are not routine unless specifically indicated.
- Proper immobilization reduces the risk of post-procedure complications, ensuring safe recovery.
A nurse is providing discharge teaching to the parents of a pediatric client following cardiac surgery. Which information should the nurse include in the discharge teaching? Select all that apply
Explanation
Cardiac surgery refers to any surgical procedure performed on the heart or the blood vessels connected to it. It is used to treat conditions such as blocked arteries, damaged valves, congenital heart defects, or irregular heart rhythms, and can be performed as open-heart surgery or through minimally invasive techniques. After cardiac surgery, comprehensive discharge teaching ensures safe recovery, prevention of complications, and promotion of healing.
Rationale for correct answers:
A. Action and side effects of medications: Parents must understand why medications are prescribed, how to administer them, and potential adverse effects to ensure compliance and recognize complications early.
B. Care of the incision and circumstances in which to contact the health-care provider: Proper incision care prevents infection. Parents should know signs of infection such as redness, swelling, drainage, or fever, and when to seek medical attention.
C. Activity restrictions and follow-up appointments: Children may have temporary limitations on physical activity to protect the sternum and incision. Follow-up visits are essential for monitoring cardiac function and wound healing.
D. Age-appropriate diet with vitamin C to promote wound healing: Nutrition supports recovery and tissue repair, with vitamin C aiding collagen formation and wound healing. A balanced diet helps maintain energy and growth during recovery.
Rationale for incorrect answer:
E. Prevention of pericarditis following dental procedures and prophylactic antibiotic use: Prophylactic antibiotics are generally reserved for certain high-risk congenital heart conditions such as previous infective endocarditis, and prosthetic valves. Routine post-cardiac surgery patients do not require prophylactic antibiotics for dental procedures, so this is not standard discharge teaching unless specifically ordered.
Test-taking strategy:
- Focus on standard post-operative teaching: medications, wound care, activity, nutrition, and follow-up.
- Eliminate items that are specific only to special populations or uncommon scenarios unless clearly indicated.
Take home points
- Discharge teaching should cover:
- Medication management and side effects
- Incision care and infection prevention
- Activity limitations and follow-up schedules
- Nutritional support for healing
- Special interventions (like prophylactic antibiotics for dental procedures) are not routine unless medically indicated.
- Effective teaching empowers parents to recognize complications and support safe recovery at home.
A nurse is suctioning a pediatric client who has just had cardiac surgery. The nurse observes tachypnea, the use of accessory muscles to breathe, and restlessness. Which action should be taken by the nurse?
Explanation
After cardiac surgery, children are at risk for respiratory complications such as atelectasis, pulmonary edema, or airway obstruction. Suctioning is sometimes necessary, but signs such as tachypnea, accessory muscle use, and restlessness indicate respiratory distress.
Rationale for correct answer:
C. Discontinue suctioning, carefully monitor the client, and notify the physician immediately: The child is exhibiting early signs of respiratory distress. Continuing suctioning could worsen hypoxia, increase intrathoracic pressure, and compromise cardiac output. Immediate action allows the healthcare team to intervene quickly and prevent further deterioration.
Rationale for incorrect answers:
A. Continue suctioning, as these are expected during the procedure: Tachypnea, accessory muscle use, and restlessness are not normal responses. Ignoring these signs risks respiratory failure.
B. Continue suctioning, but monitor closely as these could be signs of distress: Continuing suctioning while the child is in obvious distress is unsafe. Suctioning can exacerbate hypoxia and stress on the cardiovascular system, especially post-cardiac surgery.
D. Discontinue suctioning and notify the physician to insert a chest tube: There is no evidence that a chest tube is immediately indicated. The priority is assessing and stabilizing the airway, not preemptively inserting a chest tube.
Test-taking strategy:
- Recognize signs of respiratory distress in post-operative pediatric clients:
- Tachypnea, accessory muscle use, restlessness, nasal flaring, grunting.
- Stop any intervention that worsens distress and call for immediate assistance.
- Remember airway and breathing take priority in post-operative cardiac care.
Take home points
- Tachypnea, accessory muscle use, and restlessness after cardiac surgery indicate respiratory compromise.
- The nurse should discontinue sutioning immediately, monitor the client, and notify the physician.
- Continuing interventions that exacerbate distress can lead to hypoxia, decreased cardiac output, and potential cardiopulmonary arrest.
- Early recognition and intervention are critical for safety in post-cardiac surgery pediatric patients.
Exams on Pediatric anatomy and physiology of the cardiac system, tests of cardiac function, and common cardiac treatments.
Custom Exams
Login to Create a Quiz
Click here to loginLessons
 Naxlex
Just Now
Naxlex
Just Now
Notes Highlighting is available once you sign in. Login Here.
Objectives
- Understand the cardiac structure and function.
- Analyze the anatomical transition from fetal circulation to neonatal circulation and the triggers for shunt closure.
- Perform a comprehensive pediatric cardiac assessment, including grading murmurs and identifying heart sounds.
- Evaluate the hemodynamic pressures of each heart chamber and how they dictate blood flow directionality.
- Master the clinical assessment of the pediatric heart, including heart sound locations and murmur grading.
- Formulate nursing care plans for invasive procedures like cardiac catheterization and cardiac surgery.
- Synthesize pharmacological knowledge to safely administer high-alert cardiac medications in the pediatric population.
Introduction
- The pediatric cardiovascular system is responsible for delivering oxygen and nutrients to tissues while removing metabolic waste products.
- Unlike the adult heart, the pediatric heart is often more sensitive to volume and pressure changes, and its output is highly dependent on heart rate rather than stroke volume.
- Pediatric cardiac assessment is a multi-dimensional process used to evaluate the efficiency of the heart and circulatory system.
- It involves gathering a focused health history and performing a systematic physical examination. In pediatrics, this assessment must be tailored to the child's age, as clinical signs of heart disease in a neonate (such as poor feeding or diaphoresis) differ significantly from those in an adolescent (such as chest pain or syncope).
- In the pediatric population, cardiac diagnostics are essential for identifying structural defects, assessing electrical function, and monitoring the effectiveness of surgical or medical interventions.
- Nurses play a critical role in preparing the child and family for these procedures, ensuring safety, and providing post-procedural care.
- Pediatric cardiac surgery encompasses a wide range of procedures designed to repair or palliated congenital and acquired heart defects. While surgical techniques have advanced significantly, the perioperative nursing care remains a critical determinant of long-term patient outcomes.
Cardiac structure and function
Anatomy of the Heart
The heart is a muscular pump divided into four distinct chambers, each with specific pressure gradients to ensure one-way blood flow.
- Right atrium: Receives deoxygenated blood from the body via the superior and inferior vena cava. It maintains a low pressure, typically ranging from 2-6 mmHg.
- Right ventricle: Receives blood from the right atrium and pumps it to the lungs. Its systolic pressure is lower than the left side, usually 15–25 mmHg.
- Left atrium: Receives oxygenated blood from the pulmonary veins. Its pressure is slightly higher than the right atrium, typically 5-10 mmHg.
- Left ventricle: The most muscular chamber, responsible for pumping oxygenated blood to the entire body. It maintains high systemic pressures, typically 60–100 mmHg in infants, increasing with age.
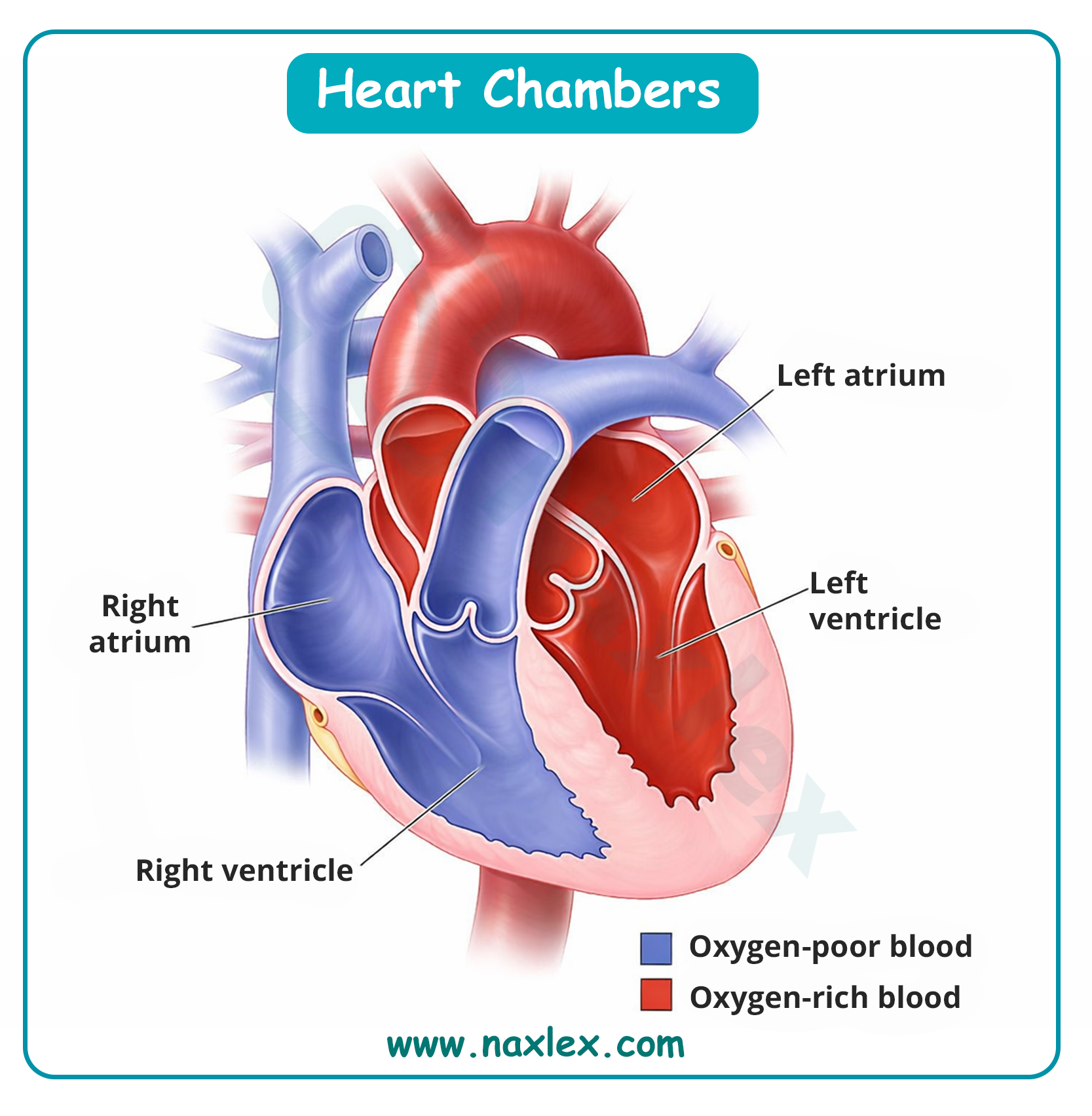
Heart Valves and Locations:
- Tricuspid valve: Located between the right atrium and right ventricle.
- Mitral (Bicuspid) valve: Located between the left atrium and left ventricle.
- Pulmonary valve: A semilunar valve located between the right ventricle and the pulmonary artery.
- Aortic valve: A semilunar valve located between the left ventricle and the aorta.
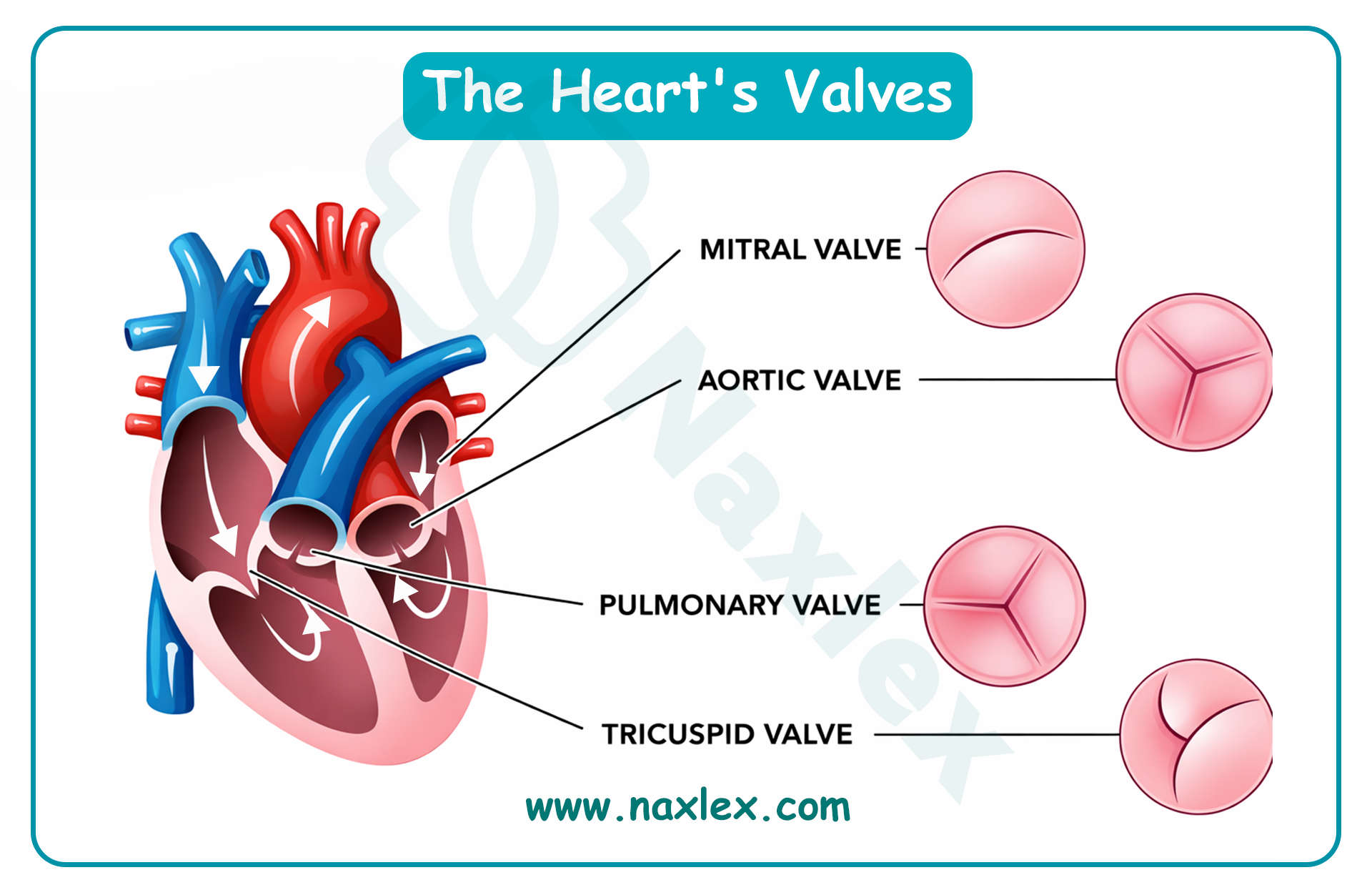
Cardiac Development and Function
- The heart is the first functional organ to develop in the embryo. It begins as a simple tube and starts beating by approximately the twenty-second day of gestation. By the eighth week of pregnancy, the four-chambered structure is complete. In pediatrics, the heart muscle (myocardium) is less compliant and has fewer contractile elements than in adults, making the infant heart very sensitive to "over-stretching" from fluid boluses.
Fetal Circulation
In utero, the lungs are non-functional and filled with fluid. Oxygenation occurs via the placenta. Three unique shunts allow blood to bypass the lungs and liver:
- Ductus venosus: Connects the umbilical vein to the inferior vena cava, allowing oxygenated blood from the placenta to bypass the liver and head straight to the heart.
- Foramen ovale: An opening in the septum between the right and left atria. It allows blood to flow from the right atrium directly to the left atrium, bypassing the non-functional lungs.
- Ductus arteriosus: A vascular bridge between the pulmonary artery and the aorta. It shunts any blood that did enter the right ventricle away from the lungs and into the systemic circulation.
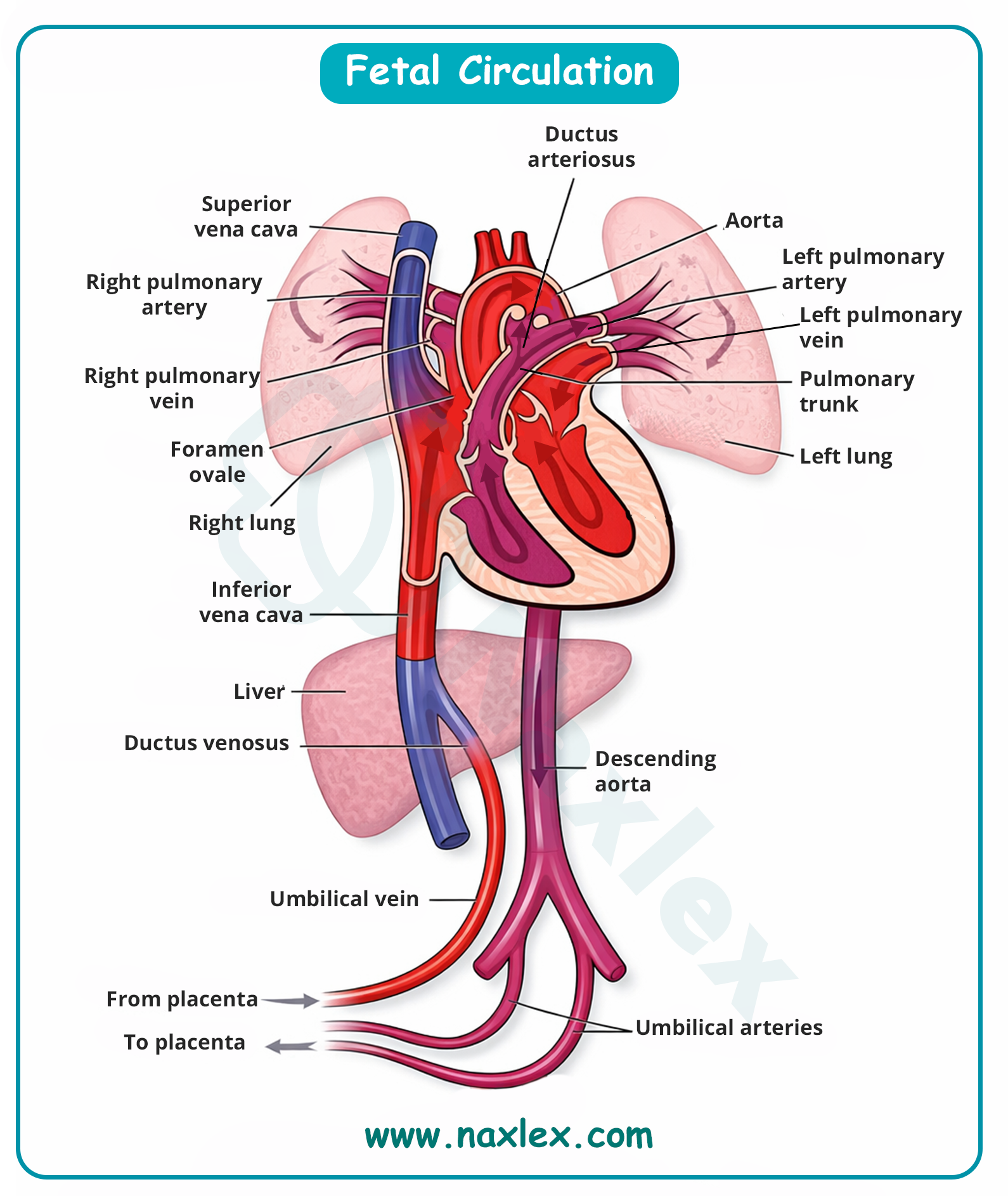
Postnatal Circulation
At birth, several changes occur simultaneously:
- The infant takes their first breath, expanding the lungs and decreasing pulmonary vascular resistance.
- The umbilical cord is clamped, removing the low-resistance placenta and increasing systemic vascular resistance.
- The foramen ovale closes due to increased pressure in the left atrium.
- The ductus arteriosus and ductus venosus constrict and close in response to increased oxygen levels and decreased prostaglandins, eventually becoming ligaments.
Conduction System
The conduction system coordinates the contraction of the heart chambers.
- Sinoatrial (SA) node: Located in the right atrium; it is the "natural pacemaker" that initiates the electrical impulse.
- Atrioventricular (AV) node: Located near the tricuspid valve; it briefly delays the impulse to allow the ventricles to fill with blood completely.
- Atrioventricular bundle (Bundle of His): The electrical bridge between the atria and the ventricles.
- Purkinje fibers: Specialized fibers that spread the impulse rapidly through the ventricular myocardium, causing synchronized contraction.
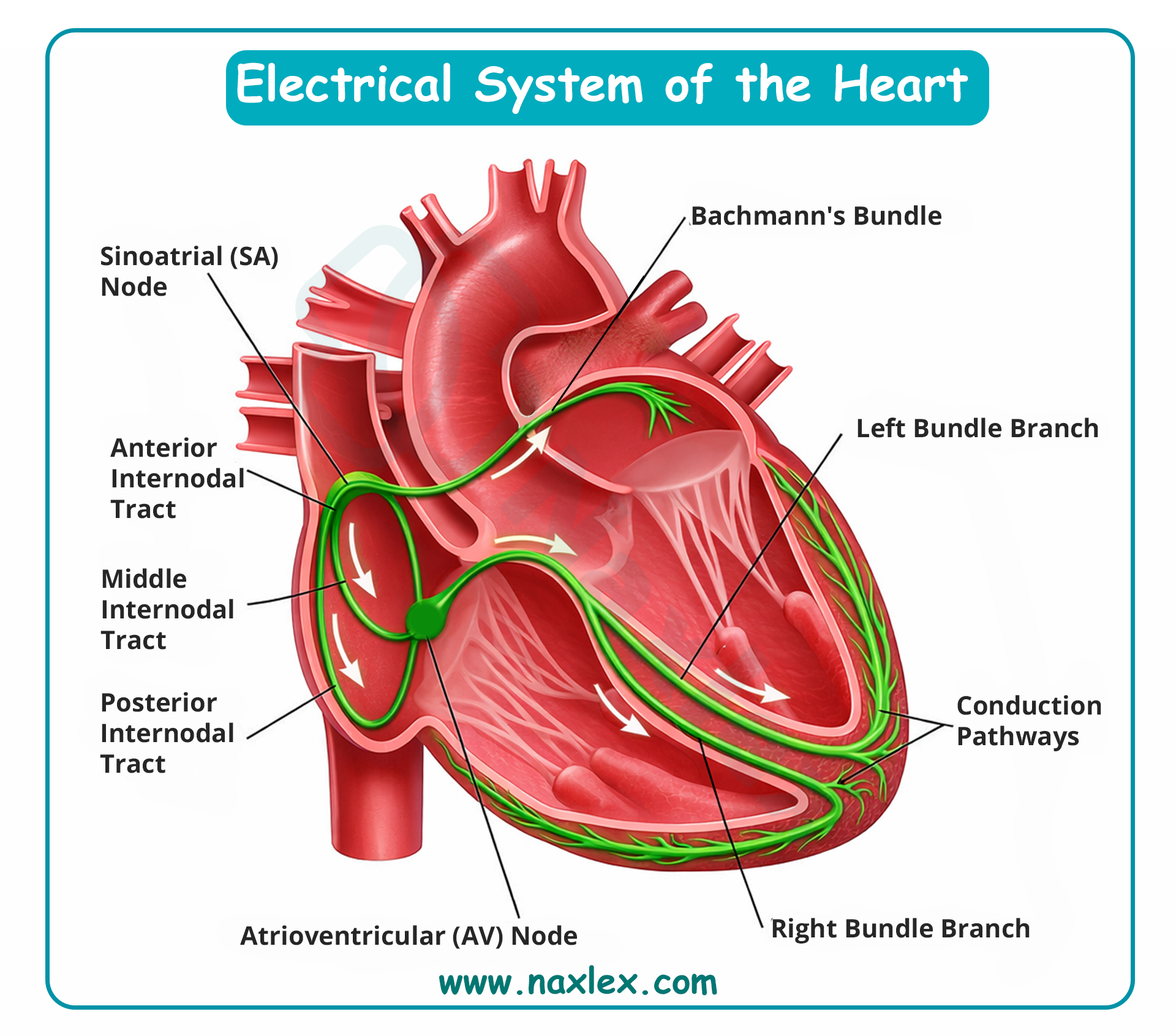
The Cardiac Cycle:
The cycle consists of Diastole (the period of ventricular relaxation and filling) and Systole (the period of ventricular contraction and blood ejection). Coordination between electrical stimulation and mechanical contraction ensures efficient circulation.
Image Title: Cardiac Cycle
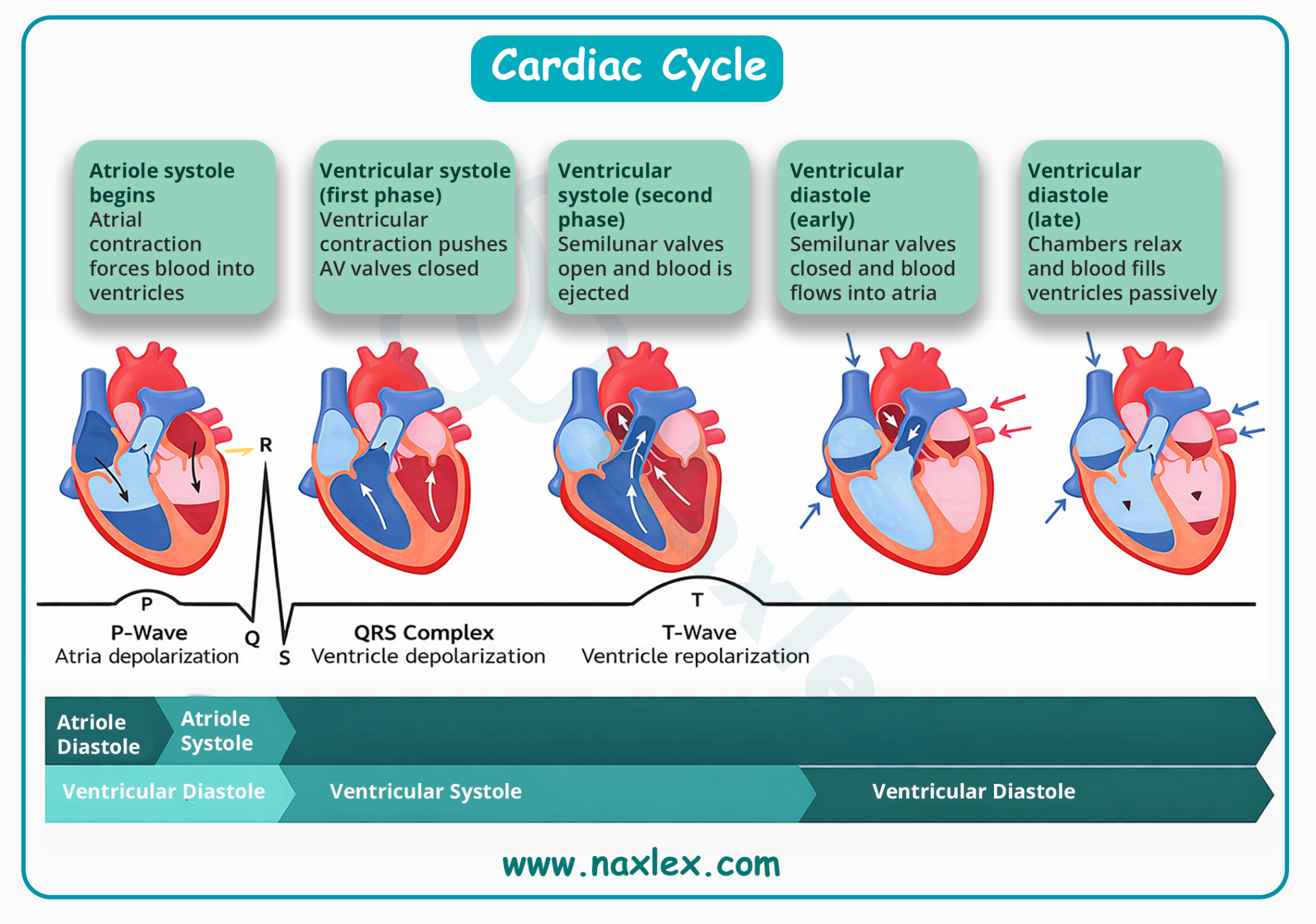
Cardiac Physiology
- Cardiac output: The total volume of blood pumped by the heart per minute. In pediatrics, cardiac output = Heart rate X stroke volume. Since stroke volume is relatively fixed in infants, they must increase their heart rate to increase output.
- Preload: The volume of blood in the ventricles at the end of diastole (the "stretch" before contraction).
- Afterload: The resistance the ventricles must pump against to eject blood into the systemic or pulmonary circulation.
- Stroke volume: The amount of blood ejected by the left ventricle with each single contraction.
- Contractility: The innate ability of the heart muscle to shorten and contract with force, independent of preload or afterload.
- Mean arterial pressure: The average pressure in a patient's arteries during one cardiac cycle. It is considered a better indicator of organ perfusion than systolic blood pressure alone.
Nursing Insight: In pediatric cardiac care, using a blood pressure cuff that is too small will provide a falsely high reading, while a cuff that is too large will provide a falsely low reading. For accurate physiology assessment, the cuff bladder should encircle eighty percent to one hundred percent of the arm circumference.
Cardiac assessment
Health History
A thorough history provides the context for physical findings. Key areas of focus include:
- Prenatal and birth history: Inquire about maternal infections (such as Rubella), diabetes, or exposure to alcohol and medications during pregnancy. Note the infant’s birth weight and any immediate postnatal respiratory distress.
- Feeding patterns: This is the "exercise stress test" for an infant. Poor feeding, taking a long time to finish a bottle (more than thirty minutes), or becoming breathless and sweaty (diaphoresis) during feeds are hallmark signs of cardiac stress.
- Growth and development: Document any failure to thrive or delays in reaching developmental milestones, which may indicate chronic hypoxemia or low cardiac output.
- Family history: Identify any history of sudden unexplained death, congenital heart defects, or early-onset cardiovascular disease in close relatives.
Physical Examination
The physical exam should be performed when the child is quiet and calm, ideally while they are held by a caregiver.
A. Inspection:
- Color: Assess for generalized cyanosis, pallor, or mottling. Distinguish between peripheral cyanosis (acrocyanosis, which can be normal in newborns) and central cyanosis (blue tongue and mucous membranes, which is always abnormal).
- Respiratory effort: Observe for tachypnea, nasal flaring, and retractions, which often accompany heart failure.
- Chest shape: Look for a "precordial bulge," which may indicate chronic cardiac enlargement.
- Clubbing: Inspect the fingertips and toes for rounding and loss of the nail bed angle, signifying chronic hypoxia.
B. Palpation:
- Pulses: Compare the strength and rhythm of the brachial and femoral pulses simultaneously. A significant delay or weakness in the femoral pulse compared to the brachial pulse is a classic sign of coarctation of the aorta.
- Capillary refill time: Press on a central site (such as the sternum) for five seconds; color should return within two to three seconds.
- Hepatomegaly: Palpate the liver margin. In infants, an enlarged liver (more than two centimeters below the right costal margin) is a sensitive indicator of right-sided heart failure.
- Thrills: Feel for palpable vibrations over the precordium, which represent very loud, turbulent blood flow.
C. Auscultation:
- Heart sounds: Identify the first heart sound (S1) “Lubb”. Caused by closure of mitral and tricuspid valves. Best heard at the apex (4th-5th ICS). It marks the beginning of systole. Identify the second heart sound (S2) “Dubb”. Caused by closure of aortic and pulmonic valves. Best heard at the base (2nd ICS). It marks the beginning of diastole. Listen for abnormal sounds like a gallop (S3 or S4) or a "click" indicating valve stenosis.
- Heart rate and rhythm: Listen at the apex for one full minute to detect arrhythmias or "skipped" beats.
Image Tittle: Heart Sounds
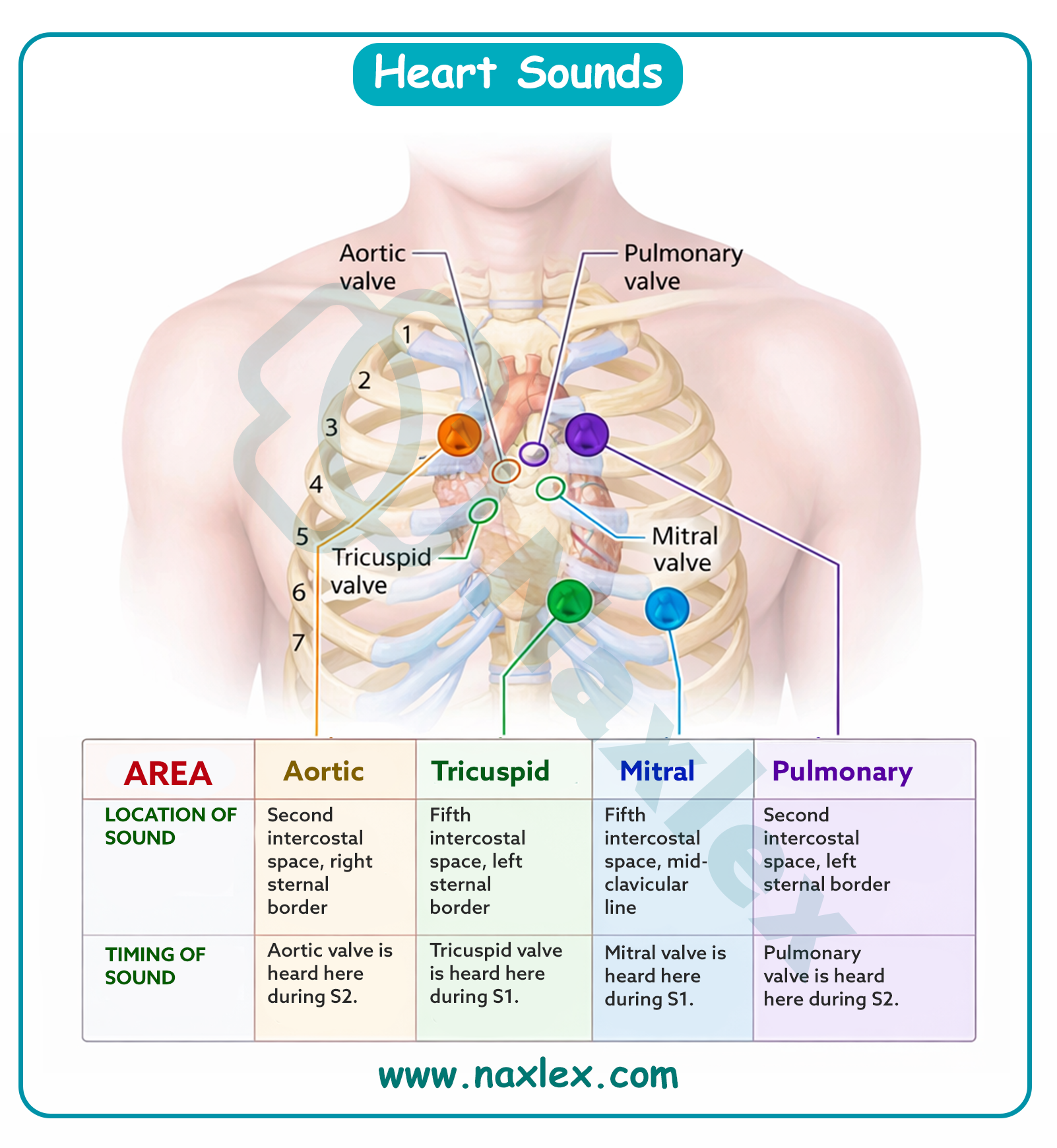
S2 Splitting
- Physiological splitting: Normal. S2 widens on inspiration and closes on expiration.
- Pathological (fixed) splitting: S2 remains split regardless of respiration. This is a hallmark sign of an atrial septal defect (ASD).
Murmurs and Grading
- Murmurs are sounds caused by turbulent blood flow. While many pediatric murmurs are "innocent" (functional), the nurse must document the murmur's timing (systolic or diastolic) and its intensity using the standard grading scale.
|
Grade |
Description |
|
I |
Very faint; only heard after "tuning in" with the stethoscope. |
|
II |
Quiet but clearly audible upon placing a stethoscope on the chest. |
|
III |
Moderately loud; easily heard with no palpable thrill. |
|
IV |
Loud; associated with a palpable thrill. |
|
V |
Very loud; can be heard with only the edge of the stethoscope touching the chest; associated with a thrill. |
|
VI |
Extremely loud; heard with stethoscope off the chest wall; associated with a thrill. |
Nursing Insight: Always assess the "four T's" of pediatric cardiac distress: tachycardia, tachypnea, tiredness (fatigue during feeds), and tummy (enlarged liver).
Common cardiac laboratory and diagnostic tests
Transthoracic Echocardiogram
- Description: A non-invasive test that uses high-frequency sound waves (ultrasound) to create images of the heart's structures.
- Detection: It detects the size of heart chambers, valve function, blood flow patterns, and structural defects such as holes in the septal walls.
- Indications: Suspected heart murmurs, cyanosis, or failure to thrive.
- Discharge teaching: Inform parents the test is painless; however, the child must remain still. If a sedative was used, monitor for sleepiness for several hours.
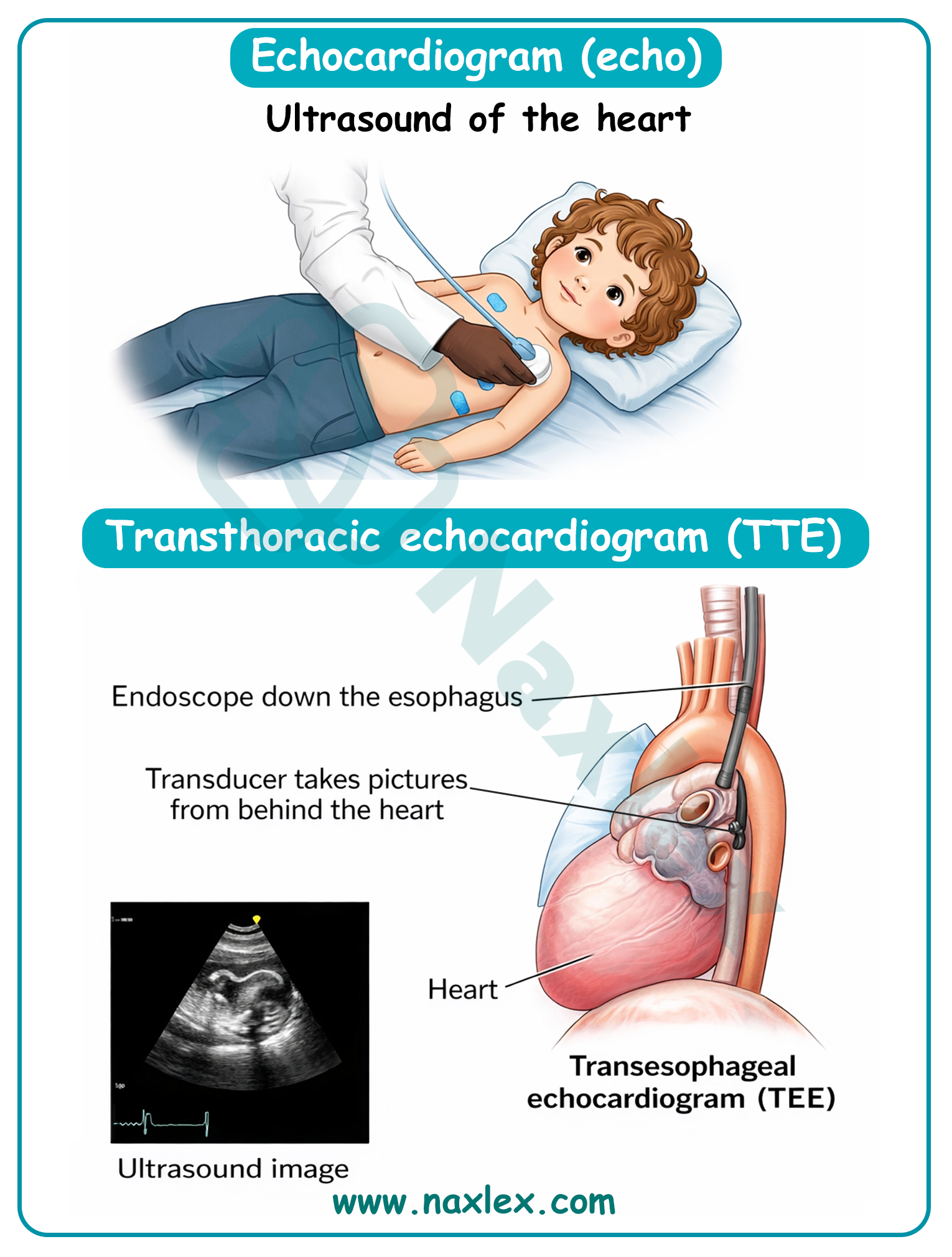
Electrocardiogram
- Description: A non-invasive recording of the electrical activity of the heart via electrodes placed on the chest and limbs.
- The normal ECG consists of the following:
- P wave: Represents the spread of the impulse over the atria (atrial depolarization). The sinus node’s electrical activity is not represented in the ECG.
- P-R interval: Represents the time that elapses from the beginning of atrial depolarization to the beginning of ventricular depolarization. It is termed P-R instead of P-Q because the Q wave is frequently absent.
- QRS complex: Represents ventricular depolarization. It is actually composed of three separate waves, the Q, the R, and the S, that result from the currents generated when the ventricles depolarize before their contraction.
- T wave: Represents ventricular repolarization.
- Q-T interval: Represents ventricular depolarization and repolarization. This interval varies with heart rate; the faster the rate, the shorter the Q-T interval. Therefore, in children this interval is normally shorter than in adults.
- ST segment: Represents the time that the ventricles are in the absolute refractory period, the period between ventricular depolarization and repolarization.
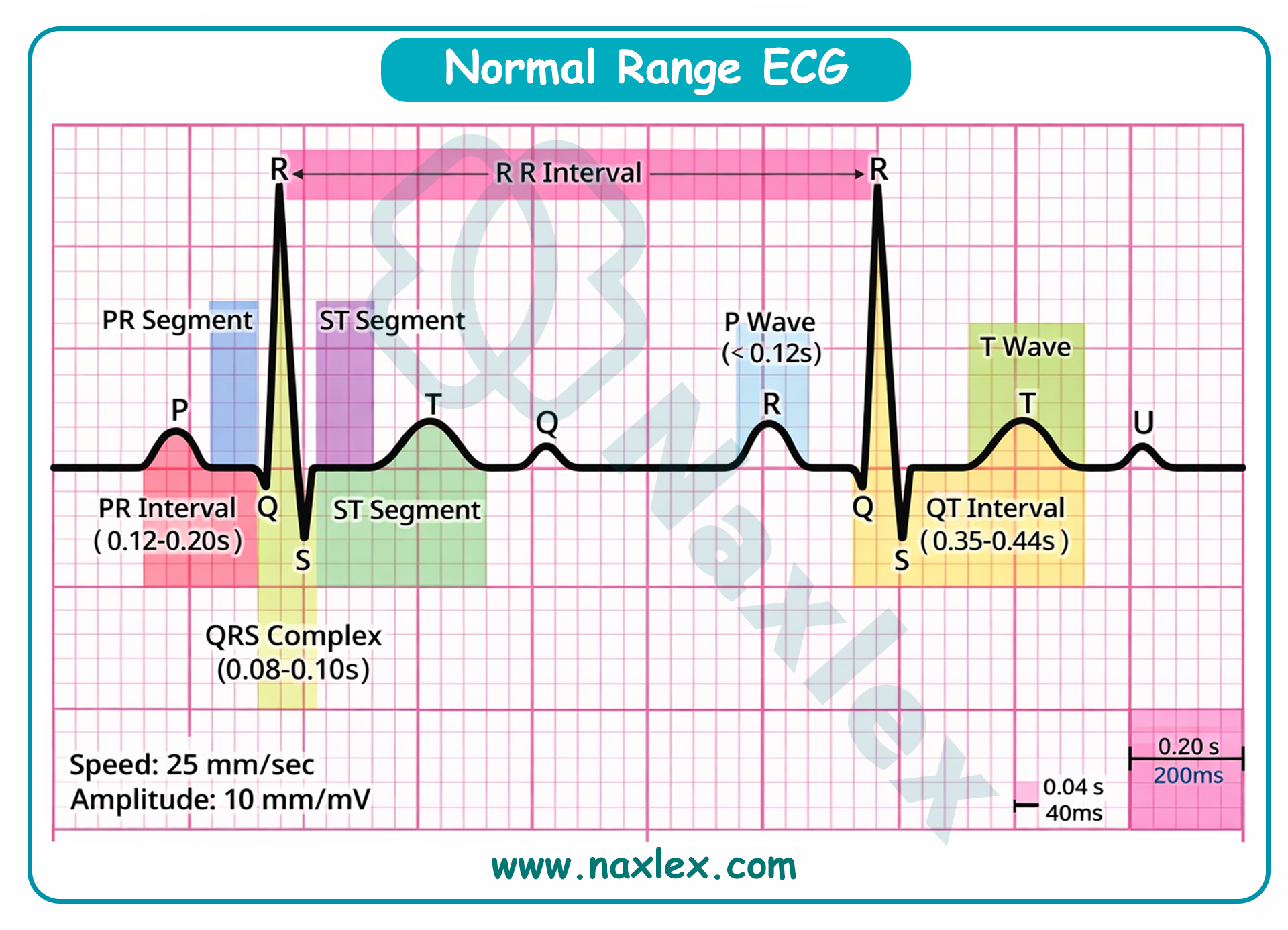
- Detection: It detects heart rate, rhythm disturbances (arrhythmias), and evidence of chamber hypertrophy or conduction delays.
- Indications: Irregular pulse, chest pain, or pre-surgical screening.
- Discharge teaching: Explain that the "stickers" do not hurt, though the adhesive might be cold or slightly uncomfortable during removal.
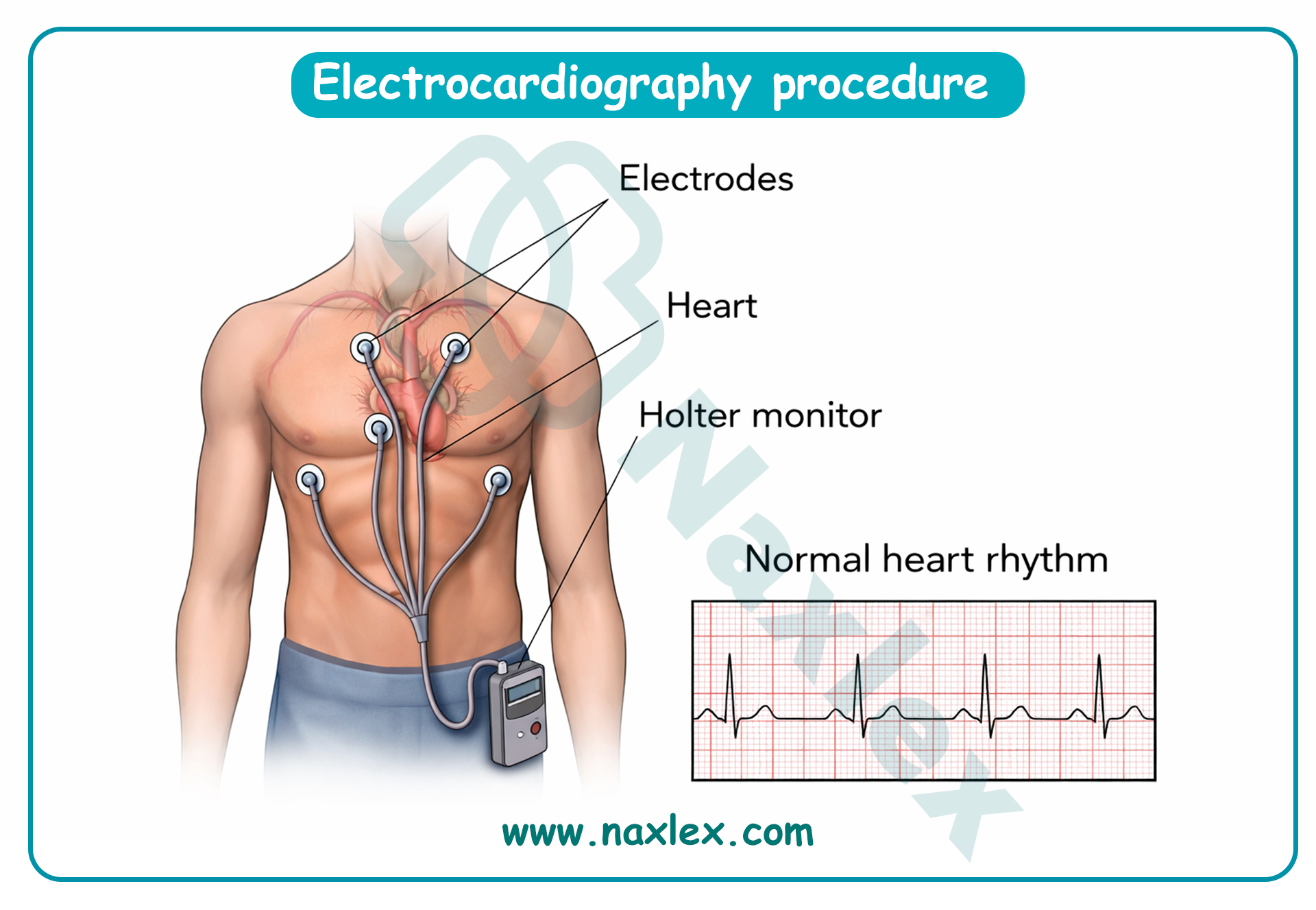
Chest Radiograph (Chest X-Ray)
- Description: A non-invasive imaging technique using ionizing radiation to visualize the chest cavity.
- Detection: It detects heart size (cardiomegaly), heart shape (such as the "boot-shaped" heart in Tetralogy of Fallot), and pulmonary vascular markings.
- Indications: Assessment of heart failure or respiratory distress.
- Contraindications: Pregnancy (in adolescent patients), though rare in pediatrics.
- Discharge Teaching: No special follow-up is required; the radiation dose is minimal.
Ambulatory Electrocardiographic Monitoring (Holter Monitor)
- Description: A non-invasive, portable device that records the heart's electrical activity continuously for twenty-four to forty-eight hours.
- Detection: It detects transient arrhythmias that may not be captured during a standard ten-second electrocardiogram.
- Indications: Palpitations, syncope (fainting), or dizziness.
- Discharge teaching: Instruct the child and parent not to get the device or electrodes wet (no bathing or swimming) and to keep a diary of symptoms.
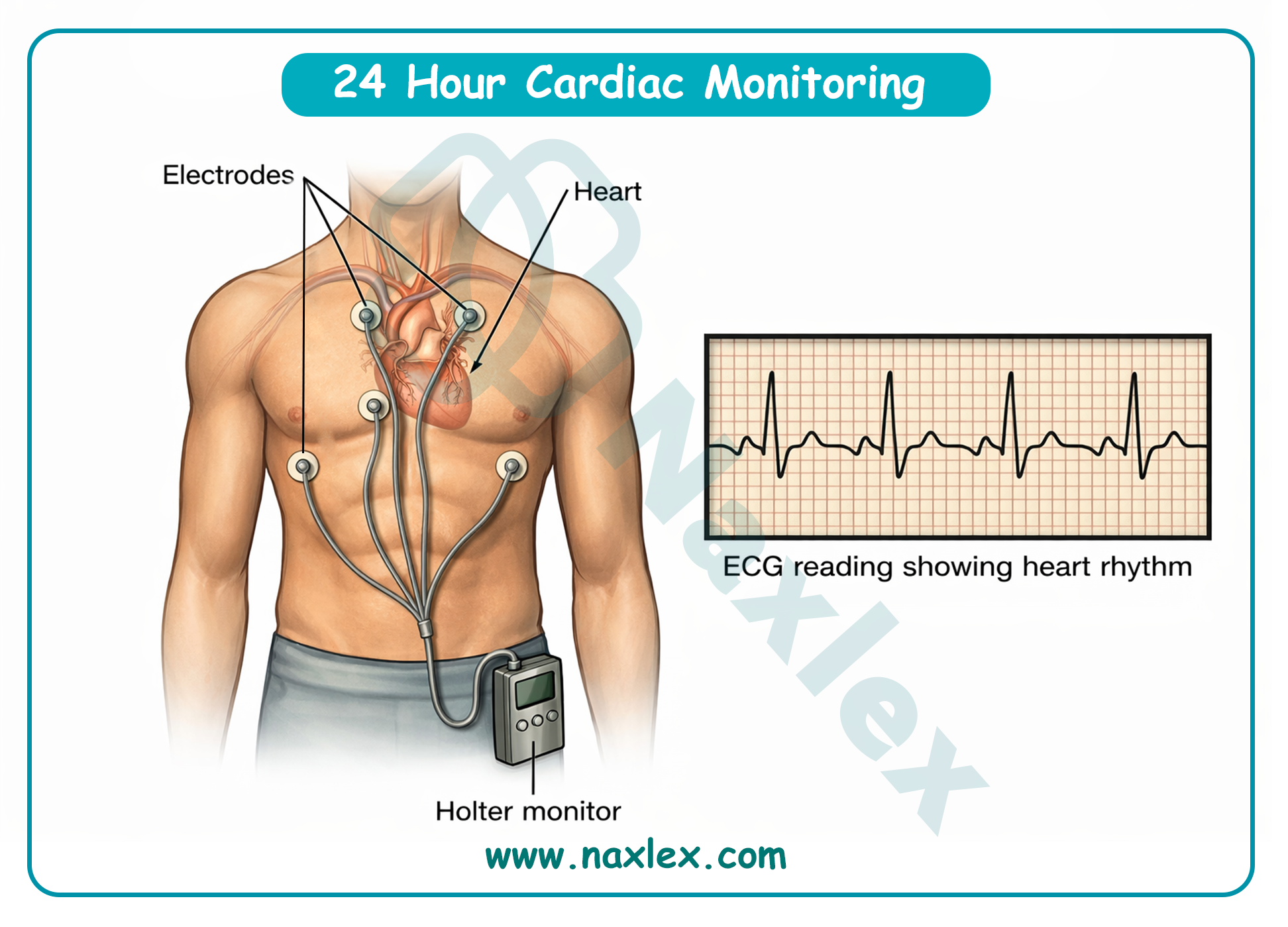
Exercise Stress Test
- Description: A non-invasive procedure where the heart's response to physical exertion is monitored using a treadmill or stationary bicycle.
- Detection: It detects exercise-induced arrhythmias, ischemia, or abnormal blood pressure responses.
- Indications: Assessing exercise tolerance in children with known heart disease or chest pain during activity.
- Contraindications: Severe aortic stenosis, uncontrolled heart failure, or acute myocarditis.
- Discharge teaching: Encourage rest and hydration after the test; report any persistent chest pain or dizziness.
Partial Pressure of Oxygen (PaO2)
- Description: An invasive test (via arterial blood gas) measuring the tension of oxygen dissolved in the arterial blood.
- Detection: It detects the efficiency of gas exchange and the severity of hypoxemia.
- Indications: Severe cyanosis or respiratory distress.
- Contraindications: Compromised peripheral circulation at the puncture site.
- Discharge Teaching: Apply pressure to the site for at least five minutes to prevent bruising or hematoma.
Hemoglobin and Hematocrit
- Description: Laboratory blood tests (invasive via venipuncture) that measure the oxygen-carrying capacity of the blood.
- Detection: It detects anemia or polycythemia (an abnormally high number of red blood cells, common in cyanotic heart disease).
- Indications: Chronic hypoxia or pre-operative assessment.
- Discharge Teaching: Keep the bandage on for several hours; ensure the child drinks plenty of fluids.
Cardiac Enzymes (Troponin and Creatine Kinase)
- Description: Invasive laboratory blood tests that measure proteins released into the bloodstream when heart muscle is damaged.
- Detection: It detects myocardial injury or inflammation (myocarditis).
- Indications: Chest pain, suspected heart muscle infection, or post-cardiac surgery.
- Discharge Teaching: Standard post-venipuncture care.
Arteriogram
- Description: An invasive imaging test where radiopaque contrast dye is injected into the arteries, followed by X-rays.
- Detection: It detects obstructions, narrowing (stenosis), or aneurysms in the blood vessels.
- Indications: Detailed visualization of vascular anatomy prior to surgery.
- Contraindications: Known allergy to contrast dye or iodine; severe renal impairment.
- Discharge Teaching: Monitor the injection site for bleeding and encourage fluid intake to flush the contrast dye from the kidneys.
Cardiac Magnetic Resonance Imaging (MRI)
- Description: A non-invasive but intensive imaging technique using powerful magnets and radio waves to create detailed images.
- Detection: It detects complex structural anatomy and evaluates ventricular function and tissue characteristics.
- Indications: Complex congenital heart defects.
- Contraindications: Permanent metal implants (such as certain pacemakers or clips) and severe claustrophobia.
- Discharge Teaching: If sedation was used, follow standard post-sedation safety protocols.
Cardiac Catheterization
- Cardiac catheterization is an invasive diagnostic and therapeutic procedure in which a thin, flexible tube (catheter) is guided through the vascular system into the heart to evaluate cardiac function or to perform corrective interventions.
Image Tittle: Cardiac Catheterization in a Child
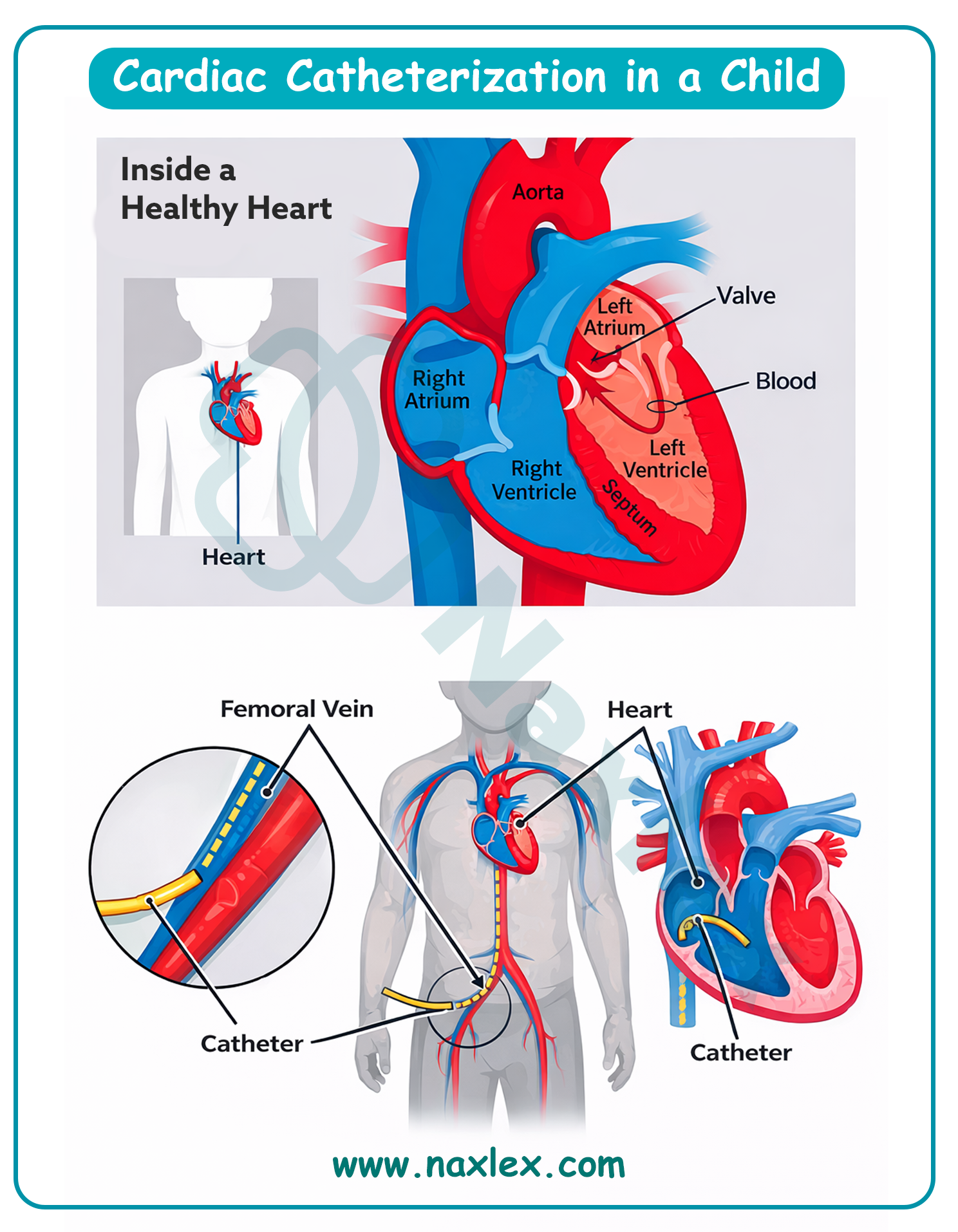
Indications
The purposes of cardiac catheterization are categorized into three primary areas:
- Diagnostic purposes: Used to identify structural defects, measure pressures within the heart chambers, calculate cardiac output, and assess the severity of shunts (the mixing of oxygenated and deoxygenated blood).
- Interventional (therapeutic) purposes: Used to treat defects. Examples include balloon angioplasty to widen a narrowed valve or vessel, stent placement to keep a vessel open, or the use of occlusion devices to plug holes like an Atrial Septal Defect or Patent Ductus Arteriosus.
- Electrophysiologic purposes: Used to map the electrical pathways of the heart to identify the source of arrhythmias and, if necessary, perform radiofrequency ablation to destroy the tissue causing the irregular rhythm.
Types of Diagnostic Cardiac Catheterization
- Right-sided catheterization: The catheter is inserted through a vein (usually the femoral vein) and advanced to the right atrium, right ventricle, and pulmonary artery. This is used to measure pressures in the right heart and pulmonary circulation.
- Left-sided catheterization (Arterial): The catheter is inserted through an artery (usually the femoral artery) and guided against the flow of blood into the aorta and left ventricle. This is used to evaluate the mitral and aortic valves and left ventricular function.
Common Catheter Insertion Sites
- Femoral vein and artery: The most common sites used in pediatrics due to their size and accessibility.
- Antecubital or basilic veins: Occasionally used in older children.
- Umbilical vein or artery: Utilized in the neonatal period (newborns) when these vessels are still patent.
- Jugular vein: Sometimes used for specific right-sided heart access or electrophysiology studies.
Nursing Care Management
Preprocedural Care:
- Assessment: Obtain an accurate height and weight (essential for calculating medication dosages and equipment size). Perform a baseline neurovascular assessment, marking the pedal pulses with a permanent marker to facilitate easy location after the procedure.
- Preparation: Ensure the child is "Nothing by Mouth" (NPO) according to age-specific guidelines to prevent aspiration during sedation.
- Education: Use age-appropriate play therapy or dolls to explain that "special pictures" will be taken of the heart and that a "bandage" will be on their leg afterward.
- Infection screen: Check for any signs of diaper rash if the femoral site is being used, as this may lead to the cancellation of the procedure due to the risk of infection.
Postprocedural Care:
- Positioning: The child must remain in bed with the affected extremity maintained straight for four to six hours to prevent bleeding at the insertion site.
- Monitoring: Vital signs are taken every fifteen minutes for the first hour, then every thirty minutes for the next hour.
- Site assessment: Closely observe the dressing for any signs of bleeding or hematoma (swelling).
- Neurovascular checks: Frequently assess the "Six Ps": Pain, Pallor, Pulses, Paresthesia, Paralysis, and Poikilothermia (temperature). Compare the affected leg to the unaffected leg.
- Hydration: Encourage oral fluids or maintain intravenous fluids to help the kidneys flush out the contrast dye.
Nursing Insight: If bleeding occurs, direct, continuous pressure is applied 2.5 cm (1 inch) above
the percutaneous skin site to localize pressure over the vessel puncture.
Discharge Teaching for Children and Caregivers
- Activity restrictions: Avoid strenuous exercise, contact sports, and heavy lifting for several days (usually three to five days) to allow the vessel to heal.
- Site care: Keep the site clean and dry. Avoid tub baths or swimming for the first two to three days; showers or sponge baths are generally preferred.
- When to call the provider: Instruct parents to seek immediate medical attention if the leg becomes cold, pale, or numb, or if there is redness, warmth, or drainage at the site.
- Medication: Review any new medications, such as low-dose Aspirin, if an occlusion device or stent was placed.
Complications
- Hemorrhage: Bleeding at the entry site, which can be internal (hematoma) or external.
- Loss of Pulse: Can occur due to a clot (thrombosis) or a spasm in the vessel used for access.
- Arrhythmias: The presence of the catheter inside the heart chambers can irritate the heart muscle and cause irregular beats.
- Contrast reaction: Allergic reactions to the iodine-based dye or kidney strain (nephropathy).
- Infection: Though rare, bacteria can be introduced into the bloodstream or the insertion site.
Common cardiac disorders treatments
A. Common Cardiac Medications
Pediatric dosing is highly sensitive and often calculated by weight (mg/kg). Accuracy is the highest priority for the nurse.
|
Medication Class |
Example |
Indications |
Contraindications / Precautions |
Nursing Insights & Side Effects |
|
Cardiac Glycosides |
Digoxin |
Heart Failure, Atrial Tachycardia. Increases contractility. |
Hypokalemia (increases risk of toxicity), bradycardia. |
Check apical pulse for 1 full minute. Hold if HR <90 (infant) or <70 (child). Monitor for vomiting (toxicity). |
|
ACE Inhibitors |
Captopril, Enalapril |
Hypertension, Heart Failure. Reduces afterload. |
Renal failure, pregnancy, hyperkalemia. |
Monitor BP before and after. Side effect: Dry cough or hypotension. |
|
Loop Diuretics |
Furosemide (Lasix) |
Fluid overload, CHF. Reduces preload. |
Anuria, severe electrolyte depletion. |
Monitor Potassium (K+) levels. Low K+ increases Digoxin toxicity risk. |
|
Beta-Blockers |
Propranolol |
Tetralogy of Fallot (Tet spells), arrhythmias. |
Asthma/Bronchospasm (due to bronchoconstriction). |
Monitor HR and BP. Can mask symptoms of hypoglycemia. |
|
Prostins |
Prostacyclin (PGE1) |
Ductal-dependent lesions (e.g., TGA, HLHS). |
Respiratory depression/Apnea. |
Keeps the ductus arteriosus open. Must have intubation equipment at bedside. |
Nursing Insight: When a child is on both digoxin and lasix, the risk for digoxin toxicity is significantly higher because Lasix wastes potassium, and low potassium makes the heart more sensitive to Digoxin.
B. Cardiac Surgery
Surgical interventions are generally categorized based on their intent and the child's physiological readiness:
- Palliative procedures: These are temporary measures used when a child is too small, too weak, or has a complex anatomy that cannot yet support a full repair. The goal is to manage symptoms, adjust pulmonary blood flow, and allow the child to grow.
- Example: The Modified Blalock-Taussig Shunt, which directs blood from a systemic artery to the pulmonary artery to increase oxygenation in cyanotic children.
- Corrective (complete) procedures: These are definitive operations intended to restore normal or near-normal heart anatomy and physiology.
- Example: Closing a ventricular septal defect with a synthetic patch or performing an arterial switch operation for transposition of the great arteries.
Indications for Surgery
Surgery is indicated when a heart defect causes:
- Inadequate oxygenation: Persistent cyanosis or "hypoxic spells" that do not respond to medication.
- Heart failure: Excessive pulmonary blood flow causing pulmonary hypertension and systemic congestion.
- Obstructed blood flow: Narrowing of valves or vessels (such as coarctation of the aorta) that increases the workload on the ventricles.
- Failure to thrive: Inability to gain weight or meet developmental milestones due to the high metabolic cost of a defective heart.
How the Procedure is Performed
Most pediatric cardiac surgeries require a median sternotomy (an incision through the breastbone) to provide full access to the heart.
- Cardiopulmonary bypass: For most corrective repairs, the heart must be stopped and emptied of blood. A "heart-lung machine" takes over the work of the heart (pumping) and the lungs (oxygenating).
- Hypothermia: The child's body temperature is often lowered to decrease metabolic demands and protect the brain and vital organs during the period of bypass.
- Myocardial protection: A cold potassium solution (cardioplegia) is used to arrest the heart and protect the heart muscle while the surgeon performs the repair.
- Decannulation and closure: Once the repair is complete, the child is gradually weaned off the bypass machine, the heart is restarted, and the chest is closed, often leaving chest tubes in place to drain excess fluid and air.
Common Complications
- Low cardiac output syndrome: A period of decreased heart function following bypass, requiring inotropic support (medications to help the heart squeeze). Signs of decreased cardiac output include weak peripheral pulses, hypotension, low urine output, delayed capillary refill, and cool extremities.
- Arrhythmias: Damage or irritation to the conduction system during surgery can cause irregular rhythms, often requiring a temporary pacemaker.
- Postpericardiotomy syndrome: An inflammatory response causing fever and fluid accumulation around the heart (pericardial effusion).
- Hemorrhage: Excessive bleeding from the surgical site or due to the effects of blood-thinning medications used during bypass.
- Neurological deficits: Potential for seizures or developmental delays related to periods of low blood pressure or bypass.
Nursing Insight: In the immediate post-operative period, the nurse must monitor chest tube output hourly. A sudden cessation of drainage is as concerning as an increase; it may indicate a clot in the tube, which can lead to cardiac tamponade characterized by the Beck’s triad the three hallmark clinical signs of cardiac tamponade: hypotension, jugular venous distension, and muffled heart sounds.
Discharge Teachings
- Incision care: Instruct caregivers to keep the incision clean and dry. They should not apply lotions, powders, or ointments until the surgeon gives approval.
- Activity restrictions: Avoid "lifting the child by the armpits" for at least six weeks to allow the sternum to heal. Discourage contact sports and heavy backpacks.
- Infection monitoring: Teach parents to monitor for redness, swelling, warmth, or drainage at the incision site, as well as a fever over 38.3 degrees Celsius.
- Pain management: Review the schedule for acetaminophen or ibuprofen and emphasize that irritability or poor feeding can be signs of pain in infants.
- Immunizations: Discuss the importance of the respiratory syncytial virus vaccine (Palivizumab) and the need for endocarditis prophylaxis (antibiotics) before dental procedures.
Summary
- The pediatric cardiac system is physiologically distinct from the adult system and undergoes major changes at birth. With the first breath, pulmonary resistance decreases, left-sided heart pressures rise, and fetal shunts (foramen ovale and ductus arteriosus) begin to close.
- In infants and young children, cardiac output depends mainly on heart rate rather than stroke volume because the heart is less compliant; therefore, tachycardia is an early sign of stress, while bradycardia can rapidly reduce cardiac output.
- The heart has four chambers supporting pulmonary and systemic circulation, with higher pressures on the left side. Pediatric hearts sit higher in the chest, and the point of maximal impulse is usually at the 4th intercostal space. Fetal circulation bypasses the lungs using specialized shunts, which normally close shortly after birth.
- Cardiac assessment in children follows a systematic approach from history to auscultation. Key history findings include feeding difficulty, poor growth, and activity intolerance. Physical assessment focuses on color, respiratory effort, pulses, liver size, and heart sounds.
- Murmurs are graded by intensity, and fixed splitting of the second heart sound suggests an atrial septal defect. Common diagnostics include echocardiography, ECG, chest radiographs, and cardiac catheterization, the diagnostic gold standard.
- Management includes weight-based medications such as digoxin, diuretics, ACE inhibitors, beta-blockers, and prostaglandins, as well as palliative or corrective cardiac surgery with careful post-operative monitoring and discharge education.
- In pediatric cardiac nursing, the parents are your best resource. If a parent says, "My baby just isn't acting right" or "They are breathing differently during feeds," believe them, it is often the first sign of compensation failure.
Naxlex
Videos
Login to View Video
Click here to loginTake Notes on Pediatric anatomy and physiology of the cardiac system, tests of cardiac function, and common cardiac treatments.
This filled cannot be empty
Join Naxlex Nursing for nursing questions & guides! Sign Up Now


